MAJOR REVIEW - Keratoconus Home Page -
Transcript of MAJOR REVIEW - Keratoconus Home Page -
297
MAJOR REVIEW
SURVEY OF OPHTHALMOLOGY
VOLUME 42
•
NUMBER 4
•
JANUARY–FEBRUARY 1998
© 1998 by Elsevier Science Inc. 0039-6257/98/$19.00All rights reserved. PII S0039-6257(97)00119-7
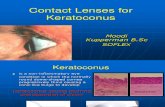
Keratoconus
YARON S. RABINOWITZ, MD
Cornea-Genetic Eye Medical Clinic, Burns and Allen Research Institute, Cedars-Sinai Medical Center and the Department of Ophthalmology, UCLA School of Medicine, Los Angeles, California, USA
Abstract.
Keratoconus is a bilateral noninflammatory corneal ectasia with an incidence of approxi-mately 1 per 2,000 in the general population. It has well-described clinical signs, but early forms of thedisease may go undetected unless the anterior corneal topography is studied. Early disease is now bestdetected with videokeratography. Classic histopathologic features include stromal thinning, iron depo-sition in the epithelial basement membrane, and breaks in Bowman’s layer. Keratoconus is most com-monly an isolated disorder, although several reports describe an association with Down syndrome,Leber’s congenital amaurosis, and mitral valve prolapse. The differential diagnosis of keratoconusincludes keratoglobus, pellucid marginal degeneration and Terrien’s marginal degeneration. Contactlenses are the most common treatment modality. When contact lenses fail, corneal transplant is the bestand most successful surgical option. Despite intensive clinical and laboratory investigation, the etiologyof keratoconus remains unclear. Clinical studies provide strong indications of a major role for genes inits etiology. Videokeratography is playing an increasing role in defining the genetics of keratoconus,since early forms of the disease can be more accurately detected and potentially quantified in a repro-ducible manner. Laboratory studies suggest a role for degradative enzymes and proteinase inhibitorsand a possible role for the interleukin-1 system in its pathogenesis, but these roles need to be moreclearly defined. Genes suggested by these studies, as well as collagen genes and their regulatory prod-ucts, could potentially be used as candidate genes to study patients with familial keratoconus. Such stud-ies may provide the clues needed to enable us to better understand the underlying mechanisms thatcause the corneal thinning in this disorder. (
Surv Ophthalmol 42
:297–319, 1998. © 1998 by ElsevierScience Inc. All rights reserved.)
Key words.
collagen genes
•
contact lenses
•
corneal thinning disorder
•
genetics
•
keratoconus
•
penetrating keratoplasty
•
segregation analysis
•
videokeratography
In 1984 a review on keratoconus and related non-inflammatory corneal thinning disorders by Krach-
mer et al
66
was published in this journal. It remainsone of the most comprehensive and complete clini-cal descriptions on this subject. In the past 14 years,computer technology and biotechnology have had amajor impact in improving our understanding ofkeratoconus and may ultimately allow us to devise amedical therapy to retard its progression. Computer-assisted videokeratoscopes are now used in clinicalpractice, and videokeratography has enhanced our
ability to detect early keratoconus in a quantifiableand reproducible manner. This will allow us to accu-rately construct family pedigrees with the familialforms of keratoconus. Biotechnology may allow usto identify a gene or genes that play a major role inthe pathogenesis of this disorder. This review fo-cuses on these advances as they relate to our under-standing of keratoconus and provides an update onbiochemical and clinical research studies and man-agement options developed since the last majorclinical review.
66
298 Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
I. Epidemiology
Keratoconus, classically, has its onset at pubertyand is progressive until the third to fourth decade oflife, when it usually arrests. It may, however, com-mence later in life and progress or arrest at any age.Rarely it may be congenital.
134
It is most commonly anisolated condition, despite multiple singular reportsof coexistence with other disorders (Table 1). Com-monly recognized associations include Down syn-drome, Leber’s congenital amaurosis, and connectivetissue disorders. For example, patients with advancedkeratoconus have been reported to have a high inci-dence of mitral valve prolapse (58%).
66,129
Atopy , eyerubbing, and hard contact lenses have also been re-ported to be highly associated with this disorder, and6–8% of reported cases have a positive family historyor show evidence of familial transmission (Table 2).
50,66
The reported incidence of keratoconus varies,with most estimates being between 50 and 230 per100,000 in the general population (approximately 1per 2,000). Prevalence is 54.5 per 100,000.
27,35,55
,
60,66
The variability in the reported incidence reflects thesubjective criteria often used to establish the diagno-sis, allowing subtle forms to be often overlooked.Keratoconus occurs in all ethnic groups with nomale or female preponderance.
II. Clinical Features
Keratoconus is a condition in which the cornea as-sumes a conical shape as a result of noninflamma-tory thinning of the corneal stroma. The cornealthinning induces irregular astigmatism, myopia, andprotrusion, leading to mild to marked impairmentin the quality of vision.
66
It is a progressive disorder
TABLE 1
Diseases Reported in Association With Keratoconus
Multisystem Disorders Ocular Disorders (Noncorneal)Alagille’s syndrome
116
Aniridia
63
Albers-Schonberg disease
40
Anetoderma and bilateral subcapsular cataracts
13
Angleman syndrome
75
Ankyloblepharon
15
Apert’s syndrome
44
Bilateral macular coloboma
39
Autographism
57
Blue sclerae
49
Anetoderma
13
Congenital cataracts
64
Bardet-Biedl syndrome
37
Ectodermal and mesodermal anomalies
68
Crouzon’s syndrome
95,160
Floppy eyelid syndrome
87
Down syndrome
24
Gyrate atrophy
64
Ehlers-Danlos syndrome
69
Iridoschisis
29
Goltz-Gorlin syndrome
162
Lebers congenital amaurosis
30
Hyperornithemia
63
Persistent pupillary membrane
63
Icthyosis
35
Posterior lenticonus
16
Kurz syndrome
164
Retinitis pigmentosa
35
Laurence-Moon-Bardet-Biedl syndrome
149
Retinal disinsection syndrome
127
Marfan’s syndrome
6
Retrolental fibroplasia
74
Mulvihil-Smith syndrome
114
Vernal conjunctivitis
48
Nail patella syndrome
49
Corneal DisordersNeurocutaneous angiomatosis
38
Atopic keratoconjunctivitis
48
Neurofibromatosis
149
Axenfeld’s anomaly
135
Noonan’s syndrome
125
Avellino’s dystrophy
121
Osteogenesis imperfecta
8
Chandler’s syndrome
43
Oculodentodigital syndrome
49
Corneal amyloidosis
63
Pseudoxanthoma elasticum
149
Deep filiform corneal dystrophy
63
Rieger’s syndrome
49
Essential iris atrophy
11
Rothmund’s syndrome
62
Fleck corneal dystrophy
63
Tourette’s disease
32
Fuchs corneal dystrophy
73
Turner’s syndrome
91
Iridocorneal dysgenesis
5
Xeroderma pigmentosa
12
Lattice dystrophy
54
Other Systemic Disorders Microcornea
63
Congenital hip dysplasia
90
Pellucid marginal degeneration
59
False chordae tendinae of left ventricle
64
Posterior polymorphous dystrophy
26
Joint hypermobility
117
Terriens marginal degeneration
63
Mitral valve prolapse
129
Measles retinopathy
94
Ocular hypertension
10
Thalesselis syndrome
138
Reference numbers in superscript.
KERATOCONUS
299
ultimately affecting both eyes, although only one eyemay be affected initially.
71,105
Symptoms are highly variable and, in part, dependon the stage of the progression of the disorder. Earlyin the disease there may be no symptoms, and kera-toconus may be noted by the ophthalmologist simplybecause the patient cannot be refracted to a clear20/20 corrected vision. In advanced disease there issignificant distortion of vision accompanied by pro-found visual loss. Patients with keratoconus fortu-nately never become totally blind from their disease.
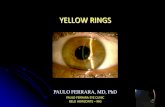
Clinical signs also differ depending on the severityof the disease (Table 2). In moderate to advanceddisease any one or combination of the followingsigns may be detectable by slit-lamp examination ofthe cornea: stromal thinning (centrally or paracen-trally, most commonly inferiorly or inferotemporally[Fig. 1A]); conical protrusion; an iron line partiallyor completely surrounding the cone (Fleischer’sring); and fine vertical lines in the deep stroma andDescemet’s membrane that parallel the axis of thecone and disappear transiently on gentle digitalpressure (Vogt’s striae [Fig. 2]). Other accompany-ing signs might include epithelial nebulae, anteriorstromal scars, enlarged corneal nerves, and in-creased intensity of the corneal endothelial reflexand subepithelial fibrillary lines.
66,80
Munson’s sign and Rizzuti’s sign are also useful ad-junctive external signs associated with keratoconus.
80
Munson’s sign is a V-shaped conformation of thelower lid produced by the ectatic cornea in downgaze.Rizzuti’s sign is a sharply focused beam of light nearthe nasal limbus, produced by lateral illumination ofthe cornea in patients with advanced keratoconus.
Patients with advanced disease may occasionallypresent with a sudden onset of visual loss accompa-nied by pain. On slit-lamp examination the conjunc-tiva may be injected and a diffuse stromal opacity isnoted in the cornea. This condition, referred to as“hydrops,” is caused by breaks in Descemet’s mem-brane with stromal imbibition of aqueous throughthese breaks (Fig. 3A). The edema may persist forweeks or months, usually diminishing gradually, withrelief of pain and resolution of the redness and cor-
TABLE 2
Signs of Keratoconus
External signsMunson’s signRizzuti phenomenon
Slit-lamp findingsStromal thinningPosterior stress lines (Vogt’s striae)Iron ring (Fleischer ring)Scarring—epithelial or subepithelial
Retroillumination signsScissoring on retinoscopyOil droplet sign (“Charleaux”)
Photokeratoscopy signsCompression of mires inferotemporally
(“egg-shaped” mires)Compression of mires inferiorly or centrally
Videokeratography signsLocalized increased surface powerInferior superior dioptric asymmetryRelative skewing of the steepest radial axes above and
below the horizontal meridian (Fig. 6)
Fig. 1. Ectatic dystrophies, the arrows point to the areasof maximal thinning. Top: Keratoconus-paracentral cor-neal thinning. Center: Pellucid marginal degeneration-inferior thinning from 4 to 8 o’clock. Bottom: Keratoglo-bus: thinning of the whole cornea from limbus to limbus.
300 Surv Ophthalmol 42 (4) January–February 1998
RABINOWITZ
neal edema ultimately being replaced by scarring(Fig. 3B).
Early in the disease process the cornea may ap-pear normal on slit-lamp biomicroscopy; however,there may be slight distortion or steepening ofkeratometry mires centrally or inferiorly. In such in-stances it is useful to dilate the pupil. Retroillumina-tion techniques and scissoring of the retinoscopic re-flex or the “Charleux” oil droplet sign are usefulclinical signs to confirm the diagnosis in suspiciouscases.
102
In these early cases, where the cornea ap-pears normal but keratoconus is suspected, measur-ing the anterior topography of the central and para-central cornea is also extremely useful to confirmthe diagnosis.
66
Several devices are currently available for detect-ing early keratoconus by measuring anterior cornealtopography. These range from simple inexpensivedevices, such as handheld keratoscopes (placidodisks), to expensive sophisticated devices, such ascomputer-assisted videokeratoscopes. With the hand-held keratoscopes, such as the Klein keratoscope,early keratoconus is characterized by a downwarddeviation of the horizontal axis of the Placido diskreflection (Fig. 4).
3,4
Until recently, nine-ring photo-keratoscopes, such as the Corneascope (Kera Corpo-ration, Santa Clara, CA), were commonly used bycornea specialists. With this device early keratoconusis depicted by compression of the mires inferiorly orinferotemporally
120
(Fig. 5).Computer-assisted videokeratoscopes, which gen-
erate color-coded maps and topographic indices, arecurrently the most sensitive and sophisticated de-vices for confirming the diagnosis of keratoconus.(A more detailed discussion is provided in “V. Topo-graphic Studies of Keratoconus.”
78
) With such de-vices, keratoconus appears as an area of increasedsurface power surrounded by concentric zones ofdecreasing surface power. Three features are com-mon to keratoconus videokeratographs that use sag-
Fig. 2. Vogt’s striae in a patient with keratoconus locatedat the level of Descemet’s membrane noted on slit-lampexamination of the cornea. (Courtesy of Stephen Orlin, MD.)
TABLE 3
Collagens in the Cornea and Their Chromosomal Location
CollagenType Chain Gene
ChromosomalLocation
I alpha 1 (I)
COL1A1
17q21-q22alpha 2 (I)
COL1A2
7q21-q22III alpha 1 (III)
COL3A1
2q31-q32IV alpha 1 (IV)
COL4A1
13q33-q34alpha 2 (IV)
COL4A2
13q33-q34alpha 3 (IV)
COL4A3
2alpha 4 (IV)
COL4A4
2alpha 5 (IV)
COL4A5
XV alpha 1 (V)
COL5A1
2q31-q32alpha 2 (V)
COL5A2
9palpha 3 (V)
COL5A3
2q31-q32VI alpha 1 (VI)
COL6A1
22qalpha 2 (VI)
COL6A2
22qalpha 3 (VI)
COL6A3
6VII alpha (VII)
COL7A1
3qVIII alpha 1 (VIII)
COL8A1
3alpha 2 (VIII)
COL8A2
1
Fig. 3. Acute hydrops. Top: Stromal opacity as a resultof corneal edema noted on initial presentation. Bottom:Resolution of the hydrops with resultant corneal scarringin the same patient 6 months later.
KERATOCONUS
301
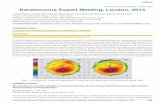
ittal topography, a localized area of increased sur-face power, inferior-superior power asymmetry, andskewed steep radial axes above and below the hori-zontal meridian (depicting irregular astigmatism,the hallmark of keratoconus [Fig. 6]).
103,156
Ultrasonic pachymetry may be useful to confirm
corneal thinning in patients with suspected kerato-conus on slit-lamp examination or videokeratogra-phy; however, it cannot be solely relied on to makethe diagnosis because of the large range and varia-tion of pachymetry readings both centrally and para-centrally in the normal population.
112
III. Histopathology
Thinning of the corneal stroma, breaks in Bow-man’s layer, and deposition of iron in the basal lay-
ers of the corneal epithelium comprise a triad of theclassical histopathologic features found in keratoco-nus (Fig. 7). Depending on the stage of the disease,every layer and tissue of the cornea can, however, be-come involved in the pathological process. Fine de-tails of these processes are most clearly appreciatedby electron microscopy.
The epithelium may show degeneration of itsbasal cells, breaks accompanied by downgrowth ofepithelium into Bowman’s layer, particles within athickened subepithelial basement membranelikelayer and between basal epithelial cells, and accumu-lation of ferritin particles within and between epi-thelial cells most prominently in the basal layer ofthe epithelium. Histopathologic features detected inBowman’s layer may include breaks filled by erup-tions of underlying stromal collagen, periodic acidSchiff–positive nodules, and Z-shaped interrup-tions, possibly due to separation of collagen bundlesand reticular scarring. Features noted in the stromaare compaction and loss of arrangement of fibrils inthe anterior stroma, decrease in the number of col-lagen lamellae, normal and degenerating fibroblastsin addition to keratocytes, and fine granular and mi-crofibrillar material associated with the keratocytes.
66
Descemet’s membrane is rarely affected exceptfor breaks seen in acute hydrops. The endotheliumis usually normal. However, some abnormalities havebeen reported, including intracellular “dark struc-tures,” pleomorphism, and elongation of cells withtheir long axis toward the cone. Gross histopatho-logic analysis of corneal buttons undergoing pene-trating keratoplasty for keratoconus has revealed thepresence of two types of cone morphology: “nipple”-
Fig. 4. Photographic placido disk images used by Amsler. Left: Normal cornea. Right: Deflection of the horizontal merid-ian labeled as keratoconus “fruste.”
Fig. 5. Egg-shaped mires or inferotemporal steepeningdetected with the Corneascope (nine-ring photokerato-scope) in a patient with early keratoconus.
302 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
type cones, located centrally, and “oval”-(sagging)type cones, located inferiorly or inferotemporally.96
These types of cones often can be distinguished onslit-lamp examination or evaluation of the anteriorcorneal topography in keratoconus patients.
Histopathologic examination of corneal buttonsin patients who have had acute hydrops reveals stro-mal edema. Descemet’s membrane separates fromthe posterior surface and retracts into scrolls, ledges,or ridges. During the repair process, corneal endo-thelium extends over the anterior and posterior sur-faces of the detached Descemet’s membrane anddenuded stroma: endothelial integrity is usually re-established 3–4 months after the acute event.136
IV. Etiology and PathogenesisA. ASSOCIATED DISORDERS
Keratoconus has been reported in various clinicalsettings. It may be an isolated sporadic disorder, or itmay be associated with other rare genetic disorders,with Down syndrome and Leber’s congenital amau-rosis, with connective tissue disorders, with hardcontact lens wear and eye rubbing, and with a posi-tive family history of the disorder.53,66,83,84 These asso-ciations, however, require critical evaluation.
By far the most common presentation of keratoco-nus is as an isolated sporadic disorder with no otherassociated systemic or ocular disease detectable byclinical evaluation. Of 300 consecutive keratoconuspatients screened for a genetic research study at theCedars-Sinai Medical Center in Los Angeles, 2 (0.6%)had Down syndrome, 2 (0.6%) had neurofibromato-sis, and 296 (99%) were isolated with no associatedgenetic disease.
Table 1 summarizes conditions reported to be as-sociated with keratoconus. For the most part, theseassociations should be considered to have occurredby chance. For example, the incidence of keratoco-nus is 1 per 2,000 and the incidence of neurofibro-matosis type 1 is 1 per 4,000 in the general popula-tion; thus, there is a 1 in 8,000,000 chance that thesetwo disorders would occur together (30 potentialcases in the USA). Rare associations with keratoco-nus are important, particularly if they occur as a re-sult of a chromosomal translocation; if the associ-ated disorder cosegregates with keratoconus it mightprovide clues as to the chromosomal location of theinherited form of keratoconus. Therefore, it isworthwhile to perform cytogenetic studies in pa-tients who have mental retardation or rare genetic
Fig. 6. Top: Keratoconus videokerato-graph (TMS-1 videokeratoscope) dem-onstrating the three classical pheno-typic features of keratoconus (usingsagittal topography): central steepen-ing, inferior-superior dioptric asymme-try, and skewing of the steepest radialaxes above and below the horizontalmeridian. Bottom: Diagram illustrat-ing calculation of the SRAX index thatquantifies the skewing of these radialaxes.
KERATOCONUS 303
disorders attributed to chromosomal translocationsand associated with keratoconus.
Down syndrome has been reported to have a highassociation with keratoconus, with reported inci-dence ranging from 0.5% to 15% (i.e., 10–300 timesmore common than in the general popula-tion).24,66,128 Similarly, there is a high incidence ofkeratoconus in patients with Leber’s congenitalamaurosis (up to 30% of patients older than 15years).2 The frequent occurrence of keratoconus hasbeen attributed to a high incidence of eye rubbing
in these two disorders, owing to increased blephari-tis in Down syndrome and an oculo-digital sign inLeber’s congenital amaurosis. However, a recentstudy of children in a school for the blind by Elder30
contradicts this theory and suggests that the associa-tion with keratoconus might be due to genetic fac-tors rather than eye rubbing.
Several reports suggest an association betweenkeratoconus and connective tissue disorders.58,62,83,
84,117 This is based on rare reports of associations ofkeratoconus with disorders of collagen metabolism,such as Osteogenesis Imperfecta and subtypes ofEhlers-Danlos syndrome, and on a study that re-ported joint hypermobility in 22 of 44 (50%) kerato-conus patients. Two recent studies, however, disputethis high association of joint hypermobility, one byan Emory University (Atlanta, GA) group137 and oneby our group at the Cedars-Sinai Medical Center. Inour study 34 of 218 (15%) keratoconus patientscompared to 10 of 183 (12%) normal age-matchedcontrols had joint hypermobility (not statistically sig-nificant (P 5 0.304).141 Other compelling evidencein support of a connective tissue abnormality in kera-toconus does, however, exist, based on two reports ofan association between patients with advanced kerato-conus and mitral valve prolapse—a 1982 study byBeardsley and Foulks7 and a more recent study bySharif et al,129 which suggests that 58% of keratoco-nus patients requiring surgery have mitral valve pro-lapse versus 7% of normal controls.
Mechanical trauma has also been implicated inthe pathogenesis of keratoconus. Although a num-ber of studies report a high association of eye rub-bing with keratoconus, a cause-and-effect relation-ship is difficult to prove.66 A recent preliminary studyat our institution, however, suggests that keratoco-nus patients do rub their eyes more often than nor-mal controls (174 of 218 [80%] versus 106 of 183[58%] [P , 0.001]).141 Contact lenses are also sug-gested as a source of mechanical trauma related tokeratoconus.42,53,66 Because early in the disease pro-cess patients have mild myopic astigmatism with clin-ically normal-looking corneas and their vision is bestcorrected with rigid contact lenses, it is extremelydifficult to determine which came first, the keratoco-nus or contact lens wear. In none of the reports cit-ing these associations were topographic studies per-formed prior to contact lens fitting to determinewhether the patients had early disease before wear-ing contact lenses. It is possible that mechanicaltrauma induced by eye rubbing and hard contactlens wear act as environmental factors that enhancethe progression of the disorder in genetically predis-posed individuals.
Atopy is often cited as being highly associated withkeratoconus. A review of the literature reveals con-
Fig. 7. Classical histopathologic features seen in kerato-conus. Top: Stromal thinning with folding artifact com-monly seen in thinned corneas. (Courtsey of Joseph Sas-sani, MD.) Center: Breaks in Bowman’s layer (arrow).(Courtesy of Gordon Klintworth, MD.) Bottom: Deposi-tion of iron in the basal epithelium (arrow). (Courtesy ofJoseph Sassani, MD.)
304 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
flicting data in favor of and against this associa-tion.66,87,113,147 In a study conducted at our institution,96 of 218 (44%) keratoconus patients had a historyor symptoms of allergic disorders versus 66 of 183(36%) normal age-matched controls (not statisti-cally significant, P 5 0.105)141
B. BIOCHEMICAL STUDIES
Despite intensive biochemical investigation intothe pathogenesis of keratoconus, the underlying bio-chemical process and its etiologic basis remainpoorly understood. Corneal thinning appears to re-sult from loss of structural components in the cor-nea, but why this occurs is not clear. Theoretically,the cornea can thin because it has fewer collagenlamellae than normal, fewer collagen fibrils perlamella, closer packing of collagen fibrils, or variouscombinations of these factors. These conditions mayresult from defective formation of extracellular con-stituents of corneal tissue, a destruction of previouslyformed components, an increased distensibility ofcorneal tissue with sliding collagen fibers or collagenlamellae, or a combination of these mechanisms.63
Early biochemical studies demonstrated that col-lagen composition in corneas with keratoconus wasunaltered.163 Recent biochemical assays and immu-nohistological studies of corneas with keratoconussuggest that the loss of corneal stroma after diges-tion by proteolytic enzymes could be caused by in-creased levels of proteases and other catabolicenzymes123 or decreased levels of proteinase inhibi-tors.41 Observations of corneal a1 proteinase inhibi-tor and a2 macroglobulin (also a major proteinaseinhibitor) confer further support to the hypothesisthat the degradation process may be aberrant inkeratoconus.122 Both inhibitors can be demonstratedimmunohistochemically in the epithelium, stroma,and endothelium of normal and pathologic humancorneas. In contrast to normal corneas and corneaswith other pathologic conditions, the staining inten-sity in the corneal epithelium of keratoconus cor-neas was markedly diminished. This decrease in a2macroglobulin in the cornea and stroma was con-firmed by Western blot assays.122 Another proteinaseinhibitor (TIMP-1) that inhibits matrix metallopro-teinase was found not to contribute to the increasedlevels of gelatinolytic activity noted in prior biochemi-cal studies of the cornea.61,92,133 These proteases andinhibitors require further study to clarify their preciserole in the pathogenesis of keratoconus.
The preceding biochemical findings may merelybe signs of a more generalized keratocyte abnormal-ity in keratoconus.153 Wilson and coworkers demon-strated that the loss of anterior stromal keratocytes,which accompanies corneal epithelial abrasion orsubepithelial ablation, is likely due to apoptotic cell
death.153 They point out that both the corneal epi-thelium and endothelium produce interleukin-1(IL-1) and that keratocytes can be shown to expressthe IL-1 receptor. Interleukin-1 induces keratocytedeath in vitro and negative keratocyte chemotaxis,and it can upregulate hepatocyte and keratinocytegrowth factors.153 It can also regulate the expressionof keratocyte metalloproteinases collagenase andcomplement factors. On the basis of this, IL-1 is pos-tulated to be a modulator of epithelial stromal inter-actions, with a role in the regulation of corneal cellproliferation, differentiation, and death.
Wilson et al have proposed a role for an IL-1 sys-tem in the cornea in the pathogenesis of keratoco-nus.153 It has previously been demonstrated thatkeratocytes from keratoconus corneas have a four-fold greater number of IL-1 receptors than normalcorneas9; Wilson et al suggest that the increased ex-pression of the IL-1 receptor sensitizes the kerato-cytes to IL-1 released from the epithelium or endo-thelium, causing a loss of keratocytes throughapoptosis and a decrease in stromal mass over time.This hypothesis makes sense of the occurrence ofkeratoconus in relation to eye rubbing, contact lenswear, and atopy, if it is presumed that epithelial mi-crotrauma leads to an increased release of IL-1 fromthe epithelium.14 Wilson et al have also suggestedthat abnormalities in the processes that regulate ap-optosis, besides the IL-1 system, could be the causeof keratoconus, even in the absence of epithelial cellinjury.153
C. GENETICS
1. Twin Studies
Although formal genetic analyses using currentmethodology have not been reported for keratoco-nus, review of the published literature providesstrong pointers to suggest genetic influences in thepathogenesis of this disorder. This includes at leasteight reports of its occurrence in both identicaltwins,33,66,93 the bilaterality of the disorder,71,105 thehigh degree of nonsuperimposable mirror imagesymmetry in the location of topographic alterationsbetween two eyes of an individual patient,156 andmultiple reports of its occurrence in family membersin two and three generations.36
Twins have a special place in the study of humangenetics because of their usefulness in comparingthe effects of genes and environment. The impor-tance of twin studies for comparison of the effects ofnature and nurture was originally pointed out byGalton in 1875.139 Diseases caused wholly or partly bygenetic factors have a higher concordance rate inmonozygotic twins than in dizygotic twins. In situa-tions where a condition does not show a simple ge-netic pattern, comparison of its incidence in
KERATOCONUS 305
monozygotic and dizygotic twin pairs can reveal thatheredity is involved; moreover, if monozygotic twinsare not fully concordant for a given condition, non-genetic factors must also play a part in its etiology.
Nine cases of keratoconus in monozygous twinshave been reported in the literature; in all instancesbut one, both twins had keratoconus. In the onewho did not have keratoconus, videokeratographyhad not been performed. We have observed at leasttwo sets of twins in which one had clinical keratoco-nus while the other was affected only as shown byvideokeratography, and two sets of dizygotic twins inwhich one was affected and the other normal asshown both clinically and by videokeratography.These observations present very strong support forgenetic influences in keratoconus; however, a formalprospective twin study comparing monozygotic ver-sus dizygotic twins without ascertainment bias is nec-essary to confirm the conclusions drawn from suchobservations.21,139
2. Family Studies
Several large series, including our own study atCedars-Sinai Medical Center, have reported a posi-tive family history in 6–10% of patients with kerato-conus.51,141 The majority of reported studies sug-gested an autosomal dominant mode of inheritancewith variable expression and included subtle formsof the disorder, such as keratoconus fruste or mildirregular astigmatism, in order to resolve the modeof inheritance. At least 74 such instances have beenreported in the ophthalmic literature: 21 cases citedby Falls and Allen,34 including one by Falls; 24 casesexamined by Ihalainen in a Finnish study;56 and 10families examined by Hammerstien.51 In Hammer-stien’s study of 52 families, keratoconus was detectedin 2 or more relatives in 10 of the families (19%).The degree of penetrance was approximately 20%.The disease was characterized by complete pene-trance and variable expressivity. Seven pedigreeswere reported by Redmond,115 who suggested thatkeratoconus fruste and high degrees of astigmatismrepresent incomplete expression of the keratoconusgene and should be taken into account in pedigreeanalysis. Five families of patients with keratoconuswere reported by Rabinowitz et al,101 who usedvideokeratography to detect abortive forms of thedisorder. In these five families, hereditary patternswere consistent with autosomal dominant transmis-sion with variable expressivity (Fig. 8). Gonzalez andMcDonnell46 detected videokeratographic abnor-malities in at least one parent of seven sets of clini-cally normal parents of patients with keratoconus.Although there are several reports in the literaturethat suggest recessive inheritance,36 none show clearevidence that three generations were examined or
that subtle forms of the disorder were sought for in-clusion in the pedigree analysis.
3. Formal Genetic Analyses
Although most studies suggest a dominant modeof inheritance, formal genetic analyses are neededto accurately define hereditary patterns for varioussubtypes of keratoconus and elucidate the role ge-netic influences may play in its pathogenesis. Formalgenetic analyses of a disease or trait are used to testwhether there is a significant genetic influence inthe etiology of the disease and to identify both themodes of inheritance of any responsible genes andtheir locations in the human genome. In a geneticanalysis, the first question to be investigated iswhether familial aggregation is the result of geneticfactors.
a. Molecular Genetic Studies
Once genetic factors have been established, thegoal of further analysis is to investigate the numberof genes that influence the disease (one, two, ormany), the relative contribution of each of the genesto the development of the disease, the mode of in-
Fig. 8. Family pedigrees of subjects studied with video-keratography. Subtle topographic abnormalities in clini-cally normal family members detectable by videokeratogra-phy only suggests a hereditary pattern consistent withautosomal dominance and variable expression. (Reprintedfrom Rabinowitz et al101 with permission of the AmericanMedical Association.)
306 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
heritance of the genes, the presence or absence ofgenetic heterogeneity (one or more diseases with asimilar phenotype), and the chromosomal locationof the gene(s). Such information has not yet for-mally been attained for keratoconus, but with therapid development of molecular and statisticalmethods, these goals are now achievable and arecurrently being pursued at our institution.21,110
Segregation analysis is a statistical method used toevaluate the mode of inheritance of a trait or dis-ease.21,31,86 A particular mode of inheritance is postu-lated for the disease, and data on the presence or ab-sence of the disease are collected from families withaffected members. These data are used to testwhether the expression of the disease is consistentwith the proposed mode of inheritance. The vari-ables analyzed in classic segregation analysis are thepresence or absence of disease, which can be basedon a qualitative or discrete (quantitative) trait. Qual-itative criteria for diagnosis of keratoconus includecorneal thinning, Vogt’s striae, Fleischer rings, andscissoring of the retinoscopic reflex with a dilatedpupil. For quantitative traits, for which clear cutoffpoints for affectation status are required and com-plex, segregation analyses using computer programsare preferred because such methods glean more in-formation from the data.21 For discrete cutoff pointsfor diagnosis using quantitative traits, videokeratos-copy indices can be used. To develop these cutoffpoints, a clear, quantifiable, and reproducible defi-nition of early keratoconus by videokeratoscopy inthe absence of clinical signs is necessary. Becausekeratoconus appears to be a complex disorder, notalways following simple mendelian modes of inherit-ance, videokeratoscopy research to provide minimaltopographic criteria for determining affectation sta-tus provides a unique opportunity to determine truemodes of inheritance and ultimately construct pedi-grees for molecular genetic analysis in appropriatefamilies with keratoconus.104 Before expensive mo-lecular studies are undertaken to investigate the he-redity and genetics of keratoconus, several areasmust be clarified through formal analysis. A defini-tion of the disorder must be established. The influ-ence of associated systemic conditions and the effectof mechanical trauma must be determined, and to-pographical changes in contact lens wearers must beidentified.126 After these factors are understood, therelationship of expressivity to age and the potentialheterogeneity of keratoconus can be determined.
Once the early phenotype has been characterizedand segregation analysis has been performed, accu-rate family pedigrees with familial keratoconus canbe constructed. This may open new avenues for in-vestigating the pathobiology of keratoconus throughgene-linkage analysis.23,131 A random marker ap-
proach with polymorphic microsatellite markers or acandidate-gene approach could be used in appropri-ate families to identify a gene locus (or multipleloci) and answer some important questions thathave been suggested by clinical and biochemical ob-servations. Is keratoconus caused by degradative en-zymes, as suggested by biochemical studies? Is therea role for the IL-1 system as previously outlined? Iskeratoconus caused by a structural abnormality ofcollagen or products involved in its regulation, assuggested by clinical observations?
To provide answers to some of the questionsraised by findings in biochemical studies, cDNAs ofthe proteinase inhibitors, proteases, or componentsof the IL-1 system could be used as candidate genesin appropriate linkage studies of appropriate kerato-conus families. Such studies may provide more de-finitive support for their role in the thinning processresulting in keratoconus.
b. Collagen Genes as Candidate Genes
The role of collagen and products involved in itsregulation is receiving intense scrutiny at our institu-tion. The high association of advanced keratoconusand mitral valve prolapse, prior reports of an associa-tion between Osteogenesis Imperfecta, and a recentreport in which keratoconus cosegregates with famil-ial osteogenesis imperfecta in three generationspoints to a genetic abnormality of connective tissuebeing responsible for at least some forms of kerato-conus.8,129 Different subtypes of Osteogenesis Imper-fecta have been shown to be caused by mutations inthe COL1A1 and COL1A2 genes.118 To test the hy-pothesis that some forms of keratoconus may resultfrom a mutation in one of the fibrillar collagens inthe cornea, we are using the complementary DNAsof the fibrillar collagens to study one large familywith autosomal dominant keratoconus, using a can-didate-gene approach.140
The collagens form a multigene family with morethan 28 members, the genes for which are known tobe dispersed to at least 12 chromosomes. As a familyof proteins, the collagens are the most abundant inthe body. The vast majority of collagen in the body istype I collagen, which is ubiquitously distributed andis the major protein in bone, skin, ligament, sclera,cornea, blood vessels, and hollow organs. Mutationsthat affect the structure or processing of the chainsof type I collagen are often expressed as generalized,connective tissue disorders, although the specific tis-sue in which the major effect is seen may vary anddetermines the clinical phenotype. With the excep-tion of types III, V, and VI collagen, which are alsodistributed in virtually all tissues, most other col-lagens have tissue-specific or structure-specific distri-bution.20 Types II, IX, X, and XI are found in hya-
KERATOCONUS 307
line cartilage and the vitreous of the eye, type IVcollagens are found in basement membranes, andtype VII collagen is found at some epithelial-mesen-chymal junctions in anchoring fibril structures. Be-cause of differences in structure, expression, and tis-sue distribution, the collagens perform differentfunctions; in different tissues the same collagen mayperform different functions.20
Collagens throughout the body function in anumber of ways. They provide tensile strength, facili-tate transparency, provide form during embryonicand fetal development, interact with other proteinsto build tissues and organs, separate cell layers dur-ing and after development, and provide filtrationbarriers between spaces. It is likely that some of thefunctions are achieved as a direct result of collagenstructure, while others depend on interactions withadditional matrix macromolecules.20
Collagens type I, III, IV, V, VI, VII, and VIII arescattered throughout different layers of the cornea(Fig. 9). The chromosomal location of the genes en-coding these collagens have been identified (Table3).20,163 These genes thus serve as excellent candi-date genes for studying keratoconus. Their inclusionor exclusion could yield valuable information. Pre-liminary studies at our institution using moleculargenetic approaches have excluded several collagengenes (Table 4). COL1A1 and COL1A2 remain excel-lent candidates and are currently being investigatedin more detail, as are new markers distal to COL6A1and COL6A2 on the telomere of chromosome 21.
4. Summary
Clinical observations, topographic studies, andpreliminary segregation analyses of families of pa-tients with keratoconus suggest that genes play a ma-jor role in the etiology of keratoconus.101,105,106,110 En-vironmental factors such as eye rubbing and hardcontact lens wear may cause progression of this dis-order in genetically susceptible individuals. The het-erogenous nature of the disease suggests that differ-ent genetic subtypes might result from differentmutations and that not all families with keratoconuswill follow classical mendelian patterns of inherit-ance. Despite the fact that to date we have made verylittle progress toward understanding what causeskeratoconus, molecular genetic approaches withDNA markers of families with keratoconus havegreat potential for providing pointers to an underly-ing genetic abnormality that causes the noninflam-matory corneal thinning found in keratoconus. Thismay ultimately lay the foundation for possible genetherapy to retard progression of the disorder inhigh-risk individuals.23,131
V. Topographic Studies of KeratoconusA. PLACIDO DISK STUDIES
In 1938 Marc Amsler, using a photographic plac-ido disk, was the first to describe early corneal topo-graphic changes in keratoconus before clinical orbiomicroscopic signs could be detected. His classicalstudies on the natural history of keratoconus docu-
Fig. 9. Diagram illustrating the distribution of collagens in the cornea.
308 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
mented its progression from minor corneal surfacedistortions to clinically detectable keratoconus. Heclassified keratoconus into clinically recognizablestages and an earlier latent stage recognizable onlyby placido disk examination of corneal topography.These early stages were subdivided into two catego-ries: keratoconus fruste, in which there is a 1–4 degreedeviation of the horizontal axis of the placido disk,and early or mild keratoconus, which has a 4–8 degreedeviation. Only slight degrees of asymmetric obliqueastigmatism could be detected in these early forms.Similar findings were absent in patients with regularastigmatism.3,4
In Amsler’s study of 600 patients, 22% had clini-cally obvious keratoconus in both eyes, 26% hadclinical keratoconus in one eye and latent keratoco-nus in the other, and 52% had latent keratoconus bi-laterally. Progression was highly variable and mostoften asymmetric. The cone could remain station-ary, progress rapidly over 3–5 years, and arrest orprogress intermittently over an extended period oftime. When Amsler reexamined 286 eyes 3–8 yearsafter the diagnosis, only 20% of the entire group, in-cluding 66% of the latent cases, had progressed. Pro-gression was most likely to occur in patients between10 and 20 years of age, decreased slightly betweenages 20 and 30, and was less likely to increase afterage 30.3,4
Levene suggests that instrument tilt or poor align-ment with respect to the corneal plane in hand heldkeratoscopes may result in incorrect interpretationof the deviation of the horizontal axis.72 Reproduc-ibility thus poses a potential problem with this device.
B. PHOTOKERATOSCOPY
The photokeratoscope produces a topographicrecord of 55–80% of the total corneal contour, but itprovides little or no information about the central 3mm of the cornea. Rowsey et al used this instrumentto study keratoconus and its progression in 827 pa-tients.25,120 The earliest sign detected, in the absenceof biomicroscopic signs, was steepening of the infer-otemporal cornea, extending peripherally over time
to involve the inferonasal, superotemporal and, last,the superonasal quadrant.
C. KERATOMETRY
The ophthalmometer (keratometer), which pro-vides information about only 2–3 points approxi-mately 3 mm apart, can detect keratoconus by show-ing distortion of its mires or central or inferiorsteepening. While steep corneas might suggest kera-toconus, there are patients with steep corneas andhigh degrees of regular astigmatism who do nothave keratoconus. Conversely, there are patientswho have keratoconus with normal central cornealcurvatures but irregular astigmatism or inferiorsteepening only. A documented increase in cornealcurvature over time as seen by keratometry is a sensi-tive indicator of keratoconus.66
D. COMPUTER-ASSISTED VIDEOKERATOSCOPY
Over the past 7 years computer-assisted videokera-toscopes have gained rapid acceptance in clinicalpractice.65 Many such devices are currently available,most using placido disk principles, although othertechnologies are rapidly emerging. (For a detaileddiscussion of computer-assisted videokeratoscopes,refer to “Corneal Topography” in The Clinical Atlas,by Lucio Burrato.84a)
The instrument we have used primarily in our to-pography studies is the Topographic Modeling Sys-tem (TMS-1, Computed Anatomy, New York, NY). Itconsists of a placido disk-type nose cone, capturingthe placido disk image into a computer-based sys-tem, which can rapidly analyze data accurately andreproducibly. Both the central and paracentral cor-nea can be measured in one sitting. This device,which uses spherically biased algorithms (sagittal to-pography), has previously been described in detailand has been shown to be highly accurate and repro-ducible on spherical surfaces and in the central twothirds of normal human corneas.47,52,81,159 Topo-graphic data points in polar coordinates using 256radial lines scanning across 25 rings are examinedand approximately 7,000 data points are generated.
TABLE 4
Preliminary Linkage Studies With Collagen Genes as Candidate Genes in Autosomal Dominant Keratoconus104
Two-Point LOD Scores Calculated With LIPED
Keratoconus Z at 0 5versus _______ 0.01 0.05 0.10 0.20 0.30 0.40COL3A1/COL5A2 27.36 22.39 21.58 20.84 20.45 20.19COL2A1 21.81 20.20 0.01 0.12 0.09 0.03GH1/COL1A1* 27.43 22.39 21.55 20.79 20.42 20.19COL6A1/COL6A2 22.35
*GH1 was used as a marker for COL1A1 because there were no good markers for COL1A1 at the time this study was per-formed.
KERATOCONUS 309
A color-coded map that allows easy appreciation ofchanges in the corneal curvature is generated. The25-ring photokeratoscope mires can be superim-posed on the maps for qualitative interpretation,and a series of quantitative indices, including simu-lated keratometry readings, are part of the data out-put.47 Because placido disk–based computer video-keratoscopes, such as the TMS-1, have the combinedfeatures of both a keratometer and photokerato-scope, recording curvature changes in both the cen-tral and paracentral cornea, they are ideally suitedfor detecting subtle topographic changes present inearly keratoconus and for documenting their pro-gression by serial topographic analysis.
E. VIDEOKERATOGRAPHY STUDIES OF KERATOCONUS
Several studies have been performed to character-ize the topographic phenotype of clinically detect-able keratoconus by videokeratography.103,156 Themajority of patients have peripheral cones, withsteepening extending into the periphery. The steep-ening in this group is usually confined to one or twoquadrants. A smaller group of patients have centraltopographic alterations. Many central cones have abow tie configuration similar to that found in natu-rally occurring astigmatism. In the keratoconus pa-tients, however, the bow tie pattern is asymmetric,with the inferior loop being larger in most instances.In contrast to eyes having with-the-rule astigmatism,the steep radial axes above and below the horizontalmeridian in keratoconus appear skewed, giving thebow tie a lazy-eight configuration. Another pattern
found in central cones is more symmetric steepen-ing without a bow tie appearance. The pattern isusually the same in both eyes, although it may bemore advanced in one eye than in the other. The pe-ripheral and central cones probably correspondroughly to the oval sagging and nipple-shaped conesdescribed by Perry et al.96
In summary, keratoconus has three characteristicsseen by videokeratography that are not present innormals: an increased area of corneal power sur-rounded by concentric areas of decreasing power,inferior-superior power asymmetry, and skewing ofthe steepest radial axes above and below the hori-zonal meridian (Fig. 6).
F. VIDEOKERATOGRAPHY PATTERN RECOGNITION: NORMAL VERSUS KERATOCONUS
Similar patterns have been noted in clinically nor-mal family members of keratoconus patients and inthe clinically normal fellow eyes of patients with clin-ically unilateral keratoconus.80,101,105 These patternsare, however, milder (as measured by dioptricpower) than the patterns noted in clinically obviouskeratoconus (Fig. 10).
While it is relatively easy to recognize patternswith color-coded maps once a practitioner hasgained experience through observing many topo-graphic maps, it is confusing and difficult for clini-cians who are inexperienced with this technique toidentify the minimal topographic criteria requiredfor a diagnosis of keratoconus based on pattern rec-ognition of a videokeratograph alone. Therefore, it
Fig. 10. Videokeratograph of formefruste keratoconus in a clinically nor-mal family member of a patient withfamilial keratoconus (see Fig. 8, A-II-5). This videokeratograph has similarbut milder features than those notedin keratoconus.
310 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
has been recommended that maps that look suspi-cious for keratoconus in the presence of a clinicallynormal eye be labelled “keratoconus suspect” untilprogression to keratoconus can be documented.151
One way to become proficient in recognizing subtlepathology is to print maps of all patients examinedin the absolute scale (in the TMS-1 this scale dividesthe cornea into 1.5 diopter [D] intervals between35 and 50 D and 5 D intervals outside of thisrange).47,155 This singular scale allows the clinician toget used to patterns descriptive of normal topogra-phy, allowing earlier recognition of subtle abnormaltopography. The normalized scale in this device,which divides the cornea into 11 equal colors, is con-fusing, and many clinically normal patients withslight inferior steepening might inadvertently be la-belled as suspect using this scale. For the purposes ofour research in trying to define an early keratoconusphenotype by videokeratography, we have compileda database of normal videokeratography patterns of195 normal individuals using this absolute scale (Fig.11). This baseline database of videokeratographypatterns (sagittal topography) to be used as a refer-ence for our longitudinal topographic studies ofkeratoconus family members can also help the clini-cian in determining whether subtle deviations incorneal topography exist in a particular patient ob-served at any time. While it has not yet been deter-mined which patterns ultimately progress to kerato-conus, our database of videokeratography patternssuggests that only 1 in 195 (0.5%) normal patientshave mild topographic features similar to, butmilder than, those seen in clinically detectable kera-toconus asymmetric bow tie with skewed radial axes([AB/SRAX] pattern, Fig. 11).108
G. VIDEOKERATOGRAPHIC “PSEUDOKERATOCONUS”
Another source of confusion in assigning minimaltopographic criteria for keratoconus are videokera-tography patterns simulating keratoconus (video-keratographic pseudokeratoconus).102,154,157 The mostcommon culprit is contact lens wear (both hard andsoft), which induces patterns of inferior steepeningthat may be very difficult to distinguish from kerato-conus.157 These patterns, however, disappear withtime after contact lens wear is discontinued. Video-keratographic pseudokeratoconus may also resultfrom technical errors during videocapturing, suchas inferior eyeball compression, misalignment of theeye with inferior or superior rotation of the globe(Fig. 12), and incomplete digitization of mires, caus-ing formation of dry spots, which simulates inferiorsteepening. Early pellucid marginal degeneration,inflammatory corneal thinning, and previous ocularsurgery can all induce patterns that simulate kerato-
conus by videokeratography.99 Awareness of theconditions that may simulate early keratoconusvideokeratographically will enhance the clinician’sability to recognize true topographic changes in earlykeratoconus.
H. QUANTITATIVE DESCRIPTORS
Developing quantitative descriptors of video-keratography patterns in keratoconus would allowfor easier recognition of patterns and enable us todevelop a quantitative phenotype that could beuniversally used to formulate minimal topographiccriteria for diagnosing keratoconus.111 In a small pre-liminary study, we developed three indices that dis-
Fig. 11. Classification scheme of normal videokerato-graphs in the absolute scale devised as a baseline to moni-tor topographic progression to keratoconus: Top A, round:B, oval: C, superior steepening; D, inferior steepening; E,irregular; F, symmetric bow tie; G, symmetric bow tie withskewed radial axes; H, asymmetric bow tie with inferiorsteepening (AB/IS); I, asymmetric bow tie with superiorsteepening; J, asymmetric bow tie with skewed radial axes(AB/SRAX). Lower two figures are a schematic illustrationof how to determine whether a pattern is AB/IS or AB/SRAX. A line is drawn to bisect the upper and lower lobesof the asymmetric bow tie (see solid lines), if there is nosignificant deviation from the vertical meridian (i.e., noskewing), the pattern is designated as AB/IS (as in bottomA); if the lines bisecting the two lobes appear skewed bymore than 308 from the vertical meridian (i.e., 1508 fromone another), it is labeled as AB/SRAX (as in Bottom B).(Reprinted from Rabinowitz et al108 with permission of theBritish Journal of Ophthalmology.)
KERATOCONUS 311
tinguished eyes with keratoconus from normals: cen-tral K (descriptive of central steepening); I-S values(inferior-superior dioptric asymmetry); and R versusL (difference between right and left central cornealpower). Videokeratography studies on 28 familymembers of five patients with keratoconus revealedthat 50% of the subjects had mild topographic ab-normalities and at least one index greater than twostandard deviations from their normal controlgroup. These abnormalities were similar to, but lesssevere than, those found in the patients with kerato-conus. It is possible that these indices are descriptiveof the earliest stages of keratoconus in normal eyesbefore they progress to keratoconus, and these ab-normalities might represent variable expression of akeratoconus gene in these families.101,104 However,longitudinal studies and serial topographic analysisare required to confirm this. Since the originalstudy, the indices have been modified and embod-ied into a computer software program where theyare analyzed with our baseline database (con-structed from 195 normals). A new index has alsobeen developed that is more specific to keratoconusand that quantifies the irregular astigmatism thattypifies the keratoconus videokeratograph, the SRAXindex (Fig. 6). Using a combination of four indices,Central K, I-S value, Sim K, and the SRAX index,98% of keratoconus videokeratographs could be dis-tinguished from a group of normal controls. Theseindices were, however, useful only in patients with1.5 D or more of astigmatism as measured by thesimulated keratometry readings.99 Work is currentlyin progress to formulate a single numeric value de-rived from these indices to provide minimal topo-graphic criteria for assigning affectation status to
keratoconus family members for use in formal pedi-gree analyses such as complex segregation analysis.109
Analyses of videokeratography data described thusfar are based on data generated by sagittal algo-rithms, which are spherically biased. Recent prelimi-nary studies suggest that tangential algorithms mayhave more promise for identifying the early topo-graphic features of keratoconus. Studies are cur-rently in progress to determine whether such algo-rithms might be the preferred method for studyingkeratoconus.98
I. VIDEOKERATOGRAPHY SCREENING FOR REFRACTIVE SURGERY
With the recent approval in the USA of the exci-mer laser for the correction of myopia, detectingearly keratoconus in the absence of slit-lamp find-ings has assumed increasing importance. In some in-stances, unpredictable results and patient dissatisfac-tion have been attributed to the existence ofundiagnosed early keratoconus in refractive surgerypatients.28,82 Because these patients do not achievehigh-quality vision with either glasses or contact lenses,they tend to seek out refractive surgery. Recent reportssuggest that patients with early keratoconus or kerato-conus suspects comprise 2–5% of patients presentingfor refractive surgery for myopia.88,154
Videokeratography screening allows the clinicianto rule out these early ectasias and other topo-graphic abnormalities before embarking on refrac-tive surgery. It is difficult to identify which subtlekeratoconuslike topographic patterns truly repre-sent early keratoconus, hence the need to formulatequantitative indices derived from patients who haveclinical signs of disease.
Fig. 12. Pseudokeratoconus error pattern (with Eysys instrument) induced from misalignment of a normal eye resultingin a pattern simulating a keratoconus videokeratograph (right); videokeratograph of early keratoconus for comparison(left). (Courtesy of R. E. Hubbe, MD, and Gary Foulks, MD.)
312 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
Two software systems using quantitative indicesfor detecting keratoconus are currently available onsome corneal topographers, the one developed byRabinowitz99 and another developed by Maeda andKlyce at the LSU Eye Center in New Orleans, Louisi-ana.76,77 Using TMS-1 videokeratographs, the LSUgroup computed 11 quantitative criteria for eachmap and trained a three-layer neural network using108 maps from 7 separate diagnostic categories. Theoverall accuracy of the trained neural network was80%. Based on eight of the quantitative criteria,Maeda and Klyce designed an “expert system” to de-tect keratoconus. The system, which is based on lin-ear discriminant analysis and a binary decision tree,identifies the map as representing keratoconus ornonkeratoconus and, based on a value from the dis-criminant analysis (the KPI), assigns the map an in-dex expressed as a percentage that suggests the se-verity of keratoconus (the KCI, Fig. 15). This systemwas able to differentiate keratoconus from a wide va-riety of other pathologies with a false positive rate of1 out of 43 and a false negative rate of 2 in 130.
The Rabinowitz software differs from the Maeda/Klyce system in several respects: it attempts only todifferentiate keratoconus from normals, not fromother pathologies in a noncontact lens wearing pop-ulation; it relies on both eyes, not a single eye in itsevaluation; its indices are derived from videokerato-graphs only of patients who have clinical signs ofkeratoconus, not from videokeratographs judged byexperts to have keratoconus without regard to clini-cal signs; and it provides clear quantitative cutoffpoints based on its indices as to which videokerato-graphs should be labeled normal or keratoconus.99
Both software programs were designed to aid theclinician in identifying abnormal topography andwere not intended as a substitute for a history, thor-ough ocular evaluation, and good clinical judgmentwhen a patient is being evaluated as a candidate forrefractive surgery.
VI. Differential DiagnosisIt is important to distinguish keratoconus from
other ectatic dystrophies and thinning disorders,such as pellucid marginal degeneration, Terrien’smarginal degeneration, and keratoglobus, becausethe management and prognosis in these disordersdiffer markedly from keratoconus. The distinctioncan usually be made by careful slit-lamp evaluation,but corneal topography evaluation is a useful ad-junct to differentiate these disorders in subtle orearly cases.107
A. PELLUCID MARGINAL DEGENERATION
Pellucid marginal degeneration is characterized bya peripheral band of thinning of the inferior cornea
from the 4 to the 8 o’clock position. There is 1–2-mmuninvolved area between the thinning and the lim-bus (Fig. 1B). The corneal protrusion is most markedabove the area of thinning, and the thickness of thecentral cornea is usually normal. Like keratoconus,pellucid marginal degeneration is a progressive dis-order affecting both eyes, although eyes may beasymmetrically affected. In moderate cases it can eas-ily be differentiated from keratoconus by slit-lampevaluation because of the classical location of thethinning. In early cases the cornea may look rela-tively normal, and in advanced cases it may be diffi-cult to distinguish from keratoconus because thethinning may involve most if not all of the inferiorcornea. In both instances videokeratography is veryuseful to make the distinction. The videokeratographhas a classical “butterfly” appearance (Fig. 13A), dem-onstrating large amounts of against-the-rule astigma-tism, as measured by simulated keratometry.79
Pellucid marginal degeneration can be differenti-ated from other peripheral corneal thinning disor-ders, such as Terrien’s marginal degeneration, be-cause the area of thinning is always epithelialized,clear, avascular, and without lipid deposition. Ter-rien’s corneal degeneration affects a similar agegroup and also causes high astigmatism; however, itmay affect both the superior and inferior corneaand is accompanied by lipid deposition and vascularinvasion. Videokeratography can also be used to dif-ferentiate these two disorders because they have dis-tinctly different topographic patterns.158
Because of the large amounts of against-the-ruleastigmatism, patients with pellucid marginal degen-eration are much more difficult to fit with contactlenses than patients with keratoconus, although spher-ical or aspheric contact lenses with large overalldiameter should initially be attempted in early-to-moderate cases. Surgery may be considered for pa-tients whose vision is not adequately corrected bycontact lenses or in patients who are contact lens-intolerant. Patients with pellucid marginal degenera-tion, however, are typically poor candidates for pene-trating keratoplasty for two reasons. First, thinningoccurs so near the limbus that the donor corneamust be placed very close to the corneal limbus, thusincreasing the chances of graft rejection. Second,because of the extreme thinning and the location ofthe thinning, penetrating keratoplasty typically in-duces large amounts of postoperative astigmatism,which may be extremely difficult to correct becauseof disparity in graft-host thickness.
Crescentic lamellar keratoplasty is a useful initialsurgical procedure in patients with pellucid mar-ginal degeneration. This procedure involves remov-ing a crescentic inferior layer of ectatic tissue bylamellar dissection and replacing it with a thicker
KERATOCONUS 313
lamellar donor graft.124 This will, in most cases, elim-inate large amounts of against-the-rule astigmatism.In some cases, the patient may become contact lens-tolerant, thus obviating a full-thickness procedure.In contact lens failures, a full-thickness centrally lo-cated penetrating keratoplasty can subsequently beperformed, encompassing part of the lamellar graftand significantly reducing the risk of graft rejectionand postkeratoplasty astigmatism (Fig. 13B).
B. KERATOGLOBUS
Keratoglobus is a rare disorder in which the entirecornea is thinned most markedly near the corneallimbus (Fig. 1C), in contrast to the localized thin-
Fig. 13. Pellucid marginal degener-ation: A: Videokeratograph with typi-cal butterfly-shaped appearance. B:Postoperative slit-lamp photo aftercombined peripheral crescentic lamel-lar keratoplasty and central penetrat-ing keratoplasty.
ning centrally or paracentrally in keratoconus.22,48,66
The cornea may be thinned to as little as 20% of nor-mal thickness, and it assumes a globular shape. Inadvanced keratoconus, the entire cornea can also bethinned and globular-shaped, making it difficult todistinguish these two entities. However, even in veryadvanced keratoconus there may be a small area ofuninvolved cornea superiorly that approaches nor-mal corneal thickness.
Keratoglobus is bilateral, but it is usually presentfrom birth and tends to be nonprogressive. It can bedistinguished from megalocornea and congenitalglaucoma because the cornea is usually of normal di-ameter. It is a recessive disorder and is often associ-ated with blue sclerae and other systemic features, incontrast to keratoconus, which is most commonly anisolated disorder.22,66,146 In contrast to keratoconus,the corneas in keratoglobus are prone to cornealrupture from even minimal trauma. Thus, hard con-tact lenses are contraindicated and protective specta-cles should be strongly encouraged. If the cornea isextremely thin, a tectonic limbus-to-limbus lamellarkeratoplasty should be considered to strengthen thecornea. A subsequent central penetrating kerato-plasty may be considered if adequate visual rehabili-tation cannot be achieved with glasses.
VII. Management of KeratoconusA. CONTACT LENSES
The management of keratoconus varies depend-ing on the state of progression of the disease. In veryearly cases, spectacles may provide adequate visualcorrection, but because spectacles do not conformto the unusual shape of the cornea and the resultant
314 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
induced irregular astigmatism, contact lenses pro-vide better correction. Contact lenses are the main-stay of therapy in this disorder and represent thetreatment of choice in 90% of patients.17,18
The type of contact lens used varies depending onthe stage of keratoconus. Early in the disease, softlenses of toric design are adequate. As the diseaseprogresses, more complex rigid gas permeable lensesare used; these include multicurve spherical-basedlenses, aspheric lenses, and biaspheric lenses. A hy-brid lens, which has a rigid central portion for ob-taining best optics and a soft hydrophilic peripheralskirt, is also popular with some practitioners.100,119,161
Fitting contact lenses in keratoconus is a complextask embraced by few contact lens practitioners. The
challenge is to keep the patient contact lens-tolerantwith good visual acuity in a cornea that may bechanging in shape over time. Common complica-tions from lenses include induced corneal abrasion,apical scarring, neovascularization from induced hy-poxia, lens discomfort, and lenses not staying on thecornea for adequate periods of time. While some re-ports suggest that rigid contact lenses induce kerato-conus and anecdotal reports contend that keratoco-nus can be arrested by good contact lens fitting,good evidence does not exist that supports either ofthese contentions. With the new contact lenses cur-rently available and with good fitting techniques,many patients with 20/40 spectacle correction mayenjoy stable 20/20–20/25 contact lens correction
Fig. 14. Correction of postkerato-plasty astigmatism in a patient withkeratoconus: A: Preoperative video-keratograph illustrating large degreeof astigmatism and stable topography6 months apart. B: Diagram illustrat-ing location of relaxing incisions andcompression sutures based on theinformation gleaned from the video-keratograph. C: Postoperative video-keratograph 2 months after sutureshad been removed. (Reprinted fromRabinowitz et al107 with permission ofIgaku Shoin Medical Publishers, Inc.)
KERATOCONUS 315
for many years. I believe that no keratoconus patientwho can tolerate contact lenses should be deniedthe good visual rehabilitation afforded by them be-cause of fear that they may enhance the progressionof the disease.
B. CORNEAL TRANSPLANT
1. Indications
Corneal transplant (penetrating keratoplasty) isthe best and most successful surgical option for kera-toconus patients who cannot tolerate contact lensesor are not adequately visually rehabilitated by them.Central scarring may preclude good vision from con-tact lenses, even when they are tolerated. A patient withkeratoconus has an approximately 10–20% chanceover his/her lifetime of needing a corneal trans-plant.132,145 Corneas in keratoconus almost never per-forate; thus, advanced thinning by itself is not neces-sarily an indication for surgery.
Acute hydrops is not necessarily an indication forpenetrating keratoplasty, because in many instancesthe hydrops resolves and the resultant scar is outsidethe visual axis. The scarring may flatten the cornea,allowing the patient to tolerate contact lenses andachieve good vision. Patients with hydrops can betreated initially with cycloplegics, steroids or nonste-roidal anti-inflammatory agents, 5% sodium chlo-ride solution (Muro 128), and, in rare instances,with bandage contact lenses.134
Buzard and Fundingsland have recently suggestedthat because of improved corneal transplant tech-niques and new and improved modalities to correctrefractive error after corneal transplantation, pa-tients whose best corrected spectacle visual acuity is20/40 or worse should be offered cornea transplants
in lieu of contact lens fitting.19 Considering the goodvisual acuity afforded to many patients who are suc-cessful contact lens wearers, this approach would beregarded by many as being too aggressive.
2. Procedures and Success Rate
Because of the avascular nature of the cornea, cor-neal transplant has a success rate of 93–96%.97,130,144,152
Advances in both eyebanking and surgical tech-niques now allow this procedure to be done on anoutpatient basis with minimal incapacitation of thepatient. Complete visual recovery may, however, takeas long as 6 months.
Patients who are candidates for penetrating kerato-plasty should be counseled that in spite of the highsuccess rate of surgery there is still a 50% chance thatthey may need contact lenses, either because of resid-ual myopia or postkeratoplasty astigmatism. To de-crease the amount of myopia, several surgeons are per-forming keratoplasties with the donor and hosttrephines of equal size (usually 7.5 mm; the incidenceof rejection is slightly higher with larger sizegrafts).45,143,144 While in many instances this reduces theamount of myopia, patients who are axial myopes maystill be left with large amounts of residual myopia.143
Large amounts of postkeratoplasty astigmatism mayremain even after all the sutures are removed. Thiscan be corrected with a combination of relaxing inci-sions and compression sutures while videokeratogra-phy is used as a guide. The residual astigmatism isthen small and and can be corrected well with rigidgas permeable lenses (Fig. 14).107 It is desirable toleave a small amount of with-the-rule astigmatism, asthe patients tolerate this better and it allows for easiercontact lens fitting than against-the-rule astigmatism.
Fig. 15. Keratoconus suspect video-keratograph (absolute scale, sagittaltopography) with Rabinowitz andKlyce diagnostic indices to aid in in-terpretation of color-coded map.
316 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
3. Complications
In compliant patients, complications after pene-trating keratoplasty are rare. These may include re-jection, postoperative astigmatism, a fixed dilatedpupil, and recurrence of keratoconus.1,67,89,142,149 Graftrejection rates in keratoconus are low and may be re-versed with medication if treated early. There havebeen isolated reports of keratoconus recurring inthe graft decades after surgery. These reports are ex-tremely rare, and it is not clear whether keratoconusactually recurred in the graft or whether there wasmild, undetected keratoconus in the donor but-tons.1,67,89 Patients will, however, often ask about re-currence, and these isolated reports should be men-tioned within this context.
C. EPIKERATOPLASTY
Epikeratoplasty for a while gained acceptance as amode of treatment for patients with keratoconuswith a clear visual axis. Although good long-term re-sults have been reported,70,148 the procedure has forthe most part been abandoned in favor of penetrat-ing keratoplasty because of the superior quality of vi-sion afforded by the latter procedure. There still is arole for epikeratoplasty in select high-risk circum-stances. For instance, in keratoconus patients withDown syndrome, epikeratoplasty might be prefera-ble to a penetrating keratoplasty because of its non-invasive nature and the decreased potential for cor-neal graft rejection.
D. EXCIMER LASER PHOTOTHERAPEUTIC KERATECTOMY
Excimer laser phototherapeutic keratectomy hasbeen demonstrated to be useful in the managementof patients with keratoconus who have nodular sub-epithelial corneal scars and who are contact lens-intolerant.150 This technique provides a smooth cor-neal surface, allowing patients to regain contact lenstolerance. The nodules may also be removed at theslit-lamp with a sharp handheld blade, potentiallywith a similar result, albeit with less precision. A re-cent small study, with short-term data only, suggeststhat the excimer laser might be useful for providingan improved refractive effect and delaying the needfor penetrating keratoplasty in patients with ad-vanced keratoconus.85 This suggested mode of treat-ment for keratoconus is not currently commonly ac-cepted and should be approached with extremecaution until long-term data on outcomes becomeavailable. Performing this procedure on an alreadythinned and irregular cornea could be hazardousand has the potential for immediate complicationsexceeding the long-term therapeutic effect.
Method of Literature SearchAll articles in Medline up to March 1997 were re-
viewed. Those considered relevant and that contrib-uted scientifically to the topics covered were includedin this article.
References1. Abelson MB, Collin HB, Gillete TE, Dohlman CH: Recurrent
keratoconus after keratoplasty. Am J Ophthalmol 90:672–676,1980
2. Alstrom CH, Olson O: Heredo-retinopathia congenitalis.Monohybride recessiva autosomalis. Hereditas Genttiskt43:1–177, 1957
3. Amsler M: Le keratocone fruste au javal. Ophthalmologica96:77–83, 1938
4. Amsler M: Keratocone classique et keratocone fruste, argu-ments unitaires. Ophthalmologica 111:96–101, 1946
5. Archer DB, Sharma NK: Irido-corneal dysgenesis. TransOphthalmol Soc UK 98:510, 1978
6. Austin MG, Schaefer RF: Marfan’s syndrome with unusualblood vessel manifestations. Arch Pathol 64:204–209, 1957
7. Beardsley TL, Foulks GN: An association of keratoconus andmitral valve prolapse. Ophthalmology 89:35–37, 1982
8. Beckh U, Schonherr U, Naumann GO: Augenklinik mit Po-liklinik, Universitat Erlangen-Nurnberg. Autosomal domi-nant keratoconus as the chief ocular symptom in Lobsteinosteogesis imperfecta tarda. Klin Monatsbl Augenheilkd206:268–272, 1995
9. Bereau J, Fabre EJ, Hecquet C, et al: Modification of pros-taglandin E2 and collagen synthesis in keratoconus fibro-blasts associated with an increase of interleukin-1 alpha re-ceptor number. CR Acad Sci, Paris 316(III):425–430, 1993
10. Bisaria KK: Bilateral keratoconus with ocular hypertensionand the natural cure of one eye. J All India Ophthalmol Soc15:197–199, 1967
11. Blair SD, Seabrooks D, Shields JW, et al: Bilateral progres-sive essential iris atrophy and keratoconus with coincidentfeatures of posterior polymorphous dystrophy: a case reportand proposed pathogenesis. Cornea 11:255–261, 1992
12. Blanksma LJ, Donders PC, Van Voorst Vander PC: Xero-derma Pigmentosum and keratoconus. Doc Ophthalmol64:97–103, 1986
13. Brenner S, Nemet P, Legum C: Jadasohn-type anetodermain association with keratoconus and cataract. Ophthalmo-logica 174:181–184, 1977
14. Bron A, Rabinowitz YS: Corneal dystrophies and keratoco-nus. Curr Opin Ophthalmol 7:71–82, 1996
15. Brown IA: Ankyloblepharon associated with keratoconus. BrJ Ophthalmol 51:138–139, 1967
16. Buiuc S, Beschea G, Jaobleceastai L, Dimitriu G: A case of bi-lateral posterior lenticonus associated with keratoconus. RevChir Oftalmol 22:299–300, 1978
17. Buxton JN: Contact lenses in keratoconus. Contact Intraoc-ular Lens Med J 4:74, 1978
18. Buxton JN, Keates RH, Hoefle FB: The contact lens correc-tion of keratoconus, in Diabezes OH (ed): Contact Lenses.The CLAO Guide to Basic Science and Clinical Practice. Or-lando, Grune and Stratton, 1984
19. Buzard KA, Fundingsland BR: Cornea transplants for kera-toconus. Results in early and late disease. J Refract Surg23:398–496, 1997
20. Byers PH: Disorders of collagen biosynthesis and structure,in Scriver CR, Beaudet AL, Sly WS, Valle D (eds): MetabolicBasis of Inherited Disease. New York, McGraw Hill, 1995, ed7, pp 4029–4077
21. Cantor RM, Rotter JI: Analysis of genetic data: methods andinterpretation, in King RA, Rotter JI, Motulsky AG (eds):The Genetic Basis of Common Diseases. 1992, pp 49–70
22. Cavara V: Keratoglobus and keratoconus. Br J Ophthalmol34:621, 1950
KERATOCONUS 317
23. Conneally PM, Rivas ML: Linkage analysis in man. Adv HumGenet 10:209–266, 1980
24. Cullen JF, Butler HG: Mongolism (Down’s Syndrome) andkeratoconus. Br J Ophthalmol 47:321–330, 1963
25. Donaldson DD: A new instrument for keratography. ArchOphthalmol 88:425–428, 1972
26. Driver PJ, Reed JW, David RM: Familial cases of keratoconusassociated with posterior polymorphous dystrophy (letter).Am J Ophthalmol 118:256–257, 1994
27. Duke-Elder S, Leigh AG: System of ophthalmology. Diseasesof the outer eye, Vol 8. London, Henry Kimpton, 1965, pp964–976
28. Durand L, Monot JP, Burillon C, Assi A: Radial keratotomyin a patient with keratoconus. Refract Corneal Surg 7:374–376, 1991
29. Eiferman RA, Law MW, Lane L: Iridoschisis and keratoco-nus. Cornea 13:78–79, 1994
30. Elder MJ: Leber congenital amaurosis and its associationwith keratoconus and keratoglobus. J Pediatr OphthalmolStrabismus 31:38–40, 1994
31. Elston RC: Segregation analysis. Adv Hum Genet 11:63–120,1981
32. Enoch E, Itzahki A, Lakshminarayanan V, et al: Visual fielddefects detected in patients with Gilles de la Tourette syn-drome: preliminary report. Int Ophthalmol 13:331–344,1989
33. Etzine S: Conical cornea in identical twins. S Afr Med J28:154–155, 1954
34. Falls HF, Allen W: Dominantly inherited keratoconus. Re-port of a family. J Genet Hum 17:317, 1969
35. Franceschetti A: Keratoconus, in King JH, McTigue JW(eds): The Cornea. World Congress. Washington, Butter-worths, 1965, pp 152–168
36. Francois J: Afflictions of the cornea, in Francois J (ed): He-redity in Ophthalmology. St Louis, CV Mosby, 297–298,1961
37. Francois J, Neetens A, Smets RM: Bardet-Biedl syndromeand keratoconus. Bull Soc Ophthalmol 203:117–121, 1982
38. Frasca G, Belmonte M: Neurocutaneous angiomatosis andkeratoconus. A new syndrome entity? Riv Otoneurooftalmol41:119–130, 1966
39. Freedman J, Gombos GM: Bilateral macular coloboma,keratoconus and retinitis pigmentosa. Ann Ophthalmol3:664–665, 1971
40. Filip O, Golu T, Filip I, et al: Keratoconus in Albers-Schon-berg disease. Oftalmologia 38:247–251, 1994
41. Fukuchi T, Yue B, Sugar J, Lam S: Lysosomal enzyme activi-ties in conjunctival tissues of patients with keratoconus.Arch Ophthalmol 112:1368–1374, 1994
42. Gasset AR, Houde WI, Garcia-Bengochea H: Contact lenswear as an environmental risk in keratoconus. Am J Oph-thalmol 85:339–341, 1978
43. Gasset AR, Worthen DM: Keratoconus and Chandler’s syn-drome. Ann Ophthalmol 6:819–820, 1974
44. Geerarts WJ: Ocular Syndromes. Philadelphia, Lea and Fe-biger, 1969, ed 2
45. Girard LJ, Esnaola N, Rao R, et al: Use of grafts smaller thanthe opening for keratoconic myopia and astigmatism. J Cata-ract Refract Surg 18:380–384, 1992
46. Gonzalez V, McDonnell PJ: Computer-assisted corneal to-pography of parents in patients with keratoconus. ArchOphthalmol 110:1413–1414, 1992
47. Gormley DJ, Gersten M, Koplin RS, Lubkin V: Corneal mod-eling. Cornea 7:30, 1988
48. Grayson M, Keates RH: Manual of diseases of the cornea.Boston, Little Brown, 1969, ed 1
49. Greenfield G, Romano A, Stein R, Goodman RM: Bluesclerae and keratoconus. Key features of a distinct heritabledisorder of connective tissue. Clin Genet 4:8–16, 1973
50. Hallerman W, Wilson EJ: Genetische betrachtungen uber denkeratoconus. Klin Monatsbl Augenheilkd 170:906–908, 1977
51. Hammerstien W: Zur genetik des keratoconus. Graefes ArchKlin Exp Ophthalmol 190:293–308, 1974
52. Hannush SB, Crawford SL, Waring GO III, et al: Accuracy
and precision of keratometry, photokeratoscopy, and cor-neal modeling on calibrated steel balls. Arch Ophthalmol107:1235–1239, 1989
53. Hartstien J: Keratoconus that developed in patients wearingcorneal contact lenses. Arch Ophthalmol 80:345–346, 1968
54. Hoang-Xuan T, Elmaleh C, Dhermy P, et al: Association of alattice dystrophy and keratoconus: anatomo-clinical studyapropos of a case. Bull Soc Ophthalmol Fr 89:35–38, 1989
55. Hofstetter H: A keratoscopic survey of 13,395 eyes. Am J Op-tom Acad Optom 36:3–11, 1959
56. Ihalainen A: Clinical and epidemiological features of kerato-conus: genetic and external factors in the pathogenesis ofthe disease. Acta Ophthalmol 178(Suppl):5–64, 1986
57. Iwaszkiewicz E: Keratoconus. II. Coexisting diseases and the-ories on its etiology and pathogenesis. Klin Oczna 91:210–211, 1989
58. Judisch GF, Waziri M, Krachmer J: Ocular Ehlers-Danlossyndrome with normal lysyl hydroxylase activity. Arch Oph-thalmol 94:1489, 1976
59. Kayazawa F, Nishimura K, Kodama Y, et al: Keratoconus withpellucid marginal corneal degeneration. Arch Ophthalmol102:895–896, 1984
60. Kennedy RH, Bourne WM, Dyer JA: A 48-year clinical andepidemiologic study of keratoconus. Am J Ophthalmol101:267–273, 1986
61. Kenney MC, Chwa M, Opbroek AJ, et al: Increased gelati-nolytic activity in keratoconus keratocyte cultures. A correla-tion to an altered matrix metalloproteinase-2/tissue inhibi-tor of metaloproteinase ratio. Cornea 13:108–113, 1994
62. Kirkham TH, Werner EB: The ophthalmic manifestations ofRothmund’s syndrome. Can J Ophthalmol 10:1–14, 1975
63. Klintworth GK: Degenerations, depositions and miscella-neous reactions of the ocular anterior segment, in Garner A,Klintworth GK (eds): Pathobiology of Ocular Disease: A Dy-namic Approach. New York, Marcel Dekker, 1994, ed 2, pp743–794
64. Klintworth GK, Damms T: Corneal dystrophies and kerato-conus. Curr Opin Ophthalmol 6:44–56, 1995
65. Klyce SD: Computer-assisted corneal topography. High reso-lution graphic presentation and analysis of keratoscopy. In-vest Ophthalmol Vis Sci 25:1426–1435, 1984
66. Krachmer JH, Feder RS, Belin MW: Keratoconus and re-lated noninflammatory corneal thinning disorders. SurvOphthalmol 28:293–322, 1984
67. Kremer I, Eagle RC, Rapuano CJ, Laibson PR: Histologic ev-idence of recurrent keratoconus seven years after kerato-plasty. Am J Ophthalmol 119:511–512, 1995
68. Kremer I, Martini AM, Cohen EJ: Keratoconus associatedwith ectodermal and mesodermal anomalies (letter). CLAOJ 18:141, 1992
69. Kumig BS, Joffe L: Ehlers-Danlos syndrome associated withkeratoconus. S Afr Med J 52:403–405, 1977
70. Lass JH, Stocker EG, Fritz ME, Collie DM: Epikeratoplasty.The surgical correction of aphakia, myopia, and keratoco-nus. Ophthalmology 94:912–925, 1987
71. Lee LR, Hirst LW, Readshaw G: Clinical detection of unilat-eral keratoconus. Aust N Z J Ophthalmol 23:129–133, 1995
72. Levene JR: An evaluation of the handheld keratoscope as adiagnostic instrument for corneal astigmatism. Br J PhysiolOpt 19:237–251, 1962
73. Lipman RM, Rubenstein JB, Torczynski E: Keratoconus andFuchs’ corneal endothelial dystrophy in a patient and herfamily. Arch Ophthalmol 108:993–994, 1990
74. Lorfel RS, Sugar HS: Keratoconus associated with retrolen-tal fibroplasia. Ann Ophthalmol 8:449–450, 1976
75. Lund AM: The Angelman syndrome. Does the phenotypedepend on maternal inheritance? Ugeskr Laeger 153:1993–1998, 1991
76. Maeda N, Klyce SD, Smolek MK, Thompson HW: Auto-mated keratoconus screening with corneal topography anal-ysis. Invest Ophthalmol Vis Sci 35:2749–2757, 1994
77. Maeda N, Klyce SD, Smolek MK: Comparison of methodsfor detecting keratoconus using videokeratography. ArchOphthalmol 113:870–874, 1995.
318 Surv Ophthalmol 42 (4) January–February 1998 RABINOWITZ
78. Maguire LJ, Bourne W: Corneal topography of early kerato-conus. Am J Opthalmol 108:107–112, 1989
79. Maguire LJ, Klyce SD, McDonald ME, Kaufmann HE: Cor-neal topography of pellucid marginal degeneration. Oph-thalmology 94:519–524, 1987
80. Maguire LJ, Meyer RF: Ectatic corneal degenerations, inKaufman H (ed): The Cornea. 1988, pp 485–510
81. Maguire LJ, Wilson SE, Camp JJ, Verity S: Evaluating the re-producibility of topography systems on spherical surfaces.Arch Ophthalmol 111:259–262, 1993
82. Mammilis N, Montgomery S, Anderson C, et al: Radial kera-totomy in a patient with keratoconus. Refract Corneal Surg7:374–376, 1991
83. McKusick VA: Heritable Diseases of Connective Tissue. StLouis, CV Mosby, 1966, ed 3
84. McKusick VA: Inherited disorders of connective tissue, inHarrison TR (ed): Principles of Internal Medicine. NewYork, McGraw Hill, 1974, ed 7, pp 2015–2020
84a. Merlin U, Cantera E: Corneal topography, in Burrato L(ed): The Clinical Atlas thoroughfare, New Jersey, Slack,1996, pp 9–93
85. Mortensen J, Ohrstrom A: Excimer laser photorefractivekeratectomy for treatment of keratoconus. J Refract CornealSurg 10:368–372, 1994
86. Morton NE: Segregation analysis, in Computer Applicationsin Genetics, Honolulu, University of Hawaii Press, 1969, pp129–139
87. Negris R: Floppy eyelid syndrome associated with keratoco-nus. J Am Optom Assoc 63:316–319, 1992
88. Nesburn AB, Bahri S, Salz J, et al: Keratoconus detected byvideokeratography in candidates for photorefractive keratec-tomy. J Refract Surg 11:194–201, 1995
89. Nirankari VS, Karesh J, Bastion F, et al: Recurrence of kera-toconus in a donor cornea 22 years after successful kerato-plasty. Br J Ophthalmol 67:32, 1983
90. Nucci P, Brancato R: Keratoconus and congenital hip dys-plasia (letter). Am J Ophthalmol 111:775–776, 1991
91. Nucci P, Trabucchi G, Brancato R: Keratoconus andTurner’s syndrome: a case report. Optom Vis Sci 68:407–408, 1991
92. Opbroek A, Kenney MC, Brown D: Characterization of a hu-man corneal metalloproteinase inhibitor (TIMP-1). CurrEye Res 12:877–883, 1993
93. Parker J, Ko W, Pavlopoulos G, et al: Videokeratography ofkeratoconus in monozygotic twins. J Refract Surg 12:180–183, 1996
94. Peduzzi MD, Torlai F, Delvecchio G: Bilateral pigmented re-tinopathy following measles: long term follow up and possi-ble association with keratoconus. Eur J Ophthalmol 1:148–150, 1991
95. Perlman JM, Zaidman GW: Bilateral keratoconus in Crou-zon’s syndrome. Cornea 13:80–81, 1994
96. Perry HD, Buxton JN, Fine BS: Round and oval cones inkeratoconus. Ophthalmology 87:905–909, 1980
97. Price FW, Whitson WE, Marks RG: Graft survival in fourcommon groups of patients undergoing penetrating kerato-plasty. Ophthalmology 98:322–328, 1991
98. Rabinowitz YS: Tangential vs sagittal videokeratographs inthe “early” detection of keratoconus. Am J Ophthalmol122:888–889, 1996
99. Rabinowitz YS: Videokeratographic indices to aid in screen-ing for keratoconus. J Refract Surg 11:371–379, 1995
100. Rabinowitz YS, Garbus JJ, Garbus C, McDonnell PJ: Contactlens selection for keratoconus using a computer-assistedvideophotokeratoscope. CLAO J 17:88–93, 1991
101. Rabinowitz YS, Garbus J, McDonnell PJ: Computer-assistedcorneal topography in family members of keratoconus. ArchOphthalmol 108:365–371, 1990
102. Rabinowitz YS, Klyce SD, Krachmer JH, et al: Videokeratog-raphy, keratoconus, and refractive surgery. Opinions. Re-fract Corneal Surg 5:403–407, 1992
103. Rabinowitz YS, McDonnell PJ: Computer-assisted corneal to-pography in keratoconus. Refract Corneal Surg 5:400–406,1989
104. Rabinowitz YS, Maumenee IH, Lundergan MK, et al: Molec-ular genetic analysis in autosomal dominant keratoconus.Cornea 11:302–308, 1992
105. Rabinowitz YS, Nesburn AB, McDonnell PJ: Videokeratogra-phy of the fellow eye in unilateral keratoconus. Ophthalmol-ogy 100:181–186, 1993
106. Rabinowitz YS, Riley C, Yang H, et al: Videokeratographystudies of keratoconus parents (abstract). Invest Ophthal-mol Vis Sci 36 (Suppl):S308, 1995
107. Rabinowitz YS, Wilson SE, Klyce SD (eds): Corneal Topogra-phy: Interpreting Videokeratography. New York, Tokyo, Ig-aku Shoin, 1993
108. Rabinowitz YS, Yang H, Akkina J, et al: Videokeratographyof normal human corneas. Br J Ophthalmol 80:610–616,1996
109. Rabinowitz YS, Yang H, Elashoff J, Rotter J: The KI-SA% in-dex: a quantitative new videokeratography algorithm em-bodying minimal topographic criteria for diagnosing kerato-conus and “suspects” (abstract). Invest Ophthalmol Vis Sci37 (Suppl):S910, 1996
110. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Familiality inkeratoconus and related topographic measures. Proceed-ings of the World Congress of the Cornea IV (Abstract). Ab-stract Book. VIII Keratoconus, 1996, p 2
111. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Videokeratogra-phy indicators of “early” keratoconus (abstract). Invest Oph-thalmol Vis Sci 34 (Suppl):S1218, 1993
112. Rabinowitz YS, Yang H, Elashoff J, Rotter J: Videokeratogra-phy and pachymetry studies in keratoconus (abstract). Oph-thalmology (Suppl):67, 1993
113. Rahi A, Davies P, Ruben M, et al: Keratoconus and coexist-ing atopic disease. Br J Ophthalmol 61:761, 1977
114. Rau S, Duncker GI: Keratoconus in Mulvihill-Smith syn-drome. Klin Monatsbl Augenheilkd 205:44–46, 1994
115. Redmond KB: The role of heredity in keratoconus. TransOphthalmol Soc 27:52–54, 1968
116. Ricci B, Lepore D, Iossa M, et al: Ocular anomalies inAlagille’s syndrome (Anomalies oculaires dans le syndromed’Alagille). J Fr Ophthalmol 14:481–485, 1991
117. Robertson I: Keratoconus and Ehlers Danlos syndrome. Anew aspect of keratoconus. Med J Aust 1:571–573, 1975
118. Rose NJ, Mackay K, Byers PH, Dalgleish R: A Gly238Ser sub-stitution in the alpha 2 chain of type I collagen results in os-teogenesis imperfecta type III. Hum Genet 95:215–218, 1995
119. Rosenthal P, Cotter JM, Clinical performance of a spline-based apical vaulting keratoconus corneal contact lens de-sign. CLAO J 21:42–46, 1995
120. Rowsey JJ, Reynolds AE, Brown R: Corneal topography. Cor-neascope. Arch Ophthalmol 99:1093–1100, 1981
121. Sassani JW, Smith SG, Rabinowitz YS: Keratoconus and bilat-eral lattice-granular corneal dystrophies. Cornea 11:343–350, 1992
122. Sawagamuchi S, Twinning SS, Yue BY, et al: Alpha 2 macro-globulin levels in normal human and keratoconus corneas.Invest Ophthalmol Vis Sci 35:4008–4014, 1994
123. Sawagamuchi S, Yue BYT, Sugar J, Giljoy JE: Lysosomal ab-normalities in keratoconus. Arch Ophthalmol 107:1507–1510, 1989
124. Schanzlin DJ, Samo EM, Robin JB: Crescentic lamellarkeratoplasty in pellucid marginal degeneration. Am J Oph-thalmol 96:253, 1983
125. Schwartz DE: Noonan’s syndrome associated with ocular ab-normalities. Am J Ophthalmol 73:955–960, 1972
126. Sczhotka L, Rabinowitz YS, Yang H: The influence of con-tact lens wear on the topography of keratoconus. CLAO J22:270–273, 1996
127. Shammas HJ, McGaughey AS: Retinal disinsertion syn-drome: report of a case. J Pediatr Ophthalmol Strabismus16:284–286, 1979
128. Shapiro MB, France T: The ocular features of Down’s syn-drome. Am J Ophthalmol 99:659, 1985
129. Sharif KW, Casey TA, Colart J: Prevalence of mitral valveprolapse in keratoconus patients. J R Soc Med 85:446–448,1992
KERATOCONUS 319
130. Sharif KW, Casey TA: Penetrating keratoplasty for keratoco-nus: complications and long term success. Br J Ophthalmol75:142–146, 1991
131. Shows TB, Sakaguchi AY, Naylor SL: Mapping the humangenome, cloned genes, DNA polymorphisms, and inheriteddisease. Adv Hum Genet 12:341–468, 1982
132. Smiddy WE, Hamburg TR, Kracher GP, Stark WJ: Keratoco-nus. Contact lens or keratoplasty? Ophthalmology 95:487–492, 1988
133. Smith VA, Hoh VB, Littleton L, Easty DL: Overexpression ofgelatinase A activity in keratoconus. Eye 9:429–433, 1995
134. Smolin G: Dystrophies and degenerations, in Smolin G,Thoft RA (eds): The Cornea: Scientific Foundations andClinical Practice, Boston, Little, Brown, 1987, ed 2, pp 448–449
135. Stokes DW, Parrish CM: Axenfeld’s anomaly associated withDown’s syndrome. Cornea 11:163–164, 1992
136. Stone DL, Kenyon KR, Stark WJ: Ultrastructure of keratoco-nus with healed hydrops. Am J Ophthalmol 82:450–458, 1976
137. Street DA, Vinokur ET, Waring GO III, et al: Lack of associa-tion between keratoconus, mitral valve prolapse and jointhypermobility. Ophthalmology 98:170–176, 1991
138. Thalasselis A, Selim AA: Keratoconus-tetany-menopause: thenew association. Optom Vis Sci 68:357–363, 1991
139. Thompson JS, Thompson MW: Twins in medical genetics ingenetics in medicine. Philadelphia, WB Saunders, 1986
140. Tiller G, Cohn D, Rabinowitz YS: Linkage analysis in familialkeratoconus (abstract). Invest Ophthalmol Vis Sci 33(Suppl):S793, 1992
141. Tretter T, Rabinowitz YS, Yang H, et al: Aetiological factorsin keratoconus. Ophthalmology 102 (Suppl):156, 1995
142. Tuft SJ, Buckley RJ: Iris ischaemia following penetratingkeratoplasty for keratoconus (Urets-Zavalia syndrome). Cor-nea 14:618–622, 1995
143. Tuft SJ, Fitzke FW, Buckley RJ: Myopia following penetrat-ing keratoplasty for keratoconus. Br J Ophthalmol 76:642–645, 1992
144. Tuft SJ, Gregory WM, Davidson CR: Bilateral penetratingkeratoplasty for keratoconus. Ophthalmology 102:462–468,1995
145. Tuft SJ, Moodaley LC, Gregory WM, et al: Prognostic factorsof progression to keratoconus. Ophthalmology 101:439–447, 1994
146. Verrey F: Keratoglobe aigu. Ophthalmologica 114:284, 1947147. Wachmeister L, Ingemannsson SO, Moller E: Atopy and
HLA antigens in patients with keratoconus. Acta Ophthal-mol (Copenh) 60:113, 1982
148. Waller SG, Steinert RF, Wagoner MD: Long-term results ofepikeratoplasty for keratoconus. Cornea 14:84–88, 1995
149. Walsh FB, Hoyt WF: Clinical neuro-ophthalmology. Balti-more, Williams and Wilkins, 1969, ed 3
150. Ward MA, Artunduaga G, Thompson KP, et al: Photothera-peutic keratectomy for the treatment of nodular subepithe-lial corneal scars in patients with keratoconus who are con-tact lens intolerant. CLAO J 21:130–132, 1995
151. Waring GO, Rabinowitz YS, Sugar J, et al: Nomenclature forkeratoconus suspects. Refract Corneal Surg 9:219–221, 1993
152. Williams KA, Muehlberg SM, Lewis RF, Coster DJ: How suc-cessful is corneal transplantation? A report from the Austra-lian Corneal Graft Register. Eye 9:219–227, 1995
153. Wilson SE, He YG, Weng J, et al: Epithelial injury induceskeratocyte apoptosis: Hypothesized role for the interleukin1 system in the modulation of corneal tissue organizationand wound healing. Exp Eye Res 62:325–337, 1996
154. Wilson SE, Klyce SD: Screening for corneal topographic ab-normalities before refractive surgery. Ophthalmology101:147–152, 1994
155. Wilson SE, Klyce SD, Husseini MD: Standardized colorcoded maps for corneal topography. Ophthalmology100:1723–1727, 1993
156. Wilson SE, Lin DTC, Klyce SD: The topography of keratoco-nus. Cornea 10:2–8, 1991
157. Wilson SE, Lin DTC, Klyce SD, et al: Topographic changesin contact lens-induced corneal warpage. Ophthalmology97:734–744, 1990
158. Wilson SE, Lin DTC, Klyce SD, Insler MS: The corneal to-pography of Terrien’s marginal degeneration. Refract Cor-neal Surg 6:15–20, 1990
159. Wilson SE, Verity SM, Conger DL: Accuracy and reproduc-ibility of the corneal analysis system and topographic model-ing system. Cornea 11:28–35, 1992
160. Wolter JR: Bilateral keratoconus in Crouzon’s syndromewith unilateral acute hydrops. J Pediatr Ophthalmol 14:141–143, 1977
161. Yeung K, Egbahli F, Weissman BA: Clinical experience withpiggyback contact lens systems on keratoconic eyes. J AmOptom Assoc 66:539–543, 1995
162. Zala L, Ettlin C, Krebs A: Fokale dermal Hypoplasie mitKeratokonus. Osophaguspappillomen und Hidrokystomen.Dermatologica 150:176–185, 1975
163. Zimmerman DL, Fischer RW, Winterhalter KH, et al: Com-paritive studies of collagens in normal and keratoconus cor-neas. Exp Eye Res 46:431–442, 1988
164. Zolog N: On congenital blindness (Kurz syndroms) (Obser-vations sur la cecite congenitale [Syndrome de Kurz]). BullMem Soc Fr Ophthalmol 82:113–116, 1969
OutlineI. Epidemiology
II. Clinical featuresIII. HistopathologyIV. Etiology and pathogenesis
A. Associated disordersB. Biochemical studiesC. Genetics
1. Twin studies2. Family studies3. Formal genetic analyses
a. Molecular genetic studiesb. Collagen genes as candidate genes
4. SummaryV. Topographic studies of keratoconus
A. Placido disk studiesB. PhotokeratoscopyC. KeratometryD. Computer-assisted videokeratoscopyE. Videokeratography studies of keratoconusF. Videokeratography pattern recognition: normals
versus keratoconusG. Videokeratographic “pseudokeratoconus”H. Quantitative descriptorsI. Videokeratography screening for refractive sur-
geryVI. Differential diagnosis
A. Pellucid marginal degenerationB. Keratoglobus
VII. Management of keratoconusA. Contact lensesB. Corneal transplant
1. Indications2. Procedures and success rate3. Complications
C. EpikeratoplastyD. Excimer laser phototherapeutic keratectomy
Supported in part by a grant from the National Institutes of HealthNEI R01-09052 and the Eye Birth Defects Research Foundation, Inc.
Reprint address: Yaron S. Rabinowitz, MD, 444 South San VicenteBoulevard, #1102, Los Angeles, CA 90048. E-Mail: [email protected]. Internet address: www.laser-prk.com