Oral habits final
-
Upload
shekhar-star -
Category
Education
-
view
197 -
download
6
Transcript of Oral habits final
ORAL HABITS
GUIDED BY,Dr. Deepika Kapoor
Department of Pediatric and Preventive DentistryCollege of Medical Sciences and Teaching HospitalBharatpur-10, Chitwan
PRESENTED BY,Sangeet Pant
Roll no. 28BDS 4th year
CONTENTS Introduction Definitions Classifications Thumb sucking Mouth breathing Tongue thrusting Bruxism Lip habits Cheek biting Nail biting Masochistic habits Conclusion References
INTRODUCTION
• Repetitive behaviours are common during childhood. Most of them are benign and self-limiting. These responses are very essential for survival of an infant and to explore the world around him/her.
• Oral habits may be a part of normal development, a symptom of deep rooted psychological basis or may be the result of abnormal facial growth.
• Digit sucking, mouth breathing, tongue thrusting, lip and nail biting, bruxism, etc may be considered as some of the common oral habits seen in children.
• These habits bring about harmful unbalanced pressures to bear upon the immature, highly malleable alveolar ridges, the potential changes in positions of teeth, and occlusion.
• One of the most valuable services that can be rendered as part of the interceptive orthodontic procedures is elimination of the abnormal habits before they can cause any damage to the developing dentition.
DEFINITIONSAccording to Boucher DC(1974):
“Habit is a tendency towards an act or an act that has become a repeated performance, relatively fixed, consistent, easy to perform and almost automatic.”
Acc. to Moyers:“ Habits are learned patterns of muscle contraction, which
are complex in nature.”
Acc. to Finn(1972):“Habit is an act, which is socially unacceptable.”
According to Dorland(1957):“Habit is a fixed or constant practice established by
frequent repetition.”
According to Buttersworth(1961):Habit is a frequent or constant practice or acquired
tendency, which has been fixed by frequent repitition.”
According to Mathewson(1982):“Oral habits are learned patterns of muscle contractions”
CLASSIFICATIONOral Habits
Obsessive(deep rooted)
Intentional or meaningful habits
E.g.: nail biting, digit sucking, lip biting
Masochistic or self-inflicting injurious
habitsE.g.: Gingival stripping
Non-obsessive(easily learned and
dropped)
Un-intentional or empty habits
E.g.: abnormal pillowing, chin
propping
Functional habitsE.g.: mouth breathing,
tongue thrusting, bruxism
CLASSIFICATIONBY WILLIAM JAMES(1923)a. Useful habits- e.g. nasal breathing
b. Harmful habits- e.g. mouth breathing
BY MORRIS AND BOHANA(1969)Pressure habits- Eg. Lip sucking, thumb and digit sucking.
Non-pressure habits- eg.mouth breathing.
Biting habit- Eg. Nail biting.
BY KINGSLEY (1958)-a) Functional oral habits- eg. Mouth breathingb) Muscular habit- eg.tongue thrustingc) Combined muscular habits- eg. Thumb and finger sucking.d) Postural habits- eg chin propping, face leaning on hand, abnormal
pillowing.
BY EARNEST KLEIN(1971)a. Intentional habits (meaningful habits)- has a definite underlying psychological disturbances.
b. Unintentional habits (empty habits)- a meaningless habit that has no need for support, they can be easily treated by reminder appliance.
BY SYDNEY FINN(1987)a) Non-compulsive habit: Habits which are easily added or dropped from the child’s behavior pattern as he/she matures.
b) Compulsive habit: It has acquired a fixation in the child to the extent that he retreats to the practice of this habit whenever his security is threatened by events which occur in his world and express a deep seated emotional need.
ACCORDING TO THE CAUSE OF THE HABIT1. Physiologic habits- eg. Nasal breathing, suckling during infancy.
2. Pathologic habits- eg. Mouth breathing.
By GraberGraber included all habits under extrinsic factors of general causes of malocclusion. These are:• Thumb/digit sucking.• Tongue thrusting.• Lip/nail biting/ bobby pin opening.• Mouth breathing.• Abnormal swallowing.• Speech defects.• Postural defects.• Bruxism.• Defective occlusal habits.
Based on the origin of the habit1. Retained habit- those that are carried over from childhood to adulthood.
2. Cultivated habit- those that are cultivated during associative life of an individual.
GENERAL CONSIDERATIONSFactors influencing dento-alveolar skeletal deformation:1. Frequency: more the child indulges his habit each day, more
the deformation.
2. Duration: longer the child performs the habit, greater the deformation.
3. Intensity: more the force applied, more the deformity.
4. Direction and type: deformity results due to the force vector applied to the bone.
BUCCINATOR MECHANISM• Starting with the decussating fibers of the orbicularis oris muscle, joining
right and left fibers in the lips, the buccinator mechanism runs laterally and posteriorly around the corner of the mouth, joining other fibers of the buccinators muscle which insert into the pterygomandibular raphe just behind the dentition.
• Opposing the buccinator mechanism is a very powerful muscle the tongue.
FUNCTIONAL EQUILIBRIUM• There should be a balance between the forces of the tongue from within the
dental arches and compensating action of the lips and cheek musculature.• Balance between these muscle forces is very important. Any deviation in
these reflexes or mechanism leads to malocclusion.
• Oral habits may not only have deleterious effects on the dentition and orofacial structures.
• There may be more than malocclusion or “age inappropriate” behavior problems.
• So inter-disciplinary approach of treatment may be required.
DEVELOPMENT OF HABIT
• At birth the neonate’s survival depends on instinctive sucking when lips and tongue are stimulated. Soon after, the mouth is used as the primary device for exploring the environment.
• The neonates inherit some instincts which are composed of elementary reflexes.
• An instinct is one where the pattern and order are inherited, while in habit the pattern and order are acquired, if constantly repeated during the lifetime of an individual.
• The development of oral habit is divided into 3 periods by Massler M (1983):– Sucking period.– Transitional period.– Biting period.
• The sucking period develops while the baby is still in the 3rd trimester in its mother’s womb. This system is the most perfectly developed system found at the time of birth so that the oral phase of a newborn is well fulfilled.
• The transition from sucking period to biting period happens in a short period called the transition period.
• The biting period develops during the pre-school age (4-5 years) and reaches a peak in school age (6-12 years).
MATURATION OF ORAL FUNCTION• The principal physiologic functions of the oral cavity are
respiration, swallowing, mastication and speech.• Respiratory needs are a primary determinant of posture of
the mandible and tongue.• At birth, if the newborn infant is to survive, an airway must
be established within a very few minutes and must be maintained thereafter.
• To open the airway, the mandible must be positioned downward and the tongue moved downward and forward away from the posterior pharyngeal wall. This allows air to be moved through the nose and across the pharynx into the lungs.
• At all times during life, respiratory needs can alter the postural basis from which oral activities begin.
• Once an airway has been established, the newborn infant's next physiologic priority is to obtain milk and transfer it into the gastrointestinal system. This is accomplished by two maneuvers: suckling and swallowing (infantile).
• Respiratory and swallowing movements and activities have been noted in utero.
• The infant exhibits two reflexes at birth that are related to sucking:– Rooting reflex- lasts until 7 months of age.– Suckling reflex- lasts until 12 months of age.
• The suckling reflex and the infantile swallow normally disappear during the 1st year of life.
• As the child grows and motor skills develop, there is improved motor control of the tongue and oral musculature.
• There appears to be gradient of oral function maturation from anterior to posterior. At birth, the lips are relatively mature and capable of vigorous suckling activity, whereas more posterior structures are quite immature. As time passes, greater activity by the posterior parts of the tongue and more complex motions of the pharyngeal structures are required.
• This principle of front-to-back maturation is particularly well illustrated by the acquisition of speech. The first speech sounds are the bilabial sounds /m/ , /p/ , and /b/-which is why an infant's first word is likely to be "mama" or "papa’‘.
• Somewhat later, the tongue tip consonants like /t/ and /d/ appear. The sibilant /s/ and /z/ sounds, which require that the tongue tip be placed close to but not against the palate, come later still, and the last speech sound, /r/, which requires precise positioning of the posterior tongue, often is not acquired until age 4 or 5.
• Infants develop the ability to control a bolus with lateral and anteroposterior movements. This helps to handle changes in the consistency of the diet and enables to control a bolus of food with increased skill.
• The transition from infantile to adult swallow is gradual and demonstrates characteristics of both; lip contraction and tongue placement against the roof of the mouth which may or may not be present. The transitional swallow may be seen in 3 to 10 years old children.
SUCKING HABITS
• There are essentially two forms of sucking (O’Brien et al, 1996):– Nutritive form.– Non-nutritive form.
• Non-nutritive sucking is considered normal for children during infancy.
• The most common form is thumb or digit sucking. Since mouth is the source of communication with outer environment, this gives the infant a feeling of warmth, a glow, a sense of satisfaction or euphoria.
• As other avenues of communication with outside world develop like visual and auditory system, the euphoria induced by the oral activity assumes less importance.
• The non-nutritive sucking habits spontaneously disappear sometimes between the 6th and 18th months of life. In some children these habits may be normal for at least another year or so.
• The oral habits detected at age of 3-6 years old are an important issue because after this age the oral habits are considered as abnormal.
NUTRITIVE SUCKING• Breast feeding and bottle feeding are the nutritive sucking habits that
provides essential nutrients.
BREAST FEEDING• Natural breast feeding is performed through enormous muscular effort.
The newborn is forced to bite, advance and retract the mandible, which helps in the development of the entire muscular system.
• Breast feeding is more than the mere nutrition provider; it is primordial factor in the correct maturation and growth of the stomatognathic system and its functions.
• Therefore, breast feeding is the best orthopedic appliance one can offer an adult’s face in terms of harmonious development.
• The milk glands are surrounded by smooth muscles, which contract to force out the milk. To obtain milk, the infant does not have to suck it from the mother’s breast and probably could not do so.
• Instead, the infant’s role is to stimulate the smooth muscle to contract and squirt milk into the mouth.
• This is done by suckling, consisting of small nibbing movements of the lips, a reflex action in infants.
• When the milk is squirted into the mouth, it is only necessary for the infant to groove the tongue and allow the milk to flow posteriorly into the pharynx and esophagus.
• The tongue, however, must be placed anteriorly in contact with the lower lip, so that the milk is in fact deposited on the tongue. The sequence of events defines an infantile swallow.
BOTTLE FEEDING• The effects of bottle feeding on dentofacial development vary according to
the types of nipples used.• When a non-physiologically designed nipple (conventional nipple) is used,
the end of the nipple is almost against the pharyngeal wall.• The liquid is then released almost directly into the digestive tract, decreasing
the period of predigestion.• The flow of milk may be too rapid due to large openings or more openings.• So, the infant will either force the nipple out or regulate or stop the flow with
tip of his tongue.• Thus certain muscles involved in breastfeeding are either immobilized
(orbicularis oris, masseter); overactive (chin muscles) or malpositioned (tongue pushed backward) and may produce an abnormal dentofacial development.
• In a physiologically designed nipples (orthodontic nipples) there is a forward movement of the tongue under the flat surface the nipple that draws it backward and upward against the hard palate of the infant.
• So, the child has to work and exercise the lower jaw.• The posterior part of tongue then pushes milk down into the
esophageal area.• The milk flows due to peristaltic like action of the tongue and
the cheeks.• The flat shape of the nipple also improves the labial seal.• It seems better adapted to the anatomy and physiology of
sucking.
SUCKING VS SUCKLING
Suckling from breast• Active process is required.• Requires participation of both
mother and infant.• Creates hermetically sealed, negative
pressure chamber within the mouth.Positions and stabilizes nipple centrally, draws tongue under mother’s lactiferous sinuses.• Peristaltic action of tongue propels
milk back to posterior pharynx.• Soft palate rises, closing off airway
during swallowing.
Feeding from bottle (sucking)• More passive activity.• Not dependent on the mother.
• Creates a partial neutral pressure vacuum within the mouth.
Rubber nipple fills the mouth, milk flows into the mouth without tongue action, even if lips are not sealed around the nipple.• Much of peristaltic tongue action is
prevented.• Less effective elevation of soft palate;
greater risk of aspiration.
NON-NUTRITIVE SUCKING• Non-nutritive sucking may be defined as the sucking of an
object (digit or pacifier) not related to the ingestion of nutrients.
• Non-nutritive sucking is considered normal for children during infancy.
• The most common form is thumb or digit sucking. Since mouth is the source of communication with outer environment, this gives the infant a feeling of warmth, a glow, a sense of satisfaction or euphoria.
• Persistence of the habit beyond the age of 4 years may be referred to as a chronic non-nutritive sucking habit.
PACIFIERS (DUMMIES/SOOTHERS/ARTIFICIAL TEATS)• Pacifiers are introduced by parents to calm the child
every time the child is irritated, and the child develops a strong attachment to the sucking object.
• The shield of the conventional pacifier has a convex curvature and the nipple has a “cherry-like” shape and thicker.
• The shield of physiologic pacifier has a concave curvature that is more suitable to the child’s face and its shape better fits the child’s oral structure.
• Zardetto et al pointed out that more occlusal and oral myofunctional alterations were detected among children who had pacifier habits compared to those with no sucking habit.
• Children were more likely to show open bite, posterior crossbite, increased overjet, and alteration in cheek mobility.
• The alterations on the primary dentition most frequently found are: anterior openbite, posterior crossbite, decrease of upper intercanine width and increased overjet.
• Oral myofunctional alterations associated are lip incompetence, lip entrapment, decrease in muscular tonicity of tongue and lips, and narrow hard palate.
PACIFIER USE AND SUDDEN INFANT DEATH SYNDROME• Sudden infant death syndrome (SIDS) is defined as “the sudden
death of an infant under 1 year of age which remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene, and review of the clinical history.” (Wimmger et al, 1991)
• Pacifier use has protective effects against SIDS:– Pacifier may keep the tongue in a more forward position, reducing the
possibility of airway occlusion, particularly in the supine position.– Pacifiers may prevent an infant from turning to a prone position,
keeping the infant’s nose off the bed.– Pacifiers may reduce the potential for gastroesophageal reflux.
ADVANTAGES OF PACIFIER SUCKING• Has a protective effect against SIDS.• Can provide comfort to the infants.• Can help to develop and strengthen the muscles used for
sucking in a preterm or recovering term infants.• Studies show that preterm infants allowed to suck on pacifier
had better weight gain and a reduced hospital stay.• Can prevent development of thumb sucking habit.• There is also evidence that coupling pacifier sucking with
gavage feeding leads the infant to associate satiety or fullness with sucking.
IF A PACIFIER IS GOING TO BE USED, IT IS IMPORTANT TO MAKE PARENTS AWARE OF THE FOLLOWING:• It should be sturdy one-piece construction.• It should have an easily grasped handle.• It should have a mouthgaurd of adequate diameter and with
ventilating holes.• It should not have any detectable strings or ribbons.• It should never be tied around a child’s neck or affixed with any
material capable of becoming wrapped around the neck.• It should be kept clean.• It should never be dipped in sugar or honey to encourage sucking.
THUMB SUCKING
• Thumb sucking is a form of non-nutritive sucking occurring as early as 29th week of gestation.
• It is commonly seen in infants and peaks 18-21 months of age.
DEFINITION• “Thumb sucking is the placement of thumb in varying depths
into the mouth.”
• Thumb sucking and finger sucking can more generally be termed as digit sucking.
THE SUCKING REFLEX• The process of sucking is a
reflex occurring in the oral stage of development and is seen even at 29 weeks of IUL, and may disappear during neonatal growth between the ages of 1 and 3.5 years.
• It is the first coordinated activity of the infant.
• It is important for meeting both psychological and nutritive needs during feeding.
• Two essential reflexes present at birth and related to this drive.– Sucking reflex (which remains until 12 months of age), and– The rooting reflex (which remains until 7 months of age) - the
movement of the infant’s head toward an object touching his/her cheek.
• Babies who are restricted from sucking due to a disease or other factors become restless and irritable.
• This deprivation may motivate the infant to suck the thumb or finger for additional gratification.
• If it continues beyond 3 years, malocclusion will result.
• The severity of the malocclusion depends on the intensity, frequency and duration of the habit.
• Clinical and experimental studies suggest that 4 to 6 hours of force per day is probably the minimum necessary to cause tooth movement.
• Therefore, a child who sucks intermittently with high intensity may not produce much tooth movement at all, whereas a child who sucks continuously for more than 6 hours can cause significant dental change.
THEORIESCLASSICAL FREUDIAN THEORY (1905)• It holds that this original response arises from an inherent psychosexual
drive suggesting that digit sucking is a pleasurable erotic stimulation of lips and mouth.
• That humans possess a biologic sucking drive.• A satisfying activity that gives the infant a feeling of well-being.• An infant associates sucking with pleasurable feelings such as hunger,
satiety and being held.• These events will be replaced in later life by transferring the sucking action
to the most suitable object available, namely thumb and finger.• If sucking continues beyond the oral phase, it becomes fixation.• Finger sucking at a later stage is usually considered a sign of regression.• Both fixation and regression are the signs of emotional disturbances.
THE LEARNING THEORY – DAVIDSON (1967)• Nonnutritive sucking stems from an adaptive response. • The infant associates sucking with such pleasurable feeling as
hunger. • These feelings are recalled by sucking the suitable objects
available mainly thumb or finger.• This theory suggests that sucking is an outlet for an excess
sucking urge because of efficient feeding either breast feeding by a nutritionally component mother or bottle feeding.
• When feeding is quickly and efficiently satisfied, the excess sucking urge expressed as non-nutritive sucking.
ORAL DRIVE THEORY – SEARS AND WISE (1982)• They suggested that the strength of oral drive is in
part a function of how long a child continues to feed by sucking.
• Thus, thumb sucking is the result of prolongation of nursing, and not the frustration of weaning.
• This theory agrees with Freud’s theory that the sucking increases the erotogenesis of the mouth.
COMBINATION OF PSYCHOANALYTIC AND LEARNING THEORY• By Eric Johnson and Brent Larson (1993)• According to them all children possess an inherent
biologic drive for sucking.• The rooting and placing reflexes are merely a means of
expression of this drive. • Environmental factors may also contribute to this
sucking drive to non nutritive sucking such as thumb or fingers.
BENJAMIN THEORY• He supported the psychoanalytic theory by
the observation of intrauterine sucking and by the neonatal reflex of rooting and placing.
• Rooting reflex consists of tilting the head towards the stimulus and opening the mouth.
• Placing is a subsequent contact between the mouth and the stimulus object.
MAINTENANCE OF THE HABIT
• Most children would cease digit sucking early in their developmental process by the age of 3 to 4 years.
• But an acute increase in the child’s level of stress or anxiety due to some underlying psychological or emotional disturbances can account for continuation of a digit sucking habit, with conversion of an empty habit into a meaningful stress reduction response.
CLASSIFICATION OF THUMB SUCKING
ACCORDING TO COOK (1995):1. α group: The thumb pushes the palate in a vertical direction and displays only little buccal wall contractions. Here the thumb applies pressure on the palate but sucking action is minimum or nil. Characteristic features, therefore, seen will be a deep palate with no posterior crossbite.
2. β group: Strong buccal wall contractions are seen and a negative pressure is created resulting in posterior crossbite.
3. γ group: Alternate positive and negative pressure iscreated. Posterior crossbite may be a feature in some cases depending on the frequency and duration of habit.
BASED ON CLINICAL OBSERVATION:• Normal Thumb Sucking:-during the first and second year
of life..• Abnormal Thumb Sucking:- habit persists beyond the
preschool periodThis can again be divided into:
(a) Psychological: The habit may have a deep-rooted emotional factor involved and may be associated with insecurities, neglect or loneliness experienced by the child.(b) Habitual: The habit does not have a psychological factor involved; however the child performs the act out of habit.
Level DescriptionLevel I (+/-) Boys or Girls of any chronological age with a habit that occurs
during sleep.Level II (+/-) Boys below age 8 with a habit that occurs at one setting during
waking hours.Level III (+/-) Boys under age 8 years with a habit that occurs at multiple
settings during waking hours.Level IV (+/-) Girls below age 8 or a boy over 8 years with a habit that occurs
at one setting during waking hours.Level V (+/-) Girls under age 8 years or a boy over age 8 years with a habit
that occurs across multiple settings during waking hours.Level VI (+/-) Girls over age 8 years with a habit during waking hours.
ACCORDING TO JOHNSON (1993) [Classified NNS based on factors that influence the severity of the habit]
(+/-) designates willingness of the parents to participate in treatment.
GRADING OF THUMB SUCKING BY SUBTELNY (1973)
TYPE A – (50%) whole digit is placed inside the
mouth with the pad of the thumb pressing over the palate
maxillary and mandibular anteriors contact is present.
TYPE B – (13-24% ) thumb is placed into the oral cavity
without touching the vault of the palate
maxillary and mandibular anteriors in contact.
TYPE C – (18% ) thumb is placed into the mouth just
beyond the first joint and contacts the hard palate and only the
maxillary incisors no contact with mandibular incisors.
TYPE D – (6%) very little portion of thumb is placed
into mouth.
PHASES OF DEVELOPMENT OF THUMB SUCKING HABIT BY MOYERS
PHASE-I: NORMAL AND SUBCLINICALLY SIGNIFICANT SUCKING:-• Extends from birth to 3 years.• This period is considered normal and does not
require any intervention.• It should be kept in mind that at the end of this
stage any vigorous thumb sucking may be carried into the next phase which then becomes abnormal. So preventive measures can be instituted.
PHASE-II: CLINICALLY SIGNIFICANT SUCKING – • Extends from 3 to 6-7 years.• It is associated with clinically significant sucking.• The habit may be meaningful or empty.• It is necessary to manage or correct the habit at this stage.
PHASE-III: INTRACTABLE SUCKING- • Thumb sucking habit persisting till phase-III.• May be a symptom more significant than associated
malocclusion.
HISTORY
• History regarding the frequency, intensity and duration of the habit.
• Remedies tried at home.• Feeding patterns.• Parental care of the child.• Presence of other habits.
EXTRAORAL EXAMINATION
DIGITS• Digits appear reddened,
exceptionally clean, chapped, with a short finger nail i.e. a clean 'dish pan thumb'.
• A chronic thumb sucker frequently has a fibrous, roughened callus on the superior aspect of the thumb.
• The habit is also known to cause deformation of the finger.
LIPS• Chronic thumb sucking
are frequently characterized by a short, hypotonic upper lip and hyperactive lower lip.
• Upper lip is passive or incompetent during swallowing.
FACIAL FORM ANALYSIS• Checked for mandibular retrusion, maxillary protrusion, high
mandibular plane angle and facial profile.– A straight profile indicates a favourable growth pattern and
the effects of the habit are self correcting when it ceases.– Convex profile is a class II growth pattern and the over jet
will remain inspite of removal of the habit.
INTRAORAL EXAMINATIONCOMMONLY OBSERVED CLINICAL PROBLEMS-
Maxillary anterior proclination and mandibular retroclination.• It is because when a child places
a thumb between the teeth, it is usually placed at an angle so that it presses lingually against the lower incisor and labially against the upper incisors.
Anterior open bite.• The digit impedes eruption
of the anterior teeth, while the posterior teeth are free to erupt.
• 1mm of elongation posteriorly opens the bite by about 2 mm.
Constriction of maxillary arch.• Failure of maxillary arch to develop
due to an alteration in the balance between cheek and tongue pressures as tongue position is lowered wen thumb is placed between the teeth.
• Cheek pressure increases against the teeth as the buccinator muscle contracts while sucking.
Posterior crossbite.• Occurs as a consequence of
constriction of the maxillary arch.
EFFECTS ON DENTOFACIAL STRUCTURES
ACCORDING TO JOHNSON AND LARSON (1993)• Effects on maxilla– Increased proclination of maxillary incisors.– Increased maxillary arch length.– Increased anterior placement of apical base of the maxilla.– Increased SNA.– Increased clinical crown length of the maxillary incisors.– Increased counter clockwise rotation of the occlusal plane.– Decreased SN to ANS –PNS angle.– Decreased palatal arch width.– Increased atypical root resorption in primary central
incisors.– Increased trauma to maxillary central incisors.
• Effects on the mandible– Increased retroclination of mandibular incisors.– Increased mandibular intermolar distance.– Increased distal position of B point.
• Effects on the Interarch Relationship– Decreased maxillary and mandibular incisor angle.– Increased overjet.– Decreased overbite.– Increased posterior crossbite.– Increased unilateral and bilateral class II occlusion.
• Effect on lip placement and function– Increased lip incompetence.– Increased lower lip function under maxillary incisors.
• Effects on tongue placement and function– Increased tongue thrust.– Increased lip to tongue resting position.– Increased lower tongue position.
• Other Effects– Risk to psychologic health.– Increased risk of poisoning.– Increased deformation of digits– Increased risk of speech defects, especially lisping.
PREVENTIONMOTIVE BASED APPROACH• The etiology of thumb sucking focuses on a predominant
psychological background.• Its prevention should be aimed towards the motive behind the
habit.• History serves as an important tool for diagnosing the etiology,
whether the habit is meaningful or empty.
CHILD’S ENGAGEMENT IN VARIOUS ACTIVITIES• Parents should be advised on keeping the child engaged in various
activities.• This gives a little time to practice the habit.
PARENTS INVOLVEMENT IN PREVENTION• When parents are at home they should be
advised to spend ample time with the child so as to put away his feeling of insecurity.
DURATION OF BREASTFEEDING• Duration of feeding should be adequate so as to
enable the child to exhaust his sucking urge and feel completely satisfied.
MOTHER’S PRESENCE AND ATTENTION DURING BOTTLE FEEDING• Bottle fed babies should be held by the mother and enough
attention should be given in the process.• This will promote a close emotional union between the
mother and the baby similar to that seen in breast feeding.
USE OF A PHYSIOLOGICAL NIPPLE• A physiological nipple should be used for bottle-feeding and
the size and number of the holes should be standardized to regulate a slow and steady flow of milk.
USE OF A DUMMY OR PACIFIER• Acquiring a digit sucking habit can be
prevented by encouraging the baby to suck a dummy instead.
• Dummies are easier to dispense with at an earlier age than is digit sucking.
TREATMENT CONSIDERATIONSTIMING• The proper timing of thumb sucking treatment is a matter of considerable
controversy.• Therapy should be postponed until the risks of the thumb sucking habit
outweigh the benefit to the patient.• It is reasonable to advise parents that the timing of thumb sucking therapy
depends on the risk profile of the habit.• In most cases, treatment for prolonged NNS habit should be initiated
between the age of four years and the eruption of the permanent incisors.
AGE FACTOR• 0-3 Years - No active intervention.• Between 3 to 6/7 years:- Active intervention of the habit. Give a detailed
explanation to the child & Parents.• 7 years and Older: - Orthodontic Intervention is needed.
PSYCHOLOGICAL STATUS OF THE CHILD• Inquire into the family status of the child• Parents are married/Single, lack of jobs, family stress, evidence of child
abuse etc• Events that precede the habit such as the dependency on a favourite toy,
problems with sleep, nightmares, nervousness and anxiousness • need for psychological consultation.
PARENTAL CONCERN REGARDING THE HABIT• advised to stop scolding, nagging• positive behavior is reinforced• Child should not be embarrassed or criticized rather help should be offered
to deal with this difficult habit.
FACTORS AFFECTING TREATMENT
DURATION OF HABIT• The older the patient, the more difficult it is to treat due
to longer duration of the habit practiced.
GENDER OF THE PATIENT• In general NNS habit is more severe in girls than in boys.
FREQUENCY OF THE HABIT• A habit generalized across multiple settings is more
difficult to treat than isolated at a specific time.
CONSCIOUS VERSUS UNCONSCIOUS• A conscious habit acquired through choice or need is
more complex and difficult to treat.
COOPERATION OF THE PARENTS AND OLDER SIBLINGS• A NNS habit maintained by some underlying psychological
disturbance is more difficult to treat than an empty habit.• A child may derive enjoyment from the habit and may be
unwilling to cooperate. They require more aggressive treatment.
COUNSELING
Best aimed at older children who can conceptually grasp the issue. Counseling with the patient on the basis of their maturity. Clinical photography and explanations with considerations of
physical appearance and social acceptance are provided as a motivational tool.
Dunlop’s Theory “Beta hypothesis” He believed that if a subject can be forced to concentrate on the performance
of the act at the time he practices it, he can learn to stop performing the act. Forced purposeful repetition of a habit eventually associates it with
unpleasant reactions and the habit is abandoned. The child should be asked to sit in front of a mirror and asked to suck his
thumb, observing him as he indulges in the habit.
REMINDER THERAPY• For those who desire to stop the habit but
need some help.• The reminder material immediately reminds
the child to remove the thumb from the mouth.
THERMOPLASTIC THUMB POST OR THUMB GUARD• Devised by Allen in 1991 where a
thermoplastic material is placed on the offending digit.
• A total of 6 weeks of treatment time is required for elimination of the habit.
ACE BANDAGE APPROACH• Nightly use of an elastic bandage
wrapped across the elbow.• Pressure exerted by the bandage
removes the digit from the mouth as the child tires and falls asleep.
CHEMICAL MEANS• Bitter and sour chemicals are
used over the thumb to terminate the practice.
• Quinine, asafetida, pepper, castor oil, femite, etc.
Three alarm system by Norton and Gellin1. Offending digit is taped and when child feels the tape in the
mouth it serves as the first alarm.2. Bandage tied on the elbow of the arm with the offending
digit, a safety pin is placed lengthwise. When child flexes the elbow the closed pin mildly jabs indicating a second alarm.
3. Bandage tightened if thumb sucking persists, serving as a third alarm.
REWARD SYSTEM
• For the child who is ready to quit the habit and just needs a reason to stop.
• Positive reinforcement may be a useful tool.• Posting a calender in noticeable location and keeping track of habit
free days can give the child sense of pride.• Praise from the parents and the dentist.• Discontinue the habit and receive a reward.
ADJUNCTIVE THERAPY/APPLIANCE THERAPY
• For more deeply ingrained habits or for patients who are more reluctant to let go of the habit.
• The appliances are not meant to be punitive.• It is preferable if the child expresses the desire to stop an oral
habit before initiating treatment.• Habit breaking appliances can be:
– Removable appliances.– Fixed appliances.
REMOVABLE APPLIANCES-• In children below age 6, where only
primary teeth are present, a removable appliance may not be well accepted because of the child’s immaturity.
• Clasps may be difficult to retain during mixed dentition period when the permanent molars are erupting.
• Easily misplaced or lost.• Patient compliance is a major factor.• But the advantage is that the child gets
freedom of wearing appliance only during critical period, such as night.
• Eg. Modified Hawley appliance, Removable palatal crib.
FIXED APPLIANCES-• It may cause a child to feel he is being
“punished”.• But has advantage that it is “cemented”
in place using a dental cement/adhesive so it does not rely on patient compliance.
• Eg. Hayrake appliance, Palatal crib, Quad helix, Bluegrass Appliance / Kentucky appliance.
VARIOUS HABIT BREAKING APPLIANCES ARE:Palatal crib-• The palatal crib is vertically disposed,
extending from the palatal region, completely encompassing the anterior openbite, and resting close to the gingival area lingual to the lower incisors when the posterior teeth are in occlusion.
• It serves as a complete mechanical barrier to the thumb or fingers.
Palatal crib
Rakes-• A rake is constructed as is the crib,
but has blunt tines or spurs projecting from the cross bars or acrylic retainer into the palatal vault.
• The tines discourage thumb sucking.• Disadvantage is that it acts more as
a punitive appliance rather than a reminder.
Rakes
Bluegrass appliance-• Haskell (1991) introduced this appliance, for
children with a continued thumb sucking habit.• It consists of a modified six-sided roller made of
Teflon to prevent injury to the tongue.• This is slipped over a 0.045’’ stainless steel wire
soldered to molar orthodontic bands.• This appliance is placed for 3-6 months.• Instructions are given to turn the roller instead
of sucking the digit.• Digit sucking is often seen to stop immediately.
Bluegrass Appliance
APPLIANCES USED FOR CORRECTION OF MALOCCLUSION DUE TO THUMB SUCKING• W-arch.• Quad helix.
W-arch Quad helix
INSTRUCTIONS GIVEN TO THE CHILD BEFORE GIVING APPLIANCE THERAPY
• There should be no mentioning about the habit. It should be told that it is a preventive measure to straighten the teeth.
• Difficulty in speech might occur for few days.• Might develop an imprint on the tongue that will
resolve when appliance is removed.• Follow up 3-4 week interval.• Assessment- check for the integrity of the appliance.• The appliance is usually worn for 4-6 months.
CURRENT STRATEGIES FOR THE TREATMENT
INCREASING THE ARM LENGTH OF THE NIGHT SUIT• For children who perform habit during
sleep.
THUMB-HOME CONCEPT• In this a small bag is given to the child to
tie around his wrist during sleep and it is explained to the child that just as the child sleeps in his home, the thumb will also sleep in its house and so the child is restrained from thumb sucking during night.
THUMB SUCKING BOOK• “The Little Bear Who Sucked His Thumb” is a book for
children written and illustrated by Dr. Dragan Antolos, an experienced dentist with a special interest in thumb sucking habit in children.
• The child relates to the story and delivers a positive message without pressure.
• It addresses the problem in fun and non-threatening way.
HAND PUPPETS
MOUTH BREATHING
• Nasal breathing is the primary mode of air intake for the humans, and it is essential for supply of properly cleansed, moistened and warmed air.
• The mouth is only a secondary emergency orifice for assuring an uninterrupted supply of air, and using it on regular basis can cause many problems.
• The term “nasal breather” is used to mean a person who breathes mostly through the nose except during exertion.
• Mouth breathers are those who breathe orally even in relaxed and restful situations.
• For normal dentofacial growth to occur there should be normal breathing.
• Mouth breathing can alter the equilibrium of pressures on the jaws and teeth and affect both jaw growth and tooth position.
DEFINTION • Sassouni(1971) :
Mouth breathing can be defined as habitual breathing through mouth instead of the nose.
• Merle(1980): Suggested the term oronasal breathing instead of mouth breathing.
• Chacker F M (1961):Defined mouth breathing as the prolonged or continued exposure of the tissues of the anterior area of the mouth to the drying effects of the inspired air.
CLASSIFICATION
Finn, 1987 Anatomic- Short upper lip does not permit complete
closure without undue effort.
Obstructive- Increased resistance or complete obstruction of normal flow of air through nasal passages.
Habitual- Breathing through mouth as a force of habit, even after the removal of abnormal obstruction.
ETIOLOGY
Increased resistance to the flow of air through the nasal passage may be considered the primary cause of mouth breathing.
Allergies, physical obstruction and chronic infections. Airway obstructions may be due to:
• Enlarged turbinates• Deviated nasal septum• Allergic rhinitis, nasal polyps• Enlarged adenoids or tonsils• Abnormally short upper lip preventing proper lip seal• Obstructive sleep apnea syndrome• Genetic predisposition• Thumb sucking or similar oral habits may be instigating agents.
CLINICAL FEATURES
• GENERAL EFFECTS– Appearance of pigeon chest.– Low grade esophagitis.– Blood gas constituents : Mouth breathers have 20% more
carbon dioxide and 20% less oxygen.
• EFFECTS ON DENTOFACIAL STRUCTURES Facial form:
Tendency towards more vertical growth pattern.Increased facial height.Increased mandibular plane angle.
Adenoid faciesLong narrow face.Narrow nose and nasal airway.Flaccid lips with short upper lip.Upturned nose exposing nares
frontally.‘V’ shaped and high palatal vault.Collapsed buccal segments of
maxilla.
Dental effectsProclined upper and lower incisors.Posterior cross bite.Tendency toward an open bite.Narrow palatal and cranial width(low set position of
tongue).Constricted maxillary arch(imbalance of forces exerted
by tongue and facial musculature).
Speech defects:Nasal tone in voice.
Lip Lip apart posture.Excessive appearance of maxillary anteriors- long face syndrome.Gummy smile.Short thick incompetent upper lip.Voluminous curled over lower lip.
External naresDisuse atrophy of the lateral nasal cartilage leading to slit like external nares with
narrow nose. Nasal mucosa becomes atrophied due to a disturbed ciliary action.
GingivaInflamed and irritating gingival tissue in the anterior maxillary arch.Hyperplastic gingiva due to continuous exposure to air drying.Heavy deposits of plaque due to decreases salivary cleansing action.Classic rolled margin and an enlarged inter dental papilla.Interproximal bone loss with presence of deep pockets.Chronic gingival condition and periodontal disease.
Other effectsOtitis media.Sense of smell and taste is decreased.
DIAGNOSIS• HISTORY • Parents should be questioned about the
Frequent lip apart posture.Frequent occurrence of tonsillitis, allergic rhinitis or otitis media.
• EXAMINATIONPatient’s breathing should be observed.Nasal breathers - lips touching lightly during relaxed breathing
whereas mouth breathers keep their lips apart.A mouth breather when asked to close his lips and take a forced deep
breath will not appreciably change the size and shape of the external nares and occasionally contracts the nasal orifices while inspiring.
CLINICAL TESTS1. Mirror test- Two-surfaced mirror is placed on the patient’s upper lip. If air condenses on upper side, the patient is a nasal breather and if it
condenses on lower side, the patient is mouth breather.
2. Butterfly test/cotton test- Take a few fibers of cotton (in butterfly shape) and place it just below
the nasal opening. On exhalation if the fibers of cotton flutter downwards, the patient is
nasal breather; otherwise the patient is mouth breather. This can also be used to determine unilateral nasal blockage.
3. Water holding test-Patient is asked to hold
water in mouth for 2-3 minutes.
A mouth breather cannot hold water for that time.
Cephalometrics - To establishAmount of nasopharyngeal spaceSize of adenoidSkeletal pattern of the patient
Inductive plethysmographry (Rhinomonometry) -To establish total air flow through nose and mouth
respectively.
Blood gas constituents-Mouth breathers have 20% more CO2 and 20% less
oxygen.
TREATMENT CONSIDERATIONS
• Age of child:Correction of mouth breathing could be expected to
decrease as the child matures.Increase in nasal passages and reduction in size of
tonsils as the child matures, thus relieving the obstruction.
• ENT Examination:To determine the condition requiring treatment
present in tonsils, adenoid or nasal septum.
CORRECTION OF MOUTH BREATHING
Symptomatic treatment:– Coating gingiva with petroleum jelly.– Clinically correcting periodontal defects occurred
due to the habit.
The treatment should be aimed at • Elimination of cause– Obstructive cause- treated surgically.– Allergic cause- prevention and control.
• Interception of the habit- Done if the habit continues even after the removal
after the cause.
ExercisesDeep breathing:
Done in morning and night .Deep inhalation through nose with arms raised sideways
and after a short period arms are dropped to the side and the air is exhaled through the mouth.
Lip exercises:Child is instructed to extend the upper
lip as far as possible to cover the vermillion border under and behind the maxillary incisors. This exercise is done for 15 to 30 mins per day for 4-5 months.
In case of protruded maxillary incisors, lower lip can be used to augment the upper lip exercise. The upper lip is first extended into the previously described position. The vermilion border of the lower lip is then placed against the outside of the extended upper lip and pressed as hard as possible against the upper lip.
Playing a wind instrumentCelluloid strip or metal disk held
between the lips.
To increase the tonicity of lips few myofunctional excercises are recommended:• Hold a sheet of paper between the lips.• Button pull exercise- a button is taken
and a thread is passed. Patient is asked to place the button behind the lips and pull the thread while restricting it from being pulled out by using lip pressure.
• Tug of war exercise- involves two buttons, with one placed behind the lips and other is pulled by the other person.
Maxillothorax myotherapy:• This was advocated by Macaray in 1960.• Used in conjunction with Macaray activator.• The stable aluminum activator is incorporated at the
angle of the mouth, with horizontal hooks to which expanding rubber bands are attached.
• The mouth breather holds the activator in the mouth and at the same time with the left and right arms alternately carries out 10 exercises thrice daily.
Oral screen Most effective way. Constructed with material compatible with oral tissues. The most
commonly utilized is synthetic resin. One must ascertain if the nasopharyngeal passage is sufficiently
patent to allow for exchange of air. If the child has no difficulty breathing through his nose and the
mouth breathing is habitual, it should be corrected by the use of oral screen.
In the initial phase windows are made in the oral screen so as not to completely block the airway passage.
The appliance is worn 2-3 hours during the day and when sleeping at night.
It prevents lip biters from placing the lower lip lingual to the upper incisors, tongue thrusters from forcing the tongue between the incisors, mouth breathers from breathing through mouth and thumb suckers from placing their fingers in the mouth.
It, therefore, serves a multiplicity of purposes.
• Correction of malocclusion-Mechanical appliances:Children with class I skeletal and
dental occlusion and anterior spacing- oral shield appliances.
Class II div I Dentition without crowding, age 5- 9 years- monobloc activator.
Class III malocclusion- Interceptive method like chin cap.
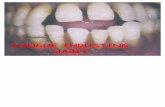
TONGUE THRUSTING
• In embryonic life, the developing tongue is considered disproportionately large in comparison to the developing mandible and it fills the embryonic oral cavity.
• In neonates the tongue is relatively large and located in the forward suckling position for nursing.
• The tip inserts through the anterior gum pads and assists in the anterior lip seal.
• This tongue position and coincident swallowing termed as infantile or visceral.
• With eruption of the incisors at about 6 months, the tongue position starts to retract.
• Over a period of 12 to 18 months as proprioception causes tongue postural and functional changes, a transitional period ensues.
• Between 2 and 4 years the functionally balanced, or mature, somatic swallow is in normal developmental patterns.
• Visceral swallow can persist well after the 4th year of life, however, it is considered dysfunctional or abnormal because of certain malocclusive characteristics.
• If the transition of infantile to mature swallow does not take place with the eruption of teeth, then it leads to what is known as the tongue thrust swallow.
• In normal swallower, the tip of the tongue contacts the palatal rugae area posterior to the maxillary anterior teeth; its midportion contacts the hard palate; its posterior aspect assumes a 45⁰ angulation against the pharyngeal wall to permit the bolus of food to move on into the digestive tract.
• Abnormal swallower is described as person who positions the tip of the tongue against or between the teeth during swallowing.
• Then the posterior aspect of the tongue contacts the posterior area of the hard palate and does not assume a 45⁰ angulation relative to the posterior pharyngeal wall.
• Masseter muscle activity is prevented and there is no molar contact during deglutition.
• Mentalis muscle is hyperactive.
MATURATION OF DEGLUTITION• The normal infantile swallow is seen in neonates and
gradually disappears with the eruption of the buccal teeth in primary dentition.
• The cessation of the infantile swallow and appearance of mature swallow are not a simple on-and-off phenomenon but elements of both intermix during the primary dentition and sometimes even into the early mixed dentition.
• The normal appearance of features of both the infantile and mature swallow is termed as “transitional swallow”.
• Diminishing of buccinators activity is part of the transitional period but the most characteristic feature of the start of cessation of infantile swallow is the appearance of contractions of the mandibular elevators during the swallow as they stabilize the teeth in occlusion.
• The arrival of the incisors leads to more precise opening and closing movements of the mandible, a more retracted tongue posture, and initiates the learning of mastication.
• As soon as bilateral posterior occlusion is established, a true chewing motions are seen to start and learning of the mature swallow begins.
• Gradually the 5th cranial nerve muscles assume the role of mandibular stabilization during the swallow, and the muscles of facial expression abandon suckling and infantile swallow and begin to learn the delicate and complicated functions of speech and facial expressions.
• The transition from infantile to mature swallow takes place over several months, aided by the maturation of neuromuscular elements, the appearance of upright head hence a change in the direction of gravitational forces on the mandible, the instinctive desire to chew, the necessity to handle textured food, dentitional development and so forth.
• The chewing pattern of the adult is quite different from that of a typical child.
• An adult typically opens straight down, then moves the jaw laterally and bring down the teeth into contact.
• Whereas a child moves the jaw laterally on opening.
• The transition from juvenile to adult pattern appears to develop in conjunction with eruption of the permanent canines at age 12.
• Adults who do not achieve normal function of the canine teeth because of a serious anterior open bite retain the juvenile chewing pattern.
NORMAL INFANTILE SWALLOW
• The jaws are apart, with the tongue between the gum pads.
• The mandible is stabilized primarily by the contraction of the muscles of the VIIth cranial nerve and the interposed tongue.
• The swallow is guided, and to a great extent controlled by sensory interchange between the lips and the tongue.
NORMAL MATURE SWALLOW• The teeth are together.• The mandible is stabilized by the contractions of the mandibular
elevators, which are primarily 5th cranial nerve muscles.• The tongue tip is held against the palate, above and behind the
incisors.• There is very little lip and cheek activity.• The amount of lip activity during the normal mature swallow
depends on the ability of the tongue to effect a complete valve seal against the teeth and alveolar process.
• During the mixed dentition, when some teeth are missing and there is normal interdental spacing, the lips may contract a bit to secure the seal
SIMPLE TONGUE THRUST SWALLOW
• It typically displays the contraction of lips, mentalis muscle and mandibular elevaters and the teeth are in occlusion as the tongue protrudes into an open bite
• There is a normal teeth together swallow,but a tongue thrust is present to seal the open bite
• The so called tongue thrust is simply an adaptive mechanism to maintaion an open bite created by something else, usually thumb sucking.
• The open bite is well circumscribed• When one fits together the dental cast of the patient they have a
precise and secure intercuspation because the occlusal position is continuously reinforced by the teeh together swallow
COMPLEX TONGUE THRUST SWALLOW
• It is tongue thrust with teeth apart swallow• The patient combines contraction of lip, facial and mentalis
muscles, lack of contraction of mandibular elevators, a tongue thrust between the teeth and teeth apart swallow
• Examination of dental cast typically reveals a poor occlusal fit and instability of intercuspation because the intercuspal position is not repeatedly reinforced during the swallow. Persistant teeth apart swallows don’t stabilize the occlusion
• They are far more likely to be the mouth breathers and to have incidence of complex tongue thrusting
• This type of tongue thrust doesn’t diminish as much with age as does the simple tongue thrust
RETAINED INFANTILE SWALLOW IN BEHAVIOUR
• True retained infantile swallowing behavior is rare.• It is defined as predominant persistent of the infantile swallowing
reflex after the arrival of permanent teeth• The patient demonstrate very strong contraction of the lips and
facial musculature• They present massive grimacing.• The tongue thrusts strongly between the teeth in front and on
both sides• Particularly noticeable are contraction of buccinators muslces • Such patients may have inexpressive faces since the 7th cranial
nerve, muscles are not being used for the delicated purpose of facial expression but rather for the massive effort of stabilizing the mandible swallowing.
Definition-• Barber(1975): Tongue thrust is an oral habit pattern related to the
persistence of an infantile swallow pattern during childhood and adolescence and thereby produces an open bite and protrusion of the anterior teeth segments.
• Schneider(1982): Tongue thrust is a forward placement of the tongue between the anterior teeth and against the lower lip during swallowing.
• Tulley (1969): Tongue thrust is a forward movement of the tongue tip between the teeth to meet the lower lip during deglutition and in sounds of speech, so that the tongue becomes interdental.
• Brauer(1965): A tongue thrust is said to be present if the tongue is observed thrusting between and the teeth don’t close in centric occlusion during deglutition
• Profitt: Defined it as placement of the tongue tip forward between the incisors during swallowing.
Classification
1. Physiologic- normal tongue thrust swallow of infancy.
2. Habitual- present as a habit even after correction of the malocclusion.
3. Functional- adaptive behavior to achieve an oral seal.
4. Anatomic- enlarged tongue.
Etiology-
• Retained infantile swallow.• Upper respiratory tract infections. • Mouth breathing, chronic tonsilitis, allergies.• Neurological disturbance- Hyposensitive palate, moderate motor
disability, disruption of sensory control and coordination of swallowing.
• Functional adaptability to transient change in anatomy- Missing incisors.
• Feeding practices and tongue thrusting- Bottle feeding.• Induced due to other oral habit.• Hereditary.• Tongue size.
Clinical manifestations-
• Extra oral findings-1. Lip posture- lip separation is greater2. Mandibular movements- average path of mandibular movement is upward and backward with the tongue moving forward.3. Speech- Problems in articulations of /s/,/n/, /t/, /d/, /l/,/th/,/z/, /v/ sounds4. Facial form- Increase in anterior facial height
• Intraoral findings-1. Tongue movements- swallowing sequences are jerky and inconsistent.2. Tongue posture- The tongue tip at rest is lower.3. Malocclusion-
– Features pertaining to maxilla- Proclination of maxillary anteriors resulting in an increased overjet- Generalized spacing between the teeth- Maxillary constrictions
– Features pertaining to mandible- Retroclination or proclination of mandible depending on type of tongue thrust
– Intermaxillary relationships - Anterior or posterior open bite based on posture of the tongue- Posterior cross bite
Diagnosis-
History:Questions pertaining to
– Swallow pattern of siblings and parents.– Where or not remedial speech was ever provided.– Upper respiratory infections, sucking habits and neuromuscular problems.– Past and present information regarding the overall abilities, interests and motivation of
the patient
Examination• Study the posture of tongue while mandible is in postural position.• Observe the tongue during various swallowing procedures, the unconscious
swallow, the command swallow of saliva and the command swallow of water, unconscious swallow during chewing.
• Simple tongue thrust
Simple tongue thrust• Normal tooth contact in posterior region• Anterior open bite• Contraction of lips, mentalis muscles
and mandibular elevators
Lateral tongue thrust:• Posterior open bite with tongue
thrusting laterally.
Complex tongue thrust: • Generalized open bite with the
absence of contraction of lip and muscle and teeth contact in occlusion.
Treatment
Lesson 1• Explain to the child the proper way to swallow.• Show him how to swallow.• Show him that facial muscles of expression are not used during proper
swallow.• Show him that he keeps his teeth apart and places his tongue in between
teeth.
Now tell him that there are 4 things he can do voluntary in the act of swallow• Close his teeth tightly together in centric occlusion• Place his tongue against the roof of his mouth.• Suck when swallowing• Bring his lips together lightly
Lesson 2• Child is taught to get not only the tip but also middle
3rd of tongue up against the roof of the mouth.• Here the child places his tongue against the roof of
his mouth and then makes clicking or popping noise.Lesson 3• Explain the rest portion of tongue.• Use the pressure point on the papilla to show the
child where he is to hold the lip.
Lesson 4 (2S)• Spot and squeeze• Spot is developed in this lesson by producing the
“ch” sound• Squeeze part is done by squeezing the tongue
vigorously against the spot.
Lession 5 (4S)• Spot,salivate, squeeze, swallow
Lesson 6• To create an awarness of the posterior tongue action,the sound
“UNKA” is used with explosive action on the “K” sound.
Lession 7• Replace tongue blades in the mouth and pt. is asked to push the
tongue hard against that which strengths the back muscle of tongue and throat.
Lession 8• Concerned about lip control.• Teach the child how to whistle.
Lesson 9• Must in all open bite cases and in children with short upper lips.• Have the child grip the mentalis muscle with his right hand and pull the lower lip
down with the thumb under the chin and the index finger over the mentalis muscles.
• Then have himboing his upper lip down to the lower lip relax it and repeat again with the count of 1,2,3,4.
Lesson 10• Child to told to produce a balloning or puffing of lower lip.
Lesson 11• Tell him to close his teeth tightly together and keep his lips wide open then suck
air vigorously and quickly.
Bruxism
Definition-Ramjford(1966)- Bruxism is the habitual grinding of
teeth when the individual is not chewing or swallowing.
Vanderas(1995) -Nonfunctional movement of the mandible with or without an audible sound occurring during the day or night.
Types-1. Daytime bruxism/Diurnal
bruxism/Bruxomania.2. Night time bruxism/Nocturnal
bruxism/Bruxism.
Etiology-• Local factors
Mild occlusal trauma or minor anatomic defects, traumatic occlusion.
• Systemic factors Intestinal parasites, subclinical nutritional
deficiencies, allergies and endocrine disorders.
• Psychological factor Emotional stress, anger, anxiety or aggression.
• Occupational factorAthletes , watch makers, die-makers, diamond
cleaners
Clinical manifestation-
Occlusal trauma. Tooth mobility. Atypical shiny wear facets with sharp edges. Pulpal sensitivity to cold. Pulp exposures. Muscular tenderness, especially lateral pterygoid and masseter muscles. Muscular fatigue on waking. Muscular hypertrophy. TMJ disorders. Headache. Grinding and tapping sound. Soft tissue trauma.
Treatment-
1. Occlusal adjustments- Any occlusal interferences should be corrected.
2. Occlusal spilnts- night guards to cover all the teeth.
3. Restorative treatment- In severe cases leading to pulp exposures.
4. psychotherapy-5. Relaxation training.6. Physical therapy.7. Drugs (ethyl chloride for pain, local
anesthetics, tranquilizers, sedatives, muscle relaxants.)
8. Acupuncture therapy.
Lip habit
Definition-Habits that involve manipulation of the lips and
peri oral structures.
Classification-1. Lip biting.2. Lip sucking.3. Lip wetting.
Etiology-
1. Malocclusion- Class II div 1 with large overbite and overjet. Child wants to produce a normal lip seal during swallowing
by placing the lower lip posterior to upper incisors.
2. Habits- In conjunction with thumb sucking habit which may result
in large overjet and overbite.
3. Emotional stress.
Clinical manifestations-• Protrusion of maxillary incisors and retrusion
of mandibular incisors.• Reddened, irritated, chapped lips with
vermillion border relocated farther outside the mouth, especially with lower lip.
• Mentolabial sulcus becomes accentuated.• Malocclusion.
Treatment-• Correction of malocclusion.• Treating the primary habit.• Appliance therapy-
Lip bumper.Oral screen.
Cheek biting• It is an abnormal habit of biting or keeping the cheek muscles in
between upper and lower posterior teeth.
Clinical features- Ulcer at the level of occlusion. Open bite. Tooth malposition in buccal segment.
Treatment- Removable crib. Vestibular screen.
Nail bitingIt is one of the most common habits in children and adults.
Etiology- Insecurity. Nervous tension.
Effects- Crowding, rotation and alteration of incisal edges of incisors. Inflammation of nail beds.
Management- Patient is made aware of the habit. Scolding, nagging and threats are avaoided. Encouraging outdoor activities. Application of nail polish, light cotton mittens as reminder.
Self injurious habits(Masochistic habits/Sadomasochistic habits/Self-mutilating habits)
Definition-Repetitive acts that result in physical damage to the individual.
Etiology-1. Organic- Lesch-Nyhan disease, De Lange’s syndrome.
2. Functional-Type A- these are injury superimposed on a preexisting lesion.Type B- injuries secondary to another established habit.Type C- injuries of unknown or complex etiology.
Frenum thrusting- If the upper incisors are slightly spaces apart, the
child may lock his labial frenum between these teeth and permit it to remain in this position for hours.
Treatment-Psychotherapy.Bandages for any oral ulcerations.Oral shield.
Bobby pin opening-Seen in girls.Opening bobby pin with anterior incisors.Notched incisors.Partially denuded labial enamel.Calling attention to the harmful habit is
enough usually to stop the habit.
CONCLUSION• As the mouth is the primary and permanent location for
expression of emotions and even is a source of relief in passion and anxiety in both children and adults, stimulation of this region with tongue, finger, nail or other materials can be a palliative action.
• Though it is difficult to delineate it, but it is important to have differentiation of abnormal from normal because, if normal development get disturbed unknowingly and at the same time, if abnormal growth or underlying psychological cause let continue without interfering at proper time or age it will lead to long lasting effect on growth & development and psychological development of the child.
• Oral habits can manifest themselves in a variety of ways. The identification of an abnormal habit and assessment of a particular habit and its immediate and long term effect on the craniofacial complex and dentition should be made as early as possible.
• The assessment of these behavior must include a thorough evaluation of the habit itself and the presence of, or the potential for oral health repercussions.
• These judgements must be coupled with the sensitive assessment of the physical and emotional status of the child and the relationship of the parent or caregiver.