MS2.Chapter 43
-
Upload
kelly-cherry -
Category
Documents
-
view
168 -
download
0
Transcript of MS2.Chapter 43

1Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Chapter 43
Amputations

2Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Amputation
• Can occur through a joint (between the bones) or through a bone itself
• Disarticulation: term used for an amputation through the joint
• The general site of the amputation is described by the joint nearest to it

3Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
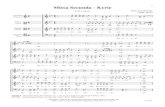
Figure 43-1

4Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Indications and Incidence
• Trauma• Common types of accidents and injuries leading to
amputation include those involving motorcycles and automobiles, farm machinery, firearms and explosives, electrical equipment, power tools, and frostbite
• Disease • Peripheral vascular disease, diabetes mellitus,
arteriosclerosis, and chronic osteomyelitis

5Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Indications and Incidence
• Tumors• Bone tumors that are very large and invasive
• Congenital defects • Convert a deformed limb into a more functional one
that can be fitted with a prosthetic device

6Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Diagnostic Tests and Procedures
• Vascular studies • Pulse volume recording • Thermography• Doppler ultrasound • Biopsy

7Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Medical Treatment
• Must include appropriate treatment and control of underlying diseases or injuries • Diet, medication, and exercise help patients with
diabetes and poor peripheral circulation • If peripheral vascular disease, encourage to stop
smoking; nicotine causes vasoconstriction • Trauma patient may have to be stabilized to
maintain normal heart rate and blood pressure

8Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Surgical Treatment
• Amputation at the lowest level that will preserve healthy tissue and favor wound healing
• Surgeon chooses one of two procedures, depending on condition of the extremity and the reason for the surgery • Closed amputations
• Create a weight-bearing residual limb, important for lower extremity amputations
• Open amputations• The severed bone or joint is left uncovered by a skin flap • Required when an actual or potential infection exists, as may
occur with gangrene or trauma

9Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Prostheses
• Artificial substitutes for missing body parts • Prosthetist creates and supervises use of prosthesis • A limb prosthesis may be placed while the patient is
still in the operating room • With lower extremity amputations, older or debilitated
patients, and infection, prosthesis fitting delayed until residual limb heals
• Can usually bear full weight on permanent prosthesis about 3 months after amputation

10Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Figure 43-2

11Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Figure 43-3

12Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Complications
• Hemorrhage and hematoma• Necrosis• Wound dehiscence• Gangrene• Edema• Contracture• Pain• Infection• Phantom limb sensation• Phantom limb pain

13Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Assessment
• Record conditions that resulted in need for amputation• Preexisting cardiovascular problems• Family history of diabetes, hypertension, and vascular diseases• Signs and symptoms that relate to the vascular condition or other
chronic and acute problems • Diet and fluid intake, intake of salt and alcohol, and use of tobacco • Exercise and rest and sleep habits as well as the effects of the
current symptoms on the patient’s usual activities • Patient’s psychosocial background may offer insight into how the
patient will tolerate treatments and procedures

14Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Physical Examination
• Height, weight, and vital signs• Assess neurovascular status • Skin color, texture, temperature, and turgor • Palpate peripheral pulses for quality, symmetry • Assess capillary refill• Sensation; ask patient to identify touch on extremities • Mental and emotional status and general cognitive
abilities; determines patient’s understanding of the illness and its implications

15Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Interventions
• Anxiety• Anticipatory grieving

16Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Postoperative Nursing Care
• Assessment• Monitor vital signs frequently in the first 48 hours• Inspect the dressing frequently for bleeding • If drain receptacle, note color and amount of drainage • Monitor patient’s temperature for elevations that may indicate
infection • Note any foul odor from the dressing • After the dressing is removed, inspect the residual limb for
edema • Document patient’s pain, including type, location, severity, and
response to treatment

17Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Postoperative Nursing Care
• Interventions• Decreased Cardiac Output • Pain• Risk for Infection• Impaired Skin Integrity and Risk for Impaired Skin Integrity• Disturbed Sensory Perception • Risk for Injury • Impaired Physical Mobility • Activity Intolerance • Self-Care Deficit • Anxiety, Fear, and Ineffective Coping • Disturbed Body Image

18Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Figure 43-4

19Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
The Older Adult Amputee
• May have needs that should be taken into consideration when planning and providing care
• Completely capable of learning but often requires smaller units of information, more repetition, more time
• During teaching process patients with glasses or hearing aids should have them in place
• Remind that phantom sensations are not uncommon or bizarre; this can reduce fear or anxiety of these sensations
• Many have one or more chronic health problems • The loss of a limb can be especially difficult; it is important to
provide psychological support

20Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Replantation
• Involves the use of a microscope and highly specialized instruments to reanastomose (reconnect) blood vessels and nerve fibers in a severed limb
• Limb sutured into its correct anatomic position • Advances in microsurgical techniques and
preservation of severed limbs have made this technique increasingly successful

21Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Indications
• For amputations through the hand or wrist • Amputated thumbs are reattached whenever possible because of
their importance in hand function • In severely injured hand in which two or more fingers are
detached, surgeon restores as many fingers as possible • Amputations above the wrist do not lend themselves as readily to
replantation because of the extensive tissue, muscle, and bone damage accompanying the injury
• In general, the greater the muscle mass injury, the less likely replantation is possible

22Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Emergency Care
• Wrap amputated parts in a clean cloth saturated with normal saline or Ringer’s lactate
• Put in a sealed plastic bag that is placed in ice water • Direct contact between the amputated part and the ice can lead to
further tissue damage and cell death • Partially amputated parts should remain attached to the patient
and be kept cool if possible • Extra care to avoid detaching any parts since even small
connections increase the chances for successful repair • Patient may require treatment for shock due to blood loss • Tourniquets should not be used unless absolutely necessary

23Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Assessment
• Assess circulatory status• Closely monitor vital signs• Inspect the residual limb (or dressing) for bleeding • Assess pain at the site of the injury and at other
locations • Measure and record fluid intake and output • Note patient’s emotional status, and assess
understanding of the preoperative activities and postoperative routines
• Identify sources of support

24Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Preoperative Nursing Care
• Interventions• Administer intravenous fluids and blood as ordered • If the dressing becomes saturated with blood, reinforce the
dressing • Report continued or excessive bleeding to the physician • Even though preparations for replantation are hurried, be
sensitive to the patient’s fear and anxiety • Accept the patient’s feelings • Provide brief, simple explanations • Administer analgesics as ordered for pain

25Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Postoperative Nursing Care: Assessment
• Monitor vital signs, intake and output, and level of consciousness
• Hourly neurovascular assessment of limb • Doppler device or pulse oximeter to evaluate
circulation • Note and record the limb’s color, capillary refill,
turgor, temperature, and sensation • Assess limb for edema because massive
edema often accompanies replantation

26Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
Postoperative Nursing Care: Interventions
• Elevate the limb • Abstain from nicotine- and caffeine-containing products
for 7 to 10 days postoperatively • Enforce a strict ban on cigarette smoking • Room at 80° F to prevent compensatory
vasoconstriction of peripheral tissues • Loosen tight or restrictive gowns or pajamas • Administer ordered drugs; monitor effects• Discuss thoughts and feelings about the replantation,
disfigurement, and loss of function

27Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• A 68-year-old patient has been brought back to the surgical unit following a below-the-knee amputation for complications associated with peripheral vascular disease. What are the most common postoperative complications in a patient with an amputation? What nursing interventions would be indicated in the immediate postoperative period?

28Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• Guidelines: The most common complications associated with amputation are hemorrhage, hematoma, edema, pain, and infection. The nurse should frequently monitor the patient during the postoperative period. The assessment should include vital signs, which can indicate fluid volume loss, infection, and other complications. The nurse should assess the surgical area for signs of drainage and bleeding, as well as the surrounding areas. The patient should also be assessed and medicated for pain and the incision should be monitored for signs and symptoms of infection, such as foul-smelling drainage, redness, swelling, and warmth, and the nurse should offer continued emotional support to the patient.

29Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• Question: What are the four most common incidences that lead to amputation? Explain your answers.

30Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• Answer: The first incidence is trauma, which is the most common cause of upper-extremity amputation. Some examples of trauma are automobile, motorcycle, explosives, firearms, and machinery accidents. The next most common cause of amputations is vascular disease. Vascular disease is the leading cause of lower-extremity amputation. Some examples of disease are diabetes mellitus, peripheral vascular disease, and arteriosclerosis. Tumors are the third most common indication for amputation. Tumors of the bone that are large and invasive can necessitate amputation. Finally, congenital defects can result in amputation or missing limbs (congenital amputation) at birth as a result of improper development in utero.

31Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• A 19-year-old patient presents to the emergency department with a severe crushing injury to his right forearm following an automobile accident. The patient will require amputation due to the severity of the injury. What diagnostic tests will likely be performed before the surgery, and what type of surgery would most likely be indicated for this patient?

32Elsevier items and derived items © 2007 by Saunders, an imprint of Elsevier, Inc.
• Guidelines: The patient will undergo diagnostic tests to determine the extent of damage to the arm and to determine the blood flow to the extremity. These are considered vascular tests. The patient will likely undergo an angiography before surgery to determine if there is any damage to the arteries and also to determine at what level the amputation needs to be performed. Because of the traumatic nature of the injury, the patient is at risk for infection in the bone and tissues that surround it. Therefore, the patient will likely undergo an open or staged amputation to monitor for signs of infection. The surgeon will attempt to amputate at the lowest possible level that will promote tissue healing and adequate blood supply.