IMCI Review
Transcript of IMCI Review
-
7/31/2019 IMCI Review
1/39
Community Health Nursing
Board Review
Integrated Management for
Childhood Illnesses (IMCI)
Prepared by:
Kit S. Lagliba, RN
-
7/31/2019 IMCI Review
2/39
At the start of a sick child
(2 months to 5 years) consultation
Determine if this is an initial or follow-up visit for this problem.
Ask the mother what the childs
problems are.
Kit Lagliba, RN
-
7/31/2019 IMCI Review
3/39
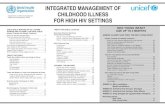
IMCI Case Management
Danger signsMain Symptoms
Nutritional statusImmunization status
Other problems
Need to Refer
Specific treatment
Homemanagement
ClassificationFocused Assessment
Identify treatmentTreat
Counsel caretakersFollow-up
TreatmentCounsel & Follow-up
-
7/31/2019 IMCI Review
4/39
Check for general danger signs
Ask: Not able to drink or breastfeed, Vomits everything,
Convulsions, orLook: Abnormally sleepy or difficult
to awaken
Need to Refer
(except in severe dehydration)
-
7/31/2019 IMCI Review
5/39
Ask about the main symptoms
Cough or difficulty in breathing
Diarrhea Fever
Ear problem
-
7/31/2019 IMCI Review
6/39
Cough or difficulty in breathing
Ask:
For how long?
Look: Count RR
Chest indrawing
Stridor
The child
must be calm.
-
7/31/2019 IMCI Review
7/39
SEVERE PNEUMONIA ORVERY SEVERE DISEASE
1st dose of antibiotic Vitamin A Breastfeeding/sugar water
URGENT REFERRAL
Any general danger sign or Chest indrawing or
Stridor
-
7/31/2019 IMCI Review
8/39
PNEUMONIA
Antibiotic for 5 days Relieve cough with safe remedy Advise mother on danger signs
Follow up in 2 days
Fast breathing
2 12 months old: 50/minute
1 year or older: 40/minute
-
7/31/2019 IMCI Review
9/39
NO PNEUMONIA: COUGH OR COLD
If cough
30 daysrefer to hospital for assessment Relieve cough with safe remedy Advise mother on danger signs
Follow up in 5 days if no improvement
No signs of pneumoniaor a very severe disease
-
7/31/2019 IMCI Review
10/39
Diarrhea: Classify
For dehydration
Persistent diarrhea
Blood in the stool
-
7/31/2019 IMCI Review
11/39
SEVERE DEHYDRATION
2 or more of the following:
Abnormally sleepy/difficult to wake Sunken eyes Not able to feed/drinking poorly Skin pinch goes back very slowly
Classify for dehydration
Plan C
-
7/31/2019 IMCI Review
12/39
IV treatment within 30 minutes
IV fluid: LRS 100 ml/kg body weight(in 6 hrs for infants; 3 hrs for children)
Plan C: To treat dehydration quickly
NO
NO
Oresol/NGT
-
7/31/2019 IMCI Review
13/39
Oresol p.o.
Plan C: To treat dehydration quickly
NO
NO
Oresol/NGT
URGENT REFERRAL
-
7/31/2019 IMCI Review
14/39
SOME DEHYDRATION
2 of the following:
Restless, irritable
Sunken eyes Skin pinch goes back slowly
Classify for dehydration
Plan B
-
7/31/2019 IMCI Review
15/39
Age < 4 mos 4-12 mos
Amount 200-400 400-700
Determine the amount (in ml) of Oresolto be given in 4 hours
= weight of the child (in kg) X 75, orif weight is unknown, use this chart.
Plan B: Treat some dehydration with ORS
-
7/31/2019 IMCI Review
16/39
Age 12 mos-2 yrs 2-5 yrs
Amount 700-900 900-1400
Determine the amount (in ml) of Oresolto be given in 4 hours
= weight of the child (in kg) X 75, orif weight is unknown, use this chart.
Plan B: Treat some dehydration with ORS
-
7/31/2019 IMCI Review
17/39
Show the mother how to give Oresol tothe child: frequent sips from a cup
If the child vomits, wait for 10 minutes.
Then continue, but more slowly. Continue breastfeeding if the child
wants to breastfeed. If the child develops puffy eyelids, stop
ORS.
Plan B: Treat some dehydration with ORS
-
7/31/2019 IMCI Review
18/39
After 4 hours: Reassess the child & classify for
dehydration.
Select appropriate plan. Begin feeding the child in the health
center.
Plan B: Treat some dehydration with ORS
-
7/31/2019 IMCI Review
19/39
NO DEHYDRATION
Not enough signs to classify asSEVERE DEHYDRATION or
SOME DEHYDRATION
Classify for dehydration
Plan A
-
7/31/2019 IMCI Review
20/39
Give extra fluid.
Plan A: Treat diarrhea at home
Up to 2 yrs 50 100 ml after each LBM
2 -4 yrs 100 200 ml after each LBM
Continue feeding.
Know when to return.
-
7/31/2019 IMCI Review
21/39
Persistent diarrhea: 14 days or more
Treat dehydration
Give Vitamin A
Refer to hospital
+ Dehydration=severe persistent diarrhea
-
7/31/2019 IMCI Review
22/39
Persistent diarrhea: 14 days or more
Advise regarding feeding
Give Vitamin A
Follow up in 5 days
No dehydration=persistent diarrhea
-
7/31/2019 IMCI Review
23/39
Blood in the stool = dysentery
Oral antibiotic for shigella for5 days
Follow up in 2 days
-
7/31/2019 IMCI Review
24/39
Fever: (history/temperature 37.5C or above)
Malaria risk?
Measles now or w/in last 3 mos
Dengue risk?
-
7/31/2019 IMCI Review
25/39
Fever: Ask about malaria risk
Residing in endemic area?OR:
Travel & overnight
stay in endemic area, or Blood transfusion
w/in past6 mos
-
7/31/2019 IMCI Review
26/39
Malaria risk +
Blood smear
Ask: Duration of fever?Present everyday?
Look: Stiff neck
Runny noseOther signs of measles
-
7/31/2019 IMCI Review
27/39
Malaria risk +any general danger sign or stiff neck
Quinine (under med. supervision)
1st dose of antibiotic, Paracetamol
Urgent referral
Very severe febrile disease/malaria
-
7/31/2019 IMCI Review
28/39
Malaria risk +, blood smear +No runny nose, no measles
Oral antimalarial
Paracetamol
Follow up in 2 days
> 7 days fever hospital for
assessment
Malaria
-
7/31/2019 IMCI Review
29/39
No malaria riskAny general danger sign or stiff neck
1st dose of antibiotic, Paracetamol
Urgent referral
Very severe febrile disease
-
7/31/2019 IMCI Review
30/39
Measles now or w/in last 3 mosClouding of cornea or
Deep or extensive mouth ulcers
1st dose of antibiotic, Vitamin A
Urgent referral
Severe complicated measles
-
7/31/2019 IMCI Review
31/39
Measles now or w/in last 3 mosPus draining from the eye or
Mouth ulcers
Vitamin A Tetracycline eye ointment
Gentian violet
Follow up in 2 days
Measles with eye or
Mouth complications
-
7/31/2019 IMCI Review
32/39
Measles now or w/in last 3 mosNo other signs
Vitamin A
Measles
-
7/31/2019 IMCI Review
33/39
If there is Dengue risk
Bleeding gums, nose, in vomitus orstools
Black vomitus or stools
Persistent abdominal painPersistent vomiting
Skin petechiae
Slow capillary refillNo signs, but fever > 3 days
Tourniquet test
-
7/31/2019 IMCI Review
34/39
Any of the danger signsor + tourniquet test
If skin petechiae, persistent abdominalpain or vomiting, or + tourniquet test
only signs, give ORS Any other signs of bleeding Plan C
Urgent referral
Do not give aspirin
Severe Dengue hemorrhagic fever
-
7/31/2019 IMCI Review
35/39
Ear problem:tender swelling behind ear
1st dose of antibiotic
Paracetamol for pain
Urgent referral
Mastoiditis
-
7/31/2019 IMCI Review
36/39
Ear discharge < 14 days orEar pain
Antibiotic for 5 days Paracetamol for pain
Wicking
Follow up in 5 days
Acute ear infection
-
7/31/2019 IMCI Review
37/39
Ear discharge for 14 days or more
Wicking Follow up in 5 days
Chronic ear infection
-
7/31/2019 IMCI Review
38/39
Visible severe wasting orEdema on both feet or
Severe palmar pallor
Vitamin A
Urgent referral
Severe malnutrition orsevere anemia
-
7/31/2019 IMCI Review
39/39
Some palmar pallor orVery low weight for age
Assess for feeding problem Pallor: iron & Albendazole
Wt for age very low: Vitamin A
Anemia or very low weight for age
Ki L lib RN