Perspectives on Bone Mechanical Properties and Adaptive Response to Mechanical Challenge
Transcript of Perspectives on Bone Mechanical Properties and Adaptive Response to Mechanical Challenge

Journul of Clinical Densitometry, vol. 2, no. 4, 423433, Winter 1999 0 Copyright 1999 by Humana Press Inc. All rights of any nature whatsoever reserved. 0 169-4 194/99/2:423433/$12.75
Perspectives on Bone Mechanical Properties and Adaptive Response to Mechanical Challenge
Yebin Jiang, MD, P H D , ~ Jenny Zhao, MD, M S , ~ Clword Rosen, M D , ~ Piet Geusens, MD, P H D , ~ and Harry K. Genant, MD’
‘Osteoporosis and Arthritis Research Group, Department of Radiology, University of California, San Francisco, CA; 2Maine Center for Osteoporosis Research and Education, St. Joseph Hospital, Bangol; ME; and 3Clinical Research Center for Bone and Joint Diseases, Dr: L. Willems-Instituut, Limburgs Universitair Centrum, Diepenbeek, Belgium
Abstract
The bones of the human skeleton serve a mechanical function besides providing a reservoir for calcium and hematopoietic homeostasis. When mechanically challenged, they usually respond and adapt; failure to do so can result in fracture. The mechanical behavior of bone is determined by bone mass and its material proper- ties and by its geometry and architecture. Therefore, in vivo noninvasive measurements of bone mass, geom- etry, and structure can predict bone strength and are usually employed as a useful-if not always reliable-way to estimate bone fragility, whereas direct bone biomechanical testing in vitro can provide detailed information about mechanical strength. Because bone strains are likely to be important regulators of bone mass and strength, exercise protocols designed to counteract the effects of osteoporosis should load the target bone with repeated high peak forces and high strain rates or high impacts on a long-term basis. Such a protocol creates varied strain distributions throughout the bone structure, producing short, repeated strains on the bone in directions to which it is unaccustomed. Exercise in this manner can maintain and perhaps increase bone mass and improve mechanical properties and neuromuscular competency, reducing skeletal fragility and the predisposition to falls.
Key Words: Bone biomechanics; bone mass and structure; mechanical usage; densitometry; physical exercise.
Introduction The organization and composition of the human
skeleton, a mechanically optimized system, reflect its functional demands: the transmission of force and stabilization of body shape, or mechanical support and protection, locomotion, and participation in
Received 11/03/98; Revised 07/17/99; Accepted 0811 1/99. Address correspondence to Dr. Yebin Jiang, Osteoporosis
and Arthritis Research Group, Department of Radiology, University of California, San Francisco, CA 94143-0628. E-mail: Yebin.Jiang @oarg.ucsf.edu
metabolism associated with mineral homeostasis. Normally, bone architecture, including mass and dis- tribution, shape, and internal arrangement, is primar- ily determined by the genetic inheritance of an individual and the responses and adaptations to mechanical loading ( I ) . According to Wolff’s Law, the geometry of the cortical bone and the patterns of trabecular structure are the results of functional adaptation to normal physiological load bearing. The molecular, cellular, and metabolic activities in bone work to maintain this mechanical environment or to respond and adapt to new loading situations, whereas failure to do so can lead to the pathological
423

424 Jiang et al.
fractures and bone pain associated with some meta- bolic bone diseases. ,'Stiffness (tan a)
L. a L-L
Load Torque (N-m)
Force (N)
Basic Background Stress and Strain
Basic knowledge of bone biomechanics begins with an introduction and understanding of its concepts and terms. The terms and concepts of stress and strain are essential and fundamental to the study of bone biomechanics. They follow the application of forces to bone and the resulting deformation of the bone. An internal resistance counters the applied force. This internal resistance is known as stress. It is usually opposite in direction but equal in magnitude to the applied force. Stress, defined as force per unit area, includes three principal types according to how loads are applied: compressive, shear, or tension. As stress is distributed over the cross-sectional area of the bone, it is expressed in units of force per unit area and is reported in pascals (1 Pa = 1 N/m2 = 0.0001451 psi), or megapascals (1 Mpa = 1,000,000 Pa).
Mechanical loads always strain or deform a bone. Strain describes the changes in dimension that bone experiences under the influence of an applied force. It is defined as relative deformation or percentage change in length. Thus, it is equivalent to the change in length divided by the original length of the bone section. For example, if a material is stretched to 101% of its original length, it has a strain of 0.01, or 1%. Strain has no units and can be reported as rela- tive deformation, such as a strain of 0.01 or 1% deformation. However, strain is usually expressed in microstrain (pstrain) units. For example, 0.1 strain = 100,000 pstrain = 10% deformation (fracture), where 100,000 pstrain should shorten a bone by 10% of that length and break the bone, and 1000 pstrain in compression would shorten a bone by 0.1 % of its original length, whereas 2000 pstrain in tension stretches a bone 0.2%.
Structural biomechanical behavior of bone depends on the following variables: the geometric property determined by the shape and size of the structure, the amount of bone or bone mass, the material property inside the bone, and accumulation of microdamage. The mechanical behavior of a bone is determined by the type, magnitude, and orienta- tion of the load on it, as well as its stiffness, strength,
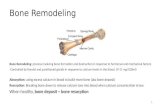
Fig. 1. Load-deformation curve of the biomechani- cal tests.
and architecture, and can be quantitatively assessed through the relationships between applied loads and the resulting deformations. These relationships gov- ern the structural behavior of whole bone and reflect the material property distribution within the bones as well as the bone geometry. In biomechanical tests, applied load and deformation as a function of time are recorded continuously. From the last load-defor- mation curve (Fig. l) , the following structural mechanical parameters can be derived: maximum strength at fracture; maximum deformation; stiffness as the ratio of applied load to resultant deformation in the linear region of the curve; and strain energy absorption before fracture, or toughness, as the area under the curve.
Strength Bone strength or its ultimate strength can be
defined as the load or corresponding strain or stress that fractures a bone. Fracture strength of normal lamellar bone can be expressed as a strain of about 25,000 k 5000 pstrain, corresponding to a change in length of 2.5%, i.e., from 100% of its original length to 97.5% of that length under com- pression, or 102.5% of it under tension, and corre- sponding to an ultimate or fracture stress of approx 130 Mpa (2).
The load-deformation curve can be divided into the elastic and plastic deformation regions by the yield point, above which stresses lead to plastic deformation and permanent damage to the bone
Journal of Clinical Densitometry Volume 2, 1999

Mechanical Properties and Usage of Bone 425
structure. The bone behaves like a good spring in the elastic deformation region; that is, the deforma- tion in the bone increases linearly with increasing load, and the bone returns to its original shape after the load is released. The rigidity or the extrinsic stiffness of the structure is shown by the slope of the elastic region in the load-deformation curve. The stress-strain curve represents the relationship between stress and strain in bone after the load is converted to stress and deformation is converted to strain using engineering formulae. The elastic or Young’s modulus is the slope of the stress-strain curve within the elastic region, which is a measure of the intrinsic stiffness of the material. The modu- lus of elasticity of bone tissue depends largely on the amount of mineral in it, i.e., the true volumetric bone mineral density (BMD) of the solid bone (3), and also on many other microstructural factors such as the arrangement of crystal and collagen fibers, composition of collagen and ground substance, microfractures, etc. (4).
Bigger bones have greater rigidity (5). The differ- ence between the extrinsic and the intrinsic stiffness can be illustrated as a comparison of the bone prop- erties from a sumo wrestler with those of a female ballet dancer. Although elastic modulus of their bones can be quite similar, the bone from the dancer has much less rigidity, because her bones might be, e.g., eight times smaller than his. This illustrates the difference between the stiffness of bone as a mater- ial and the stiffness of whole bones. The bones in the ballet dancer and the sumo wrestler have almost the same stiffness as materials, but markedly different stiffness as whole bones. Compared with the bone mass and architectural contributions, material prop- erties of bone change little with age and gender or species (2), except for contribution of microscopic heterogeneity of hyper- or hypomineralization, accu- mulations of unremodeled fatigue damage, and accumulation of cement lines to the aging process (6). Usually, the more mass the stronger the bone, because the amount of bone or bone mass in a cross- section (the bone mass contribution) affects the bone strength. In addition, the outside diameter and shape of a bone as well as its distribution, the architectural contribution, can affect the strength of a whole bone. Doubling the diameter of a bone without changing the bone mass in its cross-section, e.g., increases its
strength in bending eightfold (7). Although stronger bones usually have more bone mass, bone architec- ture can be more important than bone mass in some fracture situations (2,8).
Bone Qualily Bone quality is a term used widely in the literature
of osteoporosis research. This term is used in two ways. Some use bone quality to mean material prop- erties of bone or material quality, or the intrinsic nature of bone at the tissue level. Others use bone quality to refer to structural strength, which functions as a whole anatomical unit, because good-quality bone should be biomechanically sound. Nevertheless, in both cases, the actual meaning of bone quality is based on mechanical concepts.
When bone quality refers to material property of bone, it also includes various aspects of components of material quality, such as lamellar texture, state, and microscopic heterogeneity in mineralization of bone matrix or within individual osteons; decreased matrix mineralization; accumulation of cement lines; accumulation of unremodeled fatigue damage and microcracks or defects at the ultrastructural level; bone turnover that would replace fatigue-damaged bone; etc. (6,9,10).
When bone quality refers to structural strength, it consists of both material properties and geomet- ric properties, including bone morphology such as dimensions and architecture as well as trabecular disruption and connectivity and patchy areas of porosity (6), besides the material properties just stated in the above paragraph. A bone should show good mechanical quality for every possible kind of fracture. A good, healthy bone must show both a high mechanical quality of its constitutive material and an adequate amount and spatial distribution of the material, to cope with different deforming forces or types of fractures (8 , l l ) . It is said that in osteoporosis treatment an increase in bone quan- tity should be accompanied by an improvement in bone quality. In this sense, bone quality means bone structural strength, since the material of bone remain about the same regardless of age, gender, species, or even most bone disorders (2). Therefore, bone quality can be used to mean fragility, in which increased fragility would mean poorer bone quality and vice versa.
Journal of Clinical Densitometry Volume 2, 1999

426 Jiang et al.
Fractures or Mechanical Failure in Osteoporosis
Fractures occur as a result of bone mechanical fail- ure when heavy loads (and the stresses and strains they cause) exceed the ultimate strength of a bone. Osteoporotic fractures have their own characteristics and might be predicted from measurement of differ- ent aspects of bone biomechanical properties.
Characteristics of Osteoporotic Fractures Of most concern in osteoporosis in aging adults
are fractures of the hips, vertebral bodies, and wrists, usually caused by falls owing to impaired balance. Certain changes in bone cortex or spongiosa may make such injuries more likely to cause a fracture but do not themselves cause the fracture, since the bones fracture as a result of the fall (12). Some peo- ple develop spontaneous fractures in the vertebral bodies from voluntary activities even without falls. A combination of compression, torque, and bending loads causes most of these fractures. The shape, size, and structure of bone as well as its mass affect its resistance to these loads.
Fractures of the vertebral bodies are a result of predominantly axial compressive loads. The decreased load-bearing capacity of each vertebra is related to the material properties of the bone and changes in the vertebral trabeculae from post- menopausal and age-related bone loss. Absorption and removal of the horizontal trabeculae or lateral support crossties changes the architectural arrange- ment and results in a decrease in load-bearing capac- ity (13). The vertical trabecular bone, therefore, behaves as a column and is prone to critical buckling loads (14). A 50% decrease in cross-sectional area as a result of absorption of the horizontal trabeculae is associated with a 75% decrease in the load-bearing capacity of the vertebral body (15).
In addition to osteoporotic vertebral fracture, loss of horizontal trabeculae facilitates intertrochanteric fractures of the hip. Fractures of the wrist and hip usually begin in the metaphyseal-epiphyseal regions of the bone, which depend heavily on the trabeculae to support loads (16,17). Osteoporotic fractures usu- ally do nQt occur in the midshaft of the femur or radius (It?), which are mainly cortical bone. Since the diameter of bone expands with age with an
increase in geometrical properties such as cross-sec- tional moments of inertia, particularly in men, there is more resistance to bending and torsional loads. However, the femoral neck, though also mainly of cortical bone, is not protected in the same way, since the periosteum is absent from the part of the femoral neck within the hip joint fcr periosteal bone apposi- tion (15,19,2O). Therefore, endosteal bone resorption during the aging process results in cortical bone thin- ning but is not associated with compensation of periosteal bone apposition to increase geometry such as cross-sectional diameter and muments of inertia. Consequently, the femoral neck, with its unique anatomy, becomes prone to fracture under deform- ing forces.
Prediction of Osteoporotic Fracture The risk of fracture referred to by many investi-
gators really sums up two major factors. First, it is the risk that a given injury will cause a fracture. And, second, it includes the risk that a person will sustain such an injury, which depends heavily on occupation, leisure activities, neuromuscular coor- dination, and balance, which cannot be estimated by bone densitometry. The usefulness of bone densito- metry in osteoporosis lies in its ability to estimate whole-bone strength. Compared with BMD, bone mineral content is a better indicator of whole-bone strength (8). Computed tomography (CT) can deter- mine both bone mineral and bone geometry such as moments of inertia, and therefore provide a very reliable indicator.
Bone mass measured by densitometry can esti- mate the risk of future fracture, since fractures result, at least in part, from low bone mass. BMD is highly correlated with bone strength (21), as well as with fracture risk in patients (22). Several prospective studies have shown that measurements of bone mass can predict fracture risk, including vertebral and hip fractures (23,24). The relative risk for fracture increases by a factor of 1.5-3.0 or more for each stan- dard deviation decrease in BMD, depending on the site of measurement and the techniques used (22,25-27). BMD of the proximal femur predicts hip fractures better than measurements of other skeletal sites such as the forearm or spine (28). Measurement of bone mass at multiple anatomic sites and a combi- nation of the information might be helpful in predict-
Journal of Clinical Densitometry Volume 2, 1999

Mechanical Properties and Usage of Bone 42 7
ing the risk of hip (28) and spine (29,30) fractures for individual patients. In the elderly, the hip is likely to be the most favorable site for measurement (28).
The mechanical behavior of bone depends on the bone’s geometry and architecture as well as the mass of the tissue and its material properties. In the verte- bral bodies, the vertical and horizontal trabeculae and the intertrabecular connectivity, which might be independent of bone mass itself, also play important roles in determining bone strength and stiffness (31 j . Quantitative computed tomography (QCT) can eval- uate volumetric BMD, bone mineral distributions, cortical bone geometry, and apparent trabecular bone structure and connectivity on high-resolution images (32,33). Changes in the structural geometry of the skeleton can offset the effects of altered bone mass, although 75-80% of the variance in the ulti- mate strength of bone is attributed to BMD (15). The combination of volumetric BMD with trabecular structural parameters derived from peripheral QCT (pQCT) images, rather than either alone, improves the prediction of biomechanical properties (33).
Highly accurate assessment of bone size and den- sity can be derived from volumetric QCT examina- tion, without the artifacts of projectional radiographic and other densitometric techniques such as absorptiometry (34). Because volumetric CT examination gives such a true and highly accurate volumetric rendering, important biomechanical assessments can be derived, such as finite element analyses (35,36). Volumetric QCT plays important roles in evaluating bone geometry and determining the density of the proximal femur, which can be dif- ficult because of the femur’s complex anatomy and its dramatic three-dimensional variations in bone density. Studies employing volumetric QCT and finite analysis modeling have documented improved estimations of proximal femoral strength over global projectional densitometry (35,37). Similarly, in vitro studies have shown enhanced prediction of in vitro fracture load using subregional volumetric QCT of the hip (36).
The usefulness of the powerful tool QCT is bal- anced by its disadvantages: it is expensive to obtain and operate, and it is rarely available for routine non- clinical use. Although single energy QCT is more precise, it is less accurate (38) because of the influ- ence of intravertebral fat. Dual energy QCT is more
accurate but less precise and needs a higher radiation dose. Accuracy is a measure of the deviation of the measured from the “true” value whereas the preci- sion of a method refers to its ability to produce the same results on repeated measurements. The radia- tion dose received from QCT measurement is higher than that of dual X-ray absorptiometry (DXA) (39). All these disadvantages make QCT, in practical terms, a less satisfactory procedure than DXA. For prediction of fracture, which is the primary clinically justifiable use of bone mass measurement, DXA per- forms as well if not better than other methods.
Magnetic resonance imaging (MRI), which is noninvasive and produces no ionizing radiation, can quantify human trabecular bone structure (40,41 j and cortical bone geometry (42), as well as animal trabecular structure (43). Muscle mass and distribu- tion can also be quantified on both pQCT and MRI images.
Mechanisms Determining Bone Strength and Mass
The skeleton functions as a mechanical support and a reservoir for calcium and hematopoietic home- ostasis. When mechanically challenged, it can usu- ally respond and adapt structurally. Failure to do so can result in the development of fractures associated with bone disorders. The basic purpose of bone adap- tive structural response to mechanical challenges is to make bones strong enough to keep voluntary mechanical usage and muscle loads from causing fracture. Bone adapts its structure to past and present loads, according to some time-averaged value of many loads rather than to single or rare ones, and may respond differently to continuous or intermittent loads; for example, the peak strains or loads have much greater effects than smaller ones. These prop- erties are referred to as loading history (44).
Bone strains seem likely to be important regula- tors of bone mass distribution. Whereas in regular daily activity, the strains range from 200 to 2500 pstrain, to initiate a positive adaptive response, mechanical strain must exceed a threshold, the min- imal effective strain level, of about 1500-2500 pstrain (45). Bone seems to maintain the loading- induced peak strains at certain levels between 2000 and 3000 pstrain (46). Peak strain magnitudes mea-
Journal of Clinical Densitometry Volume 2, 1999

428 Jiang et al.
sured in various vertebrates are quite similar, ranging in amplitude from 2000 to 3500 pstrain, in running human tibia, chewing macaque mandible, galloping horse metacarpal, trotting sheep femur, and flying goose humerus (46-48). Bone strength and mass associate strongly with peak bone strains. Immobilization with minimal structural deformation and strain of <200 pstrain can inhibit the modeling and bone gain and result in increased remodeling and bone loss (49). The homeostatic regulation of bone mass mainly depends on weight bearing and the number and amplitude of episodic strains. Instead of the pattern of strain change generated by the often repeated strains of daily activity, the infre- quently repeated strains produced during unusual activities seem likely to be the most effective com- ponent of the strain environment of bone. The more novel the strain distribution, the more potent its osteogenic potential ( I ) .
While the predominant perception of biophysical modulation of bone physiology is that the signals must be large to have any morphological impact, work at the level of the organ, tissue, and cell has demonstrated that low-magnitude mechanical load can be osteogenic if induced in an appropriate fre- quency domain (48). A study in a turkey ulna model of disuse osteopenia with daily exposure to 108,000 applied loading cycles, sufficient to induce peak strains of approx 100 pstrain, showed a strong antiresorptive influence of mechanical loading with preservation of bone mass, suggesting that the fre- quency or strain rate associated with the loading stimulus also plays a critical role in the mechanism by which bone responds to mechanical strain (50). Brief exposure (daily 100 s) to low-amplitude mechanical strains (150 pstrain mechanical stimu- lus) promotes bony ingrowth and can enhance the biological fixation of cementless implants in turkey ulna. The degree of ingrowth is dependent on the fre- quency of the applied strain, since bony ingrowth is greater at 1 than at 20 Hz (51). Studies using the equine cannon bone showed that the distribution of peak strains within bone do not correspond precisely with where the skeletal response occurs (52,53). In the disuse turkey ulna with enhanced endosteal resorption, daily loading for 10 min to a peak strain of 500 pstrain can maintain bone mass at 1 and 60 Hz, since loading at 1 Hz permits substantial
endosteal resorption but stimulates substantial periosteal new bone formation whereas at 60 Hz results in little or no endosteal resorption and only minimal new bone formation at the periosteal and endosteal surfaces; lead to a loss of bone mass at 3 and 10 Hz, because of enhanced endosteal resorp- tion; and result in a net gain at 30 Hz, owing to both periosteal and endosteal new bone formation. The data indicate that signals appreciated by the perios- teum may not necessarily be relevant to endosteal surface and that different components of the strain tensor may do different things. Although modeling and remodeling strongly depend on the magnitude of the stimulus, the site of response is not where the signal is greatest, suggesting the complexity of the system ranging from site-specific sensitivity to spa- tial integration of strain information (48).
Osteocytes or lining cells may sense the strain induced at orgadtissue levels by mechanical chal- lenge. The cells are genetically programmed to detect and adapt to strains in their immediate vicin- ity ( I ) . Strain affects cells directly by changing their dimensions or indirectly through intralacular pres- sure, shear stresses, or charged fluid flow ( I ) . The cells detect compression or tension and determine a certain spatial orientation to release some factor, such as cytokines, that stimulates or inhibits uncou- pled modeling or coupled remodeling. Thus, the antagonistic forces determine local bone mass and structure. This process should optimize bone mass, the material properties of bone, and/or distribution, and provide protection against the accumulation of microfractures. Bone mechanical strength would therefore be optimized, and heavier loads would be required to induce a plastic deformation and provoke a fracture in the region (11).
The mechanostat, a mechanism proposed by Frost (54), oversees the fit of bone mass and strength to mechanical usage to make bones mechanically com- petent. It is a concept contributed by a number of important earlier investigators (44,55-57). When bone mass and strength become inadequate accord- ing to the modeling threshold criterion, modeling by drifts will increase bone mass and strength, whereas disuse-mode remodeling begins to remove them when they are no longer necessary. Daily, regular activities in adults turn modeling off and conserva- tion-mode remodeling on to maintain existing bone
Journal of Clinical Densitometly Volume 2, 1999

Mechanical Properties and Usage of Bone 429
mass and strength (2). Changing from daily regular usage to hypervigorous mechanical activities of the weight-lifting type can turn modeling on and increase bone mass and strength ( 2 3 ) .
Bone architecture is determined by two biological phases. Before birth, a provisional model is created according to predetermined patterns of genetic expression. This model determines that there will be five fingers on a hand and two bones in the leg and the forearm, and provides the principal biological mechanisms for changing bone architecture after birth. After birth, mechanical usage activates and guides the mechanisms. The size and shape of a bone are mainly determined during growth. Modeling sculpts the bone to meet both the genetically pro- grammed plan and the demands of current mechani- cal usage. The extent and rate of remodeling is reduced in adults, which is important to both joints and bones. The skeleton frequently tries to adjust its size and shape to compensate for changes in bone material (4). For example, osteoporosis involves a loss of trabecular bone mass and reduction of the failure stress of the vertebral bodies. In men, how- ever, there is a concurrent increase in vertebral diam- eter, which prevents the structural strength from being reduced to the same extent as the material strength (59). For reasons that are unclear, such com- pensation does not occur in women (4).
Muscle and Bone Regional muscle strength is important for deter-
mining the strength of the whole bone regardless of sex, age, or body habitus (60). The largest loads applied to bones during normal daily activities come from the muscles. Changes in muscle strength can change the largest voluntary loads on the bones (2). The voluntary longitudinal forces on the femur of a football player during a game can, e.g., briefly exceed five times his body weight (7,61). Aging adults who keep doing arduous physical work or weight lifting maintain their muscle strength and bone mass better than sedentary people (62-66).
Both muscle strength and lean mass have been reported to be positively associated with bone mass (67). Biceps strength best predicts hip BMD whereas grip strength independently predicts BMD of the lumbar spine and radius (68). DXA lean mass is
more strongly associated with BMD at the hip, spine, and whole body than is fat mass (65). Muscle strength and mass are directly related to BMD of adjacent skeletal segments (69), with 10-20% of the variance in BMD attributed to physical activity. The greater muscle strength and lean mass per unit of body surface area in gymnasts may also contribute to higher bone mass (70). However, the mechanical loading of swimming, resulting from muscle pull via tendon attachments to insertion sites, appears inef- fective at altering bone mineral (66). When the weight-bearing component is removed from physical activity, forces are reduced; swimming does not include any impact forces and is a completely non- weight-bearing activity (68). In one study, young women participated in a progressive high-intensity strength elbow flexion and extension training that apparently loaded the forearm bones in the direction to which they were already accustomed. This did not create sufficient strain magnitude in the shafts of the forearm bones to initiate bone formation or adapta- tion in bone geometry, despite effectively increasing muscular strength (71). Therefore, though muscle forces are the major forces affecting bone, progres- sively intense muscle forces from training did not suffice to increase bone mass, indicating that perhaps muscle forces are necessary but not sufficient for skeletal adaptive response whereas perhaps impact is itself important.
Exercise and Bone New pharmaceutical agents and biophysical
modalities may be introduced in an effort to prevent and treat osteoporosis. These treatments may affect adaptive response of bone to mechanical strain. The desired outcome of all treatment regimens is to improve bone strength (72-74) and reduce the inci- dence of fractures. Maximizing peak bone mass in early adulthood as genetically possible and minimiz- ing bone loss after menopause are very important in the prevention of osteoporosis. Other than hormone replacement therapy (HRT) and treatment with ana- bolic agents, several general approaches to prevent- ing and treating postmenopausal and age-related bone loss have been proposed. These include taking sufficient dietary calcium; using antiresorption agents such as bisphosphonates to depress disuse-
Journal of Clinical Densitometry Volume 2, 1999

430 Jiang et al.
mode bone remodeling; augmenting bone gains that occur in bone modeling during skeletal growth (the selective inhibition of osteoclast-mediated bone resorption may allow an individual to reach and/or exceed their genetically predetermined bone mass); maintaining young-adult muscle strength by engag- ing in appropriate physical exercise, such as weight lifting or its equivalent, or by using medications such as growth hormone when physical activities decrease; and discovering new agents that potentiate normal responses of bone to hypervigorous mechan- ical activities (2).
Although the important role of physical activities or mechanical loading of the bones in the develop- ment and maintenance of bone mass and strength is widely accepted, the type, intensity, frequency, and duration of activity that best produces the desired increases in mass and strength of human bones has not been clearly determined. Clinical and experi- mental research has shown that the exercise protocol should load the target bone with high peak forces and high strain rates with high impacts, creating ver- satile strain distributions throughout the bone struc- ture. In other words, exercise activities should load the bone in directions to which it is unaccustomed and should be long term and progressive but with relatively short repetitions and training sessions (75,76). Such exercise activities include gymnastics, weight lifting, jumping, squash, tennis, aerobics, and power training. It is important to encourage regular exercise and a physically active lifestyle in children and adolescents; this may lead to permanent changes in bone geometry and therefore improve bone mechanical competence and prevent osteoporosis and its fractures later in life. In adults, regular and long-standing physical loading activities can increase the ability of bone to resist fracture. By maintaining and perhaps even increasing bone mass and mechanical properties, as well as improving neuromuscular competency, such activities can reduce skeletal fragility, the predisposition to falls, and the effect of falls (58,77).
A recent meta-analysis of studies on exercise and osteoporosis suggests that exercise may slow the rate of bone loss in postmenopausal women (78), sup- porting a review that the beneficial effects of exer- cise on BMD among postmenopausal women as a result of exercise appear to be modest (79). It would
appear prudent to recommend that exercise be used in combination with both adequate calcium intake and some type of HRT for maintaining and/or increasing BMD in postmenopausal women at risk for osteoporosis (78). Estrogens may enhance the osteogenic effect of loading, especially in menopausal and postmenopausal women (77).
Continuing physical activity reduces the risk of hip fractures (80,81). Continually adapted strength training in older women has been shown to be an effective, safe, reproducible, and adaptable method of therapeutic strength training, following only two exercise sessions per week (62). Weight lifters have more bone and stronger bones than marathon run- ners, joggers, and swimmers, who put far more but smaller loads on their bones. BMD increases more when the training period lasts longer; BMD decreases when exercise stops. Therefore, therapeu- tic strength training must be performed year round and throughout one’s life (62).
Mechanical loads that impart high magnitudes are more osteotropic than low-intensity loads, and the importance of the number of loading cycles, or repe- titions, is relatively modest (44). Bone “worries” only about loads large enough to break it, and the model- ing threshold provides the natural criterion that dis- tinguishes acceptable from worrisome in that regard. Increased mechanical loading through the application of resistance such as in weight training, or increased weigh-bearing activity such as running, augments bone mass (63,64). In runners, forces on the lower limbs can be 2-5 times body weight (82) whereas those at the lumbar spine are 1.75 times body weight (83). By contrast, in gymnasts forces at the hip are as high as 10-12 times body weight (84), or 18 times body weights with each dismount from parallel bars (85). High strain rates result from rapid acceleration and deceleration movements. Gymnastics training invokes enormous impact-loading strains with few loading cycles on the skeleton, which have powerful osteogenic effects and induce high BMD (66,85).
Human studies support the animal models (57,236) in that the magnitude of loading is more important for bone than the number of cycles or repetitions (70). The loading threshold for activation of bone forma- tion is about 1050 pstrain in rats (87). Loading avian ulna at only 1000 pstrain in an unusual direction can stimulate new bone formation (86). It has been found
Journal of Clinical Densitometry Volume 2, 1999

Mechanical Properties and Usage of Bone 431
that strain produced by loading must be of sufficient magnitude to exceed a threshold or minimum effec- tive strain, as proposed by Frost (88); that strain should be applied in an intermittent, dynamic fash- ion; that loading should be novel in its magnitude and/or distribution strain within bone, i.e., different from normal daily activities; and that strain should be applied at a relatively high rate, with few loading cycles required (89). Appropriate load-bearing exer- cise should probably be done at alternate daily inter- vals ( I ) , but no more than three times a week (90).
Summary Biomechanical properties of bone, which can be
directly determined by biomechanical testing, depend on bone mass and its distribution, bone architecture and geometry, and material properties. Quantitative measurements of bone mass and struc- ture as well as geometry measured with densitomet- ric techniques such as DXA or QCT can predict bone strength and are used to evaluate fracture risk in osteoporosis. Muscle strength and mass have been reported to be positively associated with bone mass. Bone shows a structurally adaptive response to mechanical challenges and usage, making it strong enough to keep voluntary mechanical usage and muscle loads from causing fracture. Bone strains seem to be important regulators of bone mass distri- bution. Long-term exercise that loads the target bone in directions to which it is unaccustomed with short repetitions, high peak forces, and high impacts can maintain and perhaps increase bone mass and mechanical properties, improve neuromuscular com- petency, and reduce the predisposition to falls.
Acknowledgment We greatly appreciate comments provided by
Harold M. Frost, MD.
Refeseiices 1. Lanyon LE. 1996 Using functional loading to influence
bone mass and architecture: objectives, mechanisms, and relationship with estrogen of the mechanically adaptive process in bone. Bone 18:S37-S43.
2. Frost KM. 1997 Perspectives on our age-related bone loss: insights from a new paradigm. J Bone Miner Res 12:1539-1546.
3. Currey JD. 1988 The effects of porosity and mineral content on the Young’s modulus of elasticity of compact bone. J Biomech 21: 13 1-1 40.
4. Martin RB. 1991 Determinants of the mechanical properties of bone. J Biomech 24:77-88.
5. Turner CH, Burr DB. 1993 Basic biomechanical measure- ments of bone: a tutorial. Bone 14595-608.
6. Marcus R. 1996 The Nature of Osteoporosis. In: Osteoporosis. Marcus R, Feldman D, Kelsey J, eds. Academic, San Diego, 647-659.
7. Martin RB, Burr DB. 1989 Structure, function and adapta- tion of compact bone. New York: Raven.
8. Jiang Y. 1995 Radiology and histology in the assessment of bone quality. Louvain, Belgium, Peeters & Jiang.
9. Wallach S, Feinblatt JD, Avioli LV. 1992 The bone “quality” problem. Editorial. Calcif Tissue Int 51: 169-172.
10. Sherman S, Heaney RP, Parfitt AM, Hadley EC, Dutta C. 1993 NIA workshop on aging and bone quality. Calcif Tissue Int 53:SI-S180.
11. Ferretti JL. 1998 Biomechanical Properties of Bone. In: Bone Densitometry and Osteoporosis. Genant HK, Guglielmi G, Jergas M, eds. Springer, Berlin, 144-161.
12. Frost HM, Ferretti JL, Jee WSS. 1998 Perspectives: some roles of mechanical usage, muscle strength, and the mechanostat in skeletal physiology, disease, and research. Calcif Tissue Int 62: 1-7.
13. Mosekilde Li, Viidik A, Mosekilde LE. 1985 Correlation between the compressive strength of iliac and vertebral tra- becular bone in normal individuals. Bone 6:291-295.
14. Townsend PR. 1975 Buckling studies of single human tra- beculae. J Biomech 8:199-201.
15. Einhorn TA. 1992 Bone strength: the bottom line. Calcif Tissue Int 5 1 :333-339.
16. Brown TD, Ferguson AB Jr. 1978 The development of a computational stress analysis of the femoral head. J Bone Joint Surg 60A:619-629.
17. McBroom RJ, Hayes WC, Edwards WT, Goldberg RP, White AA. 1985 Prediction of vertebral body compressive fracture using quantitative computed tomography. J Bone Joint Surg 67A: 1206-1214.
18. Smith CB, Smith DA. 1976 Relations between age, mineral density and mechanical properties of human femoral com- pacts. Acta Orthop Scand 47:496-502.
19. Pankovich, AM. 1995 Primary internal fixation of femoral neck fractures. Arch Surg i 10:20-26.
20. Phemister DB. 1939 The pathology of ununited fractures of the neck of the femur with special reference to the head. J Bone Joint Surg 21:681-693.
21. Mazzess RB, Wahner HW. 1988 Nuclear Medicine and Densitometry. In: Osteoporosis: Etiology, Diagnosis, and Management. Riggs BL, Melton LJ, eds. Raven, New York,
22. Ross PD, David JW, Vogel JM, et al. 1990 A critical review of bone mass and the risk of fractures in osteoporosis. Calcif Tissue Int 46:149-161.
23. Hui SL, Slemenda CW, Johnston CC. 1988 Age and bone mass as predictors of fracture in a prospective study. J Clin Invest 81:1804-1809.
251-295.
Journal of Clinical Densitometry Volume 2, 1999

432 Jiang et al.
24. Melton LJ 111, Wahner HW, Richelson LS, O’Fallon WM, Riggs BL. 1986 Osteoporosis and the risk of hip fractures. Am J Epidemiol 124:254-261.
25. Gardsell P, Johnell 0, Nilsson B. 1991 The predictive value of bone loss for fragility fractures in women: a longitudinal study over 15 years. Calcif Tissue Int 49:90-94.
26. Black D, Cummings SR, Genant HK, Nevitt MC, Palermo L, Browner W. 1992 Axial and appendicular bone density predict fractures in older women. J Bone Miner Res 7:633-638.
27. Ross PD, Genant HK, Davis JW, Miller P, Wasnich RD. 1993 Predicting vertebral fracture incidence from prevalent fractures and bone density among non-black, osteoporotic women. Osteoporos Int 3: 120-127.
28. Cummings SR, Black DM, Nevitt MC, et al. 1993 Bone density at various sites for prediction of hip fractures: the study of osteoporotic fracture. Lancet 341: 72-75.
29. Wasnich R. 1993 Bone mass measurement: prediction of risk. Am J Med 955-105.
30. Genant HK, Lu Y, Mathur AK, Fuerst TP, Zhao S, Cummings SR. 1997 Diverse diagnostic armamentarium in bone mass measures: opportunities and dilemmas. Osteoporosi Int 7:258.
31. Ott SM, Parfitt AM, Raisz LG, Biewener T. 1993 When bone mass fails to predict bone failure. Calcif Tissue Int
32. Genant HK, Engelke K, Fuerst T, et al. 1996 Noninvasive assessment of bone mineral and structure-state of the art. J Bone Miner Res 11 :707-730.
33. Jiang Y, Zhao J, Augat P, et al. 1998 Trabecular bone min- eral and calculated structure of human bone specimens scanned by peripheral quantitative computed tomography: relation to biomechanical properties. J Bone Miner Res
34. Jergas M, Breitenseher M, Gliier CC, Yu W, Genant HK. 1995 Estimates of volumetric bone density from projec- tional measurements improve the discriminatory capability of dual X-ray absorptiometry. J Bone Miner Res 10:1101-1110.
35. Keyak JH, Rossi SA, Jones KA, Skinner HB. 1998 Prediction of femoral fracture load using automated finite element modeling. J Biomech 31: 125-133.
36. Lang TF, Keyak JH, Heitz MW, et al. 1997 Volumetric quantitative computed tomography of the proximal femur: precision and relation to bone strength. Bone 21: 101-108.
37. Lotz JC, Gerhart TN, Hayes WC. 1990 Mechanical proper- ties of trabecular bone from the proximal femur: a quantita- tive CT study. J Comput Assist Tomog 14: 107-1 14.
38. Genant HK, Cann CE, Pozzi-Mucelli RS, Kanter AS. 1983 Vertebral mineral determination by quantitative C T clinical feasibility and normative data. J Comput Assist Tomog 75.54.
39. Hassager C, Christiansen C. 1993 Assessment of Bone Mass. In: Proceedings of the 4th International Symposium on Osteoporosis and Consensus Development. Christiansen C, Riis B, eds. Analborg, Denmark, Handelstrykkeriet Aalborg ApS, 41,42.
40. Majumdar S, Genant HK, Grampp S, et al. 1997 Correlation of trabecular bone structure with age, bone mineral density,
53(Suppl. l):S7-S13.
13:1783-1790.
and osteoporotic status: in vivo studies in the distal radius using high resolution magnetic resonance imaging. J Bone Miner Res 12:lll-118.
41. Genant HK, Gordon C, Jiang Y, Lang TF, Majumdar S. 1999 Advanced imaging of bone macro and micro structure. Bone
42. Jiang Y, Zhao J, White DL, Augat P, Peterfy CG, Genant HK. Assessment of the distal radius using a dedicated extremity magnetic resonance imaging system and periph- eral quantitative computed tomography: prediction of bio- mechanical properties. Bone 23(5S):637.
43. White D, Schmidlin 0, Jiang Y, et al. 1997 MRI of trabecu- lar bone in an ovariectomized rat model of osteoporosis. Proceedings of the International Society for Magnetic Resonance in Medicine 5th Scientific Meeting and Exhibition, vol. 2, Vancouver, BC, Canada, 1021.
44. Carter DR. 1987 Mechanical loading history and skeletal biology. J Biomech 20:1095-1109.
45. Frost HM. 1990 Skeletal structural adaptations to mechani- cal usage (SATMU): I. Redefining Wolffs law: the bone modeling problem. Anat Rec 226:403422.
46. Rubin CT. 1984 Skeletal strain and functional significance of bone architecture. Calcif Tissue Int 36:Sll-S18.
47. Rubin C, McLeod KJ, Brain S. 1990 Functional strains and cortical bone adaptation: epigenetic assurance of skeletal integrity. J Biomech 23:43-54.
48. Rubin CT, McLeod KJ. 1996 Inhibition of Osteopenia by Biophysical Intervention. In: Osteoporosis. Marcus R, Feldman D, Kelsey J, eds. Academic, San Diego, 351-371.
49. Frost HM. 1993 Suggested fundamental concepts in skele- tal physiology. Calcif Tissue Int 52:14.
50. Qin YX, Rubin CT, McLeod KJ. 1998 Nonlinear depen- dence of loading intensity and cycle number in the mainte- nance of bone mass and morphology. J Orthop Res 16:482489.
51. Rubin CT, McLeod KJ. 1994 Promotion of bony ingrowth by frequency-specific, low-amplitude mechanical strain. Clin Orthop 298:165-174.
52. Rubin CT, Lanyon LE. 1982 Limb mechanics as a function of speed and gait: a study of functional strains in the radius and tibia of horse and dog. J Exp Biol 101:187-211.
53. Gross TS, McLeod KJ, Rubin CT. 1992 Characterizing bone strain distributions in vivo using three triple rosette strain gages. J Biomech 25:1081-1087.
54. Frost HM. 1996 Perspectives: a proposed general model of the mechanotat (suggestion from a new paradigm). Anat Rec 244:139-147.
55. Carter DR, Orr TE, Fyhrie DP. 1989 Relationships between loading history and femoral cancellous bone architecture. J Biomech 22:231-244.
56. Firoozbakhsh K, Cowin SC. 1981 An analytical model of Pauwels’ functional adaptation mechanism in bone. J Biomech Eng 103:246-252.
57. Rubin CT, Lanyon LE. 1984 Regulation of bone formation by applied dynamic loads. J Bone Joint Surg 66:397402.
58. Smith EL, Gilligan C. 1989 Mechanical forces and bone. J Bone Miner Res 6: 139-1 73.
59. Mosekilde L, Mosekilde L. 1990 Sex differences in age- related changes in vertebral body size, density and biome-
25 149-1 52.
Journal of Clinical Densitornetry Volume 2, I999

Mechanical Properties and Usage of Bone 433
chanical competence in normal individuals. Bone
60. Schiessl H, Ferretti JL, Tysarczyk-Niemeyer G, Willnecker J. 1996 Noninvasive Bone Strength Index as Analyzed by Peripheral Quantitative Computed Tomography. In: Paediatric Osteology: New Developments in Diagnostics and Therapy. Schonau E, ed. Elsevier, Amsterdam, 141-146.
61. Crowninshield RD, Johnston RC, Andrews JG, Brand RA. 1978 A biomechanical investigation of the human hip. J Biomech 11 :75-85.
62. Hartard M, Haber P, Ilieva D, Preisinger E, Seidl G, Huber J. 1996 Systematic strength training as a model of therapeu- tic intervention: a controlled trial in postmenopausal women with osteopenia. Am J Phys Med Rehabil 752-28 .
63. Heinonen A, Oja P, Kannus P, et al. 1995 Bone mineral den- sity in female athletes representing sports with different loading characteristics of the skeleton. Bone 17: 197-203.
64. Snow-Harter C, Bouxsein ML, Lewis BT, Carter DR, Marcus R. 1992 Effects of resistance exercise on bone min- eral status of young women: a randomized exercise inter- vention trial. J Bone Miner Res 7:761-769.
65. Snow-Harter C, Wegner M, Robinson T, Shaw JM. 1993 Determinants of femoral neck BMD in pre- and post- menopausal women. Med Sci Sports Exerc S153.
66. Taaffe DR, Robinson TL, Snow CM, Marcus R. 1997 High- impact exercise promotes bone gain in well-trained female athletes. J Bone Miner Res 12:255-260.
67. Aloia JF, McGowan DM, Vaswani AN, Ross P, Cohn SH. 1991 Relationship of menopause to skeletal and muscle mass. Am J Clin Nutr 53:1378-1383.
68. Snow CM. 1996 Exercise and bone mass in young and pre- menopausal women. Bone 18:S51-S55.
69. Vico L, Pouget JF, Calmels P, Chatard JC, Rehailia M, Minaire P. The relations between physical ability and bone mass in women aged over 65 years. J Bone Miner Res
70. Robinson TL, Snow-Harter C, Taaffe DR, Gillis D, Shaw J, Marcus R. 1995 Gymnasts exhibit higher bone mass than runners despite similar prevalence of amenorrhea and oligomenorrhea. J Bone Miner Res 10:26-35.
71. Heinonen A, Sievanen H, Kannus P, Oja P, Vuori I. 1996 Effects of unilateral strength training and detraining on bone mineral mass and estimated mechanical characteristics of the upper limb bones in young women. J Bone Miner Res
72. Jiang Y, Zhao J, Van Audekercke R, Dequeker J, Geusens P. 1996 Effects of low-dose long-term NaF preventive treat- ment on rat bone mass and biomechanical properties. Calcif Tissue Int 58:30-39.
74. Jiang Y, Zhao J, Genant HK, Dequeker J, Geusens. 1998 Bone mineral density and biomechanical properties of spine
11~67-73.
10:374-383.
1 11490-50 1.
and femur of ovariectomized rats treated with naproxen. Bone 22509-514.
73. Jiang Y, Zhao J, Genant HK, Dequeker J, Geusens P. 1997 Long-term changes in bone mineral and biomechanical properties of vertebrae and femur in aging, dietary calcium restricted and/or estrogen-deprived/-replaced rats. J Bone Miner Res 12:820-831.
75. Vuori I, Heinonen A, Sievanen H, Kannus P, Pasanen M, Oja P. 1994 Effects of unilateral strength training and detrainig on bone mineral density and content in young women. Calcif Tissue Int 5559-67.
76. Davee AM, Rosen CJ, Adler RA. 1990 Exercise patterns and trabecular bone desity in college women. J Bone Miner Res 5:245-250.
77. Kannus P, Sievanen J, Vuori I. 1996 Physical loading, exer- cise, and bone. Bone 18:SI-S3.
78. Kelley GA. 1998 Exercise and regional bone mineral den- sity in postmenopausal women: a meta-analytic review of randomized trials. Am J Phys Med Rehabil 77:76-87.
79. Chesnut CH. 1993 Bone mass and exercise. Am J Med 95:34S-368.
80. Cummings SR, Nevitt MC, Browner WS, et al. 1995 Risk factors for hip fracture in white women. N Engl J Med 332:767-773.
81. Cumming RG, Klineberg RJ. 1994 Case-control study of risk factors for hip fractures in the elderly. Am J Epidemiol
82. Subotnick SI. The biomechanics of running: implications for the prevention of foot injuries. Sports Med 2:144-153.
83. Capozzo A. 1983 Force actions in the human trunk during running. J Sports Med 23: 14-22.
84. McNitt-Gray JL, Yokoi T, Millward C. 1993 Landing strat- egy adjustments made by female gymnasts in response to drop height and mat composition. J Appl Biomech 9: 173-190.
85. Marcus R. 1996 Skeletal “impact” of exercise. Lancet 348:1326, 1327 (comment).
86. Rubin CT, Lanyon LE. 1985 Regulation of bone mass by mechanical strain magnitude: the effect of peak strain mag- nitude. Calcif Tissue Int 37:411417.
87. Turner CH. 1994 Mechanical loading thresholds for lamel- lar and woven bone formation. J Bone Miner Res 9:87-97.
88. Frost HM. 1990 Skeletal structural adaptations to mechani- cal usage (SATMU): 2. Redefining Wolffs law: the remod- eling problem. Anat Rec 226:414-422.
89. Rubin CT, Lanyon LE. 1987 Osteoregulatory nature of mechanical stimuli: function is a determinant for adaptive remodeling in bone. J Orthop Res 5:300-310.
90. Raab-Cullen DM, Akhter MP, Kimmel DB, Recker RR. 1994 Bone response to alternate-day mechanical loading in the rat tibia. J Bone Miner Res 9:203-211.
1391493-503.
Journal of Clinical Densitometry Volume 2, 1999