INSIDE - RACGP
Transcript of INSIDE - RACGP

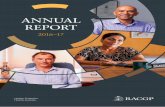
Taking ownership
Tasmania’s Dr Columbine Mullins appreciates the independence of being a GP and a practice owner
INSIDE
Conference for general practiceHighlights of the recent GP16 in Perth
AntimicrobialsWorking to challenge antibiotic resistance
RACGP digitalDelving into the new myRACGP member portal
ISSUE 11, NOVEMBER 2016
www.racgp.org.au/goodpractice

3913_BP_summit_GP_210X275.indd 1 10/10/2016 1:19 pm

Good Practice is printed on PEFC certi�ed paper, meaning that it originates from forests that are managed sustainably. PEFC is the Programme for the Endorsement of Forest Certi�cation schemes. PEFC is an international certi�cation programme promoting sustainable forest management which assures consumers that a forest product can be tracked from a certi�ed, managed forest through all steps of processing and production in the supply chain by a Chain of Custody process.
Editorial notes
© The Royal Australian College of General Practitioners 2016. Unless otherwise indicated, copyright of all images is vested in the RACGP. Requests for permission to reprint articles must be made to the editor. The views contained herein are not necessarily the views of the RACGP, its council, its members or its staff. The content of any advertising or promotional material contained within Good Practice is not necessarily endorsed by the publisher.
We recognise the traditional custodians of the land and sea on which we work and live.
3Reprinted from Good Practice Issue 11, November 2016
Published by
The Royal Australian College of General Practitioners 100 Wellington Parade East Melbourne Victoria 3002
03 8699 0414 [email protected] www.racgp.org.au/goodpractice
ABN 34 000 223 807 ISSN 1837-7769
Editor: Paul HayesJournalist: Amanda LyonsGraphic Designer: Matthew BowryProduction Coordinator: Beverley GutierrezPublications Manager: Jenni Stiffe
Advertising enquiriesSye Hughes0474 500 [email protected]
18
24
ContentsIssue 11, November 2016
10
06
22
04 Your College
RACGP news and events for November.
06 Conference for General Practice Clinical, digital, leadership
The RACGP’s 2016 Conference for General Practice
was its biggest and best yet.
10 Antimicrobials
Challenging resistance Altering general practice prescribing
can play a significant role in combating antibiotic resistance.
14 RACGP Digital Digital home
myRACGP, the RACGP’s new online portal, is a secure and easily-accessible location for
communication and exclusive content.
17 Ethics in General Practice
Patient information When can GPs disclose information
about a patient to a third party?
18 Technology in General Practice
Mobilising healthcare The possibilities presented by mobile
health are exciting, but care must be taken when implementing it within
general practice.
22 GP Profile
By design Dr Columbine Mullins has embraced the
opportunities that come with owning your own practice.
24 In My Practice
A healthy union The merger of two practices in the New South Wales town of Forbes has helped
to increase resources and improve the provision of quality healthcare.
26 RACGP Specific Interests
Dermatology Providing guidance and education across
the entire spectrum of dermatology in general practice.

4 Reprinted from Good Practice Issue 11, November 2016
Imag
es J
ohn
Mau
nder
; Jaz
min
Dan
iells
; Seb
astia
n K
irby;
Zac
h D
awes
; Joa
nne
Mac
kson
; Stri
ng T
heor
y
YOUR COLLEGE
Member forum at GP16
The second-ever RACGP member forum was held at GP16 on Friday 30 September. Once again hosted by journalist Ali Moore before a live audience, questions were pre-submitted by RACGP members or asked by those in the audience.
The forum consisted of two core panellists and two guest panellists for each the two topics, ‘digital disruption’ and ‘revalidation’, which were selected by RACGP members prior to the event.
The core panellists were Dr Bastian Seidel, new RACGP President, and Dr Sean Stevens, Deputy Chair of RACGP WA. For the first topic, ‘digital disruption’, they were joined by Dr Nathan Pinskier, Chair of the RACGP Expert Committee (REC) – eHealth and Practice Systems, and Dr Marcus Tan, CEO and Medical Director of Health Engine.
Panellists navigated questions about healthcare’s relatively slow adoption of digital technology, the drivers that might
lead to change, and possible effects on healthcare in the future. Dr Pinskier described technology as a tool rather than a solution, regardless of its potential.
‘Technology is an enabler. It is a tool to be used appropriately,’ he said.
For the second topic, ‘revalidation’, Dr Seidel and Dr Stevens were joined by Dr Janice Bell, Chair of REC – Post Fellowship Education and CEO of Western Australian General Practice Education and Training (WAGPET), and Professor Lambert Schuwirth, Strategic Professor of Medical Education at the Flinders University School of Medicine.
Panellists agreed that revalidation does not necessarily represent the best approach to ensuring patient safety and confidence in doctors. Dr Bell argued that the RACGP offers more useful educational pathways for GPs.
While Dr Seidel agreed, he also observed that the RACGP must be involved in
discussions with Federal Government over the issue to prevent a system being designed and imposed without an understanding of the needs of general practice.
Log in to shareGP or RACGP.TV to view the full video of the second RACGP member forum.
Turn to page 6 for a detailed round-up of GP16.
(L–R) Dr Bastian Seidel, Dr Marcus Tan, Ali Moore, Dr Nathan Pinskier and Dr Sean Stevens.
President Dr Bastian Seidel believes the RACGP must be involved with the Federal Government in any discussions regarding the issue of revalidation.

5Reprinted from Good Practice Issue 11, November 2016
Digital ageEach of the successful entrants in the recent GP16 photo competition provided an inspired response when asked to ‘show how you embrace the digital age in your studies or daily general practice’.
The five RACGP student members who were named winners – Zach Dawes (Qld), Jazmin Daniells (NSW), Joanne Mackson (NSW), John Maunder (Qld) and Sebastian Kirby (Vic) – were awarded a prize package that included full delegate registration for GP16, return airfare to Perth and four nights’ accommodation, valued at up to $2990.
RACGP events calendar
November 2016
VIC
Perform CPR – A workshop for GPsWednesday 9 November, 6.00–8.00 pm, RACGP House, East Melbourne
Contact 03 8699 0488 or [email protected]
WA
CPR certification course Wednesday 16 November, 6.30–8.30 pm, College House, Perth
Contact 08 9489 9555 or [email protected]
WA
Navigate the corridors of ageing: Caring for elderly patientsSaturday 12 November, 8.30 am – 4.00 pm, College House, Perth
Contact 08 9489 9555 or [email protected]
VIC
Clinical emergency management program – intermediate Friday 18 November, 8.30 am – 5.00 pm, Melbourne
Contact 03 8699 0488 or [email protected]
VIC
Psychodynamic principles workshop for GPs (part 2) Saturday 12 November, 9.00 am – 5.00 pm, RACGP House, East Melbourne
Contact 03 8699 0488 or [email protected]
VIC
Clinical emergency management program – advanced Saturday to Sunday, 19–20 November, 8.15 am – 5.00 pm Melbourne
Contact 03 8699 0488 or [email protected]
SA
Introduction to point of care ultrasound for rural GPs Saturday 12 November, 8.30 am – 4.30 pm, College House, North Adelaide
Contact 1800 636 764 or [email protected]
VIC
‘Caution ice – slippery surface’ Wednesday 23 November, 8.00–9.30 pm (registration from 7.30 pm), RACGP House, East Melbourne
Contact 03 8699 0488 or [email protected]
QLD
Clinical emergency management program – advanced Saturday to Sunday 12–13 November, 8.15 am – 5.00 pm, Queensland University of Technology, Kelvin Grove Campus, Brisbane
Contact 07 3456 8944 or [email protected]
TAS
Accredited CPR workshops for RACGP members Saturday 26 November, 9.30–10.30 am or 10.30–11.30 am, College House, Hobart
Contact 03 6234 2200 or [email protected]
NSW
Procedural skills for IMGs preparing for RMO roles Sunday 13 November, 8.45 am – 5.15 pm, RACGP House, North Sydney
Contact 02 9886 4748 or [email protected]
QLD
CPR workshop Tuesday 29 November, 6.30–8.30 pm, College House, Brisbane
Contact 07 3456 8930 or [email protected]
Visit www.racgp.org.au/education/courses/racgpevents for further RACGP events.
John Maunder: ‘Technology lets me carry my textbooks
with me – wherever I go.’
Jazmin Daniells: ‘Embracing winter sun & reviewing clinical exams. Efficient & Vit D sufficient.’
Joanne Mackson: ‘Study with the sheep, study at the snow, study anytime, anywhere I go!’
Sebastian Kirby: ‘Digital notebooks to Indigenous
health on twitter – all at the swipe of a finger.’
Zach Dawes: ‘Medicine, technology and sticky tape. Better then any anatomy textbook I've seen.’
Visit the RACGP Facebook page to view the full gallery of entries.

Imag
e xx
xxx
6 Good Practice Issue 11, November 2016
xxxxx xxxxxxxxxxx xxxxxXXXXX
xxxxxxxxxx
xxxxxxxxxxxxx
xxxxxxxx
>>
XXX
Imag
e xx
xxx
6 Good Practice Issue 11, November 2016
xxxxx xxxxxxxxxxx xxxxxXXXXX
xxxxxxxxxx
xxxxxxxxxxxxx
xxxxxxxx
>>
XXX
The length and breadth of the RACGP was on full display at its recent Annual Conference for General Practice – GP16 – held in Perth from 29 September to 1 October. All aspects of the conference theme, ‘Clinical, Digital, Leadership’, were represented through its dozens of presentations, workshops, training sessions, posters and much more.
A record number of more than 1800 GPs, healthcare professionals and other delegates came together for the conference, where they were able to mix with colleagues and celebrate general practice, and take advantage of the many learning opportunities on offer.
The first major event was the Academic Session, Fellowship and Awards Ceremony at the University of Western Australia
(UWA). The learned surrounds of UWA’s Winthrop Hall provided
a fitting location for the RACGP to
present its
annual awards, including GP, supervisor, registrar, rural registrar and general practice of the year, as well as awards from the Rural and Aboriginal and Torres Strait Islander faculties.
The Academic Session also saw the RACGP welcome a new generation of GPs with the admission of more than 120 New Fellows, acknowledging a significant milestone in the life and career of so many GPs throughout Australia.
‘We celebrate the success of the New Fellows and look forward to the contribution they will make to the future of general practice,’ Dr Frank R Jones, RACGP Immediate Past President, told the audience, including New Fellows’ friends and family.
The New Fellows, in turn, gave Dr Jones a standing ovation in thanks for his work over two years as RACGP President, a time he referred to as a ‘privilege’ and a ‘wild ride’. Dr Jones applauded the efforts of all within the RACGP, especially its members, before handing the presidential chains to new RACGP President Dr Bastian Seidel.
Clinical, digital, leadership
CONFERENCE FOR GENERAL PRACTICE
6 Reprinted from Good Practice Issue 11, November 2016
Imag
es S
tring
The
ory
PAUL HAYES
The RACGP’s 2016 Conference for General Practice was its biggest and best yet.

Imag
e xx
xxx
7Good Practice Issue 11, November 2016
XXX
Imag
e xx
xxx
7Good Practice Issue 11, November 2016
XXX
Dr Seidel commended Dr Jones’ work in raising the profile of GPs and the RACGP.
‘The RACGP has never been in a better position,’ he said. ‘The nation has finally taken notice of the RACGP as the peak body for general practice.
‘We are and always will be the united college for all general practitioners.’
A great startConference convener and RACGP WA Chair Dr Tim Koh officially opened GP16 on the morning of Thursday 29 September. Dr Koh was excited by the opportunities the conference was set to offer its delegates.
‘We will look at the challenges ahead for our profession and ask, “How can we be best prepared for those challenges and solve the problems they present?”’, he told audience members.
Phil Walleystack, renowned WA entertainer and local Noongar man, performed a stirring Welcome to Country, playing his didgeridoo alongside a cello. He used this combination as a symbol for how the people of Australia can come together in a more meaningful way.
Clockwise from far left: Convener Dr Tim Koh opened GP16; Immediate Past President Dr Frank R Jones officially handed the role to Dr Bastian Seidel at the conference; more than120 New Fellows were welcomed into the RACGP.
Twitter wallGPs took to Twitter in huge numbers throughout GP16, discussing what they were learning and experiencing using the #GP16perth hashtag.
Liz Sturgiss – @LizSturgiss What an experience! Marathon AGM and convocation. Great to be part of a passionate college! @tskkoh @RACGP #GP16Perth
Dennison Cheung – @Den_Cheung Inspirational research done by general practitioners being showcased at the #GP16Perth Research Plenary #shareGP
Michael Wright – @wrightdrmcReally helpful workshop on iron therapy in GP – iron infusion real option – esp for those oral intolerant patients. Thx @ByrneTheD #GP16perth
Charlotte Hespe – @runningdoc14Wonderful opportunity to chat with great women leaders #GP16Perth #WomenMatter @NoGreatMischief @MSmithFOAMed @ninajrobertson
Gillian Gould – @GillianSGouldHonoured to be part great session on #smoking and #respiratory @racgp @uon_research
‘You see how the oldest instrument in the world, the didgeridoo, along with the cello can work so beautifully, and that’s how we have got to do it as a people – work together and walk together on this country, hand-in-hand, to make a better nation,’ he said.
Dr Jones then addressed the audience, underlining the vital importance general practice plays in national healthcare. He praised the efforts of all GPs and the RACGP.
‘The college has raised its profile in the life of individual GPs,’ he said. ‘We are the frontline of preventive medicine and we are in an extremely fortunate position of leadership within our communities.
‘I urge you all to remain committed to our profession and the future of general practice.’
Keynote speaker Dr Sam Prince then stepped to the podium, regaling the audience with three inspirational stories about education, adventure and scabies; Bunnings warehouse, infertility and burritos; and compassion, health colliding with tech, and a grumpy CT machine. >>
Stay connectedLog in to shareGP or RACGP.TV to view video highlights from GP16.
Reprinted from Good Practice Issue 11, November 2016 7

Imag
es S
tring
The
ory
8 Reprinted from Good Practice Issue 11, November 2016
CONFERENCE FOR GENERAL PRACTICE
>> Dr Prince, a medical doctor and entrepreneur and philanthropist who is the founder of the Zambrero restaurant chain, as well as the E-magine Foundation and the One Disease not-for-profit organisation, spoke about what he had learned in and out of the healthcare profession.
In telling stories that stretched from remote Arnhem Land to Sri Lanka to Sydney, Dr Prince lauded the work of GPs and other healthcare providers, while also challenging all in the profession to ask if they could do better.
‘When I think about the doctors that have gone before us, who had so much damn resilience to change things, I wonder and imagine what general practice could look like,’ he said.
Federal Health Minister Sussan Ley closed the plenary, assuring GPs that she hears their message and understands their value to a robust healthcare system.
‘A strong primary care system is fundamental to a strong national health system,’ she said. ‘I do recognise and regularly hear your message that a dollar invested in primary care saves many
Clockwise from top left: Phil Walleystack performed a rousing Welcome to Country; keynote speaker Dr Sam Prince challenged all healthcare professionals to ask what they could do better; Rosie Batty inspired the audience at the closing plenary with her powerful comments about domestic violence and the role GPs can play in its detection and management.
more dollars down the track, and this is something I would like to continue to work in partnership with [the RACGP] to champion.
‘It’s why we’re taking up the reforms GPs have longed campaigned for, like Health Care Homes. These were reforms the RACGP brought to me via their concept for the patient-centred medical home.’
Never stop learningThis year’s conference program was, as always, packed with a vast range of events and learning opportunities, including oral presentations, hands-on workshops, active learning modules, research sessions and short papers. The broad canvas of topics included vital areas such as refugee health, respiratory and smoking, rural and remote healthcare, sexual health, chronic disease, cultural awareness, Aboriginal and Torres Strait Islander health, and many more.
The conference exhibition hall also proved a hive of activity. With a record of more than 125 exhibitors, there was plenty of choice for delegates who wanted to learn more about organisations working in the healthcare space.
The RACGP’s booth was a hub at the centre of the hall, with many of the college’s key areas represented. GPs were able to conduct a rural career health check, explore the new myRACGP member portal, check in on their QI&CPD status, and ‘have a yarn’ with the team from Aboriginal and Torres Strait Islander Health.
This year’s exhibition hall also featured the new ‘Interactive product zone’. This popular addition allowed GPs to get a genuine feel for new products and actually touch and use items on display. The ‘Recharge lounge’ was again a hit with attendees, who were able revitalise themselves with coffee and ice-cream, and even a massage.
GP16 was also the venue for the RACGP’s 59th Annual General Meeting (AGM) and Convocation.
Always a major event, Convocation provides RACGP members the opportunity to be heard on their thoughts and beliefs about the current and future states of general practice. The ongoing Governance Review was a major topic this year in what was a lengthy debate.
The AGM was followed by the RACGP’s second-ever member forum, in which GPs from all over Australia sat on a panel to delve into the member-selected topics ‘revalidation’ and ‘digital disruption’ (refer to page 4 for more information on the member forum).
GPs were able to upskill and obtain QI&CPD points with the many hands-on workshops on offer throughout the conference.

9Reprinted from Good Practice Issue 11, November 2016
Attendees were also provided with lots of opportunities for networking and socialising with their healthcare colleagues.
New Fellows and registrars were able to get together and build their own desserts at the ‘Sweet Time’ event, while students gathered at their own welcome and networking breakfast.
All delegates were invited to the GP16 Welcome Reception at the conclusion of the conference’s first day, and the RACGP Foundation’s morning walk was again a hit, with the intrepid walkers treated to a thorough tour of Perth early on Friday morning.
The conference’s social calendar closed with its spectacular Gala Dinner, where recently retired South Australian GP Dr John Litt was presented with the Rose-Hunt Award, the highest honour the RACGP bestows on any of its members.
Fitting conclusionGP16 came to an end with the closing plenary, at which inspiring domestic violence survivor and campaigner Rosie Batty addressed the audience. She reminded GPs of their powerful position and the vital
Looking to next yearPlans are well and truly underway for the RACGP’s next Annual Conference for General Practice – GP17 – to be held in Sydney 26–28 October 2017.
With an overarching theme of ‘The foundation of patient-centred care’, GP17 will provide attendees with the opportunity to connect with colleagues and broaden their clinical knowledge, while enjoying the natural beauty and vibrancy of Sydney.
Visit gp17.com.au for more information.
GP17
role they can play in helping people who are experiencing domestic violence.
‘It is in your practice ... patients who are visiting you on a daily basis will be experiencing violence in their homes,’ she said. ‘Your very role is to ask the question when you know something is wrong, when that person may be blaming themselves.
‘They may not even think they are worthy of someone like you taking the time to care.’
Dr Seidel also took to the stage in one of his first official acts as the new RACGP President, paying tribute to the efforts of the college and all of those involved in bringing together the conference.
‘GP16 has been an exceptional event,’ he said. ‘Our profession has been presented with an extraordinary range of topics that really are at the heart of general practice.’
Dr Koh called GP16 ‘the biggest and most successful RACGP conference to date’ before officially handing the conference message stick to GP17 conference convener, RACGP NSW&ACT Chair Dr Guan Yeo.
‘I am excited to officially assume the role of GP conference convener for 2017,’ Dr Yeo said.
‘I very much look forward to welcoming all of you next year in spectacular Sydney.’

10 Reprinted from Good Practice Issue 11, November 2016
Imag
es C
hris
Del
Mar
; Jus
tin C
olem
an; J
ohn
Turid
ge
ANTIMICROBIALS
According to Prof Chris Del Mar, Professor of Public Health at Bond University on the Gold Coast, this situation – antibiotic resistance – has now become a critical concern in Australia and throughout the world.
‘The antibiotic crisis has come,’ he told Good Practice. ‘We are getting reports from all around the world of multi-resistant organisms; so resistant to every antibiotic we know.’
The consequences of this development could be described as catastrophic.
‘[It could mean a return] to the pre-antibiotic era, when people died of pneumonia, and the postman got a prick on his finger from attending his rosebushes and died of septicaemia,’ Prof Del Mar said.
Such a situation would also result in significant downstream effects, with an impact on public health.
‘When you’re working in a hospital and treating patients with cancer who are vulnerable to infection, you don’t want antibiotics that don’t work,’ Prof John Turnidge, lead for the Australian Commission on Safety and Quality in Health Care’s (ACSQHC) National Antimicrobial Utilisation Surveillance Program, told Good Practice.
Medical procedures currently considered routine may also become significantly riskier for the patient.
Challenging resistance
Prof Chris Del Mar warns that widespread antibiotic resistance would have significant effects on all levels of healthcare.
Dr Justin Coleman believes GPs’ prescribing habits should always be guided by the best available evidence.
Antibiotic awareness week
Antibiotic Awareness Week, designed to raise awareness of the global problem of growing antibiotic resistance, takes place from 14–20 November. It is endorsed by the World Health Organization and all health services are encouraged to participate.
Visit the www.safetyandquality.gov.au/our-work/healthcare-associated-infection/antimicrobial-stewardship/antibiotic-awareness-week to find Australian Commission on Safety and Quality in Health Care (ACSQHC) resources and help in planning activities and education for this event.
‘As well as direct deaths from antibiotic resistance, you’d also have the inability to use antibiotic cover for high-risk procedures, which we now take as standard care,’ Prof Del Mar said. ‘That includes things like joint replacements, for example. So that means a lot of orthopaedic surgery would be too dangerous to do.’
Because there are very few new antibiotics under development for general use,2 large-scale inquiries into the phenomenon of antibiotic resistance, such as the UK’s Tackling drug-resistant infections globally: Final report and recommendations, have suggested that a major part of the solution is to reduce unnecessary antibiotic prescriptions across hospitals and primary care.3
GPs’ prescribing habits inevitably have a large effect on antibiotic use in Australia
‘Antibiotic resistance only happens if you use the antibiotics,’ Prof Del Mar said.
‘If you don’t use them, the competitive environment for the bacteria means the bacteria are at a disadvantage if they carry resistance genes.’
AMANDA LYONS
Altering general practice prescribing can play a significant role in combating antibiotic resistance.
Penicillin, the world’s first antibiotic, or ‘bacteria killer’ as it was originally known, was discovered by Scottish doctor and bacteriologist Alexander Fleming in 1928 and was being produced on a commercial scale by the 1940s. But, not long after accepting a Nobel Prize in 1945, Dr Fleming was already predicting the danger of antibiotic resistance from overuse of such medications.1

11Reprinted from Good Practice Issue 11, November 2016
XXX
[Organisation for Economic Cooperation and Development] countries,’ he said. ‘In particular, we compare poorly to a lot of European countries. Notably, [Australia prescribes] more than Scandinavia, which has done very well with reduced targeted antibiotic prescribing for years.’
According to Prof Del Mar, these rates of over-prescribing emerged from a widespread ‘better safe than sorry’ approach from earlier days in general practice, when resistance wasn’t as much of a problem. He used the case of a sore throat as a common example.
‘We know a lot of sore throats are caused by streptococcus and that you can get nasty consequences from streptococcus, including acute rheumatic fever and acute glomerulonephritis,’ he said. ‘We also know that streptococcus is very sensitive to penicillin, so it seemed very sensible to cover it with penicillin.
‘That was standard practice in all the textbooks to stop these side-effects.’
Prof Turnidge feels this type of practise has also led to patients often expecting prescriptions for antibiotics when they visit their GP.
‘An unwritten bond has been built up [between doctor and patient] in Australia that’s led to this dizzying spiral of increasing antibiotic use,’ he said.
This, Prof Turnidge believes, can be exacerbated by a fear of losing patients.
‘General practice is a private business and you’ve got to keep your customer satisfied, so to speak,’ he said. ‘There’s always a concern that if you don’t write the script, the patient will go to the GP down the road or to the 24-hour clinic to get it.’
Evidence-basedDr Coleman believes a doctor’s decision regarding whether or not to prescribe should be made according to the evidence. He used Choosing Wisely’s guidelines against overusing antibiotics to illustrate the point.
‘Choosing Wisely wouldn’t make these recommendations based just on the increased risk of resistance, because if they did a whole lot of good for the individual receiving the antibiotics would outweigh the broader harm done by increasing resistance,’ he said.
‘But what the evidence shows in so many of these instances is that … the difference antibiotics make is often quite disappointing.’
Nor is the risk of further complications from infection enough to justify many prescriptions.
‘For a GP to see a single case of acute rheumatic fever arising from sore throat, for example, would be something like one in 10 GPs’ professional lifetimes,’ Prof Del Mar said. ‘You’ve got to see a lot of sore throats to stop that one case, and it’s much the same for glomerulonephritis. >>
Prof John Turnidge calls the fact 46% of Australians took at least one course of antibiotics in 2014 ‘a mind-boggling figure’.
Achieving a reduction in antibiotic prescribing would involve a combination of patient education, finding alternatives to antibiotics, and ensuring antibiotics are only prescribed when they will be genuinely effective.
Antibiotics in general practiceWhile many of the most common antibiotic resistance scenarios occur within hospitals, general practice prescribing has also contributed to the issue.
‘GPs’ prescribing habits inevitably have a large effect on antibiotic use in Australia, just through volume of patients seen,’ Dr Justin Coleman, GP and Chair of the RACGP working group on NPS MedicineWise’s ‘Choosing Wisely Australia’ initiative, told Good Practice.
The ACSQHC’s Antimicrobial Use and Resistance in Australia (AURA) project, which explored the impact of general practice antibiotic prescribing in a 2016 report (refer to breakout on page 12 for more information), found that GPs generate 88% of antibiotic prescriptions in Australia.4
According to Prof Turnidge, a member of the AURA project reference group, the report contained a number of other concerning statistics.
‘Other figures that troubled us most were on the Pharmaceutical Benefits Scheme [PBS], which covers about 95% of all antibiotic scripts within the community,’ he said. ‘In 2014, 46% of Australians took at least one course of antibiotics, which is a mind-boggling figure.’
Dr Coleman placed Australia’s prescribing figures into a global context.
‘In terms of antibiotic prescribing, Australia ranks lower than the average OECD

12 Reprinted from Good Practice Issue 11, November 2016
ANTIMICROBIALS
>> ‘So the symptoms themselves aren’t a good cause, and the infective symptoms are much the same.’
While there are obviously cases in which antibiotic prescriptions are well-warranted, recent research has also shown that doctors who are considered ‘cautious’ prescribers actually have the same rate of adverse outcomes from infections as ‘enthusiastic’ prescribers.5
‘I think what that reflects is that GPs who are cautious prescribers still give antibiotics where they are needed,’ Dr Coleman said. ‘The difference lies in the larger numbers of people who probably don’t need the antibiotics.’
It should also be noted that antibiotics themselves can have adverse effects.
‘Doctors often forget to tell patients that antibiotics actually carry some harms with them,’ Prof Del Mar said. ‘Things like rashes, bellyache and diarrhoea, or thrush.
‘If you do the empirical work, you can see the harms that you get from antibiotics are much the same as the benefits, at the same sort of rate.’
Alternative strategiesAs Prof Del Mar explained, ‘GPs got used to using antibiotics and patients got used to expecting them.’ How can doctors counter the situation?
One method is to intervene at the prescribing stage. Prof Turnidge described a strategy that has been used in the UK called ‘delayed prescribing’, in which a script is
written for antibiotics but the patient is asked not to fill it for 48 hours.
‘It does work in the sense that only a third of patients are ever likely to fill the script. That’s the evidence we have from the UK,’ he said. ‘But the irony of that is if you need an antibiotic, you actually need it now. Waiting two days isn’t a great idea.
‘But we would continue to promote it as a strategy because it starts to send a message that, “No, you don’t need antibiotics now”.’
Another prescribing strategy being considered by the ACSQHC is introducing scripts that expire within two weeks of being written.
‘That’s quite important, because we now have information about how many antibiotics prescriptions are filled weeks, or even months, after they were written, which means that people didn’t fill it then and there, but used it later off their own bat for some other indication,’ Prof Turnidge said.
There are also a variety of different options under development in the global effort to combat antibiotic resistance.3
‘People are looking at alternatives to achieve what they need,’ Prof Turnidge said. ‘For instance, infection control strategies or chemicals other than antibiotics that can achieve the same aim.’
All agreed, however, that patient education within consultations is one of the most effective strategies for GPs.
‘It is about having that conversation with the patient at the time, getting them to understand that antibiotics are actually
rather precious things and should only be prescribed when doctors really think the patient is likely to benefit,’ Prof Turnidge said.
Prof Del Mar believes it is also important to personalise the message of antibiotic resistance for the individual.
‘I mention [to patients] that if you take antibiotics and then subsequently get an infection like meningitis or pneumonia, there’s good data to show that if you’ve got resistance on board, getting on top of those very serious infections can be more difficult,’ he said.
However, Prof Turnidge acknowledged the often-pressured nature of general practice and the importance of providing support for GPs.
‘GPs are busy. They’ve got a waiting room full of people and it’s much easier for them to write a script than sit there and explain why they’re not doing it,’ he said. ‘So we’ve somehow got to facilitate that interaction and make it worth their while.
‘That’s where we need to fix the problem, right at that critical point.’
Prof Del Mar is also keen to ensure GPs aren’t burdened by such explanations.
‘We need to provide GPs with quick ways of communicating that quite complicated information to patients, so it doesn’t make the consultation any longer,’ he said.
Although it may initially be difficult to change patient expectations, Dr Coleman believes good research provides a firm foundation for change.
‘If it is good-quality evidence, it has to change our prescribing patterns, otherwise we’re just basing [our decisions] on what has always been done,’ he said.
References1. Penicillin’s finder assays its future. The New York
Times. 26 June 1945: 21.2. The Pew Charitable Trusts. Tracking the pipeline of
antibiotics in development. Philadelphia, USA: The Pew Charitable Trusts, updated May 2016. Available at www.pewtrusts.org/en/research-and-analysis/issue-briefs/2014/03/12/tracking-the-pipeline-of-antibiotics-in-development [Accessed 27 September 2016].
3. Review on antimicrobial resistance. Tackling drug-resistant infections globally: Final report and recommendations. United Kingdom: Review on antimicrobial resistance, 2016.
4. Australian Commission on Safety and Quality in Health Care (ACSQHC). AURA 2016: first Australian report on antimicrobial use and resistance in human health. Sydney: ACSQHC, 2016.
5. Gulliford M, Moore, M, Little P, et al. Safety of reduced antibiotic prescribing for self limiting respiratory tract infections in primary care: cohort study using electronic health records. BMJ, 2016; 354:i3410.
Helpful resourcesThere are a variety of resources available to help GPs combat the rise of antibiotic and antimicrobial resistance:• The RACGP offers an activity through the gplearning platform that guides GPs in how
to communicate complex information in consultations with patients. Visit www.racgp.org.au/education/courses/activitylist/activity/?id=40869 to access the activity.
• Visit www.health.gov.au/internet/main/publishing.nsf/Content/ohp-amr.htm#tocstrategy for information on the Federal Government’s National Antimicrobial Resistance Strategy.
• The Antimicrobial Use and Resistance in Australia Project (AURA) is funded by the Federal Government and carried out by the Australian Commission on Safety and Quality in Health Care (ACSQHC). Visit www.safetyandquality.gov.au/publications/aura-2016-first-australian-report-on-antimicroibal-use-and-resistance-in-human-health to read AURA’s first comprehensive report on the issue.
• NPS MedicineWise provides information, resources and access to continuing professional development courses on antibiotic resistance. Visit www.nps.org.au/medicines/infections-and-infestations/antibiotics/for-health-professionals/antibiotic-resistance-a-problem-for-everyone for more information.

The good GPnever stops learning.
THE ONLINE PROFESSIONAL COLLABORATION SPACE
FOR RACGP MEMBERS
shareGP is now live
Log in via sharegp.racgp.org.au
4227Good Practice-Good GPshareGP-v2.indd 1 11/10/2016 1:14:00 PM

14 Reprinted from Good Practice Issue 11, November 2016
Imag
es R
AC
GP
RACGP DIGITAL
Digital home
PAUL HAYES
myRACGP, the RACGP’s new online portal, is a secure and easily-accessible location for communication and exclusive content.
With more than 33,000 members located across Australia, from large inner-city practices to solo clinics in some of the most remote places in the country, it is vital that the RACGP provides a service GPs can easily access in order to connect with their college.
Officially launched at the RACGP’s recent Annual Conference for General Practice – GP16 – in Perth, the myRACGP online portal has been developed to be a ‘digital home’ that is exclusive to RACGP members.
myRACGP is designed to provide members with a single location where they can easily access RACGP resources such as clinical guidelines, internal and external news, learning and professional requirements, classifieds, and more.
‘myRACGP is an example of the college innovating on behalf of its members,’ Dr Bastian Seidel, RACGP President and myRACGP digital adviser, told Good Practice. ‘As an academic college, the RACGP has a responsibility to provide members with the best possible resources and the development of myRACGP means they can now access those resources at a single, easy-to-navigate location.’
According to Dr Edwin Kruys, Chair of RACGP Queensland and myRACGP digital adviser, the new online hub is an improvement on what has been available to members.
‘The RACGP website contains an enormous amount of fantastic resources, but it looks a bit like my backyard shed:
Dr Edwin Kruys hopes greater online collaboration will ‘unlock the potential collective wisdom’ of GPs.
it’s so crowded that it’s often hard to find anything,’ he told Good Practice. ‘RACGP staff and its members have produced many valuable resources over the years and we have to make sure they remain easily accessible for GPs.’
As a member-based organisation, the RACGP is ultimately responsible to those members and the development of myRACGP is a solution to one of their most pressing requirements.
‘RACGP leadership responded to member feedback [regarding locating information on the website] and started the big clean up,’ Dr Kruys said. ‘And while they were at it they built a few extra bits and pieces to make life easier, and that’s myRACGP.’

15Reprinted from Good Practice Issue 11, November 2016
A one-stop-shopThe fact it provides a single online location from which GPs can access all RACGP information relevant to them is one of the fundamental benefits of myRACGP.
‘It is a landing page – or dashboard, if you like – for busy GPs,’ Dr Kruys said.
Research has found that the ability to improve clinical care through areas such as increased service efficiency and reduction in workload is one of the key facilitators of GPs’ use of digital technology.1 myRACGP includes single-click links to a number of clinical guidelines and other important resources.
‘The RACGP libraries will be at our fingertips. We can quickly do clinical searches and links to, for example, the online therapeutic guidelines,’ Dr Kruys said. ‘It will also offer a place for feedback about myRACGP, and members can quickly check their QI&CPD statement and membership information.
‘myRACGP will help to make day-to-day clinical work easier, as all the resources you need are right there in front of you on one screen.’
Dr Ayman Shenouda, rural GP and myRACGP digital adviser, believes the new portal will help RACGP members better interact with their college and take further advantage of everything it has to offer GPs.
‘The benefits are to have a member portal that you can access which tells you all about your relationship with the RACGP,’ he told Good Practice. ‘myRACGP also gives you some news in terms of what is happening in the RACGP.
‘We’re hoping that with this new portal GPs will access not only what the RACGP itself is doing, but also what
they themselves are interested in doing within the RACGP.’
As Chair of RACGP Rural, Dr Shenouda is also excited by the opportunities the streamlined myRACGP can offer GPs in more remote locations.
‘myRACGP is so helpful because rural GPs often feel a bit isolated, in terms of upskilling and their relationship with other GPs,’ he said.
Peer-to-peerThe ‘relationship with other GPs’ Dr Shenouda is keen to encourage is represented by shareGP, one of the most innovative and exciting aspects of myRACGP.
‘shareGP is so exciting because members now have a secure online space where they can feel comfortable discussing issues that matter to them,’ Dr Seidel said.
A professional collaboration space, shareGP is designed to allow members to come together with other GPs in a safe online setting.
‘shareGP works a bit like Facebook and is built specifically for those GPs who enjoy connecting with colleagues in a secure, professional social media environment,’ Dr Kruys said.
According to the RACGP’s 2015 ‘Use of technology’ survey, 73% of recent general practice graduates are comfortable with the use of these types of new technologies,
while 67% of GPs with more than 10 years’ experience are also comfortable with their use. More than half of GPs (53%) feel confident about experiencing new technologies.2
‘Our membership research shows that the younger generation of GPs use social media a lot and we believe that shareGP will fill a gap for New Fellows, registrars and others,’ Dr Kruys said. >>
RACGP President Dr Bastian Seidel believes innovations like myRACGP help the college deliver the best possible services to its members.
For membersKey myRACGP features:• myCPD – allows RACGP
members to view their QI&CPD status for the triennium and find accredited activities in order to meet their requirements.
• myResources – repository for the most popular RACGP resources, including libraries, clinical guidelines, gplearning and journals such as Australian Family Physician (AFP).
• myNews – features all of the latest RACGP news and information, including Good Practice, media releases, Twitter updates and faculty newsletters.
• myProfile – allows members to ensure their personal details are correct and up to date.
• payGP – administrative services for members who provide professional services to the RACGP.
Visit www.racgp.org.au/myracgp to access myRACGP.

16 Reprinted from Good Practice Issue 11, November 2016
Imag
e R
AC
GP
RACGP DIGITAL
eHealth The RACGP’s eHealth department includes resources designed to provide GPs with information to help them navigate a constantly evolving area of healthcare.
Subjects include:• Practice Incentive Program (PIP)• Digital Business Kits• Social medial in general practice• Telehealth • Protecting your practice• Managing the use of your
practice data• Open Primary care Technology
that is Interoperable Meaningful, Useable and Safe (OPTIMUS)
Visit www.racgp.org.au/your-practice/ehealth for more information.
>> While similar to other forms of social media, an important distinction of shareGP is that it is only available to RACGP members, ensuring users will be interacting with qualified general practice colleagues.
shareGP is Health Insurance Portability and Accountability Act (HIPAA) compliant and uses the same encryption standard utilised by the government and finance sectors. It enables members to join groups related to individual interests and subjects; share content, such as blogs and research papers; search for and connect with peers; and stay informed about issues and events important to their profession.
‘Members are able to collaborate on projects in the online space, ask and answer questions, and post content, articles, blogs, pictures and videos,’ Dr Kruys said.
shareGP is curated and moderated by members, which allows them to participate whenever and however they like.
According to Dr Shenouda, shareGP helps to fill a void among RACGP members.
‘We communicated with a lot of members and one of their priorities was to get a way of connecting with GPs and
some sort of engagement through the membership,’ he said.
‘shareGP is a member space that allows live communication among clinical experts. Part of it will be about seeking advice from expert peers.
‘So if you have a problem, you might put up a question you are facing about a patient or a diagnosis. You can have expert advice about it and some real-life communication with your fellow GPs.
‘Members are always hungry to share their issues and ideas with other members. We want to make that connection as accessible and as flexible as we can and that’s the idea behind myRACGP and shareGP.’
Dr Kruys believes this type of peer-to-peer camaraderie among general practice colleagues is a vital aspect of a representative organisation like the RACGP.
‘shareGP will encourage collaboration and further unlock the potential of our collective wisdom,’ he said. ‘I also hope shareGP will stimulate member engagement – and that we have a bit of fun along the way.’
Ready for the futureAs more and more aspects of people’s lives rely on digital technology, the healthcare profession has to continue to adapt to best service its patients.
‘We can see the younger generation [of doctors] using online spaces for a lot of their needs and patients are starting to use digital applications, too,’ Dr Shenouda said.
The development of a reliable and secure online portal like myRACGP, which will see continual improvements according to member feedback, is an example of Australia’s largest professional general practice organisation embracing technology to assist its members and help improve patient outcomes.
‘The future of digital consultation, the future of video interaction, is really coming in the next few years,’ Dr Shenouda said. ‘I think that our GPs need to be oriented to digital services and also be quick in terms of adoption of technology that can help them out in the future.
‘myRACGP is a great initiative by the RACGP in that it’s not only listening to what the GPs want, but also looking forward to what would be the needs of the future and trying to get things available as fast as we can to assist GPs, particularly rural GPs, in the quality journey.’
References1. The University of Melbourne, Department of General
Practice. Introducing the ‘e’ in health – Uses and views of e-health in the Australian primary care setting: An online survey on general practitioners. Parkville: The University of Melbourne, 2015.
2. The Royal Australia College of General Practitioners. Views and attitudes towards innovation in general practice: Survey report. East Melbourne: RACGP, 2016.
73%of recent graduates
67%of GPs with 10+ years of experience
53%
of GPs feel con�dent about experimenting with new technologies
Dr Ayman Shenouda is excited by the opportunities myRACGP will provide rural GPs.
feel comfortable with new technologies

17Reprinted from Good Practice Issue 11, November 2016
ETHICS IN GENERAL PRACTICE
A doctor will occasionally face a situation where they need to weigh up their obligation to protect patient confidentiality against acting in the ‘public interest’ in trying to protect the health or safety of the general community.
Legal obligations – privacyIn what circumstances can you disclose information about one of your patients to a third party?
Under Australian Privacy Principle Six in the Privacy Act 1988, a patient’s health information can be disclosed to a third party in certain circumstances, including when:• the patient provides their consent
for the information to be released to the third party
• it is necessary to lessen or prevent a serious threat to the life, health or safety of any individual, or to public health or safety, where it is unreasonable or impracticable to obtain the patient’s consent: – includes a threat to physical or mental health and safety
– may include a threat of serious harm to the patient or to any other unspecified individual
• it is required or authorised by or under an Australian law or a court/tribunal order (eg mandatory reporting of child abuse, a subpoena or search warrant)
• it is reasonably expected by the patient and directly related to the primary purpose of providing healthcare (eg complaints handling, audit, disclosure to a medical defence organisation)
• it is reasonably necessary for one or more enforcement-related activities conducted by, or on behalf of, an enforcement body: – a written note of the disclosure must be made
– enforcement-related activities include the prevention, detection, investigation and prosecution or punishment of criminal offences and intelligence-gathering activities
Patient information
SARA BIRD
When can GPs disclose information about a patient to a third party?
– ‘enforcement body’ includes bodies responsible for policing, criminal investigations and administering laws to protect public revenue or to impose penalties or sanctions.
Preventing a breachWhat should Dr Z have done to prevent a breach of privacy when she was contacted by the police about her patient?
She could have asked the police whether any of the exceptions to her duty of confidentiality and privacy applied. Specifically, whether the patient had given his permission for the GP to discuss his health information with the police; if the information was needed to lessen or prevent a serious threat to life, health or safety; or whether the information was necessary for an enforcement-related activity by the police.
If Dr Z was not certain in terms of how to respond to the enquiry, she could have asked the police to put their request in writing. This would have enabled her to obtain advice from her medical defence organisation, and/or discuss the situation with the patient, if appropriate.
In summary, if a patient provides you with their consent to release their health information or medical records to a third party, you should do so. In the absence of your patient’s consent, there are limited circumstances in which you can release their health information or medical records to a third party.
References1. ‘EZ’ & ‘EY’ [2015] AICmr 23. Available at oaic.gov.au/
privacy-law/determinations/2015-aicmr-23 [Accessed 6 October 2016].
2. Medical Board of Australia. Good medical practice: a code of conduct for doctors in Australia. Available at medicalboard.gov.au/Codes-Guidelines-Policies/Code-of-conduct.aspx [Accessed 6 October 2016].
A GP, Dr Z, was found to have breached a patient’s privacy and ordered to pay the patient $6500 for injury to his feelings and distress.1 The privacy breach occurred when the GP answered a phone call from the police asking if she thought her patient was psychotic.
Dr Z knew the patient well, having seen him on 26 occasions over the previous two years, but she had not seen him for two months. The GP replied to the police that, ‘it was possible, but further assessment was needed’.
Professional obligations – confidentiality and privacyAccording to the Medical Board of Australia’s Good medical practice: a code of conduct for doctors in Australia, patients have a right to expect that doctors and their staff will hold information about them in confidence, unless the release of information is required by law or public interest considerations.2
The ethical and professional duty of confidentiality dates back to Hippocrates and forms the basis of trust in the doctor–patient relationship.
This duty encourages patients to disclose information truthfully, without fear of harm, discrimination or embarrassment that may arise from the dissemination of the information.
However, the duty is not absolute and there are exceptions to the duty of confidentiality.
This article is provided by MDA National. They recommend that you contact your indemnity provider if you need specific advice in relation to your insurance policy.

Imag
es N
atha
n P
insk
ier;
Jan
Cha
ffey
18 Reprinted from Good Practice Issue 11, November 2016
Mobilising healthcareAMANDA LYONS
The possibilities presented by mobile health are exciting, but care must be taken when implementing it in general practice.
The convenience and affordability of mobile devices, including smartphones, tablets and wearable monitoring devices, has ensured their ubiquity in Australian society. According to Deloitte’s ‘Mobile Consumer Survey 2015’, 79% of all Australians own a smartphone, while six out of 10 Australian mobile consumers own multiple mobile devices.1
The pervasive nature of mobile technologies has had a revolutionary impact on the way people live their lives, changing the structure and delivery of a variety of services from food and consumer goods through to airlines and banking.
According to Dr Nathan Pinskier, GP and Chair of the RACGP Expert Committee – eHealth and Practice Systems (REC–eHPS), mobile technologies may also present innovative possibilities for the healthcare sector in the form of ‘mobile health’, or mHealth.
‘Doctors can take a laptop or tablet or anything that’s wireless to the patient,’ he told Good Practice. ‘You can have a consultation in a different setting. You can potentially even have it in a different room from the patient.’
Looking further into the future, mHealth technologies such as wearable monitoring devices could transform the way GPs manage patients with chronic disease.
‘As the technology matures and we hopefully see the evolution of the Health Care Home, the potential for general practice to be able to collate data remotely – monitor someone’s glucose, or weight, or congested cardio-failure for someone with cardiovascular disease – means GPs may become remote coordinators,’ Dr Pinskier said.
‘Technology may allow us to do things through mHealth in ways that we can’t do them today.’
Despite such possibilities, general practice is yet to embrace mobile devices with the same enthusiasm shown by patients.
‘Outside of healthcare, mobile devices are used widely. Community expectations are [geared towards] the use of mobile devices,’ Jan Chaffey, chief executive officer of the Camp Hill Healthcare general practice in Queensland, told Good Practice.
‘We have been slower to adopt this in healthcare, mainly because of problems around privacy, confidentiality and patient safety.’
The issuesDespite his enthusiasm for the possibilities of mHealth, Dr Pinskier agrees that it is important for the healthcare sector to proceed cautiously.
‘People rush to use the technology because it’s there and it’s cool and easy, but the consequences and ramifications may not always be immediately obvious,’ he said.
‘Anecdotally, we know that clinicians are using their phones and portable tablets for all sorts of purposes, but it’s not exactly clear how they are safe-guarding the information contained on those devices.’
This situation highlights a major medico-legal issue surrounding use of mobile devices in general practice: while these technologies may be fast and convenient, the information they transmit is largely unsecure. Chaffey used email communications as an example.
mHealth is an additional resource and an additional tool and, like everything, its benefits become clear over time
‘Patients expect to be able to communicate on email, but they need to be made very aware that normal, unencrypted email is not secure and people outside of the intended recipient might be able to access it,’ she said.
General practices must abide by the Federal Government’s Australian Privacy Principles relating to the handling of sensitive medical information to protect patient confidentiality. There are serious consequences for breaches of these principles, ranging from fines to legal action against the practitioner or clinic. This means that conducting doctor–patient communications on mobile devices can potentially be dangerous for both parties.
TECHNOLOGY IN GENERAL PRACTICE
Dr Nathan Pinskier regards mobile health technology as an additional tool for GPs.
Practice CEO Jan Chaffey believes mobile health technology should fit within existing workflow, rather than add to it.

‘If you’re not following the guidelines and rules around [patient information], there could be consequences down the track,’ Chaffey said.
According to Dr Pinskier, GPs who use personal mobile devices during patient care may also find themselves ensnared in practical issues related to systems and record-keeping.
‘A good example would be photography,’ he said. ‘Everyone uses their phones for photographs, hardly anyone walks around with a camera these days.
‘That’s fine in the normal environment, but in a healthcare setting you might have a patient who has a lesion or a skin condition. Taking a photo is a great idea.
‘The problem is, you’re recording it on your own device. How do you transfer it across
to the patient records? How do you ensure confidentiality and privacy of that information, and that it’s not identifiable on your phone?
‘Your phone now becomes part of the record system, unless you can move that information across.’
Dr Pinskier also described how use of personal mobile devices in general practice can cause issues in terms of doctor–patient boundaries.
‘It could be sending an SMS [short message service] to patients, which becomes an issue itself,’ he said. ‘It raises a whole new challenge around, “If I send an SMS to patients using my own phone, I’ve exposed my own phone number and compromised my own privacy. I’ve also created the expectation that I’m online 24/7”.
‘Your work–life balance gets affected.’Remote monitoring by way of wearable
devices can present a similar problem.‘There’s talk about patient devices that
can feed information to practitioners for ongoing monitoring. It’s happening in some sectors and we’ve discussed it with our practitioners,’ Chaffey said.
‘The issue for them is the timeliness of response.
‘So if a patient is constantly monitoring blood sugars, blood pressure or whatever else, and they are feeding information through to the doctor, what process is in place if there is an urgent or a semi-urgent medical situation that comes in at 10 o’clock at night? The safety factor involved with that is an issue. >>
19Reprinted from Good Practice Issue 11, November 2016
More people in health and community services choose HESTA for their super
2015 RAINMAKER EXCELLENCE AWARDS
WINNERWORKPLACE SUPER PRODUCT OF
THE YEAR - VALUE CHOICE
Supports your industry | Low fees | A history of strong returns
Issued by H.E.S.T. Australia Ltd ABN 66 006 818 695 AFSL 235249, the Trustee of Health Employees Superannuation Trust Australia (HESTA) ABN 64 971 749 321. Investments may go up or down. Past performance is not a reliable indicator of future performance. Product ratings are only one factor to be considered when making a decision. See hesta.com.au for more information. Before making a decision about HESTA products you should read the relevant Product Disclosure Statement (call 1800 813 327 or visit hesta.com.au for a copy), and consider any relevant risks (hesta.com.au/understandingrisk)
1837_HESTA_dentalhygiene_RACGP_186x106.indd 1 26/09/2016 3:31 PM

20 Reprinted from Good Practice Issue 11, November 2016
TECHNOLOGY IN GENERAL PRACTICE
>> ‘These are all things which will have to be considered and monitored very carefully in the future.’
ImplementationTimeliness of response, maintaining doctor–patient boundaries and compliance with Australian Privacy Principles are all good reasons for the cautious uptake of mHealth in the healthcare sector. Nevertheless, things are slowly advancing.
‘I have noticed that the medico-legal workshops I’ve attended in the last 12 months are moving from, “No, don’t do it”, to, “Yes, you can do it, but you need to be careful about how you do it, and always with patient consent”,’ Chaffey said.
Before a practice can even begin to grapple with issues of privacy of patient information, however, the mHealth systems themselves must be implemented. And before this can take place, the practice has to consider cost.
‘Apart from the safety and security issues, you need a business case,’ Chaffey said.
‘The majority of general practices in Australia are private businesses, so you’ve got to be very mindful that you have a business case around how [the mHealth system] is going to be funded.’
Part of this business case should address issues of data backup and continuity.
‘Once you’ve started using [the mHealth system], how do you ensure you’ve got adequate resourcing for the devices?’ Dr Pinskier said. ‘If it fails, what’s your plan for business continuity?
‘It’s easy to do things on a trial basis, but once you embed [the system] it may require additional support and resourcing.’
Chaffey also stressed the importance of ensuring new processes provide a genuine benefit before putting them into action.
‘Anything you implement needs to fit into workflow,’ she said. ‘You can’t impose extra things on GPs that will take a lot of time.
‘It’s important to work out how you fit new systems into the workflow, how [staff members are] upskilled to make sure that it doesn’t take extra time and, of course, it’s got to be of benefit to staff and patients.’
Once these aspects have been considered and implementation has been given the go-ahead, the practice administration team will be central to the process.
‘The administration team members are really the implementers,’ Chaffey said. ‘[We run an] implementation trial and train staff,
[which is] an absolutely essential part of any changes within a practice.
‘You’ve got to train everybody and put a lot of effort into that. I think that’s where we miss out a lot in healthcare in Australia – we don’t train people well enough with the systems they have to use within their practices.’
When the mHealth systems and infrastructure are in place, another essential step is to have a clear and official policy around the use of mobile devices and compliance with privacy requirements. This serves to clarify the issues and procedures for patients and practice staff members.
Chaffey’s own practice provides patients with materials on the subject.
‘We’ve got our privacy policy brochure that covers all the confidentiality issues,’ she said. ‘It’s available to the patients so they know what they can expect, and what we provide and what we do.’
As an example of how her practice system follows privacy guidelines, Chaffey described its use of SMS alerts for patients.
‘We SMS patients for appointment reminders,’ she said. ‘We also SMS for preventive health reminders, but we’ve
worded them as such that there’s absolutely no clinical information in them.
‘In both of those scenarios, it’s always done with consent from the patient.’
RACGP toolkitThe RACGP’s 2015 ‘Use of technology’ survey investigated how its members use mobile technology in their practice in order to help GPs navigate the growing terrain of mHealth.
The results of the survey informed the development of the RACGP’s new resource, mHealth in general practice: A toolkit for the effective and secure use of mobile technology (the toolkit), which was released at GP16 (refer to breakout, left, for more information).
Chaffey, who was part of the project team behind the toolkit, believes the guidance it provides will help to make implementation of mHealth devices a more manageable process.
‘It’s a very comprehensive resource that very carefully works through considering implementing mobile devices. It gives you a lot of explanation around it,’ Chaffey said. ‘It goes through some planning stages, trials, how you deliver it, how you review what you’ve done, and a step-by-step process.’
Given the constantly-evolving nature of mHealth, the RACGP is committed to updating the toolkit now and into the future.
‘[mHealth] is an additional resource and an additional tool and, like everything, its benefits become clear over time,’ Dr Pinskier said.
Dr Pinskier’s believes that while it is important to engage with the developments presented by mHealth and determine how to best use them, these devices should ultimately be considered an extension of traditional general practice, rather than a replacement.
‘We can access information and we can make that information readily available in all sorts of formats and locations that can be really convenient and beneficial,’ he said.
‘But we shouldn’t confuse the access to information with the clinical skills of a qualified medical practitioner.’
Reference1. Deloitte. Mobile consumer survey 2015 – The Australian
cut. Sydney, 2015. Available at www2.deloitte.com/au/en/pages/technology-media-and-telecommunications/articles/mobile-consumer-survey-2015.html [Accessed 16 September 2016].
RACGP resourcesThe RACGP has resources to assist GPs in implementing and managing eHealth and mHealth in their practices:• mHealth in general practice: A toolkit
for the effective and secure use of mobile technology is available at www.racgp.org.au/your-practice/ehealth/additional-resources/mhealth-in-general-practice
• Computer and information security standards (CISS) includes standards for mobile and electronic devices. It is available at www.racgp.org.au/your-practice/standards/computer-and-information-security-standards
• The RACGP is conducting its annual ‘Use of technology’ survey to gain an understanding of the ways Australian GPs are adopting technology. Visit www.racgp.org.au/your-practice/ehealth/additional-resources/racgp-technology-survey to find out more about the survey and to take part. The survey will remain open until 30 November.

racgp.org.au Healthy Profession.Healthy Australia.
2017 – 19
The NEW triennium is nearThe Royal Australian College of General Practitioners (RACGP) recently launched the new Quality Improvement and Continuing Professional Development (QI&CPD) Program for the 2017–19 triennium.
A part of the RACGP’s commitment to continually evaluate and improve the QI&CPD Program, the 2017–19 triennium will include an increased focus on re�ective learning practices.
To promote re�ective learning practice in continuing professional education, we are introducing the planning learning and need (PLAN) Category 1 Quality Improvement (QI) activity.
For more information visit racgp.org.au and search ‘QI&CPD’
2017 –19 triennium
4226 Good Practice ad-QI&CPD FP-v1.indd 1 10/10/2016 2:47:12 PM

GP PROFILE
Tasmania’s Dr Columbine Mullins tried her hand at a number of different areas of healthcare before arriving at general practice.
After finishing her medical studies at the University of Tasmania in Hobart, she decided on a change of scenery and undertook an internship at Gosford Hospital on the central coast of NSW.
‘I wanted to get out of Tassie and chase warmer weather, all that sort of stuff,’ she told Good Practice. ‘It was great being in Gosford because it was a not too big a hospital, and it had a great emergency department and a lovely feel about it. And I was living out at Terrigal where there’s beautiful beaches, so it was a really fun intern year.’
The move to Gosford was only the start of Dr Mullins’ medical journey.
‘I then took a bit of time off and did some locum work for my first year. I went up to Kempsey [NSW mid-north coast], then I went over to New Zealand and did a colorectal surgery resident job,’ she said. ‘I came back and did some more locum work around NSW, then I went to RPA [Royal Prince Alfred Hospital in Sydney] for a resident year.
‘It was very varied. I spent a fair bit of time in different emergency departments, which was quite an easy way of doing
locum work and it was fun going around different places in NSW – Lismore, Dubbo, Taree, Kempsey. It really was good.’
All of these disparate moves, however, ultimately led Dr Mullins home.
‘I had gotten married and had good friends in Tassie, and it seemed like a nice idea to come home,’ she said.
‘I ended up in a small hospital in the north of the state and did some locum work before I decided I actually wanted to do general practice, so went and started general practice in Devonport [north-west Tasmania]. I was in Devonport for about a year … and I moved back down to Hobart.’
Going her own wayHaving had such a varied start to her medical career, Dr Mullins was comfortable in the knowledge that her decision to move into general practice was an informed one.
‘You get caught up in the hospital system and the excitement of that and emergency was quite appealing, but … you don’t get to know people so well,’ she said.
‘I remember as soon as I started general practice, I thought, “I actually love this”.
‘I think you get a sense of autonomy about how you run your day. It’s very broad, very practical. You can find little areas that you have an interest in and become quite good at those.
‘But it’s really the interaction with people which is lovely. You play a pretty major part in people’s lives.
‘I suppose that’s really what it comes down to, but it took me a long time to get to that point. When I figured it out, I thought, “This is brilliant”. I really just loved it and I like the idea of being a useful doctor.’
Following time at an Aboriginal health service and four years in a large practice in Bridgewater on the outskirts of Hobart, Dr Mullins was inspired to take up ownership her own general practice.
‘I’d been to a presentation and they were talking about how the healthcare system was changing, but people really want to have their own personal physician. That resonated with me because I really appreciate and value that doctor–patient relationship,’ she said. ‘So I wanted to pursue having my own patients and being able to serve them.’
By design
PAUL HAYES
Dr Columbine Mullins has embraced the opportunities that come with owning your own practice.
22 Reprinted from Good Practice Issue 11, November 2016
Imag
es R
AC
GP
; Col
umbi
ne M
ullin
s

When the opportunity arose to step in for a retiring colleague who had owned her own practice, Dr Mullins decided to take the plunge. She officially took the reins of Rosny Park Family Practice, located about 5 km from the centre of Hobart, on 1 July this year.
‘It was probably a bit crazy, but I had always loved the idea of having my own practice and this was small enough that I could actually do it,’ she said.
After a steep learning curve of almost immediately working towards (and receiving) Australian General Practice Accreditation Limited (AGPAL) accreditation, Dr Mullins has learned a lot in her short time at the helm of her own practice.
‘It’s been challenging, but it’s been interesting,’ she said. ‘I have really enjoyed that [organisational] side of things, and also being able to make the practice how I want it to be and involve the people who I want involved.’
Shaping her own practice also means Dr Mullins has been able to treat patients, including many who have followed from her practice in Bridgewater, in the
more personal manner that general practice affords.
‘It is a really nice thing when patients turn up or say, “We’re definitely following you”, or other people that you might not know that well come in and say, “We’ve tracked you down”. That’s really sweet,’ she said.
‘Having your own practice is highly motivating, it’s absolutely rewarding and it’s not completely overwhelming or impossible. I don’t regret it at all – I’ve loved it.’
Now that the practice is accredited for registrars, Dr Mullins hopes to pass her experience onto others.
‘I like being involved in, hopefully, making good doctors,’ she said. ‘People who obviously care about their patients, are interested in their patients, have reasonable expectations about their patients and the difficulties that people face in life, and have a bit of empathy towards that.
‘Registrars are all different. They’ve all got different interests and different areas of expertise and I enjoy teaching, but they also keep me on my toes. You have to constantly be learning yourself and try and keep up to date.’
Linking with doctorsIn addition to her efforts towards making good doctors, Dr Mullins also runs a monthly Balint group for practising GPs to help improve doctor self-care and the doctor–patient relationship.
A Balint group involves a number of doctors coming together to anonymously discuss specific cases in order to examine the relationship between doctor and patient in the context of everyday consultations.1
Facilitated in part by RACGP Tasmania, Dr Mullins has found the Balint group, which she co-runs with fellow GP and President of the Balint Society of Australia and New Zealand, Dr Frank Meumann, to be extremely beneficial for all involved.
‘The point is that it helps to improve the doctor–patient relationship, so improving empathy for your patients and acknowledgement of your own difficulties that you might face in the consulting room,’ she said. ‘But it’s also a really nice self-care for GPs or psychologists or anyone working in this environment.
‘It’s all supportive. It’s not about expressing judgement about how you managed the case, but more looking at the feelings and emotions behind it.
‘With your colleagues in the group, you can relate to how they’ve felt in situations and think, “Someone else feels that way, too”, or know that you’re not alone in your frustrations or exhaustion or challenges.
‘I think it is important to create those links, whether it be a group like a Balint group, or having students or registrars involved in teaching, linking up with the RACGP, all those sorts of activities.’
Reference1. The Balint Society. A very short introduction to Balint
groups. Available at http://balint.co.uk/about/introduction [Accessed 23 September 2016].
23Reprinted from Good Practice Issue 11, November 2016
I’m a member because …I know the RACGP is the best advocate for GPs and their patients.
I have been a member of the RACGP since I first became a general practice registrar. It supported me during my training with great educational resources and collegiality, and now continues to offer education and support in other areas, such as running my own practice and providing a venue for my Balint group meetings.
When I walk into RACGP Tasmania I am always greeted by smiles and a lovely, supportive group of people.
– Dr Columbine Mullins, RACGP member since 2009.
who obviously care about their patients, are interested in their patients, have reasonable
difficulties that people face in life, and have
Dr Columbine Mullins bravely took part in this year’s World’s Greatest Shave, a charity event that helps fund research into blood cancers.

24 Reprinted from Good Practice Issue 11, November 2016
A healthy unionAMANDA LYONS
The merger of two practices in the New South Wales town of Forbes has helped increase resources and improve the provision of quality healthcare.
A ‘wheat and wool’ town of close to 10,000 people in central-western New South Wales, Forbes has long faced the traditional rural challenge of attracting GPs.
But when the town’s two general practices – Harold Street Medical Centre and Cross Street Medical Centre – joined forces after almost 40 years of co-existence to form Forbes Medical Centre, the merger proved beneficial in both expected and unexpected ways.
Funded by a Federal Government infrastructure grant for rural general practice, the 18-room medical centre was constructed opposite the Forbes District Hospital in 2010. The hospital itself has since undergone a redevelopment, helping to create a medical precinct in Forbes.
‘We have a good set-up here now. You can practise hospital medicine and general practice medicine,’ Dr Neale Somes, GP and Forbes Medical Centre practice principal, told Good Practice.
The larger practice has certainly achieved its aim of attracting more GPs to the town.
‘We have more than doubled our numbers,’ Dr Somes said. ‘When the medical centre first opened its doors there were five doctors, and now there’s 11.’
In fact, Forbes Medical Centre is about to expand even further with the planned addition of four new consulting rooms.
‘We went from thinking, “How are we going to fill up the other 12 rooms?” when the medical centre opened, to working out five years later that 18 rooms isn’t enough,’ Dr Somes said.
And it’s not only GPs that have been attracted to Forbes’ medical precinct.
‘When the medical centre opened, we might have had four or five visiting specialists, now we have 10,’ Dr Somes said.
The practice has also significantly grown its number of allied health services.
‘We’ve been able to establish our own dietitian service, physiotherapy, audiometry, sleep technicians, podiatrists, psychologist, optometrist,’ Dr Somes explained.
The increased access to a wider range of healthcare services may have been unanticipated, but it is much appreciated, especially by the local patients.
‘Patients can now get in for an appointment to see a doctor on the same day. When we opened, the waiting times were months,’ Dr Somes said. ‘And they don’t have to travel to see these specialists and allied health services.’
Teaching and learningEducation is strongly valued at Forbes Medical Centre and is carried out in a variety of ways. The training of general practice registrars has also turned out to be a good recruitment tool for the practice.
‘We are firm believers in the idea that if we can expose students and registrars to the virtues of rural medicine and the practise of true cradle-to-the-grave medicine, that will entice them to come back,’ Dr Somes said. ‘And that has paid off; five of our 11 [GPs] came here as registrars.’
Like so many medical educators, Dr Somes believes experienced practice doctors also gain from the energy and knowledge of their junior counterparts.
‘I think anybody who has seen a modern medical student or general practice registrar knows that they are very motivated and very keen,’ he said.
‘They keep you on your game and that’s been successful for us.’
It is not just students who regularly are encouraged to learn at Forbes Medical Centre. The practice also hosts a weekly teaching session for all employees.
IN MY PRACTICE
Forbes Medical Centre staff members are dedicated to continued learning and regularly take part in the practice’s education program. Im
ages
For
bes
Med
ical
Cen
tre

25Reprinted from Good Practice Issue 11, November 2016
‘Our continuing medical education program within the centre now goes once a week,’ Dr Somes said. ‘We have regular guest speakers that come on a Thursday morning and speak to us about a topic that we’re interested in.
‘For example, a sports physician is coming along to give us a talk this week. [Before that] a urogynaecologist, a psychiatrist and an orthopaedic surgeon have given us a talk.’
The practice has also developed a teaching relationship with the University of Wollongong.
‘The University of Wollongong has a program where, for year three of their four-year undergraduate degree, their medical students spend the year embedded in a general practice,’ Dr Somes explained.
‘So we have three University of Wollongong students that come here for their main clinical year.’
Forbes Medical Centre is also currently working with a research organisation on a project investigating the value of fish oil in preventing heart attacks.
Dr Somes believes it is the larger size of the practice, as well as its close proximity to the hospital, that has enabled these types of partnerships.
‘There are a lot of people coming through here, which I think has made it appealing to the University of Wollongong and organisations that want to conduct research in primary care,’ he said.
Community involvementDespite all of these exciting developments, the practice’s ultimate concern remains centred on the health and wellbeing of its patients.
‘We wouldn’t have attracted students or research or more doctors if we didn’t have this following of loyal, courteous patients,’ Dr Somes said.
‘It’s an old cliché that a practice isn’t actually the building: if the building burnt down I, as a doctor, would still have a practice because I would still have my following of patients.’
Forbes Medical Centre collects feedback from a community advisory committee to help it best serve patient needs, taking significant measures to ensure it is as representative of the town’s population as possible.
‘We try to appoint people from different aspects of the community, so a representative from the nursing home, the local chemist, the hospital, the Indigenous community, young mothers and the business community,’
Dr Somes said. ‘They meet three times a year and give us advice on what would be needed or not needed.’
While the merger between the practices has been fruitful, the practitioners at Forbes Medical Centre are also keen to preserve the memory of their forebears.
‘We didn’t want it to be as if Forbes Medical Centre sprang up out of nothing. It’s a continuation of the previous practices,’ Dr Somes said. ‘It wasn’t like those practices were destroyed or wiped out by the Forbes Medical Centre, they continued at the Forbes Medical Centre and we wanted to acknowledge that.’
Doctors at Forbes Medical Centre have worked with the town’s historical society to create informative panels about their predecessors for display on the practice walls. The panels have been well received and the practice plans to create more, including one to honour past nurses, and perhaps an ultimate panel that will trace the complete history of general practice in the town.
‘One big family tree that traces doctors who have been here in Forbes, and who succeeded which doctor and what happened to their practice,’ Dr Somes said. ‘The family tree will culminate in the Forbes Medical Centre.’
TRIENNIUM UPDATE
130points
1CPR
2Category 1activities
including 1QI activity
Only two months remaining of the 2014–16 QI&CPD trienniumWith the 2014–16 QI&CPD triennium concluding 31 December 2016, now is the perfect time to complete the Quality Improvement (QI) requirement.
What is Quality Improvement?
Quality Improvement (QI) is the process where an opportunity to change practices occurs as a result of learning.
Professional advice and a growing body of evidence demonstrate quality improvement activities leading to positive change in practices, particularly when involving a whole practice team approach.
Plan, Do, Study, Act (PDSA)
Clinical Audit Small Group Learning
Supervised Clinical Attachment (SCA)
Evidence Based Medicine Journal Club
GP Research
Examples of QI activities:
For more information visit racgp.org.au and search ‘QI&CPD’
4226 Good Practice ad QI&CPD HP-v1.indd 1 10/10/2016 2:48:21 PM

26 Reprinted from Good Practice Issue 11, November 2016
Dermatology AMANDA LYONS
The new RACGP Specific Interests Dermatology network will provide guidance and education across the entire spectrum of dermatology in general practice.
The skin is the largest organ in the body and, accordingly, dermatological problems are very common. The 2014–15 Bettering the Evaluation and Care of Health (BEACH) report found that skin problems were managed in 16.2% of general practice encounters, making them the fourth most frequent issue in GPs’ consultations.1
With such a large canvas, the range of potential dermatological issues is vast.
‘The skin is affected by environmental exposure, but also internal illness and disease,’ Assoc Prof Morton Rawlin, Chair of the new RACGP Specific Interests Dermatology network, told Good Practice. ‘Skin problems include everything from inflammatory conditions and inherited conditions, to skin cancer and melanoma.’
The subject’s importance in general practice is one of the reasons a dermatology network, with Assoc Prof Rawlin at the helm, has long been in the works.
‘I did a Diploma of Dermatology from Cardiff University [in the UK] back in the ’90s. I was one of the first Australians to do that degree,’ he said. ‘I’ve also done almost two years in the College of Dermatologists’ training program.
‘It is a significant part of my practice, and it’s what I enjoy.’
According to Assoc Prof Rawlin, despite the common nature of skin problems, GPs do not necessarily receive extensive education in the area.
‘Generally, dermatology is not particularly well trained at university and GPs develop their skills in dermatology in various ways,’ he said.
‘It really depends a little on the doctor as to how much they develop their skills.’
EducationAssoc Prof Rawlin believes that, with proper training, dermatological conditions can largely be successfully managed in general practice.
‘Dermatological issues are very common and the majority of them can be looked after by GPs, particularly if they’ve had some extra training and get the experience,’ he said. ‘There are some conditions that require specialist input, but the treatment thereafter can be looked after between the dermatologist and the GP.’
In order to better enable this relationship between GPs and dermatologists, the new network aims to provide further educational assistance GPs.
‘We will be looking at some training options for GPs and general practice registrars, and at what we need to do in order to ensure high-quality dermatological skills in general practice,’ Assoc Prof Rawlin said.
Dermatological issues are very common and the majority of them can be looked after by GPs
The Dermatology network will also provide the RACGP with guidance to help provide optimal support to members.
‘[We will] advise, for instance, the RACGP Expert Committee – Standards for General Practice about standards around dermatology practice for GPs who want to make sure they are doing skin excisions, biopsies, dermatological treatments, etc, correctly,’ Assoc Prof Rawlin said.
‘When it comes to the next review of the RACGP’s curriculum, we will be looking to have a part in that to ensure that remains up to date.
‘It is also likely that the network will have input into developing some cases for the RACGP exam, and possibly some continuing professional development [CPD] activities as well.’
While the Dermatology network has plenty of plans for the future, it has only just begun and Assoc Prof Rawlin underlined the fact it has significant scope for growth.
‘I think this network has a very broad remit in general practice and the potential to do lots of things,’ he said. ‘We are going to prioritise so we are not spreading ourselves too thin. The network will build over time.’
References1. Britt H, Miller GC, Henderson J, Bayram C, et al.
General practice activity in Australia 2014–15. Sydney: Sydney University Press, 2015. General practice series no. 38. Available at http://purl.library.usyd.edu.au/sup/9781743324523 [Accessed 12 September 2016].
RACGP SPECIFIC INTERESTS
About the networkAfter a long planning period, the RACGP’s Dermatology network was endorsed in June this year. Its goals are to increase GPs’ access to quality education in dermatology and to provide support and guidance for the design of RACGP courses, guidelines and assessments related to dermatology.
It will focus on the whole of dermatology within general practice.
Visit www.racgp.org.au/yourracgp/faculties/specific-interests or contact [email protected] for more information or to join the network.
We have some good news.Our Everyday Plus account will be the first everyday bank account to reward you with 1 Velocity Frequent Flyer Point^ for every $10 of daily average balance in your account, calculated at the end of each month.
There are no establishment or account keeping fees and you can redeem your points for flights, merchandise, holidays and more.
You will also have online and mobile banking, a 24/7 Client Service Centre and up to 10 free ATM withdrawals* from any major bank each month.
Apply now and get ready for take-o�. Visit boqspecialist.com.au/everydayplus or call 1300 131 141
The issuer of these products and services is BOQ Specialist - a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL no. 244616 (“BOQ Specialist”). Exclusively available for clients deemed by BOQ Specialist, in its sole discretion, to be engaged in the practice of medicine, dentistry and veterinary sciences. Terms and conditions, fees and charges and eligibility criteria apply. BOQ Specialist is not o�ering financial, tax or legal advice. You should obtain independent financial, tax and legal advice as appropriate. You should obtain and consider the relevant terms and conditions from boqspecialist.com.au/everydayplus before making any decision about whether to acquire the product. We reserve the right to cease o�ering these products at any time without notice. *10 free ATM transactions per month per account at BOQ, Commonwealth, Westpac, St George, NAB and ANZ branded ATMs. ^ To earn and redeem Velocity Points you must be a Velocity member. Velocity membership and Points earn and redemption are subject to the Member Terms and Conditions, available at velocityfrequentflyer.com, as amended from time to time.
Buckle up… earn Velocity Points on your everyday banking
BOQSA00602 V2 06/16

We have some good news.Our Everyday Plus account will be the first everyday bank account to reward you with 1 Velocity Frequent Flyer Point^ for every $10 of daily average balance in your account, calculated at the end of each month.
There are no establishment or account keeping fees and you can redeem your points for flights, merchandise, holidays and more.
You will also have online and mobile banking, a 24/7 Client Service Centre and up to 10 free ATM withdrawals* from any major bank each month.
Apply now and get ready for take-o�. Visit boqspecialist.com.au/everydayplus or call 1300 131 141
The issuer of these products and services is BOQ Specialist - a division of Bank of Queensland Limited ABN 32 009 656 740 AFSL no. 244616 (“BOQ Specialist”). Exclusively available for clients deemed by BOQ Specialist, in its sole discretion, to be engaged in the practice of medicine, dentistry and veterinary sciences. Terms and conditions, fees and charges and eligibility criteria apply. BOQ Specialist is not o�ering financial, tax or legal advice. You should obtain independent financial, tax and legal advice as appropriate. You should obtain and consider the relevant terms and conditions from boqspecialist.com.au/everydayplus before making any decision about whether to acquire the product. We reserve the right to cease o�ering these products at any time without notice. *10 free ATM transactions per month per account at BOQ, Commonwealth, Westpac, St George, NAB and ANZ branded ATMs. ^ To earn and redeem Velocity Points you must be a Velocity member. Velocity membership and Points earn and redemption are subject to the Member Terms and Conditions, available at velocityfrequentflyer.com, as amended from time to time.
Buckle up… earn Velocity Points on your everyday banking
BOQSA00602 V2 06/16

GP17RACGP CONFERENCE
ICC Sydney
gp17.com.au #GP17Sydney
Sydney + 26–28 October 2017 +
Register your interest to attend GP17 for your chance to WIN 1 of 6 iconic Sydney experiences * GP17 is the must-attend event on the general practice calendar. Connect with colleagues and broaden your clinical knowledge, while enjoying the natural beauty and vibrancy of Sydney.
Register your interest at gp17.com.au
The
foun
da
tion of patient-centred care
G
eneral practic
egp
Save the date
NSW: LTPS/16/07417. * Terms and conditions apply, see gp17.com.au for details.
4228 Good Practice-Full-page-v2.indd 1 11/10/2016 4:06:34 PM