Pandu kc016 hyd
-
Upload
ayurmitra-ksrprasad -
Category
Documents
-
view
2.115 -
download
11
description
Transcript of Pandu kc016 hyd

My commitment increases my level of energy. My energy increases my level of action. Myaction increases my level of success. My success increases my level of commitment.
Research in any field is the most important section of development. Ayurveda is inservice is for ages to the needy mankind to relieve their ailments and recording the factsfor the future generations. At present the Ayurveda research scholar, developing theAyurveda and understanding under the limelight of contemporary scientific backgrounds.The plagiarism is more and more now a day in the scientific community. This ishappening as the researches of the various institutions are not available for the commonresearcher. We wish to control this plagiarism by contributing the dissertations forscientific community. If you find any thesis is a copy of the previous publication, we takethis issue to the university authorities for proper action. The solution to prevent copy catsis … http://ayurvedaresearch.wordpress.com/
Dr. Shiva Rama Prasad Kethamakka

ACKNOWLEDGEMENT
I express my profound gratitude to my respected and honorable guide
Dr.V.VIJAYA BABU M.D. (Ayu.), Professor, P.G. Unit of Kaya Chikitsa., For his
excellent guidance and co-operation conducting this research work successfully.
I am highly indebted to my honoroble Dr. PRAKASH CHANDRA M.D. (Ayu.),
Proffessor Head of the department of Kayachikitsa, for his valuable timely
suggestions, thought provoding leads ideas and support in Completing this thesis
work.
I am very thankful to my co-guide Dr. RAMALINGESWARA RAO garu,
Technical Assistant and Lecturer for their precious suggestions and help through out
the study.
I convey my gratitude to the honorable Principal Dr. SADASIVA RAO, and Ex-
Superintendent L. RADHA KRISHNA MURTHY and Present Superintendent V.L.N.
SASTRY of Dr. B.R.K.R. Government Ayurvedic Hospital
I am thankful to Dr. V.V.S. RAMA SASTRY, M.D.(Ayu.), Retired professor,
and Dr.VASUDEVARAO garu retired professor, Dr. BASWANT garu Retired
Professor, Dr. M.L. NAIDU garu for their valuable suggestions and encouragement.
I am also thankful to teaching staff, Post graduate department of Kaya Chikitsa
especially Dr. VIJAYA LAKSHMI garu, Dr. NAGESWARA BABU garu, for their
precious suggestions and help throughout the study.

I express highly thankful to my Parents Sri K. RAMAKRISHNAIAH & Smt.
ARUNA whose love, support and encouragement for the initiating sources, which
directed me towards progress and success in each and every step of my life.
I express my special thanks to my Family members Mr. Vijay Kumar, Mr.Guru
Murthy, Mr. Prabhakar, Mr. Sambasivam, Prasanth, Chinnamma, Bhagya
Lakshmi, Suneela, Sujatha, Seshanka, Surya Teja, AND Ganesh for the valuabe
support which made this work possible.
I thank to my good neighbours Smt. Rajamani Garu, Mr. Srinivas & Neeraja,
whose moral support has my spirit in difficult situations.
It is pleasure to convey my thanks to my Co-PG Schoolars and friends especially
Dr. Jayalakshmi and her mother, Dr. Gnana Prasuna and her mother, Dr. V.K.M.
Lavanya, Dr.Padmaja, Dr. Sireesha, Dr. Namrata, Dr. Usha Madhuri, Dr.
Nageswara Rao, Dr. Ravi, Dr.Sivarama Krishna, Dr. Gayatri, Dr. Madhavi, Dr.
Geetha, Dr. Kavitha and Dr. Sandhya for their constent support and helped me
throughout this thesis work directly and indirectly.
I special thanks to Dr. Yashoda MD (Ayu.) lecturer, in B.R.K.R. Ayurvedic
College for her valuable suggestions and encouragment.
I sincerely thankful to Smt. Mamatha & Mr. Chakravarthy, VS GRAPHICS
helps me in the computerized of the thesis.
Hyderabad
February 2008 (Dr. K. SUNEETHA)

CONTENTS
PART – I PRELIMINARY PART
1. Intorcution 1
2. Historical Review of the disease
PART - II THE DISEASE - PANDU ROGA
1. Definition & Synonyms of the Disease 7
2. Classification 9
3. Sareera (Rachana & Kriya) 13
4. Nidana 40
5. Poorva Roopa 48
6. Roopa 51
7. Samprapti 64
8. Sadhya and Asadhya Lakshanas 67
9. Upadravas and Arishta Lakshanas 69
PART - III CHIKITSA
1. Chikitsa krama 71
2. Pathyas and Apathyas 78
PART-IV DRUG REVIEW
1. Criteria for selection of Drug 80
2. Description of individual drugs 82
3. Mode of preparation 99
PART V CLINICAL STUDY
1. Materials and Methods 101
2. Observations 105
3. Results 112
PART - VI
1. Discussion 121
2. Conclusion 125
3. Summary 127
PART - VII
Special case sheet for Pandu Roga130
2. Bibliography 134

INTRODUCTION
Ayurveda is origin from vedas, mainly from Adharavana veda. According to
Ayurveda, definition of health includes both physical and mental well being and
treatment was mentioned for both Swastha in order to preserve health and Atura in
order to treat the disease.
Chaaya and prabha are associated with skin and are based on the condition of
Bhrajaka pitta. The discoloration like the colour of ketaki dooli, swetha, peeta, harita
etc., are the manifestations of pathological process caused not only by the etiological
factors of vitiated doshas but also by consumption of mrit in pandu roga.
The pandu roga is one of the commenest alitments prevalent not only in India
but also world wide. The panduroga is included under the heading of
"Varnopalakshita Roga" ie., Varna pradhanya disease. It is known since ancient
times. The disease is referred as Vilohita, Harima, and Halima in vedas and susrutha
named it as Panaki, Laghavaka and Kumbhahwa.
William D.Whitney an eminent authority of vedic literature compared viloma
with anaemia. It is the commonest disease irrespective of age, sex and religion. It is
prevalent in women, pregnant in specific. As the prevalance of the disease is more
comparatively research studies are needed to evalutate proper eradication procedure,
with the help of the system of medicine which has been existing since many centuries
i.e. Ayurveda. The iron deficiency is the commonest nutritional dificiency world over
and its prevalence is highest in India.
According to NFHS suffering with Anaemia.
Female Children
All over India 50% 70-72%
Andhra Pradesh 52% 75%

Panduroga can be compared to a state of Anaemia in modern system of
medicine, in which the haemoglobin concentration falls bellow the accepted normal
range due to the failure of haemoglobin synthesis and other conditions mentioned in
nidana and sareera. In particular where unhygienic, low socioeconomic and faulty
food habits are the contributing factors. It is even more common in pregnant women.
Its prevalence in all the age groups and in both the sexes interested reserchers right
from ages.
The Ayurvedic classics have mentioned a number of effective formulations for
treatment of pandu roga keeping in view of the above factors, the present study
entitled as "A clinical study on the effect of Bhaskara lavana choornum in pandu
roga" is carried out.
The efficasy of this formulation in pandu roga can be justified by its indication
in Alpa rakta condition explained in the pages that follow. The preparation Bhaskara
Lavana churna is taken from Agnimanandya chikitsa Adhyaya of Bhaishadjya
Ratnavali. The drug fulfils the qualities of Bahu guna, Yogya, Sukha aswadana,
Preenana, vyadhi nashana, avipathkara and gandha varna rasopeta.
Thirty patients are randomly selected from those attending the out patient
department of post graduate unit of kayachikitsa, Dr. B.R.K.R. Govt. Ayurvedic
college / Hospital, Erragadda, Hyderabad. The drug Bhaskara lavana churna is tried
on 30 patients and results are assessed periodically.
The results are encouraging, which are discussed in length, in the chapter of
results seperately, the entire work is devided into VII parts, covering all the aspects of
the disease. Pandu roga and Drug Bhaskara Lavana Churnam.Part I consists of introduction and historic review of the disease. Part II consists of
various aspects of the disease such as definitions, synonyms, classification, sareera
Rachana, Sareera kriya, Nidana, Samprapti and other aspects. Part III consists of
chikitsa krama of pandu roga in general. Part IV consists of various aspects of drugs in
detail. Part V consists of clinical study, under which, materials and methods,
observation and results are included. Part VI consists of discussion, conclusion and
summary. Part VII consists of special case sheets and Bibliography.

HISTORICAL REVIEWAyuevedia is the most ancient system of medicine among the different systems
of medicine existing.
Vedas are apourshayas. Vedas are the oldest knowledge books known to men
according to Indian thought. So, it would be appreciable to explore the history right
from the period of Vedas to present period. On the scale of time, next to Veda are
Puranas, Upanishads and Brahmanakas, Samhitas, Sangrahas, Nighantus and
Arvacheenakala Grandhas. Now, let us consider some of the points related to
Panduroga mentioned in different texts/literature/knowledge available till date in a
stepwise manner under the following headings.
1. Veda Period
2. Purana Period
3. Samhita and Samgraha Period
4. Avracheena Period
1. Vedic Period: In Vedas there are many references about the disease Pandu.
Rigveda: Pandu roga has been mentioned under the name Harima. 'Suryanamaskaras'
and prescribed as its treatment in Rigveda.
2. Yajurveda: In Yajurveda there is a reference about Pandu. A reference from this
veda quoted that there is some relation between yakrit, kloma and pitta in relation to
Panduroga. Charaka and Susruta has elaborated this point in detail by stating that the
moolasthana of raktavaha srotas lies with yakrit and pleeha and the predominant dosha
associated with Pandu is pitta.
3. Atharvanaveda: This veda reiterated the same as above. There are references like
Vilohita, Harima, Halima which can be taken as synonyms of Pandu. The significance
of sun rays is stressed in Atharvana veda for changing the colour in Pandu roga.
Another reference from Atharvanaveda advocates godugdha as a remedy for
Panduroga.

4. Pouranika kala:Garuda Purana, valmiki Ramayana and Agni purana have also
mentioned about 'Pandu roga'. In Garuda purana lohachoorna with takra anupaana is
prescribed especially for Pandu patients, and Nidana, Lakshanas, Pathyaapathya
vicharanas are also explained in detail.
Mahabharata states that the Hastinapura king had suffered from Pandu roga
whose name itself is Pandu Raju. He acquired the disease as a curse from a saint. This
explains the karmasiddhanta of Panduroga. King Pandu acquired sterility due to Pandu
Roga as a complication and he even died of the disease.
5. Samhita & Sangraha kala: This is the golden period of ayurveda, since most of
the Ayurvedic Classics like Charakasamhita, Susruthasamhita, Bhelasamhita,
Hareetasamhita, Kasyapasamhita took shape in this period. These samhitas are the
basis of Ayurveda that is being practiced throughout the world. Panduroga has been
described in detail along with treatment in all classics as stated below.
Name of the book Sthana Chapter No.
1. Charaka Samhita Chikitsa 16th
2. Susruta Samhita Uttara 44th
3. Astanga Sangraha Nidana 13th
4. Astanga Sangraha Chikitsa 18th
5. Astanga Hridaya Nidana 13th
6. Astanga Hridaya Chikitsa 16th
7. Sarangadhara samhita Poorvakhanda 7th
8. Madhavanidana 8th
9. Bhavaprakasha Madhyamakhanda 8th
10. Vaidhya chintamani Pradhama samputa 4th
Even the works such as Chakradatta, vangasena, Yogaratnakara,
Bhaishajyaratnavali, Basavarajeeyam, Madhavanidanam and Sarangadhara samhita
also give a detailed description of Pandu roga.

We can find references of a number of medicinal plants that are proved to be
useful in Panduroga in Dhanvanthari, Kayyadeva and Astanga nighantus. The author
of Vidhyachintamani Srimad Indrakanta vallabha charyulu stated that Pandu is a
senapathy (chief of army) for the disease Kshaya.
With the advent of Rasakala, some mineral and metallic preparations replaced
the herbal drugs, after shodana and marana. Rasaratnasamucchaya, Rasapadhati and
other literatures on Rasashastra have thousands of preparations which are prescribed
for the management of Pandu.
5. Aravacheena Period: This is the starting period of modern system of medicine,
William D. Whitney, who is a known authority on vedic literature compared vilohita
mentioned in Vedas to anaemia.
Hippocrates, the father of modern medicine in 460BC, described anaemia like
symptoms such as pallor and weakness. he attributed these symptoms to the chagnes
of blood. Anaemia, in those days, was found predominately in virgins and was hence
called demarbo virgina (the sickness of virgins) by Dr. Johanns Large in 1554 A.D.
He described this is pallor of checks, breathlessness on exertion, increased pulsation
of the temporal vessels and dysponea on climbing stairs or dancing. This illness was
later termed Chlorosis and clinical use of iron was first initiated in 17th century by
Thomas Sydenham.
Dr. Grambiel andral succeeded in describing the changes of blood
micorscopically in Anaemia during 1797-1876.Also the work of Thomas Addison, during the same period contributed to the
discovery of one of the type of anaemias - The Addision's Anemia. This is later on
termed as Perinicious Anemia, After the efforts of Dr. Wilks in 1855 and Dr.
Biermer's in 1872. Another type of anemia - Spleenic Anemia was described by Dr.
Banti in 1882. Dr. Minot and Dr. Murphy in 1926, conducted a trial of diet consisting
of liver and beef, which are rich in iron. this showed considerable improvement of
Perinicious Anemia. However, they could not provide enough explanation for the
same. This was bridged by the muchapplauded work of Dr. Castle.

G.R. Minot, W.P. Murphy and G.H. Whipple in 1934 shared Nobel Prize in
Physiology and Medicine for their work concerning the treatment of Anaemia with
liver. In 460BC Hippocrates also explained the importance of consumption of liver in
combating anaemia during pregnancy. The same was also recommended by Charaka
and Susrutha in 500 B.C.
Now-a-days, there are many clinical, pathological, and diagnostic technologies
available in regards to Anaemia. As per Modern system of medicine, anaemia is of
many types. It is being treated on the whole by supplement of Iron and its source in
the form of daily nutrition or in medicines which would be seen in detail in the topics
that follow, as and when in need. This disease is prevalent in most communities due to
various causes and yet a lot has to be achieved.
The above review clearly indicates that Pandu is blood related disease, its
relation is to Raktavaha srotomoolas has long back been mentioned and Ayurvedic
physicians were aware of the disease and its management since vedic period. Thus
history of Pandu and its corelated disease. The Anaemia of Modern system of
medicine has been briefly outlined.
References:
1. Mc. Odonell and Keeth Vedic Index Vol II.
2. Whintney, W.D. Translation of Atharvana Veda, by Motilala Banarasidas,
1962.
3. Garuda Purana Chapter 184/29
4. A short history of Medicine II Edition by Singer and Underwood.
5. Pandu Roga by Pathak R.R. Published by C.A.R.I., 1987
6. Henry A.S. The Origin of the medical terms, Batlimore 1961.
7. Vedomme Ayurved.
8. Susruta Samhita Uttara sthana 44th chapter.
9. History of Indian Medicine by Dr. Rama Rao, P.V. Sharma and Others.

DEFINITION AND SYNONYMS
Charaka classified rogas according to Ruja, Varna, Samuthana, Samsthana
and Stana. In this classification the disease pandu falls in the group of varna. In panduroga there is some significant change in the normal colour of the body.
There are many definitions in Ayurvedic literature. One nirukti quated by vijaya
rakshit is
“Pandutwenopo lakshito roga pandu roga”
(madukosa)Which difenes that a person who acquires pandu varnatvam is a pandu roga.
“Swetha peeta samayukta panduvarna prakirtitaha”(Amarakosa)
The combination of white and yellow colours in equal proportion are called
pandu roga
“Pandu shabdena swetatwa mabhideeyate:
(Dalhana on S.Su.33/23)
Dalhana, the commentary on susrutha samhita, started that pandu means white
colour.
“Pandutwam teshu chaditam yato ataha pandurityuktasa rogaha”(A.H.Chi. 13/13)
Excessive colour of pandutwam is seen in panduroga
“Sarveshu chiteshyapi pandu bhavo yato adhikaha khalu panduroga”(Su. Uttara 44/4))
Excessive pandu varnam is seen in pandu roga.
“Panduhu swetavarna ketakidholi sannibha peetabhagarda varnabhedcha”(Shabdasthoma)
Pandu has been compared with ketaki dhooli or ketaki pushpa colour i.e. thatcan be considered as combination of white and yellow colours.
It can be concluded basing on the above that the disease has been regarded as an
ailment associated with colour of patient.

SYNONYMS OF PANDU ROGAThe synonyms of pandu roga available from vedic literature are vilohita, harima,
halima.
Ref – Adharvana Veda 4-9-3-, 1-22-22)
“Sa kamala panaki pandu roga kumbahwaya laghavakoalasakya vibhashyatelakshana masya kristam nibodha vakshyamyanu poorvashasthoth”
(Su.Uttara 44)
Susrutha used the terms Kamala, Panaki, Panduroga, Kumbahwayo,Laghavaka, Alasaka as synonyms of the disease.
Definition: The word Anemia is derived from two words ‘an’ which means with or
less and “emia” which means blood condition. Pandu (Anaemia) is a condition of
reduction in the haemoglobin concentration of the peripheral blood below the normallevel in relation to age and sex.
These condition of white and yellow colors in equal proportions are called
panduvarnam.
Normal adult male – 16 gms/dl
Normal adult female – 14 gms /dlAnaemia is also said to be present in adults if the "Hematocrit (packed RBC) is
less than 41% in males and 37% in males. Anemia is also seen in patients in whom the
RBC is less than the normal.
Normal adult male RBC – 5,20,000/cumm.
Normal adult female RBC – 4,700,000/cumm
References:l Charaka sutra sthanam 18/42
l Madhavanidanam
l Amarakosha
l Susrutha suthra stana 33/23 – Dalhana commentary uttara sthana – 44/4
l Astanga hridaya Chikitsa sthana – 13/3
l Sabdarnavam,
l Shabda sthoma mahanidhi

CLASSIFICATION OF PANDU ROGA
The pandu roga description available as old as from vedic literature. In vedic
literature there is no evidence of any classification regarding pandu roga. Only
synonyms such as Harima, Halima, Vilohita are found on the literature.
The detail description of pandu roga and is classification starts from Ayurvedic
samhitas only. The classification of pandu roga most of the acharyas accepted 5 types.
Those are 1. Vataja (2) Pittaja (3) Kaphaja (4) Sannipathaja
(5)Mrudbhakshanaja. But susrutha mentioned only 4 types. He excluded the
Mridbhakshanaja pandu and he explained for this as Mridbhakshanaja pandu may
include in vatadi doshaja pandu’s according to the rasa pradhanata of mrit1.
In Haritha samhita “Rukshana” pandu is appears of mridbhakshanaja pandu. The
term Rukshana may be used, because mridhbhakshanaja pandu mainly cause the
Rukshanatwa of the body2.
Astanga sangrahas and many other texts followed the same order while susrutha
mentioned four types.
Some commentators classified Pandu into eight types as follows:
1. Vataja 2. Pithaja
3. Kaphaja 4. Sannipataja
5. Mritbhakshanajanya 6. Sakhasrita kamala
7. Koshtasrita kamala 8. Haleemaka
A Classification states that Mritbhaskhanajanya Pandu falls under sannipataja
Pandu because of the following reasons.
Intake of Kashaya rasa predominant Mrit leads to Vataja Pandu
Intake of Kshara rasa predominant Mrit leads to Pittaja Pandu
Intake of Madhura rasa predominant Mrit leads to Kaphaja Pandu
Probably this may be the reason why Susruta included Mritbhaskhanajanya
Pandu under Sannipataja Pandu.

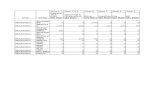
Classification of pandu according to different authors
S.No Types Vata Pitta Kapha Tridosha Mritbhakshanaja
1 Charaka 5 + + + + +
2 Susrutha 4 + + + + -
3 Vagbhata-1 5 + + + + +
4 Vagbhata-2 5 + + + + +
5 Madhavakara 5 + + + + +
6 Sarangadhara 5 + + + + +
7 Bhavaprakasa 5 + + + + +
8 Haritha 5 + + + + Rukshana
9 Yogaratnakara 5 + + + + +
10 Basavarajeeyam 5 + + + +
11 Vaidhya chintamani 5 + + + + +
MODERN ASPECT
Classification:
Classification of anaemia is 2 types
1. Pathophysiologic classification
2. Morphological classification
1. Pathophysiology classification (Based on Etiology)
1. Anaemia due to blood loss: This has further two types
Blood loss: 1. Acute haemorrhage
2. Chronic Haemorrhage
2. Anaemia due to impaired red cell formation: various causes may produce
this anaemia. These causes are
I. Deficiency of haematinic factors
Ex: A) Iron deficiency

B) B12 deficiency
C) Folate deficiency
D) Protein deficiency
II. Haemopoietic stem cell proliferation differentiation abnormality
Ex: A) Aplastic
B) Red cell aplasia
III. Bone marrow failure due to systemic diseases
A) Anaemia of infections
B) Anaemia of renal diseases
C) Anaemia of liver disease
D) Disseminated malignancy
E) Endo crinopathies
IV. Bone marrow infiltration
Ex: A) Leukaemia
B) Lymphomas
C) Myclosclerosis
D) Multiple myeoloma
V. Congenital anaemia
Eg: A) Sideroblastic anaemia
B) Congenital dyserythropoietic anaemia
III. Increased destruction (Classification of Haemolytic anaemia)
a) Haemolysis (Intransic)
1. Membrane – a) Heriditary spherocytosis
b) Eleptocytosis
2. Haemoglobin a) Sickle cell
b) Unstable haemoglobin
3. Glycolysis Pyruvati kinase etc4. Oxidation G6 PD deficiency
b) Haemolysis (Extrinsic)
1. Immune a) Auto immune
b) Drug toxicity
c) Lympho preliterative disease

2. Morphological classification:
Macrocytic anaemia: In this condition the size of RBC increases i.e. about 94.
Normal is 78-94 as M.C.H. proportionately increased. Eg: Tropical nutritional
anaemia, megaloblastic anaemia of pregnancy, pernicious anaemia1.
Normocytic anaemia: There is reduction in RBC with if all a slight increasing
MCV, MCH remains normal throughout. Eg. Sudden loss of blood due to the
antipartum, post partum haemorrhage2.
Microcytic normocytic anaemia: There is reduction in red cell volume, Hb
content with less MCH eg. Actute and chronic inflammatory disease3.
Microcytic hypochromic anaemia: Reduction in RBC volume and Hb content
and reduced MCH4.
Eg: Iron deficiency anaemia.
References:
1. Susrutha samhita uttarastana 44th chapter
2. Haritha samhita truteeya stana 8 th chapter
3. Charaka samhita sutra 18th, chikitsa 16th chapter
4. Susrutha samhita uttarastana 44th chapter
5. Astanga hridaya nidana stanam 13th chapter
6. Astanga samgraha nidana sthana 13th chapter
7. Madhava nidana 8th chapter
8. Bhavapraksha medhyamakanda II volume
9. Sarangadhara samhita
10. Yogarathnakaram madhymakhandam Vol I pandu roga prakarana
11. Haritha samhita truteeya stana 8th chapter
12. Basava rajeeyam panchama prakarana
13. Text book of pathology, by Byoid
14. Hand bood of human physiology
15. Medicine for students by Dr. Golwalla, 15th Edition
16. Davidson’s principles and practice of medicine – 15th Edition

SHAREERA RACHANA AND KRIYA
“Dosha Dhatu Mala Moolam Hi Shareeram”
Human body build up three doshas, seven dhatus and trimalas. Any disease
occurs the vitiation of dosha, doshyas from their normal functions.
I. The Doshas involved in the samprapti of pandu roga are:
1. Vyanavata
2. Samanavata
3. Pachaka pitta
4. Rajakapitta
5. Bharajaka pitta
6. Kledaka kapha
II. The Dhatus are involved in Pandu Roga are:
1. Rasa 2. Rakta
3. Mamsa 4. Medas
5. Asthi 6. Majja
III. Other factors:
1. Agni 2. Ojas
3. Yakrit 4. Pleeha,
5. Hridaya 6. Raktadharakala
7. Raktaasaya 8. Amasaya
8. Saraktamedas
Since the anatomical and physiological aspect of the above mentioned factors is
important in the study of the pandu roga. Abrief description of the above factors is
needed.

Doshas:1. Vata
a. Yyanavata:
Location: Hridaya – Seat of vyanavata (Vagbhata)
Charaka and Susruta did not mentioned about the place of Vyanavata.
Gunas:
In general, it possesses all the gunas of vayu. They are ruksha, laghu, seeta,
khara, sookshma, and chala.
Karmas:
i. Locomotion is entirely dependent on Vyana Vayu
ii. Rasa Raktadi samvahana
iii. Sweda & Asrik sravana.
iv. Sareera Chestha: Prasarana, akunchana, vinnamana, unnamana and
tiryaggamana
v. Jrimba pravartana
vi. Anna aswadana
vii. Sroto vishodhana
viii. Dhatu tarpana
b. Samanavata: The Vayu that gives strength to Pachaka pitta is called samana
vayu.
Location: It resides near pachaka pitta. It courses between Amashaya and
Pakwashaya. It is also been said that it also occurs in Sweda, Rakta, and Ambu vaha
srothas.
Gunas: In general, it possess all the gunas of vayu.
Karma: The important function of Samana Vayu is to strengthen Jataragni. Thus
it helps in the digestion of food. After digestion, it divides ahara into saara and Kitta
bhaga. According to Vagbhata, samana vata does ahara graham (accepts food) into
koshta, anna grahana, Saara-Kitta vibhajana and it pushes the Kitta into Pureesha vaha
srothas.

2. Pitta
a. Pachaka Pitta: We know that the entire body depends on the food we
consume and the way it is absorbed and assimilated into the body tissues. The type of
pitta that does the above said functions is dependent on Pachaka pitta. This pitta also
regulates digestive capacity, Dhatu parinama and provides nutrition for the body. This
is called as Pachakagni, Koshatagni, Antaragni, Kayagni, Jataragni or Agni,
depending upon the context. It has also been said that vitiation of pachaka pitta leads
to disease.
Location: Pachaka pitta is located in between Amashaya and Pakwashaya. The
region between amashaya and pakwashaya is termed as Grahani and it contains
Pittadhara kala. In other words, Pittadhara kala or Grahani is seat of Pachaka Pitta.
Gunas: Laghu, Vishra, Sara, Dravam, Sneha, Teekshna, Ushna, and Visada
Rasas: Amla and Katu
In Pachaka pitta, the tejo guna predominance is seen and because of it, the
dravatwa guna in pachaka pitta is less when compared to other pittas.
Karma: It has wide range of fuctions. The important functions among them are
as follows:
i. It digests the four types of food and liquids we consume.
ii. It differentiates Saara bhaga and Kitta bhaga of the food after digesting it
and absorbs into the body.
iii. It is termed as ‘Jatara Agni’ many times, because it controls the action of
other 12 types of agni in the body.
iv. The other factors that are dependent on the action of Pachaka pitta are
given below.
A. Ojas B. Ayu.
C. Deha pushti D. Bala
E. Utsaha. F. Health in general
G. Colour of skin
It is also said that if Kayagni is healthy, then the person achieves longevity, else,
he acquires diseases and if the Kayagni is totally destroyed, the person dies.

b. Ranjaka Pitta.
The pitta that is transforms rasa dhatu into rakta dhatu is called Ranjaka pitta or
Ranjakagni pitta.
“Amasayaasryayam Pittam ranjakam rasaranjanath” (A.H.S. 12-12)
Location: According to Susruta - Yakrit and pleeha
According to Vagbhata – Amashaya
According ot Sarangadhara – Hridaya
Gunas: Same as that of pachaka pitta
Karma: Ranjaka pitta gives colour to the Rasa Dhatu when it is circulated
through Yakrit and Pleeha and transforms it into Rakta Dhatu. This act is even
controlled by Rakta Dhatwagni.
c. Bharajaka Pitta:
The temperature of the body as well as the colour of the skin are dependent on
Bhrajaka pitta.
“Twakstham bhrajakam bhrajana twachaha” (A.H.S. 12-14)
Location: Skin is the site of Bhrajaka pitta. Avabhasini, which is the first layer
of skin, lodges Bhrajaka pitta according to Dalhana.
Gunas: Same as pachaka pitta.
Karma:
i. The main action of Bhrajaka pitta is to manintain temperature of the body.
ii. In general, Bhrajaka pitta gives different colours to the body depending upon
the Mahaboota composition of the skin.
According to Charaka
Jala & Akasa Mahabhoota predominance leads Goura Varna
Pridhvi Mahabhoota predominance leads Krishna Varna
Pridhvi & Akasa Mahabhoota predominance leads Krishna Syama Varna
According to Susruta:
Jala & Akasa Mahabhoota predominance leads to Gowra Syama Varna
iii. It reflects different characteristics of body in health and diseased states.
iv. It absorbs the oils or medicines applied over the surface of the skin, in the
form of Abhyanga, Parisheka, Avagahana and Lepana.

3. KAPHA
Kledakakapha
Location: The site of kledaka kapha is Urdhwa Amashaya
Gunas: In general, it possesses all the gunas of Kapha such as Shingdha, Seetha,
Guru, Manda, Slakshna, Sandra, and Sthira.
Karma: 1. Anna sanghata 2. Kledana
The impirement of these functions are supposed to vitiate ahara which may result
into Pandu.
Dhatus
The Dhatus that are involved in the pathogenesis of Pandu are Rasa, Rakta,
Mamsa and Meda as per several authors.
Rasa Dhatu: The involvement of rasadhatu is not directly related in the
Pathogenisis of Pandu roga samprapti. Pandu is included under rasa prodoshaja
diseases.
Location: Hridaya and Dasadhamanis. It circulates through out the body along
with Rakta with the help of Vyanavatha.
Pramana: 9 Anjalis
Rasa: Madhura
Varna: Swetha/Sukla
Formation: It is formed from Saarabhaga of ahararasa after it has been subjected
to jatarapaka and Rasadhatwagnipaka. It stays in each dhatu for a period of 3015
kalas. It circulates upwards like Agni, downwards like jala and transversely like
shabda.
Karma: 1. Tarpana 2. Jeevana & Preenama 3. Vardhana 4. Dharana
5. Yapana 6. Uttaradhatu poshana

Rakta Dhatu:
According to the Ayurvedic view, Rasadhatu contributes to the formation of the
rakta dhatu with the help of Ranjaka pitta. Therefore the Ranjakapitta plays an
essential part in the formation of the Raktadhatu.
“Tejo Rasanam sarvesrham manujanam yaduchyathe”
Pittoshmanahasia Ragena Raso Raktatramrucchati
The etiological factors of Raktadusti are similar to the Panduroga etiological
factors. The characteristic features of Pandu quite opposite to the characters of
Shuddharaktapurusha. The Pandu roga is mentioned under Rakta kshaya lakshanas.
“Yathu Yakritpleeho pittam Tasmin ranjakognirthi sangna
Sa Rasasya Ragakruduktha ha”
Location: Yakrit, Pleeha, Hridaya, Rakta vahadhamanis and Sarakta medas. It
circulates in the entire body along with rasadhatu.
Pancha bhoutika Sangatana of rakta:
“Panchabouthikam twapare Jeevarakta maharacharyaha
Visratha Dravatha Ragada spandanam Laghuta tatha
Bhumyadenam guna hothe drushanthe chatra shonita
Qualities of Rakta dhatu Bhuta Pradhanyatha
1. Visratha (Fleshy odour) Prodhweebhuta
2. Drava (Fluidity) Jalabhuta
3. Raga (movement) Agnibhuta
4. Spandhana (movement) Vayubhuta
5. Laghuta (lightness) Aakashabhuta
Rasa: Madhura/Madhura lavana rasas.
Varna of suddha rakta dhatu:
“Tapaniyendra Gopabham padmalaktaka sannibham
Gunjaphala savarnacha vishuddam vidhisonitham”

The pure blood looks lika a bright “Indragopa”
Looks like Padma (Lotus flower) and Latuka (Laksha)
Gunjaphala Savarnam – Brightly red like gunja seed. These colour indicative of
pure blood.
Pramanas: Eight Anjalis.
Gunas: Anushna, Seetha, Snigdha, Guru, Visra and Asamhata and Gunas of
Panchamahabhutas.
Karma: Jeevana, Dharana, Bala, Varna, Sukhakara, Ayushkara, Pushtikara,
Indriyaprasannatwa, mamsapushti and sparshagnanakara.
Shuddha Raktasaara Purusha Lakshanas: A person whose karnamukha,
jihwa, nasa, osthta, pani, paadatala nakha, lalata and mehana are having snigdha and
rakta Varna is regarded as Shudda Raktasaarapurusha.
Ojus:
The involvement of ojus is specifically mentioned in Charaka Chikitsa 16th
Chapter. As the formation of all Dhatus is impaired in the disease Pandu, the
formation of the essence of all Dhatus also impairs and ojokshaya lakshanas are seen.
Location Hridayam, Sarva shareeram
Types Para and Apara
Pramana Para Ojus – Asta bindu
Apara Ojus – Ardhanjali
Rasa Madhura
Varna Eshatpeeta varnam (or) Sarpivarnam.
Karma Balakaram, Vyadhi kshamatwakaram, Tushtikaram,
Pushtikaram, and it is associated with Ayu (life).

MODERN ASPECT
The circulatory system is the transport system that supplies O2 and substances
absorbed from the gastrointestinal tract to the tissues, returns CO2 to the lungs and
other products of metabolism to the kidneys, functions in the regulation of body
temperature, and distributes hormones and other agents that regulate cell function.
The circulatory (or) vascular system is divided for descriptive purpose into two
main parts
1. The Lymphatic system
2. The Blood circulatory system
The Disease pandu roga is similar to the disease 'Anaemia' of modern
medicine. Anaemia is concerned with lower haemoglobin levels in the blood. It is a
condition in which the oxygen carrying the capacity of the blood is reduced.
The blood: Blood is described liquid as a connective tissue. It acts as communication
between the cells of different parts of the body and the external environment. Blood:
constitutes 7% of the body weight. It is about 5-6 liters.
Other Physical characters of blood:
Viscocity – 4.5-5.5 (higher than water)
Temperature – About 380C ( Slightly higher than normal body temperature
PH-range – 7.35 to 7.45
Total blood volume – 72-10ml/kg body weight.
Composition of the blood:
Microscopically blood is composed of two parts.
1. Blood plasma: Contains dissolved substances (55%), water, plasma proteins
clotting factors, inorganic salts, nutrient materials, hormones, enzymes, antibodies and
gasses.

2. Formed elements: Contains cell and cell fragments (45%) – Red blood cells or
Erythrocytes, white blood cells or leucocytes and platelets or thrombocytes present
less than 1% of the total blood volume.
Formed elements: The element of the blood are:
1. Erythrocytes (Red blood cells)
2. Leucocytes (White blood cells)
I. Granular leukocytes (Granulocytes)
a. Neutrophils
b. Eosinophils
c. Basophils
II. Agranular leukocytes (Agranulocytes)
a. Moconcytes
b. Lymphocytes (T cells, B cells and Natural killers)
3. Platelets (Thrombocytes)
ERYTHROCYTES (The red blood cells)
Erythrocytes: Of all the cells of the body RBCs are most abundant. The major
Function of RBC also known as erythrocytes is to transport haemoglobin, which in
turn carries oxygen from lungs to tissues. Haemoglobin is present in RBC in humans.
RBC have other functions besides transport of hemoglobin. They contain large
quantities of carbonic anhydrase, which catalyses the reactions between water andCO2, increasing the rate of this reversible reaction to as much as several thousand
times. This makes it possible for water in blood to react with huge CO2 and thereby
transport it to lungs from tissues in the form of BiCarbonate Ion (HCO3).

The Haemoglobin in the cells is an excellent Acid – Base buffer and is
responsible for most of buffering power of whole blood.
Size and shape of RBC: Normal RBCs are bioconcave discs having a mean
diabmeter of about 7.8 m and a thickness of about 2.5 mm at the periphery and 1mm
of less in the center. The shape of RBCs can change remarkably as the cells pass
through capillaries.
Concentration of RBCs in the blood: The average volume of the red blood
cells is 83 cubic micrometer
In normal men - 5,200,000 (+/- 300,000)
In normal women – 4,700,000 (+/- 300,000)
Quantity of Hb in the cells: RBCs can accommodate 34 gms/dl of Hb in the cell
fluid, when the heamatocrit ( the percentage of blood that is in the cells- normally 40
to 45%) and the quantity of haemoglobin in each respective cells are normal. The
whole blood contains an average of Haemoglobin in
Men – 14-16 gms/dl
Women 12-15 gms/dl
Infants – 14-20 gms/dl
Each gram of pure Hb is capable of combining with about 1.39 ml of oxygen.
In normal man, Hb/dL of blood carries more than 21 ml of O2.
In normal women, Hb/dl of blood carried more than 19ml of CO2.

PRODUCTION OF RBC AS PER AGE:
l Yolk Sac: In early few weeks of embryonic life – primitive nucleated RBC areproduced.
l Liver spleen & Lymphnodes: During mid trimester of gestation – the liver isthe main organ or production of RBC, although ressonable number of RBC areproduced by spleen and lymph nodes.
l Bone marrow: During the last months of gestation – RBC are producedexclusively from bone marrow.
l Upto 5 years – Bone marrow of all the bones produces RBC.
l After 20 years – Long bones stop prodcing RBC since fatty tissues occupymost of the cavity. Beyond this age RBCs are produced by marrow ofmembraneous bones such as verterbrae, sternum, ribs and ilia.
Origin and development of Red Blood Cells: The first cell that can be
identified as belonging to the red blood cells series is the proerythroblast. Once the
proerythroblast has been formed, It divides several more times, eventually forming
many mature red blood cells. The first generation cells are called Basophilic
erythroblasts, which then develops into a Proerythroblast (Normoblast) erythroblast,
the first cells in the sequence that begins to synthesize hemoglobin. The poly
chromatophilic erythroblast next develops into an acidophilic erythroblast, in which
hemoglobin synthesis is at a maximum. In the next stage, the acidophilic erythroblast
ejects is nucleus and becomes a reticulocyte. The reticulocyte in turn becomes an
erythrocyte (or) mature red blood cell. Once the erythrocyte is formed, it leaves the
marrow and enters the blood stream.
Formation and destruction of red blood cells and recycling of hemoglobin
components.
Red blood cells live only about 120 days because of the wear and tear inflicted
on their plasma membranes as they squeez through blood circulation worn-out red
blood cells are removed from circulation and destroyed by fixed phagocytic

macrophages in the spleen and liver. The globin and heme protions of
hemoglobin are split apart. Globin is brokendown into amino acids, which can be
reused to synthesize other proteins. Iron removed from the heme portion. Associates
with a plasma protein called transferring, which transports iron in the blood stream. In
muscle fibers, liver cells, and macrophages of the spleen and liver, iron detaches from
transferring and attachs to iron storage proteins called ferritin and hemosiderin.
Upon release from a storage site or absortion from the gastrointestinal tract, iron
attaches to transferring. It is then transported to bone marrow, where RBC precursors
take it up through receptor – mediated endocytosis. For use in production of new
hemoglobin molecules. Erythropoiesis in red bone marrow results in the production of
red blood cells, which enters the circulation.
At the same time, the non-iron protion of heme is converted to biliverdin,
agreen pigment, and then into bilurubin, an orange pigment. Bilurubin enters the
blood and is transported to liver with in the liver, bilirubin is secreted by liver cells
into bile, which passed into the small intestine. Again which passed into the large
intestine, in large intestine bacteria convert bilurubin into urobilinogen. Some
urobilinogen is obsorbed back into the blood, converted to urobilin, a yellow pigment,
and excreted in urine. Most urbilinogen is eliminated in feces in the form of a brown
pigment called stercobilin, which gives feces their characteristic colour.
Erythropoietin: The principal factors that the stimulates red blood cell production is
a circulating hormone called erythropoietin.
Tissues oxygenation is a basic regulator of RBCs production. Any condition that
causes the quantity of oxygen transported to the tissues to decrease ordinarly increase
the rate of RBCs production.
Other factors controlling erythropoises: The red cells are constantly being
destroyed and regenerated. Certain factors are necessary for the formation of red
blood cells. They are:
1. Diet: Proteins are very valuable supply of essential amino acids for the synthesis of
hemoglobin.

2. Metals: Iron, Copper, Cobalt, Calcium and Manganese. Iron is essential for the
formation of hemoglobin. Copper, Cobalt, Calcium and Manganese are indirectly
helpful in the formation of RBCs.
3. Bile satls: Presence of bile salts in the intestine is essential for the proper absorption
of these metals.
4. Endocrine glands: Certain glands such as thyroid and adrenal glands are having
unknown role in the metabolism of RBC.s
5. Vitamins: Vitamin C, B complex, and Folic acid are helpful in the formation of
RBCs.
Erythropoietin and its formation: Erythropoietin is a hormone found in circulating
blood. It is a glycoprotein with molecular weight of 34,000. In the absence of
erythropoietin, hypoxia has little or no effect in stimulating RBCs production. On the
other hand, when Erythropoietin system is functional, hypoxia causes marked increase
in Erythropoietin production, and this in turn enhances RBCs production until hypoxia
is relieved.
Role of kidneys in the formation of erythropoietin: In normal person, about 90% of
all erythropoietin is formed in the kidneys. Mainly, the liver forms the remainder. The
renal tubular epithelial cells secrete the erythropoietin because anemic blood is unable
to deliver enough oxygen from peritubular capillaries to the highly oxygen –
consuming tubular cells, thus stimulating erythropoietin production.
Effect of erythropoietin on erythrogenesis: The important effect is to stimulate the
production of proerythroblasts from hemopoietic stem cells in the bone marrow. Once
the proerythroblasts are formed, the erythropoietin causes these cells also to pass more
rapidly through the different erythroblastic stages than normal, further speeding up the
production of new cells. The rapid production of cells continues as long as the person
remain in low oxygen state or unitl enough RBCs are producted to carry adequate
amounts of oxygen to the tissues.
Formation of RBCs – Requirement of Vitamin B12 and Folic Acid: For the final
maturation of RBCs, two vitamin – B12 and Folic acid are very imporntat. Both of

these are essential for the synthsis of DNA, because each in a different way is required
for the formation of Thymidine Triphosphate, an essential building block of DNA.
Therefore, lack of either of these causes diminished DNA and consequently, failure of
nuclear formation and division. Therefore, it is said that Vit. B12 and folic acid
deficiency causes ‘maturation failure’ in the process of erythropoiesis.
Folic Acid: The normal concentration range of folic acid in blood is 5-15 mg/ml. It is
found mainly in green vegetables, liver and whole grains. The reference nutrient
intake is 50g/day. Following its uptake by the mucosal cells, folate undergoes
reduction and methylation. Once, it arrives in the liver, the methyl derivative is taken
up, undergoes demethylation and the tetrahydrofolate is converted into polyglutamyl
forms with 4,5 or 6 residues. The polyglutamyl forms contstitute a store of the
vitamin. Prior to release from the store, and into the circulation, the compound is
converted to N-methyl-derivative, from which all but one of the glutamyl residues is
removed.
Folate deficiency: The members of society most liable to folate deficicney are
pregnant women and the elderly. It is now recognized as being good practice to
administer folate supplements as soon as pregnancy is confirmed and to continue until
term. In the first trimester the supplementation in prophylactic, benefiting the foetus,
because there is clear evidence that the occurance of neural tube defects such as Spina
bifida and anencephaly is reduced by as much as two-thirds. Later in the pregnancy
the supplementation is to prevent folate deficiency in the mother, which can easily
arise as foetal demands cause depletion of maternal foliate stores.
Less commonly, folate defienciey may be seen in alcoholics, in those patients
being treated with anticonvulsants and in individuals with intestinal malabsorption
conditions.
VITAMIN B12: Normal daily requirement of Vitamin B12 is 1-2 g/day. It enters into
food chain only in food of animal origin. The acid conditions and the proteinhydrolysis that commences in the stomach jointly cause the release of Vitamin B12. In
saliva and also in gastric secretions are a group of mucins, termed R-Binders.

These glycoproteins bind vitamin B12 with high affinity in the acid environment of the
stomach. In the more neutral surroundings of the duodenum the R-binders undergo
hydrolysis, thereby releasing their Vitamin B12.
Intrinsic factor: Maturation of the cell depends on a number of factors, especially the
presence of vitamin B12 and folic acid. These are present in sufficient quantity in a
normal diet. Containing dairy products, meat and green vegetables. If the absorption
of vitamin B12 depends on a glycoprotein called intrinsic factor secreted by parietal
cells in the gstric mucosa. Thus very little or none is absorbed in cases with pernicious
anaemia and after gastrectomy as the intrinsic factor absent. In main it is produced by
the body of the stomach. It is glycoprotein.
The essential property of the intrinsic factor is its ability to bind Vit B12 and to act as
a carrier. The presence of hydrochloric acid probably facilities this binding in the
stomach only the vitamin B12 part enter blood to be transported to red bone marrow.
Process of absorption:
1. The intrinsic factor binds tightly with Vit.B12 and in this bond state, Vit.
B12 is protected from digestion by the gastro intestinal enzymes.
2. Still in the bond state, the intrinsic factor binds to specific receptor sites on
the brush border membranes of the mucosal cells in the ileum.
3. VitB12 is transported into the blood by the process of pinocytosis carrying
the intrinsic factor and vitamin together through the membrane. This is a
process that is dependent on Ca.2+.
Lack of intrinsic factor, therefore causes loss of much of the vitamin, because
of both digestive enzyme action in the gut and failure of its absorption. The transport
of Vitamin B12 in the plasma occurs in association with two major binding
proteins:Transcobalamin I and Transcobalamin II.

IRON METABOLISM:
Metal ion used most frequently in association of proteins often include iron in
their structures (sometimes copper, occasionally manganese).
The use of iron as the metal in biological systems for this purpose seems, in part,
to have arisen due to its great abundance in the environment. It has greater affinity for
already association with, and dissociation from its binding sites on protein i.e., its
kinetic liability. The complexes formed, however, are thermodynamically stable. The
major iron-bearing proteins in the body are not enzymes, however, but the dioxygen-
binding and dioxygen-transport proteins myoglobin and hemoglobin.
1. Sources: All animal food eg. Meat, liver, egg etc., excepting milk and butter.
Vegetables, eg: peas, lentils, green leaves, fruit.
2. Iron intake: In the normal population, requirements for iron replacement range
from 1.0 to 3.2 mg/day, and this must derive from, dietary srouces/Although iron is
widely distributed in foodstuffs, only a proportion, which may be 10% or less, is
absorbed from the diet. For this reason, the minimal amount needed to be ingested
daily is set at 10 times the amount actually lost daily.
3. Absorption and transport: Iron is absorbed mostly from the whole of the gastro-
intestinal tract but a large amount is absorbed from the upper part of the small
intestine particularly the duodenum. Dietary iron is absorbed through the mucosal
cells as Ferrous (Fe++) form. Iron in diet is mostly present as a ferric (Fe+++) state
which is reduced to ferrous form during absorption. Vitamin C, glutathione and amino
acid – SH groups help in reduction of ferric to ferrous form. After entering the
mucosal cell as Ferrous form, the iron molecules are rapidly reconverted into ferric
state. A ferric iron as ferric – hyroxy phosphates combines with a protein, apoferritin
with a protein apoferritin of. The mucosal cells with the formation of iron-phosphorus
protein complex, ferritin, This ferritin is one of the storage forms of iron in the tissue.

4. Absorption of iron depends upon the factors: The acidity of the gastric juice
helps absorption. The gastric HCL helps reduction from ferric form to ferrous. Partial
gastrectomy often leads to iron deficiency anaemia. Calcium small amount decreases
the formation of insoluble iron phosphates and thus helps absorption but large amount
of Ca. inhibits iron assimilation. Vitamin – C increases the absorption of iron from
foods, possibly reducing the ferric iron into the ferrous state.
5. Time taken for absorption: The rate of absorption is determined by the iron
requiremen for Hb synthesis. In anaemic cases, after a single dose of iron, a rise of
serum iron takes place in 30 minutes, reaching its maximum in 3-5 hours and returns
to normal in about 12 hours. Maximum absorption is completed in 18 hours.
6. Iron storage: iron is incorporated into the iron-storage protein Ferritin, in
enterocytes, but the main stores of iron in the mammalian body are in the liver and
spleen. In addition to storage as Ferritin, iron can also be found in a form called
Haemosiderin inside the liver.
7. Iron balances: For an adult to stay healthy, the amount of iron lost each day much
be replaced by an equivalent intake. Young rapidly growing children, on the other
hand, will require a positive iron balance. The factors that influence daily iron loss,
daily iron intake and absorption from the gastrointestinal tract are to be mostly
considered.
8. Iron excretion: Iron is unique among the trace elements in that there is no
excretory system for eliminating the metal from the body. This is generally lost
through erythrocytes in bleeding. The routes for loss of iron may be classified as
either physiological or pathological.
9. Physiological Iron Losses: The adult male and the non-menstruating female lose
about 1 mg iron per day. Of this total, 50-60% is accounted for by loss from the
gastrointestinal tract, due either to biliary excretion or to the shedding of mucosal
cells. The remainder is lost with hair, sloughing of skin or in the urine. Lossess during
menstruation typically range, on average, from 1.4 to 3.2 mg Iron per day.

Losses associated with underlying pathology: A range of conditions give rise to
blood loss, but is appropriate to discuss this under Nidana.
10. Function of iron: (a) Formation of haemoglobin (b) Development of red cells (c)Oxygen carriage in blood (d) Related to tissue oxidation (e) Supplies O2 to the
muscles (f) Relation with cell nucleus and oxidation in nerver cells.
11. Deficiency signs: Iron deficiency causes secondary anaemia.
Haemolysis: By the term haemolysis is meant the disrutption of red cells with the
escape of haemoglobin from the corpascles to the plasma. Blood may be haemolysed
in the different ways:
1. By adding fact solvents – Ex: Ether, chloroform, benzene etc
2. By causing osmotic disturbance
3. Disturbing the surface tension – addition bile salts
4. Physical methods – Alternate freezing and thawing of blood breakdown
RBC
5. Mechanical – vigorous stirring and shaking
6. Addition of incompatible blood – Agglutinates the red cells.
7. Adding bacterial haemolysis
8. Adding snake venom (viper)
9. Drugs: like quinine, phenacetin, nitrates, chlorates etc.
Leucocytes (The White blood cells)
They are largest blood cells. They contain nuclei and some have granules in their
cytoplasm. White blood corpuscles are an important variety of cells in the blood.
These cells differ from the red cells in many respects. For instance.
(1) They do not contain any haemoglobin
(2) They are bigger in size
(3) They are nucleated, living cells.

(4) They are actively amoeboid
(5) They are much less in number
(6) Their span of life is shorter.
(7) Their origin is purely from extravascular tissue
(8) Their functions are absolutely different from those of red cells.
(9) There are several varieties of leucocytes, where as red cells are only one
variety. Normal leucocytes count – 4000-11000/cumm.
Classification and differential count of Leucocytes:
The classification and differential count as generally accepted two major groups:
1. Granulocytes Polymorphonuclear leukocytes)
Consequently this group includes three varieties:
A) Neutrophil
B) Eosinophil
C) Basophil
2. Agranular leukocytes (A granulocytes)
Two varieties
A) Lymphocytes
B) Monocytes
Again lymphocytes 3 types
A) T – lymphocytes
B) B- lymphocytes
C) Natural killer cells
(I) Granulocytes: These cells originate from stem cells (haemocytoblastas) in red
bone marrow and go through several developmental stages befor entering blood, a
process called granulopoiesis. They follow a common line of development through
myeloblast before differentiating into the three types. Their names represent the

dyes they take up when stained in the laboratory. Eosinophils take up the red acid dye,
basophiles take up the blue; and neutrophile are purple because they take up both
dyes.
(A) Neutrophils: Neutrophil is about 10-12m in diameter. Most numerous in the adult
blood, about 60-70%. The necleus is many-lobed; the number of lobes varies from 2
to 7 or more. Neutrophils have limited life span of around 12-24 hours in the blood.
Their main function is to protect against any foreign material that gains entry to the
body. Mainly microbes, and to remove waste material. They are attraced in large
numbers to any area of infection by chemical substances, released by damaged cells,
called ‘Chemotaxins’. Neutrophils pass through the capillary walls in the infected area
by amoeboid movement. There after they ingest and kill the microbes by a process
called “Phagocytoses”.
(B) Eosinophils: Eosinophils is 10-12 m in diameter. Eosinophils are charecterised by
their two-lobed. Nucleus they have significant proinflammatory and cytotoxic activity
and play a role in the pathogenesis of various allergic, parasitic and neoplastic
disorders. The eosinophils are amoeboid but not phagocytic. Eosinophils is about 2-
4%. The most common causes of eosinophilia in the world are allergic disorders such
as asthma, eczema and high fever. In developing contries parasitic infections are
frequently implicated. Other relatively common aetiologies are drug hypersensitivity,
various skin disease and connective tissue disorders.
(C) Basophils: Basophils is about 8-10m in diameter. The nucleus is kidney shaped.
The cytoplasm contains a large numbers of round granules which take deep basophilic
stain. Basophils are the least numerous of the blood leucocytes. Basophils secrete
histamine which causes vaso dilatation and increases the permeability of capillary
walls. Basophils and their tissue equivalent, most cells, have receptors for the protion
of I g E. They play a central role in immediate hypersensitivity reaction. Basophils

is usually associated disorders Eg. Chronic myeloid leukaemia. However it may be
reactive to a range of systemic diseases including inflametory bowel disease and
hypothyroidism. Basophil count about – 0.5-1%.
(2) A granular leukocytes (Agranulocytes): The type of leukocyte with no granules
in their cytoplasm are monocytes and lymphocytes.
(A) Monocytes: These are large mononuclear cells that originate in red bone marrow.
Monocytes are 16-18mm in diameters. Monocytes developed from monoblasts. Some
circulate in the blood and are actively motile and phagocytic, while others migrate into
the tissues where they develop into macrophage.The macrophage system, some time
called the lymphoreticular system, consisits of fixed pahgocytic cells which multiply
in situ. These cells are found in a wide variety of tissues. Eg.
Histocytes in connective tissue,
Microglia in the brain.
Kuffer cells in liver sinusoids.
Alveolar macrophages in the lungs.
Sinus – living macrophages in the spleen,
Lymphnodes & Thymus gland
Mesangial cells in glomerulus of nephron in the kidney.
Osteoclats in bone.
Monocytopenia is less frequently noted but can be severe in patients receiving
cortico steroid treatment. Monocytes count – 3.8%.
Lymphocytes: Lymphocytes are developing from haemocytoblasts in red bone
marrow. Lymphocytes are associated with protection of the body against foreign
material. Lymphocytes are spread in the blood stream to lymphoid tissue else where in
the body where they are activated i.e. they become immunologically competent

which means they are able to respond to antigens (Foreign material). Lymphocytes
count about 20-25%.
The major types of lymphocytes are T-lymphocytes, B-lymphocytes and natural killer
cells.
A. T. Lymphocytes: T.Lymphocytes, activated by thymosin in the thymus gland.
They are sensitized when they encounter an antigen for the first time. Effector cells
act directly against antigens in conjuction with phagocytes. The main T-lymphocytes
are cytotoxic and are responsible for long-term protection against some viruses,
bacteria, fungi, cancer cells, pollenfrom flowers and platns, some large molecule
drugs Eg. Pencillin. They are also responsible for the rejection of transplanted organs
T.Lymphocytes, which are responsible for cell mediated immunity.
Other T-lymphocytes are helper T cells, which activate B cells, and suppresor T-
cells, which inhibit B cell activity. T. Lymphocytes produce a number of chemical
substances
(A) Lymphokines that attract macrophages to the site
(B) Lymphotoxin that kills foreign cells eg-microbes
(C) Interferons that prevent virus reproduction inside cells.
B-Lymphocytes: B cells are derived from the stem cells of the bone marrow. B-
lymphocytes are responsible for humoral immunity. B.Lymphocytes are activated by
both microbes and their toxins. B-Lymphocytes, which are responsible for humoral
immunity. These are five subclasses IgG, IgA. IgM, IgD and IgE. The antibodies
promote phagocytosis of foreign particles and neutralize toxins.
Variations in normal count of white blood corpuscles:
a) Muscular exercise (asphyxia)
(b) Relation with after meal.
(c) Injection of adrenaline

(d) Emotional stress
(e) Relation with pregnancy and labour
(f) Increased cellular destruction from injections & surgical operations
(g) Asthma, high fever, skin disease
(h) Starvation and administration of certain chemicals like benzene.
Functions of white blood corpuscles:
(a) Phagocytosis
(b) Antibody formation
(c) Formation of fibroblast
(d) Manufacture of trephones (nutrition growth, and repair of tissues)
(e) Secretion heparin
(f) Antihistamin function
(3) Thrombocytes (Platelets):
They are very small non-nucleated discs derived from the cytoplasm of
megakaryocytes in red bone marrow. The normal platelet count is between 2,50,000 to
40,00,000/mm3 of blood. Platelets have a short life span. Normally, just 5-9 days.
Aged and dead platelets are removed by fixed macrophages in the spleen and liver.
Coagulation (Clotting): Normally, blood remains liquid as long as it stays with in its
vessels. If it is drawn from the body, however, it thickness and forms a gel. Eventually
the gel separates from the liquid. The red-coloured liquid called serum. The gel is
called clot. The process of gel formation it called clotting or coagulation. Clotting
involves several substances known as clotting factors:

Clotting factor:S.No. Synonym Source Pathway
I Fibrinogen Liver Common
II Prothrombin Liver Common
III Tissue factor (thrombo plastin) Damaged tissue &
Activated platelets Extrinsic
IV Calcium ions (Ca2+) Diet, bones, and
platelets All
V Proaccelerin, labile factor or
Accelerator globalin (ACG) Liver and platelets Extrinsic &
Intrinsic
VII Serum prothrombin conversion Liver Extrinsic
acceleralor stable factor or
proconvertin
VIII Antihemophilic factor (AHF) Platelet & Intrinsic
Antihemophilic globulin (AHG) Endothelial
IX Christamas factor, plasma Liver Intrinsic
Thromboplastin component (PTC)
Or antihemophilic factors B
X Start factor, power factor, or Liver Extrinsic &
Thrombokinase Intrinsic
XI Plasma thromboplastin Liver Intrinsic
antecedent (PTA) or antihe-
mophilic factor C
XII Hageman factor, glass factor, Liver Intrinsic
Contact factor or antihemophiliac
facrorXIII Firbin-stabilizing factor (fsf) Liver & Platelets Common
There is no factor VI, prothrombinase (prothrombin activator) is a combination of
activated factor 5 and 10.
Haemostasis blood clotting is 3 basic stages
Stage - I
Stage – II
Stage – III
Stage-I : The formation of prothrombinase is initiated by either the extrinsic or the
intrinsic pathways blood clotting.

Extrinsic path way: The extrinsic pathway of blood clotting has fewer steps than the
intrinsic pathway and occurs rapidly, with in a matter of seconds if trama is severe.
Damage to endothelim tissue protein called tissue factor (IF) also known as
thromboplastin or coagulation factor III, leaks into the blood from cells out side
(extrinsic to) blood vessels and initiates the formation of prothrombinase. IF is
mixture with of lipoproteins and phospholipids released from the surfaces of damaged
cell. It activates clotting factor VII, which next combines with factor X, thus
activating it. Once factor is activated, it combines with factor V in the presence of
calcium ions (Ca2+) to form the active enzyme prothrombinase. This completes the
extrinsic pathway.
Intrinsic pathway: The intrinsic pathway of blood clotting is more complex than the
extrinsic pathway. And it occurs more slowly, usually requiring several minutes. IF
endothelial cells (cells in the blood vessel) become roughened or damaged, blood
came in contact with collagen in the surrounding basal lamina, in addition, trama to
endothelial cells causes damage to blood platelets, resulting in the release of
phospholipids by the platelets. Contact with collagen activates clotting factor XII. In
turn, factor XII activates XI which activates factor IX. Activated factor VII (From
extrinsic pathway) also can activate factor IX. Activated factor IX joins with the factor
VIII and Platelets phospholipids to activate factor X. Once factor X is activated it
combines with factor V to form the active enzyme prothrombinase.
Stage2: Once prothrombinase is formed, the common pathway follows. In the second
stage of blood clotting, prothrombinase and Ca2+ catalyze the conversion of
prothrombin to thrombin.
Stage3: In the third stage, thrombin, the presence of Ca2+, converts fibrinogen, which
is soluble to loose fibrin threads, which are insoluble. Thrombin also activates factor
XIII (fibrin stabilizer factor), which strengthen and stabilized the fibrin threads into a
sturdy clot.
- Bleeding time – 2.5 mints.
- Prothrombin time – 11-16 sec
- Clotting time – 6-7 mints.

Blood groups
The surface of erythrocytes contain some glycoproteins and glycolipids that can
act as antigens, are normal components of one person’s RBC plasma membrane that
can trigger damaging antigen – antibody responses in other people. Based on the
presence or absence of various isoantigens. In there are four principal blood groups,
designated O, A, B and AB. These blood groups deffer in the types of antigens that
are present on the erythrocytes. Persons with type A blood have a Aantigens. Those
with type B, B antigens: Those with type AB, both A and B antigens: In addition, the
plasma of group ‘O’ blood contains antibodies to A, B and AB. Group A plasma
contains antibodies to B antigens and group B plasma contains antibodies to A
antigens. Group AB plasma has no antibodies to O, A, or B antigens. In blood
transfusions cross-matching is necessary to prevent agglutination of donor red cells by
antibodies in the plasma of the recipient because plasma of groups A, B and AB has
no antibodies to group O erythrocytes, people with group ‘O’ blood are called
‘Universal doners’. Conversely, persons with AB blood are called Universal
recipients, because their plasma has no antibodies to the antigens of the other three
groups.
In addition to the ABO blood grouping, there are Rh (Rhesus factor) – positive and
RH Negative groups. An RH-Negative person can develop antibodies to Rh positive
red blood cells if that person is exposed to Rh. Positive blood. For example, during
pregnancy a mother who is Rh negative can make antibodies for Rh-possitive cells in
the fetus is Rh positive (inherited for Rh positive). Rh-positive red cells from the fetus
can enter the maternal blood stream at the time of plancental separation and induce
Rh-positive antibodies in the mother plasm. The Rh-positive antibodies from the
mother can also reach the foetus via the placenta, and agglutionate and haemolyze
foetal red cells. This condition is known as Erythroblastosis foetalis, a haemolylic
disease of the new born.

Functions of blood:
1. Transport of respiratory gases. It transports oxygen form the lungs to all cells
and carbondioxid from cells to the lungs.
2. Transport of nutrition from the digestive organs.
3. It transports the waste products from the cells to the kidneys, lungs, and sweatglands.
4. Maintenance of water balance
5. Regulation of body PH and body temperature
6. It protects against toxins and foreign microbes.
7. It transport the enzymes and hormones to the cells
8. Regulation of blood pressure.
9. Maintenance of ion balance
10. It prevents the body fluids loss through clotting mechanism.
References:
1. Charaka Samhita, Sareera Sthana, 7th Chapter
2. Charaka Samhita, Sutra Sthana, 24th and 28th Chapters.
3. Charaka samhita, Vimana Sthana, 5,7,8 Chpater
4. Susruta Samhita, Sareera Sthana, 1st Chpater
5. Susruta Samhita, Sutra Sthana, 14th, 21st, and 42nd chapters.
6. Astanga Hridaya, Sutra Sthana, 1st, 12th, 16th, 20th Chapters
7. Principles of Anatomy and Physiology by J. Tortora.
8. Textbook of Physiology by C.C. Chatterjee.
9. Applied Physiology by Samson Wrights.
10. Textbook of Medical Physiology by Guyton & Hall
11. Human Physiology by Chakrabarti, Ghosh and Sahana
12. Will's Biochemical Basis of Mecdicine.
13. Regional and Applied Human anatomy by Dr. B.D. Chaurasia.

NIDANAThe word panchalakshana nidana indicates that there are five topics to discuss
under this text. It helps a physician to come to exact diagnosis of the disease. They are
I. NIDANA – The etiology
II. POORVAROOPA- The prodromal symptoms signs.
III. ROOPA – The signs ans symtpoms
IV. UPASAYA & ANUPASAYA – The comforting and aggravating factors
V. SAMPRAPTI - The pathogenesis.
NIDANA (Etiology)
Nidana is said to be disease producing factors and they are called as aeteological
factors in modern medicin.
“Seti kartavyatako rogotpadaka Heturn nidanam”
Means the factors, which plays an essential role in causing a disease vividha
ahita ahara vihara which cause vyadhi by vitiating doshas and dhatus.
Various factors are mentioned for the etiology of the disease. In the context of
Pandu roga all factors responsible for aggravation of pitta are termed as specific
nidanas. It can be stated that pitta prakopa nidanas cause the disease. The ahara and
vihara which are responsible for the disease can be divided into following types.
i. Ahara (Diet related factors)
ii. Vihara (behavior related factors)
iii. Manasika (psychological factors)
iv. Nidanardhakara Rogas (other diseases leading to Pandu) and
v. Acquired by papakarma (sinful act)

Ahara (Diet) related factors
1. Atikhara dravyas
2. Ati amala dravyas
3. Ati katu dravyas
4. Ati kashaya dravyas
5. Ati Ushana dravyas
6. Ati teekshana ahara
7. Vidagha dravyas
8. Asatmya dravyas
9. Nishpava
10. Masha
11. Pinyanaka
12. Tilataila
13. Mritbhakshanam (geophagia and pagophagia)
In the above stated factors kshara, amla, katu, lavana dravyas directly aggravate
to pitta. Especially, amlarasa does kapha vilayana, pitta vardhana, rakta dooshana and
sydhilya (increased catabolism). Ati lavana rasa intake leads to Raktapitta,
Amalapitta, Indralupta, vatarakata and other “pitta-rakta” related disorders.
Viruddhahara leads to vitiation of “tridoshas”. Masha is ushna veerya and in turm
increases pitta, Tila is pittakara and ushna veerya.
Ati teekshana ahara causes daha as it is of Agni boota predominance. Madhya
does pitta vitiation.
Vihara related factors:
1. Diwaswapna
2. Ati vyayama
3. Ati maidhuna

4. Panchakarma vaishamya
5. Nidra nasha
6. Vega dharana
7. Rutu Vaishamya
8. Rakta mokshana vaishamya
In the above mentioned factors ativyayama and ati mydhuna leads to increased
catabolism, thus contributing to the cause of the disease. Panchakarma vaishamya
vegavaroodha does vitiation especially to vata and thus cause disease pandu roga.
Among all Panchakarma vyshamyas, Atiraktasravam during rakta mokshana is also a
cause for the occurence of the disease.
Manasika factors:
1. Kama (desire)
2. Chinta (thinking)
3. Bhaya (fear)
4. Krodha (anger)
5. Shoka (sorrow)
Kama, shoka and bhyaya vitiate vata, krodha vitiates pitta, and chinta vitiates
vata kapha and produce vataja, pittaja and kaphaja predominant Panduroga.
Nidanardhakara factors: The disease which cause Pandu are grouped as
1. Rakta pradara
2. Raktapitta
3. Arshas
4. Krimiroga
5. Adhika raktasrava (due to abhighata)
6. Rakta arbuda
7. Rakta gulma

8. Pleehodara
9. Katikatarunamarma vedha
10. Yakrit pleeha vedha
11. Rakta atipravartanam
12. Hridroga
Apart from the above disease, all the conditions that end up in blood loss leads to
Pandu roga.
Papakarma factors: (Sinful act)
A person acquired Panduroga by sinful act according to the references from
Vaidya chintamani i.e. one who steals things of Gods and Brahmanas, one who does
not complete Agnistomadi karmas and one who kills a woman. Such persons acquire
Pandu with severe headache and with symptoms of kshaya. Such type of Pandu does
not get cured within nine years.
Thus the nidana of panu roga has been elaborately touched and discussed
because it has been said that "Chikitsa is Nidana Parivarjanam"Nidana as mentioned in different classics
Ahara (Diet) related factors:
S.No. Description Charaka Susrutha Madhavakara Haritha Vagbhta1 Kshara + - - + -
2 Lavana + + + + -
3 Katu - - - - +
4 Kashaya - - - + -
5 Atiteekshna - + + - -
6 Atiushna + - - - -
7 Virudha + - - - -
8 Vidagda + - - - -
9 Asatmya + - - - -
10 Nishpava + - - - -
11 Masha + - - - -
12 Pinyaka + - - - -
13 Tila taila + - - - -
14 Madya + - - - -
15 Mireya + + + + -
16 Amla + - - + -
17 Mrittika + + + + +

2. Vihara factors:
S.No. Description Charaka Susrutha Vagbhta Madhavakara Haritha
1 Diwaswapna + + + + +
2 Vyayama + - + + -
3 Maidhuna + + + - +
4 Panchakarma + - - - +
vaishmya
5 Rutuvaishamya + - - - -
6 Vegavidhrana + - - - -
7 Nidranashnam - - - - +
8 Avyayama - - - - +
9 Shrama - - - - +
3. Manasika factors
S.No. Description Charaka Susrutha Vagbhata Madhavakara Haritha
1 Kama + - - - -
2 Chinta + - - - +
3 Bhaya + - - - -
4 Krodha + - - - -
5 Shoka + - - - -
Charaka mentioned Pandu roga is the "Santharpanajanya Vyadhi". Though the
intake of food may be more, the disease is aquired due to pitta Vardhaka ahara as well
as viharas. This imbalanced diet contains more fats, however deficiency of vitamins
and minerals leads to anaemia.

ETIOLOGICAL FACTORS
Anaemia is caused due to various factors. They are grouped into following heading.
1. Idiopathic causes
2. Haemorrhagic anaemia
3. Dyshaemopoietic anaemia
4. Haemolytic
5. Aplastic or non-functioning Bone marrow
1. Idiopathic: Causes may be due to the anorexia. Psychiatric, autoimmune disease.
2. Haemmorhgic factors: Loss of blood due to trauma and various other causes.
a. Acute: Acute and massive haemorrhage in antipartum haemorrhage, post
partum haemorrhage, haematemesis, haemoptysis.
b. Chronic: Small and recurrent bleeding tendency such as piles, bleeding gums,
hookworms, etc, menorrhagia in females, chronic ulceration of gastro intestinal
tract, GIT malignancy, long standing haematuria oesophagical varices.
3. Dyshemopoietic (or) Due to defective blood formation:
a. Due to nutritional deficiency (or) deficiency of extrinsic factors
b. Failure of absorption of iron, proteins, B12, folic acid and vitamin C.
c. Lack of iron storage (due to liver damage large amount of iron & other
necessary elements are not stored and leads to anaemia).
d. Lack of releasing factors due to spleen enlargement.
e. Defiiency of certain minerals like copper, cobalt, manganese and certain
hormones like thyroxine, etc.
f. Endocrind disorders eg. Myxodema, Addisons disease.

4. Hemolytic anaemia:
Normally RBCs are destroyed by Reticulo – endothelial cells, situated in liver, spleen
and bone marrow.
a. Due to abnormal formation of RBCs as in spherocytosis, thalassemia and sickle
cell anaemia.
b. Due to circulating haemolytic agential haemolytic anaemia and paroxysmal
haemoglobinuria.
c. Incompatibility of blood groups and Rh incompatibilities.
d. Bacterial infections – septicemia
e. Chemical agents – Aspheramine, coaltar, derivatives and poisoning.
f. Snake venom and other poisionous bites cause anaemia due to haemolysis.
g. Cytotoxic drugs such as phenyl hydrazine, hydrochlorosis and quinine also
cause haemolysis.
5. A plastic (Non-functioning) bone marrow:
a. Lack of Utilization of haemopoetic factors by bone marrow is seen in primary
Aplasia.
b. Sometimes drugs such as chloromycetin, quinine, Benzol, Aspheramine and
gold salts depress the bone marrow, causing secondary Hypoplasia. Radium
salts, radioactive materials and X-rays also cause bone marrow.
Warm – infestation:
Parasites may cause disease Anaemia due to their presence in the lumen of the
intestine, due to infiltration into the blood stream.
Ex. Malarial Parasite may cause Anaemia due to Haemolysis (Distruction of Red
cells).
Nematodes like Ascaris, Enterobiasis (Pin warm), Tape warms and Hook warms
are caused to Anaemia in human being especially in children during the first decade of
life.

In effects individuals at all socio-economic level especially children crouded living
conditions predispose individuals to infection.
The larwas are found in warm, damp soil and infect humans by penetrating the skin.
They migrate to the lungs ascend thetrachea are swallowed and reside in the institine.
The warms then mature and attach to the intestinal wall, when they suck blood, and
shed eggs, caused by the Symptoms like Anorexia, Indigesation, Abdominal pain and
Fullness of abdomin, and Diarrhoea occurs. The major manifestation of infection is
subsequent Anaemia.
References:
Charaka Samhita, Chikista Sthana 16/7-11
Susrutha Samhita, Uttara Sthana 44/1-3
Astanga Sangraha, Nidana Sthana 13/3-6
Astanga Hridaya, Nidana Sthana 13/1-3
Madhavanidana 8/2
Hareeta Samhita, Triteeya sthana 8/3-5.
A text book of Human physiology by Dr. Sahana chakraborthy and Ghosh.
A text book of Pathology by Boiyd
Nelson Text Book of Paediatrics.

POORVA ROOPAAccording to susrutha, the sanchita and prakopita doshas are occumulated in a
particular stana it is termed as “Stana samshrayaavasta” a premonitory signs and
symptoms of manifestation of vyadhi. Those signs and symptoms which appears
earlier to the actual disease, as they are not clearly recongnisable and few in number.
These are called poorvaroopas, This is very important stage, which is to be observed
by the physician because it would be very easy to prevent the disease.
“Poorva roopam pragutpathi lakshanam Vyadhi”-
(Charaka Nidana – I Chapter)
Poorvaroopam is a state where the prodromal signs and symptoms of a disease
start to occur. In other words, it is described as the early stage of any disease. It is that
state of the disease, where Dosha – Dooshya Sammoorchana occurs, i.e. there begins
an interaction between the doshas and the dooshyas.
Poorva Roopa is of the following two types
1. Samanya poorva roopa
2. Visesha poorva roopa
Samanya poorva roopa gives information about the disease, which occur in the
following days but not the detailed description of the predominant dosha. Visesha
poorva roopa gives most of the details of the occurring disease at an early stage.
Samanya poorva roopa of Pandu are:
1. Twak sphotana
2. Shteevana
3. Gatrasaadana
4. Koota shodha
5. Avipaka
6. Hridaya spandana
7. Twak rushata
8. Swedabhava

9. Sharama
10. Shareera pandutwa
11. Mrit bhakshanaapeksha
12. Alpagni
13. Shareera krishatwa
14. Angasaada
15. Aruchi
16. Vit., Mootra, Peetatwam
Poorvaroopa – According to different acharyas:
Sl Poorvaroopa Charaka Susrutha Vagbhata Hareeta
1 Twaksphotana - + - -
2 Shteevana - + - -
3 Gatrasaada - + - -
4 Kootashodha - + - -
5 Avipaka - + - -
6 Hridayaspandana + - - -
7 Twakrushata + - - -
8 Swedabhava + - - -
9 Shrama + - - -
10 Shareerapandutwa - - - +
11 Aruchi - - + -
12 Vit, mootrapeetatwam - + - -
13 Mritbhakshanaapeksha - + - -
14 Alpagni - - + -
15 Angasaada - - + -
16 Shareerakrishatwa - - + -

Though there is no detailed description of the vishesha poorva roopas by any of
the classics, we can divide the above poorva roopas upon the doshic predominance
and can classify as follows:
S.No. Vataja P.R. Pittaja P.R. Kaphaja P.R. Mritbhakshana P.R.1 Twaksphotana Vit, mootra Shteevanam Mrit Bhakshana
Peetatwa Shteevanam
2 Angasada Avipaka Alpagni -
3 Gatrasaada - Aruchi -
4 Twakrushata - Hridayaspandana -
5 Swedabhava - Kootashodha -
6 Sareera krishatwa - Sareera pandutwa -
7 Shrama - -
POORVA ROOPA - MODERN ASPECT
There are no definitive prodromal symtpoms mentioned as such in case of
Anemia. Especially, these depend upon oxygen carrying capacity of the blood. The
severity of the signs and symptoms depend upon the degree of anemia, independent of
its type.
Lassitude and Fatigue, though are seen in the early stages of the disease, these
are seen in many other disease. Pallor of skin, mucous membranes, palms and
conjunctivae are seen after some period and these in addition to above may give a
better picture of this disease. The complete picture of the disease shall be discussed
under Roopa.
References:
Charaka Samhita Chikistasthana 16/12
Susrutha Samhita Uttara Sthana 44/5
Astanga Sangrata Nidanasthana 13/6
Astanga Hridaya Nidana Sthana 13/8
Hareeta Samhita, Trieeya sthana 8/6
Principles and Practice of Medicine by Davidson

ROOPAThis is the stage of a disease where the signs and symptoms of the disease are
totally manifested, this termed as fifth kriya. Kaala of ‘vyaktibhava’. When the
disease starts to take its stage forth kriyakala namely in the Stanasamshrayaavastha
or Poorvaroopavasta and when it is not treated the doshas get accumulated and
manifestiation into the diseased state – “ROOPA”.
“Tadeva vyaktatam yatam rupa mityabidiyate”
The poorva roopa which has attained vyakthavastha known as roopam. The
symtpems are mainly due to sroto dushti of the respective Srothases. The main srotas
involved in pandu roga is Rasavaha srota drushi.
Hence, almost all of Rasavaha sroto dushti lakshanas can be observed in pandu
symptomatology. These are Aruchi, Ashraddha, Agnimandya, Hrillasa, Arasagnatha,
Gouravam, Tandra, Angamarda, Pandutwam, Jwara, Klaibhyam, Sada, Krishnagata
and phalitya.
In general, the signs and symptoms of pandu roga are as follows:
1. Dhatu shaithilya 2., Alpa rakta 3. Ojoguna kshaya
4. Alpa medas 5. Sithil endriya 6. Hritdrava
7. Shoona akshi 8. Koota sadana 9. Kopana
10. Shteevana 11. Alpavak 12. Hataanala
13. Anna dwesha 14. Karna kshweda 15. Dourbalyata
16. Sisira dweshi 17. Shrama 18. Bhrama
19. Shoola 20. Jwara 21. Swasa
22. Gourava 23. Gatra peeda 24. Aruchi
25. Sheerna loma 26. Hata prabha 27. Nidradhikyata
28. Pindiko dwestta 29. Kati, Uru, Pada – ruk 30. Sannasakti
31. Sphurana 32. Nakha vakrata 33. Swetha akshi
34. Arosha naayasa

In addition to the above, kshayalakshanas of Rasa, Rakta, Medo, Mamsa, and
Ojus can also be observed in panduroga.
The disease is classified into five types, according to the involvement of doshas.
1. Vataja pandu roga
2. Pittaja pandu roga
3. Kaphaja pandu roga
4. Sannipathaja pandu roga
5. Mritbakshanajanya pandu roga
The lakshanas of all these varieties differ from each other, and they are stated in
below.
Lakshanas of vataja pandu roga:
S.No. Symptoms/sign Cha Su Va Ma Bha Ha
1 Aruna angata + - + + + -
2 Aruna nakha - - + - - -
3 Aruna netra - - + + + -
4 Aruna sira - - + + - -
5 Rkshna mala, mootra - - + + + -
6 Ruksha netra - - + - - -
7 Ruksha nakha - - + - - -
8 Ruksha anga + + + + + -
9 Krishna netra - + + + + -
10 Aruna mala mootra - - + - + -
11 Krishna nakha - + + - - -
12 Vata vikara - + - + + -
13 Anga marda + + - - - -
14 Jwara + - + - - -
15 Toda + - - - - -
16 Kampa + - + + + +
17 Parshwa shoola + - + + + -
18 Shirah shoola + - + - - -
19 Vitshoola + - + - - -

20 Asya vairassya + - + - - -
21 Shopha + - + - - -
22 Anaha + - + + + -
23 Balakshaya + - - - - -
24 Bhrama - - - + + -
25 Parushata - - - - - +
26 Sirogurava - - - - - +
27 Gadhavitakata - - - - - +
28 Ruksha sira - - + + - -
Lakshnas of pittaja pandu roga:
S.No. Symptoms/sign Cha Su Va Ma Bha Ha1 Shareera peeta + + + + + +2 Shareera Harita + - + - - -3 Peeta mala, mootra + + + + + +4 Peeta netra - + + + + -5 Peetha nakhata - + + - - -6 Peetha sira - + + - - -7 Harita sira + - + + + +8 Jwara + - + + + +9 Daha + + + + + +10 Trishna + - + - - -11 Moorcha + - + - - -12 Sweda + - + - - -13 Annadwesha + - + - - -14 Katu kasyam + - + - - -15 Amlodgara + - + - - -16 Ushna, Amla anupasayata + - - - - -17 Vidaha + - - - - -18 Dourgandha + - + - - -19 Binnavarchasa + + + + - +20 Dourbalya + - - - - +21 Pitta vikara - - - - - -22 Tama + + + - - -23 Shopha - + - - - +

Lakshanas of kaphaja pandu roga
S.No. Symptoms/sign Cha Su Va Ma Bha Ha
1 Swetha avabhasata + + + + + -
2 Sukla akshi + + + + + -
3 Shukla nakha - + + - - -
4 Shukla, mala, mootra + + + + + -
5 Shukla sira - + - - - -
6 Gouravam + - + + + +
7 Tandra + - + + + +
8 Chardi + - - - - -
9 Praseka + - + + + -
10 Lomaharsha + - + - - -
11 Angasadha + - - - - -
12 Moorcha + - - - - -
13 Bhrama, klama + - - - - -
14 Swasa + - + - - -
15 Kasa + - - - - +
16 Alasyam + - - + + +
17 Aruchi + - - - - -
18 Vak, Swaragraha + - - - - -
19 Katu kamata + - - - - -
20 Ushna kamata + - - - - -
21 Swayadu + - - + + +
22 Madhurasyata + - - - - -
23 Lavanakamata - - + - - -
24 Swara kshaya - - + - - -
25 Sleesma vikara - + - - - -
26 Swedana - + - - - -

The main differentiating features of vataja, pitaja & Kapha
S.No. Lakshanas of pandu Vataja Pittaja Kaphaja
1 Varna of vit, mootra Krishna Peeta Sukla
Nakha and Netra
2 Jwara Present Present Present
3 Shotha Present Absent Present
4 Kamitwa Absent Seeta Ushna./katu
5 Mukha ruchi Vairasya Katu Madhura
6 Moorcha Absent Present Present
7 Pureesha Little in quantity Bhinna Constipated
8 Varna Aruna Peetha/haritha Swetha
9 Bala Decreased Decreased
10 Other characterstics Rukshatwa Daha Gouravam
Angamardha Trishna Tandra
Krodha Swedana Chardi
Parushatwa Anannabhilasha Loma harsha
Siroruja Vidaha Sada
Dourgandha Bhrama
Klama
Swasa
Kasa
Alasya
Aruchi
Vakgraha
Swaragraha

Laskhanas of Sannipataja Pandu Roga:
Sannipatajapanduroga basically occur by the vitiation of all the three doshas (Vata,
pitta & Kapha), it possesses all the features of pandu that are mentioned under their
respective tables. However the clinical features shall differ as per the doshadhikyata.
Hareeta mentioned that sannipataja pandu has the following lakshanas in
addition to above.
Tandra Hrillasa Kshudarthata Kasa
Alasyam Shosha Moha Jwara
Swayathu Vitbhada Trishna Glani
Vamana Purushanayana
Madhava nidana added Arochaka and Haterndiya to above features.
Mrit Bhakshanajanya Panduroga:
The name Mritbhakshana janya pandu, as the name indicates, occurs due to
intake of Mrittika (mud/pica). This geophagia vitiates all the three doshas. But
depending upon the rasa of mud eaten, any of the three doshas vitiate, predominantly.
Mrit generally contain ruksha guna in predominance. This makes the food
consumed and the srotas, to dry. This leads to obstruction of srotas and even vitiates
rasa and raktadi dhatus. So the following clinical features occur in pandu Roga.
1. Destruction of bala, varna and agni
2. Shotha of ganda, akshikoota, bhru, paada, nabhi and mehana
3. Krimikoshta
4. Kapha, rakta sahita pureesha
5. Atisara
6. Indriya dourabalya
7. Srotodusti lakshanas
8. Destruction of tejus, veerya and ojus, these are specific lakshanas in addition to
the specific doshas involved.

Modern aspectClinical Aspects of Anaemia
Clinical features of anaemia reflect the diminished oxygen carrying capacity of
the blood. Their severity depends on the degree of anaemia and the pace of its
development. The Signs and Symptoms are listed below.
S.No Symptoms Signs
1 Lassitude Pallor of skin, mucous, membrane2 Easy Fatigability Palm of hands, conjunctiva3 Palpitation Tachycardia4 Breathlessness on exertion Dyspnoea on exertion5 Dizziness Tachypnoea6 Throbbing in head & ears Palpitation8 Headache Cardiac dilatation9 Dimness of vision Systolic flow murmurs10 Insomnia Oedema11 Angina Platynychia12 Parasthesia of fingers Oedema of the feet
and toes13 Loss of weight Early graying hair14 Loss of appetite Glossities15 Diarrhoea Angular stomatitis16 Flatulence Smoothening of tongue17 Constipation Dyshphagia18 Low fever Rapid pulse19 Lack of concentration Signs of cardiac failure20 Backache Vagorous arterial pulsation21 Giddiness22 Faiting of spells of blackout23 Noises in the ears24 Urinary frequency nocturia25 Loss of libido and potency26 Menorragia27 Thin lusterless hair28 Amenorrhoea29 Delayed Purberty30 PICA

Though the person is anemia, one cannot find all the signs and symptoms
mentioned above since anaemia is caused by different etiological factors, their clinical
features shall also surely differ.
Though the above mentioned clinical features give a clear idea of the disease,
diagnostic methods confirm the disease and aid in detection of the cause in many
instances.
INVESTIGATIONS
Blood examinations
1. Estimation of hemoglobin
2. Total RBC count
3. Total WBC count
4. Differential count
5. Packed cell volume (Hematocrit)
6 Blood picture
7. Electrophoretic pattern of hemoglobin
8. Erythrocyte sedimentation rate
9. Total plate let count
10. Plasma transferin
11. Total iron binding capacity
12. Serum ferritin13. Serum vit B12 levels
14. Serum folic acid estimation
15. Plasma LDH (Lactate dehydrogenase)
16. Lipid profile
17. Total bilurubin – Direct and indirect
18. Glucose profile
19. Serum proteins.
2. Urine examination: Urine must be examined for microhematuria, Albumin,
urobilurubin (bile salts and bile pigments), sugur and others.

3. Faeces: Faeces must be examined thoroughly for ova and cysts and for excessive
urobilurubin for occult blood and melena.
4. Bone marrow bipsy
5. E.C.G.: ECG should also be done because, most of the signs overlap with
congestive cardiac failure and other valvular heart diseases.
6. Endoscopy: sigmoidoscopy / proctoscopy / Gastroduodenoscopy
7. IVP : Intravenous pylogram may be useful in haematuria is present.
8. Jejunal biopsy
9. Cr-51 labelled RBC infiltration.
IRON DEFICIENCY ANEMIAS
Age Group: This type of anemia is mostly seen in children between ages of 6 months
and 2 years, and from 11 to 16 years due to spurts of growth during these periods.
This is also common in adult menstruating and childbearing aged females.
SEX: Iron deficiency anemias are mostly seen in adult females in their menstrual age
and it is almost universal during pregnancy.
DIETARY HABITS: Vegetarians are more commonly affected with Iron Deficiency
anemias than non vegetarians. Consuption of white bread, polished white rice, white
sugar etc. increases the disease incidence.
SOCIAL STATUS: Poor are predominantly affected than the rich.
CLINICAL FEATURES:
Due to Anemia: Insidious onset of easy fatigability, weakness, headache, body ache,
inability to concentrate, giddiness, palpitation, exertional dysphoea, anginal pain and
Hemic murmur.
a. Manifestation of underlying condition: For example, pain of peptic ulcer,
epigastric lump in carcinoma stomach

b. Due to Iron Deficiency Anemia
1. Tongue - Smooth and Pale (bald tongue) and Angular Stomatitis
2. Dysphagia - Formation of Mucosal webs (Plummer-Vinson Syndrome)
3. Gastritis
4. Nail changes - Thin and Fragile nails - Platynychia and Koilonychia
5. Hepatospleenomegaly
6. Pica - Perversion of appetite in form of Geophagia or Pagophagia
(excessive eating of rice)
7. Miscellaneous: Edema of feet, impaired renal function or
Hypoproteinemia, Amenorrhoea and Menorrhagia, increased intracranial
tension, long standing anemia leading to Fronto-Parietal eminence,
Parotid gland swelling and hair loss.
LABORATORY FINDINGS:
A. To establish & assess severity of anemia:
1. Blood Picture - RBC count, Hb%, and Hematocrit are decreased. MCV,
MCH, and MCHC are decreased.
2. Bone marrow - Increased cellularity from increased hemopoietic activity.
Bone Marrow Iron Stores are markedly decreased or absent.
3. RBC survival is decreased.
4. Serum Iron and Transferrin saturation are decreased. Iron Binding Capacity is
increased. Plasma Iron Clearance, Erythrocyte Iron turnover are increased.
5. Blood Picture- RBC count, Hb%, and Hematocrit are decreased. MCV, MCH
and MCHC are decreased.
6. Bone marrow - Increased cellurarity from increased hemopoietic activity
Bone marrow Iron Stores are markedly decreased or absent

7. RBC survival is decreased
8. Serum Iron and Transferrin saturation are decreased. Iron Binding Capacity is
increased.
9. Plasma Iron Clearance, Erythrocyte Iron Turnover are increased.
B. To determine cause of anemia:
1. Stool Examination for occult blood, bulky fatty stools, ankylostoma.
whipworm and amoebiea.
2. X-rays - barium meal and small bowel exam.
3. Endoscopy - Proctoscopy for detection of piles, Sigmoidoscopy and
Gastroduodenoscopy may reveal lesions not shown by x-rays.
4. Jejunal biopsy
5. Cr-51 labeled RBC injection shall detect loss of blood in faeces that detect GI
blood loss.
6. IV Pyelography
7. IV Pyelography
8. Selective angiography: If there is significant blood loss and no lesion has been
detected, local angimatous malformation.
MEGALOBLASTIC ANEMIAS
Megaloblastic anemia is caused by Vit. B12 Deficiency, folic acid deficiency,
and defective DNA synthesis (other than B12 and folic acid deficiences)
Clinical feaatures:
1. Due to anemia: Shortness of breath, dyspnoea, pallor and in older patients
angina or cardiac failure.

2. Gastrointestinal: Diarrhea, loss of appetite and weight and slightly yellow tint
of mucous membranes due to intramedullary breakdown of Hb & reduced
RBC life span.
3. Fever of mild degree
4. Mild Spleenomegaly only in 50% of patients
5. Neurological manifestation:
a. Neuropathy-Paraesthesia, stamping gait & positive Romberg's sign.
b. Subacute degeneration leading to increased leg reflexes & extensor
plantar response and sensory loss.
c. Optic neuropathy
d. Depression, impaired memory, and organic dementia
6. Miscellaneous features: Purpura & thombocytopenia, mild mal absorption
syndrome, sterility and wide spread skin pigmentation
Age: All age groups especially aged and elderly people.
SEX: Females of reproductive age are more prone for Megalobastic anemia and
during pregnancy this deficiency can even lead to umbilical cord and neural canal
deficits.
Dietary habits: Strict vegetarians (Veganism).
Social Status: Poor people are more sufferers of anemia
The above said Iron Deficiency anemia and megaloblastic anemias if untreated
lead to fatal Pernicious Anemia from severe form of blood disease, marked by
progressive decrease in RBC, muscular wekness, GI & neural disturbances
Age - 40 to 60 years
Sex - More in females
Race - Incidence highest in north Europeans
Family History - The disease is about 20 times more common in close relatives.

References:
1. Charaka Samhita, Chikitsa Sthana, 16th chapter
2. Susruta Samhita, Uttara Sthana, 44th chapter
3. Astanga Sangraha, Nidana Sthana, 13th chapter
4. Astanga Hridaya, Nidana Sthana, 13th chapter.
5. Madhava Nidana, 8th chapter
6. Hareeta Samhita, Tritiya Sthana, 8th chapter
7. Kashyapa Samhita, Sutra Sthana, 25th chapter
8. Davidsons Principles and Practice of Medicine
9. Current Medical Diagnosis and Treatment
10. Medicine for students by Dr. Golwalla
11. A.P.I. Text book of Medicine.

SAMPRAPTISamprapti is the stage wise manifestation of the disease. The disease process is
starts with nidana and then passes through Sanchaya, prakopa, prasara,
Stanasamsraya and Finally manifestation of Vyaktavastha, i.e. manifestation of
pandu. This complete disease process is called as samprapti. In other words
Samprapti gives detail information about the pathogenesis of the disease.
The term samprapti in madhavanidana is as below
"Yatha dushtena doshena yatha chanu visarpatu
Nivrutti Ramaya - Syasan samprapti jati ragati"
Samprapti can also be called dosha doosya sammurchanavasta of a particular
vyadi.
In pandu roga generally three dosas are involved and in particularly pittadosha.
The pitta prakopakara ahara and vihara are the causative factors of pandu. Because of
these nidnans pittavridhi takes place. Physiologically the formation of acchapitta,
occurs in Grahani during ahara parinama. But due to katu, amla, lavana, ushna ahara
and other causes mentioned earlier, vitiation of pitta takes place. Since Pachaka pitta
is situated in Grahani, the vitiated pitta affects the Agni. The drawatwa in this
vidagdha pitta reduces its teekshanatwa. This agni cannot digest the ahara consumed,
there by leading to vidagdha bhava.
Generally, after pachana, the food consumed is divided into Sarabhaga and
Kittabha by samana vayu and the saarabhaga is taken to hridaya. But due to vidagdha
pitta, pachana does not occur properly leading to dooshita annarasa. The annarasa is
taken by samanavayu to hridaya and transforms it into rasadhatu. The viharas like
vyayama, vyavaya etc cause vitiation of vyanavayu. The viitiated vyana vayu along
with pitta - dooshita rasadhatu circulates throughout the body through dasa dhamanis
that emerge from hridaya. The pitta dooshita rasa dhatu flows into the next dhatu for

its nourishment malformed rasa dhatu due to pittavidagdata, destructs the
raktadhatu poshakamsas and attains pandu roga, which will not be in a position to
nurish dhatus.
Finally rasadhatu lodges in the space between twak and mamsa. Then by
vitiating the kapha, vata, rakta, twak, and mamsa, it produces pandu, haritha and
haridra varnas, or various other discoloration of the skin. Of these colours, pandu is
seen predominantly. The formation of all the other dhatus is also impaired. As a
results of this, the formation of next dhatu i.e. raktadhatu is effected both qualitatively
and quantitatively. Even the essence which comes out from each dhatu also reduces in
its quantity. As the essence of all dhatus is ojus, its kshaya lakshanas can also be
observed on progression of the diseases.
In pandu the rasa dhatu dushti and there by its kshaya takes place. Hence in the
first stage of the disease, rasadhatu kshaya lakshanas are predominantly seen. Those
are Hritpeeda, Kampa, Shoonata, Trishna, Shabda Asahishnuta, and Swalpa cheshta.
In the later stages the kshaya lakshanas of other dhatus is also seen.
The nidanas for pandu pertaining to ahara are ati amla, atilavana, Atiteekshna,
madhy and mritsevana and diwaswapna and vitiation of rakta as well as ranjaka pitta.
As the place of ranjaka pitta and rakta vaha srothasas is yakrut and pleeha. The
nidanas which vitiate ranjaka pitta and rakta directly causes the kshaya of these two
and / or the qualities of these two are also altered. These are responsible for the
disease pandu. Hence ranjaka pitta and rakta kshaya lakshanas are observed in the
disease.
The consumption of mrit also vitiates the doshas and causes the disease.
Kashyarasa mrit vitiates vata, katu rasa mrit vitiates pitta and kapha is vitiated by the
madhura rasa mrit.
Generally mrit contains ruksha guna. Hence the consumption of mrit mainly
vitiates vata. Mrit does not contain any dhatu poshka amshas. It obstructs all the
srothasas as it does not get digested and prents the rasadhatu to enter into the other

dhatus. This impairs the formation of dhatus starting from rasa to sukra. This
impairs even the formation of ojus also. The resultant manifestations are loss of
energy of indriyas and tejus. Finally the disease sets in with bala, varna, and
agninashana, swelling of akshi, ganda, akshikoota, pada, nabhi, medra, krimikosta,
and atisara - as well as kapha - rakta yukta pureesha occurs. Thus samprapti of pandu
roga is discussed in detail.
References:
1. Charaka Samhita chikitsastana 16/6-11
2. Susrutha samhita nidana sthana,
3. Susrutha samhita, sareerastana
4. Susrutha samhita, uttara sthana 44/3
5. Ashtanga sangraha, sutra stana
6. Asthanga sangraha, Nidana stana 13/3-6
7. Ashtang Hridaya, sutrastana
8. Ashtang Hridaya chikitsastana 13/3-6
9. Madhava Nidana.


SADYA AND ASADYA LAKSHANASIt is very essential to decide the sadhya and asadhya of any disease before
attempting to treat it. As a general rule, the disease without any upadravas, or arista
lakshanas, which is newly manifested, which has less number of lakshanas and in
which only one dosha is involved is said sukhasadhya. Asadhya denotes the bad
prognosis of the disease. Asadhaya lakshanas are two types – Yapya and
Pratyakhyeya. Yapya is the term used when the disease is incurable and the patient
survives due to Ayusesha and the patient should have life long treatment.
Pratyakhyeya indicates achikitsa avastha of the disease.
If the patient acquired all the said lakshanas of the disease, and if it is of
chronic in nature, the disease is said to be pratyakhyeya. It has been mentioned that
the physician should leave the patient untreated, if the below mentioned asadhya
lakshanas are seen in the patient.
The following are the asadhya lakshanas of pandu
“Chirotpanna kharibhoota”1
1. Doshas occumulation in a large scale.
“Kalaprakarsha shoonana peeta darshee,”2
2. The patient has developed oedema and seeing all objects in yellow colour
“Sa kapha yuktha haritha varna baddalpa atisaree”3
3. When the patient passes baddha, alpa and haritha pureesha with kapha
“Asrikshaya swetangee”4
4. The patient is rakta kshaya – panduvarna sareera
“Chardi, moorcha, trishnardita deena swetati digdhangata”5
5. Pandu roga associated with chardi, moorcha, thrishna, deena and atipandu
varnam.

“Anta pradesha shoda and madhy sareera krisha”6
Shota in extremities and krishata in Madhya sareera.
6. When the patient is afflicted with sodha of the extremities with an
emaciation of the Madhya sareera.
Shota in guda, sephasa and mushka pradesha7.
7. When the patient has sodha of guda, shepha, mushka.
“Jwara, Atisara peedita pandu roga.”8
8. Pandu roga associated with jwara and atisara.
9. If the pandu rogi has massive intestinal worm infestation and pass feces with
blood and mucous.
10. Pandu rogi with swedana, dehajaadya, Swayadhu, Vamana, Nyanga, Sosha,
Kasa, Nidra and Brama.
The knowledge of sadhy asadhyata is essential to include or exclude the patients
in the study. If the patient develops the above clinical features, then the physician
should leave the patient untreated.
References:
1. Charaka chikitsa stana 16/32, 36
2. Susrutha uttara sthana 44-40
3. Astanga hridaya Nidana 13/15,16
4. Bhava prakasha madhyama kanda – P Prakaranam / 13,14,15,17
5. Vangaseena 19, 15
6. Yogaratnakaram 13, 16
7. Susruta sutra stana 33/22

UPADRAVAS AND ARISHTA LAKSHNAS
Upadravas: Any vyadhi or clinical features appearing on the later stage of a main
disease due to improper management are called as upadravas of the disease. When
upadravas occurred the disease becomes very difficult to treat. It denotes that the
disease should be treated as early as possible before appearing upadravas.
The upadravas that are associated with Pandu roga are as follows:
1. Aruchi 2. Pipasa 3. Chardi
4. Jwara 5. Shirashoola 6. Agni mandyam
7. Kanta shopha 8. Daurbalyam 9. Moorcha
10. Klama 11. Hridaya peedana 12. Swasa
13. Atisara 14. Kasa 15. Shoola
16. Daha 17. Ajeerna 18. Swarabedha
19. Shotha 20. Swarasada
Hence Pandu should be treated as early as possible before upadravas appear. The
dosha involvement in the upadravas may be equivalent to the main disease (or) may
not be.
Arishta lakshanas:
Arista lakshanas are Asanna marana lakshanas. These are the clinical features that
appear in the patient when the prognosis is very worse and the patient is nearing death.
In other words the signs & symptoms, which indicate death, are the Arista lakshanas.
The arishta lakshanas that appear in Pandu roga are given below:
1. Pandu varna danta, nakha netra and twak
2. Shopha and swasa
3. Trishna yukta shoola.
4. The patient expires if he gets the dream of eating pale coloured food

5. Pandu rogi sees that the environment in pandu varna.
6. Pandurogi dies immediately when pandu is associated with prameha and
bleeding through nostrils
As these above Arishta lakshanas point out the worst out come. A wise physician
should not treat them.
References:
1. Susrutha uttara stana – 44/13,39
2. Susrutha sutra shtana 33/22, 29/69
3. Hareetha samhit 4/37, 4/24
4. Susrutha sutra stana – 29/69
5. Bhavaprakasha madhyama kanda 16
6. Vanga sena 26/15
7. Yogaratnakara - /15


CHIKITSA KRAMAThe chikistsa karma means. Stage – wise treatment program of the disease. In
general, the three principles of treatment mentioned in ayurveda are
Diavavyapasraya, Yuktivyapassraya, and Satwavajaya. Daivavyaaprasraya
chikista mainly depends on praying God, doing yagnas and yagas, doing good deeds
etc Yuktivyapasraya chikitsa of pandu roga includes the following principles.
1. Nidana parivarjana
2. Snehana chikitsa
3. Shodhana chikitsa
4. Samana chikitsa
1. Nidana parivarjana:
“Samkshepathaha kriyayogo nidana parivarjanam”
Nidanaparivarjana is the first and fore most line of treatement for any disease.
The nidana (causative factors) mentioned earlier are to be avoided.
The nidana karanas of pandu roga are katu, amla, Lavana, Ushna, Teekshna
aharas, viharas – Vyayama, Vyavaya, Manasika karanas are Kama, Krodha, Bhaya,
Chinta, Shoka etc. karanas (causative factors) of pandu should be avoided.
2. Snehanam chikitsa:
Sadyanta pandvamaynam samekhaya snigdham ghritenordva madascha suddam.
Sampadayet kshaudra ghrita pragadair haritaki churnayutai prayogai
Snehana and swedana chikitsas are the poorva karmas of shodana chikitsa, but
swedana chikitsa is contra indicated in case of pandu roga, because it is pitta
pradhanavyadhi. The patients of pandu have dhatu kshayam which is due to improper
nourishment of rasadi dhatus. As a result, rukshatwa occurs in the body. This is a
necessary treatment before any shodhana karma. Shehana does srotho mardhava and
helps the doshas come out freely when sodhana karma is done. Snehapana is even
more important in case of mrit bhakshana janya pandu, because the mrit causes
rukshatwa in the srothas and causes obstruction in srotas. Sneha karma is indicated
before and after shodhana chikitsa in Mrit bhakshana janya pandu. Since Pandu

roga is pitta pradhana disease, the following tiktaghritas are mentioned for sneha
karma.
1. Pancha gavya ghritam
2. Maha tiktaka ghritam
3. Kalyana ghritam
4. Dadimadi ghritam
5. Katu ka rohinyadhi ghritam
6. Pathya ghritam
7. Danthi ghritam
8. Haridradi ghritam
9. Triphala ghritam
10. Draksha ghritam
11. Tilvakadi ghrita
12. Brahatyadi ghritam
3. Shodhana karma:
Charaka, Vagbhata and others recommended strong emesis and purgation after
giving oleation therapy.
Shodhana karma pulls out the doshas with their roots and prevents the
reoccurrence of the disease. The shodhanakarma indicated in pandu are Urdhwa
shodhanam (Vamana) and Adhah shodhanam (verechana)
A) Urdhwa shodhanam (vamana): Charaka stated that teekshana guna yukta
vamana oushadhas are indicated in pandu roga. Though susrutha contraindicated
vamana in pandu roga. Dalhana advocated Mridu vamana, when Rutu, Desha, Kala
are in favour. The drugs that are mentioned for vamana karma are
1. Dhamargava
2. Ikshwakum
3. Kritavedana.

B) Adhah shodana (virechana): Virechana is indicated in all types of pandu.
Hareetaki is advocated for virechana along with the following drugs.
1. Gomootrayukta dugdam
2. Dantiphala rasa and draksha choornam
3. Aragwadha majja with trikatu choornam
4. Phala ghrita
5. Tilwaka ghrita
6. Dadimadya ghrita
7. Pathyadi ghrita
8. Haridra di ghrita
9. Danti ghrita
10. Drakshadi ghrita
11. Doorva ghrita.Drugs for shodhana karma in panduroga according to doshic predominance :(Hetuviparitardakari chikitsa):
Name Vataja Pittaja Kaphaja Tridoshaja Mritbhakshanajanya
Cha Snigdha Tikta and Katu ruksha Tridoshahara Strong samshodana
& Madhu sheeta and Ushna of GIT
Su Snigdha Tikta and Katu ruksha Tridoshahara -
& Madhu sheeta and ushna
Vag Durgs Drugs of More Tridoshahara Strong purification
Possing bitter taste pungent dry therapy
sneha and cold and hot
potensive potency
BR Medicines Tikta and Katu ruksha Tridoshahara Strong purification
with gruta sheeta and ushna therapy
base medicines medicines
BV Mediciens Tikta and Katu ruksha,Tridoshahara Strong purification
with gruta sheeta and ushna therapy
base medicines medicines
YR Medicine Tikta and Katu ruksha, Tridoshahara Strong purification
with gruta sheeta and ushna therapy
base medicine medicines

4) Shamana chikitsa:
Samana karma of pandu according to doshic predominance
“Vatheke sneha bhuyestam paitthike tikta sheetalamSlaishmike katu tiktoshnam nimishramam saannipatheki”
l Vataja pandu roga is to be treated with snigdha and madhura dravyas.
l Pittaja pandu roga is to be treated with Tikta and Seeta dravyas.
l Kaphaja pandu roga is to be treated with katu Tikta rasa, and Ushna gunadravyas.
l Sannipathaja pandugaroga is to be treated with mishrita dravyas.
In shamana chikitsa, the following drugs are mentioned:
Single drugs:
Herbal drugs Mineral drugs
Pathy Loha bhasma / choorna
Amalaki Mandoora bhasma
Yashtimadhu Kaseesa bhasma
Draksha Abhraka bhasma
Brihat panchamoolas Swarna maksheka bhasma
Guda Silajit
Tila Pravala bhasma
Haridra Mukta bhasma
Shunti Sankha bhasma
Pippali Jasada bhasma
Bhringaraja Kantha bhasma
Kumari Tamra bhasma
Punarnava

Compound Herbo – Mineral preparations
1. Navayasa churna (Cha.Chi.16)
2. Yogarajam (Cha.Chi.16)
3. Mandhura vataka (Cha.Chi.16)
4. Ayoraja churnum (Cha.Chi.16)
5. Punarnava manduram (Cha.Chi.16)
6. Goudarista (Cha.Chi.16)
7. Beeja kalista (Cha.Chi.16)
8. Shilajet vataka (Cha.Chi.16)
9. Vyoshadhi choorna (As.Hri)
10. Kantavallabha ras (B.R.)
11. Hamsa mandooram (Y.R.)
12. Trilokyanath ras (Y.R.)
13. Chandra suryathmaka ras (Y.R.)
14. Prana vallabha ras (Y.R.)
15. Panchananavati (B.Ratna)
16. Anandodaya ras (B.Ratna)
17. Trilokya sundara ras (V.Chi)
18. Trimurthi sidda ras (V. Chi)
19. Rasa sindhoora bhooshana ras (V.Chi)
20. Udaya bhaskara ras ((V.Chi.)
21. Kameswar ras (V.Chi)
22. Pandu sudana ras (V.Chi)
23. Vangeswar ras (V.Chi)
24. Loha sundara ras (V.Chi)
25. Siddha mandoora (V.Chi)
26. Bala suryodaya ras
27. Kanta vallabha ras
28. Rajatha loha rasayanam
29. Sodhari mandoora

Avalehyas
1. Datri avalehya
2. Mandooradi avalehya
3. Vidangadi avalehya
4. Chinchadi Lehya
5. Chawan prashavalehya
Asava / Arishtas
1. Goudarishta
2. Beejakarishta
3. Dhatryarishta
4. Lohasava
5. Ayaskriti
6. Bringarajasavam
7. Kumari asavam
8. Punarnavasavam
Anupaana:
The substance that is consumed along with or after the intake of oushadha dravya is
Anupana. This may be either solid or liquid in nature. Anupaana should fulfill the
following principles.
1. It is pacify the atiteeskha guna, vyavayi and vikasi gunas of the main drug e.g.
Ghrita, Takra and Ksheera.
2. It is to stimulate the action if the drug is less potent. E.g.: Trikatu and gomootra
3. To carry the drug to specific location where its action is needed. For this a
dravya possessing yogavahi guna is needed. Eg. Madhu.
4. A drava dravya is needed as an anupana for easy swallowing of choorna (or)
gutika.
5. To create the palatability if the drug cannot be swallowed because of
reluctance.

The following are a few anupaanas mentioned in the context of pandu roga by various
authors.
1. Takra
2. Godugdha
3. Goghrita
4. Jala
5. Ikshurasa
6. Madhu
7. Gomootra
8. Triphala kashaya
9. Buffalo’s milk / mootra
Susruta mentioned that if a person had profuse blood loss he should drink blood
with madhu or take liver of a goat. (Su.Utt 44).
References:
1. Cha. Samhita chi. 16th chapter
2. Susruta, uttara, 44th chapter
3. Asthanga sangraha. Chikitsa 18th chapter
4. Ashtanga Hridaya chikitsa 13th chapter
5. Basava rajeeyam
6. Yogarathnakara
7. Bhaishajya Ratnavali
8. Vyadhya chintamani
9. Vydhya yoga Ratnavali
10. Sahasra yoga
11. Gada nighantu
12. Ayurveda vignanam
13. Saranga dhara samhit

PATHYA AND APATHYASThe knowledge of Pathya and Apathya is essential in treating the disease. All
the nidanas mentioned in nidana aspect are to be strictly considered as apathyas and
are to be avoided.
Those aharas and viharas, which are against the nidana as well as the disease are
called ‘Pathyas’. In contrary, the aggregating factors of the disease are called
‘Apathyas’.
Pathya (Upasaya): Food that are capable of causing agnideepana should form as
important principles of pathya – vyastha of pandu roga.
1. Rasa: Madhura, tikta, kashaya rasa
2. Guna: Guru, Rukshana, Teekshna gunas
3. Panchakarma: Vamana & Virechana
4. Ahara: Ahara – Godhuma, yava, shashtika danya, salidhanya
5. Yusha: Mamsarasa – Jangala mamsa & shringifish
7. Vegetables: Patola, vrudha kooshmanda, tarunakadhali phala, bimbi, vartaki,
lasuna dwaya and Jeevanthi
8. Others: Guduchi, Tanduleeyajalam, Punarnava, dronapushpi, Hareetaki,
Amlaki, Butter milk, Payasa, Ghee, Sowvearaka, Tushodaka, Navaneeta,
Gandha sara, Haridra, Vasa, Dadima, Nagakesara yavakshara, Lohabhsma and
Kunkuma.
9. Fruits: Draksha, karjura, and mango fruits
Apathyas:
1. Guru: Guru, ruksha, teekshana gunas
2. Rasa: Katu, amla rasa
1. Panchakarma: Raktamokshana, Dhumapana & Swedana.
2. Vihara: Atimaidhuna
3. Mamsarasa: Gramya mamsa rasa
4. Others: Shimbi, chitraka, masha, ambupana, pinyaka, tambula, sarsapa, sura,
all kinds of amla and virudha ahara.

Even the nidanas mentioned for the disease can also be considered as apathyas.
The knowledge of pathya and apathya is essential in diagnosing the disease. When the
nidanas, poorva roopa and roopa are not giving the perfect knowledge of the disease.
References:
1) Susruta samhita, Uttara Sthana, 44th chapter.
2) Hereeta samhita, Triteeya Sthana, 8th chapter
3) Basavarajeeyam Panchama Prakaranam
4) Asthanga Sangraha, Chikitsa Sthana, 18th chapter
5) Yogaratnakara, Madhyama Khanda.

CRITERIA FOR SELECTION OF THE DRUGThe drug selected for present clinical study is "Bhaskara Lavana Churnam". Its
anupana is "TAKRA". The administration of Bhaskara Lavana Churnam is advised in
the condition of panduroga. The drug has been selected to evaluate its efficacy in
pandu roga. The reference to the present clinical study is taken from the Baishajya
ratnavali.
"Pleehanamasmari Chaiva Swasakasaodara krimeen
Visheshatah Sarkaraadeen rogaannanavidhamstha the
Pandurogamseha vividhannasayatyasanirya tha"
(Bhaishajya ratnavali-Agnimandhya chiktsa)
The administration of Bhaskara lavana churna is advised in the condition of
Pandu, Pleehavyadhi, Krimi, Ajeerna, Aruchi, Arshas, Shoda, Amadosa. The drug has
been selected to evaluate its efficacy in pandu.
The preparation is non contraversial and the ingredients are easily available. This
formulation is easy to prepare and free from toxic effect.
The compound herbo mineral drug Bhaskara lavana churnam consists of
ingredients Samudra lavana, savarcha lavana, saindava lavana, Bida lavana, Dadima
beeja, Pippali, Pippalimula, Dhanyaka, Kalajeera, Teja patra, Talisa patra,
Nagakesara, Amla vetasa, Kalimareecha, Swetha jeera, Sunti, Twak, Ela. So this
Bhaskara lavana churnam mainly Tridoshahara, rasayana, Deepana, Pachana, Hridya,
Balya, Ruchya properties. It helps in pitta dosha samana, Deepaneeya and rakta
vardhaka. It has the direct action on Amasaya, Yakrit and Ranjaka pitta.
Agni vikriti is another importent clinical condition of pandu roga. Samagni is an
essential factor for the proper digestion and assimilation of ahara rasa, with the
mandagni avastha samyak ahara rasa formation will not take place. According to
charaka rakta poshakamsas are present in rasadhatu and owing to improper rasa
formation, proper development of raktadhatu is not possible, and the above condition
results in raktalpata.

In Bhaskara lavana choorna the pippali, pipplimula, tejo patra, Amla vethasa,
Jeeraka, Sunti, Twak and Ela mainly possess the properties of pitta dosha shamana
Agni Deepana, pachana and raktavardhakas, therefore helps in the production of
intrinsic factor and assimilation of extrinsic factor. It also avoid the accumulation by
virtue of its purgation property.
The pandu roga is pitta prakopaka vyadhi. In general the salts, main the saindava
lavana being seetagunam, Snigdhaguna, Avidhahi, Madura vipaka and Tridoshahara.
It acts pitta samaka. All salts are accepted as good preservatives which help in
reataining the potency of the prepared medicine for longer periods.
The pippali is explained as Rasayana in Ayurveda, addition of pippalli and
lavana churnas to the ingredients may help in faster absorption of the drug.
The Dadima, pippali, pappli mula, Dhanyaka, jeeraka, Tejo pathra and Twak
contains the property of krimigna. So are responsible for the elimination of worm
infestation, which is the one of the cause of the pandu roga.
The pippali, Amlavetasa, Twak, Talesaptra and contains the property of
"Ruchyam". In pandu roga imparment of the taste was seen due to rasa and Rakta
dhatu dusti. So this may help to increase the taste.
The Shunti, Jeeraka, Dhanyaka, contains 'grahi' guna, that is responsible for the
active absorption of lohasma in ahara and oushadha.
The Balya property of swethajeeraka assists in alleviating the dhatukshya and
ojokshaya, present in Pandu Roga.
The statement "Samanyam Ekatwa karam" mentioned in ayurvedic classics is
justified by asrik prasadana propperty of Dadima, Shunti, Jeeraka in pandu roga.
One of the sign of anaemia i.e. Palpitation is relived by the Hridya property of the
Amlavetasa, Dadima and Shunti.

DESCRIPTION OF INDIVIDUAL DRUGS
SAINDHAVA LAVANA
Synonyms: Sitasiva, manimantha, and sindhija, (Saindhara, sindhuphala, vasira,
sindhudesaja, Sindhu mandaja, sivasidda, palga)
Telugu - Saindava lavanam
Hindi - Saindha namak
English - Sodium chloride
Rasa - Lavana, Madhura
Guna Laghu, snigha, sukshma
Veerya - Seetha
Karma - Ruchyam, Agnideepanam, Amapachanam, Vrushyam,
Netryam.
This is commonly known as Rock-salt and is obtained in the form of hard lumps
in the mines in Beluchistan, sindh and upper Punjab. It is natural sodium-potassium
chloride.
SAMUDRA LAVANA
Rasa - Tikta, madhura
Guna - Guru
Veerya - Not very hot
Vipaka - Madhura
Karma - Agnideepanam, Virechanam, Ksharam, Not vidhahakaram(Slight alkaline), Shleshmakaram, vataharam, not causing
dryness, not causing coldness.
This is commonly salt prepared by evaporating sea water and is sodium
chloride in impure form.

SAUVARCALA LAVANASynonyms: Sauvarcala, Rucaka, Manthapaka
Telugu - Sauvarchala lavanam
Hindi - Kalanon
English - Black salt
Guna - Laghu, Visha, Sukshma,
Karma - Ruchyam, Bhedanam, Agnidepanam, Amapachanam, Slight
snehanam, Vataharam, not causing great increasing
Pitta, Vishadam, Udgara shuddi, Vibanda, Anaha, Shoolaharam.
BIDA LAVANAM
Synonyms - Bida Lavana, pakya, krtaka, dravida and asura
Telugu - Bidalavanam
Hindi - Viriya, Kalanamak
English - Black salt
Guna - Laghu, Tikshna ushna, ruksha, vyavayee
Veerya - Ushna
Karma - Slightly alkaline, Vata kapha Haram, Deepanam,
Ruchyam, Vibhandham, anaha, Vistabda, Hruthshoola,
Gowrava, Shoola haram.
This is known in the markets as kala namak or black salt and is an artificial
product, prepared by mixing saindhava, haritaki, amalaki, and sarjakshara (sodium
carbonate), boiling these in water tilt evaporation is complete. Then the mess is
broken to pieces and sold.

SHUNTISynonyms : Viswabheshaja, Nagara, Ushna, Katubadra,
Sanskrit : Nagara
Telugu : Sunti
Hindi : Sonti
English : Dry Zinger
Latin Name : Zingiber officinale
Family : Zingiberaceae
Gana : Pippalyadi, Triptighna, Deepaniya, Vachadi,
Arshoghna, Sthanya Shodana, Trishna
Nigrahana, Sheeta prasamana,
Shodhaprashamana, Pachaneeya,
Haritakyadi varga
Rasa : Katu
Guna : Laghu, Snigdha
Veerya : Ushna
Vipaka : Madhura
Parts used : Rhizome
Karma : Kapha vata hara, Deepaniya, Ruchya, Hridya
Swarya, Vrishya.
Indications : Swasa, Kasa, Chardi, Shoda, Shoola, Agnimandya,
Vibanda, udara roga.
Chemical composition : Ginger contains volatile oil. Comphene,
Phellaudreve, Zingibarine, Cincol, borncol and
Ginger oil an purgent, an Alcoresin, Ginger,
Starch mucilage, potassium, oscolate, the
Essential oil and resin.

DADIMASynonyms Phalamla, Kucaphala, Sukavallabha, Kuttima,
Phalasadava, Raktabija, Karaka, Nila patra, Raktapuspa
Botanical name punica granatum
Family punicaceae
Telugu Danimma kaya
Hindi Anar
English pomegranti
Malayalam matalam
Tamil maduli
Ganas According Caraka – hridya, chardinigrahana
Susruta – Parusakadi
Vagbhata - Parusakadi
Types According to Kaiyadevara & Bhavamisra –
3 vareities of dadima
1. Svadvamla 2. madhura 3. amla
Rasa Kasaya. Madhura, amla
Guna Laghu, snigdha
Virya Ushna
Vipaka Madhura / Amla
Karma Tridoshahara, Hridya, Sukrala, Grahi,
Dosage Fruits juice 20-50ml. decoction 40-80ml. bark powder 3-
5g
Part used Fruit
Chemical compositon Fruit peels – Kannins, Punicatin. Seeds, Estrone, Danicic
Danicic acid
Stem – Malvidin, Pentosa, Ilucosides, Tannin
Ca, Mg, Na, Iron, Tamram V B1 B2.

PIPPALI
ynonyms: Kana, Krsna, Kola, Capala, Triksna Tandula,
Magadhi, Vaidehi, Usana, Soundi.
Botanial name: Piper longum linn
Family: Piperaceae
Hindi Pipal ,
English Long pepper
Telugu Pippallu
Tamil Tippili
Bengali Pipul
Malayam Tippali
Ganas: According to Susrutha Pippalyadi, Urdhvabhagahara,
Triyushana (Trikatu) Amalakayadi, Sirovirecana.
According to Vagbhata Pippalyadi ( A.S)
Past Used : Fruit, Root
Rasa Katu,
Guna Laghu, Snigdha Tiskhana
Virya Ushna,
Vipaka Madhura
Karma: Vata Slesmahara, Dipana, Vrusya, Rasayana.
Indications: Udara, pliharoga, jwara, kustham prameha, Gulma,Arsas, sula, amavata.
Major Chemical : Essential oil, Mono and Sesquiterperes,
Caryophyllore piperine, piplartine, piperlogumine,
piperlonguminine, pipernaline, pipelanguminine,
Pipernonaline, piperundecalidine, pipercide, secamin,
b- situsteror, four aristolactams (cepharanone B,
aristolactum (u).

PIPPALI MULA
Synonyms Kana, Krisna, Kola, Capala, Tiksnatandula, Magadhi, Vaidehi,
Sauna, Soundi
Botanical name Piper longumFamily Piperaceae
Telugu Pippallu
Hindi Pippala
English Long piper
Tamil TippiliGanas According to Kasahara, Hikkanigrahana, Seroverechana,
Vamana, Triptigna, Deepaniya, Shoola prasamana
According to susrutha – pippalyadigana
According to vagbhata – pippalyadi
Types According to susrutha & vagbhata havedefined 2 varietes pippali, Gajapippali
According to Rajanighantu – provides 4 varieties of
pippali 1. pippali 2. gaja pippali 3. simhapippale
4. Vanapippale
Gunas Text Rasa Guna Veerya VipakaCharaka Katu ushna
Bhava Katu snigdha Anushna Madhura
prakasa laghu
Dhanvantari Katu snigdha ushna Madhura
Nighantu laghuKaiyyadeva Katu snigdha Anushna Madhura
Nighantu laghu
Karma Udara, pliharoga, jwara, kusta, prameha, Gulma, Arsas,
Sula, amavata
Dosage: Powder ½ -1 gramsPart used: Fruit, root
Chemical compositon Essential oil, and sesquiterphon, caryophyllene (mainly),
piperine, piplartine piper longumine, sesamin, B-site sterol, Resin, Olatile oil.

DHANYAKA
Synonyms Kustumburo, Chatra, Vittunnaka, Dhanyaka
Botanical name Corundum satirum
Family Umbellifere
Hindi Dhaniya
Telugu Dhaniyalu
English – Coriander seeds
Ganas According to Caraka – Trsnaprasamana, Sulaprasanama
According to Susrutha – Guduchyadi
According to Vaghata - Guduchyadi
Rasa Kasaya, tikta,
Guna Laghu, snigdha
Veerya Ushna
Vipaka Madhura
Karma Tridosha hara, Deepana, Paachana, Grahi
Indications Jwara, Daha, Trusna, Chardi, Kasa, Swasa, … arsas
Dosage Fruit powdar 3-6 gms, cold infusion 20-30ml
Part used Fruit, whole plant
Chemical compositon Coriandrinol (glucoside) carotene cugenol, bergapten.

TEJO PATRA
Synonyms Tumburu, tejasvini, tejovati, vanaja, sourabha
Botanical name Zanthozylum ilatum
Family Rutaceae
Hindi Tejabala
English Toothache tree
Bengali Nepali dhana
Ganas According to Caraka Sirovircchana, katu skandha
Rasa Katu
Guna Laghu, ruksa
Virya Usna
Vipaka Katu
Karma Kapha – Vata hara, Kanthya, Dipana, Pacana
Indications Hrdroga, Mukha roga, Dantaroga, Kantha roga, Hikka,
Agnimandya, Arsas, Svasa kasa, Amavata, Apatantraka,
Udara
Chemical compositon Bark – herberine, xanthoplanine
Fruit – arginine, histidine, thujene
Root - spilanthol

TALISA PARTRI
Synonyms: Dhatripatra, patradhya, sukodara
Botanical name abes webbiana
Family pinaceae
Telugu & Tamil Talisapatri
Hindi & Bengali Tallispatra
English Indian silver
Ganas: According to susruta -sirovirecana
Types : According to Yadaviji trikamjit quoted 3 varieties
(1) T. baccata (2) A. webbiana (3) R. lepidotum
Rasa Tikta, madura
Guna Laghu, tiksna
Veerya Usna
Vipaka Katu
Karma: Kapha, Vatahara, Hridya, Dipana
Indications: Svasa, Kasa, Mukharoga, Ksaya, Chardi, Aruchi,
Agnimandya, Gulma, Raktapitta, Hikka
Chemical compositon: Abesin, n-triacontanol, B.Sitosterd, betuloside,
Riboflavonoid, betuloside

NAGAKESARA
Synonyms: Ahipuspa, loha. Kanakahva, kancanahvaya, kinijilkam,
kesaram, campeyam, natam, nagam, naga kinjilkam.
Nagapuspam, naga renuka, pinjaram, phani pannagam,
rukmam, suvarnam hemapushpam.
Botanical name Mescea ferrea
Family Guttiferae
Telugu Naga kesaralu
Hindi Iron wood of assam
English Naghas
Kannada Kanchana
Ganas: Susruta – Eladi, vacadi, anjanadi, priyangvadi ganas
A.S.S. – Eladi, vacadi, anjanadi, priyanvadi
A. Hrdaya – Eladi, vacadi, Anjanadi, priyanvadi ganas
Dhanvantaric nighantu – satapuspadi varga
Shodhala – satapuspadi varga
Kaiyadeva nighantu – osadhi varga
Types: 1. Mesua ferrea 2. ochro carpus longitolas
Rasa Kasaya, tikta
Guna Ruksha, Tikta, laghu
Virya usna/anusna
Vipaka katu
Karma: Kapha pittahara,. Pramathi, Grahi, Pachana, Visahara,
sothahara, kandughna, kusthaghna
Indications: Raktarsas, Raktatisara, Raktapradara, Kusta, Visarpa,
Jvara, Chardi, Vasti vikara, Vata rakta, Sopha, Vataroga,
Siro roga, Trsna, Visa roga, Kandu
Dosage: Powder of stamens 1-3g orally
Part used: Stamens
Chemical compositon Squalene, cycloartenol, campesterol, stigmasterol,
And bitosterol

MAREECHA
Synonyms : Mareecha, ushana, Vellaja, Krishna, Dharmapattana
Sanskrit : Mareecham
Telugu : Miriyalu
Hindi : Kalimirch, mirch
English : Black peper
Latin Name : Piper nigrum
Family : Piperaceae
Gana : Deepaniya, Shoola prasamana, Krimighna (Charaka);
Pippalyadi, Tryushana (Susrutha)
Rasa : Katu
Guna : Laghu, Teekshna, Guru (Ardra)
Veerya : Ushna
Vipaka : Katu Madhura (Ardra)
Parts used : Fruit
Karma : Kaphavatahara, Deepana, Avishya
Indications : Aruchi, Kasa, Peenasa, vishamajwara, Atopam.
It is also useful in coagulative disorders. It has
Bacteriostatic and fungistatic properties.
Chemical composition : Moisture 10.6, Protein 4.8, Fat 2.7,
Carbohydrates –13.7, Fibre 6.4, Mineral matter 1.8,
Calcium – 210, Phosphorous 17, Iron 2.4,
Thiamine 0.05, Riboflavin 0.04,
Nicotinic acid 0.2, Ascorbic acid 1 mg and
Vit. A. 1800 Im. And oxalic acid etc.

SWETA JIRAKA
Synonyms Ajaji, kana, jarana, dirgha jiraka
Botanical name cuminum cyminum
Family umbelliferae
Telugu JilakarraHindi Safed jeera
English Cuminum seeds
Marathi Jircin
Kannada Jirige
Ganas: Caraka – SulaprasamanaSusruta – pippalyadi
Vagbhata - pippalyadi
Types: According to Su. Su. 46 – Jiraka dvaya
In Dhanvantari nighantu – 4 vareities
1. Jiraka (Ajaji)2. Sukla jiraka (suklajaji)
3. Krishna jiraka (krsnajaji)
4. Vanya jirah (Bhhatphali)
According to shodala– 3 varieties (1) Upakunchika
(2) Sukla (3) KrishnaRasa Katu
Guna Laghu, ruksa
Veerya Usna
Vipaka Katu
Karma: Kapha – Vata hara, Dipana – Pachana, Grahi, Visya,Atisara, Gulma, Visa roga, Netra roga.
Indications: Krimi, Jirna Jvara, Adhmana, Kustha, Grahani, Atisara,
Gulma, Visa roga, Netra roga
Dosage: Fruit powder 3-6g
Part used: FruitsChemical compositon: cuminin, isoimperatorin, cuminaldehyde,
P-cymene, diacyl glycerol, imperatorin) paspharus,
calcium, iron. Vit A.C. etc. …

KRISHNA JIRAKA
Synonyms: Udgarasodhana, sugandha
Botanical name Carum carvi
Family Umbelliferae
Telugu Nallajilakarra
Hindi Syahajira
English Black caraway
Types Certain nighantu works described sexvareiteis
1. Sveta 2. Pita 3. Krsna 4. Suksma
5. Sthula 6. Vanyajeerakas
Rasa Katu
Guna Ruksa
Veerya Usna
Vipaka Katu
Indications Jvara, Chardi, Atisara, Gulma, Adhmana, Ajeerna
Dose Fruit powder 1-3 grms
Part used Fruit
Chemical compositon Essential oil, tricylo glycerols sterols, petroselinic acid,
essential oil – carone

CHOTI ELASynonyms Korangi, Dravidi,Tuttha, Triputa, Trtisthula
Ela – Bhadra Ela
Botanical name Electtaria cardamomum
Family Scitaminae
Telugu Chinna elakules
Hindi Chotiilaychi
English Lesser cardamom
Tamil Yelakka
Kannada Elakki
Ganas Caraka – Svasahara, Angamarda prasamana, Katuka
Skandha, Sirovirecana.
Types: All the texts have mentioned 2 variation of Ela
Sukshma Ela (E. cardamomam)
Brhat Ela (A. subulatum)
Rasa Katu, Madhura
Guna Laghu, ruksa
Veerya Sita
Vipaka Katu
Karma Kapha – vatahara, hrdya, sukra nasaka, deepana,
pachana
Indications Hridroga, svasa, kasa, mutrakricchra, chardi, sirahsula,
Arsas.
Dosa Powder 0.5-1 g
Part used Seeds
Chemical compositon Camphor citral, terpeneols, cymene, heptane sitosterol

TWAK
Botanical Name Cinnamomum Zeylanica Blume
Family Lauraceae
Hindi Dalchini
English Cinnamon
Telugu Lavanga patta
Tamil Ilayangam
Bengali Daruchini
Gujarati Taja
Synonyms: Utkata, tanutvak, darusita, varanga, svadvi, tvak,
Patta, bhrngam, kavaca, sakala, saihala , latapatra,
ramapriya
Ganas According to Susruta-eladi
According to Vagbhata Eladi, trijataka
Rasa Katu,
Tikta Madhura,
Guna Laghu, Ruksha, Tiksna,
Veerya Ushna
Vipaka Katu
Karma Vata pittahara, Sukrala, Balya, Vatarsas, Grahi
Indications Kandu, Amajirna, Aruchi, Krimi, Hridroga
Part Used Stem bark, oil

ANUPANA - TAKRASynonmys : Takra, Chachika, Dandahata, Gloha Gorasa,
Drava, Amla, Kekara, Madhita, Malima, Bhagna,
Sandhika, Gorasaja, Kalasheya, Vilodita, Arista,
Udasvitm Pramadhita, Ambare, Ghula, Kevala.
Telugu : Majjiga, Challa
Hindi : Chancha, Matta
English : Butter milk
Rasa : Madhura, Amla, Kashaya
Guna : Laghu, Rooksha, Grahi, Vikasi, Sara
Veerya : Ushna
Vipaka : Madhura
Karma : On dhoshas: Tridoshaharam
Indications : Agnimandyam, Pandu, Chardi, Grahani, Arshas,
Udara, Atisara, Aruchi, Krimi etc.
Description : It is not a ready made, but it is of from milk
through some of procedures.
Regarding its preparation, there are variations Samhita to samhita, on the basis
of preparation of Takra it is of 4 types (Dhanvantari-Nighantu and Susrutha) and 5
types (Bhava Prakasha). This Takra is one of the type among these.
Details: According to Bhava Prakasha
1. Gholam - By churning curd without water
2. Madhitam - By squimming the curd; excluding the outer layer and water.
3. Takram- Which is out of churned the curd by adding 1/4 part of water to it.
4. Udwasit - Which was by churned the curd which is long with half of the
water mixed.
5. Chachika - By squimming the curd with large quantity of water.

Where as Susrutha explained 4 types of Takra, but gave the description of the
Takra preparation, as it can be prepared by squimming the curd by adding Half
quantity of water to it.
"Seethakale agnimandye cha tada vatamayeshu cha
aruchow srothasam rodhe takram syadamruthopamam
....Tattu hanti pandu medo grahanyarso mutra graha bhagandaran"
"Na takra sevi vyadata kada china takra dagdhah prabhavanti rogah
yada suranam amrutam sukhaya tatha naranam bhuvi takramahu"
(Bhava prakasha)
According the modern system, there is slight difference between milk and butter milk.
Milk and butter milk same lactic Acid, whereas butter milk will not contain fat and
contains proteins as like as milk, because this is free from butter. Butter milk contains
lacto bacilie ie., useful bacteria, which helps in the modification of milk to curd. There
is change in the action also; milk can act as mild laxative, butter milk acts in reverse
way, which is helpful for diarrhiea, as we are saying in the society.

MODE OF PREPARATIONThe preparation of Bhaskara Lavana Churna was prepared as follows according
to Baisadya Ratnavali- Agnimandhya chikitsa Chapter.
Name of the drug Quantity
Samudra Lavanam 374 gms
Dadima Beeja 187 gms
Sauvarcha lavana 234 gms
Choti Pippali 94 gms
Pippali mula 94 gms
Dhanyaka 94 gms
Kalajeera 94 gms
Saindhava lavanam 94 gms
Bida lavanam 94 gms
Tejo patra 94 gms
Talisa patra 94 gms
Naga kesara 94 gms
Amla Vetasa 94 gms
Kali mareecha 47 gms
Swetha jeera 47 gms
Sunti 47 gms
Twak 24 gms
Choti Ela 24 gms
The above mentioned ingredients were collected in pure form the market. At
first, the all drugs were individually powdered finally and then mixed together in the
quantities mentioned above. The powder was weighed and several packets were

made each containing 2 gms of the drug. These were distributed to the patients.
Dose : 2 gms thrice a day
Time : Morning, Afternoon and evening after
principle meal
Anupana : Takra
Duration of treatment : 45 days
Indications: Pandu, Pleehavyadhi, Krimi, Ajeernya, Aruchi, Arshas, Shoda,
Amadosa, Gulma, Udara, Udararoga, Kshaya, Grahani, Kusta, Malabanda,
Hritishoola, Asmari, Sarkara.
By virtue of its propperties, the compound drug works in gastrointestinal, and
nutritional deficiency anemias.

MATERIALS AND METHODS
The materials required a clinical study on the effect of "Bhaskara lavana
Choorna" in the management of Pandu roga are
1. Patients
2. Parameters
3. Drug
1. Patients:
Selection of patients: Totally, 30 patients suffering from pandu are selected
randomly from the out-patient Department of Post graduate unit, Kayachikitsa
Department of Dr. B.R.K.R. Government Ayurvedic Hospital, Erragadda,
Hyderabad.
30 patients were examined thorougly according to the Lakshanas, Dasha vidha &
Ashta sthana pareekshas, and laboratory investigations. Those patients, who have been
elicited about rogi and roga pareeksha are noted in the proforma of special case sheet
of pandu roga, which is enclosed.
Inclusion criteria:
1. Pandutwa
2. Swetha nakhata
3. Agni mandhya
4. Aruchi
5. Kapha praseekam
6. Anga mardha
7. Brama
8. Jwara

9. Pindiko dwesta
10. Tandra
11. Alasya
12. Gowravam
13. Akshi koota sodha
14. Krimi kosta
15. Daha
16. Prabha heena
17. Swayathu
18. Palpitation
Exclusion of criteria:
1. Pateints suffers with cardiac diseases
2. Patients who are below 6 grams of haemoglobin
3. Hemorrhagic disorders Eg: Hemorroids
2. Parameters: The parameters that are used in assessing the results can be divided
into two categories.
a. Subjective parameters
b. Objective parameters
a. Subjective parameters:
The following have been taken as subjective parameters.
i. Relief of clinical signs and symptoms
ii. Appearance of Rakta saara lakshanas
b. Objective Parameters:
The following have been taken as objective parameters.

i. Hemoglobin Percentage
ii. Red blood cells count
3. DRUG REGIME: The drug Bhaskara lavana choornum a compound Ayurvedic
preparations, mentioned in Baisajya Ratnavali is selected to evaluat for anti
anemic activity.
THE METHODOLOGY:
a) The aim of the study:
Normalized the levels of Hb% in the Anemia.
b) Type of trial - open trial:
c) Mode of administration - oral
d) Method of administration:
Bhaskara lavana choornum started immediately after the
diagnosis of anaemia is confirmed
e) Dose of the drug
Bhaskara lavana choornum 6gms thrice a day. It is given in
three doses of 6 gms of the each principal meal.
f) Period of drug:
The progress of the patients is observed and recorded after every 21 and 45
days. This procedure is followed for duration 45 days. After the completion
of the duration, the results are assessed based on the observations.
g) Anupana - Takram:
The drug is given continuously for 45 days without any interuption and
Pathya, Apathyas are advised.

ASSESSMENT OF RESULTS:
After completion of the treatment the results are assessed in terms of Pravara,
Madhyama and Avara. The criteria adopted for the gradation of Lakshanas is shown
by the sign '+', and absence of Lakshanas is shown by the sign '-' .
The criteria adopted for this is given below:
1. PRAVARA: The result is concluded as Pravara when,
i. All the signs and symptoms present before starting the treatment are
relieved upto to 75% with no side effects
ii. Increase in Hemoglobin levels in between 12-15 grams.
iii. Increase in RBC count is between 4.5 and 6 million cells/cumm.
2. MADHYAMA: The result is concluded as Madhyama when,
i. The signs and symtpoms present before starting treatment are relieved
upto 50%.
ii. Increase in Hemoglobin levels is between 10-12 grams
iii. Increase in RBC count is between 3.5-4.5 million cells/ comm.
3. AVARA: The result is concluded as Avara when
i. The signs and symptoms relieved upto 25%.
ii. Increase in Hemoglobin levels is less than 10 grams
iii. RBCs count is less than 3.5 million cells/cumm.
Finally, all the information regarding the patients is noted down in various tables and
bars. These are presented in diagrams, so that records could be prepared properly. The
tables showing information regarding sex incidnece, mentioned in the chapter of
observation and results.

OBSERVATIONS
Thirty patients of Pandu attending the Postgraduate Kayachikitsa, department of
Government Ayurvedic Hospital, Erragadda, Hyderabad are randomly selected for
this clinical study.
The patients are classified into various groups according to the 1. Age, 2.sex, 3.
Diet, 4. Economical status, 5. Signs and Symptoms, 6.Occupation, 7. Ahara and 8.
Prakriti.
The Signs and Symptoms, Hemoglobin Percentage and Red blood count before the
treatment are recorded. The condition of the patients is reviewed after every 15 and 45
days of treatment. It is continued up to a duration of 45 days and the observations
were recorded.
Table 1: According to Sex:
Sl.no. Sex No. of cases Percentage
1 Male 4 13.33
2 Female 25 83.33
3 Children 1 3.33
Out of thirty cases 25 cases were females, 4 cases were male and 1 male
children were seen.
No. of Patients
Male
Female
Children
3.3%
83.33%
13.33%

Table 2. According to Age:
S.No. Age group No. of male No. of female Total Percentagein year patients patients
1 0-10 1 0 1 3.33
2 11-20 0 3 3 10
3 21-30 1 9 10 33.33
4 31-40 3 9 12 40
5 41-50 0 4 4 13.33
30 patients were classified according to the ages as shown in table 2.Maximum cases
was seen in 31-40 year age group.
Table: 3 According to Diet:
S.No. Diet No. of male No. of female Total Percentagepatients patients
1 Vegetarian 2 11 13 63.33
2 Mixed 3 14 17 36.66
In the present study the vegetarians are 63.33%, ( 13 out of 30) and mixed diet were seen 36.66% (17 out of 30).
Table 4: According to Economical status:
0
1
2
3
4
5
6
7
8
9
0-10 11-20 21-30 31-40 41-50
M ale
F em ale
Age in Years
0
2
4
6
8
10
12
14
V egetarian M ix ed
M ale
Fem ale
Type of diet

Table 4: Accoridng to Economical Status :S.No. Economical No. of male No. of female Total Percentage
patients patients
1 Poor 4 15 19 63.3
2 Middle 1 8 9 30
3 Rich 0 2 2 6.66
The patients were observed as per socio-economical status based on their
monthly income. Out of 30 cases 19 casses were poor, 9 cases were middle classes, 2
cases were seen rich.
Table 5: According to Occupation:
S.No. Occupation No. of male No. of female Total Percentagepatients patients
1 Labour 3 15 18 60
2 Student 1 6 7 23.33
3 Sedentary 1 4 5 16.33
Out of 30 cases, 18 casses were labour, 7 cases were Student and 5 sedentary
cases were seen.
Table 6: According to Prakriti:S.No. Prikriti No. of male No. of female Total Percentage
patients patients
1 Vata 2 6 8 26.66
2 Pitta 1 5 6 20
3 Kapha 2 14 16 53.33
In the present study 16 casses were Kapha predominent prakriti, 6 casses were
Pitta predominent prakriti and 8 cases were seen Vata predominent prakriti.

Table 7: Symptoms present Before and After the treatment:
S.No. Symptoms BT After treatment Percentage
1 Pandutwam 30 28 93.33
2 Sweta nakhata 30 25 83.33
3 Agni nasanam 30 30 100
4 Aruchi 24 21 87.5
5 Angamardha 24 18 75
6 Kapha praseka 24 20 83.33
7 Brama 10 5 50
8 Jwara 15 13 86.66
9 Pindiko dweshta 20 14 77.77
10 Tandra 20 16 80
11 Alasya 20 16 80
12 Gowravam 25 22 88
13 Akshikoota sodha 4 2 50
14 Krimi kosta 4 2 50
15 Daha 13 10 33.33
16 Prabha heena 20 14 70
17 Swayathu 5 3 60
18 Palpitation 20 13 68.42
In the present study symtpoms and signs seen before and after the treatment

MASTER CHART, SHOWING DATA IN RELATION TO PANDUROGA
After treatment Before treatmentS.No
Name Age Sex
RegNo.
Diet Econo-micalStatus
Occupation
Prakrati 0 days 21 days 45 days Result
Hb RBC Hb RBC Hb RBC1 Rajyalaksh
mi30 F 11185 Mixed Middle Sedentar
yPitta pre. 7.0 3.2 8.2 3.8 9.4 3.2 Avara
2 Vijayalakshmi
35 F 11117 Vegetarian
Poor Student Vata pre. 6.3 2.8 7.8 3.1 8.8 3.1 Avara
3 VijayaMarry
40 F 21492 Mixed Poor Student Kaphapre.
10.5 3.4 12.1 3.1 13.1 5.1 Pravara
4. Madhavi 25 F 11186 Mixed Middle Labour Kapha pre. 8.0 4.2 9.2 4.4 11.8 3.8 Madhyama
5. Mahaboobvali
40 M 14667 Mixed Poor Labour Kapha pre. 11.5 3.2 12.3 4.9 13.2 4.8 Pravara
6 Eswaramma
40 F 19184 Vegetarian
Poor Labour Kapha pre. 10.2 3.1 11.6 3.3 13.3 3.5 Pravara
7 Ramadevi 34 F 21497 Mixed Poor Labour Kapha pre. 9.0 4.2 9.4 4.4 11.6 4.5 Madhyama
8 Rajamma 45 F 21496 Mixed Rich Student Pitta pre. 10.0 3.8 8.6 3.9 9.8 3.9 Avara9 Jayasree 31 F 13120 Vegetaria
nPoor Sedentar
yKapha pre. 9.8 3.4 10.9 4.3 13.1 4.5 Pravara
10 Asiyabegum
27 F 5553 Mixed Middle Labour Vata pre. 8.0 2.9 8.8 3.6 9.8 3.8 Avara
11 Lakshmi 45 F 11582 Vegetarian
Poor Labour Kapha pre. 10.0 4.1 9.8 4.7 11.8 4.3 Madhyama
12 Tulasi 45 F 11118 Mixed Poor Labour Vata pre. 10.2 3.8 12.2 3.3 13.0 4.6 Pravara13 Sabeyabe
gum17 F 11135 Vegetaria
nMiddle Labour Kapha pre. 10.0 3.2 11.6 3.2 13.2 3.5 Pravara
14 Sudershan 6 M 11272 Vegetarian
Poor Sedentary
Vata pre. 7.0 3.2 9.2 4.3 10.0 3.5 Avara
15 Sarada 24 F 14287 Vegetarian
Poor Sedentary
Kapha pre. 8.5 3.8 9.4 3.9 10.8 3.8 Madhyama
16 Kirankumar
22 M 8505 Mixed Middle Student Pitta pre. 10.5 3.4 12.6 4.6 14.0 5.1 Pravara
17 Sunitha 23 F 8936 Vegetarian
Poor Student Kapha pre. 10.5 3.4 11.6 3.1 12.8 4.8 Pravara
18 Sailakshmi 24 F 8507 Mixed Poor Student Vata pre. 10.5 3.8 11.4 4.3 12.9 5.2 Pravara19 Seetamma 40 F 11116 Mixed Middle Labour Pitta pre. 9.8 3.6 9.2 3.8 12.0 3.7 Madhya
ma20 Faridabeg
um42 F 17771 Vegetaria
nPoor Labour Pitta pre. 11.0 3.2 12.8 3.6 13.1 4.8 Pravara
21 Reshma 20 F 19862 Mixed Rich Labour Kapha pre. 9.8 2.7 10.2 3.5 13.8 3.5 Pravara22 Kalpana 20 F 7716 Vegetaria
nPoor Sedentar
yVata pre. 10.5 3.3 10.9 3.7 13.6 4.8 Pravara
23 Madhuri 26 F 18873 Mixed Poor Labour Kapha pre. 9.5 3.2 10.6 4.0 12.9 4.6 Pravara24 Lingaiah 32 M 21722 Vegetaria
nPoor Labour Vata pre. 9.5 3.9 11.8 3.1 12.9 4.5 Madhya
ma25 Anitha 30 F 22646 Vegetaria
nMiddle Labour Vata pre. 11.0 3.8 12.8 3.3 12.9 3.5 Pravara
26 Ananta 34 F 21316 Mixed Middle Labour Kapha pre. 10.5 3.5 11.4 3.1 13.0 4.8 Pravara27 Taribai 35 F 11114 Mixed Poor Labour Pitta pre. 7.0 2.7 10.8 4.6 13.1 4.8 Pravara28 Amribai 30 F 11115 Mixed Middle Student Kapha pre. 7.3 3.8 11.2 3.8 13.2 5.0 Pravara29 Lakshmi 32 F 11583 Vegetaria
nPoor Labour Kapha pre. 8.2 3.1 10.3 4.0 12.9 4.8 Pravara
30 Yallamaiah
40 M 24705 Vegetarian
Poor Labour Kapha pre. 10.1 3.9 11.4 3.6 11.8 4.2 Madhyama
Final Result: After the completion of 45 days of treatmentPravara 60% (16 Female and 2 Male) Madhyama 23.66% (5 Female and 2 Males), Avara
16.66% (4 Female, 1 Male)

Table 8: Haemoglobin levels before treatment
Hb levelsin grams
3.1-4 4.1-5 5.1-6 6.1-7 7.1-8 8.1-9 9.1-10 10.1-11 11.1-12 12.1-13
Males 0 0 0 1 0 0 1 2 1 0Females 0 0 0 2 5 2 8 8 0 0Total 0 0 0 3 5 2 9 10 1 0Percentage 0 0 0 10 16.7 6.6 30 33.2 3.33 0
In the present study the haemoglobin levels ranged from 6 to11.5 gms/dlbefore the treatment.
Table 9 : Heamoglobin levels after 21days oftreatment
Hb levelsin grams
6.1-7 7.1-8 8.1-9 9.1-10 10.1-11 11.1-12 12.1-13 13.1-14
Males 0 0 0 1 0 2 2 0Females 0 1 3 5 6 5 5 0Total 0 3 3 6 6 7 7 0Percentage 0 3.3 10 20 20 23.33 23.33 0
Hb levels showed gradually increased with in 21days from the starting day of treatment.
1
2
0
5
0
2
1
8
2
8
1
00
1
2
3
4
5
6
7
8
Males
Females
0
1
0
3
1
5
0
6
2
5
2
5
0
1
2
3
4
5
6
Males
Females
6.1-7 7.1-8 8.1-9 9.1-10 10.1-11 11.1-12 Hb levels (gms)

Table 10 : Heamoglobin levels after 45 days of treatment.
Hb levelsin grams
8.1-9 9.1-10 10.1-11 11.1-12 12.1-13 13.1-14 14.1-15
Males 0 1 0 1 1 2 0Females 1 3 1 4 8 8 0Total 1 4 1 5 9 10 0Percentage 3.33 13.3 3.33 16.66 30.0 33.2 0
Hb levels achieved to maximum levels with in 45 days of treatment.
Table 11: RBC levels before treatment.
RBC levels inmill/cumm
1.6-2.0 2.1-2.5 2.6-3.0 3.1-3.5 3.6-4.0 4.1-4.5 4.5-5.0 5.1-5.5
Male 0 0 0 3 2 0 0 0Female 0 0 4 11 7 3 0 0Total 0 0 4 14 9 3 0 0Percentage 0 0 13.3 46.66 30 10.0 0 0The RBC levels before the study of treatment ranged from 2.7 to 4.2 million/cumm.
7.1-8 8.1-9 9.1-10 10.1-11 11.1-12 12.1-13 Hb levels (gms)109
0
1 1
3
0
1 1
4
1
8
2
8
0
1
2
3
4
5
6
7
8
Males
Females
0
43
11
2
7
0
3
0 00
2
4
6
8
10
12
Male
Female
8.1-9 9.1-10 10.1-11 11.1-12 12.1-13 13.1-14 Hb levels (gms)
2.6-3.0 3.1-3.5 3.6-4.0 4.1-4.5 4.6-5.0RBC levels (millions/cumm)
110

Table 12: RBC levels after 21 days of treatment:RBC levels 3.1-3.5 3.6-4.0 4.1-4.5 4.5-5.0 5.1-5.5 5.6-6.0in mill/cumm
Male 1 1 1 2 0 0
Female 9 10 4 2 0 0
Total 10 11 5 4 0 0
Percentage 33.2 36.7 16.66 13.3 0 0The RBC levels showed gradually increase with in 21 days from the starting day oftreatment.
Table 13: RBC levels after 45 days of treatment:RBC levels 3.1-3.5 3.6-4.0 4.1-4.5 4.5-5.0 5.1-5.5 5.6-6.0in mill/cumm
Male 0 0 2 3 1 0
Female 6 5 3 9 1 0
Total 6 5 5 12 2 0
Percentage 19.98 16.66 16.66 40 66 0RBC levels showed best results after 45 days from starting day of treatment.
0
1
2
3
4
5
6
7
8
9
1 0
3 . 1 - 3 . 5 3 . 6 - 4 . 0 4 . 1 - 4 . 5 4 . 5 - 5 . 0 5 . 1 - 5 . 5
M a l e
F e m a l e
0
1
2
3
4
5
6
7
8
9
3 . 1 - 3 . 5 3 . 6 - 4 . 0 4 . 1 - 4 . 5 4 . 5 - 5 . 0 5 . 1 - 5 . 5
M a l e
F e m a l e
RBC levels (millions/cumm)

RESULTSThe results of the treatment of assessed periodically after 21 and 45 days till the
completion of the duration i.e.45days. the results are tabulated according to the signs
and symptoms, Hemoglobin percentage, RBC levels, percentage of result etc.
The results are assessed and graded as Pravara, Madhyama and Avara according tothe parameters mentioned in materials and methods.
Table No.1: Responsed based on Sex
S.no Sex Pravara Madhyana Avarage1 Male 2 2 02 Female 16 5 43 Children 0 0 1
The present study comprises 13.33% of adult males (4out of 30), 83.33% of
adult females (25 out of 30) and 3.33% (1out of 30) of male children. Out of these
6.7% (2out of 5) among males, 60% (16 out of 25) adult females got best result.
RBC levels (millions/cumm)

Table No.2: Responce based on Age.s.no. Age
(years)Pravara
Male FemaleMadhyama
Male FemaleAvara
Male Female1 0-10 0 0 0 0 1 02 11-20 0 3 0 0 0 03 21-30 1 5 0 2 0 24 31-40 1 6 1 2 0 15 41-50 0 2 1 1 0 1
The present study comprises of different age groups. The youngestbeing 6 years and the oldest has 45 years. Out of these, 31-40 years age got best result,followed by 0-10, 11-20,21-30,31-40 and 41-50 age groups, 2 out 5 adults Male patientsachieved best results followed by 2 madyama and one avara patients. 16 out of 25 adultsfemales got best results, followed by 5 madhyama and 4 avara patients.
2
16
0
2
5
0 0
4
1
0
2
4
6
8
10
12
14
16
MaleFemaleChildren
Pravara Madhyama Avara
112
RESPONSE BASED ON SEX
0 0
1
3
00
6
2 2
7
3
1
2 2
1
0
1
2
3
4
5
6
7
Pravara
Madhyama
Avara
0-10 11-20 21-30 31-40 41-50 RESPONSE BASED ON AGE

Table.3: Response based on Diet.s.no Type
DietPravara
Male FemaleMadhyama
Male FemaleAvara
Male Female1 Vegitarion 0 7 2 1 1 12 mixed 2 11 0 3 0 2
In the present study vegetarians are 40% (12out of 30) and mixed diet are 60%(18out of 30). Out of these 43.3% (13 out of 30) mixed diet got better results than that ofvegetarians 23.3% (7out of 30).
Table No.4: Response based on Economic status
Economic Pravara Madhyama Avara TotalStatus Male Female Male Female Male Female
Poor 1 2 3 10 0 3 15
Middle 1 5 0 3 0 0 9
Rich 0 2 0 0 0 0 2In the present study, the incidence of poor is more than that of middle class and rich
6.66% (2 out of 30) among rich, 60% (9 out of 30) among middle class, and 63.33 (15out of 30) among poor.
Table No. 5: Response based on symptoms/signs
S.No. Symptoms/Signs No.of Improved Partially Notcases improved respond
1 Pandutwam 30 25 4 1
2 Swethanakhata 30 20 5 5
3 Agnimandhya 30 25 5 0
4 Aruchi 23 18 3 3
5 Kaphapraseekam 23 16 2 6
6 Angamardha 23 18 2 3
7
13
3 32 2
0
2
4
6
8
10
12
14
Vegitarion
Mixed
Pravara Madhyama Avara
113RESPONSE BASED ON DIET

7 Brama 10 4 1 5
8 Jwara 15 10 3 2
9 Pindikodwesta 18 12 2 2
10 Tandra 20 14 2 4
11 Alasya 20 15 1 2
12 Gowravam 25 20 2 3
13 Akshikoota sodha 4 6 2 2
14 Krimikosta 4 0 2 2
15 Daha 30 15 10 5
16 Prabhaheena 20 10 4 6
17 Swayatha 5 3 1 1
18 Palpitaion 19 11 2 5
In the present study, pandutwa is an important symptoms that got considerabale
improvement. 25 out of 30 pateints showed best results with complete relief, 4 with
partial improvement and 1 case showed little response towards treatment. Other
important symptoms such as agnimandhya, aruchi, Gowravam, and kaphapraseekam
also showed greater response to the treatment. The list of sign and symptoms before
the treatment and after the treatment is tabulated above.
Table No.6: Hemoglobin levels before treatment
Hb levels Males Females Total Percentage %
Pravara 0 0 0 0
Madhyama 4 9 13 43.33
Avara 1 16 17 56.66
In the present study, the hemoglobin levels ranged from 6 to 11.5 grams/dl
before the treatment. Patients with very poor hemoglobin levels are 56.66% and
patients with average anemia are 43.33%.
0
2
4
6
8
10
12
14
16
P rava ra M adhy am a A vara
M ale
F em a le

Table. 7: Hemoglobin levels after 21 days treatment
Hb levels Males Females Total Percentage
Pravara 2 4 6 20
Madhyama 2 12 14 46.7
Avara 1 9 10 33.3
Hemoglobin levels showed gradually increase with in 21 days from the starting
day of treatment. The poor haemoglobin patients before the treatment decreased from
56.66% to 33.3%.
Table.8: Hemoglobin levels after 45 days of treatment.
Hb levels ingms
Males Females Total Percentage%
Pravara 2 16 18 60.00Madhyama 2 5 7 23.33Avara 1 4 5 16.66
Hemoglobin levels achived to maximum levels with in 45 days of treatment.60% of the
patents (18 out of 30) turned non-anemic, where as 23.33% of the patients (7 out of 30) got
moderate results, and 16.66% of the patients. (5 out of 30) did not respond much to the
treatment.
10
12
14
16

Table No.9: RBC levels before treatment
RBC levels Males Females Total Percentage
Pravara 0 0 0 0
Madhyama 2 11 13 43.33
Avara 3 14 17 56.66
The R.B.C. levels before the starting of treatment ranged from 2.7 to 4.2 mill/cumm.
The Avara group of patients are 56.66% (17 out of 30) and moderate group are
43.33% (13 out of 30).
Pravara Madhyama Avara
0
2
4
6
8
1 0
1 2
1 4
P ra va ra M a d h y a m a A va ra
M a le
F e m a le

Table 10: RBC levels after 21 days of treatment
RBC levels Males Females Total Percentage
Pravara2 2 2 4 13.33
Madhyama 2 15 17 56.66
Avara 1 8 9 30
The R.B.C. levels showed gradually increase with in 21 days from the starging day of
treatment. The Avara group of patients before the treatment decreased from 56.66% to
13.3%.
TABLE NO: 11
RBC levels after 45 days of treatment
RBC levels Males Females Total Percentage
Pravara 3 11 14 46.7
Madhyama 2 9 11 36.6
Avara 0 5 5 16.66
RBC levels showed best results after 45 days from the starting day of treatment. The
Avara group of patients with very low RBC levels before the treatment decreased
from 30% to 16.66%, Madhyama group of patients decreased to 56.66% to 36.6% and
Pravara group of patients increased to 13.33% to 46.7% with the increase in RBC
levels.
10
12

Table No. 13: Final Result After Completion of Result
Results Males Females Total Percentage
Pravana 2 16 18 60.03%
Madhyama 2 5 7 23.33%
Avara 1 4 5 16.66%
After 45 days of treatment, there is significant decrease in the clinical symptoms,
increase in the hemoglobin and RBC levels, decreased in E.S.R. levels and patients
felt comfortable.
4
6
8
10
12
14
16
Male
Female

Responced based on After Completion of Treatment
6.6%
16.6%
Table Showing statistical parameters of Hb% and RBC
S.No. Parameters Mean SD SE t P
1 Hb% 2.6 0.8 0.14 1.8 <0.1
2 RBC 0.9 0.6 0.11 1.3 <0.1
After doing paired 't' test the vaoues obtained are mean for Hb% is 2.6, SD is
0.8, SE is 0.14%, 't' is 1.8 and 'p' is <0/1.
After doing paired 't' test the values obtained are mean for RBC is 29.6, SD is
0.6, SE is 0.11, 't' is 1.3 and 'p' is <0.1.
Male
Pravara
MadhyamaAvara
Female
Pravara
Madhyama
Avara
3.3%
6.6%
6.6%
13.3%
16.6%
53.33%

DISCUSSION
Pandu roga is one of the most common disease described in Ayurveda. The
detailed description about it in all aspect is available in most of the Ayurvedic
classics. It is a highly prevalent disease. Ayurveda offers a number of effective
formulations in the management of pandu roga. The compound drug "Bhaskara lavana
churna" with takra has been selected for the clinical trial to prove its efficacy in
raktalpatha conditions.
Pandu roga being a common ailment in developing countries specially in India,
the prevalence is seen in both sexes and age groups. The females and childrens are
more prone disorder. So the present clinic trial is conducted to find out an effective
treatment for anaemia.

The etiological factors of pandu roga found in Ayurveda can be studied under 4
groups Ahara, Vihara, Manasika, and nidanurthakara Rogas, due to the excessive
intake and practice of above factors.
The disease pandu is manifested due to the predominance of pitta in the
pathogenisis of the disease, though vatadi tridoshas are vitiated in the samprapti. The
consumed food, which has the proparties of kshara, amla, lavana, ati ushna etc, acts as
predisposing and precipitating factors responsible for manifestation of the disease.
These factors cause prakopa of pitta gunas i.e. Sneha, teekshna, ushna, laghu, visra,
sara and drava. The increased dravaguna affects Agni and reduces its teekshnata.
This mandagni cannot digest the food that is consumed. Thus the agnimandhya forms
and which is followed by inadiquate rasadhatu formation, leeds to raktalpatha i.e.
pandu roga.
Pandu roga lakshanas mentioned in Ayurveda are dhatu shaitilyam, raktaalpatha,
etc. Which are the cardinal symptoms of Anaemia. The reduced
hemoglobin and packed cell volume conditions in anaemia of modern science
are comparable with raktalpata condition of pandu roga.
The compound drug i.e. "Bhaskara lavana choornam has been selected. for this
study as it is non contraversial, non-toxic, easily available and economical.
The ingredients present in this preparation; Dadima, pippali, pippali mula,
Dhanyaka, Teja patra, Naga kesara, Amla vetasa, Krishna jeeraka and Swetha Jeera,
Sunti, Twak, Sukshma ela, Samudralavanam, Sauvarchan lavana, Saindhava lavana,
Bida lavanam have properties of Rasayana, Deepana, Pachana, Hridya, Balya,
Tridosha shamaka, Ruchyam, Sodhaharam, Tridosha shamaka. These properties are
considered for their effective management of Pandu roga.

The Dadima, pippali, pappli mula, Dhanyaka, jeeraka, Tejo pathra and Twak
contains the property of krimigna. So are responsible for the elimination of worm
infestation, which is the one of the cause of the pandu roga.
The Balya property of swethajeeraka assists in alleviating the dhatukshya and
ojokshaya, present in Pandu Roga.
The statement "Samanyam Ekatwa karam" mentioned in ayurvedic classics is
justified by asrik prasadana propperty of Dadima, Shunti, Jeeraka in pandu roga.
Takram, which is used as anupana in the clinical trial, is Tridoshashamaka and
agnideepana. It can also prevent dhamani pratichaya because it is srotho sodhaka as
well as vatahara drarvya.
The gradual increase in the Hb levels is observed with in the first weak of
treatment and it reaches the maximum levels in 45 days of duration. This may increase
in Hemoglobin levels is attributed to increased production of intrinsic factors by
Bhaskara lavana churnam. The increased production of intrinsic factor also
contributes to the increased up take of lohamsa in ahara and oushadha. Improvement
in the abhyavaharana as well as and jarana shakti are also observed immediately
with in the first weak of treatment, because this preparation contains Maricha,
Shunti, Jeeraka, Amlavetasa, Nagakesara Twak, Ela and Pippali which has agni
deepana and pachana proparties.
In two pateints, purgation is noticed on the first two days of tretment. This was
thought as adverse effect noticed during the study. It got relieved after adjustment of
the dose in those pateints.
The pale discoloration of the skin, conjuctive, and nail is converted to normalcy,
with gradual increase in Hemoglobin and R.B.C. levels. This was completely
achieved by the end of the treatment.

The increased production of intrinsic factors also contributes to the increased
uptake of lohasma in ahara and oushadha. This is due to direct action of Dadima,
Shunti, Jeeraka on Amasaya, Yakrit and Ranjakapitta.
Significant decrease in E.S.R. levels is noticed in the study. This is due to anti
inflamatery, antiseptic and anodyne properties of Bhaskaralavan churnam.
Thus the reduced rakta in the body is agian replanished by the treatment with
Bhaskara lavana churnam .
The conditions of the patients before and after treatment are assessed based on
the parameters (both subjective and objective). The patients are followed up for 45
days and progress is noted as per systematically prepared special case sheet of pandu.
The results are assessed as Pravara, Avara and and madhyama based on clinical
picture and laboratory investigation.
The prevelence of pandu roga according to present study found more in females
83.33%, (25 out of 30). Than the males 16.66% .
Among these cases (7 out of 25) females were suffering with Desfunctional
uterine bleeding. It leads to Anemia. After the treatment 3 cases had moderate
relief and other 4 cases were mild relief. 1 out of 30 case was seen in pregnacy.
After the treatment she had moderate relief.
In 1 out of 30 cases one male Patient under went truma by bike accident recently.
After the treatment the patient got moderate relief.
In 1 out of 30 cases, the male child have PICA. It was improved after 45 days of
treatment.
56.66% Non-vegetarians got better results than that of vegetarians according to
diet.

Out of 30 cases 31-40 years of group got best results followed by 21-30 11-20,
age 41-50, 0-1 year age groups.
The incidence of poor is more than that of middle class and rich, because
malnutritional diet, irregular food habits. In these leads to anaemia. After the
treatment 63.3% (15 out of 30) among poor, showed better result according to socio-
economical status.
Pandutwa is an important symptom has shown considerable improvement, 70%
patients showed better results with complete regular.
Other important symptoms agnimandya, Swethanakhta; Aruchi, Gowravam,
Kapha prasekam showed greatly responce to the treatment due to action of drugs
Pippali, Mareecha, Shunti, Amlavetasa, Jeeraka, Tejoptra and Talisa patra of
Bhaskaralavana churna having Deepana, Pacchana and Rasayana properties.
Raktalpatha may have also responsed to the treatment due to Dadima. Jeeraka,
and Shunti which contains Iron.
The pathogenesis, Sareera, Drug aspect, Observations and results are discussed
elaborately under respective heading. The results are analysed statistically and
conclusions are drawn.
CONCLUSIONThe conclusions drawn from the present study are listed here under:
1. The patients of poor economical status are more prone than the middle class
and the rich.
2. The patients consuming katu and Amla rasapradhana aharas are more prone
to the disease than those who consume madhura rasa ahara.
3. In pandu roga, vitation of pitta is vriddi, but not ksheena.

4. Females are more prone to this disease than males.
5. Pregnant women are commonly afflicted with the disease.
6. The people residing in urban areas are more prone to the disease than those
residing in suburban and rural areas.
7. People with Arshas, Asrigdara and malaria are more prone to the disease.
8. The drug Bhaskara lavana churna is effective in Pandu, when the vitiated
doshas are mainly vata & Kapha.
9. The age group of 21.30 are more prone to the disease. Followed by 31-40
and 11-20. Reproductive age group in India is between 21 and 30 years in
general. This may be the reason for occurance of the disease. It is also seen
that the age group of 11-20 is also prone to the disease because of their
growing period and less intake of nutritious food is the real cause for
occurance of the disease.
10. The drug Bhaskara lavana choornam is effective in pandu, when the vitiated
doshas are mainly vata and kapha.
11. The drug can be administered with takra in pitta prakriti patients.
12. The symptoms like Dourbalyata, Aruchi, Kasa, Swasa, Shotha, Mandagni,
Ajeerna, Asya vairasyam are relieved with the drug effectively.
13. Hemoglobin and RBC levels gradually increased with oral intake of 2 grms
thrice a day of Bhaskara lavana churna with in a span of 45 days.
14. ESR levels decreased, Hb & RBC levels increased to normal range in
majority of the patients by the end of the treatment, thus proving the
efficiency of the drug.

15. It is necessary to adjust the dosage of the drug and duration of treatment
according to symptoms and signs, prakriti and koshta of the patients.
16. In a patient with history of krimi roga, oral Administration of Bhaskara
Lavanam along made him pass ascaris through faeces. This is a signifcant
finding which also indicated that Bhaskara lavana choornam could be
administered in krimi roga.17. Finally, it can be safety concluded that Bhaskara lavana churna is an effective
and cheap remedy for the most common aliment Pandu. It shoudl be usedroutienly in the management of pandu especially on mass level as it worksout to be economical.
SUMMARY1. INTRODUCTION: The disease is most common in Indian population and in
the both the sexes, especially in pregnant women. It can be compared to the state
of decreased hemoglobin and RBC levels i.e., Anemia of modern system of
medicine. The drug Bhaskara Lavana Choorna is administered to 30 patients,
attended to Out Patient Department of P.G. unit of Kayachikitsa department and
"The clinical Study on the Effect of Bhaskar Lavana Choorna on Panduroga." is
carried out.

2. HISTORICAL ASPECT: The description of the disease is being carried out
since ages. Harima, Halima and Vilohita are the terms used as synonyms for
Purana and Mahabharata. Charaka, Susruta, Vagbhata, Laghutrayee and
subsequent authors of Sangraha Granthas described the disease and chikitsa in
detail. On the other hand, Anemia is derived from Greek words 'an' and 'emia.' It
was previously termed as 'demarbo verginia' by Johnanna Lange in 1554.
3. SHAREERA (Kriya and Rachana): The main doshas involved in the
pathogenesis are Pachaka Pitta, Ranjaka Pitta, Vyana vata, Bhrajaka pitta, and
Kledaka Kapha. The dhatus involved in the pathogenesis are Rasa, Rakta,
Mamsa, Sarakta Medas and Ojus. The organs involved are Yakrit, Pleeha,
Hridaya and Amashaya. Decreased levels of Hemoglobin and RBC is noticed in
Anemia and is related to blood, its contents, Hemopoiesis, and its physiology.
4. THE DISEASE: The disease is classified as Vataja, Pittaja, Kaphaja,
Sannipataja and Mritbhakshana Janya Pandu Roga. Anemias are classified
according to pathology as Microcytic, Macrocytic or Normocytic anemias.
5. NIDANA: The factors that vitiate pitta such as usna, teekshana, amla, lavana,
katu aharas are the causative factors for Pandu Roga. The etiological factors of
anemia are Hemorrhagic, Dyshemopoietic, Hemolytic and Aplastic anemia.
6. POORVA ROOPA: Twak Sphotana, Shteevana, Gatra Saada, Koota Shodha,
Avipaka, Hridaya spandana, Swedabhava, Shrama, Anga Saada, Alpagni and
Shareera Krishatwa are the poorva roopas of Pandu Roga.
7. ROOPA: Alpa Rakta, Dhatu Shaithila, Kopana, Alpa Vak, Hata Anala, Shrama,
Bhrama are some of the important roopas of pandu roga. Rasa vaha Sroto dusti
Lakshanas are also seen in pandu roga. Pallor of cheeks, nails and mucous
membrane, fatigue and lassitude are some of the important clinical features of
Anemia.

8. SAMPRATI: Vitiated Pitta vitiates rasa Dhatu and causes the disease. The
vitiated also pitta affects the rakta dhatu causing Alpa rakta and leads to the
disease. The consumption of Mrit is also the causative factors for Pandu.
9. UPADRAVAS AND ARISHTA LAKSHANAS: Aruchi, Pipasa, Chardi,
Jwara, Shodha are important Upadravas. Shopha, swasa, Trishna etc., are the
Arishta Lakshanas.
10. SADHYASADHYATA: Pandu roga becomes asadhaya when it reaches chronic
state and occurance of Upadravas & Arishta Lakshanas is seen.
11. chikitsa krama: Chikitsa Krama of pandu roga includes the following steps.
1. Nidana Parivarjana
2. Snehana Chikitsa
3. Shodhana Chikitsa: Vamana and Virechana
4. Samana Chikitsa: Herbal, Mineral and Compound preparation
Anupanas like Takra, Madhu, Ksheera and Ghrita etc., are used for
the many preparations.
12. PATHYA APATHYA: Those ahara, aushadha, viharas, which are suitable and
not suitable to the patient and the disease as well are Pathyas and Apathyas
respectively.
13. DRUG ASPECT: The drug Bhaskara Choornam is selected for clinical study
keeping in view the disease, patients, safety, chikitsa sutra and the availability of
the drug.
14. MATERIALS AND METHODS: Patients, parameters, and drugs are the
materials required - parametery include subjective symptoms and objective
signs. The dose of drug 6 gms t.i.d. along with takra after principal meal. The
duration of treatment is 45 days.

15. OBSERVATIONS: The conditions of the patient before the treatment and along
with the course of the treatment for every 21 days is observed and recorded for
period of 45 days in total.
16. RESULTS: The results of the treatment are drawn based on the observations
made. The results are assessed as Pravara, Madhayama, and Avara, as per the
clinical symptoms and laboratory results.
17. DISCUSSION AND CONCLUSION: Pathogenesis, Shareera, Drug aspect,
Observations and Results are discussed elaborately in various angles and
conclusions are drawn based on the same.
DR. B.R.K.R. GOVERNMENT AYRUVEDIC COLLEGE/HOSPITALERRAGADDA, HYDERABAD – 500038
DEPARTMENT OF KAYA CHIKITSA – P.G. UNITSPECIAL CASE SHEETON PANDU ROGA
Name of the Patient: Regd No:Age: Sex: Married/Unmarried: Occupation:Social /Financial status:
Address:
ROGA PAREEKSHA

1. CHIEF COMPLAINTS WITH DURATION:
2. ASSOCIATED SYMTOMS:
3. HISTORY OF PRESENT COMPLAINT:
4. HISTORY OF PREVIOUS ILLNESS: Vishama Jwara / Asrigdara / Arshas/Atisara/ Arbuda/ Krimi/ Allopathic drugs/ Shastra Karma
5. FAMILY HISTORY: Suffers of Pandu – Mother/Father/ Grand parents/Others
6. PERSONAL HISTORY:a) Diet: Shakahara / mamshahara:
b) Habits: Madyapana/Dhoomapana/ Tea/ Tobacco:
c) Appetite: d) Sleep: e) Urine:
f) Bowels: g) Menstruval history:
II. PHYSICAL EXAMINATIONa) Height: b) Weight:c) Build: d) Tongue:e) Nails: f) Skin:g) Palms of hands: h) Conjunctive:i) Mucous membrane: j) Oedema:j)
III. CLINICAL EXAMINATION:
a) BP: b) PR:
c) Respiratory rate: d) Heart:
e) Lungs: f) Liver
g) Spleen: h) Temperature
ROGI PAREEKSHA:1. SHADVIDHA PAREEKSHA
1) Prakriti: Vata/Pitta/kapha2) Vikriti: Dosha – vata / pitta / kapha
Dooshya – Rasa / Rakta / mamsa / medo/Asthi/majja/sukra3) Sara: Pravara / Madhyama / Avara4) Satwa: Pravara / Madhyama / Avara5) Samhanana: Susamhana / Madhyama / Asamhana6) Pramana: Pravara / Madhayama / Avara7) Satmya: Pravara / Madhyama / Avara8) Aharashakti: Abhyavaharana shakti – Pravara / Madhyama / Avara
Jarana – Pravara / Madhyama / AvaraJatharagni – Pravara / Madhyama / Avara

9) Vayah: Bala/ Yavana / Sampoornatha / Parihari / Vriddha.10) Vyoyama shakti: Pravara / Madhyama / Avara
Desha – Jangala / Anupa / SadharanaKala – Seetha / Ushna/ Varsha
2. ASHTASTHANA PAREEKSHA:1. Nadi: Vata/ Pitta/ Kapha/ Dwandaja / Sannipataja. Sankhya - /min.
Gati – kshipra / manda
2. Mala: Varna – Peelha / swetha / Prakrita
Sama / Nirama / Vibandha.
Pravritti: Adika / Prakrita/ Alpa
3. Mootra: Varna – Peeta / Swetha / Prakrita
Pravritti – Adhika / Prakriti / Alpa
Pramana – Adhika / Prakrita / Alpa
4. Jihwa: Amayukta/ Niramayukta
5. Twak: Varnam – Pandu / Peeta / Rakta / Ruksha / Snigda
6. Shabda: Karnaksweda / Shabda asahana / Prakrita
7. Drik: Harswa drishti / Deerga drishti
Netravarnam – Swetha / Peeta / Atipeeta / Ruksha / Snigda
8. Akriti: Ksheena / Sthoola / Madhyama
Sodha – Mukha / Hasta / Pada
SROTHAS INVOLVEDPrana/ Anna/ Udaka/ Rasa/ Rakta/ Mamsa/ Medas/ Asthi/ Majja/ Sukra/ Mootra/ Purisha/Sweda/ Cheshta/ Samgna/ Manovaha/ Arthavavaha
LAKSHNAS OF PANDU ROGAVataja pandu Pittaja Pandu Kaphaja panud Mridbhakshana
panduLakshnas B A Lakshanas B A Lakshanas B A Lakshnas B Aa)Rukshatwa(paleness &Dryness)Twak MutraNetra NakhaJihwa
b) Toda(PrikingSenstion)
a) Peethatwam(yellowishness)MalaMutraNakhaJihwaTwak
d) Daha(burningsensation)
a) Suklatwam(Whiteness)TwakMutraJihwaNakhaNetra
b) Swayathu(Swelling)
a) Sotha(Swelling)AkshikutaBruMedraGudaYoni
b) Rakta,Kaphamisrita,

c)Kampa(Tremours)
d) Anaha(Distension)
e) Branma(giddiness)
f) Swasa(Shortnessof breath)
g) Dourbalya(debility)
c) trishna(Thirsty)
d) Jwara(Fever)
e) Bhinnavit/Atisara
c) Tandra(Drousiness)
d) Alasya(Slugishness)
e) Atigourava(Heavyness)
f) Aruchi(Dysphasia)
Vamana(Diarrhoea)
Nutritional Infection Endocrine Drugs
Worm infestion Bleeding disorders Genetic disorders
S.No. Ist day 21st day 45th day
1 CBP: Hb%
RBC
2 ESR
3 Stool examination
4 Urinary analysis
5 Ultra sound abdomen
6 Chest X-ray
7 Others
VYADHI VINISCHAYA:
TREATMENT UNDERTAKEN
a) Drug prescribedb) Dosage schedulec) Duration of treatment given
FINAL CONCLUSION
a) Cure in percentageb) Response to treatmentc) Special not if any

RESULT
a) Pravarab) Madhyamac) Avara
Sign. Of the Co-guide Sign. Of the Guide Sign. Of the PG.Scholar
INFORMED CONSENT
I, ................................... Son/ daughter / wife of ................................. am
exercising my free will to participate in above study as a subject. I have been informed
to my satisfaction by the attending physician the purpose of clinical evaluatin and the
nature of the drug-treatment. I am also aware of my right to opt out of the treatment
schedule at any time during the course of the treatment.
Schedule initiation Patient Signature
BIBLIOGRAPHYS.No. Name of the Book Author's Name Publication
1. Amarakosha Amara simha Choukambha Sanskrit
2 A.P.I. Textbook Hon. Brig. K.K. Association of Physicians
of medicine,II Vol Datey S.E.M. of India, Bombay, 1979
3 Astanga Hridaya V. Ramaswamy Telugu, Academy,
Hyderabad 1979

4 Astanga Sangraha V. Rangacharyulu Vavilla press, Madras
1954
5 Astanga Sangraha Puryanchlok Sri Swati enterprises,
Pandit Lalchandra Nagpur,
6 A Text Book of William Byoid 9th Edition, 1990
Pathology
7 A Text Book of N. Murgesh Satya Publishers,
Pharmacology Madhurai, 4th Edition 1997
8 Basavarajeeyam P. Satyanarayana Konda Sankaraiah Book
Rao Depot, Secunderabad
9 Bhaishajya Ambika Datta Choukambha Sanskrit
Ratnavali Sastry Samsthan, Varanasi, 1981
10. Bhava prakasha Mukkamala Sri Panduranga printing
Venkata Sastry works, Vijayawada,
2nd Edition, 1959
11. Bhava prakasha Dr. Krishnachandra Choukamba Sanskrit
Nighantu Chunekar Samsthan, Varanasi
5th Edition, 1959
12 Bhela Samhita S.V.S. Shastry CCRIM & H,
C.R.R. Sharma New Delhi, 1977
13 Chakradatta Sri Jagadeshwar Choukamba Sanskrit
Prasada Tirupathi Samsthan, Varanasi
14 Charaka Samhita Sripada Krishna Sunrise printers, Rajah-
Moorthy Shastry mundry, 4th Edition, 1989
15 Charaka Samhita Agnivesha V. Ramaswamy & Sons,
Madras
16 Clinical Medicine Praveen Kumar ELBS with Balliere,
Michael Clark Tindall, 3rd Edition, 1994
17 Clinical Methods Michael Swash ELBS series, Govt. of UK
18 Clinical Hematology Wintrobb M.M. 5th Edition
19 Clinical Methods Prof. K.R. Srikanta Choukamba Orientalia,
in Ayurveda Moorthy Varanasi, 1st Edition 1983

20 Current Medical Steven A. Schroeds Lange Medical Books,
Diagnosis and USA
Treatment
21 Digestion and C. Dwarakanath Baidyanath Ayurved
Metabolism Bhavan Pvt. Ltd. Calcutta
1st Edition
22 Dravvyaguna K. Nishteshwar AP Ayur. Literature
Improvement trust,
Hyderabad
23 Effect of Hormones Cannady 1962
in anaemia
24 Essentials of Medical K.D. Tripathi Japee Brothers Medical
Pharmacology publishers, PVT Ltd.,
New, Delhi, 1999
25. Haritha Samhita Khemaraj Sri Sri Vangeshwara
Krishnadas Mudranalaya, 1984
26. How to examine a Dr. Menino de Varghese Publishing
Patient Souza House, Bombay 1982,
5th Edition
27 Human Physiology C.C. Chaterjee Medical allied agency,
Culcutta, 11th Edition,1988
28 Human Physiology Chakrabarthi The New Book Stall,
H.N. Ghosh Calcutta
29 Human Physiology Arthur C. Guyton Prism Books Pvt. Ltd.
John E. Hall 9th Edition, 1996
30 Immunological Capplan 1963
Studies in Anemia
31 Indian Medicinal KR. Kirtikar Jayyed Press, Delhi
Plants B.D. Basu 2nd Edition, 1975
32 Indian Medicinal Orient Longman Ayurvaidhyasala,
Plants Kottakal
33 Introduction to C.Dwarakanath Choukamba Orientalia,

Kayachikitsa Varanasi, 2nd
Ediction1986
34 Kashyapa samhita Pandit Hemaraj Choukamba Sanskrit
series, Varanasi
35 Madhava Nidana M.Vishweshwar Nirnaya sagar Press,
Bombay, 1958
36 Medicine for Dr. K. Choudary Jaypee Brothers Medical
Students and Practitioners Publishers, New Delhi
1990
37 Nighantu Adarsha Bapalal G.Vaidya Choukamba Bharati
Academy, Varanasi
38 Pharmacology R.S.Satoskar & Popular Prakashan Pvt.
Bhandarkar Ltd. Bombay
39 Principles & Practic Davidson 1962
of Medicine
40 Principles of Anatomy Gerard J. Harper & Row
Tortora publications,
New york, 1984
41 Principles of Harrison 12th Edition, 1991
of Internal Medicine
42. Shabdarnavam - -
43. Shabda Raja Radhakant Vyaptistamisana Press,
Kalpadruvam Dev Bahadur Culcutta, 1808
44. Shabda ratnavali - -
45. Shabdasthoma Sri taranath Veedanyantra PRess,
Mahanidhi Takravachaspathi Calcutta, 1976
46. Sarangadhara Sarangadhara V. Ramaswami Sastrulu
Samhita Mishra & Sons, Vavilla Press,
Madras, 1952.
47. Susruta Samhita V. Ramaswami Vavilla press, Madras

Shastrulu 1954
48 Susruta Samhita Ambikadatta Choukambha Samsthan,
Sastry Varanasi, 4th Edition 1979
49 The Indian Materia Dr. K.M. Nadkarni Popular Book Depot,
Medica Bombay.
50 The Iron Deficiency Gibbson 1963
& Pernicious Anaemia
51. The Wealth of CSIR, New Delhi, 1969
India, Vol, III, VIII & IX
52. Vaidhya Chintamani Indrakanti Venkateshwara Book
Vallabhacharyulu Depot. Sec'bad. 1955
53. Vangasena Hearaja Sri Sri Venkateshwara
Krishnadasa Mudranalaya, Bombay
Shreshti 1876.
54. Yoga Ratnakara-I Yeturu Nellore, 1939.
Srinivasacharyulu

Formation and destruction of red blood cells,And the recycling of hemoglobin components.

INGREDIENTS OF BASKARA LAVANA CHURNAM
SOWVARCHA LAVANAM SAMUDRA LAVANAM
SAINDHAVA LAVANAM
BIDA LAVANAM


BHASKARA LAVANA CHURNAM
TAKRAM

RED BLOOD CELL