Module 2.5 Clinical Overview - 医薬品医療機器総合 …...CONFIDENTIAL Module 2.5 Clinical...
Transcript of Module 2.5 Clinical Overview - 医薬品医療機器総合 …...CONFIDENTIAL Module 2.5 Clinical...

CONFIDENTIALModule 2.5 Clinical Overview
1
Module 2.5
Clinical Overview
Copyright 2012 ViiV Healthcare and the GlaxoSmithKline group of companies. All rights reserved. Unauthorized copying or use of this information is prohibited.

CONFIDENTIALModule 2.5 Clinical Overview
2
TABLE OF CONTENTS
PAGE
ABBREVIATIONS ...........................................................................................................6
1. PRODUCT DEVELOPMENT RATIONALE...............................................................91.1. HIV Infection .................................................................................................91.2. Current Therapies and its Unmet Clinical Need ............................................91.3. Claimed Indication and Dosage ..................................................................111.4. Clinical Development Program....................................................................121.5. Regulatory History ......................................................................................131.6. Compliance with Good Clinical Practice (GCP)...........................................13
2. OVERVIEW OF BIOPHARMACEUTICS ................................................................132.1. Biopharmaceutical Classification ................................................................132.2. Formulation Development...........................................................................132.3. Analytical Methods......................................................................................142.4. Biopharmaceutics Studies ..........................................................................14
3. OVERVIEW OF CLINICAL PHARMACOLOGY......................................................153.1. Absorption, Distribution, Metabolism and Elimination of Dolutegravir..........15
3.1.1. Absorption ...................................................................................153.1.2. Distribution...................................................................................153.1.3. Metabolism and Excretion............................................................163.1.4. Elimination ...................................................................................16
3.2. Pharmacokinetics in Healthy Subjects and Target Patient Populations.................................................................................................173.2.1. Summary of Dolutegravir PK Parameters ....................................173.2.2. Pharmacokinetics in Special Populations.....................................19
3.2.2.1. Children......................................................................193.2.2.2. Elderly ........................................................................203.2.2.3. Renal impairment .......................................................203.2.2.4. Hepatic impairment.....................................................203.2.2.5. UGT1A1 Polymorphism..............................................213.2.2.6. Co-infection with Hepatitis B or C ...............................213.2.2.7. Population PK.............................................................21
3.3. Drug-Drug Interactions................................................................................213.3.1. Effect of Dolutegravir on the Pharmacokinetics of Other
Agents .........................................................................................213.3.2. Effect of Other Agents on the Pharmacokinetics of
Dolutegravir and Dose Recommendations...................................243.4. Pharmacodynamics ....................................................................................28
3.4.1. Effect of DTG on Cardiac Conduction ..........................................283.4.2. Effect of DTG on Renal Function .................................................28
3.5. Pharmacokinetic – Pharmacodynamic Relationships and Definition of “No Effect Boundaries”............................................................................283.5.1. PK/PD Relationship for Efficacy...................................................28
3.5.1.1. Short-Term Monotherapy............................................283.5.1.2. Long-Term Combination Therapy ...............................29
3.5.2. PK/PD Relationship for Safety .....................................................30

CONFIDENTIALModule 2.5 Clinical Overview
3
3.5.3. Definition of No Effect Boundaries of Alteration in DTG Exposure .....................................................................................30
3.6. Clinical Pharmacology Conclusions ............................................................31
4. OVERVIEW OF EFFICACY ...................................................................................324.1. Non-clinical Virology ...................................................................................324.2. Selection of Patient Populations in Pivotal and Supportive Efficacy
Studies .......................................................................................................334.3. Rationale for Dose Selection in Clinical Development.................................33
4.3.1. ART-Naïve/ART-Experienced (INI-Naïve) Subjects .....................334.3.2. ART-Experienced (INI-Resistant) Subjects ..................................34
4.4. Clinical Trial Methodology and Design (Pivotal Efficacy Study Designs) .....................................................................................................354.4.1. Studies in INI-Naïve Subjects ......................................................354.4.2. Studies in INI-Resistant Subjects.................................................35
4.5. Efficacy Endpoints and Statistical Considerations of Efficacy Analyses .....................................................................................................394.5.1. Primary and Secondary Efficacy Endpoints .................................394.5.2. Statistical Considerations.............................................................40
4.6. Efficacy Results in all Studies .....................................................................414.6.1. Enrolment of Key Demographic Subpopulations in
ING113086, ING114467, and ING111762 ...................................414.6.2. ART-Naïve...................................................................................43
4.6.2.1. Demographics and Baseline Characteristics...............434.6.2.2. Key Efficacy Endpoints...............................................434.6.2.3. Comparison of Primary Efficacy Results in
Sub-populations .........................................................454.6.3. ART-Experienced (INI-Naïve) Subjects........................................47
4.6.3.1. Demographics and Baseline Characteristics...............474.6.3.2. Key Efficacy Endpoints...............................................474.6.3.3. Comparison of Principal Efficacy Results in
Sub-populations .........................................................494.6.4. Treatment Emergent Resistance in INI-Naïve Subjects ...............494.6.5. ART-Experienced (INI-Resistant) Subjects ..................................51
4.6.5.1. Demographics and Baseline Characteristics...............514.6.5.2. Key Efficacy Endpoints...............................................514.6.5.3. Treatment Emergent Resistance in INI-
resistant Subjects .......................................................524.6.5.4. Comparison of Primary Efficacy Results in
Sub-populations .........................................................534.6.5.5. Antiviral Activity of DTG by Baseline
Resistance in INI-resistant Subjects in ING112574.................................................................53
4.7. Efficacy Conclusions...................................................................................55
5. OVERVIEW OF SAFETY .......................................................................................565.1. Introduction.................................................................................................56
5.1.1. Data Cut-off Dates .......................................................................565.2. Non-Clinical Data Relevant to Human Safety..............................................575.3. Exposure in the Clinical Development Program ..........................................575.4. Safety in Clinical Pharmacology Studies.....................................................58
5.4.1. Frequently Reported AEs.............................................................58

CONFIDENTIALModule 2.5 Clinical Overview
4
5.4.2. Deaths .........................................................................................585.4.3. Non-Fatal Serious Adverse Events ..............................................585.4.4. Adverse Events Leading to Withdrawal........................................595.4.5. Clinical Laboratory Evaluations and Vital Signs ...........................59
5.4.5.1. Hepatobiliary Adverse Events.....................................595.4.5.2. Renal Adverse Events ................................................59
5.4.6. Cardiac Evaluation.......................................................................605.5. Safety in Pediatrics - ING112578 (P1093) ..................................................605.6. Safety in Phase II and III Studies ................................................................61
5.6.1. Safety Population for Phase II and III Studies ..............................615.6.2. Common Adverse Events ............................................................62
5.6.2.1. Frequently Reported Adverse Events .........................625.6.2.1.1. ART-Naïve Adult Subjects ......................635.6.2.1.2. ART-Experienced (INI-Naïve)
Adult Subjects.........................................645.6.2.1.3. ART-Experienced (INI-Resistant)
Adult Subjects.........................................645.6.2.2. Labeling and Adverse Drug Reactions........................655.6.2.3. Supportive PK/PD Safety Analyses ............................67
5.6.3. Deaths .........................................................................................675.6.4. Serious Adverse Events...............................................................67
5.6.4.1. ART-Naïve Adult Subjects ..........................................675.6.4.2. ART-Experienced (INI-Naïve) Adult Subjects .............685.6.4.3. ART-experienced (INI-Resistant) Adult
Subjects .....................................................................695.6.5. Adverse Events Leading to Withdrawal........................................69
5.6.5.1. ART-Naïve Adult Subjects ..........................................695.6.5.2. ART-Experienced (INI-Naïve) Adult Subjects .............705.6.5.3. ART-Experienced (INI-Resistant) Adult
Subjects .....................................................................715.6.6. AEs of Special Interest.................................................................72
5.6.6.1. Hypersensitivity and Rash ..........................................725.6.6.2. Hepatobiliary Disorders ..............................................735.6.6.3. Renal Function ...........................................................745.6.6.4. Gastrointestinal (GI) Disorders ...................................765.6.6.5. Musculoskeletal Disorders..........................................765.6.6.6. Immune Reconstitution Inflammatory
Syndrome (IRIS).........................................................775.6.6.7. Other ..........................................................................77
5.6.7. Clinical Laboratory Evaluations....................................................775.6.7.1. Clinical Chemistry.......................................................775.6.7.2. Hematology ................................................................78
5.7. Vital Signs...................................................................................................785.8. Electrocardiograms.....................................................................................785.9. Safety in Special Groups and Situations .....................................................785.10. Pregnancies................................................................................................795.11. Withdrawal Effects, Abuse Potential, Overdose ..........................................795.12. Post-Marketing Experience.........................................................................795.13. Safety Conclusions .....................................................................................79
6. BENEFITS AND RISKS CONCLUSIONS...............................................................816.1. Benefits of Dolutegravir in the Treatment of HIV-1 Infection........................81

CONFIDENTIALModule 2.5 Clinical Overview
5
6.2. Risks of Dolutegravir in the Treatment of HIV-1 Infection............................846.3. Overall Dosing Recommendations..............................................................866.4. Overall Conclusions....................................................................................86
7. REFERENCES.......................................................................................................87
8. APPENDICES ........................................................................................................91Appendix Table 1 Explanation for Empty Submission Modules ...............91

CONFIDENTIALModule 2.5 Clinical Overview
6
ABBREVIATIONS
3TC lamivudineABC abacavirAE Adverse eventAIDS Acquired immunodeficiency syndromeALT Alanine aminotransferaseAPI Active pharmaceutical ingredientsATV atazanavirAST Aspartate aminotransferaseART Antiretroviral therapyAUC Area under the curveAUC(0-t) Area under the concentration-time curve from time zero
(pre-dose) to the last time of quantifiable concentrationAUC(0-) Area under the concentration-time curve over the dosing
intervalAUC(0-) Area under the concentration-time curve from time zero
(pre-dose) extrapolated to infinite timeAUC(0-24) Area under the concentration-time curve from time zero
(pre-dose) to 24 hours post dose or over 24 hoursBID Twice dailyC24 Concentration at 24 hours post doseCL/F Apparent clearance following oral dosingCmax Maximum observed concentrationCMC Chemistry, manufacturing and controlsC0 Pre-dose concentrationC0_avg Average of concentrations at time 0C Concentration at the end of the dosing periodc/mL copies per milliliterCavg Average of concentrationsCDC Centers for Disease Control and PreventionCSF Cerebrospinal fluidCI Confidence IntervalCOBI cobicistatCPSR Clinical Pharmacology Study ReportCrCL Creatinine clearanceCSR Clinical Study ReportCYP Cytochrome P450CV% Coefficient of varianceCVb Between-subject variability (or coefficient of variation)DNA Deoxyribonucleic acidDRV darunavirDTG dolutegravir, S/GSK1349572EFV efavirenzEMA European Medicines AgencyEmax Maximum effectERPF Effective renal plasma flowETR etravirine

CONFIDENTIALModule 2.5 Clinical Overview
7
EVG elvitegravirFC Fold changeFDA (US) Food and Drug AdministrationFDC Fixed dose combinationFPV fosamprenavirFTC emtricitabineGCP Good Clinical PracticeGFR Glomerular filtration rateGI GastrointestinalGSK GlaxoSmithKlineHBV Hepatitis B VirusHCV Hepatitis C VirusHIV Human Immunodeficiency VirusHIV-1 Human Immunodeficiency Virus Type 1HIV-2 Human Immunodeficiency Virus Type 2IC50 Half-maximal inhibitory concentrationICH International Conference on Harmonisation of Technical
Requirements for Registration of Pharmaceuticals for Human Use
IN IntegraseIND Investigational New DrugINI Integrase inhibitorITT-E Intent-to-Treat ExposedLOCFDB Last observation carried forward (discontinuation equals
Baseline)LPV lopinavirMAA Marketing Authorization Applicationmg MilligrammITT-E Modified Intent-to-Treat Exposedmm3 Cubic millimeterMSDF Missing, Switch or Discontinuation = FailureNDA New Drug ApplicationNDS New Drug Submissionng NanogramNRTI Nucleoside reverse transcriptase inhibitorNNRTI Non-nucleoside reverse transcriptase inhibitorOBR Optimized background regimenOCT2 Organic cation transporter 2OMP OmeprazoleOSS Overall susceptibility scorePAH Para-aminohippuratePBMC Peripheral blood mononuclear cellPDVF Protocol defined virologic failurePI Protease inhibitorPK PharmacokineticPD PharmacodynamicPP Per-protocol PSS Phenotypic susceptibility score

CONFIDENTIALModule 2.5 Clinical Overview
8
PGx PharmacogeneticsRAL raltegravirRIF RifampinRNA Ribonucleic acidRTV ritonavirt1/2 Terminal phase half-lifeTLOVR Time to Loss of Virologic ResponseTDF tenofovir disoproxil fumarateTPV tipranavirUGT Uridine diphosphate glucuronyltransferaseUNAIDS Joint United Nations Programme on HIV/AIDSUS United StatesVd/F Apparent volume of distributionVL Viral loadVz/F Apparent volume of distribution after extravascular (e.g.,
oral) administration at terminal phase
Trademark Information
Trademarks of ViiV Healthcare Trademarks not owned by ViiV Healthcare
EPZICOM AtriplaKIVEXA Isentress
StribildTruvada

CONFIDENTIALModule 2.5 Clinical Overview
9
1. PRODUCT DEVELOPMENT RATIONALE
1.1. HIV Infection
An estimated 34.2 million adults and children worldwide, were living with Human Immunodeficiency Virus (HIV)/Acquired Immunodeficiency Syndrome (AIDS) in 2011 [UNAIDS, 2012a].
In 2011, the global adult (15 to 49 years) HIV prevalence rate was 0.8% [UNAIDS, 2012b]. During that year, 2.5 million people were newly infected with HIV, and there were 1.7 million deaths due to HIV/AIDS. Of newly infected people, an estimated 1.2 million were women and girls, and 330,000 were children. As well, 3.4 million children younger than 15 years were living with HIV in 2011 [UNAIDS, 2012a]. In 2009, an estimated 370,000 children contracted HIV during the perinatal and breastfeeding period. Overall, the epidemic appears to have stabilized in most regions, although prevalence continues to increase in Eastern Europe and Central Asia and in other parts of Asia due to a high rate of new HIV infections [UNAIDS, 2010]. In 2011, Sub-Saharan Africa remained the most heavily affected region, accounting for 68% (1.7 million) of all new HIV infections among adults and children [UNAIDS, 2012b].
1.2. Current Therapies and its Unmet Clinical Need
Combination antiviral therapy with HIV type-1 (HIV-1) protease and reverse transcriptase inhibitors has significantly reduced AIDS-related morbidity and mortality. However, emerging multi-class drug-resistant HIV strains and long-term toxicities warrant development of new classes of antiretroviral therapies. Integrase inhibitors (INIs) are a newer class of antiretroviral drugs designed to block the action of the integrase (IN) viral enzyme, which catalyzes two key steps in the HIV life cycle and is responsible for insertion of the viral genome into the deoxyribonucleic acid (DNA) of the host cell. Since genome integration is a vital step in retroviral replication, it is an attractive target for HIV therapy.
Dolutegravir (DTG, GSK1349572) is an INI owned by ViiV Healthcare, which is working with GlaxoSmithKline (GSK) to develop the asset.
Raltegravir (RAL), the first marketed INI, and elvitegravir (EVG), which recently gained United States (US) Food and Drug Administration (FDA) approval (in August 2012 in a combination product), have demonstrated good antiviral activity in clinical trials, confirming the INI class as a new option for constructing effective HIV-1 treatment regimens. In the STARTMRK study, RAL demonstrated excellent antiviral activity as first-line treatment and was shown to be non-inferior to an efavirenz (EFV)-containing standard of care regimen [Lennox, 2010]. In this trial, a similar proportion of subjects randomized to RAL versus EFV [both in combination with tenofovir disoproxil fumarate/emtricitabine (TDF/FTC)] achieved undetectable HIV-1 ribonucleic acid (RNA) (<50 copies/milliliter [c/mL]) at Week 48 (86% vs. 82%) and Week 96 (81% vs. 79%). Additionally, the time to achieve viral suppression was shorter for subjects on RAL than on EFV (log rank test P<0.001).

CONFIDENTIALModule 2.5 Clinical Overview
10
Similarly, in the GS-US-236-0102 study, EVG co-formulated with the cytochrome P450(CYP) 3A4 inhibitor cobicistat (COBI), TDF, and FTC (now approved in the US as Stribild), was shown to be non-inferior to the co-formulated standard of care regimen EFV/TDF/FTC as a first-line treatment, with 87.6% versus 84.1% of patients, respectively, achieving <50 c/mL HIV RNA at Week 48 [Sax, 2012].
Integrase inhibitors have also shown potent antiviral activity in treatment-experienced patient populations. In the BENCHMRK study, patients with three-class antiretroviral resistance (naïve to INIs) received RAL or placebo plus optimized background therapy; 62% of RAL subjects (versus 33% of placebo subjects) had HIV RNA <50 c/mL at Week 48 [Steigbigel, 2008]. In Study 145, a study in INI-naïve, treatment-experienced subjects with at least two-class resistance, EVG once daily was non-inferior to RAL twice daily (BID), each administered with a background regimen that included a ritonavir(RTV)-boosted protease inhibitor (PI) and a second antiretroviral agent. At Week 48 of Study 145, 59% of the EVG group versus 58% of the RAL group achieved virologic response (<50 c/mL) [Molina, 2012].
In addition to providing good virologic suppression in treatment-naïve and treatment-experienced patients, the INIs have been well-tolerated in clinical trials. In STARTMRK, there were fewer drug-related adverse events (AEs) reported for the RAL group compared with the EFV group, and fewer subjects randomized to RAL discontinued from the study due to AEs. In GS-US-236-0102, AEs were similar between the EVG and EFV groups, with the exception of nausea (significantly higher in the EVG group), and dizziness, abnormal dreams, and rash (significantly higher in the EFV group); similar numbers of subjects in the two groups discontinued treatment because of AEs (4% versus 5%).
While these trials highlight the potent antiviral efficacy and promise of better long-term tolerability with INI-based therapy, clinical resistance to both RAL and EVG has been reported from Phase II studies in treatment-experienced subjects [Hazuda, 2007; McColl, 2007], and also from Phase III studies in both treatment-experienced [Cooper,2008; Molina, 2012] and treatment-naïve subjects [Lennox, 2010; Sax, 2012; DeJesus, 2012]. In Study 145, comparing EVG- versus RAL-based therapy in treatment-experienced subjects, among subjects who failed therapy, 16/60 (27%) and 15/72 (21%) of patients who had IN genotype data available at the time of virologic failure developed INI resistance mutations. In addition, phenotypic cross-resistance to both drugs was typical, preventing sequencing from one drug to the other [Molina, 2012]. Therefore, the development of new INIs with different resistance profiles is desirable; for many treatment-experienced patients with clinical resistance to RAL and EVG, new agents areessential for providing HIV-infected individuals an option for constructing an effective antiretroviral regimen.
There are other properties of RAL and EVG that also provide room for improvement.RAL requires BID dosing and is currently not available in a fixed dose combination (FDC) regimen. EVG requires co-administration with a pharmacokinetic (PK) booster, such as RTV or cobicistat (COBI) [German, 2010], and therefore, has the potential for clinically-significant drug-drug interactions with drugs that depend on CYP3A4 for clearance. Additionally, EVG-containing regimens had higher rates of gastrointestinal

CONFIDENTIALModule 2.5 Clinical Overview
11
(GI) AEs than a RAL-containing regimen and Atripla in treatment-experienced and treatment-naïve patients, respectively [Molina, 2012; Sax, 2012]; Stribild is also not recommended for patients with creatinine clearance (CrCL) under 70 mL/min.
Finally, both RTV and COBI (one of which is required in conjunction with EVG; COBIis a component of the FDC tablet that contains EVG/COBI/TDF/FTC) boost TDF concentrations, which may increase TDF proximal tubular toxicity [FDA, 2012].
Dolutegravir is a potent, low nanomolar inhibitor of HIV IN, which offers once-daily dosing without the requirement for pharmacokinetics boosters. Based on in vitro and clinical data, DTG demonstrates the excellent antiviral activity and tolerability typical of the INI class, with a higher barrier to resistance. Finally, most HIV isolates with resistance to RAL and EVG remain susceptible to DTG, making DTG an important option for many treatment-experienced patients with multi-class drug resistance.
1.3. Claimed Indication and Dosage
The proposed product labeling for DTG includes the following key elements:
Dolutegravir is indicated for the treatment of HIV infection in combination with other antiretroviral agents in adults and children 12 to 18 years of age.
Dolutegravir should be administered as presented below (with or without food):
Treatment-naïve Adults:
For patients initiating antiretroviral therapy for the first time (treatment-naïve), the recommended dose of dolutegravir is 50 mg once daily.
Treatment-experienced, and integrase inhibitor-naïve Adults
For patients who are treatment experienced, and have not previously been treated with an integrase inhibitor, the recommended dose of dolutegravir is 50 mg once daily.
Integrase inhibitor-resistant Adults
For patients with integrase inhibitor resistance, the recommended dose of dolutegravir is 50 mg twice daily.
Pediatric Patients
In pediatric patients (12 to less than 18 years of age and weighing greater than or equal to 40 kg) who have not previously been treated with an integrase inhibitor, the recommended dose of dolutegravir is 50 mg once daily.
There are insufficient data to recommend a dose for dolutegravir in integrase inhibitor resistant children and adolescents under 18 years of age.
There are insufficient safety and efficacy data available to recommend a dose for dolutegravir in children below age 12 or weighing less than 40 kg.

CONFIDENTIALModule 2.5 Clinical Overview
12
1.4. Clinical Development Program
The Sponsor’s strategy for the development of DTG is to file for a New Drug Application (NDA)/Marketing Authorization Application (MAA)/New Drug Submission (NDS) by demonstrating significant improvements over the first marketed INI (RAL). Improvements include activity in the presence of integrase resistant viruses and an improved dosing regimen (unboosted once daily administration) with similar or improved safety and efficacy. An additional study in treatment naïve subjects was conducted to compare a regimen containing DTG plus the abacavir/lamivudine (ABC/3TC) FDC with the co-formulated standard of care regimen EFV/TDF/FTC.
The clinical development program has been designed to achieve a broad initial indication for the treatment of HIV-1 infection in combination with other antiretroviral agents in adults and children over 12 years of age.
A full listing of studies included in this application is located in m5.2, Table of Studies. The clinical program investigating DTG involves 30 Phase I, 4 Phase II, 7 Phase III/IIIb clinical trials. In addition, there is an Investigational New Drug (IND)/Named Patient Program and an Expanded Access Program currently providing DTG to a limited number of subjects (see m5.3.5.4 ING114916 and m5.3.5.4 ING115502 Brief WrittenSummaries).
To support the proposed indication, the submission includes a Clinical Pharmacology package describing the PK and the PK/pharmacodynamic (PD) relationship of DTG in both healthy volunteers and HIV-infected subjects. Additionally, a comprehensive package of drug interaction studies has been completed to inform dosing of DTG with other antiretroviral agents as well as key concomitant medications for HIV-infected patients. PK studies in special populations, as well as PD studies to complement the safety data from all clinical trials have been completed. Finally, a PK, safety and efficacy study in HIV-infected children is ongoing and data to support dosing in children 12 to <18 years of age is included. This package is described in detail in m2.7.2.
The supportive Phase II package (Studies ING111521, ING112276 and ING112961) includes initial efficacy data as well as enabling dose-ranging data and longer-term efficacy and safety data in antiretroviral therapy (ART)-naive, -experienced and INI-resistant subjects. In these supportive efficacy studies, patients were treated with doses of dolutegravir from 2 mg daily up to 100 mg daily, administered via once daily or BIDdosing.
The pivotal Phase III Studies, ING113086, ING111762, ING114467, and ING112574 assessed DTG in HIV-infected subjects with a broad range of treatment experience and support an unrestricted indication for the treatment of HIV-infection. Studies ING113086, ING111762, and ING114467 were international, multi-center, randomized, double-blind studies, and each has the characteristics of an “adequate and well-controlled clinical trial” as described in Title 21 of the US Code of Federal Regulations, Section 314.126 and ICH Topic E 8 General Considerations for Clinical Trials. Study ING112574 is an international, multicenter study with a single arm, reflecting ethical

CONFIDENTIALModule 2.5 Clinical Overview
13
difficulties in randomizing subjects to a control arm in the multi-class resistant population studied. There are additional Phase III/IIIb studies currently ongoing.
Longer term efficacy and safety data are available from ongoing Studies ING112276 (96 weeks) and ING112961 (Cohort I 96 weeks, Cohort II 48 weeks) where up to 206subjects received DTG. Studies ING113086, ING111762, ING114467, and ING1112574 are ongoing and will continue, pending the outcome of regulatory evaluation of the marketing applications.
1.5. Regulatory History
The development program for DTG has been formally discussed with key regulatory agencies at various milestones throughout the development program (See m2.2).
1.6. Compliance with Good Clinical Practice (GCP)
All studies were undertaken in accordance with standard operating procedures of the GlaxoSmithKline Group of Companies, which comply with the principles of Good Clinical Practice. All studies were conducted with the approval of Ethics Committees or Institutional Review Boards. Informed consent was obtained for all subjects, and the studies were performed in accordance with the version of the Declaration of Helsinki that applied at the time the studies were conducted. Where required, regulatory approval was obtained from the relevant health authority.
2. OVERVIEW OF BIOPHARMACEUTICS
Data from clinical biopharmaceutics Studies ING111322, ING112941, ING113068, and ING113674, along with chemistry, manufacturing and controls (CMC) and bioanalytical methods data, form the basis of the biopharmaceutical evaluation of DTG in this submission. These studies are described in m2.7.1 (Summary of Biopharmaceutic Studies and Associated Analytical Methods); critical aspects of the results are discussed below.
2.1. Biopharmaceutical Classification
DTG sodium, Form 1, is a non-hygroscopic, crystalline solid with suitable solid state stability and oral bioavailability. DTG sodium has a solubility of 3.2 mg/ml in water at 25C; in buffered solutions across the physiological pH range 1 to 7, the solubility is significantly lower (at or below 50 g/ml). The measured permeability is approximately 3x10-4 cm/sec. The combination of low solubility with high predicted permeability puts dolutegravir in Biopharmaceutics Classification System Class II (m2.7.2, Section 1.1).
2.2. Formulation Development
Dolutegravir was administered as dolutegravir sodium in all clinical studies.
Initial Phase I studies utilized a powder for reconstitution consisting of DTG sodium, hypromellose and sodium lauryl sulphate. Doses of up to 250 mg DTG were administered in Phase I studies using this formulation.

CONFIDENTIALModule 2.5 Clinical Overview
14
Tablet formulations were then developed to provide 1 mg, 10 mg and 25 mg dose strengths for Phase II studies. These tablets contained: d-mannitol and microcrystalline cellulose as diluents, povidone as a binder, croscarmellose sodium as a disintegrant, and sodium stearyl fumarate as a lubricant. These tablets were used in Phase II studies.Based on ING112276, a dose ranging study in treatment-naive HIV-infected subjects, a dose of 50 mg dolutegravir once daily was selected for Phase III studies.
During Phase II, sodium starch glycolate was identified as a more optimal disintegrant for long-term stability compared to the croscarmellose sodium used in the Phase II tablet formulation. Two variations of the new formulation (both 25 mg tablets) were assessed against the Phase II tablet formulation (25 mg tablet) in a relative bio-availability study (ING113674).
Both 25 mg tablet variations were bioequivalent with the Phase II 25 mg tablet formulation. The variant with the lower overall tablet weight was selected to progress into Phase III with the tablet core compression weight set to deliver 50 mg of dolutegravir in a single tablet.
Micronized API is utilized in dolutegravir tablets, 50 mg. The particle size for this API to be used in the commercial formulation is supported by data obtained in Study ING113068 (m2.7.1, Section 2.1.2).
The commercial formulation is identical to the clinical trial tablet formulation used in all Phase III/IIIb studies and pediatric study, differing only in the film coat color and the degree of concavity of the tooling used to produce the tablets (m2.7.1, Section 1.3.2).
2.3. Analytical Methods
The bioanalytical methods used to measure concentrations of DTG in human plasma were sensitive, selective, accurate and reproducible. Stability of the analyte was demonstrated during sample processing and long-term storage (m2.7.1, Section 1.4).
2.4. Biopharmaceutics Studies
The key results from biopharmaceutic studies for consideration in clinical use and detailed in m2.7.1 are as follows:
The oral bioavailability of the tablet was less than that of a suspension, with mean AUC(0-t) decreased by 30% following administration of the tablet compared to the suspension formulation under the fasted condition. The rate of absorption of the drug from tablet was slower than suspension.
Changes in particle size did not have a significant impact on exposure. A formulation of un-micronized particles demonstrated similar exposure to the current tablet formulation (with micronized particles). These data support the particle size specification for the micronized API.
For DTG tablets, a 25 mg tablet with the Phase III formulation composition met the bioequivalence criteria with the 25 mg tablet used in the Phase II studies.

CONFIDENTIALModule 2.5 Clinical Overview
15
A higher strength tablet of this formulation (50 mg tablet) was manufactured at the commercial site for use in Phase III clinical trials. This 50 mg tablet has the same % weight/weight composition but made at double the tablet weight of the 25 mg tablets used to establish bioequivalence to the Phase II product. The in-vitro dissolution profiles (3 media used) of the 50 mg tablets (Phase III formulation) compare closely to the profiles of two 25 mg tablets (Phase III composition) tested per dissolution vessel (i.e. total dose level = 50 mg).
Administration with food increases the exposure of DTG. Plasma DTG AUC(0-) increased by 33%, 41%, and 66% when DTG was administered with low fat, moderate fat and high fat food, respectively. DTG can be taken with or without food based on the accumulated safety data in Phase IIb and III studies, which permitted DTG dosing without restriction to food or food content.
3. OVERVIEW OF CLINICAL PHARMACOLOGY
Critical findings from the clinical pharmacology studies conducted with DTG are discussed below. These studies are described in detail in m2.7.2 (Summary of Clinical Pharmacology).
3.1. Absorption, Distribution, Metabolism and Elimination of Dolutegravir
3.1.1. Absorption
DTG is rapidly absorbed following oral administration of tablet formulations, with no absorption lag time and a median tmax of 2 to 3 hours post dose. DTG concentration declines mono-exponentially with an average terminal half life of approximately 14 hours(m2.7.2, Section 2, Study ING111207).
DTG absorption is increased with co-administration of food (m2.7.1, Section 2.3). The moderate food effect is not considered clinically significant; therefore DTG can be taken without regard to food (m2.7.1, Section 2.3). Dosing separation is needed when DTG is to be given together with antacids (e.g. Maalox), due to chelation with polyvalent cations that decrease DTG exposure, (m2.7.2, Section2, Study ING111602); DTG should be taken 2 hours before or 6 hours after antacid dose. DTG can be dosed with multivitamins without dosing separation (m2.7.2, Section 2, Study ING111602).
The linearity of DTG pharmacokinetics is dependent on dose. Following oral administration of tablet formulations, in general, DTG exhibited nonlinear pharmacokinetics with less than dose-proportional increases in plasma exposure from 2 to 100 mg; however the increase in DTG exposure appears dose proportional from 25 mgto 50 mg.
3.1.2. Distribution
DTG is highly bound (approximately 99.3%) to human plasma proteins based on in vitro data. The apparent volume of distribution (Vd/F, following oral administration of suspension formulation) is estimated at 12.5 L (m2.7.2, Section 2, Study ING111853).

CONFIDENTIALModule 2.5 Clinical Overview
16
DTG appears to primarily bind to albumin rather than 1-acid glycoprotein (AAG) in plasma (m2.7.2 Section 3.1.4). Binding of DTG to plasma proteins was independent of DTG concentrations over the therapeutic range. Total blood and plasma drug-related radioactivity concentration ratios averaged 0.441 to 0.535, indicating minimal association of radioactivity with blood cellular components. Free fraction of DTG in plasma is estimated at ~0.23% to 1.10% in healthy subjects, ~0.4 to 0.5% in subjects with moderatehepatic impairment, 0.84 to 1.01% in subjects with severe renal impairment, and 0.49% in HIV-positive subjects (m2.7.2, Section 2, Studies ING113097, ING113125, andING116070).
DTG is present in cerebrospinal fluid (CSF). In 12 treatment-naïve subjects receiving a regimen of DTG plus abacavir (ABC)/lamivudine (3TC) for two weeks, DTG concentration in CSF averaged 18 ng/mL, ranging from 3.97 to 23.2 ng/mL (comparableto unbound plasma concentration, and above the 50% inhibitory concentration [IC50] in all subjects); CSF:plasma concentration ratio of DTG ranged from 0.11 to 0.66%. A rapid and significant decrease in HIV-1 RNA in CSF was observed after two weeks of DTG therapy (when administered with ABC/3TC) (m5.3.4.2, ING116070 Week 2 Synoptic Clinical Study Report [CSR]).
DTG is present in the female and male genital tract. DTG exposure (expressed as AUC) in cervicovaginal fluid, cervical tissue, and vaginal tissue was 6%, 10%, and 9%, respectively, of that in corresponding plasma at steady state. DTG exposure (alsoexpressed as AUC) in seminal fluid and rectal mucosal tissue was 7% and 17%, respectively, of that in corresponding plasma at steady state (m2.7.2, Section 2, Study ING115465 and Study ING116195).
3.1.3. Metabolism and Excretion
Following oral administration in humans, unchanged DTG is primarily eliminated through metabolism, and renal elimination of unchanged DTG represents less than 1% of the total dose administered. DTG is primarily metabolized via UGT1A1 with CYP3A4 as a secondary metabolic pathway (approximately 10% in a human mass balance study). DTG is the predominant circulating compound in plasma, representing 97% of plasma total radiocarbon. Fifty-three percent of total oral dose is excreted as unchanged DTG in the feces, but it is unknown if all or part of this is due to unabsorbed drug or biliary excretion of the glucuronide conjugate which can be further degraded to form the parent compound in the gut lumen. Thirty-one percent of the total oral dose is excreted in the urine, represented by ether glucuronide of DTG (18.9% of total dose), N-dealkylation metabolite (3.6% of total dose), a metabolite formed by oxidation at the benzylic carbon (3.0% of total dose), and other minor metabolites (m2.7.2, Section 2, Study ING111853).
3.1.4. Elimination
DTG has a terminal half-life of ~14 hours and a low apparent clearance (CL/F) of 0.56 L/hr (m2.7.2, Section 2, Study ING111853). The apparent clearance represents <2% of liver plasma flow, therefore the hepatic extraction ratio of DTG is low (lower than 2%). As CYP3A4 is only a secondary route of elimination of DTG, the first-pass metabolism of DTG following oral dosing is expected to be very low.

CONFIDENTIALModule 2.5 Clinical Overview
17
3.2. Pharmacokinetics in Healthy Subjects and Target Patient Populations
3.2.1. Summary of Dolutegravir PK Parameters
The pharmacokinetics of DTG in healthy subjects and target patient populations has been evaluated after single and repeat doses given orally. The plasma pharmacokinetic parameters estimates of DTG are summarized in Table 1. Based on accumulated data, there appears to be no significant difference in pharmacokinetics between healthy and HIV-infected subjects.
Table 1 Summary of Key DTG Pharmacokinetic Parameters following Single Dose 50 mg Tablet Administration in Healthy and HIV-infected Subjects
Population DTG Dose
Data Source Cmax (g/ml)
AUC (0-)(g.h/mL)
C24 (g/mL)
CL/F(L/h)
Vz/F(L/h)
t½(h)
Healthy 50 mg Phase 1 Meta-analysis
2.20(43)
43.7(45)
0.65(49)
1.14(45)
23.3(45)
14.4(19)
HIV-1 infected
50 mg ING111521 2.46(32)
40.5(33)
0.59(31)
1.23(33)
ND 11.2(29)a
Data Source: m5.3.4.2 ING111521 Clinical Pharmacology Study Report (CPSR); m5.3.5.3 CPM Table 3.3Note: Data presented are geometric mean (CV%). ND: not determined.Likely underestimated as based on 24-hour sampling window

CONFIDENTIALModule 2.5 Clinical Overview
18
Table 2 Summary of Key DTG Pharmacokinetic Parameters following 50 mg Once Daily and BID Dosing in Healthy and HIV-infected Subjects
Population DTG Dosing Regimen
Data Source Cmax (g/ml)
AUC (0-)(g.h/mL)
AUC (0-24)(g.h/mL)
C (g/mL)
Healthy 50 mg once daily (overall)
Phase 1 Meta-analysis
(m5.3.5.3)
3.62(35)
49.1(41)
49.1(41)
1.05(56)
50 mg once daily(fasted)
Phase 1 Meta-analysis
(m5.3.5.3)
2.90(34)
38.4(40)
38.4(40)
0.79(59)
50 mg once daily
(fed)
Phase 1 Meta-analysis
(m5.3.5.3)
4.21(27)
58.2(30)
58.2(30)
1.28(41)
Healthy 50 mg BID(overall)
Phase 1 Meta-analysis
(m5.3.5.3)
6.00(39)
53.0(42)
106(42)
3.02(52)
50 mg BID(fasted)
Phase 1 Meta-analysis
(m5.3.5.3)
5.33(38)
47.1(42)
94.3(42)
2.66(53)
50 mg BID(fed)
Phase 1 Meta-analysis
(m5.3.5.3)
7.77(23)
68.6(27)
137(27)
4.00(36)
HIV-1 infected
50 mg once daily(no food
restriction)
Population PK (m5.3.3.5)
3.67 (20)
53.6 (27)
53.6 (27)
1.11 (46)
HIV-1 infecteda
50 mg BID(no food
restriction)
Population PK (m5.3.3.5)
4.15(29)
37.5(35)
75.1(35)
2.12(47)
Data Source: m5.3.5.3 CPM Table 3.2, m5.3.3.5 Population PK in ART-naïve; m5.3.3.5 Population PK in ARTexperiencedNote: Data presented are geometric mean (CV%). a. DTG PK exposure from 50 mg twice daily dosing is lower in HIV-1 infected subjects (treatment-experienced) than
healthy subjects and this is considered to be due to the wide use of inducers, e.g. DRV/RTV, in the background regimen in the treatment-experienced HIV-1 infected subjects.
Following repeat dose administration, DTG achieved steady state after approximately 5 days of dosing, consistent with the estimated t½ of approximately 14 hours, and showed time-invariant PK. Accumulation ratios for DTG 50 mg once daily dosing were 1.43, 1.36, and 1.42 for AUC(0-τ), Cmax, and Cτ, respectively.
In Phase I studies in healthy subjects, the PK variability of DTG is low to moderate with between-subject (CVb%) for AUC and Cmax of 20 to 40% and for C of 30 to 65%across studies. The PK variability of DTG is slightly higher in HIV-infected subjects than healthy subjects, with CVb% of C0 (pre-dose concentration at steady state) ranging from 55% to 140% across studies. Intra-subject variability (CVw%) is lower than inter-subject variability: CVw% ranged from 8 to 20% for DTG PK parameters in Phase I studies conducted in healthy subjects and ranged from 17 to 29% in HIV-infected subjects based on population PK modeling.

CONFIDENTIALModule 2.5 Clinical Overview
19
3.2.2. Pharmacokinetics in Special Populations
3.2.2.1. Children
The pharmacokinetics of DTG in 10 antiretroviral treatment-experienced, INI-naive HIV-1 infected pediatric subjects 12 to <18 years of age was assessed in an ongoing study in children (P1093, ING112578) based on weight band dosing of ~1 mg/kg. In 9 children weighing at least 40 kg, DTG 50 mg once daily dosage resulted in DTG exposure in pediatric subjects comparable to predefined target range based on data in adults receiving DTG 50 mg once daily: 37 to 67 µg.h/mL for AUC(0-) and 0.77 to 2.26 µg/mL for geometric mean of C. One additional subject weighing 37 kg received DTG 35 mg once daily and also demonstrated PK similar to adults receiving DTG 50 mg once daily.
Table 3 Pediatric pharmacokinetic parameters
Age/weight Dolutegravir Dose Dolutegravir Pharmacokinetic Parameter EstimatesGeometric Mean (CV%)
AUC(0-24)g.hr/mL
Cmaxg/mL
C24g/mL
12 to 18 yrs, 40 kg a 50 mg once daily a 46 (43) 3.49 (38) 0.90 (59)
Data Source: m5.3.5.2. ING112578 CSR Table 14a. One subject weighing 37 kg received 35 mg once daily.
A secondary objective of this study was an assessment of efficacy. Eight of 10 subjects achieved virologic suppression (HIV-1 RNA <400 c/mL) at Week 24, with 7 of 10subjects achieving HIV-1 RNA <50 c/mL. The efficacy data further support the validity of the dosing strategy for adolescent (12 to <18 years of age), HIV-infected patients (weighing at least 40 kg) of DTG 50 mg once daily.
Safety data for this study is summarized in Section 5.5. Overall, DTG was demonstrated to be safe and well-tolerated in children 12 to <18 years of age.
Although only treatment-experienced children were enrolled in this age cohort of ING112578 (Cohort I), the primary objective of this study was the assessment of PK and safety, which would be expected to be similar in treatment-naïve patients. Consistent with adult data for DTG 50 mg once daily, variability in AUC and C24h were 43% and 59%, respectively, using an adult tablet formulation administered under modified fasting conditions in adolescents of 12 to <18 years. The Geometric Mean AUC24 for these 10 children in Cohort I was 46 g*h/mL and the C24h was 0.902 g/mL, meeting the pre-defined targeted PK exposure from adults receiving DTG 50 mg once daily (AUC0-24 37to 67 µg*h/ml and C24h 0.77 to 2.26 µg/ml). These DTG exposures have shown to be efficacious in both treatment-naïve and treatment-experienced (INI-naïve) adults in ING113086 and ING111762, respectively, and support the use of DTG 50 mg once daily in treatment-naïve and treatment-experienced (INI-naïve) 12 to <18 year olds weighing at least 40 kg.

CONFIDENTIALModule 2.5 Clinical Overview
20
The virologic and immunologic principles underlying the use of ART are considered to be similar in adults and children. With the use of antiretroviral agents, the course of HIV infection is similar in children compared to adults [Gortmaker, 2001; Doerholt, 2006]. Therefore, efficacy data and exposure-response relationship from adult studies should be relevant for the prediction of antiviral response in HIV infected children. As HIV integrase is a viral target, not a host target, it is expected that the PK/PD relationship between DTG drug exposure and antiviral activity is similar between adults and pediatricpopulations. The guiding principles of disease management in children is similar to adults with the same goals of therapy, i.e., complete suppression of viral replication as measured by plasma HIV-1 RNA and restoration of the immune system.
Therefore, the PK data from ING112578 in adolescents aged 12 to <18 years are sufficiently similar to adults to permit extrapolation of efficacy data from pharmacokinetic correlation, which is in line with the International Conference on Harmonization guidance for medicinal products in the pediatric population [European Medicines Agency (EMA), 2011].
3.2.2.2. Elderly
Pharmacokinetic DTG data in subjects of >65 years old are limited (n=12). However, population pharmacokinetic analysis of dolutegravir using data in HIV-1 infected adults showed no clinically relevant effect of age on the PK profile of DTG (m2.7.2, Section 1.3.5.3).
3.2.2.3. Renal impairment
Renal clearance of unchanged drug is a minor pathway of elimination for DTG. A study of the pharmacokinetics of DTG was performed in subjects with severe renal impairment (CLcr <30 mL/min, not on dialysis) with matched healthy adult controls. No clinically important pharmacokinetic differences between subjects with severe renal impairment (CLcr <30 mL/min) and matching healthy subjects were observed. No dosage adjustment is necessary for patients with mild, moderate, and severe renal impairment. DTG has not been studied in patients on hemodialysis. Due to high protein-binding in plasma (>99%), it is unlikely DTG PK is affected by hemodialysis.
3.2.2.4. Hepatic impairment
DTG is primarily metabolized and eliminated by the liver. In a pharmacokinetic study comparing subjects with moderate hepatic impairment (Child-Pugh Grade B) to matched healthy adult controls, the single dose exposure of DTG was similar between the two groups. No dosage adjustment is necessary for patients with mild to moderate hepatic impairment (Child Pugh grade A or B). The effect of severe hepatic impairment on the pharmacokinetics of DTG has not been studied.

CONFIDENTIALModule 2.5 Clinical Overview
21
3.2.2.5. UGT1A1 Polymorphism
There is no evidence that common UGT1A1 polymorphisms alter DTGpharmacokinetics. In a meta-analysis using pharmacogenetics (PGx) samples collected in clinical studies in healthy subjects (n=89 in total), subjects with genotypes associated with low (n=7) or reduced (n=40) activity of UGT1A1 had similar DTG exposure to subjects (n=41) with wild-type genotype. One subject had a genotype with metabolizer status as unknown. No dose adjustment for DTG is needed in subjects with genotypes conferring poor metabolizer status of UGT1A1 (*28/*28; *28/*37; *37/*37).
3.2.2.6. Co-infection with Hepatitis B or C
Population pharmacokinetic analysis indicated that hepatitis C virus (HCV) co-infectionhad no clinically relevant effect on the exposure to DTG. There are limited PK data in subjects with hepatitis B co-infection. There are no demonstrated or suspected drug interactions between DTG and commonly used drugs for the treatment of hepatitis B virus (HBV) and HCV.
3.2.2.7. Population PK
Population PK analyses using pooled pharmacokinetic data from Phase II and Phase III adult trials in HIV-infected subjects identified weight, age, gender, albumin levels, and smoking status as statistically significant covariates of DTG clearance, volume, or bioavailability. These factors resulted in changes in DTG PK parameters of <30% and are not considered clinically significant. Other factors demonstrating no significant effect were race/ethnicity, HCV co-infection, Centers for Disease Control and Prevention (CDC) classification, mild to moderate renal impairment, creatinine clearance, alanine aminotransferase (ALT), and aspartate aminotransferase (AST). No dose adjustment inDTG is required based on demographic or laboratory factors, smoking status, and disease status (CDC classification of HIV infection).
3.3. Drug-Drug Interactions
The drug-drug interaction studies are described in m2.7.2, Section 2.1.3 and Section 3.
3.3.1. Effect of Dolutegravir on the Pharmacokinetics of Other Agents
In vitro, DTG demonstrated little or no direct inhibition (IC50 values >50 M) in vitro onthe transporters BCRP, multi-drug resistance protein (MRP) 2, organic anion transporting polypeptide (OATP) 1B1, OATP1B3, organic cation transporter (OCT) 1, and Pgp, or the enzymes CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6,CYP3A, uridine diphosphate glucuronosyl transferase (UGT)1A1 or UGT2B7. In vitro, DTG did not induce CYP1A2, CYP2B6 or CYP3A4. In vitro, DTG was noted to have little or no inductive effects on the human Pregnane X Receptor (PXR), or on CYP1A2, 2B6 or 3A4 mRNA. DTG glucuronide, GSK2832500, did not inhibit MRP2, thus inhibition of biliary clearance of bilirubin glucuronides or glucuronide conjugates of co-administered drugs is not expected. Based on these data, DTG is not expected to affect the pharmacokinetics of drugs that are substrates of these enzymes or transporters.

CONFIDENTIALModule 2.5 Clinical Overview
22
In vitro, DTG inhibited the renal organic cation transporter 2 (OCT2, IC50=1.9 M or 0.82 g/mL). Based on this observation, DTG may increase plasma concentrations of drugs for which excretion is dependent upon OCT2, such as dofetilide and metformin. Co-administration of DTG and dofetilide (which has a narrow therapeutic index) is therefore contraindicated. Metformin concentrations may be increased by DTG; subjects should be monitored during therapy and a dose adjustment of metformin may be required.
Results from studies evaluating the effect of DTG on co-administered drugs are shown inTable 4. In vivo drug interaction studies also demonstrated that DTG did not affect the PK of EFV, LPV/RTV, DRV/RTV, ATV, ETR, FPV, RPV, and TVR, by comparing PK data of these agents observed when co-administered with DTG to historical data.

CONFIDENTIALModule 2.5 Clinical Overview
23
Table 4 Effect of DTG on Concomitant Medications
Concomitant drug
Concomitant drug dose DTG dose N GM Ratio (90% CI) Study Conclusion
Co-ad drug +DTG / co-ad drug alone
C24/C AUC Cmax
MDZ 3 mg SD 20 mg once daily(suspension)
10 NA 0.95(0.82, 1.10)
NA ING111322 No effect on MDZ
TDF 300 mg once daily 50 mg once daily 15 1.19(1.04-1.35)
1.12(1.01-1.24)
1.09(0.97-1.23)
ING111604 No TDF dose adjustment
Methadone Individualized dose 50 mg BID 11 Total methadone0.99
(0.91, 1.07)
R-methadone0.95
(0.89, 1.02)
S-methadone1.02
(0.93, 1.12)
0.98(0.91, 1.06)
0.95(0.89, 1.02)
1.01(0.93, 1.09)
1.00(0.94, 1.06)
0.97(0.91, 1.03)
1.03(0.97, 1.10)
ING115698 No methadone dose adjustment
Oral Contraceptive(Ortho-Cyclen)
norgestimate 0.25 mg and ethinyl estradiol 0.035 mg
50 mg BID 15 0.93(0.85, 1.03)
1.02(0.93, 1.11)
0.98(0.91, 1.04)
1.03(0.96, 1.11)
0.89(0.82, 0.97)
0.99(0.91, 1.08)
ING111855 No OC dose adjustment
RPV 25 mg once daily 50 mg once daily 16 1.21 (1.07, 1.38)
1.06 (0.98, 1.16)
1.10(0.99, 1.22)
LAI116181 No RPV dose adjustment
Data Source: m2.7.2, Table 55Note: MDZ: midazolam; OC: oral contraceptive; RPV: rilpivirine.

CONFIDENTIALModule 2.5 Clinical Overview
24
3.3.2. Effect of Other Agents on the Pharmacokinetics of Dolutegravirand Dose Recommendations
DTG is eliminated mainly through metabolism by UGT1A1with CYP3A4 as a minor route. DTG is also a substrate of UGT1A3, UGT1A9, Pgp, and BCRP; therefore drugs that affect UGT1A1, UGT3, UGT1A9, CYP3A4, Pgp, and/or BCRP may theoretically affect DTG plasma concentration.
Moderate to strong inducers of UGT1A1 and/or CYP3A4 such as etravirine (ETR), efavirenz (EFV), rifampicin (RIF), and tipranavir/ritonavir (TPV/RTV) reduced the plasma concentrations of DTG significantly; for C, reductions of75% or more were observed, which overlap with or are outside of the lower bound of the “no effect boundaries” (Section 3.5.3). Phase III Study ING111762 demonstrated that subjects receiving DTG 50mg once daily in combination with TPV/RTV and EFV had lower virologic responses (m2.7.2, Section 2.3.8 and Section 3.4.3.2), therefore DTG 50 mg twice daily dosing is recommended in INI-naïve subjects (treatment-naïve or treatment-experienced) receiving DTG in combination with these agents. As RIF reduced DTG exposure to a similar extent as TPV/RTV and EFV, DTG 50 mg twice daily is also recommended for subjects who require RIF therapy for treatment of TB infection. TPV/RTV, EFV, and RIF may also be given with DTG 50 mg twice daily dose in INI-resistant subjects with caution.
Although not formally assessed in a study, co-administration with nevirapine has the potential to decrease dolutegravir plasma concentration to the extent similar to or less than EFV due to enzyme induction. Therefore, DTG dose adjustment to 50 mg twice daily is recommended when co-administration with nevirapine is needed. Caution is warranted and clinical monitoring is recommended when the combination is given in INI-resistant patients.
Etravirine reduced DTG C by more than 80%, however the effect of ETR was mitigated by co-administration of lopinavir/ritonavir (LPV/RTV) and darunavir/ritonavir (DRV/RTV). The co-administration of DTG 50 mg once daily with ETR is not recommended unless the regimen includes the patient is also receiving concomitant atazanavir/ritonavir (ATV/RTV), LPV/RTV or DRV/RTV.
DRV/RTV 600 mg/100 mg twice daily reduced DTG AUC, Cmax, and C by 22%, 11%, and 38%, respectively, based on Phase I study; such effect is not considered clinically significant. The effect of once daily dosing of DRV/RTV (800 mg/100 mg) was evaluated in Phase III Study ING111762, which showed that subjects receiving DTG 50 mg once daily and DRV/RTV 800 mg/100mg once daily had similar DTG exposures and similar virologic responses when compared to subjects receiving DTG 50 mg once daily and DRV/RTV 600 mg/100 mg twice daily. DTG can be dosed with DRV/RTV (once or twice daily) without dose adjustment.

CONFIDENTIALModule 2.5 Clinical Overview
25
The UGT1A1 inhibitor, ATV (or ATV/RTV) increased DTG AUC by 62% to 91%. Such effect is not considered clinically significant based on accumulated toxicity data in preclinical studies and accumulated safety and tolerability data in humans receiving DTGto date. No dose adjustment is necessary when DTG is co-administered with ATV/RTV or ATV.
Results from studies evaluating the effects of co-administered drugs on the pharmacokinetics of DTG are summarized in the Table 5.

CONFIDENTIALModule 2.5 Clinical Overview
26
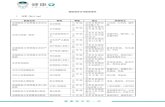
Table 5 Effect of Concomitant Medications on DTG Pharmacokinetics and Dose Recommendation
Co-administered Drug
Co-administeredDrug Dose
DTG Dose N Geometric Mean Ratio (90% CI) of DTG PK Parameters with/without Co-administered Drugs
No Effect = 1.00
Study DTG Dose Recommendation
C or C24 AUC Cmax
TDF 300 mg once daily 50 mg once daily
15 0.920(0.816-1.036)
1.005(0.908-1.113)
0.969(0.867-1.083)
ING111604 No dose adjustment
DRV/RTV 600/100 mg BID 30 mg once daily
15 0.620(0.555-0.694)
0.782(0.722-0.848)
0.892(0.825-0.965)
ING111405 No dose adjustment
LPV/RTV 400/100 mg BID 30 mg once daily
15 0.944(0.848-1.052)
0.973(0.911-1.039)
1.000(0.937-1.066)
ING111405 No dose adjustment
ETR 200 mg BID 50 mg once daily
15 0.121(0.093-0.157)
0.294(0.257-0.337)
0.484(0.433-0.542)
ING111603 Not recommended
ETR/LPV/RTV 200/400/100 mg BID
50 mg once daily
8 1.278(1.130-1.445)
1.105(1.017-1.201)
1.072(1.020-1.128)
ING112934 No dose adjustment
ETR/DRV/RTV 200/600/100 mg BID
50 mg once daily
9 0.629(0.523-0.758)
0.750(0.691-0.814)
0.882(0.781-0.997)
ING112934 No dose adjustment
Multivitamins One-a-Day 50 mg SD 16 0.679(0.560-0.824)
0.668(0.553-0.806)
0.646(0.540-0.774)
ING111602 No dose adjustment
Maalox 20 mL 50 mg SD 16 0.256(0.211-0.311)
0.264(0.218-0.318)
0.276(0.231-0.331)
ING111602 DTG should be taken 2 hours before or 6 hours after antacid
Maalox 2 hrs after
20 mL 50 mg SD 16 0.703(0.579-0.853)
0.743(0.615-0.897)
0.821(0.686-0.984)
ING111602
ATV/RTV 300/100 mg once daily
30 mg once daily
12 2.206(1.972-2.468)
1.617(1.500-1.743)
1.336(1.254-1.423)
ING111854 No dose adjustment
ATV 400 mg once daily 30 mg once daily
12 2.802(2.523-3.113)
1.911(1.802-2.026)
1.495(1.404-1.591)
ING111854 No dose adjustment
OMP 40 mg once daily 50 mg SD 12 0.954(0.752-1.209)
0.971(0.783-1.203)
0.915(0.754-1.111)
ING112941 No dose adjustment
TPV/RTV 500/200 mg BID 50 mg once daily
14 0.239(0.212-0.270)
0.409(0.379-0.443)
0.535(0.500-0.572)
ING113096 DTG 50 mg BIDc
EFV 600 mg once daily
50 mg once daily
12 0.245(0.179-0.336)
0.431(0.346-0.536)
0.608(0.506-0.730)
ING114005 DTG 50 mg BIDc
FPV/RTV 700/100 mg BID 50 mg once daily
12 0.510(0.413-0.629)
0.651(0.542-0.782)
0.763(0.632-0.921)
ING113068 No dose adjustment

CONFIDENTIALModule 2.5 Clinical Overview
27
Co-administered Drug
Co-administeredDrug Dose
DTG Dose N Geometric Mean Ratio (90% CI) of DTG PK Parameters with/without Co-administered Drugs
No Effect = 1.00
Study DTG Dose Recommendation
C or C24 AUC Cmax
RIF 600 mg once daily 50 mg BIDa
11 1.220(1.005, 1.480)
1.327(1.152, 1.529)
1.184(1.026, 1.366)
ING113099 DTG 50 mg BIDc
50 mg BIDb
11 0.277(0.228, 0.336)
0.460(0.384, 0.552)
0.565(0.489, 0.652)
RFB 300 mg once daily 50 mg once daily
9 0.700(0.566, 0.866)
0.947(0.816, 1.098)
1.156(0.978, 1.365)
ING113099 No dose adjustment
Prednisone 60 mg once daily 50 mg once daily
12 1.167(1.062, 1.281)
1.111(1.030, 1.198)
1.062(0.991, 1.139)
ING115696 No dose adjustment
BCV 800 mg q8h 50 mg once daily
13 1.080(0.911, 1.281)
1.068 (0.948, 1.203)
1.052 (0.960, 1.153)
ING115697 No dose adjustment
TVR 750 mg q8h 50 mg once daily
15 1.368(1.290, 1.450)
1.253(1.196, 1.314)
1.185(1.111, 1.264)
ING115697 No dose adjustment
RPV 250 mg once daily 50 mg once daily
16 1.223(1.149, 1.302)
1.121(1.053, 1.194)
1.130(1.055, 1.210)
LAI116681 No dose adjustment
Data Source: m2.7.2, Table 56Note: OMP: omeprazole; FPV/RTV: fosamprenavir/ritonavir; RFB: rifabutin; BCV: bocepravir; TVR: telaprevir; a. Comparison was between DTG 50 mg BID + RIF(test treatment) vs DTG 50 mg once daily (reference treatment).b. Comparison was between DTG 50 mg BID + RIF(test treatment) vs DTG 50 mg BID (reference treatment)c. Caution should be given to INI-resistant subjects.

CONFIDENTIALModule 2.5 Clinical Overview
28
3.4. Pharmacodynamics
The pharmacodynamic studies are described in m2.7.2, Section 2.2.
3.4.1. Effect of DTG on Cardiac Conduction
In a randomized, placebo-controlled, cross-over trial, 42 healthy subjects received single dose oral administrations of placebo, a supratherapeutic dose of DTG at 250 mg as suspension (exposures approximately 2-3-fold of the 50 mg twice daily dose at steady state), and moxifloxacin (400 mg, active control) in random sequence. DTG did not prolong the QTc interval for 24 hours post dose. After baseline and placebo adjustment, the maximum mean QTc change based on Fridericia correction method (QTcF) was 1.99 msec (1-sided 95% upper CI: 4.53 msec).
3.4.2. Effect of DTG on Renal Function
The effect of DTG on serum creatinine clearance (CrCL), glomerular filtration rate (GFR) using iohexol as the probe, and effective renal plasma flow (ERPF) using para-aminohippurate (PAH) as the probe was evaluated in an open-label, randomized, 3 arm, parallel, placebo-controlled study in 37 healthy subjects, who were administered DTG50 mg once daily (n=12), 50 mg twice daily (n=13) or placebo once daily (n=12) for 14 days. A modest decrease (about 10%) in CrCL was observed with DTG within the first week of treatment, consistent with that seen in clinical studies. DTG at both doses had no significant effect on actual GFR or ERPF. These data support in vitro studies which suggest that the small increases in creatinine observed in clinical studies are due to the likely benign inhibition of the organic cation transporter 2 (OCT2) in the proximal renal tubules, which mediates the tubular secretion of creatinine.
3.5. Pharmacokinetic – Pharmacodynamic Relationships and Definition of “No Effect Boundaries”
3.5.1. PK/PD Relationship for Efficacy
3.5.1.1. Short-Term Monotherapy
In a 10-day monotherapy study, ING111521, in HIV-infected ART-naïve subjects, a strong dose-response relationship and exposure-response relationship were observed. A mean decrease from Baseline on Day 11 in plasma HIV-1 RNA of 1.51 to 2.46 log10 c/mL was observed with DTG doses of 2 to 50 mg compared with placebo (0.05 log10 c/mL increase). Antiviral responses were maintained for 3 to 4 days after the last dose in the 50 mg group. Greater antiviral activity was associated with higher DTG plasma exposure. Such relationship was best described by an Emax model, withpharmacokinetic parameter C identified as the best predictor for antiviral activity (Figure 1). DTG exposure from 10 mg once daily dose approximated or exceeded EC90 and DTG exposure from 50 mg once daily are well upon the plateau of curve.

CONFIDENTIALModule 2.5 Clinical Overview
29
Figure 1 Relationship between Reduction in Log10 c/mL Plasma HIV-1 RNA from Baseline to Day 11 and Day 10 C, Best Model in ING111521
Ctau on Day 10 (ng/mL)
Pla
sma H
IV-1
RN
A C
hange f
rom
Base
line t
o D
ay 1
1 (
log10 C
opie
s/m
L)
0 200 400 600 800 1000 1200
0.0
0.5
1.0
1.5
2.0
2.5
3.0
Emax = 2.60 log10EC50 = 35.68 ng/mL
Note: Lines represent the best fitted line (solid) and 95% CI (dashed).Data source: m5.3.4.2 ING111521 CPSR, in-text Figure 1.
3.5.1.2. Long-Term Combination Therapy
Treatment-Naïve Subjects
In HIV-infected ART-naïve subjects where DTG was given in combination with nucleoside reverse transcriptase inhibitors (NRTIs), no relationship between DTG dose or pharmacokinetic exposure and antiviral response was observed at doses ranging from 10 to 50 mg once daily. The lack of dose-response or exposure-response relationship is likely due to the potency of combination therapy, resulting in 79%, 78%, and 88%achieving HIV-1 RNA values <50 c/mL at Week 96 across DTG 10, 25, and 50 mg doses (respectively) in the Phase IIb study ING112276 and an 88% response rate on DTG 50 mg once daily observed at Week 48 in the Phase III study ING113086. Such findings indicate that DTG doses of 10 to 50 mg once daily in combination with dual NRTIs achieved maximum virological suppression in this population.

CONFIDENTIALModule 2.5 Clinical Overview
30
Treatment-Experienced and INI-Naïve Subjects
In HIV-infected, ART -experienced, INI-naive subjects where DTG was given in combination with at least 1 active agent in the background regimen, average DTG trough concentration(C0_avg) was a statistically significant predictor of antiviral response at Week 24 when using all available data.
The use of moderate-strong inducers (TPV/RTV and EFV) in the background therapy was associated with reduced C0_avg and reduced virologic efficacy. Additional PK/PD analyses were thus performed, excluding subjects who were receiving these agents and those with clear evidence of noncompliance (defined as non-detectable DTG concentration observed at one or more PK visits). The results from this additional analysis showed that DTG C0_avg was no longer a predictor of virological response, suggesting that a sufficiently high DTG exposure was achieved for robust virological responses for the rest of the population. Coupled with the statistically significantly greater responses in subjects treated with DTG vs. RAL (plus background regimen), these PK/PD results support the selection of DTG 50 mg once daily for the majority oftreatment-experienced, INI-naïve subjects. DTG at a dose of 50 mg BID is recommended for subjects who require co-administration with TPV/RTV and EFV to ensure optimal responses.
INI-Resistant Subjects
In HIV-infected, INI-resistant subjects in the Phase III study ING112574, DTG trough concentration (C) was not statistically significantly correlated with antiviral activity observed at Day 8 and Week 24. These data suggested that DTG 50 mg twice daily may be at the plateau of the dose-response curve for the drug effect in INI-resistant subjects. These data support the selection of DTG 50 mg twice daily in the INI-resistant population.
3.5.2. PK/PD Relationship for Safety
Plasma DTG exposure was not correlated with the presence of the most frequent AEsincluding diarrhea, nausea, and headache or with most clinical laboratory tests of interest. There was a statistical correlation between DTG exposure and change from Baseline in total bilirubin (likely due to competition with UGT1A1) and serum creatinine (due to known OCT2 inhibition). However, such relationship is not considered clinically significant due to the small, non-progressive changes in these clinical chemistries.
3.5.3. Definition of No Effect Boundaries of Alteration in DTG Exposure
The PK/PD relationship for efficacy defines the lower bound and the PK/PD relationship for safety defines the upper bound. These “no effect boundaries” were used as justification for recommendations on whether dose adjustment was needed for drug interactions or the impact of other intrinsic or extrinsic factors on DTG PK. The lower boundary is proposed to be 25% of DTG C observed at the recommended doses (or 75% reduction in C), and currently the upper boundary cannot be determined due to good safety and tolerability profiles of DTG.

CONFIDENTIALModule 2.5 Clinical Overview
31
The definition of the lower bound of the “no effect boundaries” was based on the finding of no dose-response or PK/PD relationship for antiviral activity at DTG doses from 10 mg to 50 mg once daily in combination with NRTI backbones in Phase IIb treatment-naive trial (ING112276). DTG exposure observed at 10 mg once daily (0.30 g/mL for C) is considered as the lower bound of the “no effect boundaries”, which is 25% of Cobserved at 50 mg once daily (1.20 g/mL). Reduction in DTG C by less than 75% (whilst also accounting for variability) caused by any intrinsic or extrinsic factor is not considered clinically significant and thus does not require DTG dose adjustment.
3.6. Clinical Pharmacology Conclusions
Overall, pharmacokinetics, pharmacodynamics, PK/PD relationship in various patient populations, and drug interaction profiles of DTG support the following dose recommendation:
Treatment-naïve adults: DTG 50 mg once daily.
Treatment-experienced but integrase inhibitor-naïve adults: DTG 50 mg once daily.
Integrase inhibitor resistant adults: DTG 50 mg twice daily.
Integrase inhibitor-naïve children of 12 to <18 years of age and weighing greater than or equal to 40 kg: DTG 50 mg once daily.
No DTG dose adjustment is necessary based on age, gender, race/ethnicity, weight, smoking, CDC classification of HIV infection, HBV/HCV co-infection, UGT1A1 polymorphisms, in subjects with mild to moderate hepatic impairment (Child Pugh grade A or B), and in subjects with mild, moderate, or severe (CrCL<30 mL /min, not on dialysis) renal impairment. DTG can be co-administered with most ART or non-ART drugs without dose adjustment except for the following:
Moderate/strong metabolic inducers: DTG 50 mg twice daily is recommended when co-administered with TPV/RTV, EFV, and RIF. The co-administration of DTG50 mg once daily with ETR is not recommended unless the regimen includesconcomitant ATV/RTV, LPV/RTV or DRV/RTV.
Polyvalent metal cation-containing antacids: DTG should be dosed 2 hours prior to or 6 hours after antacids.

CONFIDENTIALModule 2.5 Clinical Overview
32
4. OVERVIEW OF EFFICACY
Efficacy has been demonstrated for dolutegravir in four Phase III studies (ING113086, ING111762, ING114467, and ING112574) in ART-naive and experienced subjects with HIV infection. Additional efficacy data is provided by longer term supportive studies ING112276 and ING112961.
The following ongoing studies did not contribute to the summary of efficacy: ING112578(P1093), ING116070 (CSF), ING114915 (FLAMINGO), ING114916 (Expanded Access Program) and ING115502 (Named Patient Program).
Module 2.7.3 (Clinical Summary of Efficacy) provides details on the individual efficacy results from the clinical program.
4.1. Non-clinical Virology
A summary of non-clinical and clinical virology can be found in m2.7.2.4 (Special Studies). DTG inhibits HIV integrase by binding to the integrase active site and blocking the strand transfer step of retroviral DNA integration which is essential for the HIV replication cycle. Key non-clinical virology is as follows:
Dolutegravir has low nM activity against wild type HIV-1 and HIV-1 in a variety of cells lines, regardless of subtype. Human serum causes approximately 75-fold increase in DTG IC50. Dolutegravir trough concentration for a single 50 mg dose in integrase inhibitor naïve subjects was 1.20 mcg/mL, 19 times higher than the estimated protein adjusted 90% inhibitory concentration (PA-IC90).
In a viral integrase susceptibility assay using the integrase coding region from 13 clinically diverse clade B isolates, dolutegravir demonstrated antiviral potency similar to that seen with laboratory strains, with a mean IC50 of 0.52 nM. When tested in peripheral blood mononuclear cell (PBMC) assays against a panel consisting of 24 HIV-1 clinical isolates (group M [clade A, B, C, D, E, F and G] and group O) and 3 HIV-2 clinical isolates, the geometric mean IC50 was 0.20 nM and IC50 values ranged from 0.02 to 2.14 nM for HIV-1, while the geometric mean IC50 was 0.18 nM and IC50 values ranged from 0.09 to 0.61 nM for HIV-2 isolates.
DTG is additive or synergistic when assayed in combination with other antiretroviral agents.
Comparative susceptibilities to DTG and RAL were obtained from 60 RAL resistant,site directed HIV-1 mutants and 6 site directed HIV-2 mutants. DTG retained activity against a vast majority of these mutants. Additionally, susceptibilities to DTG and RAL were determined for over 700 RAL resistant clinical isolates, with DTG retaining significant antiviral activity (<10 FC) against >90% of them.
The dissociation of DTG, RAL, and EVG from wild type and mutant IN proteins complexed with DNA was investigated to obtain a better understanding of INI dissociation kinetics. DTG demonstrated slower dissociation from all IN-DNA complexes tested, including those with single, double, and up to four residue IN substitutions.

CONFIDENTIALModule 2.5 Clinical Overview
33
4.2. Selection of Patient Populations in Pivotal and Supportive Efficacy Studies
The registrational studies in adults supporting this submission recruited HIV-1 infected subjects aged 18 years and older who were able to provide written informed consent. Women of child-bearing potential were eligible for enrolment if using a reliable method of contraception as permitted by labeling of comparator agents. Subjects were excluded on the basis of medical history (e.g. active CDC Category C disease with certain exceptions, moderate to severe hepatic impairment, gastrointestinal bleeding, allergy to study drugs, history of malignancies), concomitant or recent medical therapy (e.g. HIV-1 vaccines, treatments with activity against HIV-1 that are not licensed for that purpose, radiation therapy, immunomodulators, cytotoxic chemotherapeutic agents or recent use of experimental drugs) or screening laboratory values (e.g. any verified Grade 4 lab abnormalities, or liver chemistries above specified thresholds). The specific criteria applied during each phase of development reflected DTG data available at that time, and are therefore slightly different for the Phase IIb studies compared to the Phase III studies. Additionally, there are some differences amongst the Phase III studies based on the patient population enrolled or the background regimens administered. Notwithstanding the minimum inclusion and exclusion criteria defined in each protocol, investigators were also required to follow any existing country specific guidelines when making decisions about subjects who are eligible for study participation.
4.3. Rationale for Dose Selection in Clinical Development
Section 4 of m2.7.3 describes in more detail the data relevant to dose selection decisions made with DTG, and concludes with the data supporting the selected dose in ART -naive adults, ART-experienced (INI-naïve) adults and adolescents (of 12 to <18 years old and at least 40 kg of weight), and ART-experienced (INI-resistant) adults with HIV-1 infection.
4.3.1. ART-Naïve/ART-Experienced (INI-Naïve) Subjects
The 50 mg once daily dose for DTG in ART-naïve/ART-experienced (INI-naïve) subjects was selected based on the following:
Results from ING111521, 10-day monotherapy study in treatment-naive or treatment-experienced and INI-naive subjects demonstrate that once daily dosing of DTG achieved viral load declines for 2 mg, 10 mg and 50 mg of 1.54, 2.04, and 2.48 log10 c/mL, respectively. The 50 mg once daily dose achieved an inhibitory quotient (observed DTG concentration at the end of the dosing interval [C]/fold above PA-IC90) of 19, demonstrating considerable coverage above the in vitro protein adjusted target concentration of 0.064 ng/ml.
A PK/PD analysis from ING111521 evaluated the relationship between C and change in HIV RNA from Baseline. The data were fit to a maximum effect model and demonstrated that the 50 mg dose was on the plateau of the concentration-response curve after monotherapy.

CONFIDENTIALModule 2.5 Clinical Overview
34
In ING112276, a Phase IIb dose-ranging study in treatment-naive subjects that evaluated DTG at doses of 10 mg, 25 mg and 50 mg once daily with 2 NRTIs vs.EFV plus 2 NRTIs. DTG was well tolerated across all doses studied. A good safety and tolerability profile with a low discontinuation rate due to AEs was observed in all three arms with no significant dose-dependent trends in safety parameters. All three doses showed similar robust antiviral responses and no apparent dose-response relationship was observed, suggesting DTG doses from 10 mg to 50 mg once daily in combination with 2 NRTIs achieved maximum virologic suppression. Therefore, the highest dose, DTG 50 mg once daily, was selected as the dose for the Phase III studies in INI-naive population. Selection of 50 mg once daily dose was also to accommodate decreases in DTG in light of drug interactions, poor absorption, imperfect adherence, or other cause.
Efavirenz, TPV/RTV, and FPV/RTV decrease the C of DTG by 75%, 76%, and 49%, respectively (m2.7.2, Section 3.4.3). The resulting C values remain 3.4 to 5.5-fold above the protein adjusted IC90 for wild type HIV. In addition, the C values with enzyme inducers range from 0.22 to 0.35 g/mL (see m2.7.2, Section 2.3.3). Despite decreases in DTG exposures with these interactions, the DTG exposure is still comparable to or higher than those demonstrated with 10 mg once daily dosing in ING112276, supporting the selection of DTG 50 mg once daily for use in ING111762.
In summary, a dose of 50 mg once daily demonstrated safety and efficacy while providing a significant coverage in plasma exposure to account for reductions due to drug interactions or other events that could decrease concentrations. This dose was selected for Phase III studies in ART-naive and ART-experienced (INI-naïve) adult subjects.
4.3.2. ART-Experienced (INI-Resistant) Subjects
The 50 mg BID dose selection for DTG in ART-experienced (INI-resistant) subjects was based on the following:
ING112961 Cohort I evaluated 50 mg once daily in subjects with resistance to RAL, but a sub-optimal anti-viral response that was observed in some subjects harboring virus with higher fold change (FC) to DTG prompted the evaluation of an increased dose of DTG in a second cohort of subjects.
PK/PD modeling predicted that increasing the DTG dosage from 50 mg once daily to 100 mg daily dose in populations of raltegravir-resistant subjects would yield substantive improvements in treatment response.
A dose of 100 mg once daily was initially considered for evaluation, however data from healthy subjects in ING114005 demonstrated that plasma DTG exposures increase less-than-dose-proportionally from 50 mg to 100 mg. In addition, one-third of subjects did not have any appreciable increase in C between 50 mg and 100 mg doses. These data demonstrated that a 50 mg twice daily dose would provide more consistent exposures than a dose of 100 mg once daily.

CONFIDENTIALModule 2.5 Clinical Overview
35
ING112961 Cohort II evaluated DTG 50 mg twice daily in a similar population of subjects as Cohort I, but those enrolled had more limited high-level resistance to DTG. Comparison of the primary end-point (proportion of subjects with Day 11 plasma HIV-1 RNA <400 c/mL or at least 0.7 log10 c/mL below their Baseline values) between Cohort I and Cohort II suggested a higher response rate may be achieved with 50 mg twice daily of DTG.
Analyses of data through Week 24 for Cohort II (and Week 72 for Cohort I) in ING112961 confirmed the continued benefit of the 50 mg DTG twice daily regimen without overt increase of clinical or laboratory AEs compared to the 50 mg once daily regimen.
In summary, the short term antiviral response rates, pharmacokinetics, and data through Week 24 of Cohort II (and Week 72 in Cohort I) of ING112961 suggested additional benefit would be realized with DTG 50 mg twice daily compared to the DTG 50 mg once daily dose in this population harboring INI-resistant virus. Therefore the DTG 50 mg twice daily dose was selected for Phase III evaluation in this population.
4.4. Clinical Trial Methodology and Design (Pivotal Efficacy Study Designs)
The study designs details including the objectives, treatment regimens and number of patients enrolled/ randomized for pivotal and supportive efficacy studies are presented in m2.7.3, Section 1.6.
4.4.1. Studies in INI-Naïve Subjects
Pivotal efficacy studies ING113086, ING114467, and ING111762 are Phase III, international, multicenter, parallel-group randomized, double-blind, active-controlled, double-dummy studies conducted in ART-naïve (ING113086 and ING114467) and ART-experienced (INI-naïve) subjects (ING111762). Supportive study ING112276 is a Phase IIb international, multicenter, parallel group randomized partially blinded active controlled dose-ranging study conducted in ART-naïve subjects (Table 6).
4.4.2. Studies in INI-Resistant Subjects
Pivotal efficacy study ING112574 is an international, multicenter, open-label, single-arm, Phase III study to demonstrate the antiviral activity and safety of dolutegravir in HIV-1 infected adult subjects with integrase inhibitor resistance. Supportive study ING112961 is a Phase IIb international, multicenter, open-label single-arm sequential cohort pilot study in ART-experienced (INI-resistant) subjects (Table 6).

CONFIDENTIALModule 2.5 Clinical Overview
36
Table 6 Summary of Studies Supporting Clinical Efficacy of Dolutegravir in the Treatment of HIV-1 Infection
Study Number Phase Study Design Primary Objectives Durationa Regimens
Number of Patientsb
Pivotal Efficacy StudiesING113086(SPRING-2)
III Multicentre randomized, double blind, double-dummy, active-controlled, parallel group, fully-powered non-inferiority study.
Screening viral load (VL) >1000 c/mL, <10 days prior ART.No evidence of resistance at screening.
To assess safety and efficacy of DTG 50 mg once daily compared to RAL 400 mg BID both administered with fixed-dose dual NRTI therapy
48 weeks DTG 50 mg once daily; oral tablet orRAL 400 mg once daily; oral tablet
+ ABC/3TC 600 mg/ 300 mg once daily; oral tablet or+ TDF/ FTC 300 mg/ 200 mg once daily; oral tablet
DTG:413 Randomized364 Ongoing0 Completed
RAL:414 Randomized355 Ongoing0 Completed
ING114467(SINGLE)
III Randomized, double-blind, double-dummy, active-controlled, multicentre, parallel group, fully-powered non-inferiority study.
Screening VL >1000 c/mL,HLA-B*5701 negative,<10 days prior ART,No evidence of resistance at screening
To assess safety and efficacy of DTG plus ABC/3TC fixed-dose combination therapy administered once daily compared to Atripla
48 weeks DTG 50 mg once daily; oral tablet + ABC/3TC 600/300 mg once daily; oral tablet
EFV/TDF/FTC 600/200/300 mg once daily; oral tablet
DTG + ABC/3TC:422 Randomized363 Ongoing0 Completed
EFV/TDF/FTC:422 Randomized363 Ongoing0 Completed
ING111762(SAILING)
III Multicentre randomized, double-blind, active-controlled, parallel group, non-inferiority study.
2 Screening VL>400 c/mL or 1 Screening VL >1000 c/mL,at least 2-class resistance,Potential for 1 fully active agent in background regimen (BR), No INI experience
To evaluate safety and efficacy of DTG 50 mg once daily vs. RAL 400 mg BID, both administered with an investigator-selected background regimen
24 weeks DTG 50 mg once daily; oral tabletRAL 400 mg BID; oral tablet
+ Investigator-selected background regimen
DTG354 Randomized305 Ongoing1 Completedc
RAL361 Randomized189 Ongoing111 Completed

CONFIDENTIALModule 2.5 Clinical Overview
37
Study Number Phase Study Design Primary Objectives Durationa Regimens
Number of Patientsb
ING112574(VIKING-3)
III Multicentre, open-label, single arm.
Screening VL >500 c/mL,Documented virologic failure on RAL or ELV,Documented resistance to RAL or ELV,At least 3-class resistance (including INIs),Potential for 1 fully active agent in optimized background regimen (OBR)
To assess the antiviral activity of DTG administered with failing background therapy to Day 8 and thereafter with optimized background ART
24 weeks DTG 50 mg BID; oral tablet DTG 183 Enrolled155 Ongoing0 Completed

CONFIDENTIALModule 2.5 Clinical Overview
38
Study Number Phase Study Design Primary Objectives Durationa Regimens
Number of Patientsb
Supportive Efficacy StudiesING112276(SPRING-1)
IIb Randomized, multicentre, parallel group, dose-ranging.
Screening VL >1000 c/mL,Screening CD4 >200 cells/mm3,<10 days prior ART,No evidence of resistance at screening
To select a once daily oral dose of DTG administered with either ABC/3TC or TDF/FTC and to evaluate antiviral activity, safety and PK over time
96 weeks DTG 10 mg once daily; oral tabletDTG 25 mg once daily; oral tabletDTG 50 mg once daily; oral tabletEFV 600 mg once daily; oral tablet
+ ABC/3TC 600 mg/ 300 mg once daily; oral tablet
or
+ TDF/ FTC 300 mg/ 200 mg once daily; oral tablet [At the Week 96 visit, all DTG subjects were switched to the selected dose of 50 mg once daily]
DTG 10 mg53 Randomized47 Ongoingd
DTG 25 mg51 Randomized45 Ongoingd
DTG 50 mg51 Randomized46 Ongoing
EFV50 Randomized41 Completed
ING112961(VIKING)
IIb Multicentre, open-label, single arm, sequential cohort, pilot study.
Screening VL >1000 c/mL,RAL resistance at Screening,At least 3-class resistance (including INIs),Potential for 1 fully active agent in OBR (BID Cohort only)
To assess the antiviral activity of DTG containing regimen
Cohort I: 96 weeksCohort II: 48 weeks
DTG 50 mg once daily; oral tabletDTG 50 mg BID; oral tablet
DTG 50 mg once daily27 Enrolled13 Ongoing0 Completed
DTG 50 mg BID24 Enrolled19 Ongoing0 Completed
a. Weeks for evaluation of efficacy in this submission.b. For ongoing studies, the number of subjects reported as of data cutoff date (~ or data cutoff date in respective CSR).c. One subject who completed the DTG treatment decided they did not want to participate in the open label phase. d. DTG 10 mg and 25 mg subjects are currently ongoing on DTG 50 mg.

CONFIDENTIALModule 2.5 Clinical Overview
39
Estimated timings for the completion of study reports following the initial submission are presented in Table 7.
Table 7 Data Availability for Ongoing Studies
Study Identifier
Length of StudyData Available at Initial
SubmissionEstimated Completion
of Study Report
ING112578 48 weeks, with up to 3-year follow-up
10 subjects (Stage 1) from Cohort 1 through 24 weeks
/ Week 24 Analysis (Cohort 1, Stages 1 & 2)
ING116070 96 weeks (primary endpoint at Week 16)
All subjects through 2 weeks / Week 16 Analysis
ING113086 96 weeks All subjects through 48 weeks / Week 96 Analysis
ING112574 24 and 48 weeksAll subjects through Day 8, 114/183 subjects through 24 weeks
/ Week 24 (all)/ Week 48 (first 114 subjects) Analysis
ING116529 7 days double-blind phase and 48 weeks open-label phase.
No efficacy data / Day 8 Analysis
ING111762 48 weeks All subjects through 24 weeks / Week 48 AnalysisING114915 96 weeks No efficacy data / Week 48 AnalysisING114467 144 weeks All subjects through 48 weeks / Week 96 Analysis
4.5. Efficacy Endpoints and Statistical Considerations of Efficacy Analyses
4.5.1. Primary and Secondary Efficacy Endpoints
The primary endpoint for pivotal studies ING113086, ING114467, and ING111762 was analyzed using a Missing, Switch or Discontinuation = Failure (MSDF) algorithm as codified by the FDA’s “snapshot” algorithm (m2.7.3, Section 1.8).
The primary endpoints for pivotal and supportive studies are listed in Table 8. Secondary endpoints are provided in m2.7.3, Section 1.8.2.

CONFIDENTIALModule 2.5 Clinical Overview
40
Table 8 Primary Efficacy Endpoints in Pivotal and Supportive Studies
Pivotal Studies ING113086 ING114467 ING111762 ING112574Proportion of subjects with HIV-1 RNA <50 c/mL through Week 48 (MSDF)a
X X X
Mean change from Baseline in plasma HIV-1 RNA (log10 c/mL) at Day 8 (LOCFDB) (for hypothesis testing)b
X
Proportion of subjects with plasma HIV-1 RNA <50 c/mL at Week 24 (MSDF)a
X
Supportive Studies ING112961 ING112276 ING111521Proportion of subjects with Day 11 plasma HIV-1 RNA <400 c/mL or at least 0.7 log10 c/mL below Baseline
X
Proportion of subjects with HIV-1 RNA <50 c/mL through Week 16 (TLOVR) c
X
Change from Baseline in plasma HIV-1 RNA to Day 11 XDTG PK parameters following dose administration on Day 1 Xa. Analyzed using the Missing, Switch or Discontinuation = Failure (MSDF) algorithm as codified by the FDA’s
“snapshot” algorithm.b. Analyzed using a last observation carried forward (discontinuation equals baseline) (LOCFDB) dataset.c. Analyzed using to Time to Loss of Virological Response (TLOVR) algorithm
4.5.2. Statistical Considerations
Details of the statistical methodology are described in m2.7.3, Section 1.9.3.
Assumptions underlying the determination of study sample size requirements, varied across the pivotal and supportive trials:
ING113086: Assuming a 75% response rate in the RAL arm, the study required 394 evaluable subjects per arm to have 90% power with a 10% non-inferiority margin and a one-sided 2.5% significance level. The selection of a 10% non-inferiority margin has been well described [Hill, 2008]. The study was stratified on the following factors: Screening HIV-1 RNA (100,000 vs. >100,000 c/mL) and investigator-selected NRTI backbone (ABC/ 3TC vs. TDF/FTC).
ING114467: Assuming a 75% response rate in the TDF/FTC/EFV arm, the study required 394 evaluable subjects per arm to have 90% power with a 10% non-inferiority margin and a one-sided 2.5% significance level. The study was stratified on the following factors: Screening HIV-1 RNA (100,000 vs. >100,000 c/mL) and CD4+ cell count (200 vs. >200 cells/mm3).
ING111762: Assuming a 65% response rate in the RAL arm, the study required 333 subjects per arm to have 90% power with a 12% non-inferiority margin and a one-sided 2.5% significance level. Recruitment of subjects with fully PI/r susceptible virus who received DRV/RTV was capped at 170 subjects in order to help achieve at least 80% power to detect non-inferiority in the “added sensitivity (AS)” population (defined in ING111762 CSR Section 4.8.3). Assuming a response rate of 65% in that population, and a non-inferiority margin of 12%, this requires at least 249 subjects per arm. The study was stratified on the following factors: Screening HIV-1RNA (50,000 vs. >50,000 c/mL), use of DRV/RTV with or without primary PI

CONFIDENTIALModule 2.5 Clinical Overview
41
mutations (yes vs. either no DRV/RTV use or presence of primary PI mutations), and number of fully active background agents (2 vs. <2).
ING112574: Assuming a standard deviation of 0.5 log10 c/mL for the change from Baseline in plasma HIV-1 RNA at Day 8, this study required fewer than 20 subjects to be powered at 90% on the primary hypothesis test. However, the minimal sample size was expanded to 150 to 200 subjects to allow a comprehensive assessment of the safety, antiviral activity and PK of DTG in this study, acknowledging constraints on the availability of the study patient population. The primary endpoint at Week 24 is the proportion of subjects with plasma HIV-1 RNA <50 c/mL. A single arm study with 100 subjects will provide a precision (i.e. standard error) of four percentage points, which translates to a 95% confidence interval (CI) of 72% to 88% for an assumed response rate of 80% (% <50 c/mL at Week 24).
Across the pivotal and supportive studies the analysis populations upon which the efficacy analyses were based are defined in m2.7.3 Section 1.9.2.
The Intent-to-Treat Exposed population consisted of all randomized subjects who received at least one dose of investigational product. The Modified Intent-to-Treat Exposed population for the ING111762 study consisted of all randomized subjects who received at least one dose of investigational product, and who were not at one study site (Site # 083523, Investigator ID=096536, n=4 subjects enrolled) in Russia that was closed early after the sponsor became aware of GCP noncompliance issues in another ViiV Healthcare-sponsored study. The ITT-E (ING113086, ING114467, ING112574, ING112961, ING112276, and ING111521) and mITT-E (ING111762) are the primary populations for efficacy analyses.
4.6. Efficacy Results in all Studies
Due to differences in study designs and comparator arms, data from the studies was not combined and therefore, are presented in a side-by-side format for comparative purposes.
4.6.1. Enrolment of Key Demographic Subpopulations in ING113086, ING114467, and ING111762
In Studies ING113086 and ING114467 about 15% of treatment-naïve subjects enrolled were women (Table 9). In Study ING114467, a limiting factor to enrolment of women was use of a blinded comparator with pregnancy warnings for women (Atripla). However, due to the size (>800 subjects each study) of the treatment-naïve studies, a total of 130 women were treated on DTG-containing regimens in these two studies. In contrast, a higher percentage of women was enrolled in ING111762 (32%), which may be due in part to the country distribution (the study enrolled subjects in Argentina, Brazil, and South Africa). Overall, women were well-represented across the clinical program to allow for an assessment of the efficacy and safety of DTG in this key subpopulation of HIV-infected patients.
Across treatment-naïve studies, ING113086 and ING114467, 285 subjects (9 to 24%) enrolled were of African American/African heritage (Table 9). In contrast, a higher percentage of African American/African heritage subjects were enrolled into ING111762(42%), which was likely due in part to the inclusion of South Africa in this study.

CONFIDENTIALModule 2.5 Clinical Overview
42
Overall, the racial diversity (especially African American/African heritage patients) of the HIV population was well-represented across the clinical program to allow for an assessment of the efficacy and safety of DTG in this key subpopulation of HIV-infected patients.
Enrolment of geriatric subjects (65) ranged from about 1 to 2% across treatment-naïve studies. In ING113086, one subject in the DTG treatment arm was 68 years and 5 subjects in the RAL treatment arm were >65 years of age. In ING114467, one subject on DTG + ABC/3TC and 6 subjects (1%) on Atripla were 65 years old. Enrolment of subjects 50 years ranged from 10 to 24% (Table 9). In the treatment-experienced (INI-naïve) study, ING111762, 24% of subjects were 50 years including 12 subjects who were 65 years old (6 DTG and 6 RAL) (Table 9, ING111762 Week 24 CSR Table 7.8).
Other key populations, such as severly immunosuppressed and viral hepatitis co-infected patients, were adequately represented across the clinical program to allow for a robust assessment of DTG efficacy and safety.
Table 9 Proportion of Demographic Sub-populations in ING113086, ING114467, and ING111762
ART-Naïve, INI-Naive ART-Experienced, INI-NaiveING113086 ING114467 ING111762
Subgroup ofInterest
DTG50 mg
once daily+ 2 NRTIN=411n (%)
RAL400 mg
BID+ 2 NRTIN=411n (%)
DTG 50 mg+ ABC/3TConce daily
N=414n (%)
EFV/TDF/FTConce daily
N=419n (%)
DTG 50 mg once daily
+ BR
N=354n (%)
RAL 400 mg BID + BR
N=361n (%)
Females 63 (15) 56 (14) 67 (16) 63 (15) 107 (30) 123 (34)African American/African Heritage
49 (12) 39 (9) 98 (24) 99 (24) 143 (41) 160 (44)
Hepatitis C virus (HCV)
41 (10) 35 (9) 27 (7) 29 (7) 32 (9) 49 (14)
Hepatitis B virus (HBV)
7 (2) 8 (2) 1 (<1) 1 (<1) 18 (5) 17 (5)
CD4+ <50 cells/mm3
8 (2) 6 (1) 11 (3) 14 (3) 62 (18) 59 (16)
CD4+ <200 cells/mm3
55 (13) 50 (12) 56 (14) 54 (13) 173 (49) 184 (51)
CDC Category C 9 (2) 9 (2) 18 (4) 17 (4) 173 (49) 158 (44)
Age 50 years 41 (10) 46 (12) 53 (13) 44 (11) 85 (24) 84 (23)Data Source: ING113086 Week 48 CSR Table 6.9, Table 6.10, Table 6.12, Table 6.13, Table 6.21, ISE Table 1.1ING114467 Week 48 CSR Table 6.10, Table 6.11, Table 6.13, Table 6.14, Table 6.22, ISE Table 1.2ING111762 Week 24 CSR Table 6.10, Table 6.13, Table 6.14 and Table 7.8.

CONFIDENTIALModule 2.5 Clinical Overview
43
4.6.2. ART-Naïve
4.6.2.1. Demographics and Baseline Characteristics
Overall, enrolment into ING113086 and ING114467 reflects the demographic characteristic of the general ART-naïve population with HIV infection. Median age was 35 years, ~15% were female and ~20% were African American/ African Heritage (Table 9).
Other Baseline characteristics were well-distributed across the studies and treatment arms. Median Baseline HIV-1 RNA ranged from 4.52 to 4.70 log10 c/mL, and median Baseline CD4 cell count ranged from 335 to 362 cells/mm3, which likely reflects current guidelines and clinical practice for early treatment initiation (m2.7.3, Section 3.1).
4.6.2.2. Key Efficacy Endpoints
In treatment-naïve subjects, DTG administered once daily with two NRTIs demonstrated non-inferiority to RAL at Week 48 (ING113086: Adjusted Treatment Difference [95% CI] +2.5% [-2.2%, +7.1%]) and co-administered with ABC/3TC demonstrated superiority compared to Atripla (ING114467: Adjusted Treatment Difference [95% CI] +7.4% [+2.5%, +12.3%], p=0.003). Consistent response rates (i.e., HIV-1 RNA <50 c/mL; 88% for both studies) were observed across the two studies for the DTG treatment regimens. Per protocol and other sensitivity analyses in both studies support the primary endpoint in each study. The statistically significant difference in response rates noted in ING114467 was primarily due to lower discontinuations due to AEs on the DTG regimen (m2.7.3 Section 3.2.1.1).
Consistent with prior studies of INIs, rapid virologic responses were observed on DTG-based and RAL-based regimens (Figure 2 and Figure 3). The time to virologic suppression was significantly faster on DTG + ABC/3TC (28 days) when compared to TDF/FTC/EFV (84 days), hazard ratio: 2.32 [2.00, 2.68], p<0.001. This analysis was pre-specified and adjusted for multiplicity.

CONFIDENTIALModule 2.5 Clinical Overview
44
Figure 2 ING113086 Week 48, Proportion (95% CI) of Subjects with Plasma HIV-1 RNA <50 c/mL (Snapshot) by Visit
Data Source: ING113086 Week 48 CSR Figure 7.1
Figure 3 ING114467 Week 48 Proportion of Subjects with Plasma HIV-1 RNA <50 c/mL Snapshot Analysis by Visit
Note: confidence intervals are derived using the normal approximation. (Triangles: DTG+ABC/3TC once daily, Squares: Atripla once dailyData Source: ING114467 48 Week CSR Figure 7.1

CONFIDENTIALModule 2.5 Clinical Overview
45
The rapid and significant viral load reductions seen with DTG containing regimens were associated with substantial and sustained CD4 increases over 24 to 48 weeks. At Week 48 the median CD4 increases were comparable with RAL (+230 cell/mm3; both arms, ING113086) (m2.7.3, Table 43).
In Study ING114467, using the Repeated Measures Mixed Model Analysis, DTG+ABC/3TC was statistically superior to Atripla with respect to change from Baseline in CD4 in Week 48 (Adjusted mean change from Baseline: DTG+ ABC/3TC 267 cells/mm3 and Atripla 208 cells/mm3, difference 58.9 [33.4, 84.4] p <0.001). Differences in CD4 cell counts were seen as early as Week 4 and persisted through Week 48. This analysis was pre-specified and adjusted for multiplicity.
HIV-associated conditions in subjects treated with DTG compared to RAL and Atripla were assessed over time by summaries of the incidence of post-Baseline HIV conditions, and by the proportion of subjects with disease progression. Across treatment-naïve studies, there was a similar low incidence of HIV associated conditions (1 to 3% across all treatment-naive studies; Data Source: ING113086 Week 48 CSR and ING114467Week 48 CSR), and in the number of subjects with HIV disease progression (m2.7.3, Table 44).
4.6.2.3. Comparison of Primary Efficacy Results in Sub-populations
Results of various subgroup analyses supported the findings of the primary analysis (m2.7.3, Section 3.3.1). To assess the generalizability of the primary analysis results, consistency of the treatment difference was explored within subgroups. Homogeneity of the treatment difference was formally tested within each strata related to randomization in pre-specified analyses. Other subgroups were explored based on summaries of the treatment differences within the group to identify any potential interaction.
In the treatment-naïve studies ING113086 and ING114467, there was no clinically meaningful difference between the proportion of subjects aged <50 years or 50 years in the DTG treatment groups who achieved HIV-1 RNA <50 c/mL by Week 48 (m2.7.3, Section 3.3.1.1, Table 60). These studies showed similar responses in the DTG treatment groups for the primary efficacy endpoint in other categories including gender and race (m2.7.3, Section 3.3.1.1, Table 60).
Across treatment-naive studies, the DTG response rate was comparable to or better than comparator for subjects whose Baseline HIV-1 RNA was >100,000 c/mL and for subjects whose Baseline HIV-RNA was ≤100,000 c/mL (m2.7.3, Section 3.3.1.2, Table 61). In ING114467, an identical 7% response difference in favor of the DTG-containing arm was observed in each of these strata. As seen in prior studies with other antiretrovirals, responses in general were higher in subjects with Baseline HIV-1 RNA 100,000 c/mL when compared to subjects whose Baseline HIV-1 RNA was >100,000 c/mL (m2.7.3, Section 3.3.1.2, Table 61).
Analysis according to Baseline HIV-1 RNA level supports the conclusion that treatment effects are not heterogeneous across the predefined strata in ING113086 and ING114467(ING113086 Week 48 CSR Section 6.2.1, ING114467 Week 48 CSR Section 6.2.2).

CONFIDENTIALModule 2.5 Clinical Overview
46
Good treatment responses were also observed across Baseline CD4+ cell count categories(Table 10). In subjects with <200 CD4+ cells at Baseline, the DTG arm showed a bigger treatment difference in ING113086 and a smaller treatment difference in ING114467. These differences were not statistically significant, and are likely attributable to the low number of subjects with low CD4+ cell counts. In addition, in ING114467, higher response rates were maintained in the DTG + ABC/3TC in subjects with 200 cells at Baseline (Table 10).
Finally, in ING113086, no significant differences in response were observed according to investigator-selected NRTI backbones, providing further support for the non-inferiority of DTG vs. RAL in treatment-naïve subjects (Table 10).
Table 10 Treatment Response based on Stratification Factors: HIV-1 RNA <50 c/mL by Baseline HIV-1 RNA, CD4+ cell count, Background NRTI in ART-Naïve Subjects
Response <50 c/mL ING113086a,b ING114467a,c
Week 48/ Snapshot Week 48/ SnapshotDTG 50 mg once daily+ 2 NRTIN=411
RAL 400 mg BID + 2 NRTI
N=411
DTG 50 mg + ABC/3TC once daily
N=414
EFV/TDF/FTC once daily
N=419Baseline HIV-1 RNA≤100,000 c/mL 267/297 (90) 264/295 (89) 253/280 (90) 238/288 (83)>100,000 c/mL 94/114 (82) 87/116 (75) 111/134 (83) 100/131 (76)Baseline CD4+ cell count
<200 cells/mm3 43/55 (78) 34/50 (68) 45/57 (79) 48/62 (77)
200 cells/mm3 318/356 (89) 317/361 (88) 319/357 (89) 290/357 (81)
Background NRTIABC/3TC 145/169 (86) 142/164 (87) -TDF/FTC 216/242 (89) 209/247 (85)Other - -Data Source: ING113086 Week 48 CSR Table 7.5, Table 7.6 and Table 7.7; ING114467 Week 48 CSR Table 7.10.a. Baseline HIV-1 RNA: The lower ends of the 95% CIs for the treatment differences are above -10%. The test for
evidence against homogeneity of the treatment difference across high and low Baseline HIV-1 RNA was not statistically significant.
b. Background NRTI: The lower ends of the 95% CIs for the treatment differences are above -10%. The test for evidence against homogeneity of the treatment different across NRTI backbones was not statistically significant. In this study, investigators chose the dual NRTI backbone of either ABC/3TC or TDF/FTC for each subject. Overall, 41% of subjects received ABC/3TC, and 59% of subjects received TDF/FTC (m5.3.5.1, ING113086 Week 48 CSR Table 6.26).
c. Baselines CD4: The test for evidence against homogeneity of the treatment different across high and low Baseline CD4 was not statistically significant
Notes:ABC/3TC = ABC 600 mg and 3TC 300 mg in the form of EPZICOM/KIVEXAEFV/TDF/FTC = EFV 600 mg, TDF 300 mg, FTC 200 mg in the form of Atripla.N = Number of subjects in each treatment group.

CONFIDENTIALModule 2.5 Clinical Overview
47
Among subjects with low viral load (100,000 c/mL) receiving ABC/3TC, response rates were similar between the DTG and RAL treatment groups (DTG 87%, RAL 88%) (m2.7.3, Section 3.3.1.2, Table 62). Among subjects with low viral load (100,000 c/mL) and receiving the TDF/FTC NRTI, response rates between the DTG and RAL treatment groups again were similar (DTG 92%, RAL 91%).
Among subjects with high viral load (>100,000 c/mL) receiving ABC/3TC, response rates were similar between the DTG and RAL treatment groups (DTG 81%, RAL 82%). For subjects with viral load >100,000 c/mL receiving TDF/FTC, response rates were more disparate (DTG 83%, RAL 71%) (m2.7.3, Section 3.3.1.2).
4.6.3. ART-Experienced (INI-Naïve) Subjects
4.6.3.1. Demographics and Baseline Characteristics
The study population was very diverse in both race and gender, with 42% African American / African heritage and 32% female subjects. Of the 230 women entered in the study, 138 (60%) were enrolled in countries outside of North America and Europe (Data Source: ING111762 Week 24 CSR Table 6.23). The majority of non-white subjects were enrolled in North America (44%) and non-European countries (52%). The median age of the mITT-E population was 43.0 years (m2.7.3, Section 3.1.2).
Baseline characteristics were well balanced across the treatment groups. Study subjects had relatively advanced HIV-1 disease with a median Baseline CD4 cell count of 200 cells/mm3 and almost half of the study population having CDC Category C Classification at entry. Subjects predominantly had HIV-1 subtype B (68%), but subjects with a variety of subtypes were enrolled, including A1, AB, AE, AG, BF, C, CD, complex, F, F1, and G (Data Source: ING111762 Week 24 CSR, Section 5.4).
Overall, subjects enrolled in this study had prior treatment with and resistance to a broad range of ART (m2.7.3, Section 3.1.2, Table 30 and Table 31): 47% of subjects had previously been exposed to drugs in three or more ART classes. Baseline resistance testing indicated that overall, similar proportions of subjects had 2-class resistance (364/715; 51%) versus resistance to three or more classes (351/715; 49%).
4.6.3.2. Key Efficacy Endpoints
In ING111762 study, virologic suppression (HIV-1 RNA <50 c/mL) in the DTG arm (79%) was statistically superior to the RAL arm (70%), based on the Week 24 prespecified analysis of outcomes of the FDA Snapshot (MSDF) algorithm (mITT-EPopulation). This treatment difference was statistically significant in favor of DTG (adjusted difference and 95% CI, +9.7% [+3.4%, +15.9%], p=0.003). This result is supported by the Per-Protocol analysis where 81% and 72% of DTG and RAL subjects, respectively, achieved plasma HIV-1 RNA <50 c/mL at Week 24 (treatment difference and 95% CI +9.3% [+3.0%, +15.7%], Data Source: ING111762 Week 24 CSR Table 7.2).

CONFIDENTIALModule 2.5 Clinical Overview
48
There were fewer virologic nonresponders using the Snapshot (MSDF) algorithm through Week 24 in the DTG group compared to the RAL group (DTG: 15%; RAL: 24%) (m2.7.3, Section 3.2.2.1, Table 46).
The proportion of subjects with plasma HIV-1 RNA <50 c/mL using Snapshot (MSDF)analysis for the mITT-E Population increased steeply in both treatment groups from Baseline to Week 4, then tended to plateau starting at Week 8 through Week 24 (Figure 4).
Figure 4 ING111762 Week 24, Proportion (95% CI) of Subjects with Plasma HIV-1 RNA <50 c/mL by Visit – Snapshot (MSDF) Analysis (mITT-E Population)
Data Source: ING111762 Week 24 CSR Figure 7.1Note: confidence intervals are derived using the normal approximation.
Mean and median CD4+ cell counts increased from Baseline to Week 24 in the DTG and RAL groups. The mean changes in CD4+ cell count from Baseline were +113.9 cells/mm3 in the DTG group and +105.8 cells/mm3 in the RAL group at 24 weeks (m2.7.3, Section 3.2.2.2, Table 47).
HIV-associated conditions in subjects treated with DTG compared to RAL were assessed over time by summaries of the incidence of post-Baseline HIV conditions, and by the proportion of subjects with disease progression. There was a similar low incidence of HIV associated conditions, excluding recurrences (DTG: 3%; RAL: 5%; Data Source: ING111762 Week 24 CSR, Section 6.4). The number of subjects with HIV disease progression was low (n=8 or 2% in each arm progressed to CDC Class C or death)(m2.7.3, Section 3.2.2.2, Table 48). RAL had cases of progressions from a lower class to Class C (n=3) and had 2 cases of progression to death; whereas the only progressions to Class C for DTG were from Class C to New Class C.

CONFIDENTIALModule 2.5 Clinical Overview
49
4.6.3.3. Comparison of Principal Efficacy Results in Sub-populations
Higher response rates in the DTG vs. RAL arm were consistent across subgroups defined by almost all clinical characteristics. The exceptions were age (50 years) and the use of boosted darunavir, where RAL responses were comparable to DTG (m2.7.3, Section 3.3.2).
Across stratification factors, the treatment difference between DTG and RAL was maintained, with the exception of DRV use without primary PI mutations. In the RAL arm, virologic response rates were higher in subjects who used DRV/RTV without primary PI mutations (81% by Week 24) than in those who either did not use DRV/RTVor used DRV/RTV in the setting of primary PI mutations. The difference in virologic response rates between DTG and RAL were thus diminished in those subjects receiving DRV/RTV without primary PI mutations. The treatment difference between DTG and RAL were otherwise maintained across stratification factors including Baseline HIV-1 RNA ( and >50 000 c/mL) and by the number of fully active background agents as measured by Baselins PSS (2 and <2) (m2.7.3, Section 3.3.2.2., Table 64). The treatment differences in favor of DTG over RAL were maintained across key demographic subgroups (including race and gender), with the exception of age (m2.7.3, Section 3.3.2.1, Table 63). In subjects aged 50 years, the RAL virologic response rate was comparable to the DTG treatment group (m2.7.3, Section 3.3.2, Table 63). The treatment differences favoring DTG were consistent by HIV subtype as well (Clade B vs. Clade C vs. Other).
4.6.4. Treatment Emergent Resistance in INI-Naïve Subjects
A lower rate of confirmed virological failure with development of resistance mutations or decreased susceptibility to any drugs in the regimen was observed in the DTG treatment arms compared to EFV in ING114467 and RAL in ING113086 and ING111762.
Protocol defined virologic failure (PDVF) rates in ING113086 and ING114467 were low and consistent for the DTG-containing regimens (5% and 4%, respectively), despite stringent PDVF criteria (confirmed HIV-1 RNA 50 c/mL at or after Week 24).
In the ING111762 Week 24 analysis, treatment-experienced (INI-naive) subjects receiving DTG were less likely to have genotypic or phenotypic evidence of treatment-emergent resistance at PDVF (confirmed plasma HIV-1 RNA levels ≥400 c/mL on or after Week 24; full definition in ING111762 Week 24 CSR, Section 7.1). In a pre-specified analysis, there was a statistically significant difference in favor of DTG for the proportion of mITT-E subjects harboring virus with evidence of INI Resistance by Week 24 (DTG: 2/354 (0.6%); RAL: 10/361(2.8%); p=0.016).
Across the treatment-naive studies, no subjects on DTG treatment arms developed clinically relevant INI resistance mutations, but subjects on comparator agents (RAL, EFV) developed clinically relevant resistance mutations to these third agents. In ING111762, there were two subjects in the DTG arm with emergent integrase-defined substitutions. Both had experienced virologic rebound instead of non-response, had no defined integrase resistance substitutions at Baseline, and acquired a substitution at R263

CONFIDENTIALModule 2.5 Clinical Overview
50
in the integrase open reading frame. In each case the DTG fold change was <2, as was the maximum RAL fold change. Neither of these subjects with emergent substitutions at R263 had RAL-associated secondary mutations at Baseline.
Furthermore, no mutations were noted to background NRTI (ART-naive studies) with 50 mg DTG-based regimens in comparison to Atripla or RAL-based regimens in treatment-naïve subjects (Table 11). There were few examples of emergent resistance to the background regimen at PDVF in the RAL arm (6/361) or the DTG arm (3/354) in ART-experienced subjects (m2.7.2.4).
Table 11 Number of Protocol-Defined Virologic Failures (+/- Resistance to integrase, NNRTI, BR) in ART-Naïve and ART-experienced Subjects
ART-Naïve Adults
ING113086 ING114467
Week 48 Week 48
DTG 50 mg once daily + 2 NRTIN=411
RAL 400 mg BID
+ 2 NRTIN=411
DTG 50 mg + ABC/3TC once daily
N=414
EFV/TDF/FTC once daily
N=419
Protocol-defined Virologic Failure, n (%) 20 (5) 28 (7) 18 (4) 17 (4)
Genotype/phenotype Determinable, n (%)
INI-r Mutations Present 0 1/18 (6)a 0c 0
NNRTI-r Mutations Present - - 0 4 (24)d
NRTI-r Mutations Present 0 4/19 (21)b 0 1 (6)e
ART-Experienced Adults
ING111762
Week 24
DTG 50 mg once daily + BR
N=354
RAL 400 mg BID + BR
N=361
Protocol-defined Virologic Failure 14 (4) 34 (9)
Genotype/phenotype Determinable
INI Mutations Present 2/9 (22%)f 9/27 (33)
Data Source: ING113086 Week 48 CSR Table 7.22, Table 12.2, Table 12.4, and Listing 43; ING114467 Week 48 CSR Table 7.7, Table 12.2, Table 12.4, and Listing 47; ING111762 Week 24 CSR Table 12.2 and Table 7.10. R=resistance to integrase, NNRTI and BRa. T97T/A, E138E/D, V151V/I, N155Hb. A62A/V (n=2), K65K/R, K70K/E, M184M/I, M184M/V, M184Vc. IN Substitution (n=1) E157Q/P at Week 24. DTG FC = 1.13; RAL FC = 1.26d. K101E, K101K/N, K103N, G190G/A (2)e. K65K/Rf. DTG (n=2): R263R/K FC=1.12 and R263K FC=1.93.
Supporting the Phase III finding in treatment-naïve subjects, in ING112276, no subjects receiving the Phase III selected dose of DTG 50 mg once daily had a confirmed PDVF (400 c/mL) through Week 96, and no virologic resistance was observed in this treatment group. A low rate of confirmed PDVF was observed in the DTG 10 mg and 25 mg

CONFIDENTIALModule 2.5 Clinical Overview
51
treatment groups and the EFV treatment group. No subjects demonstrated integrase ornon-nucleoside reverse transcriptase inhibitor (NNRTI) resistance at PDVF. The only demonstrated virologic resistance mutation was a single case of M184V, consistent with 3TC/FTC resistance, in a subject receiving TDF/FTC and DTG 10 mg once daily(m2.7.2.4).
4.6.5. ART-Experienced (INI-Resistant) Subjects
4.6.5.1. Demographics and Baseline Characteristics
Overall, in Studies ING112961 and ING112574 there was a good representation of female (23% to 25%) and African heritage (21% to 27%) subjects in the study population. There was no clinically meaningful difference between studies with respect to gender or age; median age was about 47 years.
Subjects enrolled in Studies ING112961 and ING112574 had advanced HIV-1 disease, were highly antiretroviral treatment experienced, with extensive multi-class viral drug resistance at Baseline (m2.7.3, Table 38). There was a good representation of all major integrase resistance pathways (m2.7.3, Table 40).
4.6.5.2. Key Efficacy Endpoints
The primary efficacy endpoint in ING112574 comprised the change from Baseline in plasma HIV-1 RNA at Day 8 and an assessment of the proportion of subjects with <50 c/mL HIV-1 RNA at Week 24. Assessing all subjects who had the opportunity to reach Week 24 before the data cut-off, 63% of this Week 24 ITT-E population (N=114) achieved viral suppression to <50 c/mL based on the Snapshot algorithm (Data Source: ING112574 Week 24 CSR Table 7.21). A comparable proportion (66/101, 65%) was observed in this analysis for the Per Protocol population (Data Source: ING112574 Week 24 CSR Table 7.4). Additionally, a significant mean reduction of 1.43 log10 c/mL HIV-1 RNA at Day 8 compared to Baseline was observed for the ITT-E population with an equivalent reduction observed for the Per Protocol population (Table 12).
The primary endpoint in ING112961 was the proportion of subjects with Day 11 plasma HIV-1 RNA <400 c/mL or reduced by at least 0.7 log10 c/mL compared to Baseline. Twenty-three of 24 (96%, CI: 79%, 100%) subjects in Cohort II (those receiving the 50 mg BID dose chosen to be carried into Phase III studies) achieved the primary endpoint (Data Source: ING112961 Cohort II Week 48 CSR Table 7.1).

CONFIDENTIALModule 2.5 Clinical Overview
52
Table 12 ING112574: Mean Change from Baseline in Plasma HIV-1 RNA log10c/mL at Day 8
(LOCFDB, ITT-E)
N Mean (SD) 95% CI p-value a
Baseline 183 4.26 (0.93)
Change from Baseline Day 8 182b -1.43 (0.61) (-1.52,-1.34) <0.001
(LOCFDB, Day 8 PP population)
N Mean (SD) 95% CI p-value a
Baseline 173 4.26 (0.93)
Change from Baseline Day 8 173 -1.43 (0.60) (-1.52,-1.34) <0.001Data Source: ING112574 Week 24 CSR Table 7.1 and Table 7.2a. p-value is derived by testing the hypothesis of no change from Baseline at the two-sided 5% significance level using Student's t-test. b. One subject at no Day 8 visitNote: Proportion of CFB 0.5 log10 c/mL or <400 c/mL at Day 8: 169/183 (92%).
There were similar increases in CD4+ cell counts over time across in these INI-resistant subjects in ING112961 and ING112574. The median change from Baseline to Week 24in CD4+ cells ranged from +65 to +79 cells/mm3 across both studies. At Week 48, the median change from Baseline in CD4 cells was 100 cells/mm3 in ING112961.
Across the INI-resistant subjects in ING112961 and ING112574, there was a similar low incidence of HIV-associated conditions (5% to 8% Data Source: ING112961 Cohort II Week 48 CSR, Section 6.5: ING112574 Week 24 CSR, Section 6.5). Little disease progression to CDC category C or death was observed in this salvage population, alignedwith the overall immune recovery (m2.7.3, Section 3.2.4.2, Table 55).
In ING112574, few subjects had non-Clade B virus [Clade A (n=1), AG (n=1), Complex(n=2), D (n=2), G (n=1)]. Nevertheless, all 7 subjects harboring non-B clade viruses experienced significant response to DTG, with a change from Baseline in plasma HIV-1 RNA at Day 8 ranging from -1.41 log10 c/mL to -2.30 log10 c/mL.
4.6.5.3. Treatment Emergent Resistance in INI-resistant Subjects
In Cohort II of ING112961, 5/24 (21%) subjects met the definition for PDVF (confirmed plasma HIV-1 RNA levels ≥400 c/mL on or after Week 16; full definition in ING112961 Cohort I Week 48/Cohort II Week 96 CSR, Section 4.5.1) through Week 24. No new PDVFs were identified through Week 48, except for one subject with unconfirmed suspected failure at Week 40 who withdrew from the study at Week 40 due to protocol violation (non-compliance to Investigational Product). Of the 5 subjects with PDVF, no subjects harboring viruses with the Y143 (n=1) or N155 (n=1) pathway at Baseline experienced PDVF with treatment-emergent resistance. The remaining 3 subjectsharboring virus with Q148 +1 additional IN resistance associated mutations at Baselinehad further evolution in integrase, resulting in a virus with Q148H + >3 additional INI associated resistance mutations; significant increases in DTG FC were observed for these three subjects. At Day 11 and Week 24, no novel mutations were identified (all have previously been described as RAL and/or EVG resistance-associated mutations).

CONFIDENTIALModule 2.5 Clinical Overview
53
In ING112574, the PDVF (confirmed plasma HIV-1 RNA levels ≥400 c/mL on or after Week 24; full definition in ING112574 Week 24 CSR, Section 4.9.6.6) rate through Week 24 (26/114, 23%) was similar to ING112961. For these 26 subjects, 16 (62%) had Q148 plus associated mutations detected in the Baseline IN genotype. Of the remaining 10 subjects, 2 subjects had N155H and 8 subjects did not have primary resistance detected at Baseline. Thirteen subjects (50%) had treatment-emergent IN resistance at the time point of virological failure. For 11/13 subjects with treatment-emergent IN resistance detected at PDVF, a mutation at Q148 (along with associated mutations) wasseen at Baseline or was present on historical testing. The only mutations that were identified have been previously described for the integrase class.
4.6.5.4. Comparison of Primary Efficacy Results in Sub-populations
Data were not pooled from ING112961 and ING112574. Very few subjects in ING112961 harbored virus with higher levels of resistance to DTG (n=3 in the Q148+2 group and n=0 for DTG FC 10). Therefore, pooling the studies would not add substantially to the ability of data from ING112574 to identify subgroups at risk of non-response.
In ING112574, multivariate analyses of factors impacting response indicated Baseline resistance to be the strongest predictor of response at both Day 8 and Week 24 (m2.7.3,Section 3.3.3.1). At Day 8, both Baseline DTG FC and pre-specified IN mutation category models fitted the Day 8 response equally well (m2.7.3, ING112574 Week 24 CSR, Section 6.2.1.2). However at Week 24 the lowest AIC value and best model fitness was determined for the pre-specified IN mutation categories model (m2.7.3, ING112574 Week 24 CSR, Section 6.3.2.2). This indicated that Baseline integrase genotypic resistance would be a better predictor of response to DTG than phenotypic DTG FC. In addition to these multivariate analyses, formal analyses of antiviral response by Baseline resistance (phenotypic or genotypic) to DTG was performed in an attempt to determine a clinical phenotypic cut-off and a genotypic guidance for use of DTG in INI-resistantadults individuals. These analyses are summarized below (m5.3.5.4 ING112574 Genotypic/Phenotypic Cut off Analysis Written Summary).
4.6.5.5. Antiviral Activity of DTG by Baseline Resistance in INI-resistant Subjects in ING112574
As per the FDA Guidance for Industry and the EMA guideline, analyses of antiviral activity of DTG observed in ING112574 were conducted according to genotypic and/or phenotypic resistance [FDA, 2007; EMA, 2009]. In this analysis, no precise phenotypic FC cut-off could be defined to effectively predict antiviral activity at both Day 8 and Week 24. Three integrase mutation groups could be derived and were found to correlate with antiviral response: ‘No Q148 mutation’ (Y143, N155H, T66, and E92Q mutations or historical evidence of INI resistance), ‘Q148+1’ (Q148H/K/R with one secondary mutation [G140A/C/S, L74I, E138A/K/T]), and ‘Q148+2’ (Q148H/K/R with two or three secondary mutations [G140A/C/S, L74I, E138A/K/T]).
More than 90% of subjects achieved full response (>1 log10 c/ml decline in HIV-1 RNA or <50 c/mL HIV-1 RNA) at Day 8 in the group of subjects with 155/143/66/no primary mutation detected. In subjects with Q148 mutations, virologic response at Day 8

CONFIDENTIALModule 2.5 Clinical Overview
54
decreased with increasing number of secondary mutations, however approximately half of subjects with Q148+2 secondary mutations still achieved full response at Day 8(Table 13).
Table 13 Virologic Response (Plasma HIV-1 RNA) at Day 8 by Derived Baseline IN Resistance Mutation Group (Day 8 Virologic Outcome Population, N=177)
INI Mutations at Baseline Number of Subjects
Mean CFB (SD)c at Day 8 % >1 log10 Decline or <50 c/mL at Day 8
No Q148H/K/R mutationsa 122 -1.59 (0.51) 92%Q148 + 1 secondary mutationb 35 -1.18 (0.52) 71%
Q148 + 2 secondary mutationsb 20 -0.92 (0.81) 45%
Data Source: m5.3.5.4 ING112574 Geno/Pheno Cut-Off Analyses for Annex B Table 12.106 and Table 12.110a. CFB: Change from Baseline; SD: Standard deviation.b. Includes Baseline primary IN resistance mutations N155H, Y143C/H/R, T66A, E92Q and primary mutation not
detected at Baseline.c. G140A/C/S, E138A/K/T, L74I.
After the monotherapy phase (i.e., Day 8 visit), subjects were able to optimize their background regimen, where possible; per protocol, subjects needed to have at least one fully active agent to combine with DTG 50mg BID. Of the 114 subjects who completed 24 weeks on study or discontinued before data cutoff, 72 (63%) had <50 c/mL RNA at Week 24 (Snapshot algorithm). In subjects with Q148 mutations, virologic response at Week 24 decreased with increasing number of secondary mutations. Background overall susceptibility score (OSS) was not associated with Week 24 response (Table 14), highlighting the independent activity of DTG in driving sustained virologic responses in this INI-resistant population.
Table 14 Number and % of Subjects with HIV-1 RNA <50 c/mL at Week 24 by OSS of OBR and Derived IN Resistance Mutation Group (Snapshot) (Week 24 Virologic Outcome Population, N=101)
Derived IN Mutation Group OSS=0 OSS=1 OSS=2 OSS>2 Total
No Q148H/K/R mutationsa 2/2 (100%) 24/29 (83%) 21/28 (75%) 10/13 (77%) 57 (79%)
Q148 + 1 secondary mutationb 2/2 (100%) 3/7 (43%) 4/11 (36%) - 9 (45%)
Q148 + 2 secondary mutationsb 1/2 (50%) 0/7 - - 1 (11%)
Data Source: ING112574 Geno/Pheno Cut-Off Analyses for Annex B Table 12.107a. Includes Baseline primary IN resistance mutations N155H, Y143C/H/R, T66A, and primary mutation not detected.b. G140A/C/S, E138A/K/T, L74I.
Although reduced virologic responses were observed, HIV-1 infected adults harboring viruses with Q148+ 2 secondary integrase inhibitor resistance mutations and/or high level of DTG FC in IC50, this subgroup of subjects with INI resistance is small. In the Screening population of ING112574, 26/269 (10%) of subjects harbored viruses with Q148+ 2 secondary integrase inhibitor resistance mutations (ING112574 Week 24 CSR, Table 96). In a separate analysis of approximately 700 unrelated clinical isolates with raltegravir resistance, viruses with Q148+ 2 secondary integrase inhibitor resistance mutations represented only 13% of the population and those with DTG FC >10

CONFIDENTIALModule 2.5 Clinical Overview
55
represented only 6% of the population (m2.7.2.4, Section 4.1.12.3.2). Additionally, evaluation of ~1000 RAL- resistant isolates from to demonstrated a decreasing proportion of Q148+≥2 pathway isolates over time (m2.7.2.4, Section 4.1.12.3.3). Therefore, it is anticipated that a minority of patients will harbor virus with Q148+2 and thus, DTG dosed at 50 mg twice daily will be efficacious in the majority of the viral population in INI-resistant patients.
4.7. Efficacy Conclusions
In treatment-naïve, HIV-infected adult subjects, DTG 50 mg once daily was shown to be an efficacious dose, and non-inferior to RAL in combination with a background regimen with dual NRTIs. When used in combination with ABC/3TC, DTG was shown to be superior to Atripla (EFV/TDF/FTC), a result driven by better tolerability of the DTG-based regimen.
In treatment-experienced, HIV-infected adult subjects naïve to INIs, DTG 50 mg once daily was shown to be efficacious, and was associated with a statistically greater response rate when compared to RAL in combination with up to a 2-drug, investigator-selected background regimen.
In treatment-experienced, INI-resistant adult subjects, DTG 50 mg twice daily was shown to have antiviral activity in short-term functional monotherapy in 2 studies (one Phase IIb and one Phase III) and was shown to be efficacious to 24 weeks in combination with investigator-selected optimized background regimen, despite the limited activity of available OBR. This supports the use of this dose in combination with other antiretroviral therapy in treatment-experienced, INI-resistant adults.
DTG 50 mg once daily has a higher barrier to resistance in INI-naive patients, as demonstrated in the treatment-experienced (INI-naive) study ING111762 where significantly fewer virologic failures and significantly fewer subjects with INI resistance were observed when compared with RAL. Data from two studies (ING113086 and ING114467) including over 1600 treatment-naive patients are also supportive of DTG’s higher barrier to resistance, given that no subjects on the DTG regimen developed resistance to either the INI or the background NRTIs, whereas resistance to both the third agent and the background NRTIs was observed in both the RAL and EFV-based comparator arms.
Increases in CD4+ cell counts were observed for subjects receiving DTG-containing regimens across all patient populations that were evaluated in the Phase II and III program. These CD4 cell count increases were similar in comparison with RAL in treatment-naïve and treatment-experienced subjects and were greater than those observed with EFV-containing regimens in treatment-naïve subjects.
There was no evidence of a diminished response to DTG in specific patient subgroups, such as gender, age (< or 50 years), race, level of immunosuppression (low CD4 cell counts or CDC Category C). However, there are limited data in INI-naïve subjects aged 65 (n=27).

CONFIDENTIALModule 2.5 Clinical Overview
56
As shown in in vitro studies, DTG was highly active with broad activity against all HIV-1 and HIV-2 isolates tested. No difference in virologic response by HIV-1 Clade (or isolate) was observed in a large, international Phase III study (ING111762) in treatment-experienced subjects. A limited number of non-B clade viruses were included in the other Phase III studies, but no differences in protocol-defined virologic failure were noted in subjects harboring non-B viruses in the treatment-naïve and INI-resistant studies.
5. OVERVIEW OF SAFETY
5.1. Introduction
Safety data supporting the use of DTG in the treatment of HIV infection has been collected from 30 Phase I, 4 Phase II, 7 Phase III/ IIIb clinical trials, as well as acompassionate use and an expanded access program. A full listing of individual studies and study descriptions are provided in m2.7.4, Sections 1.1.3 and 1.1.4.
Within this safety section, the study results are presented in the following groupings, and are also analyzed and presented in the same groupings within the Integrated Safety Summary (m5.3.5.3) and the Clinical Summary of Safety (m2.7.4):
Completed clinical pharmacology studies: includes Phase I studies in healthy adult volunteers and a Phase IIa study in ART-naïve HIV- infected adults (collective safety data are presented in Section 5.4).
Pediatric subjects (INI-naïve): ING112578 (P1093)
ART-naïve adult subjects: ING112276, ING113086, and ING114467
ART-experienced (INI-naïve) adult subjects: ING111762
ART-experienced (INI-resistant) adult subjects: ING112961 and ING112574
No additional safety issues have been identified in ongoing studies. Additional detail related to safety results of ongoing studies is presented in m2.7.4.
5.1.1. Data Cut-off Dates
For the majority of the Phase IIb and IIIa/b studies, the safety data cut-off occurred prior to the end of with the exception of ING111762 (data cut-off: ).Details of individual study cut-off dates are provided in m2.7.4, Section 1.1.2.
An additional cut-off date of for deaths, other SAEs, and pregnancies was applied to all ongoing studies for complete disclosure of safety information. These data were not integrated, but are reported separately as listings in m5.3.5.3 and are described under corresponding sections of the m2.7.4 as applicable.

CONFIDENTIALModule 2.5 Clinical Overview
57
5.2. Non-Clinical Data Relevant to Human Safety
The safety of DTG has been well characterized in a comprehensive battery of nonclinical studies (m2.4, Nonclinical Overview). The overall nonclinical safety data are supportive of the clinical use of DTG in the treatment of ART-naïve and ART-experienced (INI-naïve) adults, and in INI-naïve children 12 to <18 years at the recommended dose of 1mg/kg once daily. For ART-experienced adults with INI resistance, the recommended dose is 50 mg BID, also supported by the overall nonclinical safety data.
The effect of daily treatment with high doses of DTG has been evaluated in repeat oral dose toxicity studies in rats (up to 26 weeks) and in monkeys (up to 39 weeks). The primary effect of dolutegravir was gastrointestinal intolerance or irritation in rats and monkeys at doses that produce systemic exposures approximately 32 and 1.2 times the 50 mg human clinical exposure based on AUC, respectively. Because GI intolerance is considered to be due to local drug administration, mg/kg or mg/m2 metrics are appropriate determinates of safety cover for this toxicity. GI intolerance in monkeys occurred at 30 times the human mg/kg equivalent dose (based on 50 kg human), and 10.5 times the human mg/m2 equivalent dose for a total daily clinical dose of 50 mg.
The overall nonclinical reproductive and developmental toxicity profile for DTG in rats and rabbits suggests that DTG is not teratogenic and has a low potential for fetal risk.
DTG showed no genotoxic risk as assessed in a standard battery of in vitro and in vivogenotoxicity studies. An assessment of the route of synthesis showed no impurities, intermediates, solvents or other agents that may suggest a genotoxic risk. Overall, there is not believed to be a genotoxicity risk with DTG drug substance.
DTG has also shown no carcinogenic potential in two carcinogenicity studies (standard 2-year mouse and rat studies).
In summary, the toxic potential of DTG has been well characterized in a comprehensive nonclinical development program. These data are considered adequate to support the proposed clinical use as a treatment of HIV.
5.3. Exposure in the Clinical Development Program
See m2.7.4, Section 1.2 for full presentation of exposure data.
As of the analysis cut-off date, a total of 2663 subjects (2026 HIV-infected and 637 healthy) have been exposed to at least one dose of DTG in the entire clinical development program for this product. This total comprises:
526 healthy subjects and HIV-infected subjects from the Integrated Clinical Pharmacology Studies Analysis (Data Source: CPM Table 1)
1,571 HIV-infected subjects from the Phase IIb and Phase III studies (Data Source: ISO Table 2.501, Table 2.502, and Table 2.503)

CONFIDENTIALModule 2.5 Clinical Overview
58
139 adult healthy subjects from the five additional Phase I studies that were ongoing at data cut-off date for the Integrated Clinical Pharmacology Studies Analysis (i.e., ING113125, ING115697, ING115465, ING116915, and ING114580)
284 HIV-infected subjects who received at least one dose of DTG as part of ongoing Phase IIIb clinical trials (ING114915, ING116070 and ING116529), which were all fully enrolled by
110 HIV-infected adult subjects received DTG up to through the ongoing compassionate use program (ING115502 and ING114916), which is still enrolling patients
33 adolescents and children in the ongoing pediatric study ING112578 (P1093) have been exposed to DTG to the same data lock point; this study is also still enrolling patients.
5.4. Safety in Clinical Pharmacology Studies
Data is presented in this safety summary using three “dosing periods”, in which treatment is combined regardless of dose and duration: Placebo, DTG alone, and DTG with combination drug. As such, subjects who may have been exposed to both PBO and DTG could have AEs in both dosing periods.
5.4.1. Frequently Reported AEs
Overall there were relatively fewer AEs reported from the clinical pharmacology studies than the Phase IIb/III studies (m2.7.4, Section 5.6.2, Table 79). The most frequently reported AEs from healthy subjects receiving DTG in the clinical pharmacology studies were headache (n=75 [14%]), nausea (n=32 [6%]), dizziness (n=22 [4%]) and diarrhea (21 [4%]), which were similar to observations from the Phase IIb/III studies in HIV-infected adults (m2.7.4, Section 2.1.1.1.1 and Section 2.1.1.1.2).
While not frequent, reports of dizziness were observed in the DTG treatment groups and not for placebo. There were 11 subjects who experienced ocular icterus in the “all DTG” group. All 11 of these events were in the atazanavir drug interaction study (ING111854). None of the subjects experienced this event while on DTG alone. Of the most common AEs reported in at least 5% in any analysis group, only headache (14% vs. 3%) and nausea (6% vs. 3%) were reported more frequently in subjects dosed with DTG than those receiving placebo (m2.7.4, Section 5.6.2, Table 79).
5.4.2. Deaths
No deaths were reported in any of the completed clinical pharmacology studies.
5.4.3. Non-Fatal Serious Adverse Events
There were two SAEs reported from the clinical pharmacology studies (m2.7.4, Section 2.1.3.4). One subject had a manic episode which was considered unrelated to DTG in ING112941, and another subject in ING113099 had a suspected rifamycin

CONFIDENTIALModule 2.5 Clinical Overview
59
hypersensitivity syndrome while receiving rifabutin and DTG (event was considered related to study drugs).
5.4.4. Adverse Events Leading to Withdrawal
Based on the clinical pharmacology integrated analysis, there were 12 subjects (12/559, 2%) who had AEs that led to discontinuation of study drug. There were no safety trends noted leading to discontinuation across the clinical pharmacology studies.
Study ING113096 was the only study that had more than two subjects who withdrew due to an AE. This was a drug interaction study with tipranavir/ritonavir, and 4/18 subjects developed alanine aminotransferase (ALT) and aspartate aminotransferase (AST)elevations that resulted in the permanent discontinuation of investigational product and withdrawal from the study. These elevations occurred in subjects receiving TPV/RTV 500/200 mg or DTG 50 mg + TPV/RTV 500/200 mg. In all four subjects, the increase in ALT and AST began during dosing of TPV/RTV alone (Period 2), though 2 subjects were withdrawn after the ALT continued to increase early in Period 3 (DTG + TPV/RTV).
5.4.5. Clinical Laboratory Evaluations and Vital Signs
No trends were noted during the conduct of the Phase I/IIa studies to suggest DTG has a clinically significant effect on clinical chemistries (the exception of creatinine noted below), hematological parameters, or vital signs.
5.4.5.1. Hepatobiliary Adverse Events
No subject in the clinical pharmacology studies met criteria for drug induced liver injury (DILI) defined as ALT and/or AST >3 times ULN and total bilirubin >1.5 times the ULN.
Analysis of liver chemistries (Alkaline phosphatase, ALT, AST, total and direct bilirubin) demonstrated no pattern of difference from placebo subjects and those receiving DTG (alone or with other drugs), with the exception of increased rates of increased bilirubin seen in the DTG and atazanavir drug interaction study during ATV administration and increased rates of liver enzyme elevations in the DTG and TPV/RTV drug interaction study in subjects during TPV/RTV administration (see m2.7.4, Section 5.6.7).
5.4.5.2. Renal Adverse Events
A small, reversible increase in creatinine of approximately 0.11 mg/dL for subjects receiving DTG was observed; this was approximately a 10% increase (versus a zero increase in the placebo subjects). Occasional increases in both DTG and placebo subjectswere observed for trace proteinuria, with few subjects on DTG increasing one level (from trace to 1+). There were no AEs of renal disorders reported in the integrated analysis of safety in clinical pharmacology studies. Equivalent data from Phase IIb/III in HIV infected patients are presented, and the clinical implications are discussed, in Section 5.6.6.3.

CONFIDENTIALModule 2.5 Clinical Overview
60
Study ING114819 was a dedicated study to assess the effect of DTG on renal plasma flow and glomerular filtration rate (GFR). The results indicated that serum creatinineincreased, and hence, calculated creatinine clearance decreased in subjects receiving DTG 50 mg once daily and twice daily. DTG at 50 mg once daily and 50 mg BID had no significant effect on GFR compared to placebo over 14 days based on iohexol clearance. In addition, neither treatment significantly changed para-aminohippurate (PAH) clearance clearance (See m2.7.2 Section 2.1.5.3 for details).
5.4.6. Cardiac Evaluation
In study ING111856, a single supra-therapeutic dose of DTG (250 mg) had no significant effect on cardiac repolarization in a population of 42 healthy subjects, when compared to moxifloxacin (400 mg; active control) or placebo. In this study, with demonstrated ability to detect small effects, the upper bound of the two-sided 90% confidence interval for the largest placebo adjusted, baseline-corrected QTcF was below 10 ms, the threshold for regulatory concern. Since the study had adequate sensitivity to detect a positive QT effect with moxifloxacin, it is concluded that this study was valid (See m2.7.4Section 2.1.5.6.3 for details).
More generally in the 26 completed clinical pharmacology studies, there were only singular reports of arrhythmia and supraventricular tachycardia in the subjects receiving DTG alone. No significant ECG findings were reported. No syncope was reported.
5.5. Safety in Pediatrics - ING112578 (P1093)
Limited safety data are available from an ongoing study in the pediatric population and are described herein from 10 adolescent (12 to <18 years of age) subjects receiving at least 24 weeks of DTG once daily in combination with an investigator-selected, optimized background regimen in ING112578. Nine of 10 subjects in the pediatric population received a DTG 50 mg once daily dose, and 1 pediatric subject, weighing <40 kg, received DTG 35 mg once daily (~1 mg/kg dosing).
Nine of 10 subjects reported a clinical AE; the AEs reported in more than 1 subject included cough, lymphadenopathy, and sinus congestion. All AEs were reported as Grade 1 or 2 (mild or moderate) in intensity. No AEs were deemed related to study drug by the reporting investigators. No deaths, non-fatal SAEs, or withdrawals due to AEs have been reported to date in this ongoing pediatric study. Adverse events of special interest for the DTG development program (as defined in m2.7.4 Section 2.1.5), were rarely reported from this cohort of subjects, with only single episodes of rash, diarrhea and nausea reported.
Clinical chemistry abnormalities were reported by 9/10 (90%) subjects. Minimal absolute changes from Baseline were observed; none were serious, deemed clinically significant, or considered related to DTG by the investigator. No hematology abnormalities were reported.
No subjects met liver stopping criteria, nor did any subjects have ALT elevations 3X ULN. One Grade 3 asymptomatic elevated lipase was reported at Day 344 (Week 48) which was not considered related to DTG. One subject had a Grade 1 increase in CPK.

CONFIDENTIALModule 2.5 Clinical Overview
61
Similar to observations in adult subjects, adolescent subjects had small increases in creatinine that appeared at Week 2 and remained stable to Week 24, when an increase in the mean, but not the range, was observed. Only 1 subject had a treatment-emergent change in urine dipstick protein analysis, with trace amounts present at Week 24 (with negative protein at Baseline).
No clinically significant changes in diastolic or systolic blood pressure, respiratory or pulse rates, or temperature were noted.
5.6. Safety in Phase II and III Studies
5.6.1. Safety Population for Phase II and III Studies
The Safety population used for the safety analyses consists of all subjects who received at least one dose of investigational product. This population is described in m2.7.4, Section 1.1.4.
For the pivotal studies, 2557 subjects are included: 1182 subjects received DTG once daily, 183 subjects received DTG twice daily and 1192 subjects received comparator drug.
A total of 980 subjects in the ART-naïve population (ING112276, ING113086, and ING114467) and 357 subjects in the adult ART-experienced (INI-naïve) population (ING111762) received a DTG-containing regimen (DTG once daily, DTG 50 mg once daily + ABC/3TC). The majority of these subjects were still ongoing at the time of this analysis (87%). In the Phase III studies, patient populations with a broad set of Baseline characteristics were enrolled as follows:
In ING113086, 822 HIV-1 infected, ART-naïve adults were randomized and received at least one dose of either DTG 50 mg once daily or RAL 400 mg twice daily. At Baseline, median patient age was 36 years, 14% were female, 15% non-white, 12% had hepatitis B and/or C co-infection and <1% were CDC Class C, these characteristics were similar between treatment groups.

CONFIDENTIALModule 2.5 Clinical Overview
62
In ING114467, 833 HIV-1 infected, ART-naive adults were randomized and received at least one dose of DTG 50 mg once daily + ABC/3TC or EFV/TDF/FTC. At Baseline, median patient age was 35 years, 16% were female, 32% non-white, 7% had hepatitis C co-infection and 4% were CDC Class C, these characteristics were similar between treatment groups.
In ING111762, 724 HIV-1 infected, ART-experienced (INI-naïve) adults were randomized to receive either DTG 50 mg once daily or RAL 400 mg twice daily. At Baseline, median age was 43 years, 32% were female, 51% non-white, 17% had hepatitis B and/or C co-infection and 44% were CDC Class C.
A total of 234 ART-experienced (INI-resistant) subjects from ING112961 and ING112574 received a DTG-containing regimen (DTG 50 mg once daily or DTG 50 mg twice daily). Eighty-three percent of subjects were still ongoing at the time of this analysis.
In ING112574, 183 subjects enrolled. At Baseline, median age was 48 years, 23% were female, 29% non-white, and 20% had hepatitis B and/or C co-infection. Median Baseline CD4 cell count was 140 cells/mm3, median duration of prior ART was 13 years, and 56% were CDC Class C.
5.6.2. Common Adverse Events
For ART-naïve and ART-experienced (INI-naïve) patients, the safety profile for DTG 50 mg once daily was comparable to RAL and generally favorable to Atripla and EFV. The most frequently observed AEs across patient populations were diarrhea, nausea, and headache, which were typically Grade 1 or 2 in severity, and typically did not lead to discontinuation from studies. Gastrointestinal (GI) tolerability was comparable to RAL-and EFV-containing regimens. Few cases of hypersensitivity reaction and/or severe rash were seen, and the rates of these events were comparable to or lower than RAL- and EFV-containing regimens, respectively. No subjects were reported to have the most serious forms of rash, such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), or erythema multiforme (EM). The incidence of mild to moderate skin reactions with DTG were comparable to or lower than observed with RAL- or EFV-containing regimens, respectively. Finally, psychiatric and nervous system disorders with DTG were comparable to RAL and favorable to both Atripla and EFV, in terms of reporting rates, nature and severity. Overall, the AE profile was generally similar to RAL and improved when compared with an EFV-containing regimen.
Treatment-experienced (INI-resistant) subjects were treated with DTG 50 mg twice daily to ensure durable efficacy in subjects with baseline DTG resistance. As a group, this population had more advanced HIV disease and received more concomitant ART. Nevertheless, the AE profile was similar to that reported for treatment-naïve and treatment-experienced (INI-naïve) subjects receiving DTG 50 mg once daily.
5.6.2.1. Frequently Reported Adverse Events
Details of frequently reported AEs are provided in m2.7.4, Section 2.1.1.

CONFIDENTIALModule 2.5 Clinical Overview
63
5.6.2.1.1. ART-Naïve Adult Subjects
Diarrhea, nasopharyngitis, nausea, headache, and fatigue were the most commonly reported clinical AEs and occurred at similar rates across the treatment groups (see ISO Table 2.17 for a full listing of AEs). Insomnia was observed at a significantly higher frequency with DTG in ING114467. However, the incidence was lower than EFV in ING112276 and similar to RAL in ING113086. In ING114467, insomnia events were generally mild in intensity, with only one subject discontinuing on the DTG+ABC/3TC arm (vs. two subjects discontinuing on the EFV/TDF/FTC arm). Data on insomnia are further described in m2.7.4, Section 2.1.5.8.2. AE rates between DTG and RAL were generally similar, and AEs such as dizziness, rash, and abnormal dreams occurred at higher frequencies in the EFV and/or Atripla treatment groups. The majority of events reported in DTG and comparator groups were considered Grade 1 or Grade 2 in intensity, with few Grade 3 or Grade 4 AEs reported.
Table 15 Summary of Common Adverse Events by Frequency (in at Least 5%of Subjects in the Combined DTG Group) – ART-Naïve Population
Preferred term ING112276 ING113086 ING114467 TOTAL DTGonce daily
N=980
DTGonce daily
+ 2 NRTI
N=155
EFV 600 mg
once daily
+ 2 NRTIN=50
DTG 50 mg
once daily+ 2 NRTI
N=411
RAL 400 mg BID
+ 2 NRTI
N=411
DTG 50 mg + ABC/3TC once daily
N=414
EFV/TDF/FTC once daily
N=419
n (%)a n (%)a n (%)a n (%)a n (%)a n (%)a n (%)a
Any event 142 (92) 46 (92) 343 (83) 346 (84) 369 (89) 387 (92) 854 (87)Diarrhea 25 (16) 7 (14) 49 (12) 51 (12) 72 (17) 75 (18) 146 (15)Nausea 23 (15) 7 (14) 60 (15) 54 (13) 59 (14) 57 (14) 142 (14)Nasopharyngitis 22 (14) 5 (10) 53 (13) 54 (13) 62 (15) 60 (14) 137 (14)Headache 22 (14) 3 (6) 53 (13) 49 (12) 55 (13) 56 (13) 130 (13)Insomnia 13 (8) 6 (12) 22 (5) 18 (4) 64 (15) 43 (10) 99 (10)Fatigue 7 (5) 6 (12) 20 (5) 19 (5) 54 (13) 50 (12) 81 (8)Upper respiratory tract infection
11 (7) 1 (2) 29 (7) 26 (6) 36 (9) 43 (10) 76 (8)
Dizziness 8 (5) 11 (22) 23 (6) 24 (6) 37 (9) 148 (35) 68 (7)Cough 15 (10) 2 (4) 20 (5) 18 (4) 24 (6) 29 (7) 59 (6)Depression 11 (7) 6 (12) 21 (5) 18 (4) 23 (6) 26 (6) 55 (6)Pyrexia 11 (7) 4 (8) 21 (5) 22 (5) 23 (6) 22 (5) 55 (6)Abnormal dreams
3 (2) 4 (8) 12 (3) 8 (2) 30 (7) 72 (17) 45 (5)
Bronchitis 9 (6) 5 (10) 22 (5) 18 (4) 20 (5) 15 (4) 51 (5)Back pain 7 (5) 4 (8) 16 (4) 20 (5) 23 (6) 17 (4) 46 (5)a. Number and percent of subjects with adverse event.Data Source: ISO Table 2.17

CONFIDENTIALModule 2.5 Clinical Overview
64
5.6.2.1.2. ART-Experienced (INI-Naïve) Adult Subjects
The most commonly reported individual AEs among subjects receiving DTG were diarrhea, upper respiratory tract infection, headache, nausea and cough, with no appreciable difference between treatment groups (m2.7.4, Table 18). Overall, individual AE rates between DTG and RAL were generally similar.
Table 16 Summary of Common Adverse Events by Frequency (in at least 5% of Subjects in any Treatment Group– ART-Experienced, INI-Naïve Population
Preferred term DTG 50 mg once daily + BR
N=357n (%)a
RAL 400 mg BID + BR
N=362n (%)a
Any event 265 (74) 281 (78)Diarrhea 72 (20) 62 (17)Upper respiratory tract infection 38 (11) 29 (8)Headache 31 (9) 29 (8)Nausea 26 (7) 28 (8)Cough 29 (8) 23 (6)Urinary tract infection 26 (7) 18 (5)Influenza 21 (6) 21 (6)Nasopharyngitis 21 (6) 18 (5)Fatigue 15 (4) 23 (6)Vomiting 17 (5) 20 (6)Rash 18 (5) 17 (5)Data Source: ISO Table 2.524a. Number and percent of subjects with adverse event.
5.6.2.1.3. ART-Experienced (INI-Resistant) Adult Subjects
The most commonly reported individual AEs were diarrhea, bronchitis, nausea, headache and pyrexia (Table 17). Diarrhea, nausea, and headache are further described under m2.7.4, Section 2.1.5.5.3 and Section 2.1.5.7.3. The majority of events reported were considered Grade 1 or Grade 2 in intensity, with few Grade 3 or Grade 4 AEs. In the ART-experienced, (INI-resistant) studies, more Grade 3 events were reported (m2.7.4, Section 2.1.1.1.3), but this patient population had more advanced HIV (m2.7.4, Section 1.3.2.2.3) and a wide variety of concomitant antiretrovirals and other concomitant medications, which likely contributed to this finding.

CONFIDENTIALModule 2.5 Clinical Overview
65
Table 17 Summary of Common Adverse Events by Frequency (in at Least 5% of Subjects in the Combined DTG Group) – INI-Resistant Population
Preferred term ING112961 ING112574 TOTAL
Cohort IDTG 50 mg once daily
N=27a
Cohort IIDTG 50 mg BID
N=24a
DTG 50 mg BID
N=183a
DTG BID
N=207a
Any event 26 (96) 23 (96) 147 (80) 170 (82)Diarrhea 5 (19) 9 (38) 25 (14) 34 (16)Bronchitis 4 (15) 6 (25) 13 (7) 19 (9)Headache 4 (15) 2 (8) 16 (9) 18 (9)Pyrexia 4 (15) 5 (21) 13 (7) 18 (9)Nausea 2 (7) 2 (8) 17 (9) 19 (9)Cough 3 (11) 4 (17) 13 (7) 17 (8)Fatigue 1 (4) 4 (17) 12 (7) 16 (8)Insomnia 5 (19) 1 (4) 9 (5) 10 (5)Nasopharyngitis 2 (7) 1 (4) 10 (5) 11 (5)Asthenia 5 (19) 2 (8) 5 (3) 7 (3)Injection site reaction 1 (4) 2 (8) 9 (5) 11 (5)Upper respiratory tract infection 1 (4) 2 (8) 9 (5) 11 (5)Rash 0 1 (4) 10 (5) 11 (5)a. Number and percent of subjects with adverse event.Data Source: ISO Table 2.18
5.6.2.2. Labeling and Adverse Drug Reactions
Adverse reactions listed in the Company Reference Safety Information (RSI) and LocalCountry Labeling include events that have been assessed as being at least possibly causally related to dolutegravir.
Sponsor causality was by evaluation of the frequency and severity of AEs that were considered by investigators to be related to DTG treatment. Study investigators were obligated to assess the relationship between investigational product (IP) and the occurrence of each AE/SAE. A ‘reasonable possibility’ of relatedness to IP is meant to convey that there are facts/evidence or arguments to suggest a causal relationship, rather than a relationship cannot be ruled out. The investigator was instructed to use clinical judgment to determine the relationship. Alternative causes, such as natural history of the underlying diseases, concomitant therapy, other risk factors, and the temporal relationship of the event to the investigational product were to be considered and investigated. The investigator is also instructed to consult the Investigator Brochure (IB) and/or Product Information (for marketed products, which may be comparators or included in a treatment regimen) in the determination of his/her assessment. For the company RSI, and where it is required in Local Country Labeling that adverse events are presented by System Organ Class and frequency, adverse events judged by the investigator to be reasonably attributable to DTG, with a frequency of at least 1% in the combined database of all DTG subjects (n=1571), were selected for inclusion in the label and are presented below (Table 18).

CONFIDENTIALModule 2.5 Clinical Overview
66
Table 18 Drug Related Adverse events with a frequency of 1% in Integrated Safety Database
Preferred term Total DTGN=1571n (%)
Any event 508 (32)Nausea 124 (8)Diarrhea 93 (6)Headache 68 (4)Dizziness 48 (3)Insomnia 54 (3)Fatigue 43 (3)Abnormal dreams 37 (2)Vomiting 32 (2)Flatulence 22 (1)Abdominal pain upper 18 (1)Rash 22 (1)Pruritus 19 (1)Data Source: ISO Table 2.511
Events that occurred below the 1% threshold but where there was a reasonable possibility of causal relationship to DTG treatment, including events that were indicative of typical severe drug-induced adverse reactions (e.g., Hypersensitivity, hepatitis) were considered for inclusion, independent of the incidence. Hypersensitivity and hepatitis were considered possibly related and added to the Company RSI/Local Country Labeling. Those events (e.g., abdominal pain and discomfort) related to an event of higher frequency (e.g., upper abdominal pain) were also selected for inclusion.
Class label statements such as immune reconstitution syndrome were also included.
The frequency categories of events for the label were derived from the frequency of all adverse events in the total DTG population (regardless of causality; Data Source: ISO Table 2.508), not just the frequency of events considered to be at least possibly related by the investigator (Table 18). These categories are defined according to MedDRA convention, as follows:
Very common: 1/10Common: 1/100 to <1/10Uncommon: 1/1000 to <1/100.
Where adverse events are to be presented as a subset of data from clinical trials (e.g. US Prescribing Information), events for inclusion were assessed by evaluation of the frequency and severity of each AE considered by investigators to be related to DTG in the four pivotal Phase III clinical trials. A cut-off was applied to Grade 2 to 4 events with a frequency of 2% of subjects in any treatment arm within these four studies.
Laboratory abnormalities with a worsening grade from baseline in 2% (for Grades 3 to 4 combined) were provided where required.

CONFIDENTIALModule 2.5 Clinical Overview
67
5.6.2.3. Supportive PK/PD Safety Analyses
A summary of the exposure response relationship for safety endpoints from the treatment-naïve and treatment-experienced populations is provided in m2.7.2, Section 3.4.4. No association was observed between DTG exposure and the most frequently reported AEs or specific lab abnormalities (e.g., ALT). However, correlations between DTG C0 and change from Baseline in total bilirubin and serum creatinine were observed, which were likely due to competition between DTG and unconjugated bilirubin for UGT1A1 and an expected effect of DTG due to inhibition of OCT2, respectively.
5.6.3. Deaths
A complete discussion concerning deaths in the dolutegravir clinical development program can be found in m2.7.4, Section 2.1.2.
As of the submission cut-off date, there were 16 deaths reported across the DTG clinical studies and compassionate use program. Six deaths were reported in the pivotal and supporting clinical trials investigating the ART-naïve population (3 on DTG50 mg once daily, 1 on RAL and 2 on Atripla) and two in the ART-experienced (INI naïve) population (both on RAL). Four deaths (2 receiving DTG 50 mg once daily and 2 receiving DTG 50 mg BID) were reported in the pivotal and supporting clinical trials investigating the ART-experienced (INI-resistant) population. Four deaths were reported in other ongoing studies (ING116529) and the compassionate use program (ING115502) in subjects receiving DTG 50 mg BID.
None of the deaths on DTG were considered related to study drug. Deaths were generally due to comorbidities seen in HIV-infected patients.
5.6.4. Serious Adverse Events
No trends in SAEs were noted across the patient populations assessed in the clinical program. The only SAEs reported consistently across the clinical program were pneumonia and suicidal ideation or attempt, but these events were reported in both DTG and comparator treatments and are more frequently observed in HIV-infected patients than in the general population. Suicide is discussed further in m2.7.4 Section 2.1.5.8 [Jia, 2012]. The definition of a Serious Adverse Event and details of the reported SAEs are provided in m2.7.4, Section 2.1.3.
5.6.4.1. ART-Naïve Adult Subjects
The rate of subjects developing at least one SAE at the time of data cut-off for this analysis was low and similar between treatment groups (Table 19).
With the exception of suicide attempt, depression, and neurosyphilis in the EFV group (which were reported in 1 subject each in ING112276), all other individually reported SAE preferred terms had a reporting rate of <1% across all treatment groups.

CONFIDENTIALModule 2.5 Clinical Overview
68
Table 19 Summary of Serious Adverse Events in at Least Two Subjects in the Combined DTG Group – ART-Naive Population
Preferred term ING112276 ING113086 ING114467 TOTAL DTGonce daily
N=980
DTGonce
daily + 2 NRTI
N=155
EFV 600 mg
once daily + 2
NRTIN=50
DTG 50 mg
once daily+ 2 NRTI
N=411
RAL 400 mg
BID + 2 NRTI
N=411
DTG 50 mg + ABC/3TC once daily
N=414
EFV/TDF/FTC once daily
N=419Any event 16 (10) 7 (14) 33 (8) 36 (9) 37 (9) 35 (8) 86 (9)Suicide attempt 0 1 (2) 2 (<1) 3 (<1) 2 (<1) 1 (<1) 4 (<1)Drug hypersensitivity 0 0 3 (<1) 0 1 (<1) 0 4 (<1)Pneumonia 1 (<1) 0 0 2 (<1) 2 (<1) 2 (<1) 3 (<1)Appendicitis 0 0 1 (<1) 3 (<1) 1 (<1) 0 2 (<1)Neurosyphilis 0 1 (2) 1 (<1) 0 1 (<1) 0 2 (<1)Syphilis 0 0 0 0 2 (<1) 0 2 (<1)Foot fracture 1 (<1) 0 0 0 1 (<1) 1 (<1) 2 (<1)Intentional overdose 0 0 0 1 (<1) 2 (<1) 0 2 (<1)Humerus fracture 1 (<1) 0 0 0 1 (<1) 0 2 (<1)Road traffic accident 1 (<1) 0 0 0 1 (<1) 0 2 (<1)Pyrexia 1 (<1) 0 0 1 (<1) 1 (<1) 0 2 (<1)Osteoarthritis 0 0 1 (<1) 0 1 (<1) 0 2 (<1)Data Source: ISO Table 2.39
Few SAEs were considered reasonably attributable to IP by reporting investigators across treatment groups, with no emerging trends apparent for DTG from these data.
5.6.4.2. ART-Experienced (INI-Naïve) Adult Subjects
No patterns were observed as all SAEs were reported in 1% of subjects in each treatment group (Table 20).
Table 20 Summary of Serious Adverse Events in at least Two Subjects in any treatment group – ART-Experienced, INI- Naïve Population
Preferred term DTG 50 mg once daily + BR
N=357n (%)
RAL 400 mg BID + BR
N=362n (%)
Any event 28 (8) 41 (11)Pneumonia 2 (<1) 4 (1)Post operative wound 0 2 (<1)Suicidal ideation 3 (<1) 1 (<1)Alcohol withdrawal syndrome 2 (<1) 0Depression 2 (<1) 0Pancreatitis 2 (<1) 1 (<1)Anemia 0 2 (<1)Dehydration 0 2 (<1)Cerebrovascular accident 0 2 (<1)Data Source: ING111762 Week 24 CSR Table 8.13

CONFIDENTIALModule 2.5 Clinical Overview
69
5.6.4.3. ART-experienced (INI-Resistant) Adult Subjects
The reporting rate of subjects developing at least one SAE at the time of data cut-off for this analysis was low for this treatment population with advanced HIV disease(Table 21).
Table 21 Summary of Serious Adverse Events in at least Two Subjects in the Combined DTG Group – INI-Resistant Population
Preferred term ING112961 ING112574 TOTALCohort I
DTG 50 mg once daily
N=27
Cohort IIDTG 50 mg BID
N=24
DTG 50 mg BID
N=183
DTG BID
N=207Any event 6 (22) 8 (33) 27 (15) 35 (17)Pneumonia 0 0 4 (2) 4 (2)Gastroenteritis viral 0 1 (4) 1 (<1) 2 (<1)Progressive multifocal leukoencephalopathy 0 0 2 (1) 2 (<1)Pyrexia 0 0 2 (1) 2 (<1)Dehydration 0 0 2 (1) 2 (<1)Pleural effusion 0 0 2 (1) 2 (<1)Coronary artery disease 0 2 (8) 0 2 (<1)Data Source: ISO Table 2.40
The most frequent individually reported SAE is pneumonia, otherwise all other SAEs had a reporting rate of <1% across the two studies.
5.6.5. Adverse Events Leading to Withdrawal
Few subjects receiving DTG developed AEs resulting in the permanent discontinuation of IP and withdrawal from the study. There were no discernible trends for AEs leading to withdrawal for the DTG or comparator treatment groups, as most of these events were isolated cases in individual studies. However, withdrawals due to liver stopping criteria were noted on DTG and comparator arms across the Phase IIb and III studies. For the various study treatment populations, these events were frequently confounded by concomitant medications, co-infection with hepatitis B or C virus, concomitant alcohol or drug misuse, or a combination thereof.
Details of AEs leading to withdrawal are provided in m2.7.4, Section 2.1.4.1.
5.6.5.1. ART-Naïve Adult Subjects
AEs leading to permanent discontinuation of IP and withdrawal from the study were more commonly reported for the Atripla and EFV treatment groups, compared to DTG and similar between the DTG and RAL treatment groups.
Subjects in Atripla and EFV treatment groups more frequently developed psychiatric disorders resulting in withdrawal, and subjects receiving Atripla more frequently developed nervous system disorders resulting in withdrawal, compared to other treatment groups.

CONFIDENTIALModule 2.5 Clinical Overview
70
Table 22 Summary of Adverse Events Leading to Withdrawal/Permanent Discontinuation of Investigational Product by System Organ Class –ART-Naïve Population
System organ class ING112276 ING113086 ING114467Preferred term DTG
once daily + 2 NRTI
N=155
EFV 600 mg
once daily+ 2 NRTIN=50
DTG 50 mg Once
Daily + 2 NRTIN=411
RAL400 mg BID + 2 NRTI
N=411
DTG 50 mg +
ABC/3TC Once Daily
N=414
EFV/TDF/FTC Once Daily
N=419
TOTAL DTGonce daily
N=980Any event 4 (3) 5 (10) 10 (2) 9 (2) 10 (2) 42 (10) 24 (2)Skin and subcutaneous tissue disorders
1 (<1) 0 1 (<1) 1 (<1) 2 (<1) 8 (2) 4 (<1)
Psychiatric disorders 0 3 (6) 1 (<1) 2 (<1) 2 (<1) 15 (4) 3 (<1)Immune system disorders 0 1 (2) 1 (<1) 1 (<1) 2 (<1) 3 (<1) 3 (<1)Infections and infestations 0 0 2 (<1) 3 (<1) 1 (<1) 2 (<1) 3 (<1)Injury, poisoning and procedural complications
1 (<1) 0 0 1 (<1) 2 (<1) 0 3 (<1)
Gastrointestinal disorders 1 (<1) 0 1 (<1) 2 (<1) 0 8 (2) 2 (<1)Investigations 0 0 2 (<1) 2 (<1) 0 1 (<1) 2 (<1)Nervous system disorders 0 0 1 (<1) 1 (<1) 0 13 (3) 1 (<1)General disorders and administration site conditions
0 2 (4) 1 (<1) 0 0 7 (2) 1 (<1)
Renal and urinary disorders 0 0 0 0 1 (<1) 2 (<1) 1 (<1)Hepatobiliary disorders 0 0 1 (<1) 1 (<1) 0 0 1 (<1)Neoplasms benign, malignant and unspecified (incl cysts and polyps)
1 (<1) 0 0 0 0 1 (<1) 1 (<1)
Cardiac disorders 0 0 1 (<1) 0 0 0 1 (<1)Social circumstances 0 0 1 (<1) 0 0 0 1 (<1)Metabolism and nutrition disorders
0 0 0 0 0 2 (<1) 0
Musculoskeletal and connective tissue disorders
0 0 0 1 (<1) 0 1 (<1) 0
Respiratory, thoracic and mediastinal disorders
0 0 0 0 0 2 (<1) 0
Blood and lymphatic system disorders
0 0 0 1 (<1) 0 2 (<1) 0
Ear and labyrinth disorders 0 0 0 0 0 3 (<1) 0Data Source: ISO Table 2.43
With the exception of suicide attempt, neurosyphilis and depression in the ING112276EFV group, all other individually reported AE preferred terms resulting in withdrawal had a reporting rate of <1% across all treatment groups.
5.6.5.2. ART-Experienced (INI-Naïve) Adult Subjects
There were few AEs leading to discontinuation of investigational product in either group and there were no discernible patterns of events (Table 23).

CONFIDENTIALModule 2.5 Clinical Overview
71
Table 23 Summary of Adverse Events Leading to Withdrawal/Permanent Discontinuation of Investigational Product by System Organ Class –ART-Experienced (INI- Naïve) Population
System organ class DTG 50 mg Once Daily + BR
N=357n (%)
RAL 400 mg BID + BR
N=362n (%)
Any event 6 (2) 13 (4)Hepatobiliary disorders 2 (<1) 3 (<1)Infections and infestations 1 (<1) 4 (1)Gastrointestinal disorders 0 4 (1)Neoplasms benign, malignant and unspecified (including cysts and polyps) 0 3 (<1)Renal and urinary disorders 2 (<1) 1 (<1)Investigations 1 (<1) 1 (<1)Blood and lymphatic system disorders 0 1 (<1)Immune system disorders 1 (<1) 0Metabolism and nutrition disorders 0 1 (<1)Musculoskeletal and connective tissue disorders 1 (<1) 0Psychiatric disorders 0 1 (<1)Respiratory, thoracic and mediastinal disorders 0 1 (<1)Skin and subcutaneous tissue disorders 0 1 (<1)Data Source: ING111762 Week 24 CSR Table 8.15
5.6.5.3. ART-Experienced (INI-Resistant) Adult Subjects
Few subjects developed AEs resulting in the permanent discontinuation of IP and withdrawal from the study. All individually reported AEs resulting in the permanent discontinuation of IP and withdrawal from the study had a rate of <1%.
Table 24 Summary of Adverse Events Leading to Withdrawal/Permanent Discontinuation of Investigational Product in at least Two Subjects in any Treatment Group – ART-Experienced (INI-Resistant)Population
System organ class ING112961 ING112574 TOTALDTG 50 mg
BID
N=207
Preferred term Cohort IDTG 50 mg
Once Daily + BRN=27
Cohort IIDTG 50 mg BID + BR
N=24
DTG 50 mg BID + BR
N=183Any event 2 (7) 2 (8) 5 (3) 7 (3)Investigations 0 0 2 (1) 2 (<1)Skin and subcutaneous tissue disorders 0 0 2 (1) 2 (<1)Blood and lymphatic system disorders 1 (4) 1 (4) 0 1 (<1)Nervous system disorders 1 (4) 0 1 (<1) 1 (<1)Hepatobiliary disorders 0 0 1 (<1) 1 (<1)Metabolism and nutrition disorders 0 1 (4) 0 1 (<1)Psychiatric disorders 0 1 (4) 0 1 (<1)Data Source: ISO Table 2.44

CONFIDENTIALModule 2.5 Clinical Overview
72
5.6.6. AEs of Special Interest
The AEs of Special Interest (AESI) have been determined for DTG based on pre-clinical and/or clinical safety data for DTG, labeling and/or regulatory authority interest for approved integrase inhibitors and/or the INI class, and/or regulatory authority requirements. Details on the AEs of Special Interest section are included in m2.7.4, Section 2.1.5.
5.6.6.1. Hypersensitivity and Rash
Severe, potentially life-threatening, and fatal skin reactions, including cases of SJS and TEN, and hypersensitivity reactions are listed events in the Local Country Prescribing Information for the first marketed INI, RAL [Isentress US Package Insert, revised April 2012, Isentress EU Summary of Product Characteristics, 2012].
The ABC (600 mg)/3TC (300 mg) once daily FDC tablet was used in all of the three supportive/pivotal Phase IIb/III clinical trials in ART-naïve subjects, either as: randomized study medication (ING114467) or investigator-selected dual NRTI backbone (ING112276 and ING113086). The most important risk associated with the ABC component of the FDC is a well characterized drug-related hypersensitivity reaction (HSR), which is generally manageable. HLA-B*5701 has been shown to be highly associated with ABC HSR, and the practice of pre-therapy screening for and exclusion of patients with HLA-B*5701 reduces the risk of HSR [EPZICOM US Prescribing Information, 2012; KIVEXA EU Summary of Product Characteristics, 2011]. Thus, screening for and exclusion of subjects with HLA-B*5701 was required for all subjects in the DTG program who received (or had the potential to receive due to blinding) ABC-containing products.
Drug hypersensitivity is about 100 times more common in HIV-1-infected patients than in the general population [Carr, 2000] and skin rash is associated with many antiretrovirals [NIA, 2012].
In the DTG clinical program, reporting rates for “Rash” of any grade were low for DTG,comparable with RAL, and lower than observed for EFV/Atripla. Cases of HSR and/or severe skin reactions with or without systemic involvement were rarely seen for DTG. Reporting rates were comparable to RAL and less than observed for EFV/Atripla. Cases reported for DTG and RAL were generally confounded by co-suspect medications thatwere considered to have contributed to the event. With the exception of the Atripla treatment group in ING114467, rash or hypersensitivity events leading to discontinuation of IP and withdrawal of subjects from study have been infrequent.
No episodes of serious rash such as SJS, TEN or erythema multiforme have been reported for the DTG development program to date.
There is no evidence for increased risk of rash with or without systemic symptoms with either DTG 50 mg once daily in INI-naïve subjects or DTG 50 mg twice daily in INI-resistant subjects. Due to identification of a case of HSR with organ dysfunction in a treatment-naïve subject in ING113086 and additional confounded cases identified in treatment-experienced subjects, labeling for DTG is proposed to reflect a warning about

CONFIDENTIALModule 2.5 Clinical Overview
73
hypersensitivity reactions, including monitoring for liver enzymes if HSR is observed for a patient on DTG.
5.6.6.2. Hepatobiliary Disorders
Non-clinical data suggested a possible, albeit low, risk for hepatobiliary toxicity with DTG. Due to comorbidities (e.g., hepatitis B and C co-infection) and co-administered medications (e.g., antiretrovirals) in HIV-infected patients, it is recommended to monitorliver chemistries in the clinical setting; hepatitis has been described for other antiretrovirals.
For treatment-naïve subjects, Week 48 data from ING113086 indicated that, overall, the incidence of treatment emergent liver chemistry toxicities was similar between DTG and RAL. Eleven subjects met liver stopping criteria, 7 for DTG (2%) and four for RAL (<1%). Most of these cases were confounded by underlying diseases or concomitant medications that are considered more likely than study drug to have caused these events. From the ING114467 48 Week data, the incidence of treatment emergent liver chemistry toxicities for DTG+ABC/3TC was lower than observed for the Atripla comparator arm,and lower when compared to both the DTG and RAL treatment groups in ING113086.
For treatment-experienced subjects, safety data suggests no excess risk of hepatic toxicity for DTG. In ING111762, excluding observations for HBV and/or HCV co-infected subjects (described below), the incidence of liver chemistry elevations on DTG were comparable to RAL, and in an advanced HIV population receiving multiple concomitant medications in ING112574, the incidence of treatment emergent liver chemistry toxicities for DTG 50 mg BID was comparable to DTG 50 mg once daily in ING111762 (less HBV and/or HCV co-infected subjects).
In most cases where liver abnormalities have been noted across the development program, the following circumstances have been present: the co-administered antiretroviral treatment included drugs with well-described bilirubin or liver enzyme elevations; and/or hepatitis virus co-infection was evident; and/or subjects had a medical history of alcohol abuse.
For subjects with hepatitis B and/or C co-infection, immune reconstitution as a result of HIV virologic and immunologic responses, along with inadequate therapy for hepatitis B co-infected subjects, likely contributed to significant elevations in liver chemistries. As several ART-experienced subjects were allowed to restart DTG or continued DTG without progression of liver enzyme elevations, drug-induced liver injury in this setting seems less likely in this patient population.
Eight subjects were identified across the program who were hepatitis B co-infected and with clinically significant flares of liver chemistries and/or HBV IRIS: 2 subjects in ING113086 (DTG: 1, RAL: 1), 1 subject in ING112574, and 5 subjects in ING111762. (DTG: 5, RAL: 0). Of the cases identified on DTG, 5/7 were not on HBV active therapy at the time of liver chemistry elevation and 5/7 had HBV active therapy discontinued at the start of DTG therapy. All subjects had HIV virologic and immunologic responses to DTG.

CONFIDENTIALModule 2.5 Clinical Overview
74
Subjects who were treatment-naive were not eligible to re-start study drugs due to wide availability of other therapeutic options. Subjects who were treatment-experienced could be considered for restart of DTG, after careful review of each case with the ViiV Healthcare Safety and Labeling Committee. Three subjects (1 in ING112574, 2 in ING111762) restarted or continued DTG after or in conjunction with the start of HBV active therapy (e.g., TDF/FTC or entecavir). For all 3 of these cases, liver chemistries have remained within normal limits after restart (or continuation of DTG). Therefore, if subjects are not receiving HBV active therapy at the start of potent HIV therapy, there is an increased risk for HBV IRIS or flare in the setting of HIV viral decline and immunologic improvement. The improved efficacy noted for DTG for the entire population in ING111762 may be contributing to higher rates of HBV-related IRIS in the hepatitis co-infected population in this study.
For hepatitis C virus co-infected subjects, the risk for significant liver chemistry increases in the setting of HIV virologic and immunologic responses does not appear as profound as that identified for HBV, but HCV IRIS may also contribute to the findings across the clinical program. Across all studies and patient populations, comparable rates of liver chemistry elevations were noted in HCV co-infected subjects across treatment groups.
Across all patient populations, safety data supports the administration of DTG in HIV-infected patients co-infected with hepatitis B and/or hepatitis C, with awareness of the need for appropriate HBV therapy and the possibility of HBV/HCV flares or IRIS after the start of DTG therapy. The sponsor plans to include recommended measures to manage the risk of HBV/HCV IRIS in the Warnings and Precautions Section in the proposed labeling.
5.6.6.3. Renal Function
Mild elevations of serum creatinine have been observed with DTG. These are related to a likely benign effect on creatinine secretion via blockade of the OCT2 receptor, which is responsible for tubular secretion of creatinine. In a Phase I study to assess renal pharmacodynamic effects, DTG at 50 mg once daily and 50 mg BID had no significant effect on GFR compared to placebo over 14 days based on iohexol clearance. In addition, neither treatment significantly changed PAH clearance, a measure of effective renal plasma flow.
Small increases in serum creatinine were observed on the DTG arms in each of the Phase IIb and III studies (range 9.66 mol/L at Week 48 for the combined 50 mg once daily dose in the ART naïve treatment population to 11.57 mol/L at Week 24 for the combined 50 mg twice daily dose in ART- experienced [INI-naïve] treatment population). These were evident from Week 1 but plateaued with no evidence of subsequent increase. Smaller mean increases in serum creatinine (range 4.66 to 6.5 mol/L) were noted on RAL treatment arms in ING113086 and ING111762, and declines in mean change from baseline values for creatinine (range -2.36 to -0.7 mol/L) were observed on EFV-containing treatment regimens.

CONFIDENTIALModule 2.5 Clinical Overview
75
A low incidence of graded creatinine elevations has been observed on DTG, and no Grade 3 to 4 toxicities have been observed in the 48 Week data from either ING113086 or ING114467. There were few subjects who developed acute renal failure accompanied by Grade 3 or 4 creatinine elevations. These subjects participated in ING111762 or ING112574 receiving DTG or RAL (ING111762 only), and all had confounding medical conditions or medications that likely caused or contributed to the events.
Transient increases in urine protein by dipstick in a minority of subjects were noted in the Phase IIb studies, prompting quantitative measures of urine albumin in Phase IIb and III studies (albumin is the protein detected by the dipstick test). These changes were not progressive in nature, were not associated with clinically significant changes for individual subjects with respect to AEs, graded lab abnormalities or withdrawals, and were not supported by more reliable, quantitative measures of albuminuria. Median increases in spot urine albumin/creatinine values were comparable between DTG and comparator treatment groups (RAL or EFV-containing regimens) and between DTG 50 mg BID and 50 mg once daily in the Phase III clinical studies. Importantly, tubular and glomerular urine protein was evaluated in the Phase I study assessing the renal safety of DTG, and no association between DTG dosing at 50 mg once daily or BID and proteinuria was observed in this study.
Finally, DTG is unlikely to potentiate nephrotoxicity observed with tenofovir. DTG does not increase serum concentrations of tenofovir, an antiretroviral known to be associated with renal tubular toxicity. Importantly, the in vitro and in vivo evidence to date suggests that DTG does not impact renal tubule transporters responsible for tenofovir elimination. DTG’s effect on creatinine secretion is via OCT2, which affects cation transport into the renal tubule. DTG has not been shown to affect the transport of anions. OAT1 (organic anion transporter) and OAT3 are responsible for anion (e.g., tenofovir) transport into the renal tubule. As serum tenofovir concentrations are not increased with co-administration with DTG, OAT inhibition by DTG is highly unlikely. MRP2 and MRP4 are anion transporters responsible for the transport of anions (e.g., tenofovir) from the renal tubule to the urine, and DTG has been shown not to inhibit MRP2, which also makes inhibition of MRP4 by DTG unlikely. Polymorphic MRP4 that decreases tenofovir renal clearance by 15% also increases plasma tenofovir concentrations by 32% [Kiser, 2008], which was not observed in the drug interaction study assessing the impact of DTG on tenofovir PK. Based on these data, an interaction with tenofovir at the renal tubule is considered unlikely.
In review of creatinine changes by NRTI backbone across the treatment-naïve studies, the median and interquartile ranges of change over time were similar, with no evidence of deterioration in the renal tolerability of DTG due to concomitant tenofovir (m2.7.4, Section 2.1.5.3). Additionally, 6/346 (2%) of subjects receiving DTG + TDF/FTC and 20/634 (3%) of subjects receiving DTG + ABC/3TC had treatment-emergent Grade 1 or 2 creatinine elevations, and no subjects had treatment-emergent Grade 3 or 4 elevations in creatinine on either NRTI backbone co-administered with DTG. Therefore, there is currently no clinical evidence that DTG potentiates the nephrotoxicity observed with tenofovir.

CONFIDENTIALModule 2.5 Clinical Overview
76
5.6.6.4. Gastrointestinal (GI) Disorders
As noted in Section 5.2, the primary effect of dolutegravir in nonclinical studies was gastrointestinal intolerance or irritation. Additionally, gastrointestinal symptoms are frequent adverse events with antiretroviral medications [DHHS, 2012]. As noted in Section 5.6.2 diarrhea and nausea were some of the most frequently observed AEs across patient populations, which were typically Grade 1 or 2 in severity and typically did not lead to discontinuation from studies. Events indicative of general GI intolerance (i.e., diarrhea, nausea, vomiting, and abdominal pain AE preferred terms only and no derivatives) with DTG 50 mg once daily were comparable to RAL- and EFV-containing regimens in treatment-naïve and –experienced subjects. Additionally, the general GI intolerance adverse event rate was comparable for INI-resistant subjects receiving DTG 50 mg BID and subjects receiving DTG 50 mg once daily.
Few cases of gastric or peptic ulcer disease were reported in treatment-naïve and INI-resistant subjects and were typically related to concomitant medications (e.g., aspirin) or medical conditions (Non-Hodgkin’s lymphoma). No cases of gastric ulcer or peptic ulcer disease were reported in ART-experienced (INI-naïve) subjects. Adverse eventsconsidered potentially indicative of GI ulcerative lesion as identified by Sponsor medical review were rarely reported in any of the patient populations. Hemoglobin concentrations also increased over time on DTG regimen, as would be expected from the positive effects of ART.
Nonclinical evidence for GI toxicity with DTG thus did not translate into significant findings in double blinded randomized clinical trials; a similar rate and nature of GI events were reported for DTG compared to RAL and EFV, and there was no evidence for an increased risk of GI ulcerative lesions.
5.6.6.5. Musculoskeletal Disorders
CPK elevations in subjects receiving DTG in the ART-naïve population were comparable to RAL and EFV-containing regimens. Most CPK elevations were asymptomatic and investigators were able to confirm high degrees of physical activity preceding the CPK elevations in the majority of cases. In the ART-experienced (INI-naïve) population, more subjects receiving RAL reported musculoskeletal disorders versus those receiving DTG, with fewer subjects on DTG experiencing Grade 3 or 4 events. The incidence of events reported for the ART-experienced (INI-resistant) population was lower than in the INI-naïve (ART-naïve and ART-experienced) population, despite the higher daily dose of DTG. Finally, no cases of drug-related rhabdomyolysis have been reported on DTG across the clinical program.
Therefore, no increased risk for clinically significant or serious musculoskeletal disorders has been identified for DTG.

CONFIDENTIALModule 2.5 Clinical Overview
77
5.6.6.6. Immune Reconstitution Inflammatory Syndrome (IRIS)
As detailed in m2.7.4, Section 2.1.5.9, for the Phase III clinical trials, potential IRIS cases were reviewed and adjudicated by senior ViiV Healthcare physicians (ING113086) or the Independent Data Monitoring Committee (IDMC; ING114467, ING111762, ING112574). For the ART-naïve and INI-resistant patient populations, few cases of IRIS were identified and incidence rates were similar between DTG 50 mg once daily and comparator treatments or DTG 50 mg BID.
Based on medical adjudication of IRIS-like events in the ART-experienced (INI-naïve) patient population in ING111762, subjects with hepatitis B or C co-infection receiving DTG were at greater risk for HBV or HCV IRIS than those receiving RAL. For other medical conditions frequently implicated in IRIS events, there was a low rate of IRIS cases for both DTG and RAL.
5.6.6.7. Other
No clinically significant safety findings were identified in the following AEs of special interest (discussed in more detail in m2.7.4 Section 2.1.5):
Torsades de Pointe
Nervous System Disorders
Psychiatric Disorders Including Suicidality
Neoplasms, Benign, Malignant, and Unspecified (including Cysts and Polyps)
Cardiovascular Disorders
5.6.7. Clinical Laboratory Evaluations
See m2.7.4, Section 3 for details of laboratory data.
5.6.7.1. Clinical Chemistry
Details of Clinical Chemistry safety findings can be found in m2.7.4, Section 3.1.
ART-naïve adult subjects: The majority of subjects (80% to 94%) across all studies and individual comparative arms had treatment emergent Graded clinical chemistry toxicities. A small proportion, 12 to 15%, had Grade 3 to 4 toxicities and the incidence was similar in all treatment groups across all the studies.
ART-experienced (INI-naïve) adult subjects: Similar to ART-naïve subjects, the majority of DTG (82%) and RAL (86%) subjects had treatment-emergent graded abnormalities. A small proportion (DTG: 15%, RAL: 16%) had Grade 3 to 4 toxicities.
ART-experienced (INI-resistant) adult subjects: Although a high proportion of subjects (85%) had a post-Baseline graded change in clinical chemistry, the majority were Grade 1 and Grade 2 with few Grade 3 to 4 events.

CONFIDENTIALModule 2.5 Clinical Overview
78
Liver and renal findings are discussed in Section 5.6.6.1 and Section 5.6.6.3, and are detailed in m2.7.4, Section 3.1.1, and Section 3.1.2, respectively. CPK results are discussed in detail in m2.7.4, Section 3.1.3.
There was no evidence of a clinically significant impairment of the lipid profile by DTG treatment in the Phase III studies. Changes in lipid parameters were generally small in both treatment and comparator groups in INI-naïve study populations, and did not appear to be adversely affected by the larger DTG 50 mg BID dose in the INI- resistant populations.
5.6.7.2. Hematology
Details of Hematology safety results can be found in m2.7.4, Section 3.2. There were no clinically significant trends in treatment emergent hematology abnormalities across all populations.
5.7. Vital Signs
There were no clinically significant patterns of changes in vital signs (weight, heart rate, systolic and diastolic blood pressure) across the studies (Phase I, II, and III).
5.8. Electrocardiograms
No subjects had a QTcF >500 msec, and few subjects had change from Baseline in QTcF or QTcB 60 msec. Additionally, few clinically significant ECG abnormalities were reported, and no trends were observed in these abnormalities. ECGs are discussed in Section 4.2 of m2.7.4.
In study ING111856 (m2.7.4, Section 2.1.5.6.3), DTG had no significant effect on cardiac repolarization.
5.9. Safety in Special Groups and Situations
The effect of intrinsic factors (i.e., gender, age, race, and hepatitis co-infection) and extrinsic factors associated with the patient environment (i.e., the effect of food) are discussed in m2.7.4 Sections 5.1 and 5.2, respectively, including the outcome of applicable PK analyses.
In general, gender, age, and race did not significantly impact rates of AEs or laboratory abnormalities reported across treatment groups. The representation of special groups (i.e., women, African American/African heritage, age 50) allowed an analysis of safety in these groups. Minor exceptions for gender were noted, such as a higher incidence of vomiting in treatment-naïve women receiving DTG, and differences in laboratory abnormalities in men and women, including more anemia in women and more ALT and CPK increases in men. Minor exceptions were also noted for race, with more African heritage, treatment-naïve subjects experiencing neutropenia; this is likely related to lower neutrophil counts in this racial group. These differences were not considered treatment-limiting.
Overall, the safety profile was similar across gender, age and race.

CONFIDENTIALModule 2.5 Clinical Overview
79
5.10. Pregnancies
No studies have been conducted with DTG in pregnant women, and pregnant women were excluded from the DTG clinical studies. Pregnancy outcomes from female subjects who became pregnant during the conduct of the Phase I to IIIb clinical studies and the compassionate use program conducted with DTG to date, are presented in m2.7.4, Section 5.4.
As of the submission cut-off date, there were 27 pregnancies reported across the DTG clinical studies and compassionate use program. Adverse outcomes have been reported for four of these cases; one was ectopic (Atripla) and three (one each for DTG, RAL and Atripla) resulted in spontaneous abortion (all between 5 and 12 weeks gestation).
Reproductive toxicity is not considered to be a risk for DTG based on the non-clinical and clinical findings to date.
5.11. Withdrawal Effects, Abuse Potential, Overdose
No studies to investigate the potential for withdrawal and rebound effects, or the potential for abuse or dependency with DTG have been performed. There is currently limited experience with DTG overdose (i.e., any dose above 50 mg once daily in INI-naïve adults; 50 mg BID in INI-resistant adults; and 1 mg/kg once daily with a maximum daily dose of 50 mg in INI-naïve pediatric patients). Single daily doses up to 250 mg have been administered orally to healthy subjects in clinical pharmacology study ING111856; with no unexpected adverse effects reported. The INI class of compounds has no known drug abuse potential. There are no data suggesting that DTG has the potential to imply illicit use, abuse, or dependency on DTG. In nonclinical studies, no effects related to DTG administration on central and peripheral nervous system or body temperature were noted following dosing withdrawal. There is no clinical evidence to suggest withdrawal or rebound effects of DTG. There have been no studies to investigate the effect of DTGon driving performance or the ability to operate machinery.
5.12. Post-Marketing Experience
Dolutegravir is not marketed in any country in the world. All safety data included in this submission are from clinical studies conducted with dolutegravir.
5.13. Safety Conclusions
Overall the safety profile for DTG, combined with the efficacy and virology profile, supports a favorable risk/benefit compared to other ARVs.
Based on limited available data in children and adolescents (12 to less than 18 years of age), there were no additional types of adverse reactions beyond those observed in the adult population.
The safety profile for DTG 50 mg once daily in INI-naïve subjects was comparable to RAL and generally favorable compared to Atripla and EFV.

CONFIDENTIALModule 2.5 Clinical Overview
80
DTG dosed 50 mg twice daily in highly ART-experienced (INI-resistant) subjects with advanced HIV disease resulted in a safety profile comparable to DTG 50 mg once daily in both ART-naïve and ART-experienced (INI-naïve) subjects, despite the advanced stage of disease and multiple concomitant medications.
Hypersensitivity is an uncommon but recognized risk for ART containing DTG regardless of dose or treatment population.
Cumulative data suggests a hepatic safety profile for DTG that is comparable to RAL or EFV.
Safety and pharmacokinetic data supports the administration of DTG in HIV-infected patients co-infected with hepatitis B virus and/or hepatitis C virus.
ART-experienced subjects with HBV co-infection receiving DTG were noted to have significant liver chemistry elevations in the setting of HIV virologic and immunologic responses to DTG and withdrawal (or lack of) HBV active therapy. The pattern of injury is likely consistent with IRIS and/or inadequate HBV therapy rather than direct liver injury due to DTG. Treatment-experienced subjects with hepatitis C virus co-infection may be at greater risk of HCV IRIS with DTG due to improved HIV virologic responses versus RAL.
Overall, the renal profile of DTG is comparable to comparators in Phase III studies (i.e., RAL and EFV). Mild elevations of creatinine on DTG are related to a likely benign effect on creatinine secretion via blockade of the OCT2 receptor, do not progress on continued treatment with DTG, and revert towards Baseline after DTG discontinuation.
The gastrointestinal profile for DTG 50 mg once daily was comparable to RAL and Atripla, was similar for the DTG 50 mg once daily and twice daily dose, and did not indicate an increased risk for peptic ulcers or serious erosions, as was seen in animal toxicity studies.
The musculoskeletal profile for DTG was generally comparable to that observed for RAL and Atripla treatment groups in INI-naive subjects, and there was no evidence of excess risk of musculoskeletal disorders for DTG 50 mg BID in INI-resistant subjects.
Despite the rapid decline in HIV-1 RNA observed on DTG, IRIS cases were generally infrequent on DTG, and the rates of IRIS on DTG were comparable to those observed on RAL and EFV.
ART-experienced (INI-naïve) subjects with hepatitis B and/or C virus co-infection receiving DTG may be at greater risk for IRIS than those receiving RAL, due to improved HIV virologic and immunologic responses with DTG compared to RAL, and withdrawal (or lack of) HBV active therapy in HIV/HBV co-infected subjects. Particular diligence should be applied in initiating or maintaining effective hepatitis B therapy (referring to treatment guidelines) when starting dolutegravir-based therapy in hepatitis B virus co-infected patients.
There was no evidence of a clinically significant impairment of the lipid profile by DTG treatment in the Phase III studies.

CONFIDENTIALModule 2.5 Clinical Overview
81
No effect of gender, age, or race on safety profile of DTG has been observed (beyond what might be expected for each subgroup).
6. BENEFITS AND RISKS CONCLUSIONS
HIV remains a serious and life-threatening infection for millions of patients around the world. HIV infection is characterized by deterioration in immune function. If left untreated or suboptimally treated, the subsequent occurrence of opportunistic infections and malignancies ultimately results in death. The treatment of HIV-1 disease has been significantly advanced by the availability of highly active antiretroviral therapy (HAART), which initially is based upon therapy with two NRTIs and a third agent such a NNRTI, boosted PI, or INI. However, each of these third agents has limitations that require accommodation, whether due to tolerability concerns, potency in patients with high viral loads, food restrictions, dosing complexity, or significant drug interactions that preclude co-administration with other ART. New antivirals that are effective for multi-drug resistant HIV are also critical for those patients who have no other options.
Dolutegravir given once daily has demonstrated advantages over RAL (the first marketed INI) which is given twice daily in both treatment-naïve and treatment-experienced patients. In treatment-experienced (INI-naïve) patients, a statistically higher proportion of patients receiving DTG plus background therapy achieved virologic success when compared to RAL plus background therapy through 24 weeks. DTG + ABC/3TC also demonstrated superior efficacy with improved tolerability over EFV/TDF/FTC in treatment-naïve patients. Importantly, DTG given twice daily has also demonstrated robust antiviral activity and a favorable safety profile in patients with the greatest medical need—extensively treatment-experienced patients with resistance to integrase inhibitors.
6.1. Benefits of Dolutegravir in the Treatment of HIV-1 Infection
Novel safe and effective drugs are needed for all sectors of the HIV population, including adults who are initiating ART for the first time, treatment-experienced adults (INI-naïve and INI-resistant), and pediatric patients. Dolutegravir is being developed as a treatment for all of these populations, and has distinct advantages over the most widely used therapies as follows:
Significantly improved efficacy for treatment-naïve patients over EFV-based regimen
Significant increase in efficacy for treatment-experienced (INI-naïve) patients over RAL
Efficacious in treatment-experienced (INI-resistant) patients, where no satisfactory alternative exists
Improved tolerability versus current preferred regimen with substantial reduction of treatment-limiting adverse drug reactions
High barrier to resistance, with no INI or NRTI resistance seen to date in treatment-naives on DTG regimen, and significantly lower resistance versus RAL in treatment-experienced subjects

CONFIDENTIALModule 2.5 Clinical Overview
82
Convenient once daily dosing (treatment-naïve and treatment-experienced, INI naïve), without need for pharmacokinetic booster
A new treatment option for adolescent (12 to <18 years) HIV-infected, INI-naïve patients
The results from four pivotal studies (Studies ING113086, ING112574, ING111762, and ING114467) provide substantial evidence of effectiveness for dolutegravir as a treatment for HIV-1 infection in combination with other antiretroviral agents.
DTG with two NRTIs was highly effective in ART-naïve subjects. High rates of virologic suppression [HIV-1 RNA <50 c/mL]) were observed in both studies of ART-naïve subjects; consistent responses were demonstrated in important subgroups as defined by Baseline HIV-1 RNA, NRTI backbone, CD4 cell count, gender, race, and age. DTG + NRTI backbone demonstrated comparable efficacy to RAL + NRTI backbone at Week 48. DTG + ABC/3TC achieved a statistically superior response through 48 weeks against the preferred FDC tablet Atripla (tenofovir/emtricitabine/efavirenz) in a HLA-B*5701 negative population, a result that was driven in large part by improved tolerability of the DTG-containing regimen.
In ING111762, virologic suppression (HIV-1 RNA <50 c/mL) in the dolutegravir arm (79%) was statistically superior to the raltegravir arm (70%), based on the Week 24 prespecified analysis (p=0.003), in this treatment-experienced, INI-naïve patient population. The difference in virologic response rate was driven by better overall virologic efficacy with DTG.
DTG 50 mg twice daily was effective for patients with resistance to INIs and associated extensive antiretroviral resistance to other agents, with efficacy rates comparable to or better than other antiretroviral agents utilized for within-class resistance in historical studies. Virologic responses in ING112574 were not clearly associated with the activity of the background antiviral agents but were best correlated with baseline DTG resistance (as determined by baseline genotype).
With regards to safety and tolerability, the DTG-containing regimen (DTG+ABC/3TC) in ING114467 was associated with significantly fewer withdrawals due to AEs in comparison with Atripla in a HLA-B*5701 negative population. In addition, subjects receiving Atripla were significantly less likely to develop dizziness, abnormal dreams, rash, anxiety and somnolence (i.e., relative risk values and 95% confidence intervals were <1), with statistically significant differences also observed in predefined neuropsychiatricrates compared to DTG in a pre-specified, exploratory analysis conducted as part of ING114467. Additionally, the safety profile for DTG was comparable to RAL in 2 treatment populations – treatment-naïve and treatment-experienced (INI-naïve). Finally, an advanced HIV population on a wide variety of concomitant antiretrovirals and other concomitant medications had a similar safety profile with a higher daily dose of DTG (50 mg BID).
Another important benefit of DTG is the different virologic profile versus other available INIs. Overall, the structural and electronic characteristics of DTG’s metal-binding scaffold, along with its binding position within the integrase catalytic pocket, may

CONFIDENTIALModule 2.5 Clinical Overview
83
contribute to slower dissociation kinetics, which have been observed for DTG compared with RAL and EVG, both for wildtype and INI-resistant integrase protein. Theprolonged DTG binding to mutant integrase protein is associated with its distinct resistance profile; since prolonged binding is observed with mutant integrase protein, this may decrease the opportunity for resistance to develop, and would be consistent with a higher barrier to resistance.
Confirming these in vitro attributes, DTG-based regimens had a higher barrier to resistance in ART-experienced (INI-naïve patients), as demonstrated in ING111762where significantly fewer virologic failures with INI resistance were observed when compared with RAL. Data from ING113086 and ING114467 were also supportive, as no subjects on the DTG regimens developed resistance to either the INI or the background NRTIs, whereas resistance to both the third agent and the background NRTIs was observed in both the RAL and EFV-based comparator arms.
In the setting of INI-resistance, DTG had efficacy across a broad range of mutational patterns, with robust virologic responses across the viral populations which represent the majority of INI-resistant viruses. Additionally, the most prevalent treatment-emergent mutations detected were IN resistance-associated secondary mutations that were added to a viral genotype with IN primary mutations present. All treatment-emergent mutations detected in the setting of pre-existing INI resistance were well characterized RAL and/or EVG resistance associated mutations.
Dolutegravir offers once-daily dosing in patients without INI resistance, no requirement for pharmacokinetic boosters and few dose adjustments for drug interactions. DTG can also be dosed without regard to meals, as there is no significant food effect. DTG also exhibits less PK variability, with more predictable exposures and lower risk of achieving inadequate or toxic exposures.
No clinically significant effect of age, weight, gender, race, ethnicity, smoking, HBV/HCV co-infection, disease status (CDC classification of HIV infection), and polymorphism of drug-metabolizing enzymes was observed on DTG concentrations, therefore no dose adjustment of DTG is needed in subjects based on these patient characteristics. Furthermore, no dose adjustment for DTG is needed in subjects with mild to moderate hepatic impairment (Child Pugh grade A or B) or in subjects with mild, moderate, or severe (CrCL<30 mL/min, not on dialysis) renal impairment. DTG can be used in HBV or HCV-co-infected subjects, as no clinically significant differences in DTG PK nor drug interactions with concomitant viral hepatitis therapy were observed or expected.
Finally, DTG represents a new option for therapy of adolescents with HIV infection. DTG PK in adolescents of at least 40 kg of body weight is similar to adults, and although data is limited, the safety profile is comparable to adults. Therefore, INI-naïve pediatric subjects can take the adult dose of 50 mg once daily.

CONFIDENTIALModule 2.5 Clinical Overview
84
6.2. Risks of Dolutegravir in the Treatment of HIV-1 Infection
The most common AEs seen in the dolutegravir clinical development program were diarrhea, nausea, and headache. These events occurred at similar rates across the treatment groups, were generally mild in intensity, and were typically not treatment limiting. In the treatment-naïve subjects, the only AE observed at significantly higher frequency with DTG+ABC/3TC versus Atripla was insomnia, with event rate differences observed in ING114467only. In all other studies, rates of insomnia were generally low and were comparable between DTG and RAL. Insomnia was not treatment limiting in the clinical program. Neuropsychiatric events otherwise occurred at a comparable rate for subjects on DTG versus RAL, in a pre-specified, exploratory analysis conducted as part of ING114467, and at a statistically significantly lower rate compared with Atripla.
As observed with RAL, HSR, characterized by rash, constitutional findings, and in few cases, organ dysfunction including liver injury have been observed in the DTG clinical studies. This risk will be highlighted as a Warning and Precaution in the label and patient information, including a recommendation to immediately discontinue DTG if HSR develops. Clinical status including liver enzymes should be monitored and appropriate therapy initiated in these patients. Other serious rash conditions, such as Stevens-Johnson syndrome, erythema multiforme and toxic epidermal necrolysis have not been observed across the DTG clinical program.
The hepatic safety of DTG appears generally comparable to the widely prescribed comparators, RAL and TDF/FTC/EFV in treatment-naïve patients, including those co-infected with HBV or HCV. For the overall population, a similar hepatic profile was observed in treatment-experienced patients, taking into account concomitant antiretrovirals and higher rates of hepatitis B and C co-infection.
Immune reconstitution syndrome is a labeled risk for other antiretrovirals. Data from this clinical program indicates that the overall risk for immune reconstitution with DTG-based therapy is not in excess of comparator agents, with the possible exception of HBV and HCV IRIS with initiation of DTG-based therapy. Treatment-naïve and -experienced patients were identified across the program who were hepatitis B co-infected and had clinically significant flares of liver chemistries and/or HBV IRIS. In treatment-experienced, HBV co-infected patients, the significant liver inflammation was associated with discontinuation of HBV active therapy and HIV virologic and immunologic responses to DTG. Recurrence of this liver inflammation has not been observed in those ART-experienced patients allowed to restart or continue DTG in conjunction with initiating hepatitis B therapy, thus supporting the view that these cases are related to hepatitis B flares or IRIS. Additionally, liver chemistry elevations were noted in hepatitis C co-infected patients but were generally balanced across treatment arms and, in most cases, were non-progressive or treatment-limiting. Instead, they were also associated with HIV virologic and immunologic responses across treatment groups. This view was confirmed by review of cases by the Independent Data Monitoring Committee. The sponsor intends to describe the risk for immune reconstitution syndromein general (and in particular for patients co-infected with HBV/HCV) and appropriate measures to manage this risk in the prescribing information and patient information leaflet.

CONFIDENTIALModule 2.5 Clinical Overview
85
Non-clinical GI findings did not result in higher rates of GI events (including nausea and diarrhea events) versus comparators. GI erosions noted in nonclinical studies did not translate into increased risk for GI ulcers or related conditions on DTG in the clinical setting. Hemoglobin concentrations also increased over time on DTG regimen, as would be expected from the positive effects of ART. PK-AE analyses did not show any relationship between DTG exposure and the occurrence of nausea or diarrhea across the patient populations.
Non-clinical data suggest that there are no specific risks to the fetus from dolutegravirtreatment. There are limited clinical data on the effect of dolutegravir on the developing human fetus. It is the intent of the sponsor that women who become pregnant while on DTG therapy will be encouraged to participate in the North American and European pregnancy registries, to assess the presence or absence of teratogenic effects of DTG.
In vitro, DTG inhibited the renal organic cation transporter (OCT2) and may increase plasma concentrations of drugs dependent on OCT2 for clearance (dofetilide and metformin). The co-administration of DTG and dofetilide is contraindicated. Careful monitoring is recommended when starting the combination of DTG with metformin, and metformin dose adjustments may be required.
Although patients 65 years of age were eligible for enrolment into the clinical studies, few did so. Consequently there are insufficient data to determine a meaningful benefit/risk assessment in this population. However, the safety profile of DTG in patients 50 years of age appeared comparable to those <50 years of age, and the pharmacokinetics of DTG were not affected in patients with moderate declines in liver function or severe declines in renal function. Population pharmacokinetic analysis of dolutegravir also showed that there was no clinically significant effect of age ondolutegravir exposure.
Thus far the clinical development program for dolutegravir has treated a limited number of pediatric patients. However, the PK of DTG in adolescents treated with 50 mg once daily was consistent with PK in adults, and the tolerability and efficacy of DTG-based therapy has been favorable to date. ING112578 (P1093) has completed enrolment of adolescents to support the safety and efficacy of DTG in subjects 12 to <18 years of age; the study plans to enroll sequential groups of subjects in descending age-based cohorts in order to support updated DTG dose recommendations for children as young as 4 weeks of age.
All medications have AE profiles which must be assessed prior to use, allowing for an appropriate risk/benefit assessment. Relative to other current treatment options, DTG has an acceptable safety profile in patients with HIV who have not been treated before with INIs, and it has the potential to provide significant benefit with optimized background therapy in most adults with multi-drug resistance that includes resistance to the currently marketed INIs.

CONFIDENTIALModule 2.5 Clinical Overview
86
6.3. Overall Dosing Recommendations
The data collected in the clinical program suggests that in INI-naïve (treatment-naïve or treatment-experienced) adults patients, dolutegravir therapy with 50 mg once daily is safe and effective in combination therapy. The same 50 mg once daily dose is recommended for INI-naïve adolescents 12 to 18 years of age and weighing at least 40 kg. In INI-resistant adults, the recommended dose of DTG is 50 mg twice daily, in combination with other antiretrovirals.
6.4. Overall Conclusions
There remains a significant need for new antiretrovirals that can treat multi-drug resistant strains of HIV. Moreover, patients and their physicians would benefit from antiretroviral agents that deliver the combination of potent antiviral efficacy, good tolerability, and ease of use (once daily administration without regards to food or major drug interactions). Dolutegravir has been shown to be a highly effective treatment option, having demonstrated statistically improved responses when compared to standard of care regimen (EFV/TDF/FTC in treatment-naives, and RAL plus optimized background therapy for treatment experienced patients who have not been treated with INIs previously). DTG-based regimens have also demonstrated a higher barrier to resistancein INI-naïve patients, as demonstrated in ING111762 where fewer virologic failures and statistically significantly fewer subjects with INI resistance were observed when compared with RAL through Week 24. Finally, DTG-based regimens have also demonstrated excellent tolerability, evidenced by the low rate of discontinuations due to AEs across the clinical program.
Identified risks for DTG-based therapy include hypersensitivity reactions, hepatitis, immune reconstitution syndrome (including in the setting of HBV/HCV co-infection), and a potentially serious drug interaction with dofetilide. Appropriate labeling and risk management activities, tailored to the geographic regions where DTG will be marketed, are described in this application. Dolutegravir compares well with other antiretroviral agents, in both efficacy and tolerability. There are a substantial number of patients who are in need of new agents to treat drug-resistant HIV, and that offer the unique combination of efficacy and tolerability that encourage life-long adherence for this chronic infection. Dolutegravir has been developed to provide much needed improvements in the control of HIV disease.

CONFIDENTIALModule 2.5 Clinical Overview
87
7. REFERENCES
Carr A and Cooper DA: Adverse effects of antiretroviral therapy. Lancet 2000; 356(9239):1423-1430.
Cooper DA, Steigbigel RT, Gatell JM, et al. Subgroup and resistance analyses of raltegravir for resistant HIV-1 Infection. N Engl J Med 2008; 359:355-65.
DeJesus E, Rockstroh JK, Henry K, et al. Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate versus ritonavir-boosted atazanavir plus co-formulated emtricitabine and tenofovir disoproxil fumarate for initial treatment of HIV-1 infection: a randomized, double-blind, phase 3, non-inferiority trial. Lancet2012;379(9835):2429–2438.
Department of Health and Human Services (DHHS), Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Updated 27 March 2012. Available online at: http://aidsinfo.nih.gov/guidelines. Data accessed: October 30, 2012.
Doerholt K, Duong T, Tookey P, Butler K, Lyall H, Sharland M, Novelli V, Riordan A, Dunn D, Walker AS, Gibb DM. Outcomes for human immunodeficiency virus-1-infected infants in the United Kingdom and Republic of Ireland in the era of effective antiretroviral therapy. Ped Infect Dis J 2006; 25:420-426.
EPZICOM US Prescribing Information, 2012. Available at http://www.viivhealthcare.com/~/media/Files/G/GlaxoSmithKline-Plc/pdfs/Epzicom-PI-MG-May-2012.pdf. Date Accessed: October 30, 2012.
European Medicines Agency (EMA ICH Topic E 11Clinical Investigation of Medicinal Products in the Paediatric Population, Doc. Ref. CPMP/ICH/2711/99*. January 2011. Available at: http://www.emea.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002926.pdf. Date Accessed: September 9, 2012.
European Medicines Agency (EMA), Committee for Medicinal Products for Human Use (CHMP). Guideline on the clinical development of medicinal products for the treatment of HIV infection, Doc. Ref. EMEA/CHMP/EWP/9147/2008-corr*. London, adopted 22 October 2009. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/12/WC500017055.pdf. Date accessed: October 30, 2012.
FDA ad comm. Briefing Information for the Antiviral Drugs Advisory Committee (AVDAC) Meeting, May 11, 2012 available at: http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/AntiviralDrugsAdvisoryCommittee/ucm303394.htm. Date accessed: September 9, 2012.

CONFIDENTIALModule 2.5 Clinical Overview
88
FDA Guidance for Industry: Role of HIV Resistance Testing in Antiretroviral Drug Development, October 2007, available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071173.pdf. Date accessed: August 18, 2012.
German P, Warren D, West S, Hui J, Kearney B. Pharmacokinetics and Bioavailability of an Integrase and Novel Pharmacoenhancer-Containing Single-Tablet Fixed-Dose Combination Regimen for the Treatment of HIV. J Acquir Immune Defic Syndr2010:55:323–329.
Gortmaker SL, Hughes M, Cervia J et al. Effect of combination therapy including protease inhibitors on mortality among children and adolescents infected with HIV-1. N Engl J Med 2001; 345(21):1522-1528.
Hazuda DJ, Miller MD, Nguyen BY, et al. Resistance to the HIV-integrase inhibitor raltegravir: analysis of protocol 005, a phase II study in patients with triple-class-resistant HIV-1 infection. Program and abstracts of the 16th International HIV Drug Resistance Workshop; June 12-16, 2007; Barbados, West Indies. 2007. Abstract 8.
Hill A and Sabin, C. Designing and Interpreting Noninferiority Trials in Naïve and Experienced Patients. AIDS 2008;22(8):913-921.
International AIDS Society (IAS) Guidelines – Update of the Drug Resistance Mutations in HIV-1: Topics in HIV Medicine. December 2009; 17(5). Available at: https://www.iasusa.org/sites/default/files/tam/17-5-138.pdf. Date accessed: November 13, 2012.
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) Guidance for Industry: E 10 Choice of Control Group and Related Issues in Clinical Trials. U.S. Department of Health and Human Services Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER), May 2001. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM073139.pdf. Date Accessed: September 9, 2012.
Isentress Package Insert, revised April 2012.
Isentress, EU Summary of Product Characteristics, 2012. Available at http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000860/WC500037405.pdf. Date Accessed: October 30, 2012.
Jia CX, Mehlum L, Qin P. AIDS/HIV infection, comorbid psychiatric illness, and risk for subsequent suicide: a nationwide register linkage study. J Clin Psychiatry. 2012 Sep 4. pii: 12m07814. [Epub ahead of print]

CONFIDENTIALModule 2.5 Clinical Overview
89
Kiser JJ, Carten ML, Aquilante CL, Anderson PL, Wolfe P, King TM, Delahunty T, Bushman LR, and Fletcher CV. The Effect of Lopinavir/Ritonavir on the Renal Clearance of Tenofovir in HIV-infected Patients. Clin Pharmacol and Therap2008;83(2):265-272.
KIVEXA EU Summary of Product Characteristics, 2011. Available at http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000581/WC500043730.pdf. Date Accessed: October 30, 2012.
Lennox JL, DeJesus E, Berger DS, et al. Raltegravir Versus Efavirenz Regimens in Treatment-Naive HIV-1–Infected Patients: 96-Week Efficacy, Durability, Subgroup, Safety, and Metabolic Analyses. J Acquir Immune Defic Syndr 2010;55(1):39-48.
McColl DJ, Fransen S, Gupta S, et al. Resistance and cross-resistance to first-generation integrase inhibitors: insights from a Phase II study of elvitegravir (GS-9137). Program and abstracts of the 16th International HIV Drug Resistance Workshop; June 12-16, 2007; Barbados, West Indies. 2007. Abstract 9.
Molina J, Cohen C, Katlama C, et al. Safety and Efficacy of Darunavir (TMC114) With Low-Dose Ritonavir in Treatment-Experienced Patients : 24-Week Results of POWER 3. JAIDS 2007;46:24–31.
Molina J, LaMarca A, Andrade-Villanueva J, Clotet B, et al. Efficacy and safety of once daily elvitegravir versus twice daily raltegravir in treatment-experienced patients with HIV-1 receiving a ritonavir-boosted protease inhibitor: randomised, double-blind, phase 3, non-inferiority study. Lancet Infect Dis 2012;12: 27–35.
National Institute on Aging (NIA) (National Institutes of Health). HIV, AIDS, and Older People. Updated April 2012. Available at: http://www.nia.nih.gov/health/publication/hiv-aids-and-older-people. Date Accessed: September 9, 2012.
National Institutes of Health Health and Human Services Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents Mar 2012. Available at: http://aidsinfo.nih.gov/guidelines/html/1/adult-and-adolescent-arv-guidelines/0/. Date Accessed: November 13, 2012.
Sax PE, DeJesus E, Mills A, et al. Co-formulated elvitegravir, cobicistat, emtricitabine, and tenofovir versus co-formulated efavirenz, emtricitabine, and tenofovir for initial treatment of HIV-1 infection: a randomised, double-blind, Phase 3 trial, analysis of results after 48 weeks. Lancet 2012;379(9835):2439–2448.
Steigbigel RT, Cooper DA, Kumar PN et al. Raltegravir with Optimized Background Therapy for Resistant HIV-1 infection. N Engl J Med 2008; 359(4):339-354.
UNAIDS (Joint United Nations Programme on HIV/AIDS). Report on the global AIDS epidemic. December 2010. Available at: http://www.unaids.org/globalreport/. Date accessed: September 9, 2012.

CONFIDENTIALModule 2.5 Clinical Overview
90
UNAIDS 2012a. Fact Sheet: The Global AIDS Epidemic; 2012. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/201207_FactSheet_Global_en.pdf. Date Accessed: September 9, 2012.
UNAIDS 2012b. Core Slides: Global Summary of the AIDS Epidemic; July 2012. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/201207_epi_core_en.pdf. Date Accessed: September 9, 2012.

CONFIDENTIALModule 2.5 Clinical Overview
91
8. APPENDICES
Appendix Table 1 Explanation for Empty Submission Modules
Module Title Explanation5.3.1.1 BA study reports The absolute bioavailability of DTG has not been
established. The low solubility of DTG in buffered solutions and its non-specific binding present significant challenges to an IV formulation for DTG even at very low doses, as explained in m2.7.1. Comparative BA and BE study reports for ING113674, ING114556 and ING114581 can be found in m5.3.1.2
5.3.1.3 In-vitro/In-vivo Correlation Study reports The development of an in-vitro/in-vivo correlation is not considered necessary and has not been progressed. This is described in m2.7.1 and based on ING113068,which demonstrated similar exposure with tablets containing different particle sizes.
5.3.2.1 Plasma Protein Binding SR Studies on the binding of dolutegravir to human plasma protein are contained in m4.2.2.3.
5.3.2.2 Reports of Hepatic Metabolism and Drug Interaction Studies
Hepatic metabolism was examined in ING111853 (m5.3.3.1). Drug interaction studies are listed under Extrinsic Factor PK Study Reports in m5.3.3.4.
5.3.2.3 Reports of studies using other human biomaterials
Specific studies to examine the effect of other humanbiomaterials on PK were not conducted.
5.3.3.2 Patient PK & Initial Tolerability Report The tolerability of dolutegravir was first tested in healthy volunteers using an oral suspension in ING111207 (m5.3.3.1). The tolerability of the dolutegravir tablet was first tested in the repeat dose study testing for relative bioavailability in ING111322 (m5.3.3.1).
5.3.6 Reports of post-marketing studies There is no information on post-marketing experience since dolutegravir is not a marketed product.
5.3.7 Case Report Forms and Individual Patient Listings
Available upon request