Lapjag Ugd 8 Feb - English
-
Upload
asri-paramytha -
Category
Documents
-
view
13 -
download
0
description
Transcript of Lapjag Ugd 8 Feb - English

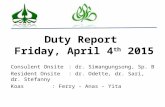
Doctors on duty : dr. Gerald, dr. Karen & dr. FitriaCoass on duty : Asri Paramytha
Twinda Rarasati
EMERGENCY REPORT7TH FEBRUARY 2015

PATIENTS RECAPITULATION Mrs. S 77 yo, ADHF, Hypertension stage I
Mrs. M 55 yo, Urticaria
Mrs. A 37 yo, Unilateral pleural efusion
Mrs. S 32 yo, Gum bleed susp DHF
Mr. S 67 yo, Dyspneu ec susp pelural efusion
Mr. S 83 yo, susp pneumonia in Geriatri
Mrs. E 60 yo, Sepsis ec. Pneumonia
Mr. T 50 yo, Acute ecsaserbation COPD
Mr. D 54 yo, ACS

PATIENT’S IDENTITY• Name : S • Sex : Female• Age : 32 years old• Marital Status : Married• Address : Lampung• Medical Record : 45 03 87• Time of Arrival : 10:10 am

ANAMNESIS• Autoanamnesa and Alloanamnesa on 07/02/15 at 10:10 AM
• Chief Complain: Gum-bleeding
• Additional Complain: Fever, nausea, dizyness, vomit, low appetite and constipation

CURRENT ILLNESS
The patient was admitted to the RSPAD due to gum bleeding. The gum-bleeding was started 1 hour before admission, 4 times and was still bleeding during the anamnesis. Gum-bleed was not preceed by any kind of trauma. Patient also complained having fever since 4 days before admission. Fever was felt continously.

CURRENT ILLNESS
The temperature doesn’t increase at the night or decrease in the morning. The patient did not measure the temperature during the fever. Fever was accompanied with dizzyness. Patient didn’t complain any nosebleed or pain behind her eye. Patient also complained having nausea and vomit. Patient vomitted 2 times before admission, vomit consists of fluid and food, no blood. Patient had low appetite since 4 days before admission. Patient had problems with her defecation.

CURRENT ILLNESS
She was constipated since 4 days before admission. There was no complain about urination. Patient came from Lampung 5 days before admission. Patient had gone to a clinic and was prescribed Paracetamol, Amoxicilin, a medicine for her nausea, stomach, and vitamin (patient could not remember the names of the medicine).

• Patient never experienced the same symptoms before
• No family member are experiencing the same symptoms
PAST ILLNESS
FAMILY ILLNESS

PHYSICAL EXAMINATIONVITAL SIGNS
• General State : Mild Sickness• Consciousness : Compos Mentis• Blood Pressure : 100/70 mmHg• Pulse : 96 x/minute, regular• Respiratory Rate : 20 x/minute, cepat dalam• Temperature : 36.6oC• Body Weight : 54 kg• Body Height : 162 cm• BMI : 20.57 (Normoweight)

PHYSICAL EXAMINATIONGeneral Examination• Head : Normocephal• Eye : anemic conjunctiva (-/-), icteric sclera (-/-), • Ears : normotia, discharge (-)• Nose : septum deviation (-), discharge (-)• Mouth : Gum bleed (+)• Neck : lymph nodes enlargement (-)

• Thorax : symmetric, intercostal retraction (-)• Cor : regular 1st and 2nd heart sound, murmur (-),
gallop (-) • Pulmo : vesicular breathing sounds +/+, ronkhi -/-, wheezing
-/-• Abdomen : flat, not distended, timpani, no enlargement of liver
& lien, BS normal, tenderness in epigastric area (-)• Extremities : cold, pitting edema (-), cyanosis (-)
CRT < 2 seconds, rumple leed (-)

DIAGNOSTIC PLANS
RESULT NORMAL RANGE
Hematologi rutin:
Hb 16.4 13 - 18 g/dl
Ht 47 40 – 52 %
Erythrocyte 5.6 4.3 - 6.0 mil /ul
Leukocyte 3420 4800 - 10800/ul
Thrombocyte 24000 150000 - 400000/ul
MCV 83 80 – 96 fL
MCH 29 27 - 32 pg
MCHC 35 32 – 36 g/dL
LABORATORIUM

RESUME
Patient, female, 32 yo, was admitted to the RSPAD due to gum bleeding. The gum-bleeding was started 1 hour before admission, 4 times and was still bleeding during the anamnesis. Patient also complained having fever since 4 days before admission. Fever was felt continously.
Fever was accompanied with dizzyness. Patient also complain having nausea and vomit. Patient vomitted 2 times before admission, vomit consists of fluid and food, no blood. Patient had low appetite since 4 days before admission. Patient had problems with her defecation. She was constipated since 4 days before admission.
Patient came from Lampung 5 days before admission. Patient had gone to a clinic and was prescribed Paracetamol, Amoxicilin, a medicine for her nausea, stomach, and vitamin.
From the physical examination, the blood pressure was 100/70 mmHg and gum bleed (+). From the laboratory findings, there were found thrombocytopenia and leukopenia.

PROBLEMS LIST
• Gum bleed on Fever day 4

Gum bleed ec. Supsect DHF DD/ Typhoid Fever
• Anamnesis: Patient had gum bleed since a few hours before admission. Also had fever 4 days before admission. Nausea (+) Vomiting (+) Low appetite (+)
• Physical examination: gum bleed (+)
• Lab finding: leukopenia (3240) & thrombocytopenia (24.000)
• Plan:
• Diagnostic: Complete blood count, IgM IgG
• Therapy: IVFD RL 30 tpm
ASSESSMENT FOR WORKING DIAGNOSE

DD/ Typhoid Fever
• Anamnesis: Patient had fever 4 days before admission. Nausea (+) Vomit (+). Constipation (+)
• Physical examination: Rumple leed (-)
• Lab finding: leukopenia (3240)
• Plan:
• Diagnostic: Tubex TF
• Therapy:
ASSESSMENT FOR WORKING DIAGNOSE

PROGNOSIS
• Qua ad vitam : ad bonam
• Qua ad functionam : ad bonam
• Qua ad sanationam : Dubia

THANK YOU