Aortic Root Pseudoaneurysm Following Surgery for Aortic Valve ...
OUTCOME OF AORTIC VALVE REPAIR FOR AORTIC...
Transcript of OUTCOME OF AORTIC VALVE REPAIR FOR AORTIC...

i
OUTCOME OF AORTIC VALVE REPAIR FOR AORTIC
REGURGITATION COMPLICATING VENTRICULAR
SEPTAL DEFECT – A RETROSPECTIVE OBSERVATIONAL
STUDY
Thesis submitted for the partial fulfilment for the
requirement of the
Degree of MCH (Cardiovascular and thoracic Surgery)
BY
DR. S.P.MAHENDRANATH
MCH CARDIOVASCULAR AND THORACIC SURGERY RESIDENT
2015-2017
DEPARTMENT OF CARDIOVASCULAR AND THORACIC
SURGERY
SREE CHITRA TIRUNAL INSTITUTE FOR MEDICAL
SCIENCES AND TECHNOLOGY, TRIVANDRUM
KERALA, INDIA - 695011

ii
DECLARATION
I hereby declare that this thesis entitled “OUTCOME OF
AORTIC VALVE REPAIR FOR AORTIC REGURGITATION
COMPLICATING VENTRICULAR SEPTAL DEFECT– A
RETROSPECTIVE OBSERVATIONAL STUDY” has been
prepared by me under the capable guidance of Dr.Baiju S
Dharan, Professor, Department of Cardiothoracic and
Vascular Surgery, Dr.Sabarinath Menon, Associate
Professor, Department of Cardiothoracic and Vascular
Surgery, Dr. K. Jayakumar, Senior Professor, Head of the
department of Cardiothoracic and Vascular Surgery, at Sree
Chitra Tirunal Institute for Medical Sciences & Technology,
Thiruvananthapuram.
DR. S.P. MAHENDRANATH
MCH Cardiovascular &
Thoracic Surgery Resident
Department of Cardiovascular
& Thoracic Surgery
Place : Thiruvananthapuram
Date :

iii
CERTIFICATE This is to certify that the thesis entitled “OUTCOME OF AORTIC
VALVE REPAIR FOR AORTIC REGURGITATION
COMPLICATING VENTRICULAR SEPTAL DEFECT–A
RETROSPECTIVE OBSERVATIONAL STUDY” for the degree of
MCH(CARDIOVASCULAR AND THORACIC SURGERY) has been
carried out by Dr. S.P.MAHENDRANATH under our direct
supervision and guidance.
The work done in connection with this dissertation has been
carried out by the
candidate himself and is genuine.
GUIDE:
Dr. BAIJU S DHARAN
Professor
Department of Cardiovascular and
Thoracic Surgery,
SCTIMST, Thiruvananthapuram, India
CO-GUIDE: CO-GUIDE:
Dr. SABARINATH MENON Dr. K. JAYAKUMAR
Associate Professor Senior Professor and Head
Department of Cardiovascular Department of Cardiovascular
and Thoracic Surgery and Thoracic surgery.
SCTIMST, Thiruvananthapuram, India SCTIMST
Thiruvananthapuram, India

iv
SREE CHITRA TIRUNAL INSTITUTE FOR MEDICAL
SCIENCES
AND TECHNOLOGY
Thiruvananthapuram, India
CERTIFICATE
This is to certify that this thesis entitled “OUTCOME OF
AORTIC VALVE REPAIR FOR AORTIC REGURGITATION
COMPLICATING VENTRICULAR SEPTAL DEFECT – A
RETROSPECTIVE OBSERVATIONAL STUDY” has been prepared by
Dr. S.P. MAHENDRANATH, MCH Cardiovascular and thoracic
surgery Resident, Division of Cardiovascular and thoracic Surgery
at Sree Chitra Tirunal Institute for Medical Sciences & Technology,
Thiruvananthapuram. He has shown keen interest in preparing
this project.
Dr. K JAYAKUMAR
Senior Professor, Head of the department
Department of Cardiovascular
and Thoracic Surgery
SCTIMST, Thiruvananthapuram
Place: Thiruvananthapuram Date:

v
ACKNOWLEDGEMENT
I take this opportunity to express my deep sense of gratitude and
thanks to all those who have been instrumental in the successful
completion of this work. I am deeply indebted to my esteemed teacher
and guide, Dr.Baiju S Dharan, Professor, Department of Cardiothoracic
and Vascular Surgery, Sree Chitra Tirunal Institute for Medical Sciences
and Technology for her unremitting encouragement, avid support and
invaluable guidance throughout the course of my study.
I would also like to express my deep gratitude and regards to my co-
guide, Dr.Sabarinath Menon,, Department of Cardiothoracic and
Vascular Surgery at, Sree Chitra Tirunal Institute for Medical Sciences
and Technology. Without his guidance, support and personal
involvement, the work could never have been completed.
I express my sincere thanks to my co-guide Dr.K.Jayakumar for his
constant support and guide throughout the conduct of study.
All my teachers Dr. Vivek Pillai, Dr Vargheese T Panicker, Dr.Bineesh R,
Dr.Sudip Dutta Buruah and Dr.Sowmia Ramanan, have been extremely
helpful during the conduct of the study and have given their invaluable
opinion and constructive criticism.
My sincere thanks to my fellow residents, Dr.Abid Iqbal, Dr.Debabrata
Gohain, Dr.Nikhil. P.K and Dr.Prakash Goura for their help throughout
the study period.
I would like to take this opportunity to show my gratitude to all my
patients who volunteered to be part of this study.
DR. MAHENDRANATH S P

vi
CONTENTS
SL.NO TOPIC PAGE
NUMBER
1 INTRODUCTION 1
2 AIM AND OBJECTIVE 3
3 REVIEW OF LITERATURE 4
4 MATERIALS AND METHODS 21
5 RESULTS 26
6 TABLES AND CHARTS 35
7 DISCUSSION 43
8 CONCLUSION 50
9 BIBLIOGRAPHY 51
10 ABBREVIATIONS
11 APPENDICES
DATA COLLECTION FORM
IEC APPROVAL FORM
MASTER CHART
PLAGIARISM CHECK FORM

1
INTRODUCTION
Aortic regurgitation (AR) in patients with ventricular septal
defect (VSD) occurs in those anatomical types that are located close
to or in direct contact with the aortic valve1. This subset of patients
form a relatively rare group of patients with an incidence ranging
between 5% and 10%.Perimembranous and doubly committed juxta-
arterial defects are the commonly affected types. Rarely, it can occur
in outlet muscular VSD also2.
Prolapse of the valvular cusps caused by the venturi effect of the
ventricular septal defect jet, abnormal commissural suspension, lack
of appositional forces and lack of continuity between the aortic
media, annulus of aortic valve and the ventricular septum have been
the commonly proposed pathological anatomic mechanisms of
regurgitation3. The right coronary cusp (RCC) is the usually involved
cusp. This is followed in line by the non-coronary cusp whereas, the
involvement of the left coronary cusp is very rare. The prolapsing
cusps render the valve incompetent and cause significant damage to
the valve cusp and annulus.The prolapsing AV may completely close
the VSD so that the shunt may disappear but leaving behind the
regurgitation to progress3.

2
Surgical closure of the defect with aortic valve repair is
indicated for these patients irrespective of the grade of preoperative
aortic regurgitation and it is recommended to close the defect at the
earliest4. The technique of valve repair is decided based on the
mechanism(s) of regurgitation5
Despite increasing interest in pediatric aortic valve repair aortic
valve replacement is unavoidable in certain circumstances. With
limited options for valve replacement and lack of prospective studies,
the superiority of one prosthesis over the other cannot be
ascertained6. Metaanalysis has shown that all the currently available
valve substitutes are associated with suboptimal outcome in
children6. Hence a durable aortic valve repair is the need of the hour.
This study aims to evaluate the outcome of patients who
underwent aortic valve repair procedures for aortic regurgitation
complicating VSD and to also to assess the predictors for their
outcomes after surgery.

3
AIM AND OBJECTIVE: 1. To identify the demographic parameters affecting a durable
valve repair
2. To assess the effect of preoperative disease severity on disease
recurrence
3. To compare the outcomes of various surgical techniques of
aortic valve repair for AR complicating VSD on short term
follow up

4
REVIEW OF LITERATURE
EPIDEMEOLOGY
Ventricular septal defect accounts for 25 % of the acyanotic
congenital heart disease7. The true incidence of ventricular septal
defect in the general population is unpredictable because most of
them close spontaneously in utero. The incidence ranges from 5
to 50 per 1000 live births and 0.3 per 1000 adults8.
Among the patients with VSD the incidence of aortic cusp
prolapse may range between 4% and 9 % and the incidence of AR is 2-
6 %9 . The reported incidence of cusp prolapse in subarterial VSD is
40 % and in perimembranous VSD is 12 %10 . The incidence of AR is
related to the age . It is rarely present at birth but usually develops
after 2 years of age and progresses over the second decade to severe
AR
MORPHOLOGY
THE INTERVENTRICULAR SEPTUM
The morphology of right ventricle in patients with normal
atrioventricular connection is usually divided into three segments
using a tripartite approach. It includes the inlet, apical (trabecular)
and outlet components. The inlet (atrioventricular) septum is located
immediately beneath the septal leaflet of tricuspid valve. The

5
membranous septum is located immediately beneath the anteroseptal
commissure. It is divided into the atrioventricular part between the
left ventricle and the right atrium and the interventicular part located
between the right and the left ventricles. This division of the
membranous septum is anatomically by the hinge of attachment of
the tricuspid valve. The conal or the outlet septum is located just
beneath the inter leaflet triangle between the RCC and the NCC. It is
wedged between the left anterosuperior and right posteroinferior limbs
of the trabecula septomarginalis (TSM)from below.
PERIMEMBRANOUS VSD
Perimembranous VSDs are the most common type of VSD
accounting for approximately 80% of patients operated on for primary
VSD11. These defects are also called junctional VSDs as they are
located in the junctional area between the trabecular and outlet
(conal) portions of the ventricular septum and between the posterior
and anterior divisions of the trabecula septomarginalis (septal band).
Perimembranous VSDs can be juxtatricuspid (abutting the
tricuspid valve), juxtamitral and juxta-aortic12. These
perimembranous VSDs are conoventricular in nature and they about
the commissural area between the noncoronary and right coronary
cusps of the aortic valve whereas the other VSDs are only
juxtatricuspid. In hearts with these as well as in hearts with

6
perimembranous VSDs, the bundle of His passes along the
posteroinferior border of the defect.
OUTLET SEPTAL VSD (DOUBLY COMMITTED SUBARTERIAL VSD)
The defect within the outlet portion of the RV account
for approximately 5% to 10% of patients treated operatively for
VSD. VSDs in this location are also in the outlet portion of the LV. In
contrast to perimembranous VSDs, they are more beneath the right
aortic cusp than the commissure between it and the noncoronary
cusp.
VSDs in this area are bordered by a space over which lie the
pulmonary and aortic valve13. VSDs of this type are more common in
Asians than in white or black races14. Subarterial VSDs may be
circular, diamond shaped, or oval with the long axis lying
transversely. When viewed from the LV aspect, these defects are in the
outflow portion of the ventricular septum beneath the right coronary
cusp (or commissure between it and the left cusp). The aortic and
pulmonary valve cusps are separated by only a thin rim of fibrous
tissue. The right aortic cusp and (less often) noncoronary cusp may
prolapse into the upper margin of the defect, with or without aortic
regurgitation.
The postero inferior margin of RV outlet VSDs are well
separated from the tricuspid valve annulus by a band of muscle. As a

7
result, they are well above the bundle of His and the conduction
system is related to such a VSD as it is with the other
perimembranous defects. Outlet VSD may sometimes be associated
with severe overriding of the aorta, and it is then termed double outlet
right ventricle (DORV) with doubly committed VSD. The same type of
VSD may also be seen in double outlet left ventricle (DOLV), in which
the pulmonary artery severely overrides the VSD.
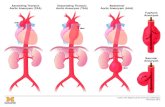
PATHOPHYSIOLOGY OF AR- THE VENTURI EFFECT
Prolapse may result in part from lack of support of the aortic
sinus of Valsalva and “anulus” by the infundibular septum15,
although because most large perimembranous defects are closely
adjacent to the aortic “anulus” and very few have associated
regurgitation, this cannot be the entire explanation.A structural defect
in the base of the sinus may also play a role when the VSD is small.
Loss of continuity of the aortic media from the aortic “anulus” and the
ventricular septum has also been proposed as a mechanism.
Hemodynamic influences can also aggravate the tendencies
towards AR. Such influences are more marked once AR develops,
resulting in progressive prolapse and distortion. The most widely
accepted mechanism of cusp prolapse is the Venturi effect17. It
describes the changes in velocity and pressure that occur when fluid
passes through conduits of varying diameter. When the conduit caliber

8
decreases, fluid velocity increases and pressure decreases. Thus, when
there is restriction to flow through a VSD and an aortic valve cusp is
adjacent to the defect, it is vulnerable to being drawn into the high-
velocity, low-pressure jet as blood shunts from the left to right
through the restrictive VSD. This displaces the unsupported “anulus”
outward and downward into the RV.
During late systole, the aortic cusp prolapses into the VSD and
is thus acted upon by direct pressure from the cavity of the LV,
displacing both “anulus” and cusp into the RV. During diastole, the
high pressure in the aortic root distends the dilated sinus, with
further displacement of the aortic “anulus” toward the RV. As a result
the sinus dilates, the distending force becomes greater from increase
in wall tension.
Evidences supporting the Venturi effect as the predominant
cause of aortic cusp prolapse and subsequent AR include:
The Venturi effect requires a restrictive VSD. Previous studies
in the era of near-routine cardiac catheterization indicate that
most of the defects are restrictive with near normal pulmonary
pressure.
A minimum shunt with a Qp/Qs ratio of 1.4 is required to
induce sufficient cusp distorsion and aortic valve prolapse

9
Aortic regurgitation complicating VSD is an acquired lesion. AR
or prolapse with VSD is not present at birth and is diagnosed
after infancy
The nadir of the affected leaflet would be expected to lie within
the stream of the shunt. This is consistent with observations
that overriding of the involved cusp is commonly noted. The
override of the aortic cusp in perimembranous VSDs has been
identified as a risk factor for developing cusp prolapse and
subsequent AR.
ANATOMICAL CLASSIFICATION OF VSD - AR SYNDROME
Kawashima et al, proposed the following classification for aortic
incompetence (AI) complicating VSD in 197318. The classification was
according to the location of the VSD, the anatomic type of the right
ventricular outflow tract, and the severity of the aortic cusp herniation
Type I: Supracristal VSD and AI (60%)
o Type IA: Without aortic cusp herniation
o Type IB: Aortic cusp herniation and conal muscular
rim beneath the pulmonic valve
o Type IC: Aortic cusp herniation without a conal
muscular rim beneath the pulmonic valve.

10
Type II: Infracristal VSD and AI (20%)
o Type II A: Aortic cusp herniation and conal muscular
rim beneath the pulmonic valve
o Type II B: Aortic cusp herniation without a conal
muscular rim beneath the pulmonic valve
Type III: Infracristal VSD and AI with infundibular pulmonic
stenosis (PS) (14%)
Type IV: Supracristal VSD and AI with infundibular
pulmonic stenosis PS (6%)
In type IA defect, the cause of AI was not related to the existence
of the VSD. A bicuspid aortic valve or abnormal shortening of a
coronary cusp may be the etiology.
In type IB, there was a thin rim of conal musculature beneath
the pulmonic valve when seen from the right side through right
ventriculotomy. Herniation of the aortic cusp is usually mild or
moderate in this type. No significant pressure gradient was
detected across the right ventricular outflow. The herniated
cusp appeared to be the right coronary cusp (RCC) in most
cases.
In type IC, there is no conal muscular rim beneath the pulmonic
valve and therefore, the aortic and pulmonic valves were in
direct apposition. The RCC herniates into the defect and the
degree of cusp herniation is moderate or severe. A systolic

11
pressure gradient of 25 mmHg or more may be present at the
right ventricular outflow tract due to the obstruction resulting
from herniation of the aortic cusp. Presence of deformed cusps
may be associated with this type of defects.
The AI in type IIA is not directly related to the existence of a
VSD as it is in type IA.
CLINICAL EXAMINATION
Alexander S Nadas, M.D., Otto G.et al19 had proposed that a
patient with aortic regurgitation complicating VSD can have the
following auscultatory findings
A systolic murmur, usually grade IV (scale of VI) or louder heard
at the left sternal border. The maximal intensity will be at the
lower left sternal border, where assumes the quality of a
murmur of ventricular septal defect.
In many instances this systolic murmur may be transmitted
very well to the pulmonary area, where it assumes a stenotic
character.
A protodiastolic murmur of aortic regurgitation will be present,
by definition, in every case, although in many instances and
this would not be heard until some years after the discovery of
the systolic murmur.

12
In contrast to the loud systolic murmur, the aortic blow was
usually of grade-III intensity, or less, and seldom lasted
throughout diastole.
A continuous murmur with maximal intensity just before the
second heart sound as heard in patients with a patent ductus
arteriosus may be observed.
The systolic murmur was loudest in mid-systole, decreased
toward the second sound, and was then followed with increased
intensity by the protodiastolic murmur. Thus, there appeared to
be a hiatus between systolic and protodiastolic murmur,
resulting in a to-and-fro character.
A mid-diastolic rumble, resembling an Austin Flint murmur,
probably caused by increased mitral valve flow, will be heard in
some patients.
The heart sounds will be difficult to judge because of the
murmurs accompany most of the cardiac cycle.
An ejection click may be heard at the apex.
A systolic thrill may be present at the mid lower left sternal
border.
The cardiac impulse is usually hyperkinetic and involved
principally, but not exclusively, the left ventricle.
Left chest prominence was noted frequently, particularly in the
older children with marked aortic regurgitation. At the time of
catheterization, when the auscultatory evidence of aortic

13
regurgitation was usually clear-cut, a wide pulse pressure was a
common finding.
Hounding carotid pulses with a low dicrotic notch and a pistol-
shot sound may heard over the femoral artery in patients with
significant aortic run off.
RADIOLOGICAL FINDINGS
shows cardiac enlargement. While the left ventricle is almost
uniformly dilated, additional right ventricular enlargement may be
present. The pulmonary vessels are within normal limits or only
mildly engorged. This absence of marked pulmonary vascular
engorgement was helpful in differentiating ventricular septal defect
with aortic regurgitation from patent ductus arteriosus.
ELECTROCARDIOGRAM FINDINGS
The chest leads of the electrocardiogram shows left ventricular
preponderance with left ventricular hypertrophy. Left ventricular
hypertrophy with ST and T-wave changes may be present.
Biventricular hypertrophy may be an associated finding in some
patients. The, frontal plane mean QRS axis, in the majority, is
between +30 and +90°. In an occasional patient, incomplete right
bundle-branch block or first degree atrioventricular block may be
observed.

14
ECHOCARDIOGRAPHIC EVALUVATION OF AORTIC
REGURGITATION20
A systemic evaluation of aortic regurgitation includes the following
steps:
Confirm diagnosis
Quantify the degree of AR
Define mechanism of AR
Define etiology of AR
Evaluate LV response to p/v overload
Identify associated abnormalities
ESTABLISHING THE DIAGNOSIS
The prolapsed aortic cusp is almost always the right coronary
cusp (RCC) and prolapse is diagnosed when there was a distinct
projection of any part of the RCC from the natural curve of the sinus
of Valsalva. In the long axis view of the aortic valve, we measured the
length of the prolapse of the RCC into the VSD at end-systole.
QUANTIFYING THE DEGREE OF AR
Severity of AR18 was graded according to the level to which the narrow
jet reached as follows:
GRADE 1(trivial): Jet reaches just beneath the aortic valve
GRADE 2(slight): Jet is confined to the left ventricular outflow tract
GRADE 3 (moderate): Jet reaches the mid portion of the left ventricle
GRADE 4(severe): Jet reaches the left ventricular apex.

15
MECHANISM OF AORTIC REGURGITATION
El khoury et al20 had proposed a classification, based on the
mechanism of aortic regurgitation in 2000. According to them the
functional aortic root was divided into two components, namely
ventriculo aortic junction (VAJ) and the sinotubular junction (STJ).
TYPE I: Normal valve cusps mobility
TYPE IA: Dilation of the sinotubular junction and ascending
aorta
TYPE IB: Dilation of aortic sinuses, sinotubular junction and
ascending aorta
TYPE IC: Dilation of ventriculoaortic junction, aortic
sinuses, sinotubular junction and ascending aorta
TYPE ID: cusp perforation
TYPE II: Increased valve movement
TYPE III: Restrictive valve movement
The type of aortic regurgitation can be made out based on the
nature of the regurgitant jet
Central jet: TYPE IA, TYPE IB, TYPE IC
Paracentral jet: TYPE ID
Eccentric jet:
Away from the prolapsing cusp – TYPE II
Towards the more restricted cusp –TYPE II
The reference value for aortic root dilation on TEE long axis-view are:
Annulus (≥1.6 cm/m²)
Sinus (≥2.1 cm/m²)

16
ST junction (≥1.9 cm/m²)
Predictors of a durable repair according to Kindermann et al20:
Absence of more than mild residual AR
Effective height ≥ 9 mm
Coaptation length ≥ 4 mm
SEVERITY OF CUSP PROLAPSE21
RCC deformity index (RCCD) is obtained by dividing the
prolapse length by the ring diameter of the aortic valve. On the short-
axis view of the aortic valve, we measured the length between each
commissure at end-diastole just before valve opening.
RCC imbalance index (R/L) is calculated as the length
between the commissure of the right and left coronary cusps and that
of the right and non-coronary cusps divided by the length between the
commissure of the right and left coronary cusps and that of the left
and non-coronary cusps
SURGICAL TECHNIQUES FOR AORTIC VALVE REPAIR
TRUSLER PROCEDURE22
One or more leaflets can be repaired by the Trusler method of
plication. This procedure is carried out at the commissure adjacent to
the prolapsed cusp (usually the right or noncoronary cusp). A 5-0 or
6-0 polypropylene suture is placed through the fibrous lacunae at the

17
midpoint of each cusp. Cusps can then be assessed for elongation and
attenuation. Cusp plication is performed at the elongated free edges of
the aortic valve cusps. A 5-0 or 6-0 PTFE suture is woven between the
right and noncoronary cusps to adjust the excessive length of the
prolapsed cusp to the adjacent aortic wall. Repair may be reinforced
by pledgets (pericardial or felt) or a small cap of polyester secured as a
pledget over both affected cusps adjacent to the commissure. Hisatomi
and colleagues proposed pledget stitch aortoplasty to make the aortic
cusps protrude for even greater aortic cusp coaptation29. The stitch at
the center of the valve is removed after VSD repair. Approach to the
VSD is appropriate to the location of the defect and may be transaortic
if the defect is accessible. Any infundibular stenosis is relieved by
excising trabecular muscle bands between the infundibular septum
and free wall of the RV and, when necessary, by mobilizing and
excising parietal and septal extensions of the infundibular septum
and portions of the moderator bands.
An entirely different technique has been successfully used by
Carpentier, Chauvaud and colleagues. Its basic feature is triangular
excision and reconstruction of the prolapsing cusp. Combined with
this is an anuloplasty of the left ventriculo aortic junction. They also
recommend that the VSD be repaired through the aortic root, using a
glutaraldehyde treated pericardial patch.

18
2. YACOUB PROCEDURE23
Yacoub and colleagues have proposed another alternative repair
that addresses the basic morphologic defect more completely. All
anatomic components of defect are corrected by a simple transaortic
repair. A transverse aortotomy is made. Extent of dilatation of the
right coronary sinus and exact definition of the thin area of sinus
resulting from discontinuity between aortic valve “anulus” and media
of aorta are accurately defined. A series of pledget-reinforced mattress
sutures are placed through the crest of the ventricular septum slightly
on the RV side to avoid injuring the conduction system. Sutures are
passed through the “anulus” of the aortic valve and then used to the
plicate the thin portion of the sinus of Valsalva and continued until
strong aortic tissue supported by aortic media is reached. Tying of
sutures results in closing the VSD, elevating the right coronary
anulus and cusp, and reducing the size of the right coronary sinus
and RV outflow tract bulge.
Repair of the defect is possible in all cases regardless of VSD
size, which is usually slitlike, because there are always redundant
tissues in the septum and aortic sinus in the vertical plane. Plication
of redundant tissues toward the media of the aortic sinus elevates the
aortic valve cusp and anulus, displacing them centrally towards the
aortic lumen. This results in increased aortic valve coaptation and
restored aortic valve competence. This operation can be applied to

19
patients with doubly committed subarterial VSDs with AR and thus
may apply to the Asian population, in whom these types of defects are
common. If the valve requires replacement, the RV (or pulmonary
trunk) should be opened before valve insertion, the VSD repaired, the
RV closed, and then the aortic valve replaced. This sequence is
advised because occasionally it may be necessary to place sutures
from the prosthetic valve ring across the upper margin of the VSD
patch where it extends between the base of the right and noncoronary
cusps (in the region normally occupied by the membranous septum).
Sutures in this area should be securely buttressed with pledgets.
Although a freehand allograft has been used successfully for valve
replacement under such circumstances, degree of distortion of the
aortic sinuses often makes accurate placement difficult.
Allograft aortic root replacement or aortic valve replacement
with a pulmonary autograft (Ross procedure) is probably a better
choice. When there is also a true thin-walled aneurysm of the sinus of
Valsalva at the base of the right aortic cusp and a VSD, repair is more
difficult because the sinus must also be repaired. If the aortic valve
requires excision and replacement, excision should include the base of
the cusp and the thinned area of the sinus wall, which becomes
continuous with the VSD and is incorporated into its closure. Again,
under such circumstances, the prosthetic valve suture line will cross
the polyester patch. Aortic root replacement may be a simpler

20
solution. When the valve is suitable for plication, the base of the cusp
is preserved and sutured back to the patch.

21
STUDY METHODOLOGY
The study was a hospital-based retrospective non-randomised
observational study involving human subjects. It was done in 50
patients who have undergone aortic valve repair for aortic
regurgitation complicating ventricular septal defect in the congenital
heart disease wing of the Department of Cardiovascular and thoracic
Surgery between January 2010 and December 2014 after obtaining
clearance from the Institute Research Committee and Institute Ethics
Committee.
INCLUSION CRITERIA
All patients who have undergone aortic valve repair for aortic
regurgitation complicating ventricular septal defect during the study
period were included in the study.
EXCLUSION CRITERIA
Patient undergoing Aortic valve repair for aetiology other than
aortic regurgitation complicating Ventricular septal defect
Patients who had lost to follow up during the follow up period.
DEFINITION
Disease recurrence : appearance of AR of Grade 2 or more
during any time in the follow up period.

22
Treatment failure: Need for valve replacement during any time
in the study period.
SAMPLE SIZE CALCULATION
The minimum sample size required will be 30.The exact sample
size was calculated with an expected power of 80% and to detect a
small difference with an effect size of 0.50 and alpha error of 0.025.
The sample size required was estimated to be 38. The study was
begun to analyse at least a minimum of 38 patients.
METHODOLOGY
The list of patients who have undergone aortic valve repair for
AR complicating VSD was obtained from the electronic medical
records using relevant terminologies in the preoperative,
postoperative diagnosis and the procedure executed.
The list obtained was screened and the patients falling within
the inclusion criteria were included in the study.
The medical records were reviewed for demographic data and for
clinical data including the pre op echo findings, intraoperative
findings, operation record, anaesthesia record, intraoperative
transoesophageal ECHO findings and the follow up details. The
data collected were recorded in the observation chart
Demographic data on the age of the patient a surgery, sex,
height (in meter), weight (in kilogram) and body surface area
were collected.

23
Preoperative transthoracic echo was analysed for the following:
Anatomic type of VSD
Anatomy of the aortic valve
Severity of AR
Mechanism of AR
Cusps‟ prolapsing
Degree of cusp deformity
Size of the aortic annulus
Operation record was analysed for the following:
Intraoperative findings on the anatomy of aortic
valve (bicuspid/tricuspid/others), the type of VSD,
Cusps prolapsingMechanism of AR
Nature of cusps
Type of aortic repair performed
Annulus dimensions and type of annuloplasty
Route(s) of VSD approach
Additional procedures performed (if any)
Intraoperative transoesophageal echo findings were
analysed for the following:
Anatomic type of VSD
Anatomy of the aortic valve
Severity of AR
Mechanism of AR

24
Cusps‟ prolapsing
Degree of cusp deformity
Size of the aortic annulus
Residual VSD after procedure
Leaflet coaptation height
Degree of regurgitation
Immediate postoperative transthoracic echo was analysed
for the
Presence of AR
Severity of AR
Mechanism of AR
The patients follow up records at the first month, sixth
month and at the end of first year. It was analysed for the
transthoracic echo findings of
Presence of AR
Severity of AR
Mechanism of AR
METHOD OF ANALYSIS
Statistical analysis was performed using SPSS version 22 for
Windows.

25
All categorical data related to patients characteristics, clinical,
laboratory and surgical parameters were recorded and
presented as frequencies and percentages.
Continuous variables like age, height, weight, BSA were
presented as mean with standard deviation and compared using
Independent Student t test
All the categorical data between the various groups were
compared using Chi-Square or Fischer‟s exact test.
The trend of aortic regurgitation from discharge till the final
view was represented as grades. The mean of ranks during each
review was computed and compared using Friedman test.
All statistical analysis was carried out for two tailed significance
and a „p‟ value ≤ 0.05 was considered statistically significant.

26
RESULTS
I.0 IMPACT OF THE DEMOGRAPHIC PARAMETERS ON THE
DISEASE RECURRENCE
1.1 SEX
Table 2.1 shows, 9(75%) male patients and 3(25%) female
patients had disease recurrence compared to 24 (63.2%) male patients
and 14 (36.8%) female patients had no recurrence during follow up.
When the recurrence was compared between boys and girls using Chi-
squared test, the difference was not statistically significant.
The²value was 0.570 and the p value was 0.450.
1.2 AGE
Table 2.2 shows, the mean age of the patients at surgery, who
had disease recurrence was 7.9 ± 5.3 years and that of who did not
have recurrence was 9.4 ±5.8 years. When the recurrence was
compared between the two groups using student t-test, the difference
was not statistically significant. The t value was 0.770 and the p value
was 0.445.
1.3 BODY WEIGHT
Table 2.2 shows, the mean weight of the patients at surgery,
who had disease recurrence was 20.5 ± 8.8 kg and that of who did not
have recurrence was 25.2 ± 13.8 kg. When the recurrence was
compared between the two groups using student t-test, the difference
was not statistically significant. The t value was 1.099 the p value

27
was 0.277.
1.4 HEIGHT OF THE PATIENT
Table 2.2 shows, the mean height of the patients at surgery,
who had disease recurrence was 1.0 ± 0.1 m and that of who did not
have recurrence was 1.0 ± 0.3 kg. When the recurrence was compared
between the two groups using student t-test, the difference was not
statistically significant. The t value was 0.968the p value was 0.338.
1.5 BODY SURFACE AREA
Table 2.2 shows, the mean body surface area of the patients at
surgery, who had disease recurrence was 0.7 ± 0.2 m² and that of who
did not have recurrence was 0.8 ± 0.3kg. When the recurrence was
compared between the two groups using student t-test, the difference
was not statistically significant. The t value was 0.968 the p value was
0.338.
2.0 IMPACT OF ANATOMICAL FACTORS ON THE DISEASE
RECURRENCE
2.1 VALVE ANATOMY
Table 2.3 shows, 10 (83.3%) of patients with tricuspid valve and
2 (16.7%) with bicuspid valve had disease recurrence. When the
recurrence was compared between the two groups, using Chi- squared
test, the difference was not statistically significant. The ² value was
0.326 and the p value was 0.568.

28
2.2 ANATOMICAL LOCATION OF VSD
From table 2.4, it is known that, of the 12 patients who had
disease recurrence, 8 (66.7%) had subaortic type of VSD and 4(33.7%)
patients had doubly committed VSD. None of the patients with outlet
muscular VSD had disease recurrence.When the recurrence was
compared between the various types of VSD, using Chi- squared test,
the difference was not statistically significant. The ² value was 2.210
and the p value was 0.331.
2.3 SURGICAL APROACH TO VSD CLOSURE
We infer from table 2.5 that, 8 (66.7%) of the 12 patients with
recurrence had their VSD closed from the right atrium (trans-RA).
Whereas, 4 (33.3%) of the 12 patients with recurrence had their VSD
closed from the pulmonary artery (trans-PA). Five patients (13.2%)
whose VSD were closed from the aorta and 2 (5.3%) patients whose
VSD was closed via right ventricle did not have any disease
recurrence.When the recurrence was compared between the various
types of surgical approach, using Chi- squared test, the difference was
not statistically significant. The ² value was 3.150 and the p value
was 0.359.

29
3.0 IMPACT OF THE PREOPERATIVE GRADE OF AORTIC
REGURGITATION ON THE DISEASE RECURRENCE
Table 2.6 shows, a total of 17 (345) patients had moderate grade
of aortic regurgitation and 33 (66%) had severe grade of aortic
regurgitation prior to surgery. Three (25%) patients with moderate
grade of aortic regurgitation and9 (75%) patients with severe grade of
aortic regurgitation had disease recurrence. When the recurrence was
compared between preoperative grades of aortic regurgitation, using
Chi- squared test, the difference was not statistically significant. The
² value was 0.570 and the p value was 0.45
4.0 EFFECT OF THE SURGICAL TECHNIQUES ONRECURRENCE
RATES
We draw the following inferences from the data in Table 2.7.
4.1 Central plication
A total of 11 patients had undergone this procedure accounting
for 22 % of the repairs in this study.
Of the 11 patients who underwent the procedure, 5 patients had
disease recurrence. Hence, the recurrence rate was 45.45% for
this technique.
Considering all the procedures, 5 out of the 12 cases who had
recurrence belong to this group, amounting to 41.7% of disease
recurrence in this study.

30
4.2 Triangular resection
A total of 13 patients had undergone this procedure accounting
for 26 % of the repairs in this study.
Of the 13 patients who underwent the procedure, 3 patients had
disease recurrence. Hence, the recurrence rate was 23.08% for
this technique.
Considering all the procedures, 3 out of the 12 cases who had
recurrence belong to this group, amounting to 25 % of disease
recurrence in this study.
4.3 Trusler repair
A total of 20 patients had undergone this procedure accounting
for 40% of the repairs in this study.
Of the 20 patients who underwent the procedure, 4 had disease
recurrence. Hence, the recurrence rate was 20 % for this
technique.
Considering all the procedures,4 out of the 12 cases who had
recurrence belong to this group, amounting to 33.3% of disease
recurrence in this study.
4.4 Pericardial patch repair
A total of 2 patients had undergone this procedure accounting
for 4 % of the repairs in this study.

31
Of the 2 patients who underwent the procedure, none had
disease recurrence. Hence, the recurrence rate for this
technique was nil.
Considering all the procedures, none of the 12 cases who had
recurrence belong to this group, amounting to zero percent
disease recurrence in this study.
4.5 Yacoub repair
A total of 4 patients had undergone this procedure accounting
for 8 % of the repairs in this study.
Of the 4 patients who underwent the procedure, none had
disease recurrence. Hence, the recurrence rate for this
technique was nil.
Considering all the procedures, none of the 12 cases who had
recurrence belong to this group, amounting to zero percent
disease recurrence in this study.
The disease recurrence was compared between the various
techniques of aortic valve repair, using Chi- squared test, the
difference was not statistically significant. The ²alue was 4.468 and
the p value was 0.346

32
5.0 EFFECT OF ANNULOPLASTY ON DISEASE RECURRENCE
From table 2.8, it is known that, 14 (28%) of the patients had
undergone annuloplasty along with the aortic valve repair in this
study. Six out this 14 patients had disease recurrence. Whereas, six
out of the 36 patients who had not undergone annuloplasty also had
disease recurrence.When the recurrence was compared between the
two groups, using Chi- squared test, the difference was not
statistically significant. The ² value was 3.791 and the p value was
0.052.
6.0 THE EFFECT OF ADDITIONAL SURGICAL PROCEDURES ON
THE DISEASE RECURRENCE
From table 2.9, it is known that, a total of 14 (28%) patients had
undergone additional surgical procedures.
ICR was done in 11(22%) of the patients of which 2 (4%) of the
recurrence. This accounted for 16.7% of recurrence in the
study.
SOV repair was done in 1 (2%) patient who did not have
recurrence.
Mitral valve repair was done in 1(2%) who had recurrence. This
accounted for 4 % of recurrence in the study.
When the recurrence was compared between the groups, using
Chi- squared test, the difference was not statistically significant. The
² value was 8.059 and the p value was 0.153.

33
7.0 TREND OF THE GRADES OF AORTIC REGURGITATION OVER
THE FOLLOW UP PERIOD
From table 3.1 we infer,
At the time of discharge, 11 (22%) had no aortic regurgitation,
33 (66%) had mild grade of aortic regurgitation, 6 (12%) had
moderate grade of regurgitation and none had severe grade of
aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 2.98.
At the time 1st month follow up, 9 (18%) had no aortic
regurgitation, 35 (70%) had mild grade of aortic regurgitation, 6
(12%) had moderate grade of regurgitation and none had severe
grade of aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 3.04.
At the time of 6th month follow up, 8 (16%) had no aortic
regurgitation, 39 (78%) had mild grade of aortic regurgitation, 3
(6%) had moderate grade of regurgitation and none had severe
grade of aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 2.89.
At the time of 1st year follow up, 9 (18%) had no aortic
regurgitation, 33 (66%) had mild grade of aortic regurgitation, 7
(14%) had moderate grade of regurgitation and 1 (2%) had
severe grade of aortic regurgitation. The mean rank (grade of
aortic regurgitation) at the time of discharge was 3.07.

34
At the time of 2nd year follow up, 9(18%) had no aortic
regurgitation, 34 (68%) had mild grade of aortic regurgitation, 6
(12%) had moderate grade of regurgitation and 1(2%) had severe
grade of aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 3.02.
The mean of ranks during each of the visit was compared using
Friedman test to assess any significant change in the trend of the
grade of AR during the follow up period. The p value was 0.749 and
the difference was not statistically significant.

35
Table 1.1
Demographic Parameters of the study population
1. Sample size 50 (100%)
2. Gender
Male 33(66%)
Female 17(34%)
3. Age (in years) 9.02±5.67
4. Weight (in kilograms) 24.04±12.82
5. Body Surface Area (metre²) 0.82±0.30
6.Valve anatomy
Tricuspid 44(88%)
Bicuspid 06(12%)
7. Type of VSD
SAVSD 35(70%)
DCVSD 11(22%)
OUTLET MUSCULAR VSD 04(08%)
TABLE 2.1
Comparison of the sex with disease recurrence
Sex
Recurrence
Total
χ2 p Yes No
N % N % N %
Male 9 75.0 24 63.2 33 66.0
0.570 0.450 Female 3 25.0 14 36.8 17 34.0
Total 12 100.0 38 100.0 50 100.0

36
TABLE 2.2
Comparison of demographic parameters with disease
recurrence
Recurrence t
p value Yes No
Mean SD Mean SD
Age ( in years) 7.9 5.3 9.4 5.8 -0.770 0.445
Weight ( in Kg) 20.5 8.8 25.2 13.8 -1.099 0.277
Height (in meter) 1.0 0.1 1.0 0.3 -0.968 0.338
BSA (in m2 ) 0.7 0.2 0.8 0.3 -1.093 0.280
TABLE 2.3
Comparison of valve anatomy with disease recurrence
VALVE ANATOMY
Recurrence Total
χ2 P
value Yes No
N % N % N %
TAV 10 83.3 34 89.5 44 88.0
0.326 0.568 BAV 2 16.7 4 10.5 6 12.0
Total 12 100.0 38 100.0 50 100.0
TABLE 2.4
Comparison of the type of VSD with disease recurrence
TYPE OF VSD
Recurrence Total
χ2 P Yes No
N % N % N %
SAVSD 8 66.7 27 71.1 35 70.0
2.210 0.331
DCVSD 4 33.3 7 18.4 11 22.0
Outlet
Muscular VSD 0 0.0 4 10.5 4 8.0
Total 12 100.0 38 100.0 50 100.0

37
TABLE 2.5
Comparison of the surgical approach with disease
recurrence
SURGICAL
APROACH TO
VSD
Recurrence
Total
χ2 P Yes No
N % N % N %
Trans Aortic 0 0.0 5 13.2 5 10.0
3.150 0.369
Trans RA 8 66.7 24 63.2 32 64.0
Trans PA 4 33.3 7 18.4 11 22.0
Trans RV 0 0.0 2 5.3 2 4.0
Total 12 100.0 38 100.0 50 100.0
TABLE 2.6
Comparison of preoperative severity of regurgitation with
disease recurrence
PREOP AR
GRADE
Recurrence
Total
χ2 p Yes No
N % N % N %
Moderate 3 25.0 14 36.8 17 34.0
0.570 0.450 Severe 9 75.0 24 63.2 33 66.0
Total 12 100.0 38 100.0 50 100.0

38
TABLE 2.7
Comparison of the surgical technique with disease
recurrence
SURGICAL TECHNIQUE
Recurrence Total
χ2 P Yes No
N % N % N %
1. Central
plication 5 41.7 6 16.2 12 24
4.468 0.346
2. Triangular
resection 3 25.0 10 27.0 13 26
3. Trusler
repair 4 33.3 16 43.2 20 40
4. Pericardial
patch repair 0 0.0 2 5.4 2 4
5. Yacoub
repair 0 0.0 3 8.1 3 6
Total 12 100.0 37 100.0 50 100.0

39
TABLE 2.8
Comparison of annuloplasty with disease recurrence
Recurrence
Total χ2 P ANNULOPLASTY Yes No
N % N % N %
Not done 6 50.0 30 78.9 36 72.0
3.791 0.052 Done 6 50.0 8 21.1 14 28.0
Total 12 100.0 38 100.0 50 100.0
TABLE 2.9
Comparison of additional procedures done with disease
recurrence
ADDITIONAL
PROCEDURE
Recurrence
Total
χ2 P Yes No
N % N % N %
No
additional
procedure
9 75.0 27 71.1 36 72.0
8.059 0.153
ICR 2 16.7 9 23.7 11 22.0
SOV repair 0 0.0 1 2.6 1 2.0
MV repair 1 8.3 0 0.0 1 2.0
Total 12 100.0 38 100.0 50 100

40
TABLE 3.1
TREND OF AORTIC REGURGITATION ON FOLLOW UP
Grade of Aortic
regurgitation
At discharge
First follow
up
Second
follow up
Third
follow up
Fourth
follow up
N % N % N % N % N %
No 11 22.0 9 18.0 8 16.0 9 18.0 9 18.0
Mild 33 66.0 35 70.0 39 78.0 33 66.0 34 68.0
Moderate 6 12.0 6 12.0 3 6.0 7 14.0 6 12.0
Severe 0 0
0 0 0 0 1 2.0 1 2.0
Total 50 100.0 50 100.0 50 100.0 50 100.0 50 100.0
'
Ranks Mean Rank
AR AT DISCHARGE 2.98
POST OP AR AT FOLLOW UP 1 3.04
POST OP AR AT FOLLOW UP 2 2.89
POST OP AR AT FOLLOW UP 3 3.07
POST OP AR AT FOLLOW UP 4 3.02
Friedman test p=0.749

41
TABLE 3.2
Comparison of various surgical techniques and types of VSD on
disease recurrence
SURGICAL
TECHNIQUE
TYPE OF VSD Total
SAVSD DCVSD Outlet VSD
N % N % N % N %
Central Plication 9 75.0 1 8.3 2 16.7 12 100.0
Triangular resection 10 76.9 2 15.4 1 7.7 13 100.0
Trussler repair 14 70.0 6 30.0 0 0.0 20 100.0
Pericardial Patch 1 50.0 1 50.0 0 0.0 2 100.0
Yacoub repair 1 33.3 1 33.3 1 33.3 3 100.0
Total 35 70.0 11 22.0 4 8.0 50 100.0
χ2 =8.854 p=0.354
TABLE 3.3
Comparison of various surgical techniques and the surgical
approach to the VSD closure on disease recurrence
SURGICAL
TECHNIQUE
ROUTE OF VSD REPAIR
Trans Aortic
Trans RA
Trans PA
Trans RV
N % N % N % N % N %
Central Plication 0 0.0 11 91.7 1 8.3 0 0.0 12 100.0
Triangular resection 1 7.7 9 69.2 2 15.4 1 7.7 13 100.0
Trussler 2 10.0 11 55.0 6 30.0 1 5.0 20 100.0
Pericardial Patch 1 50.0 0 0.0 1 50.0 0 0.0 2 100.0
Yacoub 1 33.3 1 33.3 1 33.3 0 0.0 3 100.0
Total 5 10.0 32 64.0 11 22.0 2 4.0 50 100.0
χ2 =13.487 p=0.335

42
FIGURE 1 TREND OF GRADES OF AORTIC RGURGITATION
DURING FOLLOW UP (IN PERCENTAGE)
2218 16 18 18
6670
7866 68
12 126
14 12
0 0 0 2 2
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
At discharge First follow up Second follow up Third follow up Fourth follow up
No Mild Moderate Severe

43
DISCUSSION
The earliest description of aortic cusp prolapse and
regurgitation complicating ventricular septal defects occurring in the
outlet septal region was in 1921 by Laubry and Pezzi24. Garamella and
Starr et al in 1960 first descibed the surgical technique for this
relatively rare congenital heart disease25. Since then, the surgical
techniques had continued to evolve. Yacoub et al in 199723 was the
most recent to describe such a technique of valve repair. With the
surgical techniques being described more recently, the consensus
regarding the patient selection for each technique has been a grey
area. Similarly, though the natural course of disease has been
elucidated in detail by many authors, the factors predicting surgical
success or failure have not been described, particularly in the Asian
population. Thus, this study aimed at identifying the factors that
predict a durable valve in this rare subset of patients.
Hung-Chi Lue, Atsuyoshi Takao et al had shown there is a
tendency for increase in male preponderance in patients with aortic
regurgitation complicating VSD.26 Similar to their observation, male
patients in this study accounted for two third (66%) of the population
with girls forming the rest. Male population also accounted for 75 % of
the recurrence. But when the difference between the two groups was
analysed the difference was not statistically significant (p = 0.450).

44
Komai et al had concluded from their study that “the most
prudent strategy for the patient with VSD and aortic cusp prolapse is
early closure of the VSD before the onset of AR”17. But in our study all
patients had developed aortic regurgitation prior to the procedure. The
age of patients in our study ranged from 1 year to 27 years. The mean
age at surgery being 8.65±5.6 yrs. This is slightly higher to what
Komai et al had speculated from their study which had a median age
of 4.6 years. Hiba Gaafar Salih, Sameh R. Ismail et al in a recent
study, similar to this study employing patients with overt cusp
prolapse prior to surgery also had the mean age of patients 3.8 ± 2.6
years.
The relatively higher age of our patients was because of a
multitude of socioeconomic factors rather than scientific factors. The
poor literacy level and low socioeconomic status of the population our
institution caters to were the major hurdles in getting the patients at
an early age for surgery. This accounts for the considerable level of
delay in diagnosis and referral, withstanding the fact of the long
waiting list of patients for surgery in our institution which is a tertiary
care level hospital.
The comparison of mean age of patients who had disease
recurrence and who did not in this study from table 1.1, had shown
no statistically significant difference between the two groups. We thus

45
infer, aortic valve repair can be safely attempted even in the patients
presenting late in their natural course, with no extra added risk of
recurrence with their younger counterparts. Nevertheless, it is not a
prudent option to delay the surgery.
This study had 6 (12%) patients with bicuspid aortic valve in
contrast to the 1-2% in the general population27. The mechanism of
aortic regurgitation in this group of patients was of El khoury type II
caused by the cusp prolapse unrelated to the occurrence of the VSD18.
All the 6 patients had a perimembranous type of VSD, 5 of which were
repaired by the transatrial approach while in the sixth case, it was
repaired via the transaortic route. Two among these 6 patients
developed disease recurrence by definition, accounting for 16.7 % of
the total recurrences in the study. In both the patients, the severity of
regurgitation declined from grade 2 to grade 1 by the end of first year
and remained the same till the second year follow up. In contrast,
patients with tricuspid aortic valve formed 88% (44/50) of the total
population with 10 recurrences accounting for 83.3% of recurrence.
The comparison of recurrences between the two groups with
anatomically different valve leaflets had shown no statistically
significant difference (p= 0.568). The increased risk of recurrence after
valve repair in patients with bicuspid aortic valve proposed by Okita et
al28 in their study was not established in our study.

46
Most of the patients in this study had perimembranous VSD
accounting for 70 % of population, followed by doubly committed VSD
accounting for 22% and the rest 8% was by outlet muscular VSD. This
was in contrast to the results of previous study by Hisatomi K and
Kosuga K et al29, which had documented increased incidence of
doubly committed VSD in the Asian population.
Okita et al28 had shown increased risk of residual AR with
perimembranous VSD rather than outlet VSDs. When the recurrence
of AR was compared between the various types of VSD in this study,
from table 2.4, the difference was not statistically significant (p=
0.331).
With the echocardiographic evaluation of preoperative severity
of aortic regurgitation, 34% of the study population had moderate
(grade 2) aortic regurgitation and 66% of the population had severe
(grade 3 or more) aortic regurgitation. The incidence of recurrence
was 25% and 75 % for the moderate and the severe grades of AR
respectively. The difference between the two groups on comparison
showed no statistical significance (p= 0.450). The severity of
preoperative aortic regurgitation thus had not precluded a safe valve
repair in patients with AR complicating VSD.
Trusler repair was the most frequently performed procedure in

47
this study with a total of 20 (40 %) cases. Four (20%) out of the 20
patients who underwent this procedure had recurrence. Annuloplasty
was done in 6 of these patients for aortic annulus dilation (≥2 SD).
ICR was done in 3 of these patients for right ventricular outflow
obstruction. Also, from table 3.2 and table 3.3 we know that, the type
of VSD and the route of repair had no bearing on the recurrence. The
recurrence is hence independent of the type of VSD, the surgical
approach to VSD closure, performance of annuloplasty or an
additional procedure. It is probably the growth of the valve per se
accounting for the recurrence of the disease after Trusler repair.
Further, the qualitative analysis of the regurgitant jet by
echocardiogram is essential for elucidating the exact mechanism
involved. But, this analysis was not done in the study.
Similarly, the effect of all the other surgical techniques the
patients had undergone was analysed for the recurrence, including
the Carpenteir technique, Yacoub technique and pericardial patch
repair. Analysis had revealed that there is no difference in terms of
risk of recurrence of one procedure over the other. Subanalysis of the
effect of the various anatomical type of VSD and the surgical approach
to VSD closure on the recurrence of each of the surgical procedure,
had also shown to have no statistically significant difference (table 3.2
and table 3.3).

48
Annuloplasty was done in 14 (28 %) patients with dilated
annulus. This was in addition to addressing the leaflet pathology. Six
out of 14 patients had recurrence, but with no statistically significant
difference on comparison. None of the patients had stenosis during
follow up rather. The addition of subcommissural annuloplasty had
thus found not been associated with an additional risk to patients
undergoing aortic valve repair.
The trend of the grade of aortic regurgitation in the study
population is as shown in table 3.1. The mean of ranks during each
visit was computed and was compared between each visits. But the
difference was not statistically significant. Though there was minor
changes in the number of patients in each of the grades, the mean of
the ranks over the entire study population had not changed
significantly.
Although by the definition in this study,12 patients had
developed recurrence, 11 of those twelve patients had grade 2
(moderate) aortic regurgitation and only 1 patient had severe (grade
3)aortic regurgitation. On analysis of the transthoracic
echocardiographic mechanism of the recurrence, all the recurrence
were intravalvar leaks. All of them were detected on regular follow up
visit and none of the patients were symptomatic for the regurgitation
during the follow up period. Excluding the one patient who required

49
valve replacement in the immediate postoperative period, none of the
other patients either of life in required a replacement or medical
management for their valve leak. The quality of life in all the patients
who had undergone valve repair had definitely improved during follow
up though it was not objectively analysed in the study.
The study was limited by the small sample size and its
retrospective nature though it had analysed a subset of patients with
very low disease incidence. The duration of follow up was also
relatively less to determine the recurrence of the disease considering
the growth potential of the patients in this study who were
predominantly in the pediatric age group. The subjective evidence of
improvement in thequality of life of this population was very evident in
the study. But an objective measurement of the quality of life of this
population would have given the real impact of valve repair in this
rare subset of patients on their clinical as well as socioeconomic
status. Aortic valve repair in patients with aortic regurgitation
complicating ventricular septal defect was thus a safe and durable
procedure considering the short term outcomes. A prospective
randomised trial would be the solution to the questions unanswered
in the study.

50
CONCLUSION
Outcome after aortic valve repair in patients with AR
complicating VSD is not affected by demographic factors like
age, sex, height, weight and the body surface area of the
patients.
Aortic valve repair however, can be safely attempted in patients
presenting with AR late in the course of the disease without
increased risk of recurrence.
Repair of a bicuspid valve associated with VSD can be done
satisfactorily with no added risk of failure of repair.
Anatomical factors like the type of VSD and surgical approach
to VSD closure did not affect the outcome after valve repair.
Additional surgical procedures and annuloplasty during valve
repair have no adverse effect on the outcome of valve repair.
The superiority of one surgical procedure over the other for
aortic valve repair is not evident from our study. A prospective
randomised trial is needed to establish the same.

51
BIBLIOGRAPHY
1. Leung MP, Beerman LB, Siewers RD, Bahnson HT, Zuberbuhler
JR. Long-term follow-up after aortic valvuloplasty and defect
closure in ventricular septal defect with aortic regurgitation. Am
J Cardiol 1987;60:890.
2. Hisatomi K, Kosuga K, Isomura T, Akagawa H, Ohishi K, Koga
M. Ventricular septal defect associated with aortic regurgitation.
Ann ThoracSurg 1987;43:363.
3. Tatsuno K, Konno S, Ando M, Sakakibara S. Pathogenetic
mechanisms of prolapsing aortic valve and aortic regurgitation
associated with ventricular septal defect. Circulation 1973;48:
1028-37.
4. Suresh Babu Hale, Kristen Finucane, Tee-ling Chan, Elizabeth
Rumball, Tom Gentles. Midterm results of repair of
perimembranous or conal ventricular septal defects using the
transaortic direct suture technique. Ann ThoracSurg 2009.
5. MunirBoodhwani, Laurent de Kerchove, David Glineur, Jean
Rubuy,PhilippeNoirhomme and Gebrine El Khoury .Repair-
oriented classification of aortic insufficiency: Impact on surgical
techniques and clinical outcomes. J of Thor and Cardio Surgery,
2009.
6. Jonathan R, G.Etnel, Lisa C, Elmont, EbruErtekin,
M.MostafaMokhles, Peter L, de Jong MD, Johanna J, M.
Takkenberg. Outcome of aortic valve replacement in children- A
systemic review and metaanalysis. J of Thor and Cardio
Surgery, 2015.

52
7. Baker EJ, Ayton V, Smith MA, Parsons JM, Ladusans EJ,
Anderson RH, et al. Magnetic resonance imaging at a high field
strength of ventricular septal defects in infants. Br Heart J
1989;62:305.
8. Barratt-Boyes BG, Simpson M, Neutze JM. Intracardiac surgery
in neonates and infants using deep hypothermia with surface
cooling and limited cardiopulmonary bypass. Circulation
1971;43:I25.
9. Nadas AS, Thilenius OG, LaFarge CG, Hauck AJ. Ventricular
septal defect with aortic regurgitation: medical and pathologic
aspects. Circulation 1964;29:862-73.
10. Ttsuno K, Ando M, Takao A, Hatsune K, Konno S. Diagnostic
importance of aortography in conal ventricular septal defect. Am
Heart J 1975;89: 171.
11. Smolinsky A, Castaneda AR, Van Praagh R. Infundibular septal
resection: surgical anatomy of the superior approach. J
ThoracCardiovascSurg 1988; 95:486.
12. Beerman LB, Park SC, Fischer DR, Fricker FJ, Mathews RA,
Neches WH, et al. Ventricular septal defect associated with
aneurysm of the membranous septum. J Am CollCardiol 1985;
5: 118.
13. Soto B, Becker AE, Moulaert AJ, Lie JT, Anderson RH.
Classification of ventricular septal defects. Br Heart J 1980;
43:332.

53
14. Tatsuno K, Ando M, Takao A, Hatsune K, Konno S. Diagnostic
importance of aortography in conal ventricular septal defect. Am
Heart J 1975;89:171.
15. Tatsuno K, Konno S, Ando M, Sakakibara S. Pathogenetic
mechanisms of prolapsing aortic valve and aortic regurgitation
associated with ventricular septal defect. Circulation
1973;48:1028-37.
16. Yacoub MH, Khan H, Stavri G, Shinebourne E, Radley-Smith R.
Anatomic correction of the syndrome of prolapsing right
coronary aortic cusp, dilatation of the sinus of Valsalva, and
ventricular septal defect. J ThoracCardiovascSurg 1997;113:25.
17. Tatsuno K, Konno S, Ando M, Sakakibara S. Pathogenetic
mechanisms of prolapsing aortic valve and aortic regurgitation
associated with ventricular septal defect. Circulation
1973;48:1028-37.
18. Yasunaru Kawashima, M.D., MicHiakiDanno, M.D., YuKi Hi Ko
Shimizu, M.D., Hikaru Matsuda, M.D., Takeshi Miyamoto, M.D.,
TsuYoshi Fujita, M.D.,Ventricular Septal Defect Associated with
Aortic Insufficiency, Anatomic Classification and Method of
Operation; Circulation 1973.
19. Alexandar S. Nadas, M.D., Otto G. Thilenius, M.D., C.Grant
Lafarge, M.D.,Anna J. HauckM.D.,Ventricular Septal Defect
with Aortic Regurgitation, Medical and Pathologic Aspects;
Circulation 1964.

54
20. Echo assessment of Aortic Regurgitation and its
mechanismsWorkshop: Reconstruction of the Aortic Valve and
Root.
21. Severity Indices of Right Coronary Cusp Prolapse and Aortic
Regurgitation Complicating Ventricular Septal Defect in the
Outlet Septum Which Defect Should Be Closed? Hideshi Tomita,
MD; Yoshio Arakaki, MD; Yasuo Ono, MD; Osamu Yamada, MD;
ToshikatsuYagihara, MD*; Shigeyuki Echigo, MD.
22. Trusler GA, Moes CA, Kidd BS. Repair of ventricular septal
defect with aortic insufficiency. J ThoracCardiovascSurg
1973;66:394.
23. Yacoub MH, Radley-Smith R, de Gasperis C. Primary repair of
large ventricular septal defects in the first year of life. G Ital
Cardiol 1978;8:827.
24. Laubry C, Pezzi C. Traitedes maladies carpentales du coeur. In
Laubry C, Routier D, Soulie P. Les souffles de (a maladie de
Roger). Rev Med Paris 1933;50:439.
25. Garamella JJ, Cruz AB Jr, Heupel WH, Dahl JC, Jensen NK,
Berman R. Ventricular septal defect with aortic insufficiency:
successful surgical correction of both defects by the transaortic
approach. Am J Cardiol 1960;5:266.
26. Hung-Chi Lue, Atsuyoshi Takao et ai,Subpulmonic ventricular
septal defect, Proceedings of the third Asian congress of
Pediatric Cardiology Nov 28th 1983.

55
27. Hiba GaafarSalih, Sameh R. Ismail, Mohamed S. Kabbani2,
Riyadh M. Abu‑Sulaiman. Predictors for the Outcome of Aortic
Regurgitation After Cardiac Surgery in Patients with Ventricular
Septal Defect and Aortic Cusp Prolapse in Saudi Patients; Heart
views 2016.
28. Okita Y, Miki S, Kusuhara K, Ueda Y, Tahata T, Yamanaka K,
et al. Long-term results of aortic valvuloplasty for aortic
regurgitation associated with ventricular septal defect. J Thorac
Cardiovasc Surg 1988; 96:769.
29. Hisatomi K, Isomura T, Sato T, Kawara T, Kosuga K, Ohishi K,
et al. Aortoplasty for aortic regurgitation with ventricular septal
defect. J Thorac Cardiovasc Surg 1994;108:396.

OBSERVATION CHART
NAME
HOSPITAL NO
AGE AT SURGERY
SEX
HEIGHT
WEIGHT
BSA (DERIVED)
PRE OPERATIVE PARAMETERS
Anatomy of the aortic valve :BAV/ TAV/OTHERS
Mechanism of regurgitation:
Grade of AR at diagnosis :MILD/MODERATE/SEVERE
Aortic annulus dimensions: (in mm)
Type of VSD
INTRAOPERATIVE
Type of procedure executed
Need for additional procedures
POSTOPERATIVE
Grade of AR in the immediate postoperative
period:MILD/MODERATE/SEVERE
Grade of AR at
1st monthly :MILD/MODERATE/SEVERE
Half yearly :MILD/MODERATE/SEVERE
Annual follow up:MILD/MODERATE/SEVERE
REOPERATION
Type of procedure
Time of procedure

S NO NAME SEX AGE WEIGHT HEIGHT BSA TYPE OF VSDROUTE OF VSD REPAIRVALVE ANATOMYSURG TECHANNULOPLASTYADD PROCEDUREPREOP ARAR AT DISCHARGE
FIRST SECOND THIRDFOURTH
1 ABHIMANYU S PILLAI 0 5 15 0.99 0.64 1 2 1 1 1 3 1 1 1 2 2
2 ABHINAV 0 8 30 1.02 0.92 2 3 1 2 0 0 2 2 2 2 2 1
3 ABINAYA 1 6 20 0.95 0.73 1 2 2 2 0 0 3 1 1 1 1 1
4 ADHIN JOSE 0 4 17 0.87 0.64 2 3 1 3 0 0 3 1 1 1 2 2
5 ADITHYA 0 10 25 1.12 0.88 1 2 1 1 1 0 2 0 0 2 2 2
6 AJITHA 1 8 18 0.96 0.69 2 3 1 3 1 0 3 0 0 0 0 0
7 AMAL SHAN 0 9 22 1.2 0.86 1 2 1 1 0 0 3 1 1 1 1 1
8 ANAMIKA 1 3 14 0.85 0.57 1 2 1 2 0 0 3 1 1 1 0 0
9 ANJAH 0 14 40 1.28 1.19 2 3 1 3 0 0 3 1 1 1 1 1
10 ANNA JAMUNA 1 9 28 0.95 0.86 1 2 1 1 1 0 3 1 1 1 1 1
11 ANZIL 0 6 21 0.86 0.71 1 2 1 3 1 0 2 1 1 1 1 1
12 ARJUN P A 0 12 32 1.03 0.96 2 3 1 2 0 0 2 1 1 1 1 1
13 ASWATHY ARUN 1 11 15 0.95 0.63 1 2 2 3 1 3 2 1 1 1 1 1
14 BHAVANA 1 10 24 1.25 0.91 1 2 1 2 0 0 2 1 1 1 1 1
15 EDWIN THOMAS 0 10 25 1.18 0.91 2 3 1 6 0 3 3 1 1 1 1 1
16 FATHIMA FIDA 1 1 9 0.65 0.40 1 2 1 1 0 3 3 0 0 0 0 0
17 GOKUL 0 10 30 1.45 1.10 1 1 1 3 0 0 3 1 1 1 2 2
18 GOUTHAM VIJAY 0 8 24 0.89 0.77 1 2 1 2 0 0 3 0 1 1 3 3
19 IDRIS P Y 0 9 23 0.96 0.78 3 2 1 6 0 5 3 1 1 1 1 1
20 JASMIN SEJI 1 22 40 1.24 1.17 2 3 1 3 0 0 2 0 1 1 2 2
21 JUVAN THOMAS 0 2 11 0.81 0.50 1 2 1 2 0 0 2 0 0 0 0 0
22 JEYA MARY 1 8 18 1.01 0.71 1 2 1 1 1 0 3 2 2 2 2 2
23 LIJO 0 16 40 1.35 1.22 1 2 1 3 1 3 2 1 1 1 1 1
24 MEEVAL THOMAS 1 5 15 0.87 0.60 1 1 1 5 0 0 3 0 0 0 0 0
25 MUHAMMED ALFIN 0 2 10 0.77 0.46 3 1 1 2 0 0 2 0 0 0 0 0
26 NANDANA 1 3 15 0.89 0.61 2 3 1 1 1 6 3 2 2 1 1 1
27 NASEEHA 1 9 28 1.02 0.89 1 2 2 3 0 0 2 1 1 1 1 1
28 NEWJIN 0 7 12 0.85 0.53 3 2 1 1 0 0 2 1 1 1 1 1
29 NEERAJA RAJ 1 3 7 0.79 0.39 1 2 1 3 0 3 2 1 1 1 1 1
30 PRIYADHARSHINI 1 9 17 0.85 0.63 1 2 1 2 1 0 3 1 1 1 1 1
31 RAHUL 0 4 16 0.92 0.64 2 3 1 3 0 0 3 1 1 1 1 1
32 SAHAD 0 17 35 1.15 1.06 1 2 1 1 0 0 3 0 1 1 1 1
33 RIFANA 1 2 14 0.95 0.61 3 2 1 1 1 3 2 1 1 1 1 1
POST OP FOLLOW UP

34 SANTHANA KUMAR 0 20 55 1.6 1.56 1 2 1 2 0 3 2 1 1 1 1 1
35 SHABINA 1 14 45 1.45 1.35 1 2 1 1 0 0 2 1 0 0 0 0
36 SUDHA 1 10 55 1.45 1.49 1 4 1 2 1 3 3 1 1 1 1 1
37 SURESH M 0 27 68 1.71 1.80 1 4 1 3 0 3 3 1 1 1 1 1
38 TINTO MATHEW 0 25 40 1.32 1.21 2 3 1 4 0 4 3 1 1 1 1 1
39 VIGNESH 0 10 23 0.94 0.77 1 2 1 3 0 0 3 1 1 1 1 1
40 VISHNU 0 7 23 0.93 0.77 1 2 1 3 0 0 3 1 1 1 1 2
41 VYSHNAV 0 9 18 0.82 0.64 1 2 1 3 0 0 3 0 0 0 0 0
42 KRISHNA SANGEETHA 0 7 18 0.88 0.66 1 1 1 3 0 0 3 1 1 1 1 1
43 SREESHMA 0 5 15 0.87 0.60 1 2 1 3 0 0 2 1 1 1 1 1
44 THASNI 0 12 24 1.02 0.82 1 2 1 1 0 3 3 2 2 1 1 1
45 SHAMLA SHERIN 0 10 25 0.99 0.83 1 1 2 4 0 0 3 1 1 1 1 1
46 MUHAMMED MIHRAN 0 2 6 0.77 0.36 1 2 1 3 1 0 3 1 1 1 2 2
47 ANJANA 0 6 14 0.8 0.56 1 2 2 3 1 0 3 2 2 1 1 1
48 VINOD 0 10 25 0.95 0.81 2 3 1 3 0 0 3 0 0 0 0 0
49 SELVAKUMAR 0 7 18 1.04 0.72 1 2 2 2 0 0 3 2 2 1 1 1
50 ANITHA 0 8 20 0.95 0.73 1 2 1 2 0 0 3 1 1 1 1 1
1.0274 0.82
12.8237 0.30
CODES USED
1-TAV1-CENTRAL PLICATION0- NOT DONE0- NO ADD PROC
0- MALE 1- SAVSD1- TRANS AORTIC2-BAV2-RCC TRIANGULAR 1-DONE1-ICR
1- FEMALE 2-DCVSD2- TRANS RA3-TRUSSLERSSOV REPAIR1 MILD
3- OUTLET MUSCULAR VSD3- TRANS PA4-PERICARDIAL PATCH3-MV REPAIR2 MODERATE
4-TRANS RVYACOUB 3 SEVERE
0 NO AR
GRADE OF AR

Plagiarism Checker X Originality Report
Similarity Found: 2%
Date: Sunday, October 08, 2017
Statistics: 68 words Plagiarized / 4008 Total words
Remarks: Low Plagiarism Detected - Your Document needs Optional Improvement.
-------------------------------------------------------------------------------------------
OUTCOME OF AORTIC VALVE REPAIR FOR AORTIC REGURGITATION COMPLICATING
VENTRICULAR SEPTAL DEFECT-A RETROSPECTIVE OBSERVATIONAL STUDY
INTRODUCTION Aortic regurgitation in patients with ventricular septal defect (VSD)
occurs in those anatomical types that are located close to or in direct contact with the
aortic valve. This subset of patients form a relatively rare group of patients with an
incidence ranging between 5% and 10%.Perimembranous and doubly committed
juxta-arterial defects are the commonly affected types. Rarely, it can occur in outlet
muscular VSD also.
Prolapse of the valvular cusps caused by the venturi effect of the ventricular septal
defect jet, abnormal commissural suspension, lack of appositional forces and lack of
continuity between the aortic media, annulus of aortic valve and the ventricular septum
have been the commonly proposed pathological anatomic mechanisms of regurgitation.
The right coronary cusp (RCC) is the usually involved cusp.
This is followed in line by the non-coronary cusp whereas, the involvement of the left
coronary cusp is very rare. The prolapsing cusps render the valve incompetent and cause
significant damage to the valve cusp and annulus. The prolapsing AV may completely
close the VSD so that the shunt may disappear but leaving behind the regurgitation to
progress.
Surgical closure of the defect with aortic valve repair is indicated for these patients
irrespective of the grade of preoperative aortic regurgitation and it is recommended to
close the defect at the earliest. The technique of valve repair is decided based on the
mechanism(s) of regurgitation Despite increasing interest in pediatric aortic valve repair
is unavoidable in certain circumstances.

With limited options for valve replacement and lack of prospective studies the
superiority of these one prosthesis over the other cannot be ascertained. Metaanalysis
has shown that all the currently available valve substitutes are associated with
suboptimal outcome in children. Hence a durable aortic valve repair is the need of the
hour.
This study aims to evaluate the outcome of patients who underwent aortic valve repair
procedures for aortic regurgitation complicating VSD and to also to assess the
predictors for their outcomes after surgery. METHODOLOGY The study was a
hospital-based retrospective non-randomised observational study involving human
subjects. It was done in 50 patients who have undergone aortic valve repair for aortic
regurgitation complicating ventricular septal defect in the Department of Cardiovascular
and thoracic Surgery between January 2010 and December 2015 after obtaining
clearance from the Institute Research Committee and Institute Ethics Committee.
INCLUSION CRITERIA All patients who have undergone aortic valve repair for aortic
regurgitation complicating ventricular septal defect during the study period were
included in the study. EXCLUSION CRITERIA Patient undergoing Aortic valve repair for
aetiology other than aortic regurgitation complicating Ventricular septal defect Patients
who had lost to follow up SAMPLE SIZE CALCULATION The minimum sample size
required will be 30.The exact sample size was calculated with an expected power of 80%
and to detect a small difference with an effect size of 0.50 and alpha error of 0.025.
The sample size required was estimated to be 38. The study was begun to analyse at
least a minimum of 38 patients. METHODOLOGY The list of patients who have
undergone aortic valve repair for AR complicating VSD was obtained from the electronic
medical records using relevant terminologies in the preoperative, postoperative
diagnosis and the procedure executed.
The list obtained was screened and the patients falling within the inclusion criteria were
included in the study. The medical records were reviewed for demographic data and for
clinical data including the pre op echo findings, intraoperative findings, operation
record, anaesthesia record, intraoperative transoesophageal ECHO findings and the
follow up details.
The data collected were recorded in the observation chart Demographic data on the age
of the patient a surgery, sex, height (in meter), weight (in kilogram) and body surface
area were collected. Preoperative transthoracic echo was analysed for the following:
Anatomic type of VSD Anatomy of the aortic valve Severity of AR Mechanism of AR

Cusps‟ prolapsing Degree of cusp deformity Size of the aortic annulus Operation record
was analysed for the following: Intraoperative findings on the anatomy of aortic valve
(bicuspid/tricuspid/others), the type of VSD, Cusps prolapsing Mechanism of AR Nature
of cusps Type of aortic repair performed Annulus dimensions and type of annuloplasty
Route(s) of VSD approach Additional procedures performed (if any) Intraoperative
transoesophageal echo findings were analysed for the following: Anatomic type of VSD
Anatomy of the aortic valve Severity of AR Mechanism of AR Cusps‟ prolapsing Degree
of cusp deformity Size of the aortic annulus type Residual VSD after procedure Leaflet
coaptation height and Degree of regurgitation Immediate postoperative transthoracic
echo was analysed for the Presence of AR Severity of AR Mechanism of AR The patients
follow up records at the first month, sixth month and at the end of first year.
It was analysed for the transthoracic echo findings of Presence of AR Severity of AR
Mechanism of AR METHOD OF ANALYSIS Statistical analysis was performed using SPSS
version 22 for Windows. All categorical data related to patients characteristics, clinical,
laboratory and surgical parameters were recorded and presented as frequencies and
percentages.
Continuous variables like age, height, weight, BSA were presented as mean with
standard deviation and compared using Independent Student t test All the categorical
data between the various groups were compared using Chi-Square or Fischer‟s exact
test. The trend of aortic regurgitation from discharge till the final view was represented
as grades.
The mean of grades during each review was computed and compared using Wilcoxin
rank sum test. All statistical analysis was carried out for two tailed significance and a „p‟
value = 0.05 was considered statistically significant RESULTS RESULTS IMPACT OF THE
DEMOGRAPHIC PARAMETERS ON THE DISEASE RECURRENCE SEX Table 2.1
shows, 9 (75%) male patients and 3(25%) female patients had disease recurrence
compared to 24 (63.2%) male patients and 14 (36.8%) female patients had no recurrence
during follow up. When the recurrence was compared between boys and girls using Chi-
squared test, the difference was not statistically significant. The ?² value was 0.570 and
the p value was 0.450. AGE Table 2.2 shows, the mean age of the patients at surgery,
who had disease recurrence was 7.9 ± 5.3
years and that of who did not have recurrence was 9.4 ± 5.8 years. When the recurrence
was compared between the two groups using student t-test, the difference was not
statistically significant. The t value was 0.770 and the p value was 0.445. BODY WEIGHT
Table 2.2 shows, the mean weight of the patients at surgery, who had disease recurrence

was 20.5 ± 8.8
kg and that of who did not have recurrence was 25.2 ± 13.8 kg. When the recurrence
was compared between the two groups using student t-test, the difference was not
statistically significant. The t value was 1.099 the p value was 0.277. HEIGHT OF THE
PATIENT Table 2.2 shows, the mean height of the patients at surgery, who had disease
recurrence was 1.0 ± 0.1
m and that of who did not have recurrence was 1.0 ± 0.3 kg. When the recurrence was
compared between the two groups using student t-test, the difference was not
statistically significant. The t value was 0.968 the p value was 0.338. BODY SURFACE
AREA Table 2.2 shows, the mean body surface area of the patients at surgery, who had
disease recurrence was 0.7 ± 0.2
m² and that of who did not have recurrence was 0.8 ± 0.3kg. When the recurrence was
compared between the two groups using student t-test, the difference was not
statistically significant. The t value was 0.968 the p value was 0.338. IMPACT OF
ANATOMICAL FACTORS ON THE DISEASE RECURRENCE VALVE ANATOMY Table 2.3
shows, 10 (83.3%) of patients with tricuspid valve and 2 (16.7%) with bicuspid valve had
disease recurrence.
When the recurrence was compared between the two groups, using Chi- squared test,
the difference was not statistically significant. The ?² value was 0.326 and the p value
was 0.568. ANATOMICAL LOCATION OF VSD From table 2.4, it is known that, of the 12
patients who had disease recurrence, 8 (66.7%) had subaortic type of VSD and 4(33.7%)
patients had doubly committed VSD. None of the patients with outlet muscular VSD had
disease recurrence.
When the recurrence was compared between the various types of VSD, using Chi-
squared test, the difference was not statistically significant. The ?² value was 2.210 and
the p value was 0.331. SURGICAL APROACH TO VSD CLOSURE We infer from table 2.5
that, 8 (66.7%) of the 12 patients with recurrence had their VSD closed from the right
atrium (trans-RA). Whereas, 4 (33.3%) of the 12 patients with recurrence had their VSD
closed from the pulmonary artery (trans-PA). Five patients (13.2%) whose VSD were
closed from the aorta and 2 (5.3%) patients whose VSD was closed via right ventricle did
not have any disease recurrence.
When the recurrence was compared between the various types of surgical approach,
using Chi- squared test, the difference was not statistically significant. The ?² value was
3.150 and the p value was 0.359. IMPACT OF THE PREOPERATIVE GRADE OF AORTIC

REGURGITATION ON THE DISEASE RECURRENCE Table 2.6 shows, a total of 17 (345)
patients had moderate grade of aortic regurgitation and 33 (66%) had severe grade of
aortic regurgitation prior to surgery.
Three (25%) patients with moderate grade of aortic regurgitation and 9 (75%) patients
with severe grade of aortic regurgitation had disease recurrence. When the recurrence
was compared between preoperative grades of aortic regurgitation, using Chi- squared
test, the difference was not statistically significant. The ?² value was 0.570 and the p
value was 0.45 EFFECT OF THE SURGICAL TECHNIQUES ON RECURRENCE RATES We
draw the following inferences from the data in Table 2.7.
Central plication A total of 11 patients had undergone this procedure accounting for 22
% of the repairs in this study. Of the 11 patients who underwent the procedure, 5
patients had disease recurrence. Hence, the recurrence rate was 45.45% for this
technique. Considering all the procedures, 5 out of the 12 cases who had recurrence
belong to this group, amounting to 41.7% of disease recurrence in this study.
Triangular resection A total of 13 patients had undergone this procedure accounting for
26 % of the repairs in this study. Of the 13 patients who underwent the procedure, 3
patients had disease recurrence. Hence, the recurrence rate was 23.08% for this
technique. Considering all the procedures, 3 out of the 12 cases who had recurrence
belong to this group, amounting to 25 % of disease recurrence in this study.
Trusler repair A total of 20 patients had undergone this procedure accounting for 40%
of the repairs in this study. Of the 20 patients who underwent the procedure, 4 had
disease recurrence. Hence, the recurrence rate was 20 % for this technique. Considering
all the procedures, 4 out of the 12 cases who had recurrence belong to this group,
amounting to 33.3% of disease recurrence in this study.
Pericardial patch repair A total of 2 patients had undergone this procedure accounting
for 4 % of the repairs in this study. Of the 2 patients who underwent the procedure,
none had disease recurrence. Hence, the recurrence rate for this technique was nil.
Considering all the procedures, none of the 12 cases who had recurrence belong to this
group, amounting to zero percent disease recurrence in this study.
Yacoub repair A total of 4 patients had undergone this procedure accounting for 8 % of
the repairs in this study. Of the 4 patients who underwent the procedure, none had
disease recurrence. Hence, the recurrence rate for this technique was nil. Considering all
the procedures, none of the 12 cases who had recurrence belong to this group,
amounting to zero percent disease recurrence in this study.

The disease recurrence was compared between the various techniques of aortic valve
repair, using Chi- squared test, the difference was not statistically significant. The ?²alue
was 4.468 and the p value was 0.346 EFFECT OF ANNULOPLASTY ON DISEASE
RECURRENCE From table 2.8, it is known that, 14 (28%) of the patients had undergone
annuloplasty along with the aortic valve repair in this study. Six out this 14 patients had
disease recurrence.
Whereas, six out of the 36 patients who had not undergone annuloplasty also had
disease recurrence. When the recurrence was compared between the two groups, using
Chi- squared test, the difference was not statistically significant. The ?² value was 3.791
and the p value was 0.052. THE EFFECT OF ADDITIONAL SURGICAL PROCEDURES ON
THE DISEASE RECURRENCE From table 2.9, it is known that, a total of 14 (28%) patients
had undergone additional surgical procedures. ICR was done in 11(22%) of the patients
of which 2 (4%) of the recurrence.
This accounted for 16.7% of recurrence in the study. SOV repair was done in 1 (2%)
patient who did not have recurrence. Mitral valve repair was done in 1(2%) who had
recurrence. This accounted for 4 % of recurrence in the study. When the recurrence was
compared between the groups, using Chi- squared test, the difference was not
statistically significant. The ?² value was 8.059 and the p value was 0.153. TREND OF THE
GRADES OF AORTIC REGURGITATION OVER THE FOLLOW UP PERIOD From table 3.1
we infer, At the time of discharge, 11 (22%) had no aortic regurgitation, 33 (66%) had
mild grade of aortic regurgitation, 6 (12%) had moderate grade of regurgitation and
none had severe grade of aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 2.98. At the time 1st month follow up, 9
(18%) had no aortic regurgitation, 35 (70%) had mild grade of aortic regurgitation, 6
(12%) had moderate grade of regurgitation and none had severe grade of aortic
regurgitation. The mean rank (grade of aortic regurgitation) at the time of discharge was
3.04.
At the time of 6th month follow up, 8 (16%) had no aortic regurgitation, 39 (78%) had
mild grade of aortic regurgitation, 3 (6%) had moderate grade of regurgitation and
none had severe grade of aortic regurgitation. The mean rank (grade of aortic
regurgitation) at the time of discharge was 2.89. At the time of 1st year follow up, 9
(18%) had no aortic regurgitation, 33 (66%) had mild grade of aortic regurgitation, 7
(14%) had moderate grade of regurgitation and 1 (2%) had severe grade of aortic
regurgitation. The mean rank (grade of aortic regurgitation) at the time of discharge was
3.07.

At the time of 2nd year follow up, 9(18%) had no aortic regurgitation, 34 (68%) had mild
grade of aortic regurgitation, 6 (12%) had moderate grade of regurgitation and 1(2%)
had severe grade of aortic regurgitation. The mean rank (grade of aortic regurgitation)
at the time of discharge was 3.02. The mean of ranks during each of the visit was
compared using Friedman test to assess any significant change in the trend of the grade
of AR during the follow up period. The p value was 0.749 and the difference was not
statistically significant DISCUSSION The earliest description of aortic cusp prolapse and
regurgitation complicating ventricular septal defects occurring in the outlet septal
region was in 1921 by Laubry and Pezzi.
Garamella and Starr et al in 1960 first descibed the surgical technique for this relatively
rare congenital heart disease. Since then, the surgical techniques had continued to
evolve. Yacoub et al in 1997 was the most recent to describe such a technique of valve
repair. With the surgical techniques being described more recently, the consensus
regarding the patient selection for each technique has been a grey area.
Similarly, though the natural course of disease has been elucidated in detail by many
authors, the factors predicting surgical success or failure have not been described,
particularly in the Asian population. Thus, this study aimed at identifying the factors that
predict a durable valve in this rare subset of patients. Hung-Chi Lue, Atsuyoshi Takao et
al had shown there is a tendency for increase in male preponderance in patients with
aortic regurgitation complicating VSD.
Similar to their observation, male patients in this study accounted for two third (66%) of
the population with girls forming the rest. Male population also accounted for 75 % of
the recurrence. But when the difference between the two groups was analysed the
difference was not statistically significant (p = 0.450).
Komai et al had concluded from their study that “the most prudent strategy for the
patient with VSD and aortic cusp prolapse is early closure of the VSD before the onset of
AR”. But in our study all patients had developed aortic regurgitation prior to the
procedure. The age of patients ranged from 1 year to 27 years. The mean age at surgery
being 8.65 ± 5.6 yrs. This is slightly higher to what Komai et al had speculated from their
study which had a median age of 4.6 years.
Hiba Gaafar Salih, Sameh R. Ismail et al in a recent study, similar to this study employing
patients with overt cusp prolapse prior to surgery had the mean age of patients 3.8 ±
2.6 years. The relatively higher age of our patients is because of a multitude of
socioeconomic factors rather than scientific factors.

The poor literacy level and low socioeconomic status of the population our institution
caters to are the major hurdles in early age at surgery. This accounts for the
considerable level of delay in diagnosis and referral, withstanding the fact of the long
waiting list of patients for surgery in our institution which is a tertiary care level hospital.
But, the comparison of mean age of patients who had disease recurrence and who did
not, had shown no statistically significant difference between the two groups. We thus
infer, aortic valve repair can be safely attempted even in the patients presenting late in
their natural course, with no extra added risk of recurrence with their younger
counterparts. Nevertheless, it is not a prudent option to delay the surgery.
This study had 6 (12%) patients with bicuspid aortic valve in contrast to the 1-2% in the
general population. The mechanism of aortic regurgitation in this group of patients was
El khoury type II caused by the cusp prolapse unrelated to the occurrence of the VSD. All
the 6 patients had a perimembranous type of VSD, 5 of which were repaired by the
transatrial approach while in the sixth case, it was repaired via the transaortic route. Two
among the 6 patients developed disease recurrence by definition, accounting for 16.7 %
of the total recurrences in the study.
In both the patients, the severity of regurgitation declined from grade 2 to grade 1 by
the end of first year and remained till the second year follow up. In contrast, patients
with tricuspid aortic valve formed 88% (44/50) of the total population with 10
recurrences accounting for 83.3% of recurrence. The comparison of recurrences between
the two groups had shown no statistically significant difference (p= 0.568).
This rules out the increased risk of recurrence after valve repair in patients with bicuspid
aortic valve in this study population. Most of the patients in this study had
perimembranous VSD accounting for 70 % of population, followed by doubly
committed VSD accounting for 22% and the rest 8% is by outlet muscular VSD.
This is in contrast to the results of previous study by Hisatomi K and Kosuga K et al,
which had documented increased incidence of doubly committed VSD in the Asian
population. Okita et al had shown increased risk of residual AR with perimembranous
VSD rather than outlet VSDs. When the recurrence of AR was compared between the
various types of VSD in this study, from table 2.4, the difference was not statistically
significant (p= 0.331).
With the echocardiographic evaluation of preoperative severity of aortic regurgitation,
34% of the study population had moderate (grade 2) regurgitation and 66% of the

population had severe (grade 3 or more) regurgitation. The incidence of recurrence was
25% and 75 % respectively, the difference between the two groups on comparison
showed no statistical significance (p= 0.450).
The severity of aortic regurgitation thus doesn‟t preclude a safe valve repair in patients
with AR complicating VSD. Trusler repair was the most frequently performed procedure
in this study with a total of 20 (40 %) cases. Four (20%) out of the 20 patients who
underwent this procedure had recurrence. Annuloplasty was done in 6 of these patients
for aortic annulus dilation (=2 SD).
ICR was done in 3 of these patients for right ventricular outflow obstruction. Also, from
table 3.2 and table 3.3 we know that, the type of VSD and the route of repair had no
bearing on the recurrence. The recurrence is hence independent of the type of VSD, the
surgical approach to VSD closure, performance of annuloplasty or an additional
procedure.
It is probably the growth of the valve per se accounting for the recurrence of the
disease. Further, the qualitative analysis of the regurgitant jet by Echocardiogram is
essential for elucidating the exact mechanism involved. But, this analysis was not done
in the study.
Similarly, the effect of all the other surgical techniques the patients had undergone was
analysed for the recurrence, including the Carpenteir technique, Yacoub technique and
pericardial patch repair. Analysis had revealed that there is no difference in terms of risk
of recurrence of one procedure over the other. Subanalysis of the effect of the
anatomical type of VSD and the surgical approach to VSD closure on the recurrence of
each of the surgical procedure, had also shown to have no statistically significant
difference (table 3.2 and table 3.3). Annuloplasty was done in 14 (28 %) patients with
dilated annulus.
This was in addition to addressing the leaflet pathology. Six out of 12 patients had
recurrence, but with no statistically significant difference on comparison. None of the
patients had stenosis during follow up. The addition of subcommissural annuloplasty
has thus found not been associated with additional risk to patients undergoing aortic
valve repair.
The trend of the grade of aortic regurgitation in the study population is as shown in
table 3.1. The mean of ranks during each visit was computed and was compared
between each visits. But the difference was not statistically significant. Though there was
minor changes in the number of patients in each of the grades, the mean of the ranks

over the entire study population had not changed significantly.
Although by the definition in this study,12 patients had developed recurrence, 11 of
those twelve patients had grade 2 (moderate) aortic regurgitation and only 1 patient
had severe (grade 3)aortic regurgitation. On analysis of the transthoracic
echocardiographic mechanism of the recurrence, all the recurrence were intravalvar
leaks.
All of them were detected on regular follow up visit and none of the patients were
symptomatic for the regurgitation during the follow up period. Excluding the one
patient who required valve replacement in the immediate postoperative period, none of
the other patients either of life in required a replacement or medical management for
their valve leak.
The quality of life in all the patients who had undergone valve repair had definitely
improved during follow up though it was not objectively analysed in the study. The
study was limited by the small sample size and its retrospective nature though it had
analysed a subset of patients with very low disease incidence. The duration of follow up
was also relatively less to determine the recurrence of the disease considering the
growth potential of the patients in this study who were predominantly in the pediatric
group. The subjective evidence of improvement in the quality of life of this population
was very evident in the study.
But an objective measurement of the quality of life of this population would have given
the real impact of valve repair in this rare subset of patients on their clinical and
socioeconomic status. Aortic valve repair in patients with aortic regurgitation
complicating ventricular septal defect was thus a safe and durable procedure
considering the short term outcomes. A prospective randomised trial would be the
solution to the unanswered questions in the study.
INTERNET SOURCES:
-------------------------------------------------------------------------------------------
0% - http://emedicine.medscape.com/article/15
0% - https://www.nhlbi.nih.gov/health/health-
0% - http://www.hopkinsmedicine.org/gastroent
0% - https://www.bsecho.org/congenital-heart-
0% - https://link.springer.com/article/10.100
0% - http://journals.sagepub.com/doi/10.1177/

0% - http://www.heartviews.org/article.asp?is
0% - http://www.scielo.br/scielo.php?script=s
0% - https://www.scribd.com/document/32673515
0% - Empty
0% - https://www.journalrmc.com/volumes/13945
0% - http://emedicine.medscape.com/article/90
0% - http://journals.lww.com/innovjournal/Pag
0% - http://www.heart.org/HEARTORG/Conditions
0% - http://www.jtcvsonline.org/article/S0022
0% - https://link.springer.com/article/10.216
0% - http://www.heartviews.org/article.asp?is
0% - https://link.springer.com/article/10.100
0% - http://heart.bmj.com/content/83/1/81
0% - https://trialsjournal.biomedcentral.com/
0% - http://heart.bmj.com/content/102/18/1479
0% - http://www.linguee.de/englisch-deutsch/u
0% - http://www.sciencedirect.com/science/art
0% - https://www.researchgate.net/file.PostFi
0% - https://link.springer.com/content/pdf/10
0% - https://link.springer.com/content/pdf/10
0% - https://link.springer.com/article/10.100
0% - http://www.sciencedirect.com/science/art
0% - https://www.researchgate.net/publication