Genitourinary System Urinary System for Male & Female Reproductive System for Male.
Male rep. system
-
Upload
markjay-pena -
Category
Health & Medicine
-
view
184 -
download
3
Transcript of Male rep. system
Organs and tissues involved in the production and maturation of
gametes and in their union and subsequent development as
offspring.
Functions of Reproductive
System
• Production of
gametes
• Fertilization
• Development and
nourishment of a
new individual
• Production of sex
hormones
Formation of Gametes
The formation of
gametes in males
and females occurs
by a cell division
called meiosis
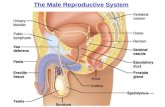
Male Reproductive
System
• Produces and
transfers sperm cells
to the female and
produces hormones
that influence sexual
functions and
behaviors. Consists of
testes, accessory
structures, ducts, and
penis
Scrotum
Sac-like structure
containing the testes
• Dartos Muscle -
Layer of loose
connective tissue
and a layer of
smooth muscle
• Cremaster Muscles
– extensions of
abdominal muscles
into the scrotum
Testes
• Also called Male gonads
• Oval organs, 4-5 cm long, within the scrotum
• Seminiferous tubules –sperm cells develop
• Germ cells – embedded in the sustentacularcells
• Sustentacular cells or Sertoli – large and extended from the periphery to the lumen of seminiferous tubule
• Interstisial cells or LeydigCells – secretes testosterone
Spermatogenesis
Formation of sperm
cells
Spermatogonia –
most peripheral
germ cell
Sperm cell –
contains head,
midpiece, and
flagellum
Ducts
After their production, sperm cells are transported through the seminiferous tubules and series of ducts to the exterior of the body
Rete testis – tubular network where in seminiferous tubule of each testis empties
Efferent ductules – carry sperm cells from the testis to a tightly coiled series of threadlike tubules that form a comma shaped structure on the posterior side of the testis called epididymis
Epididymis – sperm cells continue to mature until the time it can swim and bind to oocytes
Capacitation – occur after ejaculation of semen into the vagina prior to fertilization
Ductus Deferens
Also called vas deferens
45 cm
Contains smooth muscle which contracts in peristaltic waves to propel sperm cells from the epididymis through the ductus deferens
emerges from the epididymis and ascends along the posterior side of the testis to become associated with the blood vessels and nerves that supply the testis which forms the spermatic cord
Seminal vesicle and
ejaculatory duct
Seminal Vesicle – sac shaped gland
Ejaculatory duct – short duct extends from the seminal vesicle to the ampulla of the ductusdeferens join
Urethra – passageway for urine and male reproductive fluids
• Urinary bladder to distal end of the penis• Prostatic urethra
• Membranous urethra
• Spongy urethra
Penis
Male organ of copulation and functions in the transfer of sperm cells from the male to the female
Three columns of erectile tissue:
• Two columns forms the dorsal portion and the sides of the penis and are called corpora cavenosa
• Third column – smaller and occupies the ventral portion of penis and is called corpus spongiosum
• Glans penis – expands over the distal end of the penis to form a cap
• Prepuce – loose fold of skin that covers the glans penis
Glands
The seminal vesicles are glands consisting of many saclike structures located next to the ampulla of the ductus deferens.
Two glands
1. Prostate gland • consists of both glandular and
muscular tissue
• Size and shape of walnut
• Surrounds the urethra and two ejaculatory ducts
• Consists of capsule and numerous partitions
• 10-20 short ducts that carry the secretions of the prostate gland to the prostatic urethra
2. Bulbourethrel glands• Also called as cowper’s
gland
• Pair of small, mucus secreting glands located near the base of the penis
• Size of a pea but they decrease in size with age
• A single duct from each gland enters the urethra
Puberty
• Sequence of events by which a child is transformed into a young adult
• Begins at ages 12-14
• Completed at the age of 18
• Testosterone • Major male hormone secreted
by the testes
• Necessary for spermatogenesis
• Secondary male characteristics• Hair distribution and growth
• Skin texture
• Fat distribution
• Skeletal muscle growth
• Changes in the larynx
Male sexual behavior and
the male sex act
Testosterone is
required for normal
sexual behavior
• Male sex act
• Emission
• Ejaculation
• Orgasm (Climax
• Resolution
Sensory Impulses and
Integration
• Rhythmic massage
of the penis
• Psychic stimuli
• Ejaculation while
sleeping ( Wet
dreaming )
Disorders
(Causes and Treatment)
Erectile Dysfunction (ED)
• Also called Impotence
• Inability to achieve erections
• Caused by reduced testosterone secretion resulting from hypothalamic, pituitary, or testicular complications
• Due to defective stimulation of that erectile tissue by nerve fibers or reduced response of the blood vessels to neutral stimulation
• Can be corrected by taking oral medications such as sildenafil(Viagra), tadalafil (Cialis), or verdanafil (Livitra), or by having specific drugs injected to the base of the penis
• These drugs increases blood flow into the erectile tissue of the penis, resulting in erection for many minutes
Infertility
• Reduced or diminished fertility
• Caused by low sperm cell count due to damage in the testes as a result of trauma, radiation, cryptorchidism or infections such as mumps, which blocks the ducts in the epididymis
• Also caused by inadequate secretion of luteinizing hormone and follicle-stimulating hormone
• Fertility can be achieved by collecting several ejaculations, concentrating the sperm cells and inserting them into the female’s reproductive tract, a process called artificial insemination
Reference: Seeley’s Essentials of Anatomy and Physiology, Eight Edition