Out-of-field photon dose following removal of the flattening filter from a medical accelerator
Transcript of Out-of-field photon dose following removal of the flattening filter from a medical accelerator
This content has been downloaded from IOPscience. Please scroll down to see the full text.
Download details:
IP Address: 128.235.251.161
This content was downloaded on 17/08/2014 at 16:59
Please note that terms and conditions apply.
Out-of-field photon dose following removal of the flattening filter from a medical accelerator
View the table of contents for this issue, or go to the journal homepage for more
2010 Phys. Med. Biol. 55 2155
(http://iopscience.iop.org/0031-9155/55/8/003)
Home Search Collections Journals About Contact us My IOPscience
IOP PUBLISHING PHYSICS IN MEDICINE AND BIOLOGY
Phys. Med. Biol. 55 (2010) 2155–2166 doi:10.1088/0031-9155/55/8/003
Out-of-field photon dose following removal of theflattening filter from a medical accelerator
Stephen F Kry1, Oleg N Vassiliev and Radhe Mohan
Department of Radiation Physics, The University of Texas MD Anderson Cancer Center,Houston, TX, USA
E-mail: [email protected]
Received 3 December 2009, in final form 11 February 2010Published 19 March 2010Online at stacks.iop.org/PMB/55/2155
AbstractThe aim of this paper is to determine the effect of removing the flatteningfilter from a linear accelerator on the out-of-field photon dose. A MonteCarlo model was used to simulate 6 MV and 18 MV photon beams from aVarian 2100 accelerator with the flattening filter in place and with it removed.The out-of-field photon doses and composition (head leakage, patient scatterand collimator scatter) were calculated from square open fields in a watertank as a function of distance from central axis, field size and depth. Theout-of-field doses resulting from intensity-modulated radiation therapy to theprostate at 6 MV were also calculated, with and without the flattening filter,to sensitive organs in an anthropomorphic Rando phantom. Removal of theflattening filter reduced the out-of-field dose near the treatment field (<3 cmfrom the field edge) because of decreased collimator scatter. It increasedthe out-of-field dose at intermediate distances from the field edge (3–15 cm)because of increased patient scatter. At greater distances, the out-of-field dosewas decreased because of reduced head leakage. For the clinical treatmentexamined, the out-of-field dose was generally reduced following removal ofthe flattening filter, particularly at large distances from the treatment field.Removal of the flattening filter may be advantageous by reducing the out-of-field dose to the patient. This could contribute to reducing the long-termrisk of secondary malignancies. In general, however, the out-of-field dosedepends on treatment and patient parameters, and a reduction may not alwaysbe achievable.
1. Introduction
An undesired by-product of radiation therapy is radiation outside the treatment field (Stovallet al 1995, van der Giessen 1996, Followill et al 1997, Kry et al 2005a, Howell et al 2006,
1 Author to whom any correspondence should be addressed.
0031-9155/10/082155+12$30.00 © 2010 Institute of Physics and Engineering in Medicine Printed in the UK 2155
2156 S F Kry et al
Reft et al 2006). This out-of-field radiation may originate from leakage through the acceleratorhead shielding (leakage), scatter from the collimator system (collimator scatter), or internalscatter within the patient (patient scatter) (Kase et al 1983, Cozzi et al 2001). The relativeimportance of these three components to the out-of-field dose depends on treatment energy,field size, distance from the central axis and depth in the patient. In general, patient scatterpredominates near to the treatment field, while head leakage predominates far from thetreatment field (beyond ∼20 cm from the field edge) (Kase et al 1983).
Low doses of radiation, such as the out-of-field dose received by radiotherapy patients,may induce a host of late effects such as secondary cancers (Brenner et al 2000, Boice et al1985, Ron 2003, Preston et al 2003), heart disease (Preston et al 2003) and strokes (Prestonet al 2003). A recent study of second cancers following childhood cancer found that 66%of second cancers occurred at the edge of the treatment field (no more than 2.5 cm insidethe treatment field and no more than 5 cm outside of the edge of it), and 22% occurred >5cm away from the treatment field (Diallo et al 2009). It is clearly beneficial to minimize theout-of-field radiation. However, this conflicts with the current trend in modern radiotherapy.Compared to conventional therapy, intensity-modulated radiation therapy (IMRT) treatments,in particular, have been found to increase out-of-field doses (Kry et al 2005a, Howell et al2006), which may increase the risk of late effects (Followill et al 1997, Hall and Wuu 2003,Kry et al 2005b).
Removal of the flattening filter (FF) from the beam line may ameliorate the problem ofthe increased out-of-field dose. The FF scatters a large number of photons that contribute tothe out-of-field dose (Cozzi et al 2001). Furthermore, its removal improves the efficiency oftreatment-dose delivery (less integral target current is required to deliver a treatment (Vassilievet al 2006a)), which should reduce accelerator head leakage. Removal of the flattening filterduring stereotactic radiotherapy was found in a case study to reduce the out-of-field dose by17–50% (O’Brien et al 1991), and it has been proposed that its removal may also reduce theout-of-field dose during IMRT (Hall and Wuu 2003). While it appears possible, and in manyways advantageous, to deliver radiation therapy treatments with the flattening filter removedfrom a traditional medical accelerator (O’Brien et al 1991, Fu et al 2004, Vassiliev et al 2006a,2006b, 2007a, 2007b , 2009, Ponisch et al 2006a, Titt et al 2006a, 2006b, Kry et al 2007a,2008, Mesbahi 2007a, 2007b , 2009, Cashmore 2008, Stathakis et al 2009, Kragl et al 2009),the out-of-field dose associated with such modified treatments has not yet been studied indetail.
In this study, we used Monte Carlo simulations to determine the out-of-field photondoses delivered both with and without the flattening filter at 6 MV and 18 MV. Althoughquantifying the out-of-field photon dose during clinical treatments is the ultimate goal, suchtreatments depend on the patient, tumor location, planning strategy and planning system,thereby preventing an evaluation of the underlying issues governing the out-of-field dosefollowing removal of the flattening filter. Therefore, in this study we primarily examinedsquare, open fields from which more general conclusions may be drawn and examine only acase study for IMRT results. Although neutrons make a contribution to the out-of-field doseat high treatment energies, they were not explicitly addressed in this study because they havebeen previously evaluated for flattening filter-free therapy (and were found to be substantiallyless important) (Kry et al 2007a, 2008).
Stray photon dose following flattening filter removal 2157
2. Methods and materials
2.1. Monte Carlo model
A detailed model of a Varian 2100 accelerator (Varian Medical Systems, Palo Alto, CA),including a Millennium 120-leaf multileaf collimator (MLC) (Ponisch et al 2006b) and headshielding, was previously developed in MCNPX (Hendricks et al 2004). The model simulatedelectrons of 6.2 MeV (6 MV) or 18.0 MeV (18 MV) striking the bremsstrahlung target, andtracked photons and electrons throughout the accelerator and phantom.
The Monte Carlo model was operated with the flattening filter present (FF mode) andwith the flattening filter absent (flattening-filter free (FFF) mode). At 18 MV, the flatteningfilter was completely removed in the FFF mode, while at 6 MV a 2 mm thick copper plate,which was necessary to eliminate electrons penetrating the bremsstrahlung target (Titt et al2006a), was substituted for the flattening filter.
This model has been benchmarked against measurements with the flattening filter presentfor both 6 MV and 18 MV photon beams within the treatment field (Ponisch et al 2006b) aswell as outside the treatment field (Kry et al 2006, 2007b). Additionally, calculated doses havebeen found to agree with measurements, particularly in the field penumbra region, with theflattening filter removed, both at 6 MV and 18 MV (Ponisch et al 2006a). Due to this extensivebenchmarking, only minimal spot-checking measurements of the simulated data were includedin the current study. In particular, the out-of-field dose up to 50 cm from the central axis wasboth calculated and measured from a 10 × 10 cm2 open field using a 6 MV beam. Simulationsfollowed the methodology outlined in the following section, except that an acrylic phantomwas simulated. Measurements were made with thermoluminescent dosimeters (TLD-100;Harshaw) in an acrylic phantom, and the TLD were read by the Radiological Physics Center,which has an extensive history of TLD use (Kirby et al 1992).
2.2. Open fields
Irradiation of a large water tank (200 cm × 200 cm × 30 cm deep) at a 100 cm source-to-surface distance was simulated at both 6 MV and 18 MV in the FF and FFF modes. Forall four configurations, the photon dose was calculated by scoring electron energy deposition(type 1 electron pedep mesh tally (Hendricks et al 2004)) in the in-plane direction (patientsuperior–inferior). Four hundred million particle histories were run for each simulation, andweight windows were used to minimize uncertainties. Calculations were done for 4 × 4 cm2,10 × 10 cm2 and 15 × 15 cm2 fields, each defined by the MLC with the jaws positioned0.2 cm beyond the MLC edge.
The doses calculated with and without the flattening filter were normalized for each energyand field size so the same dose was delivered to the shoulder of the profile. Specifically, allprofiles were normalized at each depth examined to the dose at 0.4 cm inside the nominal fieldedge.
The sources of the out-of-field photon dose were also evaluated for the FF and FFFmodes from the 10 × 10 cm2 field. Specifically, the total out-of-field dose (T) was divided intocollimator scatter (C), patient scatter (P) and head leakage (L) components using the followingrelationship and methodology:
T = C + P + L. (1)
The total out-of-field dose, T, was calculated as detailed in the previous paragraph except thatphoton kerma was tallied to reduce statistical uncertainties. The head leakage component,L, was calculated by repeating this simulation but killing (i.e. removing from the simulation)
2158 S F Kry et al
1.E+00
1.E+01
1.E+02
1.E+03
1.E+04
1.E+05
0 10 20 30 40 50 60
Distance from isocenter (cm)
Do
se/M
U (
µGy)
Measured
Calculated
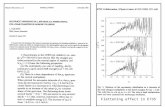
Figure 1. Measured and calculated out-of-field dose (μGy/MU) as a function of distance fromthe central axis. The treatment field was a 10 × 10 cm2 open FFF field at 6 MV.
all particles that exited the opening of the MLC (thereby removing all collimator scattersand patient scatters). The combination of collimator scatter and leakage components(L + C) was calculated next by repeating the initial simulation a third time but killing allparticles that struck the surface of the water tank within the primary field (thereby removingall patient scatters). The C, P and L components of equation (1) at each location could thenbe individually determined based on knowledge of T, L and L + C.
2.3. Clinical treatment
The out-of-field dose from IMRT prostate therapy at 6 MV was evaluated with the flatteningfilter present and absent. This was done using an FF and an FFF treatment plan developedin Eclipse v8.0 (Varian Medical Systems) following clinical planning guidelines (eight-fieldstep-and-shoot technique). Planning procedures for IMRT of the prostate with and withoutthe flattening filter have been previously outlined (Vassiliev et al 2007a). Each plan offeredcomparable prostate coverage and sparing of the bladder, rectum and femoral heads. Theplan was developed for an anthropomorphic Rando phantom (Radiology Support DevicesInc., Long Beach, CA) that underwent a full-body computed tomography (CT) scan and forwhich major organs were previously contoured (Kry et al 2005a). The CT image of the Randophantom was converted to MCNPX format using Scan2MCNP (White Rock Science, LosAlamos, NM). The dose in the phantom was calculated from the simulated IMRT treatmentsat 64 locations throughout the phantom, including locations in the prostate, testes, colon,stomach, liver, esophagus, lungs, heart and thyroid.
3. Results
3.1. Benchmarking
Measured and calculated doses outside of the treatment field are shown in figure 1 for an FFFbeam. Very good agreement was observed; in examining the local percent difference, theaverage magnitude of the difference between measurement and calculation was <9%. Thisagreement is very similar to what was observed with the flattening filter in place (Kry et al2006), and confirms the accuracy of the simulations.
Stray photon dose following flattening filter removal 2159
10x10 Field at5 and 15 cm depths
1.E-10
1.E-09
1.E-08
1.E-07
1.E-06
1.E-05
-50 -30 -10 10 30 50
Distance from Central Axis (cm)
Dose
(A
U)
5 cm FFF
5 cm FF
15 cm FFF
15 cm FF
Figure 2. Dose (in arbitrary units) from a 6 MV, 10 × 10 cm2 open field at 5 cm and 15 cm depthsin water. Fields used flattening-filter (FF) or flattening-filter-free (FFF) mode, and the relative dosefrom each mode was normalized at each depth to be equivalent at the shoulder of the primary field.
6 MV4x4 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose R
atio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 3. Ratio of FFF/FF dose as a function of distance from the edge of a 4 × 4 cm2 open fieldat 6 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
3.2. Open fields
The doses as a function of distance from the central axis from flattening-filter and flattening-filter-free 6 MV beams are shown in figure 2 for a 10 × 10 cm2 open field at 5 cm and15 cm depths in water. The curves are normalized at the shoulder for each depth and showcomparable out-of-field doses for both beams near the treatment field but lower doses from theFFF beam at increasing distances from the treatment field. The difference between out-of-fielddoses in the FF and FFF modes is examined in more detail in figures 3–5, in which the ratioof the FFF to FF doses is shown for 4 × 4 cm2, 10 × 10 cm2 and 15 × 15 cm2 fields. For eachfield size, the dose ratio is shown as a function of distance from the edge of the treatment fieldat 5 cm and 15 cm depths in water.
Several trends are apparent for all field sizes and both depths. Within a fewcm (∼ <3 cm) of the edge of the treatment field, the dose is lower in the FFF mode than inthe FF mode. At distances between approximately 3 cm and 15 cm from the edge of the field,the dose is typically higher in the FFF mode. At distances beyond approximately 15 cm from
2160 S F Kry et al
6 MV10x10 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose
Ratio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 4. Ratio of FFF/FF dose as a function of distance from the edge of a 10 × 10 cm2 openfield at 6 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
6 MV15x15 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose R
atio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 5. Ratio of FFF/FF dose as a function of distance from the edge of a 15 × 15 cm2 openfield at 6 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
the edge of the field, the dose tends to be lower for the FFF mode, although the effect dependson the field size and depth. The out-of-field dose from the FFF beam is only half that of the FFbeam from the 4 × 4 cm2 field at these greater distances. As field size increased, the relativeFFF dose tended to increase, particularly far from the treatment field. That is, the ability ofthe FFF beam to reduce the out-of-field dose was less for larger fields. This was also observedto be the case as depth increased. In summary, the FFF beam, as compared to the FF beam,was most advantageous (i.e. conferred the least dose) at distances farther from the treatmentfield, for smaller fields and at shallower depths.
Similar data are presented in figures 6–9 for FF and FFF 18 MV beams. In figure 6, thephoton doses from a 10 × 10 cm2 field are shown as a function of distance from the centralaxis at 5 cm and 15 cm depths in water. The FFF-to-FF dose ratios are shown in figures 7–9for 4 × 4 cm2, 10 × 10 cm2 and 15 × 15 cm2 fields as a function of distance from the fieldedge. The FFF beam reduced the out-of-field dose more at 18 MV than at 6 MV. At 18 MV,similar to 6 MV, the FFF dose was less than the FF dose very near to the field, but could begreater than the FF dose at distances of 3–15 cm from the field edge, and was then much lessthan the FF dose at greater distances. Also similar to the 6 MV beams, the out-of-field doses
Stray photon dose following flattening filter removal 2161
10x10 Field at5 and 15 cm depths
1.E-09
1.E-08
1.E-07
1.E-06
1.E-05
1.E-04
-50 -30 -10 10 30 50
Distance from Central Axis (cm)
Do
se
(A
U)
5 cm FFF
5 cm FF
15 cm FFF
15 cm FF
Figure 6. Photon dose (in arbitrary units) from an 18 MV, 10 × 10 cm2 field at 5 cm and15 cm depths in water. Fields used flattening-filter (FF) or flattening-filter-free (FFF) mode, andthe relative dose from each mode was normalized at each depth to be equivalent at the shoulder ofthe primary field.
18 MV4x4 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose R
atio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 7. Ratio of FFF/FF photon dose as a function of distance from the edge of a 4 × 4 cm2
open field at 18 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
at 18 MV were most reduced with the FFF mode for smaller fields, greater distances from thefield edge and shallower depths, where the FFF dose could be less than half that of the FFmode.
The composition of the out-of-field dose is shown in figure 10 for the FF and FFF modesat 5 cm depth from the 10 × 10 cm2 field. With the flattening filter removed, the head leakagewas substantially reduced as compared to when the filter was in place. Similarly, with theflattening filter removed, the collimator scatter was reduced, particularly very close to the fieldedge. Countering these benefits, patient scatter was increased. Even though patient scatter wasnot drastically increased, it comprises a large fraction of the total out-of-field dose, particularlyclose to the treatment field, and therefore has a large impact on the total out-of-field dose.
2162 S F Kry et al
18 MV10x10 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose R
atio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 8. Ratio of FFF/FF photon dose as a function of distance from the edge of a 10 × 10 cm2
open field at 18 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
18 MV15x15 Field
0.00
0.25
0.50
0.75
1.00
1.25
0 15 30 45
Distance from Field Edge (cm)
Dose R
atio
(FF
F/F
F)
5 cm depth
15 cm depth
Figure 9. Ratio of FFF/FF photon dose as a function of distance from the edge of a 15 × 15 cm2
open field at 18 MV. The dose ratio is shown at both 5 cm depth and 15 cm depth.
3.3. Clinical treatment
The out-of-field photon doses from prostate IMRT at 6 MV are shown as a function of distancefrom the central axis in figure 11. Near to the treatment field (within 15 cm from the centralaxis) the FF and FFF doses were comparable, with the FFF dose being slightly lower thanthe FF dose (between 90% and 102% of the FF dose). Farther away from the treatment field,the dose from the FFF treatment became markedly less than that from the FF treatment. Atdistances beyond 20 cm from the central axis the dose was, on average, 30% less with the filterremoved. For this clinical case, the out-of-field doses were typically more reduced than theywere for an open field of comparable size because of beam modulation as discussed below.
4. Discussion
Our work found that removing the flattening filter typically reduced the out-of-field dose bothvery close to and far from the edge of the treatment field (<3 cm and >15 cm). However,
Stray photon dose following flattening filter removal 2163
1.E-05
1.E-04
1.E-03
1.E-02
1.E-01
1.E+00
0 10 20 30 40 50
Distance from field edge (cm)
Do
se (
A.U
.)
T FF T FFF
L FF L FFF
C FF C FFF
P FF P FFF
Figure 10. Composition of a 10 × 10 cm2 field at 6 MV with the flattening filter (FF; solid line)and without it (FFF; dashed line). Total out-of-field dose (T) is divided into patient scatter (P),collimator scatter (C) and head leakage (L) components.
10
100
1000
10000
0 10 20 30 40 50 60
Distance from Central Axis (cm)
Dose (
mG
y)
FF
FFF
Figure 11. Out-of-field dose from a complete course of IMRT to the prostate using 6 MV beamswith the flattening filter (FF) and without the flattening filter (FFF).
between these distances, the dose was often higher with the flattening filter removed. Thesetrends in the out-of-field dose may be understood in terms of head leakage, collimator scatterand patient scatter. When the flattening filter was removed, a source of scatter in the acceleratorhead was removed, decreasing the amount of collimator scatter and reducing the out-of-fielddose very near the treatment field. However, at distances between 3 cm and 15 cm from thefield edge, the dose was often greater when the filter was removed due to increased patientscatter as the unflattened photon beam has a lower average energy (Vassiliev et al 2006b)and, therefore, a higher propensity for scattering. At distances farther from the treatment field(>15 cm) where head leakage begins to dominate the out-of-field dose, the dose was muchlower with the FFF beam. This occurs with the flattening filter removed because the deliveryefficiency is increased as the primary photon beam is no longer attenuated by the flatteningfilter. Less target current is required to deliver a given dose (Vassiliev et al 2006a); thus, headleakage is reduced.
2164 S F Kry et al
The reduction in the out-of-field photon dose was more pronounced with smaller fieldsthan with larger. This resulted from two factors. First, smaller fields have less patient scatterrelative to head leakage, and the FFF modality has an advantage in terms of head leakagebut a disadvantage in terms of patient scatter. Therefore, the advantage of the FFF beam willbe maximized in smaller treatment fields. Second, with smaller fields the primary beam isdelivered through the thickest portion of the flattening filter; the delivery of such a small fieldwas much more efficient with the filter removed and head leakage was correspondingly reducedby a substantial amount. In contrast, with larger fields, the flattening filter is much thinner atthe edge of the treatment field (where the open fields were normalized). Consequently, withthe flattening filter removed, there was less of an increase in treatment delivery efficiency.Correspondingly, there was a smaller reduction in head leakage.
The reduction in the out-of-field dose was also a slight function of depth. At deeperdepths, patient scatter has been shown to play a more dominant role (Kase et al 1983). As theFFF modality produces more patient scatter than the FF mode, the FFF mode is less beneficialat 15 cm depth as compared to 5 cm depth.
Based on the results of the open fields, the results from the IMRT cases are reasonable.That is, doses were comparable near to the treatment field, but were reduced in the FFF modefar from the treatment field. The reduction in the out-of-field dose was greater for the clinicalIMRT case than for the square fields. This is because the out-of-field dose also depends on themodulation of the treatment field during IMRT. Increased treatment-field modulation increaseshead leakage while not largely affecting patient scatter. Increased importance of head leakageis a situation that favors the flattening filter-free machine. FFF therapy would therefore bebest at reducing the out-of-field dose for highly modulated treatments.
The statistical uncertainties associated with the Monte Carlo calculations were, on average,3%, but could exceed 10% in individual tally voxels with very low doses. The uncertainty inthe dose ratio, in particular, could therefore be substantial at large distances from the treatmentfield. However, based on multiple data points shown in the figures, the trends in the dataare nevertheless clear. Furthermore, Monte Carlo modeling inaccuracies are believed to benegligible when comparing FF to FFF fields or treatments as the only difference betweenthese models is the presence of the flattening filter. This particular component is among themost accurately modeled and has been previously shown to produce accurate in-field dosecharacteristics (Ponisch et al 2006b).
The trend we observed in the out-of-field photon dose from FFF therapy was generallyconsistent with that measured previously by O’Brien et al (1991) for stereotactic radiosurgeryat 6 MV with an AECL Therac-6 linac. They found a reduction in the out-of-field dose by17% near to the treatment field and 50% far from the treatment field. Compared to the IMRTtreatments examined in the current study, O’Brien et al (1991) measured a greater reductionin dose with the FFF mode. However, this discrepancy is reasonable considering the natureof their study that employed very small fields. Such fields maximize the benefit of FFF.
Although the out-of-field dose was often reduced through the removal of the flatteningfilter, examination of the large open field data (figures 5 and 9) indicates that the out-of-fielddose could easily be higher in the FFF mode. The FFF mode has an advantage over theFF mode when head leakage plays a large role relative to patient scatter. The optimal FFFtreatment for reducing the out-of-field dose as compared to an FF treatment would use smallfields, irradiate a site far from sensitive organs and employ highly modulated treatment fields.Sites such as the prostate, an extremity, or a stereotactic treatment will generally offer reducedout-of-field doses with the FFF mode. However, treatment of a site, such as the breast, withlarge fields, low modulation and an abundance of nearby sensitive organs, may not be a goodcandidate for FFF therapy in the context of reducing the out-of-field dose. When considering
Stray photon dose following flattening filter removal 2165
the risk of second cancers, reduced out-of-field doses must be evaluated relative to the locationof sensitive organs, particularly within 5 cm from the field edge where Diallo et al (2009)observed an abundance of second cancers to be induced.
5. Conclusions
The relative out-of-field photon dose from IMRT therapies delivered with, versus without, theflattening filter was found to depend on treatment parameters. Removal of the flattening filterreduced collimator scatter and head leakage but increased patient scatter. Consequently, theout-of-field dose was lower with the removal of the flattening filter for smaller fields, at greaterdistances from the treatment field and for more modulated treatment fields, but was higher forlarger, less modulated fields and at locations nearer to the treatment field.
For clinical treatments, delivery with a FFF linac may offer an advantage to the patient interms of the reduced out-of-field dose, and accordingly, reduced risk of secondary malignancyto these out-of-field organs. If reduction in the out-of-field dose is a motivating factor intreatment selection, it may be achieved with the FFF mode. However, this advantage must beverified and considered along with the proximity of second tumors to the treatment field (forexample, as located by Diallo et al (2009)).
References
Boice J D Jr et al 1985 Second cancers following radiation treatment for cervical cancer: an international collaborationamong cancer registries J. Natl Cancer Inst. 74 955–75
Brenner D J et al 2000 Second malignancies in prostate carcinoma patients after radiotherapy compared with surgeryCancer 88 398–406
Cashmore J 2008 The characterization of unflattened photon beams from a 6 MV linear accelerator Phys. Med.Biol. 53 1933–46
Cozzi L, Buffa F M and Fogliata A 2001 Dosimetric features of linac head and phantom scattered radiation outside theclinical photon beam: experimental measurements and comparison with treatment planning system calculationsRadiother. Oncol. 58 193–200
Diallo I et al 2009 Frequency distribution of second solid cancer locations in relation to the irradiated volume among115 patients treatment for childhood cancer Int. J. Radiat. Oncol. Biol. Phys. 74 876–83
Followill D, Geis P and Boyer A 1997 Estimates of whole-body dose equivalent produced by beam intensity modulatedconformal therapy Int. J. Radiat. Oncol. Biol. Phys. 38 667–72
Fu W, Dai J, Hu Y, Han D and Song Y 2004 Delivery time comparison for intensity-modulated radiation therapywith/without flattening filter: a planning study Phys. Med. Biol. 49 1535–47
Hall E J and Wuu C 2003 Radiation-induced second cancers: the impact of 3D-CRT and IMRT Int. J. Radiat. Oncol.Biol. Phys. 56 83–8
Hendricks J S et al 2004 MCNPX user’s manual, version 2.5e Report LA-UR-04-0569 (Los Alamos, NM: LosAlamos National Laboratory)
Howell R M, Hertel N E, Wang Z, Hutchinson J and Fullerton G D 2006 Calculation of effective dose frommeasurements of secondary neutron spectra and scattered photon dose from dynamic MLC IMRT for 6 MV,15 MV, and 18 MV beam energies Med. Phys. 33 360–8
Kase K R, Svensson G K, Wolbarst A B and Marks M A 1983 Measurements of dose from secondary radiationoutside a treatment field Int. J. Radiat. Oncol. Biol. Phys. 9 1177–83
Kirby T H, Hanson W F and Johnston D A 1992 Uncertainty analysis of absorbed dose calculations fromthermoluminescence dosimeters Med. Phys. 19 1427–33
Kragl G et al 2009 Dosimetric characteristics of 6 and 10 MV unflattened photon beams Radiother. Oncol. 93 141–6Kry S F et al 2005a Out-of-field photon and neutron dose equivalents from step-and-shoot intensity modulated
radiation therapy Int. J. Radiat. Oncol. Biol. Phys. 62 1204–16Kry S F et al 2005b The calculated risk of fatal secondary malignancies from intensity-modulated radiation therapy
Int. J. Radiat. Oncol. Biol. Phys. 62 1195–203Kry S F et al 2006 A Monte Carlo model for calculating out-of-field dose from a Varian 6-MV beam Med.
Phys. 33 4405–13
2166 S F Kry et al
Kry S F et al 2007a Reduced neutron production through use of a flattening filter free accelerator Int. J. Radiat. Oncol.Biol. Phys. 68 1260–4
Kry S F et al 2007b A Monte Carlo model for out-of-field dose calculation from high-energy photon therapy Med.Phys. 34 3489–99
Kry S F, Howell R M, Titt U, Salehpour M and Vassiliev O N 2008 Energy spectra, sources, and shieldingconsiderations for neutrons generated by a flattening filter-free Clinac Med. Phys. 35 1906–11
Mesbahi A 2007a Dosimetric characteristics of unflattened 6 MV photon beams of a clinical linear accelerator: aMonte Carlo study Appl. Radiat. Isot. 65 1029–36
Mesbahi A 2009 A Monte Carlo study on neutron and electron contamination of an unflattened 18-MV photon beamAppl. Radiat. Isot. 67 55–60
Mesbahi A, Mehnati P, Keshtkar A and Farahollahi A 2007b Dosimetric properties of a flattening filter-free 6-MVphoton beam: a Monte Carlo study Radiat. Med. 25 315–24
O’Brien P F, Gillies B A, Schwartz M, Young C and Davey P 1991 Radiosurgery with unflattened 6-MV photonbeams Med. Phys. 18 519–21
Ponisch F, Titt U, Kry S F, Vassiliev O N and Mohan R 2006a Properties of unflattened photon beams shaped by amulti-leaf collimator Med. Phys. 33 1738–46
Ponisch F, Titt U, Kry S F, Vassiliev O N and Mohan R 2006b MCNPX simulation of a multi-leaf collimator Med.Phys. 33 402–4
Preston D et al 2003 Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer diseasemortality: 1950–1997 Radiat. Res. 160 381–407
Reft C S, Runkel-Muller R and Myrianthopoulos L 2006 In vivo and phantom measurements of the secondary photonand neutron doses for prostate patients undergoing 18 MV IMRT Med. Phys. 33 3734–42
Ron E 2003 Cancer risks from medical radiation Health Phys. 85 47–59Stathakis S, Esquivel C, Butierrez A, Buckey C R and Papanikolaou N 2009 Treatment planning and delivery of
IMRT using 6 and 18 MV photon beams without flattening filter Appl. Radiat. Isot. 67 1629–37Stovall M et al 1995 Fetal dose from radiotherapy with photon beams: report of AAPM Radiation Therapy Committee
Task Group No. 36 Med. Phys. 22 63–82Titt U et al 2006a A flattening filter free photon treatment concept evaluation with Monte Carlo Med.
Phys. 33 1595–602Titt U, Vassiliev O N, Ponisch F, Kry S F and Mohan R 2006b Monte Carlo study of backscatter in a flattening filter
free clinical accelerator Med. Phys. 33 3270–3Van Der Giessen P 1996 A simple and generally applicable method to estimate the peripheral dose in radiation
teletherapy with high energy x-rays or gamma radiation Int. J. Radiat. Oncol. Biol. Phys. 35 1059–68Vassiliev O N et al 2006a Dosimetric properties of photon beams from a flattening filter free clinical accelerator Phys.
Med. Biol. 51 1907–17Vassiliev O N et al 2006b Monte Carlo study of photon fields from a flattening filter free clinical accelerator Med.
Phys. 33 820–7Vassiliev O N et al 2007a Treatment planning study of prostate cancer intensity-modulated radiotherapy with a Varian
Clinac operated without a flattening filter Int. J. Radiat. Oncol. Biol. Phys. 68 1567–71Vassiliev O N et al 2009 Stereotactic radiotherapy for lung cancer using a flattening filter free accelerator J. Appl.
Clin. Med. Phys. 10 14–21Vassiliev O N, Titt U, Kry S F, Mohan R and Gillin M T 2007b Radiation safety survey on a flattening filter-free
medical accelerator Radiat. Prot. Dosim. 124 187–90