Malignant interstitial cell carcinoma of the testis: Report of two cases with steroid synthetic...
-
Upload
stephen-davis -
Category
Documents
-
view
213 -
download
0
Transcript of Malignant interstitial cell carcinoma of the testis: Report of two cases with steroid synthetic...

Malignant Interstitial Cell Carcinoma of the Testis:
Report of Two Cases with Steroid Synthetic Profiles, Response to Therapy, and Review of the Literature
STEPHEN DAVIS, MD, NANCY A. DI MARTINO, MD, AND GEORGE SCHNEIDER, MD
Two cases of malignant interstitial cell carcinoma of the testis are reported. The first patient had no evidence of a virilizing syndrome. Basal plasma testosterone (T) was decreased, whereas plasma lutein- izing hormone, estrone (E,), and androstenedione were elevated. These findings were diagnostic of a defect in T secretion as a result of a partial 17-hydroxysteroid dehydrogenase deficiency as seen in male pseudohermaphroditism. In the second patient, showing gynecomastia and atrophic testis, endocrine studies revealed high plasma T and estradiol (E2); all measured A4 and A5 precursors of T were elevated resembling the pattern seen in virilizing adrenal carcinomas. Both patients were treated with radio- therapy without demonstrable effect. Chemotherapy -consisting of a combination of cis-platinum, vinblastine, and bleomycin; then cyclophosphamide, doxorubicin, and vincristine; and finally o,p'- DDD-was unsuccessful in reducing tumor bulk. Since malignant Leydig cell carcinomas are rare, this paper reviews the literature and makes recommendations concerning treatment.
Cancer 47:425-431, 1981.
ESTICULAR NEOPLASMS represent approximately T 1% of all tumors in man; those derived from the Leydig cell (interstitial cell) are rare, constituting 1% of all testicular neoplasm^.'^ The malignant form of inter- stitial cell tumors (ICT) is uniquely rare, with only 19 cases previously described in the literature. The benign ICT. in its usual presentation, is well known for its ability to induce precocious puberty in boys, a result of its secretion of androgens; however, the rarity of the malignant variety has precluded an adequate study of its steroid synthetic activities. The report of Lipsett et CII." is the only definitive study published. In their case, the steroid secretion pattern was similar to that of virilizing adrenal carcinomas with increased production of C- 19 steroids and 21-deoxypregnane analogues.
In this presentation, two cases of biopsy-proven metastatic Leydig cell carcinomas are described. In the first case, the steroid synthetic pattern resembled that seen in virilizing adrenal carcinomas; in the second case, the hormonal pattern was that of a 17-hydroxy- steroid dehydrogenase deficiency, as seen in patients
From the OncologyiClinical Immunology and Endocrine Sections, Veterans Administration Medical Center, East Orange, New Jersey: and the College of Medicine and Dentistry of New Jersey, New Jersey Medical School Newark, New Jersey.
Address for reprints: Stephen Davis, M.D. , Chief, Oncology Section, Veterans Administration Medical Center, East Orange, NJ 07019.
Accepted for publication March 11, 1980.
with male pseudohermaphroditism.l".llJ1 Radiotherapy and chemotherapy were given without any demonstra- ble effect. Previously reported data are reviewed con- cerning the treatment of this rare disease, and an ap- proach to early diagnosed cases is suggested.
Case Reports
Case I: D.C., a 61-year-old Black man, a Jehovah's Wit- ness and father of four children, was admitted to a hospital in November 1971 with a right testicular mass. The remainder of the physical examination was unremarkable. He under- went a right orchiectomy . There was extensive replacement of the testicular parenchyma by tumor tissue. Microscopic examination identified an interstitial cell carcinoma (con- firmed by the staffpathologists at the Armed Forces Institute of Pathology). Routine laboratory studies and chest roentgeno- gram showed no abnormalities. Lymphangiogram and endo- crine studies were not performed.
The patient did well until October 1974, when he noted a "swelling in the groin." Physical examination revealed a hard, non-tender, 3 x 4 cm right inguinal node, but was otherwise negative. Lymph node biopsy revealed metastatic interstitial cell carcinoma, When radical retroperitoneal lymph node dissection was performed, four nodes were found to contain tumor cells. The patient refused postoperative radiotherapy. Chest roentgenograms were normal, as were results of 24-hour urine analysis for 17-keto steroids and 17-hydroxysteroids.
In May 1978, the patient was first seen by us and admitted to the hospital complaining of severe left-sided chest pain
0008-543Xi8li011510425 $0.85 0 American Cancer Society
425

426 CANCER January 15 1981 Vol. 47
exaggerated by movement. The physical examination was unremarkable. There was no gynecomastia or ambiguous genitialia. Routine laboratory studies, including hematology, liver enzyme tests, and electrolytes were within normal limits. Electrocardiogram was unremarkable. Nuclear bone and liver scans were normal. Chest roentgenograms revealed a multilobular mass to the left of the anterior mediastinum and nodular masses in the left hilus.
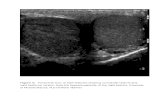
The patient consented to an anterior mediastinostomy with biopsy. Microscopic examination showed interstitial cell carcinoma (Fig. 1). Endocrine studies were performed at this point.
The patient was subsequently treated with combination chemotherapy consisting of cis-platinum ( I5 mg/m2 daily by i.v. infusion for five days); vinblastine (5 mg/m2 on days 1 and 8); and bleomycin (10 units daily by continuous infusion for five days). This regimen was repeated every 28 days. The chemotherapy was changed (since no response was demon- strated for the previous regimen) to cyclophosphamide (400 mg/m* on day I); vincristine (2 mg on days 1 and 8); and doxo- rubicin (40 mdm2 on day 1) repeated every three weeks. No tumor reduction occurred after nine weeks. Radiation ther- apy, using an 8-million electron volt (MEV) linear accelerator, to a total dose of 5000 rad to the mediastinum and hilum also failed to evoke a tumor response. The patient refused a thora- cotomy for tumor debulking. Twelve grams of o,p’-DDD daily over an 8-week period failed to induce a response. The patient died in May 1979; no autopsy was performed.
Case 2: M.J., a 74-year-old white man, was admitted to a hospital in June 1975 complaining of a right testicular mass which had been present for at least two years. Physical exarni- nation was otherwise unremarkable. Results of routine blood tests, (including a complete blood count) electrolyte studies, and liver enzyme tests were normal. Chest roentgenogram was normal. A right orchiectomy was performed. Histopatho-
FIG. 1. Low-power photomicorgraph of malignant Leydig cell tumor biopsied from the mediastinum (Case 1) (x240).
logic examination revealed an interstitial cell tumor with few mitotic figures, and no angioinvasion or Reinke crystals were noted. However, there was lymphatic invasion. A postopera- tive lymphangiogram was reported as normal, as was the 24- hour urine excretion of 17-hydroxysteroids and 17-keto- steroids.
The patient did well until September 1977, when he was first seen by us. At that time, he was admitted to the hospital with a history of vomiting and abdominal pain. Physical examina- tion revealed bilateral gynecomastia, and atrophic left testis. The abdomen was distended and tympanic with decreased bowel sounds. Abdominal roentgenograms were consistent with small bowel obstruction. Exploratory laparotomy re- vealed an unresectable mass, which was surgically bypassed. Adrenal glands were normal in size and consistency. The patient recovered without sequelae. The pathologic diagnosis was metastatic interstitial cell tumor (Fig. 2). Three weeks later, the patient underwent endocrine testing.
Total abdominal irradiation (total dose 3600 rad) delivered by an 8 MEV linear accelerator failed to result in tumor reduc- tion as evaluated by computerized tomography. Combination chemotherapy with cis-platinum, vinblastine, and bleomycin (as described for patient I ) ; then cyclophosphamide. vincris- tine, and doxorubicin (described for patient I ) ; and finally 0,- p’-DDD 10 gm/daily was attempted. No reduction in tumor size was noted with any of the regimens. The patient died in June 1978. N o autopsy was performed.
Materials and Methods
Serum testosterone (T) was measured after ether extraction via radioimmunoassay using an antibody prepared against T-3-0xime-albumin.~ Dialyzable T was measured by the equilibrium dialysis method of Chopra et a f . 4 using a 1:5 serum dilution. Free T was

No. 2 MALIGNANT LEYDIG CELL CARCINOMA . Davis et a f . 427
FIG. 2. High-power photomicrograph of biopsy obtained from exporatory lapa- rotomy performed on Case 2. Histolog- ically, the tumor is a malignant Leydig cell carcinoma ( ~ 9 6 0 ) .
calculated by multiplying the total T by the dialyzable fraction.
Serum androstenedione (A) and 17-hydroxyproges- terone (HP) were measured by direct radioimmuno- assay as previously described.8.12 Dehydroepiandros- terone sulfate (DHEAS) was measured after two ether extractions of serum via r ad io imm~noassay .~~ Serum cortisol was measured directly from serum by radio- immunoassay using a Corning Immunophase Kit. Pro- lactin was measured using a commercial kit from Serono (Boston, Mass.) and ACTH using a commercial kit from CIS Radiopharmaceuticals (Bedford, Mass.). Serum luteinizing hormone and follicle-stimulating hormone (LH) (FSH) were measured by radioimmuno- assay using a double antibody separation technique.21*22
Serum estradiol (E,) and estrone (El) were measured after an ether extraction of serum using specific anti- bodies made against E2-6-carboxymethyloxime-bovine albumin or E 1-6 carboxymethyloxime-bovine-albu- min, as previously described. 1 8 3 3 2 Urinary hydroxy- steroids (17-HS) and ketosteroids (17-KS) were meas- ured using standard techniques. 29.42
Human chorionic gonadotropin (HCG) stimulation was performed by administering HCG 4000 U/day i.m. for five consecutive days. Blood was obtained for T , A, HP, DHEAS, FSH, El , E2, ACTH, cortisol, and pro- lactin at 0800 hours of the sixth day. Urine for 17-HS and 17-KS was collected on the last day of HCG admini- stration. Fluoxymesterone (40 mg daily) and dexameth- asone (8 mg daily) was administered for five days on separate occasions. Blood was obtained for measure- ment of the above hormones plus LH at 0800 hours of
the sixth day. Urine was collected for 17-KS and 17-HS on the sixth day of drug administration.
Results
17-Ketosteroids ( K S ) and Corticoids ( H S )
The urinary excretion of 17-KS and 17-HS in Case 1 were within normal limits, 16.0 mg and 4.2 mg, respec- tively. These values were not altered by fluoxymester- one, 40 mg daily (Table 1). The administration of HCG 4000 U/daily for five days increased the 17-KS excretion slightly to 21.2 mg; however, it still remained within normal range. It is conceivable that 1 l-deoxy- 17-keto- steroids (DHEA, androsterone, etiocholanolone) were elevated secondary to HCG stimulation; however, we did not fractionate the urine.
In Case 2, urinary 17-KS were markedly elevated (365 mg), whereas 17-HS excretion was minimally ele- vated (13.7 mg). The urinary 17-KS level was not sup- pressed by dexamethasone, 8 mg daily. HCG adminis- tration (as above) increased 17-KS (610 mg). Following administration of HCG, 17-HS rose to 20.2 mg. The ex- cretion decreased to within the normal range (9.3 mg) following administration of dexamethasone and was unaffected by fluoxymestrone suppression (15.9 mg).
Plasma Hormones
Plasma T in Case 1 was decreased (83 ng/dl). The dialyzable fraction was normal so that the calculated free T was, likewise, markedly decreased (2.0 ng/dl), plasma A (847 pgldl), DHEAS (345 pg%) El (10.0

428 CANCER Juiiuury 15 1981 V O l . 47
TABLE I . Endocrine Studies: Case 1
Normal value
Patient
Basal HCG Fluoxymestrone levels stimulation suppression
Urinary steroidsi24 hours 17-ketosteroids 17-hydroxysteroids
Plasma steroids Testosterone Androstenedione Dehydroepiandrosterone sulfate Estrone Estradiol
FSH LH Prolactin ACTH Cortisol
Plasma pituitary
9-22 mg 3- 10 mg
350- 1000 ngidl 50- 150 ngidl 100-250 pgidl I .O-6.0 ngidl 1.0-4.0 ngidl
5-20 mlu/ml 5-20 rnIuiml 5- 15 ngiml 5 - 120 pgiml 5-25 pgidl
16.0 4.2
83.0 847.0 345.0
10.0 4.7
25.5 21.1 12.9 29.2 11.6
21.2 7.8
351.0 5 160.0 1590.0 NT*
7.3
9.6
31.5 41.6
9. I
-
13. I 6.4
97.0 1120.0 669.0 NT
3 . 2
<5.0 <5.0
9.8 NT 12.6
* NT-Not tested.
ng/dl), and LH (21.1 mIU/ml) were all elevated (Table 1). The i.m. injection of HCG induced increases in T , DHEAS, and EZ, whereas plasma A rose to proportion- ately greater levels (S160 ng/dl). FSH was appropriately depressed. Fluoxymesterone failed to suppress A and DHEAS to below basal levels despite nondetectable levels of LH and FSH (Table 1).
In Case 2, plasmaT, A , DHEAS, E,, EZ, 17-hydroxy- progesterone (HP) and prolactin were markedly ele- vated above normal values (Table 2). The separate administration of dexamethasone and fluoxymesterone failed to significantly alter plasma steroid levels; how- ever, HCG led to a rise in plasma T, A, DHEAS, HP, El , E2. HCG caused suppression of FSH to undetect- able levels, and prolactin was unchanged. The plasma T:A ratio remained at approximately 4: 1 following dexamethasone and fluoxymesterone administration.
Discussion
Malignant interstitial cell tumors of the testis occur in adult males. In the 19 reported cases of malignancy, the age at time of manifestation ranged from 29 to 82 years, with a mean age of 60 years. The majority of patients were seen with a painless scrota1 mass, as in our two cases. Although this tumor is classically a func- tioning one, none of the 19 recorded cases initially pre- sented with endocrine complaints. The result of excess androgen production in children produces precocious puberty, but in adult males the effect is not dramatic. Gynecomastia occurred in three cases but developed long after the tumor was metastatic.
There is controversy as to exactly what constitutes malignancy in interstitial cell tumors. Currently, the accepted criteria for malignancy is proven metastases.
However, Gharpure9 suggests that a diagnosis of malig- nancy could be made without waiting for the develop- ment of metastases if the following four features are present:
(1) Marked pleomorphism of cells. (2) Gian-t atypical mitoses. (3) Lack of brownish lipochrome pigment in the cyto-
(4) Tumor emboli in the lymphatic vessels. The problem with these criteria is that cellular atypia
and mitotic activity are found to a greater or lesser de- gree in benign interstitial cell tumors as well and, there- fore, have little prognostic value in determining the fu- ture behavior of a particular tumor. Warren and O l ~ h a u s e n ~ ~ have described local invasion in “benign” interstitial tumors, but Silverberg”6 feels that these tumors with invasion of the capsule, epididymis, lymphatic and vascular channels, or spermatic cord would have probably proven to be malignant if they had not been resected. It is our opinion that lymphatic and local invasion is a presumptive sign of malignancy.
The initial treatment for malignant interstitial cell tumor of the testis is orchiectomy. However, due to the small number of reported cases in the literature, there is no consensus as to which mode of therapy is most efficacious after the initial orchiectomy . Five cases were treated unsuccessfully with radiation as the pri- mary therapy for relapse. 1 6 7 2 6 3 3 s , 3 7 , 4 0 Both our patients received radiotherapy to the primary tumor also with- out an objective response, as measured by chest roent- genogram and CAT scan.
Two patients underwent surgical intervention for relapse with apparent success. 1 7 3 2 R Lockhard reported a patient who had a bilateral radical retroperitoneal lymphadenectomy two months after orchiectomy be-
plasm.

No. 2 MALIGNANT LEYDIC CELL CARCINOMA . Davis et al. 429
TABLE 2. Endocrine Studies: Case 2
De xamet hasone Fluoxymestrone Basal levels HCG stimulation suppression suppression
Urinary steroidsi24 hours 17-ketosteroids 17-hydroxysteroids
Plasma steroids Testosterone Androstenedione Dehydroepiandrosterone sulfate Hydroxyprogesterone’ Estrone Estradiol
FSH LH Prolactin ACTH Cortisol
Plasma pituitary hormones
365.0 13.7
2148.0 465.0 560.0 301.0
1.5.4 23.6
<5.0 <5.0 62.5 62.8 18.4
610.0 20.2
3740.0 888.0 942.0 497.0
27.6 39.8
<S
78.4 46.4 14.2
-
419.0 9.3
2519.0 610.0 597.0 273.0
12.6 19.7
i s . 0 6 . 0 42.2
<5.0 <5.0
284.0 15.0
1746.0 524.0 408.0 282.0
18.4 24.6
C5.0 <5.0 so. I 71.0 11.6
* Normal-’IS- IS0 ng/dl.
cause of a small filling defect in one node on the lymph- an~i0gram.I~ Pathologic examination confirmed the suspicious node. The patient, at the time of the report, had been followed for only six months, so the efficacy of this mode of therapy cannot be evaluated at this time. Parker reported a case of a man who presented with gynecomastia and three pulmonary nodules eight years after orchiectomy.2s The patient underwent lingu- lectomy and wedge resection of the posterior basal segment of the left lower lobe and survived nine more years with no evidence of metastatic disease at the time of death.
Six patients received chemotherapy as the therapy for metastatic disease.’.L3.L9.25 Vincristine, cyclophos- phamide, methotrexate, actinomycin-D, and predni- sone as single agents or in combination failed to evoke a tumorcidal response. 1~13~16~19,25~37 An apparent response to chemotherapy occurred with a patient who was admitted three years postoperatively with jaundice, as- cites, and pedal edema.’ Laparotomy revealed unre- sectable abdominal metastases. The patient received o,p’-DDD, along with dexamethasone over the course of several months. The jaundice and the distended abdominal veins disappeared and the “liver decreased in size.” Sixteen months later he developed a soft tissue metastases which, according to the author, responded to increased doses of o,p’-DDD; the liver continued to increase in size, however, and the patient died four months later. Remissions have been reported with o,p’- DDD in some cases of Cushing’s syndrome and in adrenocortical carcinoma. The rationale for using o,p’-DDD in Leydig cell carcinoma is based on the fact that the tumor is similar to virilizing adrenocortical carcinoma in its hormone excretion pattern. This similarity in steroid biosynthetic patterns would be
expected since both the testis and adrenal cortex arise from the mesenchymal cells of the coelomic epithelium lining the posterior abdominal wall. Even with maximally tolerated o,p‘-DDD doses, no tumor reduction was seen in both our patients.
It is obvious that multimodal chemotherapeutic regi- mens used in our patients were unsuccessful in evoking a response despite the fact that cis-platinum regimens have recently shown to be highly efficacious in the treatment of germ cell tumors of the testis. We are not aware of the previous use of cis-platinum in Leydig cell carcinomas. Similarly, vinca alkaloids, cyclosphamide, and doxorubicin proved to be totally ineffectual.
It is apparent, from an extensive literature review, that irradiation as adjunctive therapy provides only symptomatic relief with minimal demonstrable regres- sion of disease. Similarly, chemotherapy also appears to offer little benefit in metastatic disease. The relatively slow growth of the tumor and its refractoriness to ther- apy suggests to us that the most rational approach to the therapy of Leydig cell tumors in adults would be orchiectomy and retroperitoneal lymphadenectomy even if malignant potential cannot be ascertained. Lymphadenectomy offers little surgical risk but accur- ately stages the disease while removing tumor-bearing nodes. If metastases are demonstrated, adjunct radio- therapy appears warranted for its possible efficacy in residual microscopic disease. Surgical resection also appears to offer the best therapeutic alternative to bulk recurrent disease.
Endocrinologic investigation of patients with meta- static Leydig cell tumors are quite limited. Lipsett el al. l4 have performed the most detailed study of a patient with this disease. Their work indicated this tumor re- sembled a virilizing adrenocortical carcinoma. Their

430 CANCER January 15 1981 VOl. 47
patient had high serum T levels, high T production rates, and increased urinary T. Using isotopic studies, it was suggested that DHEAS was the source of practi- cally all the T and thus very little T was actually being secreted by the tumor. In addition, this patient had in- creased 17-KS, A,5 steroid, andestrogen excretion in the urine. The tumor responded to HCG, but was not sup- pressed with fluoxymesterone.
Other studies of malignant Leydig cell tumors have not been as detailed. In general, urinary 17-KS are in- creased but have been found normal in two c a s e ~ . ' ~ - ~ ~ Serum T has been found to be normal in the case reports of Lockhart" and Ober,2s whereas it was elevated in the case of Lipsett et a / . Urinary estrogens have generally been increased when they have been measured, and gynecomastia has been present in 25% of patients with increased urinary estrogens.
The present report revealed two strikingly different steroidal profiles. In patient I , there was very high serum A, moderately high levels of DHEAS and estrone, minimally elevated E, levels, and a low plasma T value with a normal dialyzable fraction. Pituitary gonado- tropins were slightly elevated. Urinary 17-KS and 17- HS and plasma cortisol were normal. This hormonal pattern resembles that seen in patients with congenital absence of 17-hydroxysteroid dehydrogenase and sub- sequent male pseudohermaphroditism. These patients have markedly elevated serum levels of A , elevated LH and El levels, and low T.10.11,3' These criteria have been fulfilled in our Case 1 with metastatic Leydig cell tumor. The ratio of T:A in normal men is 4: I . After HCG, this ratio is further exaggerated in favor of T.4' In Case 1 , the basal T:A ratio was l:lO, which decreased to 1:15 following HCG; this reduction is in keeping with a par- tial enzyme defect. A detailed analysis of the endocrine data has been published elsewhere.'
In patient 2, there were extraordinarily high levels of urinary 17-KS, plasma T, A, DHEAS, HP, El , EP. Pituitary gonadotropins were not detectable. Urinary 17-HS were slightly increased. HCG stimulation caused significant increases in T, A, DHEAS, and HP. The T:A ratio was maintained at approximately 5: l . The hormonal pattern described in this case closely resem- bles that seen in patients with virilizing adrenocortical carcinomaIs and in the case of Leydig cell carcinoma described by Lipsett et al. No tracer studies could be performed so the source of the marked elevation of serum T could not be delineated; however, the elevation of both DHEAS and HP suggests that the tumor was synthesizing increased amount of both A4 and As ster- oids from cholesterol.
Plasma El was modestly elevated in patient I , and E l and E, markedly increased in patient 2. HCG led to increased serum E, in Case 1 , and further increased
both E, and E2 in patient 2. The HCG-induced response could have occurred by direct secretion of estrogens by the tumor or through peripheral conversion of andro- gens. Patient I resembled the pseudohermaphrodite reported by Givens er a f . l o in that he did not have gyne- comastia. The absence of gynecomastia was due to low E, levels. However, patient 2 did show gynecomastia and his E, level was increased sixfold.
To our knowledge, prolactin levels have not been measured in patients with metastatic Leydig cell tumors. Patient 1 had a normal basal serum prolactin level which rose with HCG stimulation. Patient 2 had a high basal prolactin level. The hyperprolactinemia would appear secondary to the secondary elevations in estrogens .
In both our cases, fluoxymesterone did not suppress plasma androgens and estrogens below basal levels. This suggests relative autonomy of steroid production by the Leydig cell neoplasm, yet the capacity to re- spond to HCG was preserved.
REFERENCES
I . Abelson D, Bulaschenko H, Trommer PR, Valdes-Dapena A. Malignant interstitial-cell tumor of the testis treated with o,p'-DDD. Metabolism 1966; 15:242-256.
2. Beds TF, Pierce GB. Schroeder CF. The ultrastructure of human testicular tumors. J Urol 1965; 93( 1):64-73.
3. Chen JC, Zorn EM, Hollberg MC, Wieland RG. Antibodies to testosterone-3-bovine serum albumin, applied to assay of serum 17p- 01 androgens. Clin Chern 1971: 17:581.
4. Chopra I J , Abraham GE, Chopra U, Solomon DH, Odell WD. Circulating estradiol 178 in males with Grave's disease. N Engl J Med 1972; 286: 124.
5 . Collins DH, Cameron Katherine M. Interstitial tumor Er J Urol 1964; 36:62-69.
6. Dalgaard JB . Hesselberg F, Interstitial cell tumors of the testis: Two cases and a survey Acra Pnthol Microbiol Scand 1957; 41:
7. Davis S, DiMartino N A , Schneider G. 17B-hydroxysteroid dehydrogenase deficiency in malignant interstitial cell carcinoma of the testis. J Clin Endorr ind Metnb (In press).
8. Forest MG. Use of highly specific antibodies against 17 hy- droxyprogesterone in a simplified non-chromatographic radioimmuno- assay and in the simultaneous determination of 4 sex hormones. Hormones Rex 1976: 7:260.
9. Gharpure V V . A case of malignant interstitial-cell tumor of the testis in man. J Porhol Eacteriol 1950; 62:113.
10. Givens J R , Wiser WL, Summitt RL, er a / . Familial male pseu- dohermaphroditism without gynecomastia due to deficient testicular 17-ketosteroid reductase activity. N Engl J Med 1974; 291:938.
1 1 . Goebelsman U, Horton R, Mestreran JH. Male pseudoherma- phroditism due to testicules 17B-hydroxysteroid dehydrogenase deficiency. J Clin Endocrinol Metab 1973; 36:867.
12. Kirschner MA. Determination of androgens in biological fluids. In: Rothfield, B, ed. Nuclear medicine in vitro. New York: J.B. Lippincott, 1974:164.
13. Largiader F, Malignant tumor of Leydig's interstitial cells of testis. Frankfurt Z Parhol I%O: 70:630-639.
14. Lipsett MB, Sarfaty GA. Wilson H, Bardin CW, Fishman LM. Metabolism of testosterone and related steroids in metastatic inter- stitial cell carcinoma of the testis. J Clin Invesr 1966; 45: 1700.
15. Lipsett MB. Wilson H. Adenocortical cancer: Steroid bio- syntheses and metabolism evalusted by urinary metabolites. J Clin Endocrinol Metab 1962: 22:906.
219-233.

No. 2 MALIGNANT LEYDIG CELL CARCINOMA ‘ Davis et a / . 43 1
16. Livesay JE, Brance HE, Eaton WL, Interstitial cell carcinoma of the testis: A case report. Am J Roentgenol 1972; 115:728-73 I .
17. Lockhart JL, Dalton DL, Vollmer RT, Glenn JF. Nonfunction- ing interstitial cell carcinoma of testis. Urology 1976; 8(4):392-394.
18. Loriaux DL, Ruder HJ, Lipsett MB. Measurement of estrone sulfate in plasma. Steroids 1971; 18:463.
19. Mahon FB, Gosset F, Trinity RG, Madsen PO. Malignant interstitial cell testicular tumor. Cancer 1973; 31: 1208- 1212.
20. Masson P., Deus cancers Leydigiens de I’homme; leur com- parison avec les tumeurs interstitielles experimentales de la souris. Rev Can B i d 1943: 2:168-243.
21. Midgley AR Jr. Radioimmunoassay: A method for human LH, Endocrinology 1966; 79: 10.
22. Midgley AR Jr. Radioimmunoassay for human FSH. J Clin Endocrinol Metab 1967; 427:295.
23. Nation WF, Edmondson HA, Hammack RW, Interstitial cell tumors of the testis: Report of three new cases. Arch Surg 1944; 48:415 -422.
24. Nieschlag E, Loriaux DL, Lipsett MB. A specific radio- immunoassay for plasma dehydroepiandrosterone. Steroids 1972; 19:669.
25. Ober WB, Kabakon B, Hecht H. Malignant cell tumor of the testis: A problem in endocrine oncology. Bull N Y Acad Med 1976: 52:561.
26. Ohlsen AS, Ronn G . Leydig-cell carcinoma: With report of a case. Acra Chir Scand 1957: (1 12):411.
27. Ogata S. Kaneko R. Malignant tumor of interstitial cells in an intraperitoneal undescended testis with large post-op metastases. Fukuoka Igaku Zasshi 1917; 10:478-497.
28. Parker RG. The treatment of apparent solitary pulmonary metastases. J Thorac Surg 1958; 36:81-87.
29. Peterson RE, Pierce CE. Determination of urinary neutral 17-ketosteroids, In: Sunderman FW, Sunderman FW Jr, eds. Clinical Medicine. Philadelphia: J.B. Lippincott, 1960.
30. Rezek P, Hardin HC. Bilateral interstitial cell tumor of the testicle: Report of one case observed fourteen years. J Urol 1955; 74( 5 ) : 628- 635.
31. Saez JM, De Peretti A, Morera AM. Familial male pseudoher- maphroditism with gynecomastia due to a testicular 17-ketosteroid reductase defect. J Clin Endocrinol Metab 1971; 32:604.
32. Schneider G. Kirschner MA, Berkowitz R, Ertel NH. In- creased estrogen production in obese man. J Clin Endocrinol Merab 1979; 48:633.
33. Scully RE, Cohen RB. Ganglioneuroma of adrenal medulla containing cells morphologically identical to hilus cells (extraparen- chymal Leydig cells). Cancer 1961; 14:421-425.
34. Sharnoff JG, Lisa JR. Malignant tumor of interstitial cells of testis with prostatic carcinoma. J Urol 1943; 50:471-473.
35. Short M, Coe JI. Malignant interstitial cell tumor ofthe testis: A case report. J Urol 1963: 89:851-855.
36. Silverberg SG, Thompson JW, Higashi G, Baskim AM. Malig- nant interstitial cell tumor of the testis: Case report and review. J Urol 1966: 96:356-363.
37. Tamoney HJ, Noriega A. Malignant interstitial cell tumor of the testis. Cancer 1969; 24:547-551.
38. Tedeschi CG, Burke IT. Paratesticular interstitial cell tumor. Cancer 1951: 4:312-318.
39. Warren S, Olshausen KW. Interstitial cell growths of the testicle. A m J Pafhol 1943: 19:307.
40. Ward JS, Krantz S , Mendeloff J , Haltiwanger W. Interstitial- cell tumor of the testis: Report of two cases. ./ Clin Endocrinol Metah 1960: 20: 1622- 1632.
41. Weinstein RL, Kelch RP, Jenner MR, Kaplan SL, Grumbach MM. Secretion of unconjugated androgens and estrogens by the normal and abnormal human testis before and after HCG. J Clin Invest 1974; 53: I .
42. Wilson H. Lipsett MB. Use of periodate oxidation in the clin- ical analysis of urine corticoids. Anal Biochern 1963; 5:214.