OPTIMISING PATIENT FUNCTION FOLLOWING ELECTIVE · PDF file · 2017-09-21BASED...
Transcript of OPTIMISING PATIENT FUNCTION FOLLOWING ELECTIVE · PDF file · 2017-09-21BASED...
© Arthritis Research UK 2009
1
OPTIMISING PATIENT FUNCTION FOLLOWING ELECTIVE TOTAL HIP REPLACEMENT: HOME-BASED PROGRESSIVE RESISTANCE TRAINING VS. ROUTINE REHABILITATION.
FEEDBACK FOLLOWING PRELIMINARY SEARCH
QUERY: REF OA-001
Received: 30th Oct. 2009 Feedback to CSG: 20th Nov. 2009 (latest), 16th Nov. 2009 (sent)
SEARCH METHODOLOGY
The content of this feedback report refers only to the most relevant material located under each of the evidence headings and is drawn predominantly from author abstracts or research recommendations within Guidelines. The question is posed in the context of head-to-head studies that consider the comparative effectiveness of home-based progressive resistance training of the lower limb muscles with routine rehabilitation programs, following elective total hip replacement surgery for osteoarthritis. However, studies comparing different perioperative and postoperative exercise/physical therapy-based rehabilitation regimes/programs have also been included to provide a complete overview of the current literature pertaining to the effectiveness of different rehabilitation regimes following total hip replacement. This report therefore focuses on material that makes a clear connection between total hip replacement surgery and associated rehabilitation programs. Material prior to 2005 has also been excluded unless it relates very specifically to the question posed. Where no specific detail of review methodology is given, these reviews are collected in section D. Further details of all the studies included in this report are shown in the appendix, sorted by report section and author name.
Criteria used (PICO): Who? (population) Patients with osteoarthritis affecting the hip, who undergo (total) hip replacement surgery. What? (intervention/exposure/measure) Postoperative rehabilitation programs Comparison Standard/usual or other post-operative care/rehabilitation programs
What is measured? What are the outcomes? Self-reported pain; physical function; range of movement; muscle strength; activity; return to work; patient satisfaction; other relevant measures.
Location and setting Worldwide; Community.
2
Exclusion Criteria None Databases Searched NLH (Bandolier, National Library of Guidelines, NICE Guidance, International Guideline, CKS, Clinical Evidence, DUETS, NHS Evidence Specialist Collections); EMBASE; MEDLINE; PEDro; Centre for Reviews and Dissemination (DARE, NHS EED and HTA); MetaRegister of Clinical Trials (active registers); ClinicalTrials.gov; Cochrane Database of Systematic Reviews; Cochrane Central Register of Controlled Studies. Types of Study Head-to-head, controlled or outcome trials/studies. Keywords searched Osteoarthritis, hip, replacement, arthroplasty, rehabilitation, exercise, physiotherapy, training, rehabilitation, program(s)/programme(s). Keywords were used separately or in combination; truncation was used where possible; MESH words included where possible. Date limits 2000 to date for searches to scope background; 2006 to date for general inclusion in feedback (see Methodology) Summary of available evidence
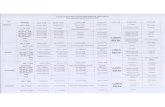
EVIDENCE TYPE
INCLUDED IN FEEDBACK
A Controlled trials (Current and Closed) 12
B Systematic Reviews 2
C Evidence Summaries 1
D Narrative reviews 1
E Case Studies 33 1
F Peer-reviewed articles 1
G Intellectual Property Office 0
RESULTS
Whilst a number of studies focus specifically on patients with osteoarthritis that undergo unilateral or total hip arthroplasty, also included are those with patients that undergo hip or knee arthroplasty due to osteoarthritis, or studies where a diagnosis of osteoarthritis is not part of the inclusion criteria but is, in fact, the main reason patients undergo joint arthroplasty.
1 40 articles
3
A: Controlled Trials
Includes details from: ISRCTN Register – trials; Action Medical Research; Leukaemia Research Fund; MRC; NHS R&D HTA Programme; NIH records on ClinicalTrials.gov; The Wellcome Trust; UK Clinical Trials Gateway and other archive registers.
One trial specifically compares resistance training to neuromuscular electrical training and conventional rehabilitation programs (A12), this trial is complete and the outcomes have been published in an academic journal: it is included in Section E of the report (see Appendix A for citation). Other trials focus on: weight bearing following total hip replacement (A9, A7) or hip or knee replacement (A11) surgery; preoperative exercise regimes prior to hip (A3) or hip or knee (A1) replacement surgery for osteoarthritis; postoperative treatments and rehabiliation/exercise regimes (A2, A4, A6, A10) including cost-effectiveness analysis (A5, A8). Whilst the majority of the trials appear to be completed, no publications or reports of results were found. Trail end dates were used to sort the following table.
ID Trial Details: title, sponsor and web-link Study Period
A1 Preoperative exercise in patients undergoing total hip or knee replacement - A Randomized Controlled Trial. University of Southern Denmark http://ClinicalTrials.gov/show/NCT01003756
2009-2012
A2 Effectiveness of two types of treatment in restoring muscle after hip or knee Surgery. National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) http://ClinicalTrials.gov/show/NCT00393848
2006-2011
A3 Feasibility of a therapeutic exercise before total hip replacement. Hospital Gelderse Vallei, Netherlands http://controlled-trials.com/ISRCTN09005050
2007-2008
A4 Ergometer cycling after replacement of the hip or knee joint. Verein zur Förderung der Rehabilitationsforschung in Schleswig-Holstein http://ClinicalTrials.gov/show/NCT00951990
2005-2008
A5 Cost efficacy of a clinical pathway to patients undergoing hip and knee replacement surgery. University of Aarhus http://ClinicalTrials.gov/show/NCT00175201
2005-2008
A6 Treatment and rehabilitation of patients with hip arthroplasty to regain walk and work efficiency and quality of life. Norwegian University of Science and Technology http://clinicaltrials.gov/show/NCT00638417
2006-2007
A7 Effect of post-operative weight bearing status on clinical and radiological outcome of cementless femoral component. Department of Health (UK) http://www.controlled-trials.com/ISRCTN53323735
2005-2007
4
A8 Alberta hip and knee replacement project. Alberta Bone and Joint Health Institute http://ClinicalTrials.gov/show/NCT00277186
2005-2006
A9 Safety of non-delayed weight bearing after total hip replacement with non-cemented fiber metal taper stem. Vanderbilt University http://ClinicalTrials.gov/show/NCT00179088
2003-2006
A10 A targeted strengthening program following total hip replacement. University of Melbourne http://ClinicalTrials.gov/show/NCT00222300
2003-2005
A11 Weight-bearing recommendations after replacement of the hip or knee joint. Verein zur Förderung der Rehabilitationsforschung in Schleswig-Holstein http://ClinicalTrials.gov/show/NCT00266396
2002-2004
A12 Muscle function in elderly postoperative patients Bispebjerg Hospital http://ClinicalTrials.gov/show/NCT00559780
2000-2003
B: Systematic reviews
Only those reviews with a detailed methodology were considered for this section. Other literature reviews considered relevant have been shown under section D.
There are no systematic reviews that specifically focus on postoperative resistance training for hip arthroscopy (due to osteoarthritis). However, a recent review of physiotherapy exercise in general, after hip replacement surgery for osteoarthritis, concludes there is currently insufficient good quality evidence to draw any conclusions about its effectiveness (Minns Lowe, Barker, Dewey, & Sackley, 2009). A Cochrane review examines multidisciplinary rehabilitation programs following hip or knee joint replacement surgery and concludes home-based care may be beneficial but stresses the low quality of the current evidence-base (Khan, Ng, Gonzalez, Hale, & Turner-Stokes, 2008). Both reviews highlight the lack of high quality evidence and surmise that further high quality research is required. Other systematic reviews which may be of interest, but not included in the appendix, include a Cochrane review of preoperative education prior to hip or knee replacement surgery and its effect on postoperative outcomes (Mcdonald, Hetrick, & Green, 2004) and a systematic review of performance based methods for assessing physical function of patients with hip or knee osteoarthritis (Terwee, Mokkink, Steultjens, & Dekker, 2006).
5
C: Good Quality Evidence summaries (inc. guidelines)
Recently published guidelines from the National Institute for Health and Clinical Excellence (NICE) for the care and management of adults with osteoarthritis (The National Collaborating Centre for Chronic Conditions, 2008), from The European League Against Rheumatism (EULAR) for hip osteoarthritis (Zhang et al., 2005) and from the Osteoarthritis Research Society International (OARSI) for hip and knee osteoarthritis (Zhang et al., 2007; 2008) make no mention of postoperative rehabilitation protocols or best practice.
D: Non-Systematic Reviews (no methodology given)
Two non-systematic reviews are pertinent to this report. One examines the evidence for postoperative rehabilitation following hip arthroscopy for osteoarthritis and concludes that, at the time (2002), there were no trials to determine the most effective exercise protocols (Brander & Mullarkey, 2002). The second considers physical rehabilitation prior to and following hip and knee arthroscopy and suggests postoperative regimes are beneficial following hip replacement (Dauty, Genty, & Ribinik, 2007). Both reviews highlight the lack of good quality evidence and the need for further quality research.
OTHER POTENTIALLY USEFUL INFORMATION E: Case Studies
Only two studies (3 papers), both RCTs, specifically mention resistance training in the context hip replacement surgery for osteoarthritis. The first compares the effect of resistance training, electrical muscle stimulation and usual rehabilitation i.e. functional exercise on musculature and length of hospital stay following unilateral hip replacement (Suetta et al., 2004; Suetta et al., 2008). Only resistance training based rehabilitation led to a reduced hospital stay and improved musculature, although functional muscle performance also improved with electrical muscle stimulation. In the second study, resistance training was part of the routine rehabilitation protocol for patients undergoing hip arthroplasty. This was compared to routine rehabilitation with electric muscle stimulation. Whilst both regimes resulted in improvement in muscle strength and consequently functional independence, there was greater benefit with electric muscle stimulation, although both groups were comparable in terms of walking tests and length of hospital stay (Gremeaux, et al., 2008). The remaining studies included in this review focus on a diverse range of perioperative and postoperative rehabilitation regimes, and have been subdivided into inpatient and outpatient or community based programs. Perioperative and inpatient postoperative rehabilitation A total of 18 studies (19 articles) addressed inpatient rehabilitation programs following hip or knee surgery, which have been further subdivided according to type of therapy. Early weight bearing: Four RCTs (Strom, Huss, & Larsson, 2006; Strom, Nilsson, Milbrink, Mallmin, & Larsson, 2007; Thien, Ahnfelt, Eriksson, Strömberg, & Kärrholm, 2007; Unver, Karatosum, Gunal, & Angin, 2004) and two cohort studies (Karatosun, Unver, & Gunal, 2008; Merle, Rougier, Belaid, Cantalloube, & Lamotte, 2009) focus on the issue of early full-weight bearing following total hip
6
arthroplasty. There appears to be no significant differences in functional outcomes or re-operation rates between early full- or partial-weight bearing regimes, although early on full-weight bearing may be associated with less limb stability and greater energy expenditure. Intensive physiotherapy: Two controlled studies examined the effects of intensive vs. usual physiotherapy program following THR surgery (Lilikakis, Gillespie, & Villar, 2008; Peck, Foster, & McLauchlan, 2006). Both concur that intensive physiotherapy reduces length of hospital stay; the former indicating this was due to the earlier achievement of milestones e.g. independent walking. Accelerated/Multidisciplinary rehabilitation: Three related studies (2 RCTs and 1 controlled study) examine the efficacy and (cost-) effectiveness of accelerated/multidisciplinary perioperative rehabilitation compared to usual care following hip and knee replacement surgery (Larsen, Sorensen, Hansen, Thomsen, & Soballe, 2008; Larsen, Hansen, Thomsen, Christiansen, & Soballe, 2009; Larsen, Hvass, Hansen, Thomsen, & Soballe, 2008). Accelerated rehabilitation was more clinically and cost effective than usual care. A cohort study indicates that accelerated rehabilitation can improve patient self-efficacy, which is associated with better health outcomes, following hip arthroplasty (Dohnke, Knauper, & Muller-Fahrnow, 2005). Other regimes: Randomised controlled trials investigating novel inpatient rehabilitation regimes indicate benefit above that of usual rehabilitation protocols for:
aquatic physiotherapy (Rahmann, Brauer, & Nitz, 2009)
continuous passive motion exercises (Wilk & Franczuk, 2005)
tailored 8-week exercise therapy starting preoperatively (Gilbey et al., 2003) however, no additional benefit was found when patients received
osteopathic manipulation (Licciardone et al., 2004). Miscellaneous (total hip arthroscopy due to OA): An RCT compared an optimised perioperative care regime to conventional care for patients following hip arthroscopy and found conventional care superior with regards functional outcomes (Petersen, Andersen, & Soballe, 2008). A controlled cohort study (with very low sample sizes) found patients undergoing inpatient rehabilitation after surgery showed greater improvement than patients attending a sub-acute rehabilitation unit (Johanson, Cohen, Snyder, McKinley, & Scott, 2009). A customised guide may help improve patient outcomes and satisfaction during hospitalisation for hip replacement (Fortina et al., 2005). Postoperative rehabilitation following discharge from hospital A total of 13 studies (18 articles) addressed postoperative rehabilitation programs following discharge from hospital after hip or knee surgery, which have been further subdivided according to type of rehabilitation program and therapy. Home vs. inpatient: A number of studies suggest similar long-term outcomes for patients receiving home-based compared to inpatient rehabilitation regimes following hip (or knee) replacement surgery:
Randomised controlled trial (Mahomed et al., 2008)
Controlled cohort studies, patients were not randomised in these studies as to qualify for home-based rehabilitation a number of criteria had to be met (Iyengar, Nadkarni, Ivanovic,
7
& Mahale, 2007; Jester & Hicks, 2003a, b; Mahomed, Koo Seen Lin, Levesque, Lan, & Bogoch, 2000; Tribe et al., 2005).
In addition, home-based programs appear to be significantly cheaper and therefore more cost-effective. Home care regimes: A RCT examined the effectiveness of a ‘streamlined’ vs. established home care program both included physical therapy. The streamlined program involved home visits prior to joint replacement surgery but fewer visits overall. No differences in patient outcomes were found and therefore the streamlined program, which was markedly less costly, was considered a more efficient service (Weaver et al., 2003). Targeted exercise: Studies suggest that targeted postoperative exercise/physiotherapy programs following discharge from hospital are effective at improving patient outcomes. Benefits appear to exceed those of traditional rehabilitation programs, and are independent of location or supervision:
Randomised controlled trails o intensive short-term exercise vs. usual care (Bulthuis et al., 2007; Bulthuis,
Mohammad, Braakman-Jansen, Drossaers-Bakker, & van de Laar, 2008): intensive program also costs less and is therefore more cost-effective.
o maximum strength straining plus usual vs. usual rehabilitation (Husby et al., 2009) o supervised centre-based vs. unsupervised home-base targeted strengthening
exercises (Galea M.P. et al., 2008) o arm exercises using an ergometer plus usual vs. usual rehabilitation (Grange et al.,
2004; Maire et al., 2003; Maire et al., 2004; Maire et al., 2006)2
Controlled-cohort study o class-based vs. one-to-one home-based physiotherapy (Coulter, Weber, & Scarvell,
2009): class-based protocol is significantly cheaper. Late rehabilitation programs: Two RCTs suggest that targeted 6- or 8-week exercise programs aimed at patients that undergo total hip arthroplasty after at least 4 months can further improve hip function and strength above usual care (Trudelle-Jackson & Smith, 2004; Unlu, Eksioglu, Aydog, Aydod, & Atay, 2007): further location of program i.e. home vs. hospital does not influence outcome. Other studies The following studies are not detailed in the appendix but may be of interest for any future research:
appropriateness, sensitivity and/or roundedness of various outcome measures used for assessing patients undergoing hip (and knee) arthroscopy (Kennedy, Stratford, Hanna, Wessel, & Gollish, 2006; Lindemann, et al., 2006; Oberg, Oberg, Sviden, & Nordwall Persson, 2005; Pisoni, Giardini, Majani, & Maini, 2008; Stratford, Kennedy, & Riddle, 2009)
effect of preoperative physiotherapy and education on postoperative outcomes following hip or knee arthroscopy (Ferrara, et al., 2008; Rooks, et al., 2006; Vukomanovic, Popovic, Durovic, & Krstic, 2008).
2 All patients resided at a rehabilitation centre during the study.
8
F: Peer-reviewed articles
One article presents a commentary on the role of perioperative physiotherapy following hip and knee surgery (Lenssen & de Bie, 2006). It indicates that postoperative Continuous Passive Motion and intense physical exercise is beneficial and that in order to maximise the benefit exercise regimes need to be maintained after discharge.
G: Intellectual Property Office
None
CONCLUSION
The majority of articles included in this report present randomised controlled study designs and systematic reviews that rate as medium/high-level evidence: however, caution is needed as many of these studies have a small sample size. In general, the current evidence base suggests that postoperative exercise/physiotherapy regimes are beneficial for patients with hip (and hip or knee) osteoarthritis following hip (and hip or knee) arthroplasty, increasing functional outcomes and quality of life.
Only two studies in the report, both low-quality RCTs with small sample sizes, specifically examine the effectiveness of resistance training postoperatively but before discharge, both focus on patients undergoing hip replacement resulting from osteoarthritis. The first study revealed resistance training to be superior to both electrical muscle stimulation and the usual regime provided. The second found that electric muscle stimulation in addition the usual rehabilitation regime (which included resistance training) had greater benefit than the usual protocol alone.
Other studies indicate that post-discharge rehabilitation programs involving targeted or intensive physiotherapy and physical exercise regimes are more effective in terms of patient outcomes than conventional programs, irrespective of location or supervision.
In summary, this report identifies the lack of high quality RCT evidence as a necessary research direction in establishing the effectiveness of home-based supervised resistance training in the rehabilitation of patients undergoing total hip arthroplasty as a result of osteoarthritis.
9
ABBREVIATIONS
ADL Function in Daily Living
AQoL Assessment of Quality of Life Questionnaire
CES-D Center for Epidemiologic Studies Depression Scale
EPMROM Escola Paulista de Medicina Range of Motion Scale
EQ-5D EuroQual-5D Health Survey
FIM Functional Independence Measure
HAQ Health Assessment Questionnaire
HOOS Hip dysfunction and Osteoarthritis Outcome Score
HRQoL Health Related Quality of Life
KOOH Knee injury and Osteoarthritis Outcome Score
MACTAR The McMaster Toronto Arthritis Patient Preference Disability questionnaire
OA Osteoarthritis
QALYs Quality-Adjusted Life Years
QoL Quality of Life
RA Rheumatoid arthritis
RAND-36 Research and Development 36-item Health Survey
RCT Randomised Controlled/Clinical Trial
ROM Range of Motion
SF-36 Short-Form-36 Health Survey
SF-6D Short-Form-6D Health Survey
THA Total hip arthroplasty
THR Total hip replacement
TJR Total joint replacement
TUG Timed Up & Go test
VAS Visual Analogue Scale
WOMAC Western Ontario and McMaster Universities Osteoarthritis Index
10
REFERENCES
Brander, V.A., & Mullarkey, C.F. (2002). Rehabilitation after total hip replacement for osteoarthritis. Physical Medicine & Rehabilitation, 16(3), 415-431.
Bulthuis, Y., Drossaers-Bakker, K.W., Taal, E., Rasker, J., Oostveen, J., van't Pad Bosch, P., Oosterveld, F. & van de Laar, M. (2007). Arthritis patients show long-term benefits from 3 weeks intensive exercise training directly following hospital discharge. Rheumatology, 46(11), 1712-7.
Bulthuis, Y., Mohammad, S., Braakman-Jansen, L.M., Drossaers-Bakker, K.W., & van de Laar, M.A. (2008). Cost-effectiveness of intensive exercise therapy directly following hospital discharge in patients with arthritis: Results of a randomized controlled clinical trial. Arthritis & Rheumatism, 59(2), 247-54.
Coulter, C. L., Weber, J. M., & Scarvell, J.M. (2009). Group physiotherapy provides similar outcomes for participants after joint replacement surgery as 1-to-1 physiotherapy: A sequential cohort study. Archives of Physical Medicine & Rehabilitation, 90(10), 1727-33.
Dauty, M., Genty, M., & Ribinik, P. (2007). Physical training in rehabilitation programs before and after total hip and knee arthroplasty. Annales De Réadaptation Et De Médecine Physique, 50, 462-468.
Dohnke, B., Knauper, B., & Muller-Fahrnow, W. (2005). Perceived self-efficacy gained from, and health effects of, a rehabilitation program after hip joint replacement. Arthritis & Rheumatism, 53(4), 585-92.
Ferrara P.E., Rabini A., Aprile I., Maggi L., Piazzini D.B., Logroscino G., Magliocchetti, L.G., Amabile, E., Tancredi, G., Aulisa, A.G., Padua, L. & Bertolini, C. (2008). Effect of pre-operative physiotherapy in patients with end-stage osteoarthritis undergoing hip arthroplasty. Clinical Rehabilitation, 22(10-11), 977-986.
Fortina, M., Carta, S., Gambera, D., Crainz, E., Ferrata, P., & Maniscalco, P. (2005). Recovery of physical function and patient's satisfaction after total hip replacement (THR) surgery supported by a tailored guide-book. Acta Bio-Medica De l Ateneo Parmense, 76(3), 152-6.
Galea M.P., Levinger P., Lythgo N., Cimoli C., Weller R., Tully E., McMeeken, J., & Westh, R. (2008). A targeted home- and center-based exercise program for people after total hip replacement: A randomized clinical trial. Archives of Physical Medicine and Rehabilitation, 89(8), 1442-1447.
Genêt, F., Gouin, F., Coudeyre, E., Revel, M., & Rannou, F. (2007). The benefits of ambulatory physiotherapy for patients able to leave the surgery department directly for home just after total hip replacement. development of french guidelines for clinical practice. Annales De Réadaptation Et De Médecine Physique, 50, 776-782.
Gilbey, H. J., Ackland, T. R., Wang, A. W., Morton, A. R., Trouchet, T., & Tapper, J. (2003). Exercise improves early functional recovery after total hip arthroplasty. Clinical Orthopaedics & Related Research, (408), 193-200.
Grange, C. C., Maire, J., Groslambert, A., Tordi, N., Dugue, B., Pernin, J. N., & Rouillon, J.D. (2004). Perceived exertion and rehabilitation with arm crank in elderly patients after total hip arthroplasty: A preliminary study. Journal of Rehabilitation Research and Development, 41(4), 611-620.
Gremeaux V., Renault J., Pardon L., Deley G., Lepers R., & Casillas J.-M. (2008). Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip
11
osteoarthritis in elderly patients: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 89(12), 2265-2273.
Husby, V. S., Helgerud, J., Bjorgen, S., Husby, O. S., Benum, P., & Hoff, J. (2009). Early maximal strength training is an efficient treatment for patients operated with total hip arthroplasty. Archives of Physical Medicine & Rehabilitation, 90(10), 1658-67.
Iyengar, K. P., Nadkarni, J. B., Ivanovic, N., & Mahale, A. (2007). Targeted early rehabilitation at home after hip and knee joint replacement: Does it work? Disability and Rehabilitation, 29(6), 495-502.
Jester, R., & Hicks, C. (2003a). Using cost-effectiveness analysis to compare hospital at home and in-patient interventions. part 1. Journal of Clinical Nursing., 12, 13-19.
Jester, R., & Hicks, C. (2003b). Using cost-effectiveness analysis to compare hospital at home and in-patient interventions. part 2. Journal of Clinical Nursing., 12, 20-27.
Johanson, M. A., Cohen, B. A., Snyder, K. H., McKinley, A. J., & Scott, M. L. (2009). Outcomes for aging adults following total hip arthroplasty in an acute rehabilitation facility versus a subacute rehabilitation facility: A pilot study. Journal of Geriatric Physical Therapy, 32(2), 29-35.
Karatosun, V., Unver, B., & Gunal, I. (2008). Hip arthroplasty with the thrust plate prosthesis in patients of 65 years of age or older: 67 patients followed 2-7 years. Archives of Orthopaedic & Trauma Surgery, 128(4), 377-381.
Kennedy, D. M., Stratford, P. W., Hanna, S. E., Wessel, J., & Gollish, J. D. (2006). Modeling early recovery of physical function following hip and knee arthroplasty. BMC Musculoskeletal Disorders, 7
Khan, F., Ng, L., Gonzalez, S., Hale, T., & Turner-Stokes, L. (2008). Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. Cochrane Database of Systematic Reviews, (2), CD004957.
Larsen, K., Hansen, T. B., Thomsen, P. B., Christiansen, T., & Soballe, K. (2009). Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. Journal of Bone and Joint Surgery, 91, 761-772.
Larsen, K., Sorensen, O. G., Hansen, T. B., Thomsen, P. B., & Soballe, K. (2008). Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: A randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthopaedica, 79(2), 149-159.
Larsen, K., Hvass, K., Hansen, T., Thomsen, P., & Soballe, K. (2008). Effectiveness of accelerated perioperative care and rehabilitation intervention compared to current intervention after hip and knee arthroplasty. A before-after trial of 247 patients with a 3-month follow-up. BMC Musculoskeletal Disorders, 9(1), 59.
Lenssen, A.F., & de Bie, R.A. (2006). Role of physiotherapy in peri-operative management in total knee and hip surgery. Injury, 37 Suppl 5, S41-3.
Licciardone, J. C., Stoll, S. T., Cardarelli, K. M., Gamber, R. G., Nr, S. J., & Winn, W. B. (2004). A randomized controlled trial of osteopathic manipulative treatment following knee or hip arthroplasty. JAOA: Journal of the American Osteopathic Association, 104(5), 193-205.
12
Lilikakis, A. K., Gillespie, B., & Villar, R. N. (2008). The benefit of modified rehabilitation and minimally invasive techniques in total hip replacement. Annals of the Royal College of Surgeons of England, 90(5), 406-11.
Lindemann, U., Becker, C., Unnewehr, I., Muche, R., Aminian, K., Dejnabadi, H., Nikolaus, T., Puhl, W., Huch, K., Drienhöfer, K.E. (2006). Gait analysis and WOMAC are complementary in assessing functional outcome in total hip replacement. Clinical Rehabilitation, 20(5), 413-420.
Mahomed, N.N., Davis, A.M., Hawker, G., Badley, E., Davey, J.R., Syed, K.A., Coyte, P.C., Gandhi, R. & Wright, J.G. (2008). Inpatient compared with home-based rehabilitation following primary unilateral total hip or knee replacement: A randomized controlled trial. Journal of Bone & Joint Surgery, American Volume, 90(8), 1673-1680.
Mahomed, N.N., Koo Seen Lin, M.J., Levesque, J., Lan, S., & Bogoch, E.R. (2000). Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement. Journal of Rheumatology, 27(7), 1753-8.
Maire, J., Dugue, B., Faillenet-Maire, A. F., Smolander, J., Tordi, N., Parratte, B., Grange, C. & Rouillon, J.D. (2006). Influence of a 6-week arm exercise program on walking ability and health status after hip arthroplasty: A 1-year follow-up pilot study. Journal of Rehabilitation Research & Development, 43(4), 445-449.
Maire, J., Dugué, B., Faillenet-Maire, A. F., Tordi, N., Parratte, B., Smolander, J. & Rouillon, J.D. (2003). Recovery after total hip joint arthroplasty in elderly patients with osteoarthritis: Positive effect of upper limb interval-training. Journal of Rehabilitation Medicine : Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine, 35(4), 174-179.
Maire, J., Faillenet-Maire, A. F., Grange, C., Dugué, B., Tordi, N., Parratte, B. & Rouillon, J.D. (2004). A specific arm-interval exercise program could improve the health status and walking ability of elderly patients after total hip arthroplasty: A pilot study. Journal of Rehabilitation Medicine : Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine, 36(2), 92-94.
Mcdonald, S., Hetrick, S. E., & Green, S. (2004). Pre-operative education for hip or knee replacement. Cochrane Database of Systematic Reviews, 1(CD003526)
Merle, J., Rougier, P., Belaid, D., Cantalloube, S., & Lamotte, D. (2009). Is early weight bearing resumption beneficial after total hip replacement? Orthopaedics & Traumatology, Surgery & Research, 95(2), 127-33.
Minns Lowe, C. J., Barker, K. L., Dewey, M. E., & Sackley, C. M. (2009). Effectiveness of physiotherapy exercise following hip arthroplasty for osteoarthritis: A systematic review of clinical trials. BMC Musculoskeletal Disorders, 10
Oberg, T., Oberg, U., Sviden, G., & Nordwall Persson, A. (2005). Functional capacity after hip arthroplasty: A comparison between evaluation with three standard instruments and a personal interview. Scandinavian Journal of Occupational Therapy, 12(1), 18-28.
Peck, C. N., Foster, A., & McLauchlan, G. J. (2006). Reducing incision length or intensifying rehabilitation: What makes the difference to length of stay in total hip replacement in a UK setting? International Orthopaedics, 30(5), 395-8.
Petersen, M. K., Andersen, N. T., & Soballe, K. (2008). Self-reported functional outcome after primary total hip replacement treated with two different periopera-tive regimes: A follow-up study involving 61 patients. Acta Orthopaedica, 79(2), 160-7.
13
Pisoni, C., Giardini, A., Majani, G., & Maini, M. (2008). International classification of functioning, disability and health (ICF) core sets for osteoarthritis. A useful tool in the follow-up of patients after joint arthroplasty. European Journal of Physical & Rehabilitation Medicine., 44(4), 377-85.
Rahmann, A. E., Brauer, S. G., & Nitz, J. C. (2009). A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: A randomized controlled trial. Archives of Physical Medicine & Rehabilitation, 90(5), 745-55.
Rooks, D. S., Huang, J., Bierbaum, B. E., Bolus, S. A., Rubano, J., Connolly, C. E., Alpert, S., Iversen, M.D. & Katz, J.N. (2006). Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis & Rheumatism, 55(5), 700-708.
Stratford, P. W., Kennedy, D. M., & Riddle, D. L. (2009). New study design evaluated the validity of measures to assess change after hip or knee arthroplasty. Journal of Clinical Epidemiology, 62(3), 347-52.
Strom H., Huss K., & Larsson S. (2006). Unrestricted weight bearing and intensive physiotherapy after uncemented total hip arthroplasty. Scandinavian Journal of Surgery, 95(1), 55-60.
Strom, H., Nilsson, O., Milbrink, J., Mallmin, H., & Larsson, S. (2007). The effect of early weight bearing on migration pattern of the uncemented CLS stem in total hip arthroplasty. Journal of Arthroplasty, 22(8), 1122-9.
Suetta, C., Andersen, J. L., Dalgas, U., Berget, J., Koskinen, S., Aagaard, P., Magnusson, S.P., Kjaer, M. (2008). Resistance training induces qualitative changes in muscle morphology, muscle architecture, and muscle function in elderly postoperative patients. Journal of Applied Physiology, 105(1), 180-6.
Suetta, C., Magnusson, S. P., Rosted, A., Aagaard, P., Jakobsen, A. K., Larsen, L. H., Duus, P. & Kjaer, M. (2004). Resistance training in the early postoperative phase reduces hospitalization and lead to muscle hypertrophy in elderly hip surgery patients - a controlled randomized study. Journal of the American Geriatrics Society, 52, 2016-2022.
Terwee, C. B., Mokkink, L. B., Steultjens, M. P., & Dekker, J. (2006). Performance-based methods for measuring the physical function of patients with osteoarthritis of the hip or knee: A systematic review of measurement properties. Rheumatology, 45(7), 890-902.
The National Collaborating Centre for Chronic Conditions,. (2008). Osteoarthritis: National clinical guideline for care and management in adults. London: The Royal College of Physicians.
Thien, T. M., Ahnfelt, L., Eriksson, M., Strömberg, C., & Kärrholm, J. (2007). Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: A prospective randomized comparison using radiostereometry. Acta Orthopaedica, 78(6), 730-739.
Tribe, K. L., Lapsley, H. M., Cross, M. J., Courtenay, B. G., Brooks, P. M., & March, L. M. (2005). Selection of patients for inpatient rehabilitation or direct home discharge following total joint replacement surgery: A comparison of health status and out-of-pocket expenditure of patients undergoing hip and knee arthroplasty for osteoarthritis. Chronic Illness, 1(4), 289-303.
Trudelle-Jackson, E., & Smith, S. S. (2004). Effects of a late-phase exercise program after total hip arthroplasty: A randomized controlled trial. Arch Phys Med Rehabil, 85, 1056-1062.
Unlu E., Eksioglu E., Aydog E., Aydod S.T., & Atay G. (2007). The effect of exercise on hip muscle strength, gait speed and cadence in patients with total hip arthroplasty: A randomized controlled study. Clinical Rehabilitation, 21(8), 706-711.
14
Unver B., Karatosum V., Gunal I., & Angin S. (2004). Comparison of two different rehabilitation programmes for thrust plate prosthesis: A randomized controlled study. Clinical Rehabilitation, 18(1), 84-91.
Vukomanovic, A., Popovic, Z., Durovic, A., & Krstic, L. (2008). The effects of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanitetski Pregled, 65(4), 291-297.
Weaver, F. M., Hughes, S. L., Almagor, O., Wixson, R., Manheim, L., Fulton, B. & Singer, R. (2003). Comparison of two home care protocols for total joint replacement. Journal of the American Geriatrics Society, 51, 523-528.
Wilk, M., & Franczuk, B. (2005). Rehabilitation of patients after hip arthroplasty using continous passive motion. [Rehabilitacja pacjentow po artroplastyce biodra z zastosowaniem ciaglego ruchu biernego] Fizjoterapia Polska, 5(1), 8-14.
Zhang, W., Doherty, M., Arden, N., Bannwarth, B., Bijlsma, J., Gunther, K., Hauselmann, H.J.; Herrero-Beaumont, G., Jordan, K., Kaklamanis, P., Leeb, B., Lequesne, M., Lohmander, S., Mazieres, B., Martin-Mola, E. Pavelka, K., Pendleton, A., Punzi, L., Swoboda, B., Varatojo, R., Verbruggen, G., Zimmermann-Gorska, I. & Dougados, M. (2005). EULAR evidence based recommendations for the management of hip osteoarthritis: Report of a task force of the EULAR standing committee for international clinical studies including therapeutics (ESCISIT). Annals of the Rheumatic Diseases, 64, 669-681.
Zhang, W., Moskowitz, R. W., Nuki, G., Abramson, S., Altman, R. D., Arden, N., Bierma-Zeinstra, S., Brandt, K.D., Croft, P., Doherty, M., Dougados, M., Hochberg, M., Hunter, D.J., Kwoh, K., Lohmander, L.S. & Tugwell, P. (2007). OARSI recommendations for the management of hip and knee osteoarthritis, part I: Critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis & Cartilage, 15(9), 981-1000.
Zhang, W., Moskowitz, R. W., Nuki, G., Abramson, S., Altman, R. D., Arden, N., Bierma-Zeinstra, S., Brandt, K.D., Croft, P., Doherty, M., Dougados, M., Hochberg, M., Hunter, D.J., Kwoh, K., Lohmander, L.S. & Tugwell, P. (2008). OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis & Cartilage, 16(2), 137-62.
15
FULL TEXT APPENDIX SECTION A – CONTROLLED TRIALS
ID
Title and Weblink Sponsor; Start - end date; status
Summary
A1 Preoperative exercise in patients undergoing total hip or knee replacement - a randomized controlled trial. http://ClinicalTrials.gov/show/NCT01003756
University of Southern Denmark 2009-2012 not yet open for recruitment (n=160)
Randomised controlled trial to assess effectiveness of pre-operative neuromuscular exercise on patient outcomes.
Assessment at 1 month pre-operatively, 3 months and 1 year post-operatively. Primary outcome measure self-reported physical function KOOS/HOOS subscale ADL function; secondary outcome measures self-reported pain and QoL (KOOS/HOOS subscales), observed physical function and muscle strength.
Adults, 18 years and over, with osteoarthritis and scheduled for elective primary, unilateral total hip or knee replacement.
A2 Effectiveness of two types of treatment in restoring muscle after hip or knee surgery. http://ClinicalTrials.gov/show/NCT00393848
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) 2006-2011 currently recruiting (n=120)
Randomised controlled trial to evaluate effects of two postoperative interventions aimed at preserving muscle protein following hip or knee surgery.
Primary outcomes, muscle protein synthesis and breakdown measured after hospitalisation; secondary outcomes, function and muscle mass measured prior to surgery and at 2 and 6-8 weeks post-operatively.
Adults (30-80 years) scheduled for surgery due to OA, avascular necrosis, fracture, or TJR revision of knee or hip.
A3 Feasibility of a therapeutic exercise before total hip replacement. http://controlled-trials.com/ISRCTN09005050
Hospital Gelderse Vallei, Netherlands 2007-2008 complete (n=20)
Randomised controlled trial to assess effectiveness of short-term (3-6 weeks) pre-operative exercise program (twice a week) for older patients awaiting total hip arthroplasty.
Primary outcome measures, occurrence of adverse effects, adherence to treatment, motivation and appreciation. Secondary outcome measures, pre-operative effectiveness & post-operative effectiveness including functional mobility (Iowa Level of Assistance Scale)
Adults (70 years and over) awaiting total hip arthroplasty as a result of OA.
16
A4 Ergometer cycling after replacement of the hip or knee joint. http://ClinicalTrials.gov/show/NCT00951990
Verein zur Förderung der Rehabilitationsforschung in Schleswig-Holstein 2005-2008 complete (n=457)
Randomised controlled trial to evaluate the effectiveness of ergometer cycling during rehabilitation following hip or knee replacement therapy.
Assessment at 3 months to 24 months? using as primary outcome measure WOMAC Physical Function; Secondary outcome measures, WOMAC Pain and Stiffness, SF-36, Patient satisfaction and Lequesne Hip or Knee Score.
Adults (18 years and older) awaiting elective unilateral hip or knee replacement due to OA or femoral head necrosis.
A5 Cost efficacy of a clinical pathway to patients undergoing hip and knee replacement surgery. http://ClinicalTrials.gov/show/NCT00175201
University of Aarhus 2005-2008 complete (n=80)
Randomised controlled trial, with cost efficacy and cost effectiveness analysis, to evaluate (cost?) effectiveness of a proactive care and rehabilitation program compared to current care.
Assessed at discharge, 3, 12 and 24 months post-discharge. Primary outcome measures, length of stay, QoL (EQ-5D and SF-36/SF-6D); secondary measures, pain and disability (Harris Hip Score/Danish Knee Arthroplasty Register Score).
Adults with primary OA of hip or knee and waiting for total joint replacement surgery.
A6 Treatment and rehabilitation of patients with hip arthroplasty to regain walk and work efficiency and quality of life. http://clinicaltrials.gov/show/NCT00638417
Norwegian University of Science and Technology 2006-2007 complete (n=24)
Randomised controlled trial to assess comparative effectiveness of treatment followed by an intensive physical training program or conventional rehabilitation program.
Outcome measures – not specified
Adults (18-65 years old) with primary, unilateral OA undergoing hip arthroplasty.
A7 Effect of post-operative weight bearing status on clinical and radiological outcome of cementless femoral component. http://www.controlled-trials.com/ISRCTN53323735
Department of Health (UK) 2005-2007 complete (n=40)
Randomised controlled trial to assess clinical and radiological outcomes of full vs partial weight bearing following THR.
Assessed pre-operatively and at 6 weeks, 6 months, 1 and 2 years post-operatively. Outcome measures, migration of stem (radiologically), Harris Hip Score, WOMAC and SF-36.
Patients following cementless total hip replacement.
17
A8 Alberta hip and knee replacement project. http://ClinicalTrials.gov/show/NCT00277186
Alberta Bone and Joint Health Institute 2005-2006 complete (n=3434)
Randomised controlled trial to establish effectiveness, with regard to patient outcomes and cost-effectiveness, of a new arthroplasty care model compared to existing conventional approach.
Assessed at 3 and 12 months post surgery. Primary outcome measure, QoL; secondary outcome measures, health resource utilisation, wait time, safety, cost utility, patient and provider satisfaction.
Adults (18 years and over) undergoing hip or knee arthroplasty.
A9 Safety of non-delayed weight bearing after total hip replacement with non-cemented fiber metal taper stem. http://ClinicalTrials.gov/show/NCT00179088
Vanderbilt University 2003-2006 complete? (n=33) ongoing at last update,Nov 06
Randomised controlled trial to compare effect of immediate weight bearing activity vs no weight bearing following cementless total hip replacement.
Assessment pre-operatively? and at 6 weeks, 3 months, 1 and 2 year post-operatively. Outcome measures, femoral stem subsidence, return to work status at 2 years, patient’s walking status, joint ROM, presence of pain and severity if present, Harris Hip Score and SF-36.
Adults (18-90 years old) undergoing primary total hip arthroplasty due to any form of arthritis affecting the hip.
A10 A targeted strengthening program following total hip replacement. http://ClinicalTrials.gov/show/NCT00222300
University of Melbourne 2003-2005 complete (n=30)
Randomised controlled trial to evaluate effectiveness of post-operative lower limb strengthening program compared to usual care.
Primary outcome measure, lower limb strength (step test); secondary outcome measures, WOMAC pain, stiffness and function scores, function (Timed up-and-go test), AQoL, Spatiotemporal measure of walking, hip joint torques.
Patients who had undergone uncomplicated total hip replacement within previous 6-8 weeks and able to walk 45m independently.
A11 Weight-bearing recommendations after replacement of the hip or knee joint. http://ClinicalTrials.gov/show/NCT00266396
Verein zur Förderung der Rehabilitationsforschung in Schleswig-Holstein 2002-2004 complete? (n=352), ongoing at last update, Dec 05.
Randomised controlled trial – exact details not provided.
Outcome measures, WOMAC physical function score, leg specific stiffness and pain, SF-36 physical component, Lequesne Hip/Knee score.
Patients with osteoarthritis or femoral head necrosis due to receive elective unilateral hip or knee joint replacement
18
A12 Muscle function in elderly postoperative patients http://ClinicalTrials.gov/show/NCT00559780 (Suetta et al., 2004; Suetta et al., 2008)
Bispebjerg Hospital 2000-2003
Two part study comprising a cross-sectional survey and an intervention study. The latter consisted of a randomised controlled trial to compare effectiveness of resistance training, neuromuscular electrical stimulation of the quadriceps muscle and standard rehabilitation programs in older post-operative patients. To establish if there was any benefit to patients receiving additional training in the early post-surgical phase.
Outcomes measures – not specified Adults (60 years and over) undergoing unilateral hip replacement due to osteoarthritis.
SECTION B – SYSTEMATIC REVIEWS
Year Title Sample Methodology/Comments Summary
2009 Effectiveness of physiotherapy exercise following hip arthroplasty for osteoarthritis: a systematic review of clinical trials (Minns Lowe et al., 2009).
Prospective comparative clinical trials that compare physiotherapy exercise with standard/usual care, or two type of physiotherapy exercise regimes, after hospital discharge following elective primary total hip replacement arising from OA.
Computerised search (to April 2007) unrestricted by date or language of: AMED, CINAHL, EMBASE, KingsFund database and MEDLINE. Hand search of articles in Physiotherapy and Physical Therapy, and conference proceedings in Journal of Bone and Joint Surgery.
27 relevant studies identified, of which 8 met criteria for inclusion in the review.
Outcomes of interest: function, quality of life, mobility, range of hip joint motion and muscle strength.
Concludes insufficient evidence of good quality currently available to establish effectiveness of physiotherapy exercise after primary hip arthroplasty for OA. Indicates further well-designed studies are required.
2008 Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy. (Khan et al., 2008).
Cochrane Review
RCTs comparing multidisciplinary rehabilitation programs with routine services following hip or knee replacement due to arthropathy (including OA and RA).
Computerised search of Cochrane Musculoskeletal Group Trials Register, Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and CINAHL, Australian Medical Index, UK NHS National Research Register and citation search using SCISEARCH (September 2006)
50 relevant studies identified, of which only 5 met inclusion criteria for the review: covering inpatient and home-base rehabilitation. Outcomes of interest include limitation in impairment and activity/function, limitation in participation, cost of episode of care, length of stay, service utilisation, readmission, mortality rates and carer burden/strain.
Concludes some evidence (silver level) to suggest early multidisciplinary rehabilitation programs can improve outcomes following hip or knee replacement. Highlights the need for further high quality research.
19
SECTION C – GUIDELINES
C1. The benefits of ambulatory physiotherapy for patients able to leave the surgery department directly for home just after total hip replacement. Development of French guidelines for clinical practice (Genêt, Gouin, Coudeyre, Revel, & Rannou, 2007). The SOFMER (French Society of Physical and Rehabilitation Medicine) methodology, which includes a systematic review, collection of current practice and external review by a multidisciplinary expert committee, was used to develop these guidelines. Of the 60 relevant studies identified in the literature search only 16 satisfied the inclusion criteria. These studies indicated some benefit of ambulatory physiotherapy for patients discharged home directly following THR, namely improved muscle strength and function. Studies are, however, methodologically limited and future trials are deemed necessary. The current guidelines recommend ambulatory physiotherapy (as directed by French clinical practice) for patients discharged home directly from the surgical department.
SECTION D – NON-SYSTEMATIC REVIEWS
Year Title Sample Methodology/Comments Summary
2002 Rehabilitation after total hip replacement for osteoarthritis (Brander & Mullarkey, 2002)
N/K1
Studies of rehabilitation interventions pre- and post- total hip arthroplasty surgery resulting from OA.
N/K3 Approx 120 articles reviewed for this article1.
Concludes that there are no prospective randomised trials to determine the most efficacious exercise protocols following surgery. Highlights need for more research to establish most safe, efficacious and cost-effective rehabilitation regimes following THA.
2007 Physical training in rehabilitation programs before and after total hip and knee arthroplasty (Dauty, Genty & Ribinik, 2007).
Literature reviews or RCTs that investigate physical training as part of the rehabilitation regime before and/or after knee or hip arthroplasty.
Computerised search (1966-2006) of MEDLINE and Cochrane Database. Studies judged using PEDro criteria.
152 relevant studies identified of which 14 were included in the review: 2 reviews, 7 studies concerning THA and 5 TKA.
Results are difficult to interpret due to sample sizes, different physical training regimes, use of different outcome measures, high drop out rates and no matched control population. Conclude that current evidence suggests no benefit to pre-operative physical training for either THA or TKA. In contrast, postoperative benefit was indicated for THA, but insufficient evidence was available regarding the effect for TKA. All studies suggested supervised physical training, and some also that training was progressive and adaptive. Further good quality research is suggested, including cost-effectiveness studies.
3 A full copy of this article could not be obtained to clarify the methodology used.
20
SECTION E – CASE STUDIES
Year Title Sample Methodology/Comments Summary
2008 Cost-effectiveness of intensive exercise therapy directly following hospital discharge in patients with arthritis: results of a randomized controlled clinical trial (Bulthuis et al., 2008)
RCT.
85 patients with arthritis (OA and RA) admitted to hospital for flare-up or elective hip or knee arthroplasty. Randomised to receive a 3-week intensive exercise training program (n=50) or usual care (n=35). Note this is part of a larger study consisting of 114 patients in total.
To evaluate cost-effectiveness and cost-utility of an intensive exercise training regime directly after hospital discharge compared to usual care.
Assessed at baseline and at 3, 13, 26 and 52 weeks. Costs measured prospectively on a monthly basis.
Outcomes: QALYs (SF-6D and VAS personal health), HAQ, MACTAR, EPMROM, cost and incremental cost effectiveness.
Patients receiving intensive exercise showed a significantly greater improvement in VAS personal health, MACTAR and EPMROM outcomes at 6 months compared to those receiving usual care. No significant difference in SF-6D was detected at 6 months, and at 1 year outcomes were similar for both groups.
At 1 year post-discharge, the intensive exercise program was substantially cheaper €718 per patient, resulting in a reduction in mean total cost per QALY.
Concludes that intensive exercise training following hospital discharge results in better QoL at lower cost after 1 year than usual care. Highlights such training should be implemented after hospital discharge of patients with arthritis
2007 Arthritis patients show long-term benefits from 3 weeks intensive exercise training directly following hospital discharge (Bulthuis et al., 2007).
RCT.
114 patients with arthritis (OA and RA) admitted to hospital for flare-up or elective hip or knee arthroplasty. Randomised to receive a 3-week intensive exercise training program (n=60) or usual care (n=54).
To assess the efficacy of a short-term intensive rehabilitation regime after discharge from hospital.
Assessed at baseline and at 3, 13, 26 and 52 weeks. Outcomes: EPMROM, HAQ, MACTAR, HRQoL and RAND-36.
16 patients lost to follow up.
The intensive exercise program resulted in faster and greater improvement in patients compared to usual care with regards all outcome measures except HRQoL. At final follow up EPMROM and MACTAR remained significantly higher, and mean differences clinical greater, in the intensive exercise group compared to usual care. Concludes intensive exercise training following discharge from hospital, improves return of function for patients with arthritis.
2009 Group physiotherapy provides similar outcomes for participants after joint replacement surgery as 1-to-1 physiotherapy: a sequential cohort study (Coulter, Weber & Scarvell, 2009).
Controlled cohort study.
51 consecutive patients able to weight-bear following hip or knee replacement surgery for OA. Two groups those operated in first 4 months - group physiotherapy, those in second 4 months - individualised home physiotherapy for post-operative rehabilitation.
To compare effectiveness and efficiency of class-based vs. home-based physiotherapy for patients undergoing TJR surgery. Assessed preoperatively, at discharge and at 5 and 12 weeks post-operatively. Outcomes WOMAC, SF-36, TUG test, knee ROM, 6-m walk test, patient evaluation questionnaire and staff time costs.
Both groups showed significant improvement in outcomes at 12 weeks post-operatively compared to discharge, with no significant differences discernable between groups.
Class-based physiotherapy was accessed more frequently than the individualised program, although the physiotherapist’s time was less per patients per visit in the class-based compared to home setting. Concludes that class-based physiotherapy is a more efficient service without any compromise to patient outcomes.
21
2005 Perceived self-efficacy gained from, and health effects of, a rehabilitation program after hip joint replacement (Dohnke, Knauper & Muller-Fahrnow, 2005)
Cohort study.
1065 patients undergoing multidisciplinary rehabilitation following hip replacement.
To examine effects of multidisciplinary inpatient rehabilitation program following hip replacement.
Assessed at admission, discharge and 6-month follow up. Outcomes: disability, pain, depressive symptoms and self-efficacy to deal with disability and pain.
Significant improvements in pain, disability, depressive symptoms and self-efficacy at discharge compared to admission. Patients with higher self-efficacy at baseline or with large improvements in self-efficacy during the rehabilitation program had significantly better health outcomes. In general these differences were similar at 6-month follow up.
Concludes that a routine multidisciplinary inpatient rehabilitation program can improve patient self-efficacy following hip replacement surgery.
2005 Recovery of physical function and patient's satisfaction after total hip replacement (THR) surgery supported by a tailored guide-book (Fortina et al., 2005)
Cohort study.
365 consecutive patients with OA undergoing associated THR surgery. Provided with a customised guide outlining the hospitalisation period and postoperative rehabilitation program.
To assess the effect of providing a customised guide on patients’ outcomes.
Assessed at preoperatively, discharge and 3-month follow up. Outcomes: Harris Hip Scpre and patient satisfaction questionnaire.
Overall satisfaction was high at discharge and at 3 months postoperatively (>80%). There was significant improvement in Harris Hip Scores postoperatively compared to baseline. With greatest improvement in pain and physical function scores.
Concludes that the guide was well accepted by patients and was effective at improving patient satisfaction and early recovery following surgery.
Nb: recovery and satisfaction may have been independent of guide.
2008 A targeted home- and center-based exercise program for people after total hip replacement: A randomized clinical trial (Galea M.P. et al., 2008).
RCT.
23 patients with unilateral THR randomised to unsupervised home-based (n=12) or supervised centre-based (n=11) exercise programs lasting 6 weeks.
To compare outcomes of patients receiving targeted home- or centre-based exercise programs.
Assessed at baseline and followed-up at 8 weeks. Outcomes: QoL, physical function (TUG test, stair climbing, and 6-min walk test), WOMAC and spatiotemporal measures of gait.
Both groups showed significant improvement in QoL, stair climbing, TUG and 6-min walk tests, walking speed, cadence, step length, double-support time and step length symmetry and differential, at follow up. However, no significant differences between regimes were indicated.
Concludes targeted strengthening exercise is effective, leading to significant improvements for patients following THR: irrespective of whether unsupervised at home or supervised at a centre.
2003 Exercise improves early functional recovery after total hip arthroplasty (Gilbey et al., 2003).
RCT.
57 patients undergoing THA due to OA. Randomized to receive routine physical therapy or an 8-week customised exercise program prior to THA which continued post-operatively.
To assess effectiveness of a exercise program for patients undergoing THA compared to usual care.
Assessed 8 and 1 week preoperatively and 3, 12 and 24 weeks postoperatively. Outcomes: strength, ROM and physical function tests (WOMAC).
Groups were similar at baseline. 1 week prior to surgery only the exercise group showed significant improvement in WOMAC, combined hip strength and hip flexion ROM.
Postoperatively the exercise group had significantly better outcomes all time points compared to controls.
Concludes that perioperative exercise programs are effective at improving recovery of physical function following THA in patients with hip OA.
22
2004 Perceived exertion and rehabilitation with arm crank in elderly patients after total hip arthroplasty: a preliminary study (Grange et al., 2004).
Pilot RCT.
14 older patients with OA leading to THA. Randomised into a control group who received traditional rehabilitation (n=7, mean age 75.4 ± 5.1 years) or a training group who received additional arm-crank training (n=7, mean age 74.9 ± 5.0 years).
To assess effects of a 6-week arm crank rehabilitation program on physiological, perceptual and physical outcomes.
Outcomes: heart rate, perceived exertion, cardioventilatory and functional responses.
At the outset of the training program no relationship between heart rate and perceived exertion was found, however, at the end of the program 5 patients showed a significant heart rate and perceived exertion relationship. Cardioventilatory and functional outcomes of the arm-crank group were significantly greater than the control group.
Concludes that following habituation most patients’ physical sensations are connected to physiological responses. In such cases, perceived exertion could be used to regulate exercise intensity toward the end and following rehabilitation.
2008 Low-frequency electric muscle stimulation combined with physical therapy after total hip arthroplasty for hip osteoarthritis in elderly patients: a randomized controlled trial (Gremeaux et al., 2008).
RCT.
29 patients referred for rehabilitation following THA for OA. Randomised into usual care i.e. physical therapy including resistance training (n=13, mean age 76±10 years) or simultaneous low-frequency electric muscle stimulation of bilateral quadriceps and calf muscles together with conventional physical therapy (n=16, mean age 78±8 years).
To evaluate effects of low-frequency electric muscle stimulation associated with usual physiotherapy care on elderly patients after THA for OA.
Assessed before and after 5 weeks rehabilitation. Outcomes: maximal isometric strength of knee extensors, FIM, 6-min walk test, 200m fast walk test and length of stay.
Low-frequency electric muscle stimulation was well tolerated and was associated with a significantly greater improvement in knee extensor strengthening on operated side, better balance of muscle strength between both legs, greater improvement in FIM scores, compared to usual care. Both regimes gave similar results regarding walk tests and length of stay.
Concludes that low-frequency electric muscle stimulation is safe and tolerated by patients following THA for OA. Furthermore it facilitates greater knee extensor strengthening than usual care, which is associated with greater functional independence following THA.
2009 Early maximal strength training is an efficient treatment for patients operated with total hip arthroplasty (Husby et al., 2009)
RCT.
24 patients with OA leading to THA randomly assigned to maximal strength training (leg press & abduction 5 x weekly for 4 weeks in addition to conventional care) or conventional rehabilitation (supervised physical therapy 3-5 x weekly for 4 weeks).
To compare outcomes of maximal strength training vs. conventional rehabilitation.
Assessed 1 and 5 weeks post-operatively.
Outcomes: 1-repetition maximum (1RM) leg press strength, 1RM abduction strength, rate of force development, gait patters, work efficiency and QoL.
Maximal strength training results in significantly higher performance in leg press, rate of force development and hip abduction, with a trend towards greater work efficiency (p=0.065), after 4-weeks training compared to conventional rehabilitation. No significant differences between the groups concerning gait variables, work efficiency or QoL were detected 5 weeks post-operatively. Concludes that maximal strength training is a viable and effective rehabilitation method for regaining muscular strength following THR surgery.
23
2007 Targeted early rehabilitation at home after hip and knee joint replacement: does it work? (Iyengar et al., 2007).
Cohort study.
1034 patients undergoing THR or TKR surgery, of which 394 were eligible for the targeted early rehabilitation at home scheme (RAHS). OA was the primary diagnosis in the majority (>97%) of patients. Mean age of RAHS group=72.9 years.
To evaluate the benefit and cost effectiveness of RAHS following THR or TKR surgery.
Outcomes: length of hospital stay, duration on the scheme, number of bed days saved, cost appraisal, readmission rate and complication rate.
There was a marked reduction in the length of in-patient stay for patients on the RAHS without any increase in complication rate. Patient with THR required significantly fewer visits by the rehabilitation team than those who had had TKR surgery.
The RAHS resulted in significant saving for the trust without any increase in readmission or complication rates.
2003 Using cost-effectiveness analysis to compare Hospital at Home and in-patient interventions. Parts 1 & 2 (Jester & Hicks, 2003a, b).
Cohort study.
109 patients with a diagnosis of OA of hip or knee booked for total hip or knee replacement surgery. 64 patients received Hospital at Home (HaH) care, and 45 specialist orthopaedic in-patient care following surgery. Mean age 74 years (range 64-86).
To compare the effectiveness and cost-effectiveness of (HaH) and in-patient care following total joint replacement.
Assessment preoperatively, day of discharge from hospital or HaH scheme, 6 weeks and 6 months postoperatively Outcomes: WOMAC, modified Hospital Patient Satisfaction Index, post-operative complications, impact on carers (HaH group, interview and VAS of help given) and cost-benefit analysis.
Both groups showed a reduction in symptoms across time, and no significant difference between inpatient and HaH groups for joint pain or difficulty was found, however the HaH group showed markedly lower levels of joint stiffness. Overall, the HaH group showed significantly greater satisfaction than the inpatient group. Post-operative complication rates were similar across the groups.
Concludes that HaH was significantly more effective in terms of patient satisfaction and reduction of joint stiffness, and comparable to in-patient care for joint pain, disability and complication rates. Regarding cost-effectiveness HaH was found to be less costly than traditional in-patient care primarily as a result of reduced hospital stay. Conclude however that early discharge to HaH should remain a matter of informed choice for patients and their families
2009 Group physiotherapy provides similar outcomes for participants after joint replacement surgery as 1-to-1 physiotherapy: a sequential cohort study (Johanson et al., 2009).
Cohort study.
36 patients, aged 65-88 years, receiving rehabilitation following THA as a result of OA.
Retrospective study of 32 patients who receive inpatient rehabilitation; prospective descriptive study of 4 patients accessing 2 sub-acute rehabilitation units.
To assess comparable short-term effectiveness of inpatient vs. sub-acute rehabilitation units.
Outcome: FIM scores
Greater improvement in total FIM scores and the motor and self-care subscales was observed for patients receiving inpatient rehabilitation compared to those accessing sub-acute rehabilitation units.
Concludes that further research is needed to investigate the functional outcomes of different rehabilitation settings and programs (including intensity and duration) for older patients following THA surgery.
24
2008 Hip arthroplasty with the thrust plate prosthesis in patients of 65 years of age or older: 67 patients followed 2-7 years (Karatosun, Unver & Gunal, 2008).
Retrospective cohort study. 67 patients (50 female, 17 male; 71 hips) >65 years old who underwent hip arthroplasty resulting from primary or secondary coxarthrosis, followed by accelerated rehabilitation programs. First consecutive 36 patients - partial weight bearing from 2nd post-operative day and full weight bearing after 6 weeks; following 31 patients - full weight bearing from day 2. Mean age 71 (range 65-89).
To assess the outcomes of a cementless thrust plate prosthesis in patients over 65 years of age and to establish a suitable rehabilitation regime.
Assessed preoperatively and followed up over a mean of 48 (range 28-87) months post-operatively.
Outcomes: Harris Hip Score and radiographic assessment.
The Harris Hip Score was highly significantly increased at final follow-up compared to pre-operative scores. However, time of full weight bearing did not affect Harris Hip Scores.
Concludes that for older patients, thrust plate prosthesis is indicated together with an accelerated rehabilitation program with early weight bearing.
Nb: some patients were also enrolled in another study which involved 8 weeks physiotherapy and education pre-operatively. Results should be viewed with caution.
2009 Cost-effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty (Larsen et al., 2009).
Cost effectiveness study associated with an RCT (described in study below, see Larsen, Sorensen, et al. 2008).
To assess the cost effectiveness of an accelerated periopertive care and rehabilitation regime compared to standard rehabilitation regime for patients undergoing THA or TKA.
Activity-based costing analysis conducted from patients’ visit prior to surgery to one year post-operatively.
The accelerated regime was significantly cheaper than the standard rehabilitation regime. Patients who had THA and received the accelerated regime had significantly greater gain in QALYs compare to patients under the standard regime. In contrast there was no clinical or significant difference in QALYs between the two regimes for patients who underwent TKA.
Concludes an accelerated perioperative care and rehabilitation program can be clinically more effective and cost saving after THA, however, whilst it is cost saving following TKA no further clinical benefit is gained.
2008 Effectiveness of accelerated perioperative care and rehabilitation intervention compared to current intervention after hip and knee arthroplasty. A before-after trial of 247 patients with a 3-month follow-up (Larsen, Hvass, et al., 2008).
Controlled cohort study.
247 patients undergoing elective primary THA or TKA, largely as a result of OA. 105 patients prior to, and 142 after, the implementation of an accelerate perioperative care and rehabilitation program.
To assess the effectiveness of an accelerated perioperative care and rehabilitation regime for patients following total joint replacement surgery.
Outcomes: length of stay in hospital, adverse effects within 3 months post surgery.
The length of stay was significantly reduced with the introduction of the accelerated program. However, no significant differences in adverse effects postoperatively were found.
Concludes the accelerated perioperative care and rehabilitation program following THA or TKA was effective, and the results obtained concurred with those from the efficacy study (see below).
25
2008 Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up (Larsen, Sorensen, et al., 2008).
RCT.
87 patients receiving primary THR, or knee replacement surgery. Randomised to receive a new accelerated perioperative care and rehabilitation procedure, or current perioperative care.
To evaluate efficacy of an accelerated perioperative care and rehabilitation regime for patients recovering from joint replacement.
Assessed at baseline and at 3-month follow up.
Outcome measures: length of stay and QoL (EQ-5D)
The mean length of stay in hospital for patients receiving the new perioperative care and rehabilitation procedure was significantly shorter than those receiving usual care. Furthermore at follow-up there was significantly greater improvement in QoL in the new intervention group.
Concludes that a novel accelerated perioperative care and rehabilitation for patients undergoing THR or knee replacement surgery is effective and has additional benefits for patients and the hospital.
2004 A randomized controlled trial of osteopathic manipulative treatment following knee or hip arthroplasty (Licciardone et al., 2004).
RCT.
60 patients (42 women, 18 men) undergoing hip or knee arthroplasty for OA or hip fracture. Randomised to receive osteopathic manipulative treatment or sham treatment, in addition to standard care.
To evaluate the efficacy of osteopathic manipulative treatment for patients undergoing joint replacement surgery.
Outcomes: Functional Independence score, analgesic use, length of stay, rehabilitation efficiency and SF-36 (at outset of rehabilitation and 4 weeks post-discharge).
Across 19 outcomes measure, the only significant difference between groups indicated was with functional independence score, which was significantly lower in the osteopathic manipulative group.
Stratified analysis showed that poorer outcomes were associated with patients undergoing knee arthroplasty only.
Concludes that osteopathic manipulation is not an effective treatment for this population.
2008 The benefit of modified rehabilitation and minimally invasive techniques in total hip replacement (Lilikakis, Gillespie & Villar, 2008).
Controlled cohort study.
122 patients (130 hips) undergoing THR (due to OA, exception 2 patients with avascular necrosis). 44 (retrospective) patients - usual care pathway; 38 consecutive patients - novel rehabilitation protocol; 40 consecutive patients - novel rehabilitation along with modified, minimally invasive THR surgery.
To evaluate whether an intensive rehabilitation program alone or with a modified, minimally invasive surgical procedure, affects speed of rehabilitation and/or length of hospital stay following THR.
Primary outcomes, length of stay in hospital, and time to: walking with a frame with assistance, independent walking with crutches and practising stairs.
The new rehabilitation program alone was associated with a significant reduction in time take to achieve assisted walking, independent walking and stairs, and length of stay in hospital compared to the conventional care pathway.
The addition of the modified surgical procedure was associated with further significant reduction in time taken to achieve the assisted walking and stairs tasks, and length of stay.
Concludes a new rehabilitation program can reduce length of hospital stay and speed up rehabilitation, however, modified minimally invasive THR has further short-term benefits following THR.
26
2008 Inpatient compared with home-based rehabilitation following primary unilateral total hip or knee replacement: a randomized controlled trial (Mahomed et al., 2008).
RCT.
234 patients undergoing primary unilateral total hip or knee replacement. Randomised to receive home-base or inpatient rehabilitation.
To evaluate and compare the effectiveness and costs of home-based vs. inpatient rehabilitation following TJR surgery.
Assessed pre-operatively and at 3 and 12 months post-operatively.
Outcomes: Cost, Patient satisfaction, WOMAC and SF-36.
The prevalence of postoperative complications was similar in both groups of patients.
Patients in both groups showed significant improvement with regard to the 3 outcomes measures at 3 and 12 months follow up compared to baseline. However, no significant difference across groups was identified.
In-patient rehabilitation was significantly more expensive than home-based care.
Concludes that despite concerns regarding the early discharge of patients from hospital, no difference in outcomes found. Therefore, home-based rehabilitation is a more cost-effective regime following TJR surgery.
2000 Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement (Mahomed et al., 2000).
Retrospective cohort survey. 146 older patients who had undergone THR or TKR surgery.
To ascertain determinants of rehabilitation setting, i.e. home-based or inpatient, and the influence on early functional outcomes, following total joint replacement.
Assessed at mean follow up of 8 months post operatively.
Outcomes: WOMAC, SF-36 and patient satisfaction.
96 patients completed the survey (mean age = 66 years, 70% women, 79% primary diagnosis of OA).
39% of patients received home-based rehabilitation; determinants include male sex, preference for home-based care and knowledge regarding total joint replacement.
No significant differences between patients in the different rehabilitation settings were indicated by WOMAC, SF36 or patient satisfaction questionnaires.
Conclude that these results support the continued use of home-based rehabilitation.
2006 Influence of a 6-week arm exercise program on walking ability and health status after hip arthroplasty: a 1-year follow-up pilot study (Maire et al., 2006).
Pilot RCT.
14 elderly patients undergoing THA due to OA, randomised to control rehabilitation (6 week program) or training group with addition of arm exercises using an ergometer. Resident at rehabilitation centre for duration of study.
To evaluate the effect of an upper-limb interval-training program after THA.
Assessed 1 month prior, and at 2 and 12 months post surgery.
Outcomes: WOMAC and 6-min walking test.
Both groups of patients significantly improved in performance and WOMAC scores over the study period. However, the group undertaking additional training showed a significantly greater improvement than those receiving usual rehabilitation.
Concludes upper-limb training may have an important role in post-operative THA.
27
2004 A specific arm-interval exercise program could improve the health status and walking ability of elderly patients after total hip arthroplasty: a pilot study (Maire et al., 2004).
RCT.
14 elderly patients undergoing THA due to OA, randomised to control rehabilitation (6 week program) or training group with addition of arm exercises using an ergometer. Resident at rehabilitation centre for duration of study.
To evaluate the effect of an upper-limb interval-training program after THA.
Assessed 1 month prior, and at 2 months post surgery.
Outcomes: VO2, WOMAC and 6-min walking test.
There was a significant improvement in all dimensions of WOMAC across both groups (except controls for physical function dimension). The training group showed greater VO2 peak, distance walked and functional status than controls.
Concludes that improved physical fitness and functional status in the training group appear to reflect greater health status.
2003 Recovery after total hip joint arthroplasty in elderly patients with osteoarthritis: positive effect of upper limb interval-training (Maire et al., 2003).
RCT.
14 elderly patients undergoing THA due to OA, randomised to control rehabilitation (6 week program) or training group with addition of arm exercises using an ergometer. Resident at rehabilitation centre for duration of study.
To evaluate the effect of an upper-limb interval-training program after THA.
Assessed 1 month prior, and at 2 months post surgery.
Outcomes: VO2, WOMAC and 6-min walking test.
VO2 was significantly greater in the training group only, patients in this group also walked significantly further than those receiving control rehabilitation.
Conclude the results highlight the importance of physical training for postoperative rehabilitation programs for patients undergoing THA.
2009 Is early weight bearing resumption beneficial after total hip replacement? (Merle et al., 2009).
Cohort study.
14 patients (8 men, 6 women) attending rehabilitation centre following THR. Age: 57-86 years.
To assess effect of early weight bearing on postural balance control.
Postural behaviour assessed in uncontrolled and imposed conditions.
Outcomes: centre of resultant & plantar pressure, centre of gravity.
Weight bearing by the implanted extremity led to a significant increase in all outcome measures along the mediolateral axis only. Furthermore, greater displacement along the mediolateral axis was found for the healthy limb compared to the implanted limb.
Concludes early weight bearing during rehabilitation leads to less stability and greater energy expenditure. This must be considered when devising rehabilitation protocols for patients under THR.
2006 Reducing incision length or intensifying rehabilitation: what makes the difference to length of stay in total hip replacement in a UK setting? (Peck, Foster & McLauchlan, 2006).
Controlled trial.
96 patients undergoing standard (n=45) or minimal incision (n=51) THA. Patients received either routine or an intensive physiotherapy rehabilitation program. Patients matched by sex, age and body mass index.
To compare outcomes of standards vs. minimal incision THA techniques and routine vs. intensive rehabilitation.
Assessed pre-operatively at 1 year following surgery.
Outcomes: Blood loss, length of stay, Oxford Hip Score.
With regards to rehabilitation the intensive physiotherapy regime led to shorter post-operative stay in hospital compared with routine rehabilitation.
Concludes that intensive post-operative physiotherapy can significantly reduce the length of stay in hospital for patients undergoing THA.
28
2008 Self-reported functional outcome after primary total hip replacement treated with two different perioperative regimes: a follow-up study involving 61 patients (Petersen, Andersen & Soballe, 2008)
Mixed: RCT and cohort study.
79 patients (of which 61 fulfilled criteria) randomised to received optimised perioperative care or conventional perioperative care. Also, age matched controls from 4098 non-institutionalised Danish adults collected by the Danish National Institute of Public Health.
To assess the effect of optimising perioperative care on self-reported functional outcomes.
Assessed pre-operatively and at discharge with WOMAC.
Assessed against controls at 6 months after THR surgery using SF-36.
Postoperatively, the conventional perioperative group showed significantly greater improvement in total WOMAC and the WOMAC function subscale than the optimised care group. All other outcomes were similar.
At 6 months, THR patients scored significantly higher in the SF-36 general health subscale, but significantly lower in 3 SF-36 physical subscales
Concludes that optimisation strategies during admission do not appear to affect functional outcomes following THR. Furthermore, it is suggested that may be the potential for physical functioning is not met in these patients and that further studies are required.
2009 A specific inpatient aquatic physiotherapy program improves strength after total hip or knee replacement surgery: a randomized controlled trial (Rahmann, Brauer & Nitz, 2009).
RCT.
65 patients (30 men, mean age 69.6± 8.2 years) undergoing primary hip or knee arthroplasty for OA. Randomised to aquatic physiotherapy, non-specific water exercise or additional ward physiotherapy (control).
To assess effect of inpatient aquatic therapy in addition to conventional ward physiotherapy.
Evaluation preoperatively and at 14, 90 and 180 days after surgery.
Primary outcome measures: hip abductor strength, walking speed and self-reported disability (WOMAC).
Note primary assessment at day 14 after which patient was free to undertake whatever rehabilitation they chose (i.e. not controlled).
Baseline demographics of the three groups did not differ significantly.
At day 14, hip abductor strength was significantly greater in the aquatic physiotherapy group compared to the other two groups: there was no significant difference across groups for the remaining outcome measures. Although relative differences between groups favoured aquatic physiotherapy. No adverse side-effects of aquatic physiotherapy occurred.
Concludes that specific inpatient aquatic physiotherapy is safe and beneficial for early recovery of hip strength following joint replacement. Highlights the need for further research to confirm the findings.
2007 The effect of early weight bearing on migration pattern of the uncemented CLS stem in total hip arthroplasty (Strom, Huss & Larsson, 2007).
RCT.
42 patients, under 65 years of age, undergoing THA as a result of OA. Randomised to early unrestricted weight bearing and intensive physiotherapy, or to partial weight bearing with self-training.
To assess the effect of early weight bearing on an uncemented CLS stem used for THA.
Evaluated at 3 and 24 months post-operatively.
Outcomes: radiosterometic assessment.
Subsidence of the CLS stem was similar in both groups at 24 months post-operation, and the actual loading on the operated leg did not affect subsidence.
Concludes that early full weight bearing coupled with intensive physiotherapy does not increase the risk of early loosening when using an uncemented CLS stem in THA.
29
2006 Unrestricted weight bearing and intensive physiotherapy after uncemented total hip arthroplasty (Strom, et al., 2006).
RCT.
36 patients (19 women, 17 men) undergoing uncemented THA. Randomised to unrestricted weight bearing and intensive physiotherapy, or 3-months partial weight bearing with short self-training program. Mean age 54.4 years.
To assess the effectiveness of partial weight bearing and intensive physiotherapy following THA.
Assessed at 1 week, and at 3, 6 and 12 months post-operatively.
Outcomes: load during walking and muscle strength during abduction.
The average peak load was significantly greater for the unrestricted weight bearing group than the partial weight bearing group 1 week and 3 months post-operatively. However, no significant differences were apparent at 6 and 12 months follow up.
Concludes that the effect of unrestricted weight bearing and intensive physiotherapy on muscle strength following THA is debatable.
2008 Resistance training induces qualitative changes in muscle morphology, muscle architecture, and muscle function in elderly postoperative patients (Suetta et al., 2008).
RCT.
36 patients (60-86 years old) scheduled for unilateral hip replacement surgery as a result of OA. Randomised to receive: resistance training; electrical stimulation; or usual rehabilitation i.e. functional exercise.
To compare effects on musculature of different post-operative training regimes.
Assessed at baseline and followed up at 5 and 12 weeks post-operatively.
Outcomes: maximal dynamic muscle strength, muscle fibre area, muscle fibre pennation angle and stair walking power.
Resistance training resulted in a significant increase in all outcomes measures compared to baseline. No significant changes were observed for patients receiving electrical stimulation or usual rehabilitation.
Concludes that this study highlights the importance of resistance training in rehabilitation procedures for older patients following hip replacement surgery.
2004 Resistance training in the early postoperative phase reduces hospitalization and lead to muscle hypertrophy in elderly hip surgery patients - a controlled randomized study (Suetta et al., 2004).
RCT.
36 patients (60-86 years old) scheduled for unilateral hip replacement surgery as a result of OA. Randomised to receive: resistance training; electrical stimulation; or usual rehabilitation i.e. functional exercise.
Nb resistance training and electrical stimulation both in addition to usual rehabilitation regime.
To assess effects of immobilization and surgery on muscle size and function in older patients and to identify effective rehabilitation training regimes.
Assessed at baseline and followed up at 5 and 12 weeks post-operatively.
Outcomes: quadriceps cross-sectional area, isokinetic muscle strength, functional muscle performance and length of hospital stay.
Length of hospital stay was significantly shorter for the resistance training group compared to usual care. There was significant increase in cross-sectional area and muscle strength in the resistance training group only, although functional performance significantly improved in both resistance training and electrical stimulation groups (similar across the two groups).
Concludes that postoperative resistance training leads to significant improvement in muscle cross sectional area, strength and functional performance: benefits not seen with the usual rehabilitation regime. In addition, resistance training markedly reduced the length of hospital stay for older patients after hip arthroplasty.
30
2007 Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry (Thien et al., 2007).
RCT.
43 consecutive patients (23 women, 20 men) undergoing THA as a result of OA. Randomised to partial or full weight bearing during first 6 weeks post-operatively. Mean age 53 (range 41-63) years.
To evaluate the effects of full and partial weight bearing following cementless THA.
Assessed at baseline and 3 months post-operatively.
Outcomes: stem migration and rotation, cup translation and rotation, and femoral head penetration (using radiostereometric analysis).
At follow up there were no significant differences in any outcomes of partial or full weight bearing patient groups.
There were no re-operations during the first year.
Concludes full weight bearing is justified following uncemented THA.
2005 Selection of patients for inpatient rehabilitation or direct home discharge following total joint replacement surgery: a comparison of health status and out-of-pocket expenditure of patients undergoing hip and knee arthroplasty for osteoarthritis (Tribe et al., 2005).
Cohort study?
180 patients undergoing hip or knee replacement due to OA. Following acute care in hospital, patients were either discharged immediately to return home, or admitted to inpatient rehabilitation care before discharge home.
To compare patient outcomes and out-of-pocket expenses of patient
Assessed at before surgery and 1 year post-operatively. Outcomes: out-of-pocket expenses, SF-36 and WOMAC.
At 1 year post surgery, all groups showed significant improvement in patient outcome compared to at baseline. No significant differences were observed between groups.
Hip home and rehabilitation, and knee home patients all reported low out-of-pocket expenses over the year following surgery. Concludes that most patients can be discharged directly home following joint replacement surgery with excellent post-operative outcomes at 1 year. Further RCTs are suggested to explore which patients are most suitable for rehabilitation.
2004 Effects of a late-phase exercise program after total hip arthroplasty: a randomized controlled trial. (Trudelle-Jackson & Smith, 2004).
RCT
34 patients who had undergone THA 4-12 months previously. Randomised to a hip-exercise intervention focused on strength and postural stability exercises, or the control group that received basic isometric and ROM exercises (akin to early rehabilitation). Nb: reason for THA not stated
To assess effects of a late-phase exercise program on patients who had THA 4-12 months previously.
Assessed at outset and end of 8-week exercise program.
Outcomes: 12-item Hip Questionnaire, fear of falling, hip extensor, flexor, abductor and knee extensor muscle torque, and postural stability.
28 patients completed the study.
There was a significant improvement in self-perceived function, muscle strength and postural stability for patients receiving the hip-exercise intervention, in contrast, controls showed no change in any outcomes measured. Fear of falling remaining similar in both groups across the two time points. Concludes that specific hip-exercise programs focused on controlled weight bearing should be used 4-12 months post operatively to improve muscle strength and postural stability of patients after THA.
31
2007 The effect of exercise on hip muscle strength, gait speed and cadence in patients with total hip arthroplasty: A randomized controlled study (Unlu et al., 2007).
RCT.
26 patients randomised into home-exercise, in-hospital supervised exercise, and controls (no intervention).
To assess the effects of home vs. in-hospital exercise programs targeted at patients at least 1 year after receiving THA.
Assessed prior to start of program and after 6 weeks. Main outcomes: maximum isometric abduction torque of hip abductor muscles, gait speed and cadence.
Both the home and in-hospital exercise programs led to improvements in all three outcome measures. The controls also showed improvement in gait speed and cadence. However, both exercise groups improvement was significantly greater than that of controls for all outcomes, with the in-hospital exercise program resulting in greater improvement in maximal isometric abduction torque than the home group.
Concludes that both home and supervised exercise regimes are effective interventions 1 year after surgery. Furthermore, it is suggested that home exercise with regular supervision may be an appropriate recommendation.
2004 Comparison of two different rehabilitation programmes for thrust plate prosthesis: A randomized controlled study (Unver, Karatosum, Gunal & Angin, 2004).
RCT.
51 patients (60 hips) undergoing THA. Randomly assigned to early partial weight bearing or early full weight bearing.
To evaluate the effects of early weight bearing following THA using a thrust plate prosthesis.
Assessed pre-operatively and at 3 months post-operatively. Outcomes: ROM, muscle strength, functional test (6-min walk), hip function (Harris Hip Score) and radiographic parameters.
Patients in the early full weight bearing group performed transfer activities earlier, had a shorter stay in hospital and were able to walk further at discharge than patients in the early partial weight bearing group.
At follow up the full weight bearing group had significantly better Harris Hip Scores, muscle strength, functional tests and shorter length of time on crutches than the partial weight bearing group. Concludes patients undergoing THA with thrust plate prosthesis respond beneficially to an accelerated rehabilitation program involving early full weight bearing activity.
2003 Comparison of two home care protocols for total joint replacement (Weaver et al., 2003).
RCT.
136 patients due to undergo elective TKR or THR primarily due to OA. Randomised to received existing care (n=67) or novel home-care protocol involving preoperative visits and fewer postoperative visits (n=69) Mean age 72 ± 7 years.
To assess the effectiveness of a “more-efficient” home visit protocol, i.e. less home visits, in the management of patients following THR or TKR.
Outcomes assessed 6 months postoperatively include functional status, lower extremity function, HRQoL, patient satisfaction, use and cost of healthcare services in the 6 months following surgery.
There were no significant differences in functional outcomes or HRQoL between patients receiving the two different home care protocols. Overall patient satisfaction was similar across the two groups although there was a tendency (but non significant p=0.059) for greater satisfaction with access to care for the novel home-care group.
Home healthcare costs were significantly lower (55%) for the new compared to the existing protocol; other costs were similar. Concludes that the new care protocol resulted in more efficient delivery of care without any compromise regarding patient outcomes.
32
2005 Rehabilitation of patients after hip arthroplasty using Continuous Passive Motion (Wilk & Franczuk, 2005).
RCT.
98 patients undergoing THR for OA. Randomised to begin rehabilitation 7 days after surgery involving Continuous Passive Motion (CPM), or tradition rehabilitation.
To evaluate outcomes of a rehabilitation program involving CPM.
Assessed prior to surgery and at 3, 7 and 10 days, and 1, 3 and 6 months post-operatively.
Outcomes: ROM, muscle strength, and Merle D’Aubigne Scale.
Patients receiving CPM rehabilitation had better outcomes and also had a significant reduction in pain symptoms and a shorter hospital stay than patients receiving traditional care.
Concludes that CPM during early rehabilitation markedly accelerates the rehabilitation process, is associated greater pain reduction resulting in greater comfort during exercise and a reduction in the length of stay in hospital.
SECTION F – PEER-REVIEWED ARTICLES
Year
Title Sample Methodology/ Comments
Summary
2006 Role of physiotherapy in peri-operative management in total knee and hip surgery (Lenssen & de Bie, 2006).
N/A N/K Concludes that physiotherapy combined with aerobic and strength training is of benefit for patients with hip or knee OA during both pre- and post-operative stages. When surgery is imminent, physiotherapy can aid by increasing self esteem and reducing depression and anxiety associated with surgery.
Post-operatively intensive physical exercise and Continuous Passive Motion results in quicker recovery times, shorter hospital stays and increased ROM. To maximise postoperative outcomes it is recognised that maintaining exercise regimes after discharge should be encouraged.