Potential of Allogeneic Adipose-Derived Stem Cell–Hydrogel ... · ing diabetic foot ulcers....
Transcript of Potential of Allogeneic Adipose-Derived Stem Cell–Hydrogel ... · ing diabetic foot ulcers....

Potential of Allogeneic Adipose-Derived Stem Cell–Hydrogel Complex for Treating Diabetic Foot UlcersKyung-Chul Moon,1 Hyun-Suk Suh,2 Ki-Bum Kim,1 Seung-Kyu Han,1 Ki-Won Young,3 Jin-Woo Lee,4 andMi-Hyung Kim5
Diabetes 2019;68:837–846 | https://doi.org/10.2337/db18-0699
Mesenchymal stem cells (MSCs) may hold greatpromise for treating diabetic wounds. However, it isdifficult for a clinician to use MSCs because they havenot been commercialized. Meanwhile, a new commercialdrug that contains adipose-derived stem cells (ASCs)has been developed. The purpose of this study was toexamine the potential of allogeneic ASC sheets for treat-ing diabetic foot ulcers. Fifty-nine patients with diabeticfoot ulcers were randomized to either the ASC treatmentgroup (n = 30) or a control group treated with polyure-thane film (n = 29). Either an allogeneic ASC sheet orpolyurethane film was applied on diabetic woundsweekly. These wounds were evaluated for a maximumof 12 weeks. Complete wound closure was achieved for73% in the treatment group and 47% in the control groupat week 8. Complete wound closure was achieved for82% in the treatment group and 53% in the control groupat week 12. The Kaplan-Meier median times to completeclosure were 28.5 and 63.0 days for the treatment groupand the control group, respectively. There were no se-rious adverse events related to allogeneic ASC treat-ment. Thus, allogeneic ASCs might be effective and safeto treat diabetic foot ulcers.
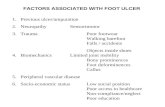
The pathophysiologic relationship between diabetes andimpaired wound healing is complicated. Attenuated ac-tivities of cells that play a key role in wound healingcontribute to the impairment of tissue restoration indiabetic ulcers. Keratinocytes and fibroblasts isolatedfrom diabetic foot ulcers show lower proliferative poten-tial and attenuated growth factor production (1). There-fore, there is considerable interest in the treatment ofdiabetic foot ulcers with biological dressings and/ortissue-engineered products.
Mesenchymal stem cells (MSCs) may hold great promisefor treating diabetic wounds because they have advantagesas allogeneic and autologous cells. MSCs demonstrate lowlevels of immunity-assisted rejection with the ability todivide without apoptosis (2,3). Even after 20 or 30 cycles ofcell doubling in culture, they still retain their initial stemcell properties (4).
Bone marrow stroma has been a main source of MSCs.Previous studies performed by our group have demon-strated that bone marrow–derived MSCs can synthesizehigher amounts of collagen, fibroblast growth factor, andvascular endothelial growth factor in vitro than dermalfibroblasts. Furthermore, they showed greater activity interms of granulation tissue formation, epithelialization,and angiogenesis in vivo, indicating their potential use inaccelerated wound healing (2,5,6). However, there havebeen no commercial drugs that contain bone marrow–derived MSCs to treat diabetic foot ulcers.
Recently, adipose-derived stem cells (ASCs) have beendemonstrated to be one of the main sources of MSCs(7–10). Kato et al. (11) have shown that allogeneic trans-plantation of an ASC combined with artificial skin canaccelerate wound healing in Zucker diabetic fatty ratsin vivo. McLaughlin and Marra (12) demonstrated thatASC sheets can increase wound healing compared withuntreated controls in vivo. Furthermore, ASCs showedgreater activity in terms of epithelialization, angiogenesis,and secretion of growth factors (11). Moreover, a bioengi-neered dermal substitute comprised of allogeneic ASCs hasbeen commercialized to help diabetic wound healing. Thepurpose of this study was to examine the potential ofhydrogel-based allogeneic ASC sheets for treating diabeticfoot ulcers.
1Department of Plastic and Reconstructive Surgery, Korea University Guro Hospital,Seoul, South Korea2Department of Plastic Surgery, Asan Medical Center, Seoul, South Korea3Department of Foot and Ankle Surgery, Eulji Medical Center, Seoul, South Korea4Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul,South Korea5Anterogen Co. Ltd., Seoul, South Korea
Corresponding author: Seung-Kyu Han, [email protected]
Received 25 June 2018 and accepted 17 December 2018
Clinical trial reg. no. NCT02619877, clinicaltrials.gov
K.-C.M. and H.-S.S. contributed equally to this work.
© 2019 by the American Diabetes Association. Readers may use this article aslong as the work is properly cited, the use is educational and not for profit, and thework is not altered. More information is available at http://www.diabetesjournals.org/content/license.
Diabetes Volume 68, April 2019 837
PHARMACOLOGY
AND
THERAPEUTIC
S

RESEARCH DESIGN AND METHODS
This was a randomized, comparator-controlled, single-blind, parallel-group, multicenter study in which patientswith diabetic foot ulcers were recruited consecutively fromfour centers in Korea. This trial was registered withClinicalTrials.gov (clinical trial reg. no. NCT02619877).This clinical study protocol and informed consent docu-ment were also approved by the appropriate InstitutionalReview Board for each participating center and the Foodand Drug Administration (FDA) of Korea (study codeALLO-ASC-DFU-201).
PatientsThe major inclusion criteria were as follows: age between18 and 80 years; patients with type 1 or type 2 diabetes;longer than 4 weeks for the history of ulcer at screening;wound size between 1 and 25 cm2; and wound depth ofWagner grade 1 and 2. Additional criteria were as follows:blood flow around the ulcer was detectable by a Dopplertest, ankle-brachial index range of.0.7 to,1.3, or trans-cutaneous oxygen pressure .30 mmHg. Key exclusioncriteria included a change in wound size of .30% within1 week from screening, wound infection, being HIV pos-itive, HbA1c .15%, and postprandial blood glucoselevel .450 mg/dL.
Once patients were enrolled, they were randomized intoone of two treatment groups. Randomization scheduleswere stratified according to a clinical center using apermuted-block method with a block size of four to sixthrough SAS.
Between November 2015 and October 2016, 24, 11, 12,and 12 patients with diabetic foot ulcers, respectively,from the Korea University Guro Hospital, Eulji GeneralHospital, Asan Medical Center, and the Yonsei UniversitySeverance Hospital were included in this clinical trial. Ofthese 59 subjects, 5 subjects in the control group wereexcluded before the study because of the withdrawal ofconsents and the ineligibility of criteria such as smallwound size (,1 cm2). Therefore, the assessment of a mod-ified intention-to-treat (ITT) set was conducted on dataavailable from the remaining 54 subjects. Five subjects inthe treatment group and five subjects in the control groupwere further excluded before completion of the studybecause of the occurrence of adverse events and protocolviolations such as violation of the timeline. Of the remain-ing 44 subjects, 25 were assigned to the treatment groupand 19 were assigned to the control group. Three subjectsin the treatment group and two subjects in the controlgroup were excluded because of violations of eligibilitycriteria such as high serum glucose levels (.450 mg/dL)during the study period. Therefore, assessment of themodified per-protocol (mPP) set was conducted on dataavailable from the remaining 39 subjects who completedthe study (Fig. 1). Demographics and wound character-istics of subjects in the two groups at baseline are shown inTable 1.
Allogeneic ASC Sheet PreparationAllogeneic ASC sheet (ALLO-ASC-Sheet; Anterogen, Seoul,South Korea) is a 5 3 5 cm hydrogel sheet containingallogeneic ASCs. Briefly, ASCs were obtained from thesubcutaneous fat tissue of healthy donors who providedinformed consent before undergoing liposuction. Obtainedadipose tissues were rinsed with PBS (Hyclone, Logan, UT) inDMEM/Ham’s F-12 (DMEM; Hyclone) containing 0.025%type I collagenase (Invitrogen, Carlsbad, CA) for 80 min at37°C according to the manufacturer protocol. The top lipidlayer was removed, and the remaining liquid portion wascentrifuged at 300g for 10 min at 4°C. The stromal vascu-lar fraction was collected and cultured in DMEM to obtainthe required number of ASCs. ASCs seeded onto thehydrogel matrix were cultured until the number of ASCsreached about 1 3 106 cells/sheet. They were stored fro-zen at 280°C according to the undisclosed manufacturerprotocols.
ASCs were characterized by their expression of stromalcell–associated markers such as CD10, CD13, CD29, CD44,and CD90. These cells were negative for the expression ofhematopoietic stem cell–associated markers (CD34 andCD45). The genomic stability of ASCs was evaluated bykaryotyping analysis. A series of additional efficacy releasetests were performed for the final product, includingconfirmation of the cell count and assessment of cellviability. ASCs were subjected to a series of quality controlsto ensure their purity, safety, and potency that wereapproved by the FDA of Korea.
TechniquesIn the treatment group, the ulcer was cleaned to remove dirtand other debris with 3% hydrogen peroxide followed bysaline solution. The allogeneic ASC sheet, which was storedat 280°C, was thawed at room temperature for 1–2 min,tailored according to the wound size and shape, and applieddirectly to the wound bed as a primary dressing. It was thencovered with a polyurethane foam (Mepilex; MolnlyckeHealth Care, Gothenburg, Sweden) as a secondary dressing.The graft and polyurethane foam were left on the woundfor 7 days. Dressing changes were scheduled at weeklyintervals. If found necessary, the patient returned to thehospital two to three times per week after application ofthe graft so that the wound could be examined. Only thesecondary dressing was changed. In the control group, allconditions including management for diabetic foot ulcerswere set up to be identical to those for the treatmentgroup. A meshed polyurethane film with silicone adhesive(Mepitel; Molnlycke Health Care) was applied as a primarydressing over the wound. It was then covered with thesame secondary dressing used for the treatment group.Visits and dressing changes for the control group werescheduled in the same way as for the treatment group.
All patients with ulcers on weight-bearing sites or sitesotherwise subjected to pressure when wearing shoes hadpressure off-loaded using foam dressings with a hole onthe ulcer site and footwear with cushioning insoles.
838 Stem Cells for Diabetic Ulcers Diabetes Volume 68, April 2019

EvaluationWounds were evaluated weekly until the 12th weekvisit. When the ulcer was completely healed before the12th week visit, treatment was stopped but visits werecontinued as scheduled until week 12 to evaluatelong-term safety. Wound evaluation was performed
in a single-blinded fashion. Patients did not knowwhether or not their wounds had been treated withASC sheets. However, wound evaluators were aware ofthe method of treatment. Photographs were captured atbaseline, follow-up, and the last visit using standard-ized photographic equipment.
Figure 1—A CONSORT diagram illustrating the flow of patients included in this study.
diabetes.diabetesjournals.org Moon and Associates 839

Table 1—Demographic and baseline characteristics of subjects
ParameterTreatment group
(N = 22)Control group
(N = 17)Total
(N = 39) P value
Sex, N (%) Male 14 (63.6) 13 (76.5) 27 (69.3) 0.389*Female 8 (36.4) 4 (23.5) 12 (30.8)
Age, years Mean 6 SD 59.9 6 13.3 68.4 6 9.9 63.6 6 12.5Median 60.5 70.0 66.0 0.034*Min, Max 26.0, 80.0 43.0, 79.0 26.0, 80.0
Smoking history, N (%) Nonsmoker 11 (50.0) 9 (52.9) 20 (51.3) 1.000‡Ex-smoker 6 (27.3) 5 (29.4) 11 (28.2)Smoker 5 (22.7) 3 (17.6) 8 (20.5)
Height, cm Mean 6 SD 167.9 6 11.4 167.3 6 7.3 167.7 6 9.7Median 166.0 167.5 167.0 0.839*Min, Max 143.0, 190.9 152.0, 179.9 143.0, 190.9
Body weight, kg Mean 6 SD 72.9 6 15.7 73.3 6 14.2 73.1 6 14.9Median 68.5 75.0 70.4 0.938*Min, Max 58.0, 124.3 51.6, 101.0 51.6, 124.3
BMI, kg/m2 Mean 6 SD 25.8 6 4.1 26.2 6 5.0 25.9 6 4.5Median 25.4 25.7 25.5 0.787*Min, Max 20.6, 36.3 19.4, 40.5 19.4, 40.5
Glycated hemoglobin A1c at screening visit, % Mean 6 SD 7.9 6 1.6 8.1 6 1.7 8.0 6 1.6Median 7.9 8.0 8.0 0.739*Min, Max 5.3, 10.5 5.5, 10.9 5.3, 10.9
Postprandial blood glucose atscreening visit, mg/dL Mean 6 SD 193.0 6 96.5 208.5 6 94.8 199.7 6 94.8
Median 144.0 165.0 163.0 0.618*Min, Max 65.0, 369.0 91.0, 445.0 65.0, 445.0
Serum albumin at screening visit, g/dL Mean 6 SD 4.1 6 0.4 4.1 6 0.3 4.1 6 0.4Median 4.1 4.1 4.1 0.988*Min, Max 3.3, 5.3 3.7, 4.9 3.3, 5.3
Diabetes duration, months Mean 6 SD 205.7 6 128.0 239.7 6 117.3 220.5 6 123.0Median 186.0 234.0 191.0 0.399*Min, Max 1.0, 496.0 72.0, 433.0 1.0, 496.0
Diabetes type, N (%) Type 1 1 (4.5) 0 (0) 1 (2.6) 1.000‡Type 2 21 (95.5) 17 (100) 38 (97.4)
Eye disorders, N (%) Yes 13 (59.1) 9 (52.9) 22 (56.4) 0.701§No 9 (40.9) 8 (47.1) 17 (43.6)
Renal disorder, N (%) Yes 7 (31.8) 10 (58.8) 17 (43.6) 0.092§No 15 (68.2) 7 (41.2) 12 (56.4)
Cardiovascular disorder, N (%) Yes 18 (81.8) 16 (94.1) 34 (87.2) 0.363‡No 4 (18.2) 1 (5.9) 5 (12.8)
Neuropathy history, N (%) Yes 13 (59.1) 11 (64.7) 24 (61.5) 0.721†No 9 (40.9) 6 (35.3) 15 (38.5)
Duration of diabetic foot ulcers, months Mean 6 SD 6.7 6 11.0 10.2 6 23.3 8.2 6 17.3Median 3.0 3.0 3.0 0.875†Min, Max 1.0, 52.0 1.0, 99.0 1.0, 99.0
Wagner grade, N (%) Grade 1 14 (63.6) 11 (64.7) 25 (64.1) 0.945§Grade 2 8 (36.4) 6 (35.3) 14 (35.9)
Ulcer location, N (%) Right 13 (59.1) 8 (47.1) 21 (53.8) 0.455§Left 9 (40.9) 9 (52.9) 18 (46.2)
Dorsal 11 (50.0) 12 (70.6) 23 (59.0) 0.195§Plantar 11 (50.0) 5 (29.4) 16 (41.0)Forefoot 20 (90.9) 11 (64.7) 31 (79.5) 0.068‡Midfoot 1 (4.5) 1 (5.9) 2 (5.1)Hindfoot 1 (4.5) 5 (29.4) 6 (15.4)
Wound size, cm2 Mean 6 SD 2.0 6 0.9 2.8 6 2.0 2.3 6 1.5Median 1.7 1.8 1.8 0.335†Min, Max 1.0, 4.5 1.1, 7.6 1.0, 7.6
Continued on p. 841
840 Stem Cells for Diabetic Ulcers Diabetes Volume 68, April 2019

The mPP population was used for primary and second-ary efficacy analysis in this study. The modified ITTpopulation was used for the safety analysis and summariesthat included all subjects who were treated with ASCsheets and had visited the clinic at least once.
Primary efficacy criterion was the percentage of subjectswho achieved complete wound closure within the 8-weekstudy period. Secondary efficacy criteria were the pro-portion of subjects who achieved complete wound closurewithin the 12-week study period, the time required forcomplete wound closure in patients who achieved com-plete healing within 12 weeks, the rate of wound sizereduction from baseline, and the proportion of subjects byWagner grade at each week. In addition, post hoc analyseswere performed to evaluate the efficacy of the treatmentand prognostic factors such as wound depth and location.Wound size was determined using a Visitrak DigitalPlanimetry Wound Measurement System (Smith &Nephew, Hull, U.K.).
For the safety study, information on adverse events,adverse drug reactions, serious adverse events, and seriousadverse drug reactions was collected at each visit. Safetywas also monitored at indicated timepoints by evaluatingadverse event reports, laboratory assessments, and vitalsigns. A systematic immunologic study was conducted todetect anti-HLA panel reactive antibodies at baseline, the1st week, and the 12th week after ASC treatment.
Ulcer recurrence and adverse events of healed ulcerswere monitored for 2 years after healing by reviewingmedical records and/or through telephone interviews. Thisfollow-up study was registered with ClinicalTrials.gov(clinical trial reg. no. NCT03183804) and the FDA of Korea(study code ALLO-ASC-DFU-202).
Statistical AnalysesBased on previous studies (13,14), the number of subjectswas calculated in this study. The weighted complete heal-ing was the sum of number of subjects with completehealing in each study divided by the sum of the number ofsubjects used in each study. The weighted complete healingwas 0.81 in the treatment group and 0.45 in the controlgroup. The following values were used to calculate thenumber of subjects: type I error (a) = 5%, power of test =
80%, complete healing rate in the treatment group = 0.81,and complete healing rate in the control group = 0.45.Where each complete healing rate was pt for the treatmentgroup and pc for the control group, the two-sided nullhypothesis and alternative hypothesis were as follows: nullhypothesis, pt = pc; alternative hypothesis, pt � pc.
In this study, Z0.975 was 1.96 and Z0.80 was 0.84.Therefore, the number of subjects in each group couldbe calculated as follows (15):
N ¼�Z12a=2 þ Z12b
�2nptð12 ptÞ þ pcð12 pcÞo
fðpt 2 pcÞ2 ∂g2
¼ð1:96þ 0: 84Þ2
n0:81ð12 0:81Þ þ 0:45ð12 0:45Þ
o
fð0:812 0:45Þ2 0g2¼ 24:28
Considering a dropout rate of broadly 10%, the number ofsubjects in each group was 26.97 (= 24.28/(12 0.10)), anda sample size of 54 (= 27 3 2) randomly assigned subjectswas required. Based on our experience from previousclinical trials for treating diabetic foot ulcers, ;10% ofsubjects experienced unexpected events related to diabetes-related complications and high-risk comorbidities. There-fore, we added another 10% of subjects, bringing the totalnumber of subjects enrolled in this study to 59.
Pearson x2 test was used to evaluate the proportion ofsubjects who achieved complete wound closure and thesafety set. Log-rank test and independent t test or Wil-coxon rank sum test were used to evaluate the timerequired for complete closure and the rate of woundsize reduction, respectively. The median time to completeclosure was also estimated using the Kaplan-Meiermethod. A P value,0.05 was considered to be statisticallysignificant.
RESULTS
The proportion of subjects achieving complete woundclosure at week 8 in the treatment group was 73%(16 of 22 subjects). It was 47% (8 of 17 subjects) in thecontrol group (P = 0.102).
Table 1—Continued
ParameterTreatment group
(N = 22)Control group
(N = 17)Total
(N = 39) P value
Cause of ulcer, N (%) Trauma 1 (4.5) 0 (0.0) 1 (2.6) 0.523‡Pressure by shoes 16 (72.7) 12 (70.6) 28 (71.8)
Unknown 3 (13.6) 1 (5.9) 4 (10.3)Others 2 (9.1) 4 (23.5) 6 (15.4)
Amputation history, N (%) Toe 10 (45.5) 3 (17.6) 13 (33.3) 0.068§Total 11 (50.0) 4 (23.5) 15 (38.5) 0.092§
Surgical history of target site, N (%) Yes 14 (63.6) 8 (47.1) 22 (56.4) 0.301‡No 8 (36.4) 9 (52.9) 17 (43.6)
Max, maximum; Min, minimum. *Independent t test. †Wilcoxon rank sum test. ‡Fisher exact test. §Pearson x2 test.
diabetes.diabetesjournals.org Moon and Associates 841

For results of secondary efficacy criteria, the proportionof subjects achieving complete wound closure at week 12 inthe treatment group was 82% (18 of 22 subjects) and 53%(9 of 17 subjects) in the control group (P = 0.053). Themean time required for complete wound closure was40.8 6 5.3 days in the treatment group and 51.2 63.9 days in the control group. The Kaplan-Meier mediantime to complete wound healing was 28.5 days for thetreatment group and 63.0 days for the control group (P =0.033) (Fig. 2). The rate of wound size reduction at week1 was 49.6 6 25.7% in the treatment group and 23.0 632.2% in the control group (P = 0.007). The rate of woundsize reduction was also statistically significant between thetwo groups at 9 of 12 study weeks (Fig. 3). Post hocanalyses were performed to further explore other prog-nostic factors such as baseline wound depth and locationthat might affect the efficacy of the treatment (Fig. 4 andTables 2 and 3).
Incidence rates of adverse events are shown in Table 4.None of these events were related to study dressings.There were no significant differences between the twogroups. The incidence of serious adverse event was similarbetween the treatment and control groups. Cellulitis onuntargeted sites, paresthesia, uncontrolled diabetes, andcardiac arrest occurred as serious adverse events. However,none of these serious adverse events was considered to berelated to the treatment. No other serious adverse eventswere found in either group. No clinically meaningfulchanges from baseline clinical and laboratory parameters,including serum chemistry, hematology, urinalysis, andvital signs, occurred in any of these patients.
In the systematic immunologic study, 16 subjects (11 inthe treatment group and 5 in the control group) showedanti-HLA antibodies .1,500 fluorescence intensity valuesat the 1st week and the 12th week. Among these subjects,
three (27%) in the treatment group and one (20%) in thecontrol group showed a slight elevation of antibodies at the12th week. However, we observed no obvious clinical signsof rejection such as erythema, local inflammatory signs, orvisible signs of necrosis, as described in previous studies(16,17), in these subjects.
Ulcer recurrences and adverse events in healed ulcerswere successfully monitored for 2 years for 16 subjects inthe treatment group and 8 subjects in the control group.We reviewed the medical records of subjects who attendedroutine appointments for seven subjects in the treatmentgroup and six subjects in the control group. Nine subjectsin the treatment group and two subjects in the controlgroup were interviewed over the telephone. Two subjectsin the treatment group and no subjects in the control
Figure 2—Kaplan-Meier diagram showing results on the time to wound closure.
Figure 3—Rate of wound size reduction from baseline over time.
842 Stem Cells for Diabetic Ulcers Diabetes Volume 68, April 2019

group showed ulcer recurrence 6 months after completionof the trial, but these ulcers that recurred eventuallyhealed. We noted no adverse events related to wounddressings in either group for 2 years after completion ofthe trial.
DISCUSSION
The development of advanced wound-healing technologyhas triggered the use of cells to overcome the limitations ofconventional methods. Various commercially available al-logeneic cell-scaffold complexes have been developed andwidely used for treating diabetic foot ulcers (18–21). Re-cently, a new bioengineered dermal substitute composed ofcultured autologous fibroblasts seeded on a hyaluronic acid
sheet (Hyalograft 3D; ChaBio & Diostech, Seoul, SouthKorea) was developed. However, in several cases, autolo-gous primary cells are not accessible or are unavailable insufficient numbers because they may not have enoughproliferative capacity for treatment in patients with di-abetes due to cellular senescence in the presence of highglucose concentrations (22–24).
Therefore, stem cells may hold great promise foraddressing the need for viable cell sources, and MSCshave attracted much attention in the bioengineering field.The therapeutic potential of allogeneic ASCs has beenwidely explored (11,12,25–27). However, most of thesestudies are in vitro or in vivo studies. Our study might bethe first report demonstrating the efficacy of a commer-cially available allogeneic ASC in a scaffold for treatingdiabetic foot ulcers. Cultured ASCs are derived from anunrelated allogeneic donor. They can be stockpiled. A cellbank enables large-scale production, and an ASC sheet canbe stored at 280°C. It is stable for 12 months. Theallogeneic ASC sheet can maintain cell viability and po-tency up to 1 year and sustain its specifications duringtransport and storage. The sheet is available immediatelyand is convenient to use for physicians and patients.Unlike autologous ASCs, no biopsy is necessary. Patientsdo not need to wait for cells to be processed. The ASC sheetis nearly ready-made when the patient arrives at the clinic.
Figure 4—Proportion of Wagner grade at every visit week.
Table 2—Proportion of subjects with complete woundclosure at weeks 8 and 12 by baseline Wagner grade
BaselineWagner grade
Treatment group, n/N(%) (N = 22)
Control group, n/N(%) (N = 17)
Week 8Grade 1 11/14 (78.6) 7/11 (63.6)Grade 2 5/8 (62.5) 1/6 (16.7)
Week 12Grade 1 12/14 (85.7) 8/11 (72.7)Grade 2 6/8 (75.0) 1/6 (16.7)
diabetes.diabetesjournals.org Moon and Associates 843

Prior to this phase II clinical trial study, a phase I trialwas carried out to evaluate early safety of the treatment.For the phase I trial, five subjects were enrolled. There wasno adverse event. Complete wound closure was achievedfor all subjects within 8 weeks (unpublished observations).This phase II clinical trial involving allogeneic ASC prod-ucts also showed promising results. At the 8th and 12th
weeks after the treatment, more subjects in the treatmentgroup had complete wound healing compared with thosein the control group. Statistically, there were borderlinedifferences. Other parameters demonstrated statisticallysignificant differences. In detail, the mean time to com-plete wound healing was shorter for the treatment groupcompared with that for the control group (P = 0.033). Therate of wound size reduction was also statistically signif-icant between the two groups at 9 of 12 weeks of studyperiod. The results of post hoc analyses indicated thatmore subjects with Wagner grade 2 in the treatment groupachieved complete wound closure compared with those inthe control group.
The results of the 2-year follow-up study showed thatulcers recurred in two subjects in the treatment group6 months after completion of the trial, although their ulcerlocations were the toe tip and the plantar foot, areas thatare vulnerable to pressure. Therefore, ulcer recurrencemight not have been related to the ASC treatment. Inaddition, we observed no adverse events related to thetreatment for 2 years after completion of the study.
The exact mechanism of action of allogeneic ASCsremains unknown. They might be able to exert their effectsthrough several mechanisms, including the release ofvarious growth factors such as vascular endothelial growthfactor, hepatocyte growth factor, transforming growthfactor-b1, insulin-like growth factor-1, epithelial growthfactor, and keratinocyte growth factor to promote angio-genesis, collagen synthesis, and epithelialization (11).ASCs may produce extracellular matrix proteins, induceproliferation of native fibroblasts, protect cells from a nox-ious environment to aid in wound healing, and enhancethe regeneration of new tissue. In addition, ASCs have ananti-inflammatory effect by inhibiting T-cell activation,thereby inhibiting the cellular signaling pathway of im-mune cells and resulting in decreased inflammatory mol-ecules such as tumor necrosis factor-a and interferon-g. Acombination of these processes is likely to be involved intheir action mechanisms (11,27,28).
Diabetic foot ulcers present a difficult treatment prob-lem because the pathophysiology of the condition involvesmultiple factors such as peripheral neuropathy, peripheralvascular disease, repetitive trauma or pressure, and super-imposing foot infection. However, many diabetic footulcers are delayed or fail to heal despite standard treat-ment such as debridement, infection control, pressure off-loading, and lower extremity revascularization because ofattenuated activities of cells contributing to wound heal-ing. In patients with diabetes, delayed wound healing mayresult in serious complications such as osteomyelitis andmajor/minor amputation (29–32); the longer the ulcerpersists, the greater the possibility that serious complica-tions will develop in the patient that can lead to hospi-talization, and delayed wound healing may increasemedical, economic, and social burdens. Therefore, effortsto reduce the time to complete wound closure are impor-tant for treating diabetic foot ulcers. In the current study,
Table 3—Proportion of subjects with complete woundclosure by wound location at week 12
LocationTreatment group, n/N (%)
(N = 22)Control group, n/N (%)
(N = 17)
Dorsal 4/4 (100.0) 3/6 (50.0)
Plantar 7/11 (63.6) 0/5 (0.0)
Border 3/3 (100.0) 6/6 (100.0)
Tip 4/4 (100.0)
Total 18/22 (81.8) 9/17 (52.9)
Table 4—Adverse events in treatment and control groups
Treatmentgroup, n (%)(N = 30 )
Control group,n (%)
(N = 24)P
value*
Abdominal pain 1 (3.3) 0 (0.0) 1.000
Back pain 0 (0.0) 1 (4.2) 0.444
Blood pressureincreased 1 (3.3) 0 (0.0) 1.000
Cardiac arrest 1 (3.3) 0 (0.0) 1.000
Cellulitis 0 (0.0) 2 (8.3) 0.193
Constipation 0 (0.0) 1 (4.2) 0.444
C-reactive proteinincreased 0 (0.0) 1 (4.2) 0.444
Diabetes inadequatecontrol 1 (3.3) 0 (0.0) 1.000
Diabetic neuropathy 1 (3.3) 0 (0.0) 1.000
Dizziness 1 (3.3) 0 (0.0) 1.000
Dyspnea 1 (3.3) 0 (0.0) 1.000
Hyperglycemia 1 (3.3) 2 (8.3) 0.579
Hyperkalemia 0 (0.0) 1 (4.2) 0.444
Nasopharyngitis 0 (0.0) 1 (4.2) 0.444
Nephropathy 0 (0.0) 1 (4.2) 0.444
Edema 1 (3.3) 0 (0.0) 1.000
Osteoporosis 1 (3.3) 0 (0.0) 1.000
Pain in extremity 2 (6.7) 1 (4.2) 1.000
Paresthesia 1 (3.3) 2 (8.3) 0.579
Pleural effusion 0 (0.0) 1 (4.2) 0.444
Proteinuria 1 (3.3) 0 (0.0) 1.000
Pyelonephritis acute 1 (3.3) 0 (0.0) 1.000
Pyrexia 0 (0.0) 1 (4.2) 0.444
Trigger finger 1 (3.3) 0 (0.0) 1.000
*Fisher exact test.
844 Stem Cells for Diabetic Ulcers Diabetes Volume 68, April 2019

subjects in the treatment group showed significantly fastercomplete wound closure than did those in the controlgroup (P = 0.033). This study suggested that the time tocomplete wound closure could be reduced simply byapplying allogeneic ASC sheets in patients with diabetes.This is the key highlight of our study.
In this study, the follow-up duration was 12 weeksbecause many previous similar clinical trials for diabeticwound healing also used 12 weeks for the follow-upduration (13,14,18,32–35). For precise assessment ofthe efficacy of the allogeneic ASC treatment, we excludedexternal confounding factors that could have affected thetreatment such as vascular insufficiency and infection.Therefore, 12 weeks might be enough to assess the timeto complete wound closure in patients with diabetes afterstandardized diabetic foot ulcer management. It is impor-tant to emphasize that allogeneic ASC treatment must beused along with other standard principles of diabetic footulcer management, including debridement, infection con-trol, pressure off-loading, and revascularization (21,36).Without adhering to these important principles, addingan active adjunctive modality is unlikely to result inimproved healing rates. Patients with diabetic foot ulcerswho do not exhibit significant signs of wound healingdespite good metabolic control, acceptable vascularity(transcutaneous oxygen pressure .40 mmHg), adequatepressure off-loading, and absence of infection might begood responders to allogeneic ASC treatment.
The current study has some limitations. First, ourstudy had all the limitations inherent in a phase II trial.For example, the sample size was relatively small al-though the number of subjects was determined by powercalculation. Although acknowledging the implications ofmultiplicity adjustments was important for helping tointerpret the trial results, we did not consider correctingthe additional significance level using adjustment for ainflation because multiplicity adjustments may not benecessary in exploratory trials (37,38). Among the param-eters of this study, differences in the proportion ofsubjects with complete wound closure were statisticallyat borderline. Furthermore, the percentage of subjectswith a history of amputation, a risk factor for replication,in the treatment group was more than two times that inthe control group. On the contrary, more older subjectswere enrolled in the control group compared with thetreatment group. Therefore, a phase III trial study shouldbe followed with large sample size of subjects to establishthe effect of allogeneic ASCs with certainty. Second,wound evaluation was performed in a single-blind fash-ion. Wound evaluators knew whether or not patientswere in the ASC-treated group, which might have affectedthe results. However, this was unavoidable because thewound evaluators could discriminate between ASC sheetsand polyurethane films. Therefore, it was difficult toconduct a double-blind design in this study. To increasetransparency, our design included careful checks ofthe extent to which evaluators were blinded to group
allocation. Third, further studies are necessary to de-termine the optimal interval for ASC application. Theapplication of ASCs more frequently than once a weekmight reduce the time to healing.
In summary, the results of this study showed that anallogeneic ASC sheet might be effective and safe to treatnonischemic diabetic foot ulcers without infection.
Acknowledgments. The authors thank all patients and health careprofessionals who contributed to make the trial possible. In addition, the authorsthank the investigators for their commitment, time, and effort.Funding and Duality of Interest. This study was supported by grantsfrom Anterogen (Seoul, South Korea) and the Ministry of Health & Welfare, Republicof Korea (grant HI16C1037). This research also was supported by a grant from theKorea Health Technology R&D Project through the Korea Health Industry De-velopment Institute. No other potential conflicts of interest relevant to this articlewere reported.Author Contributions. K.-C.M. had direct access to original data,interpreted the data, critically revised the draft of the manuscript, wrote the finalversion of the manuscript, and approved the final manuscript. H.-S.S. had directaccess to original data; contributed to data recording; identified, treated, andmonitored study participants; critically revised the draft of the manuscript; andapproved the final manuscript. K.-B.K. had direct access to original data,contributed to data analyses and handling, critically revised the draft of themanuscript, and approved the final manuscript. S.-K.H. coordinated the work; haddirect access to original data; contributed to data recording; interpreted the data;identified, treated, and monitored study participants; critically revised the draft ofthe manuscript; and wrote and approved the final version of the manuscript.K.-W.Y. and J.-W.L. identified, treated, and monitored study participants; haddirect access to original data; contributed to data recording; critically revisedthe draft of the manuscript; and approved the final manuscript. M.-H.K. was aresearcher and supervised laboratory analyses of this study. K.-C.M. is the guarantorof this work and, as such, had full access to all the data in the study and takesresponsibility for the integrity of the data and the accuracy of the data analysis.Prior Presentation. Parts of this study were presented in abstract form atPRS Korea 2018: the 76th Congress of the Korean Society of Plastic andReconstructive Surgeons and the 2nd Asian Forum for Fat & Stem Cells, Seoul,South Korea, 9–11 November 2018; the 6th World Congress for World Associationfor Plastic Surgeons of Chinese Descent, the 2018 Asian Pacific Plastic andReconstructive Surgery Forum, and the 2018 Annual Meeting of Taiwan Society ofPlastic Surgery, Taipei, Taiwan, 29 November to 1 December 2018; and the 8thCongress for the Korea Association of Stem Cell and Tissue Regeneration, Seoul,South Korea, 2 December 2018.
References1. Robson MC. Cytokine manipulation of the wound. Clin Plast Surg 2003;30:57–652. Han SK, Yoon TH, Lee DG, Lee MA, Kim WK. Potential of human bone marrowstromal cells to accelerate wound healing in vitro. Ann Plast Surg 2005;55:414–4193. Conget PA, Minguell JJ. Phenotypical and functional properties of humanbone marrow mesenchymal progenitor cells. J Cell Physiol 1999;181:67–734. Kim JB, Chun KW, Han SK, Kim WK. Effect of human bone marrow stromalcell allograft on proliferation and collagen synthesis of diabetic fibroblasts in vitro. JPlast Reconstr Aesthet Surg 2010;63:1030–10355. Lee CH, Han SK, Choi WI, Kim WK. Effect of human bone marrow stromalcells and dermal fibroblasts on collagen synthesis and epithelization. Ann PlastSurg 2007;59:713–7196. Han SK, Chun KW, Gye MS, Kim WK. The effect of human bone marrowstromal cells and dermal fibroblasts on angiogenesis. Plast Reconstr Surg2006;117:829–835
diabetes.diabetesjournals.org Moon and Associates 845

7. Tabatabaei Qomi R, Sheykhhasan M. Adipose-derived stromal cell in re-generative medicine: a review. World J Stem Cells 2017;9:107–1178. Bora P, Majumdar AS. Adipose tissue-derived stromal vascular fraction inregenerative medicine: a brief review on biology and translation. Stem Cell ResTher 2017;8:1459. Maria OM, Shalaby M, Syme A, Eliopoulos N, Muanza T. Adipose mesen-chymal stromal cells minimize and repair radiation-induced oral mucositis. Cy-totherapy 2016;18:1129–114510. Cao Y, Gang X, Sun C, Wang G. Mesenchymal stem cells improve healing ofdiabetic foot ulcer. J Diabetes Res 2017;2017:932834711. Kato Y, Iwata T, Morikawa S, Yamato M, Okano T, Uchigata Y. Allogeneictransplantation of an adipose-derived stem cell sheet combined with artificial skinaccelerates wound healing in a rat wound model of type 2 diabetes and obesity.Diabetes 2015;64:2723–273412. McLaughlin MM, Marra KG. The use of adipose-derived stem cells as sheetsfor wound healing. Organogenesis 2013;9:79–8113. You HJ, Han SK, Lee JW, Chang H. Treatment of diabetic foot ulcers usingcultured allogeneic keratinocytes—a pilot study. Wound Repair Regen 2012;20:491–49914. Lavery LA, Fulmer J, Shebetka KA, et al.; Grafix Diabetic Foot Ulcer StudyGroup. The efficacy and safety of Grafix for the treatment of chronic diabetic footulcers: results of a multi-centre, controlled, randomised, blinded, clinical trial. IntWound J 2014;11:554–56015. Huebner AR, Fina AD. The stochastically curtailed generalized likelihoodratio: a new termination criterion for variable-length computerized classificationtests. Behav Res Methods 2015;47:549–56116. Falanga V, Margolis D, Alvarez O, et al.; Human Skin Equivalent InvestigatorsGroup. Rapid healing of venous ulcers and lack of clinical rejection with an al-logeneic cultured human skin equivalent. Arch Dermatol 1998;134:293–30017. Briscoe DM, Dharnidharka VR, Isaacs C, et al. The allogeneic responseto cultured human skin equivalent in the hu-PBL-SCID mouse model of skinrejection. Transplantation 1999;67:1590–159918. Marston WA, Hanft J, Norwood P, Pollak R; Dermagraft Diabetic Foot UlcerStudy Group. The efficacy and safety of Dermagraft in improving the healing ofchronic diabetic foot ulcers: results of a prospective randomized trial. DiabetesCare 2003;26:1701–170519. Steinberg JS, Edmonds M, Hurley DP Jr, King WN. Confirmatory data from EUstudy supports Apligraf for the treatment of neuropathic diabetic foot ulcers. J AmPodiatr Med Assoc 2010;100:73–7720. Han SK, Choi KJ, Kim WK. Clinical application of fresh fibroblast allograftsfor the treatment of diabetic foot ulcers: a pilot study. Plast Reconstr Surg 2004;114:1783–178921. Han SK, Kim HS, Kim WK. Efficacy and safety of fresh fibroblast allografts inthe treatment of diabetic foot ulcers. Dermatol Surg 2009;35:1342–134822. Hehenberger K, Heilborn JD, Brismar K, Hansson A. Inhibited proliferation offibroblasts derived from chronic diabetic wounds and normal dermal fibroblaststreated with high glucose is associated with increased formation of l-lactate.Wound Repair Regen 1998;6:135–141
23. Moon KC, Lee JS, Han SK, Lee HW, Dhong ES. Effects of human umbilicalcord blood-derived mesenchymal stromal cells and dermal fibroblasts on di-abetic wound healing. Cytotherapy 2017;19:821–82824. You HJ, Han SK. Cell therapy for wound healing. J Korean Med Sci 2014;29:311–31925. Kaisang L, Siyu W, Lijun F, Daoyan P, Xian CJ, Jie S. Adipose-derived stemcells seeded in Pluronic F-127 hydrogel promotes diabetic wound healing. J SurgRes 2017;217:63–7426. Madonna R, Delli Pizzi S, Tartaro A, De Caterina R. Transplantation ofmesenchymal cells improves peripheral limb ischemia in diabetic rats [publishedcorrection appears in Mol Biotechnol 2014;56:777]. Mol Biotechnol 2014;56:438–44827. Cianfarani F, Toietta G, Di Rocco G, Cesareo E, Zambruno G, Odorisio T.Diabetes impairs adipose tissue-derived stem cell function and efficiency inpromoting wound healing. Wound Repair Regen 2013;21:545–55328. Shin L, Peterson DA. Human mesenchymal stem cell grafts enhance normaland impaired wound healing by recruiting existing endogenous tissue stem/progenitor cells. Stem Cells Transl Med 2013;2:33–4229. Falanga V. Wound healing and its impairment in the diabetic foot. Lancet2005;366:1736–174330. Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burdenof diabetic foot disease. Lancet 2005;366:1719–172431. Bolton LL. Quality randomized clinical trials of topical diabetic foot ulcerhealing agents. Adv Wound Care (New Rochelle) 2016;5:137–14732. Veves A, Falanga V, Armstrong DG, Sabolinski ML; Apligraf Diabetic FootUlcer Study. Graftskin, a human skin equivalent, is effective in the managementof noninfected neuropathic diabetic foot ulcers: a prospective randomized mul-ticenter clinical trial. Diabetes Care 2001;24:290–29533. DiDomenico LA, Orgill DP, Galiano RD, et al. Use of an aseptically processed,dehydrated human amnion and chorion membrane improves likelihood and rate ofhealing in chronic diabetic foot ulcers: a prospective, randomised, multi-centreclinical trial in 80 patients. Int Wound J 2018;15:950–95734. Tettelbach W, Cazzell S, Reyzelman AM, Sigal F, Caporusso JM, Agnew PS. Aconfirmatory study on the efficacy of dehydrated human amnion/chorion mem-brane dHACM allograft in the management of diabetic foot ulcers: a prospective,multicentre, randomised, controlled study of 110 patients from 14 wound clinics.Int Wound J 2019;16:19–2935. Park KH, Han SH, Hong JP, et al. Topical epidermal growth factor spray forthe treatment of chronic diabetic foot ulcers: a phase III multicenter, double-blind, randomized, placebo-controlled trial. Diabetes Res Clin Pract 2018;142:335–34436. Han SK, Kim HR, Kim WK. The treatment of diabetic foot ulcers with un-cultured, processed lipoaspirate cells: a pilot study. Wound Repair Regen 2010;18:342–34837. Bender R, Lange S. Adjusting for multiple testing—when and how? J ClinEpidemiol 2001;54:343–34938. Wason JM, Stecher L, Mander AP. Correcting for multiple-testing in multi-arm trials: is it necessary and is it done? Trials 2014;15:364
846 Stem Cells for Diabetic Ulcers Diabetes Volume 68, April 2019