Leukemia
-
Upload
roneet-ghosh -
Category
Documents
-
view
36 -
download
2
Transcript of Leukemia

INTRODUCTION
Leukemia is a type of cancer of the blood or bone marrow characterized by an abnormal increase of immature white blood cells called "blasts", it affects the spongy centre of bones where our blood cells are formed. Leukemia is a broad term covering a spectrum of diseases. In turn, it is part of the even broader group of diseases affecting the blood, bone marrow, and lymphoid system, which are all known as hematological neoplasms. The disease develops when blood cells produced in the bone marrow grow out of control. The word Leukemia comes from the Greek leukos which means "white" and aima which means "blood". It is cancer of the blood or bone marrow (which produces blood cells). A person who has leukemia suffers from an abnormally increased production of blood cells, generally leukocytes in high quantities. When you have leukemia, the bone marrow starts to make a lot of abnormal whiteblood cells, called leukemia cells. They don't do the work of normal white blood cells, they grow faster than normal cells, and they don't stop growing when they should. Over time, leukemia cells can crowd out the normal blood cells. This can lead to serious problems such as anemia, bleeding, and infections.
Fig: A Wright's stained bone marrow aspiratesmear from a patient with precursor B-cell acute lymphoblastic leukemia.
Leukemia cells can also spread to the lymph nodes or other organs and cause swelling or pain. The DNA of immature blood cells, mainly white cells, becomes damaged in some way. This abnormality causes the blood cells to grow and divide chaotically. Normal blood cells die after a while and are replaced by new cells which are produced in the bone marrow. The abnormal blood cells do not die so easily, and accumulate, occupying more and more space. As more and more space is occupied by these faulty blood cells there is less and less space for the normal cells - and the sufferer becomes ill. Quite simply, the bad cells crowd out the good cells in the blood. Significant research into.the causes, diagnosis, treatment, and prognosis of leukemia is being done. Hundreds of clinical trials are being planned or conducted at any given time. Studies may focus on effective means of treatment, better ways of treating the disease, improving the quality of life for patients, or appropriate care in remission or after cures.
Page | 1

Brief History
Leukemia was first observed by pathologist Rudolf Virchow in 1845. Observing an abnormally large number of white blood cells in a blood sample from a patient, Virchow called the condition Leukämie in German, which he formed from the two Greek words leukos (λευκός), meaning "white", and aima (αίμα), meaning "blood". Around ten years after Virchow's findings, pathologist Franz Ernst Christian Neumann found that one deceased leukemia patient's bone marrow was colored "dirty green-yellow" as opposed to the normal red. This finding allowed Neumann to conclude that a bone marrow problem was responsible for the abnormal blood of leukemia patients.
By 1900 leukemia was viewed as a family of diseases as opposed to a single disease. By 1947 Boston pathologist Sydney Farberbelieved from past experiments that aminopterin, a folic acid mimic, could potentially cure leukemia in children. The majority of the children with ALL who were tested showed signs of improvement in their bone marrow, but none of them were actually cured. This, however, led to further experiments.
In 1962, researchers Emil J. Freireich Jr. and Emil Frei III used combination chemotherapy to attempt to cure leukemia. The tests were successful with some patients surviving long after the tests.
CLASSIFICATION AND PATHOPHYSIOLOGY OF LEUKEMIA
Page | 2

Clinically and pathologically, leukemia is subdivided into a variety of large groups. There are several different types of leukemia. In general, leukemia is grouped by how fast it gets worse and what kind of white blood cell it affects.The first division is between its ''acute'' and ''chronic'' forms:
Acute leukemia is characterized by the rapid increase of immature blood cells. This crowding makes the bone marrow unable to produce healthy blood cells. Immediate treatment is required in acute leukemia due to the rapid progression and accumulation of the malignant cells, which then spill over into the bloodstream and spread to other organs of the body. Acute forms of leukemia are the most common forms of leukemia in children.
Chronic leukemia is distinguished by the excessive build up of relatively mature, but still abnormal, white blood cells. Typically taking months or years to progress, the cells are produced at a much higher rate than normal cells, resulting in many abnormal white blood cells in the blood. Whereas acute leukemia must be treated immediately, chronic forms are sometimes monitored for some time before treatment to ensure maximum effectiveness of therapy. Chronic leukemia mostly occurs in older people, but can theoretically occur in any age group.
Additionally, the diseases are subdivided according to which kind of blood cell is affected. This split divides leukemias into lymphoblastic or lymphocytic leukemias and myeloid or myelogenous leukemias:
In lymphoblastic or lymphocytic leukemias, the cancerous change takes place in a type of marrow cell that normally goes on to form lymphocytes, which are infection-fighting immune system cells. Most lymphocytic leukemias involve a specific subtype of lymphocyte, the B cell.
In myeloid or myelogenous leukemias, the cancerous change takes place in a type of marrow cell that normally goes on to form red blood cells, some other types of white cells, and platelets.
Cell type Acute Chronic
Lymphocytic leukemia(or "lymphoblastic")
Acute lymphoblastic leukemia (ALL) Chronic lymphocytic leukemia (CLL)
Myelogenous leukemia(also "myeloid" or "nonlymphocytic")
Acute myelogenous leukemia (AML)(or myeloblastic)
Chronic myelogenous leukemia (CML)
Combining these two classifications provides a total of four main categories. Within each of these four main categories, there are typically several subcategories. Finally, some rarer types are usually considered to be outside of this classification scheme.
Page | 3

Acute lymphoblastic leukemia (ALL) is the most common type of leukemia in young children. This disease also affects adults, especially those age 65 and older. Standard treatments involve chemotherapy and radiotherapy. The survival rates vary by age: 85% in children and 50% in adults. Subtypes include precursor B acute lymphoblastic leukemia, precursor T acute lymphoblastic leukemia, Burkitt's leukemia, and acute biphenotypic leukemia.
Chronic lymphocytic leukemia (CLL) most often affects adults over the age of 55. It sometimes occurs in younger adults, but it almost never affects children. Two-thirds of affected people are men. The five-year survival rate is 75%. It is incurable, but there are many effective treatments. One subtype is B-cell prolymphocytic leukemia, a more aggressive disease.
Acute myelogenous leukemia (AML) occurs more commonly in adults than in children, and more commonly in men than women. AML is treated with chemotherapy. The five-year survival rate is 40%. Subtypes of AML include acute promyelocytic leukemia, acute myeloblastic leukemia, and acute megakaryoblastic leukemia. Acute myeloid leukemia (AML) is a cancer of the bone marrow and blood characterized by the rapid uncontrolled growth of immature white blood cells known as myelocytes. The disease is more common in adults than in children, with the average age at diagnosis being more than 65 years. However, diagnostic procedures and treatment of children and adults are similar. In order to understand the best treatment options available for AML, patients should know the classification or histologic subtype of the cancer and the results of analyses of chromosomes determined by cytogenetic examination. These are tests performed on a sample of the patient’s bone marrow. AML is frequently associated with abnormal chromosomes of the leukemia cells. Knowing the specific chromosomal abnormalities associated with leukemia is important for determining specific treatments and outcomes.
The following table reports the outcomes of treatment according to whether favorable or unfavorable cytogenetics were present in patients with AML treated with standard intensive chemotherapy. The table illustrates the importance of cytogenetic analyses in adults.
Page | 4

ALL11%
CLL26%
AML31%
CML15%
others17%
Fig: Demographics of Leukemia Patients (2001 Data)
Sources from Leukemia, Lyphoma, Myeloma Facts 2001
Chronic myelogenous leukemia (CML) occurs mainly in adults; a very small number of children also develop this disease. Treatment is with imatinib (Gleevec in US, Glivec in Europe) or other drugs. The five-year survival rate is 90%. One subtype is chronic monocytic leukemia. Chronic myeloid leukemia (CML) is the abnormal growth of relatively mature myeloid (white blood) cells. Half of all patients with CML are diagnosed after the age of 67. CML is associated with a chromosomal abnormality in which genetic material from chromosome 9 is transferred to chromosome 22. The chromosome containing the genetic switch is called the Philadelphia chromosome; this chromosome plays a role in the development of CML. The exchange of genetic information that produces the Philadelphia chromosome brings together two genes: the BCR (breakpoint cluster region) gene on chromosome 22 and the ABL (Ableson leukemia virus) gene on chromosome 9. The combination of these two genes into the single BCR-ABL gene results in the production of a protein that contributes to uncontrolled cell growth. Initially in CML, there is a gradual increase in mature, abnormal myeloid cells in the bone marrow. These cells eventually spill into the blood and other organs, causing symptoms such as fatigue from anemia or an enlarged spleen. The increase in leukemic cell numbers occurs slowly at first and is referred to as the chronic phase, but these cells invariably begin to increase more rapidly and/or include less mature cells, resulting in the accelerated or blastic phase. In order to understand the best treatment options available for chronic myeloid leukemia, it is important to know the phase of leukemia, since all new treatment information concerning chronic myeloid leukemia is categorized and discussed by the phase of disease.
Page | 5

Patients in the chronic phase of CML have stable disease with only minor symptoms, no cancer outside the bone marrow or spleen and white blood cell and platelet blood counts that are usually greater than normal.
Accelerated Phase: When chronic myeloid leukemia is difficult to control with Gleevec® (imatinib) or other therapies, the white blood count begins to increase. New symptoms may appear and old symptoms may worsen. The spleen may enlarge and/or new abnormal chromosomes can be detected in the bone marrow cells. Eventually, the leukemia becomes completely resistant to treatment and the bone marrow becomes overburdened with large numbers of immature white blood cells known as “blasts”. A diagnosis of accelerated phase requires at least one of the following:
The persistent presence of 10-30% myeloblasts in the bone marrow or peripheral blood.
A major increase of the white blood cell count to over 50,000, platelet counts that are increased or decreased and red blood cell levels that are low despite treatment.
Progressive enlargement of the spleen.
Growth of leukemia outside the bone marrow or spleen.
The presence of any cytogenetic abnormality in addition to a Philadelphia chromosome.
Persistent unexplained fever or bone pain.
Blastic Phase: Greater than 30% myeloblasts in marrow or blood
A flowchart to demonstrate the various subtypes of Leukemia are as follows:-
Page | 6

Some rarer types are usually considered to be outside of this classification scheme.
Hairy cell leukemia (HCL) is sometimes considered a subset of chronic lymphocytic leukemia, but does not fit neatly into this pattern. About 80% of affected people are adult men. No cases in children have been reported. HCL is incurable, but easily treatable. Survival is 96% to 100% at ten years.
T-cell prolymphocytic leukemia (T-PLL) is a very rare and aggressive leukemia affecting adults; somewhat more men than women are diagnosed with this disease. Despite its overall rarity, it is also the most common type of mature T cell leukemia; nearly all other leukemias involve B cells. It is difficult to treat, and the median survival is measured in months.
Large granular lymphocytic leukemia may involve either T-cells or NK cells; like hairy cell leukemia, which involves solely B cells, it is a rare and indolent (not aggressive) leukemia.
Adult T-cell leukemia is caused by human T-lymphotropic virus (HTLV), a virus similar to HIV. Like HIV, HTLV infects CD4+ T-cells and replicates within them; however, unlike HIV, it does not destroy them. Instead, HTLV "immortalizes" the infected T-cells, giving them the ability to proliferate abnormally. Human T cell lymphotropic virus types I and II (HTLV-I/II) are endemic in certain areas of the world.
Page | 7

SIGNS AND SYMPTOMS OF LEUKEMIA
Damage to the bone marrow, by way of displacing the normal bone marrow cells with higher numbers of immature white blood cells, results in a lack of blood platelets, which are important in the blood clotting process. This means people with leukemia may easily become bruised, bleed excessively, or develop pinprick bleeds (petechiae).
White blood cells, which are involved in fighting pathogens, may be suppressed or dysfunctional. This could cause the patient's immune system to be unable to fight off a simple infection or to start attacking other body cells. Because leukemia prevents the immune system from working normally, some patients experience frequent infection, ranging from infected tonsils, sores in the mouth, or diarrhoea to life-threatening pneumonia or opportunistic infections. Finally, the red blood cell deficiency leads to anaemia, which may cause dyspnea and pallor. Some patients experience other symptoms, such as feeling sick, having fevers, chills, night sweats, feeling fatigued and other flu-like symptoms. Some patients experience nausea or a feeling of fullness due to an enlarged liver and spleen; this can result in unintentional weight loss. Blasts affected by the disease may come together and become swollen in the liver or in the lymph nodes causing pain and leading to nausea.
If the leukemic cells invade the central nervous system, then neurological symptoms (notably headaches) can occur. All symptoms associated with leukemia can be attributed to other diseases. Consequently, leukemia is always diagnosed through medical tests. The word leukemia, which means 'white blood', is derived from the disease's namesake high white blood cell counts that most leukemia patients have before treatment. The high number of white blood cells are apparent when a blood sample is viewed under a microscope. Frequently, these extra white blood cells are immature or dysfunctional. The excessive number of cells can also interfere with the level of other cells, causing a harmful imbalance in the blood count.
Some leukemia patients do not have high white blood cell counts visible during a regular blood count. This less-common condition is called aleukemia. The bone marrow still contains cancerous white blood cells which disrupt the normal production of blood cells, but they remain in the marrow instead of entering the bloodstream, where they would be visible in a blood test. For an aleukemic patient, the white blood cell counts in the bloodstream can
Page | 8

be normal or low. Aleukemia can occur in any of the four major types of leukemia, and is particularly common in hairy cell leukemia.
Also a sincere attempt to understand the pathophysiology of CVA, techniques used to measure the biochemical substances in blood, risk factors, prognosis, treatment of CVA, referring to literature databases about the biochemical effects has also been done. Data and statistics about the disease has also been provided in the report from reliable sources such as the World Health Organisation (WHO) website.
An appropriate understanding about the graveness of the disease and about the ground reality has also been approached. As far as the economic status of the patients were concerned it could be safely assumed that they belong to lower middle class and impoverished economic background since the study was done in a government run medical college. The photocopies of some of the investigations have also been included with prior permission.
Blood clotting is poor - As immature white blood cells crowd out blood platelets, which are crucial for blood clotting, the patient may bruise or bleed easily and heal slowly - he may also develop petechiae (a small red to purple spot on the body, caused by a minor hemorrhage).
Affected immune system - The patient's white blood cells, which are crucial for fighting off infection, may be suppressed or not working properly. The patient may experience frequent infections, or his immune system may attack other good body cells.
Anemia - As the shortage of good red blood cells grows the patient may suffer from anemia - this may lead to difficult or labored respiration (dyspnea) and pallor (skin has a pale color caused by illness).
Other symptoms - Patients may also experience nausea, fever, chills, night sweats, flu-like symptoms, and tiredness. If the liver or spleen becomes enlarged the patient may feel full and will eat less, resulting in weight loss. Headache is more common among patients whose cancerous cells have invaded the CNS (central nervous system).
Precaution - As all these symptoms could be due to other illnesses. A diagnosis of leukemia can only be confirmed after medical tests are carried out.
Page | 9

CAUSES OF LEUKEMIA
Experts say that different leukemias have different causes. The following are either known causes, or strongly suspected causes:
Artificial ionizing radiation
Viruses - HTLV-1 (human T-lymphotropic virus) and HIV (human immunodeficiency virus)
Benzene and some petrochemicals
Alkylating chemotherapy agents used in previous cancers
Maternal fetal transmission (rare)
Hair dyes
Genetic predisposition - some studies researching family history and looking at twins have indicated that some people have a higher risk of developing leukemia because of a single gene or multiple genes.
Down syndrome – pe ople with Down syndrome have a significantly higher risk of developing leukemia, compared to people who do not have Down syndrome. Experts say that because of this, people with certain chromosomal abnormalities may have a higher risk.
Electromagnetic energy - studies indicate there is not enough evidence to show that ELF magnetic (not electric) fields that exist currently might cause leukemia. The IARC (International Agency for Research on Cancer) says that studies which indicate there is a risk tend to be biased and unreliable.
No single known cause for any of the different types of leukemia exists. The known causes, which are not generally factors within the control of the average person, account for relatively few cases. The different leukemias likely have different causes.
Leukemia, like other cancers, results from mutations in the DNA. Certain mutations can trigger leukemia by activating oncogenes or deactivating tumor suppressor genes, and thereby disrupting the regulation of cell death, differentiation or division. These mutations may occur spontaneously or as a result of exposure to radiation or carcinogenicsubstances.
Among adults, the known causes are natural and artificial ionizing radiation, a few viruses such as human T-lymphotropic virus, and some chemicals, notably benzene and alkylating chemotherapy agents for previous malignancies. Use of tobacco is associated with a small increase in the risk of developing acute myeloid leukemia in adults. Cohort and case-control studies have linked exposure to some petrochemicals and hair dyes to the development of some forms of leukemia. A few cases of maternal-fetal transmission have
Page | 10

been reported. Diet has very limited or no effect, although eating more vegetables may confer a small protective benefit. No single known cause for all of the different types of leukemia exists. The different leukemias likely have different causes.
Known causes include natural and artificial ionizing radiation, viruses such as Human T-lymphotropic virus, and some chemicals, notably benzene and alkylating chemotherapyagents for previous malignancies. Use of tobacco is associated with a small increase in the risk of developing acute myeloid leukemia in adults. They concluded that there is limited evidence that high levels of ELF magnetic (but not electric) fields might cause childhood leukemia.
Exposure to significant ELF magnetic fields might result in twofold excess risk for leukemia for children exposed to these high levels of magnetic fields. Until the cause or causes of leukemia are found, there is no way to prevent the disease. Even when the causes become known, they may not be readily controllable, such as naturally occurring background radiation.
Viruses have also been linked to some forms of leukemia. Experiments on mice and other mammals have demonstrated the relevance of retroviruses in leukemia, and human retroviruses have also been identified. The first human retrovirus identified was human T-lymphotropic virus, or HTLV-1, which is known to cause adult T-cell leukemia. Some people have a genetic predisposition towards developing leukemia. This predisposition is demonstrated by family histories and twin studies. The affected people may have a single gene or multiple genes in common. In some cases, families tend to develop the same kinds of leukemia as other members; in other families, affected people may develop different forms of leukemia or related blood cancers. In addition to these genetic issues, people with chromosomal abnormalities or certain other genetic conditions have a greater risk of leukemia. For example, people with Down syndrome have a significantly increased risk of developing forms of acute leukemia (especially acute myeloid leukemia), and Fanconi anemia is a risk factor for developing acute myeloid leukemia.
Whether non-ionizing radiation causes leukemia has been studied for several decades. The International Agency for Research on Cancer expert working group undertook a detailed review of all data on static and extremely low frequency electromagnetic energy, which occurs naturally and in association with the generation, transmission, and use of electrical power. They concluded that there is limited evidence that high levels of ELF magnetic (but not electric) fields might cause childhood leukemia. Exposure to significant ELF magnetic fields might result in twofold excess risk for leukemia for children exposed to these high levels of magnetic fields. However, the report also says that methodological weaknesses and biases in these studies have likely caused the risk to be overstated. No evidence for a relationship to leukemia or another form of malignancy in adults has been demonstrated. Since exposure to such levels of ELFs is relatively uncommon, the World Health Organization concludes that ELF exposure, if later proven to be causative, would account for just 100 to 2400 cases worldwide each year, representing 0.2 to 4.9% of the total incidence of childhood leukemia for that year (about 0.03 to 0.9% of all leukemias).
Page | 11

DIAGNOSIS OF LEUKEMIA
Diagnosis is usually based on repeated complete blood counts and a bone marrow examination following observations of the symptoms, however, in rare cases blood tests may not show if a patient has leukemia, usually this is because the leukemia is in the early stages or has entered remission. A lymph node biopsy can be performed as well in order to diagnose certain types of leukemia in certain situations.
Following diagnosis, blood chemistry tests can be used to determine the degree of liver and kidney damage or the effects of chemotherapy on the patient. When concerns arise about visible damage due to leukemia, doctors may use an X-ray, MRI, or ultrasound. These can potentially view leukemia's effects on such body parts as bones (X-ray), the brain (MRI), or the kidneys, spleen, and liver (ultrasound). Finally, CT scans are rarely used to check lymph nodes in the chest.
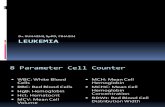
Fig: Complete Blood Count
Despite the use of these methods to diagnose whether or not a patient has leukemia, many people have not been diagnosed because many of the symptoms are vague, unspecific, and can refer to other diseases. For this reason, the American Cancer Society predicts that at least one-fifth of the people with leukemia have not yet been diagnosed.
Fig:Bone Marrow Examination
Page | 12

Mutation in SPRED1 gene has been associated with a predisposition to childhood leukemia. SPRED1 gene mutations can be diagnosed with genetic sequencing. In 2007, the germline loss-of-function mutations in SPRED1 were reported to originate a new autosomal dominant human disorder with multiple cafe´-au-lait spots, axillary freckling, macrocephaly, and learning difficulties. conclusion is that SPRED1 disorder generates predisposition to leukemia in children. The existence of an N-Ras mutation in this case infers that the SPRED mutation may have been a predisposing event that partially deregulated Ras signaling but acquired complex karyotype structural abnormality are essential to generate fully transformation to AML.
Page | 13

TREATMENT OF LEUKEMIA
Most forms of leukemia are treated with pharmaceutical medication, typically combined into a multi-drug chemotherapy regimen. Some are also treated with radiation therapy. In some cases, a bone marrow transplant is useful. Treatments for leukemia include:
Chemotherapy , which uses powerful medicines to kill cancer cells. This is the main treatment for most types of leukemia.
Radiation treatments . Radiation therapy uses high-dose X-rays to destroy cancer cells and shrink swollen lymph nodes or an enlarged spleen. It may also be used before a stem cell transplant.
Stem cell transplant . Stem cells can rebuild your supply of normal blood cells and boost your immune system. Before the transplant, radiation or chemotherapy may be given to destroy cells in the bone marrow and make room for the new stem cells. Or it may be given to weaken your immune system so the new stem cells can get established.
Biological therapy . This is the use of special medicines that improve your body's natural defenses against cancer.
For some people, clinical trials are a treatment option. Clinical trials are research projects to test new medicines and other treatments. Often people with leukemia take part in these studies.Some treatments for leukemia can cause side effects. Your doctor can tell you what problems are common and help you find ways to manage them.
Acute lymphoblastic
Management of ALL focuses on control of bone marrow and systemic (whole-body) disease. Additionally, treatment must prevent leukemic cells from spreading to other sites, particularly the central nervous system (CNS) e.g. monthly lumbar punctures. In general, ALL treatment is divided into several phases:
Induction chemotherapy to bring about bone marrow remission. For adults, standard induction plans include prednisone, vincristine, and an anthracycline drug; other drug plans may include L-asparaginase or cyclophosphamide. For children with low-risk ALL, standard therapy usually consists of three drugs (prednisone, L-asparaginase, and vincristine) for the first month of treatment.
Consolidation therapy or intensification therapy to eliminate any remaining leukemia cells. There are many different approaches to consolidation, but it is typically a high-dose, multi-drug treatment that is undertaken for a few months. Patients with low- to average-risk ALL receive therapy with antimetabolite drugs such
Page | 14

as methotrexate and 6-mercaptopurine (6-MP). High-risk patients receive higher drug doses of these drugs, plus additional drugs.
CNS prophylaxis (preventive therapy) to stop the cancer from spreading to the brain and nervous system in high-risk patients. Standard prophylaxis may include radiation of the head and/or drugs delivered directly into the spine.
Maintenance treatments with chemotherapeutic drugs to prevent disease recurrence once remission has been achieved. Maintenance therapy usually involves lower drug doses, and may continue for up to three years.
Alternatively, allogeneic bone marrow transplantation may be appropriate for high-risk or relapsed patients.
Chronic lymphocytic Leukemia
Decision to treat
Hematologists base CLL treatment on both the stage and symptoms of the individual patient. A large group of CLL patients have low-grade disease, which does not benefit from treatment. Individuals with CLL-related complications or more advanced disease often benefit from treatment. In general, the indications for treatment are:
Falling hemoglobin or platelet count
Progression to a later stage of disease
Painful, disease-related overgrowth of lymph nodes or spleen
An increase in the rate of lymphocyte production
Typical treatment approach
CLL is probably incurable by present treatments. The primary chemotherapeutic plan is combination chemotherapy with chlorambucil or cyclophosphamide, plus a corticosteroidsuch as prednisone or prednisolone. The use of a corticosteroid has the additional benefit of suppressing some related autoimmune diseases, such as immunohemolytic anemia orimmune-mediated thrombocytopenia. In resistant cases, single-agent treatments with nucleoside drugs such as fludarabine, pentostatin, or cladribine may be successful. Younger patients may consider allogeneic or autologous bone marrow transplantation.
Acute myelogenous Leukemia
The treatment of AML occurs in 2 phases. All histologic subtypes are currently treated the same way except for acute promyelocytic leukemia (M3 subtype).
The initial treatment phase of AML is called remission induction and the goal of remission induction therapy is to achieve a complete remission or disappearance of all detectable leukemia cells. After a complete remission is achieved, the second phase of treatment, post-
Page | 15

remission therapy, begins. Post-remission therapy is necessary because, although there may be no detectable cancer cells after remission induction, undetectable leukemia cells still exist and the leukemia will return without additional post-remission therapy. Post-remission therapy is often referred to as consolidation.
Many different anti-cancer drugs are effective for the treatment of AML. Treatments vary somewhat according to the age of the patient and according to the specific subtype of AML. Overall, the strategy is to control bone marrow and systemic (whole-body) disease, while offering specific treatment for the central nervous system (CNS), if involved.
In general, most oncologists rely on combinations of drugs for the initial, induction phase of chemotherapy. Such combination chemotherapy usually offers the benefits of earlyremission and a lower risk of disease resistance. Consolidation and maintenance treatments are intended to prevent disease recurrence. Consolidation treatment often entails a repetition of induction chemotherapy or the intensification chemotherapy with additional drugs. By contrast, maintenance treatment involves drug doses that are lower than those administered during the induction phase.
Fig: CHOP Therapy
Chronic myelogenous Leukemia
There are many possible treatments for CML, but the standard of care for newly diagnosed patients is imatinib (Gleevec) therapy. Compared to most anti-cancer drugs, it has relatively few side effects and can be taken orally at home. With this drug, more than 90% of patients will be able to keep the disease in check for at least five years, so that CML becomes a chronic, manageable condition.
In a more advanced, uncontrolled state, when the patient cannot tolerate imatinib, or if the patient wishes to attempt a permanent cure, then an allogeneic bone marrow transplantation may be performed. This procedure involves high-dose chemotherapy and radiation followed by infusion of bone marrow from a compatible donor. Approximately 30% of patients die from this procedure.
Page | 16

Hairy cell
Decision to treat
Patients with hairy cell leukemia who are symptom-free typically do not receive immediate treatment. Treatment is generally considered necessary when the patient shows signs and symptoms such as low blood cell counts (e.g., infection-fighting neutrophil count below 1.0 K/µL), frequent infections, unexplained bruises, anemia, or fatigue that is significant enough to disrupt the patient's everyday life.
Typical treatment approach
Patients who need treatment usually receive either one week of cladribine, given daily by intravenous infusion or a simple injection under the skin, or six months of pentostatin, given every four weeks by intravenous infusion. In most cases, one round of treatment will produce a prolonged remission.
Other treatments include rituximab infusion or self-injection with Interferon-alpha. In limited cases, the patient may benefit from splenectomy (removal of the spleen). These treatments are not typically given as the first treatment because their success rates are lower than cladribine or pentostatin.
T-cell prolymphocytic
Most patients with T-cell prolymphocytic leukemia, a rare and aggressive leukemia with a median survival of less than one year, require immediate treatment.
T-cell prolymphocytic leukemia is difficult to treat, and it does not respond to most available chemotherapeutic drugs. Many different treatments have been attempted, with limited success in certain patients: purine analogues (pentostatin, fludarabine,
Page | 17

cladribine), chlorambucil, and various forms of combination chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisone CHOP, cyclophosphamide, vincristine, prednisone [COP], vincristine, doxorubicin, prednisone, etoposide, cyclophosphamide, bleomycinVAPEC-B). Alemtuzumab (Campath), a monoclonal antibody that attacks white blood cells, has been used in treatment with greater success than previous options.
Some patients who successfully respond to treatment also undergo stem cell transplantation to consolidate the response.
Juvenile myelomonocytic
Treatment for juvenile myelomonocytic leukemia can include splenectomy, chemotherapy, and bone marrow transplantation.
Page | 18

EPIDEMIOLOGY OF LEUKEMIA
In 2000, approximately 256,000 children and adults around the world developed a form of leukemia, and 209,000 died from it.[2] This represents about 3% of the almost seven million deaths due to cancer that year, and about 0.35% of all deaths from any cause. Of the sixteen separate sites the body compared, leukemia was the 12th most common class of neoplastic disease, and the 11th most common cause of cancer-related death.
About 245,000 people in the United States are affected with some form of leukemia, including those that have achieved remission or cure. Approximately 44,270 new cases of leukemia were diagnosed in the year of 2008 in the US. This represents 2.9% of all cancers (excluding simple basal cell and squamous cell skin cancers) in the United States, and 30.4% of all blood cancers.
Among children with some form of cancer, about a third have a type of leukemia, most commonly acute lymphoblastic leukemia. A type of leukemia is the second most common form of cancer in infants (under the age of 12 months) and the most common form of cancer in older children. Boys are somewhat more likely to develop leukemia than girls, and white American children are almost twice as likely to develop leukemia than black American children. Only about 3% cancer diagnoses among adults are for leukemias, but because cancer is much more common among adults, more than 90% of all leukemias are diagnosed in adults
Page | 19

MODERN ADVANCEMENTS IN TREATMENT AND DIAGNOSIS OF LEUKEMIA
1.)Mutation in SPRED1 gene has been associated with a predisposition to childhood leukemia :Diagnosis of Chilhood Leukemia can be done
(Reference: Pasmant E, Ballerini P, Lapillonne H et al. SPRED1 disorder and predisposition to leukemia in
children. Blood 2009; 114:1131. )
(Reference:Batz C, Hasle H, Bergsträsser E, et al. (2010). "Does SPRED1 contribute to leukogenesis in juvenile myelomonocytic leukemia (JMML)?". Blood 115 (12): 2557–8.doi:10.1182/blood-2009-12-
260901. PMID 20339110)
Mutation in SPRED1 gene has been associated with a predisposition to childhood leukemia. SPRED1 gene mutations can be diagnosed with genetic sequencing. Sprouty-related, EVH1 domain-containing protein 1 (Spred-1) is a protein that in humans is encoded by the SPRED1gene located on chromosome 15q13.2 and has seven coding exons. Spred-1 is a member of the Sprouty family of proteins and is phosphorylated by tyrosine kinase in response to several growth factors. The encoded protein can act as a homodimer or as a heterodimer with SPRED2 to regulate activation of the MAP kinase cascade. Defects in this gene are a cause of neurofibromatosis type 1-like syndrome (NFLS).
Mutations in this gene are associated with
Legius syndrome.
Childhood leukemia
Fig: SPRED1 Gene
Page | 20

Sprouty-related, EVH1 domain containing 1
Available structures
PDB Ortholog search: PDBe, RCSB
List of PDB id codes
Identifiers
Symbols SPRED1; NFLS; hSpred1; spred-1
External IDs OMIM: 609291 MGI: 2150016HomoloGene: 24919 GeneCards: SPRED1 Gene
[show]Gene Ontology
Orthologs
Species Human Mouse
Entrez 161742 114715
Ensembl ENSG00000166068 ENSMUSG00000027351
UniProt Q7Z699 Q924S8
RefSeq (mRNA) NM_152594.2 NM_033524.2
RefSeq (protein) NP_689807.1 NP_277059.1
Location (UCSC) Chr 15:
38.54 – 38.65 Mb
Chr 2:
117.12 – 117.18 Mb
PubMedsearch [1]
2.) Gene Mutations Linked with AML(Acute Mylegeneous Leukemia) Outcome
(Reference: Patel JP, Gonen M, Figueroa ME et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. New England Journal of Medicine. 2012;366:1079-89.)
Page | 21

Among patients with acute myeloid leukemia (AML), those with certain genetic changes may benefit from high-dose induction chemotherapy. These results were published in the New England Journal of Medicine.
Acute myeloid leukemia is a cancer of the bone marrow and blood characterized by the rapid uncontrolled growth of immature white blood cells known as myelocytes. The disease is more common in adults than in children, with the average age at diagnosis being more than 65 years.
For several types of cancer—including AML—researchers are attempting to develop more individualized approaches to treatment by using specific characteristics of the cancer to guide treatment choices.
One factor that can affect response to treatment is the cancer’s genetic makeup. To explore how a broad range of genetic alternations affect AML’s prognosis and response to treatment, researchers examined 18 genes in 398 patients under the age of 60. The patients were participants in a clinical trial that compared high-dose and standard-dose daunorubicin.
The researchers identified several genetic alterations that affected AML prognosis. Information about the presence or absence of each of these may allow doctors to more accurately classify AML as favorable-risk, intermediate-risk, or unfavorable-risk.
Genetic changes were also linked with response to high-dose chemotherapy: patients with certain changes in the DNMT3A, NPM1, or MLL genes had better outcomes with high-dose chemotherapy than with standard-dose chemotherapy. In contrast, patients without changes in these genes did not benefit from high-dose chemotherapy.
These results suggest that more extensive genetic profiling of AML may influence treatment decisions and provide better information about a patient’s prognosis. The goal of this type of research is more individualized and more effective cancer treatment.
3.) Marqibo Approved for Treatment of Philadelphia-Negative ALL
(Reference: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm315027.htm)
Page | 22

The U.S. Food and Drug Administration (FDA) has approved Marqibo® (vincristine sulfate liposome injection) to treat adults with Philadelphia chromosome negative (Ph-) acute lymphoblastic leukemia (ALL) whose leukemia has returned or progressed following two or more treatment regimens. Adult ALL is a malignant disease or cancer of the blood characterized by the rapid uncontrolled growth of abnormal, immature white blood cells known as lymphoblasts. There are approximately 6,000 new cases of adult ALL each year in the United States, with approximately 1,500 deaths. Philadelphia chromosome negative (Ph-) ALL is a rare subset of the disease. Marqibo is a new, targeted, nanoparticle-encapsulated, cancer agent designed to improve efficacy and reduce toxicity. Marqibo contains vincristine, a commonly used anti-cancer agent, encased within a liposome, a drug delivery vehicle. Marqibo is administered via weekly injection.
4.) One Subset of Childhood Acute Lymphoblastic Leukemia is Best Treated with Chemotherapy
(Reference: Schrappe M, Hunger SP, Pui CH, et al. Outcomes after induction failure in childhood acute lymphoblastic leukemia. New England Journal of Medicine. 2012; 366:1371-1381.)
A subset of young patients with acute lymphoblastic leukemia (ALL) who fail to achieve remission after the initial weeks of intense chemotherapy known as induction therapy appear to have better outcomes with additional chemotherapy rather than bone marrow transplantation, according to the results of an international study published in the New England Journal of Medicine.
ALL—a fast-growing cancer of the white blood cells—is the most commonly diagnosed type of leukemia in children. Each year, there are approximately 6,000 new cases of ALL diagnosed in the United States.
The treatment of childhood ALL is carried out in two phases. The initial treatment phase is called remission induction and its goal is to achieve a complete remission or disappearance of all detectable leukemia cells in the peripheral blood and bone marrow. After a complete remission is achieved, the second phase of treatment, called post-remission therapy, begins. Post-remission therapy is necessary because despite achieving a complete remission of leukemia with induction treatment, hidden undetectable leukemia cells still exist and the leukemia will return without additional post-remission therapy.
5.) Arzerra™ Approved for Refractory Chronic Lymphocytic Leukemia
Page | 23

(Reference:Genmab and GSK press release. GSK and Genmab receive accelerated approval for ARZERRA™Available at:http://www.gsk.com/media/pressreleases/2009/2009_us_pressrelease_10077.htm Accessed October 28, 2009.)
The targeted therapy Arzerra™ (ofatumumab) has been granted accelerated approval by the U.S. Food and Drug Administration for treatment of patients with chronic lymphocytic leukemia (CLL) that is refractory to Fludara® (fludarabine) and Campath® (alemtuzumab).
Chronic lymphocytic leukemia (CLL) is the most common form of adult leukemia. The American Cancer Society estimates that approximately 15,000 people will be diagnosed with CLL this year. Currently, there are approximately 95,000 people in the United States living with CLL.
CLL is characterized by the production of atypical lymphocytes. Lymphocytes are specialized immune cells that exist in two forms: B- and T-cells. These cells are produced in the bone marrow and each serves a specific function in aiding the body fight infection.
6.) Childhood CT Scans Linked to Leukemia and Brain Cancer Later in Life
(Reference:Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. The Lancet, Early online publication: June 7, 2012. Available at: doi:10.1016/S0140-6736(12)60815-0)
Children and young adults who undergo multiple computed tomography (CT) scans have an increased risk of leukemia and brain tumors in the decade following their first scan, according to the results of a study published in The Lancet.
CT scans are a common diagnostic tool used for imaging body tissues and organs. A CT scan takes a series of detailed pictures of areas inside the body taken from different angles. The pictures are created by a computer linked to an X-ray machine. A CT scan can reveal some soft-tissue and other structures that cannot even be seen in conventional X-rays.
Children who suffer head injuries or who have been diagnosed with a life-threatening illness might undergo one or more CT scans during the diagnostic and treatment process. The risk with CT scans is that they deliver a dose of ionizing radiation to the area of the body being scanned. Even at low doses, ionizing radiation can cause damage that may increase the risk of cancer. Children typically face a higher risk of cancer from ionizing radiation exposure than do adults exposed to similar doses.
7.) Survivors of Some Childhood Cancers May Face Cognitive Impairment
Page | 24

(Reference: Kadan-Lottick NS, Zeltzer LK, Liu Q, et al. Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. Journal of the National Cancer Institute [early online publication]. May 10, 2010.)
Survivors of non-central nervous system (CNS) childhood cancers reported a statistically and clinically significantly higher rate of neurocognitive impairment than their cancer-free siblings, according to the results of a study published in the Journal of the National Cancer Institute.
The survival rate for childhood cancer is high, with 80% of children and adolescents surviving five or more years. One potential late effect for these survivors is neurocognitive impairment, which can affect quality of life and overall daily functioning. Children who survive CNS cancers face impaired neurocognitive functioning due to the location of their tumors as well as the treatment directed at the cranial area; however, some research indicates that even survivors of non-CNS cancers are faced with impaired cognitive functioning.
A retrospective analysis involved 5,937 adult survivors of non-CNS cancers and 382 siblings. Participants completed neuropsychological assessments and were then compared. The data indicated that survivors of childhood cancers were 50% more likely than their cancer-free siblings to face cognitive impairment.
13% of survivors experienced impairment in task efficiency compared with 7.3% of siblings.
12.5% of survivors experienced impaired memory compared with 7.6% of siblings.
21.2% of survivors experienced impaired emotional regulation compared with 14.4% of siblings.
REFERENCES
Page | 25

1. Leukemia, in Mosby’s Medical, Nursing &Allied Health Dictionary, Fourth Edition,
Mosby-YearBook, Inc.,1994, p. 903
2. Mathers, Colin D, Cynthia Boschi-Pinto, Alan D Lopez and Christopher JL Murray
(2001). "Cancer incidence, mortality and survival by site for 14 regions of the
world". Global Programme on Evidence for Health Policy Discussion Paper No. 13(World
Health Organization).
3. "SEER Stat Fact Sheets: Leukemia". National Cancer Institute. 2011. ""Approximately
10.8% were diagnosed under age 20""
4. Jameson, J. N. St C.; Dennis L. Kasper; Harrison, Tinsley Randolph; Braunwald, Eugene;
Fauci, Anthony S.; Hauser, Stephen L; Longo, Dan L. (2005). Harrison's principles of
internal medicine. New York: McGraw-Hill Medical Publishing Division.ISBN 0-07-
140235-7.
5. Finding Cancer Statistics » Cancer Stat Fact Sheets »Chronic Lymphocytic
Leukemia National Cancer Institute.
6. Colvin GA, Elfenbein GJ (2003). "The latest treatment advances for acute myelogenous
leukemia". Med Health R I 86 (8): 243–6. PMID 14582219.
7. Patients with Chronic Myelogenous Leukemia Continue to Do Well on Imatinib at 5-Year
Follow-Up Medscape Medical News 2006.
8. American Cancer Society (2010). "How is Leukemia Diagnosed?". Detailed Guide:
Leukemia - Adult Chronic. American Cancer Society. Retrieved 4 May 2010
9. Pasmant E, Ballerini P, Lapillonne H et al. SPRED1 disorder and predisposition to leukemia
in children. Blood 2009; 114:1131.
10. Cullen M, Steven N, Billingham L, Gaunt C, Hastings M, Simmonds P, Stuart N, Rea D,
Bower M, Fernando I, Huddart R, Gollins S, Stanley A (2005). "Antibacterial prophylaxis
after chemotherapy for solid tumors and lymphomas.". N Engl J Med 353 (10): 988–
98. doi:10.1056/NEJMoa050078. PMID 1614828411. Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, Glick JH, Coltman
CA Jr, Miller TP (1993). "Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin's lymphoma.". N Engl J Med 328 (14): 1002–6. doi:10.1056/NEJM199304083281404. PMID 7680764.
12. Pasmant E, Ballerini P, Lapillonne H et al. SPRED1 disorder and predisposition to leukemia
in children. Blood 2009; 114:1131.
13. Kadan-Lottick NS, Zeltzer LK, Liu Q, et al. Neurocognitive functioning in adult survivors
of childhood non-central nervous system cancers. Journal of the National Cancer
Institute [early online publication]. May 10, 2010.
14. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and
subsequent risk of leukaemia and brain tumours: a retrospective cohort study. The Lancet,
Early online publication: June 7, 2012. Available at: doi:10.1016/S0140-6736(12)60815-015. Genmab and GSK press release. GSK and Genmab receive accelerated approval for
ARZERRA™Available Page | 26

at:http://www.gsk.com/media/pressreleases/2009/2009_us_pressrelease_10077.htm Accessed October 28, 2009.)
16. Schrappe M, Hunger SP, Pui CH, et al. Outcomes after induction failure in childhood acute
lymphoblastic leukemia. New England Journal of Medicine. 2012; 366:1371-1381.
17. Patel JP, Gonen M, Figueroa ME et al. Prognostic relevance of integrated genetic profiling
in acute myeloid leukemia. New England Journal of Medicine. 2012;366:1079-89.
18. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm315027.htm
19. Batz C, Hasle H, Bergsträsser E, et al. (2010). "Does SPRED1 contribute to leukogenesis
in juvenile myelomonocytic leukemia (JMML)?". Blood 115 (12): 2557–
8.doi:10.1182/blood-2009-12-260901. PMID 20339110.
Page | 27