Hypertension: Medical Management and Nutritional Approaches.
-
Upload
hillary-greene -
Category
Documents
-
view
217 -
download
1
Transcript of Hypertension: Medical Management and Nutritional Approaches.

Hypertension: Medical Management and Nutritional Approaches

Hypertension Persistently high arterial blood
pressure Systolic blood pressure above 140
mm Hg and/or diastolic blood pressure above 90 mm Hg
Normotensive = 120/80 mm Hg Prehypertensive = 120–139/80-89
mm Hg Stage 1 hypertension = 140–159/90-
99 mm Hg Stage 2 hypertension = >160/>100
mm Hg

Prevalence and Incidence 29% of adult US population Related to body mass index High prevalence in African Americans 5% of pediatric population; prevalence increases
with age Strong positive relationship between blood pressure
and risk of CVD events

Pathophysiology
Blood pressure is a function of cardiac output multiplied by peripheral resistance
Affected by diameter of blood vessel Atherosclerosis decreases diameter, increases blood
pressure Drug therapy increases diameter, lowers blood
pressure

Circulatory Systems in the BodyCirculatory Systems in the Body
1. Coronary—supplies blood to heart muscle (can form collateral circulation)
2. Cerebral—supplies blood to head3. Splanchnic—supplies blood to abdomen
(exercise removes blood and food attracts blood to this area)
4. Pulmonary—supplies blood to lungs (O2 and CO2 exchange)
1. Coronary—supplies blood to heart muscle (can form collateral circulation)
2. Cerebral—supplies blood to head3. Splanchnic—supplies blood to abdomen
(exercise removes blood and food attracts blood to this area)
4. Pulmonary—supplies blood to lungs (O2 and CO2 exchange)

Measures of Heart Function
1. Beats or pulse2. BP systolic and diastolic3. ECG

Determinants of Blood Pressure
1. Blood volume2. Vascular resistance to pressure3. Heart stroke volume

Cardiac Output
■ Amount of blood pumped by heart (vol/min)■ Stroke volume times heart rate

Vascular Resistance
■ Viscosity of blood■ Width of vessels—(constriction or dilation)—controlled by muscle tone in vessel walls

Regulation of Blood PressureRegulation of Blood Pressure
1. Sympathetic nervous system (SNS)—responds immediately; baroreceptors monitor BPVasomotor center in brainSNS innervated tissues contract or dilate vascular bed
2. Renin-angiotensin system—retains Na and H2O to increase blood volume; constricts blood vessels; increases aldosterone
3. Kidneys—respond to renin-angiotensin system; aldosterone and antidiuretic hormone (ADH) are sent out as needed
1. Sympathetic nervous system (SNS)—responds immediately; baroreceptors monitor BPVasomotor center in brainSNS innervated tissues contract or dilate vascular bed
2. Renin-angiotensin system—retains Na and H2O to increase blood volume; constricts blood vessels; increases aldosterone
3. Kidneys—respond to renin-angiotensin system; aldosterone and antidiuretic hormone (ADH) are sent out as needed

Homeostatic Control of Blood Pressure
Short term—Sympathetic nervous system—Vasoconstriction—Vasodilation
Long term—Fluid volume—Renin-angiotensin system

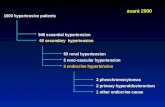
Hypertension
1. 90% HTN is essential HTN (cause unknown; perhaps prenatal impacts?)
2. 10% HTN is secondary to other diseases3. HTN is a risk factor for MI, CVA, renal failure

Renin-Angiotensin CascadeRenin-Angiotensin Cascade
Redrawn from Guyton AC: Textbook of medical physiology, ed 8, Philadelphia, 1991, WB Saunders.

Causes of HypertensionCauses of Hypertension
Algorithm content developed by John Anderson, PhD, and Sanford C. Garner, PhD, 2000.

Risk Factors for Developing Hypertension
Risk Factors for Developing Hypertension
(Adapted from National High Blood Pressure Education Program Working Group report on primary prevention of hypertension. Arch Intern Med 153:186, 1993. Copyright 1993, American Medical Association. Reprinted with permission.)

Risk Stratification in Patients with Hypertension
Risk Stratification in Patients with Hypertension
(From The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. sixth report (JNC VI). Arch Intern Med 157:2413, 1997.)

Uncontrolled HypertensionUncontrolled Hypertension
Leads to increased Workload on heart Damage to arteries Atherosclerosis Coronary heart disease esp. CHF Strokes Transient ischemic attacks (TIAs) Kidney damage Microvascular hemorrhages in brain and eye
Leads to increased Workload on heart Damage to arteries Atherosclerosis Coronary heart disease esp. CHF Strokes Transient ischemic attacks (TIAs) Kidney damage Microvascular hemorrhages in brain and eye

The DASH Diet Trials
Randomized feeding trial comparing effects of 3 diet patterns: control, high fruits/vegetables, and high fruits/vegetables/whole grains/lowfat dairy (DASH diet)
DASH diet high in potassium, magnesium, calcium, fiber and low in fat, saturated fat, and cholesterol
DASH diet significantly lowered BP in all groups, but especially in African-Americans

Effects of Diet on BP (DASH Trial)

OMNI-Heart Feeding Study
Subjects were 164 adults with prehypertension or stage 1 hypertension, 55% African American, mean BMI 30
Compared effect of 3 healthy diet patterns—all reduced in saturated fat and cholesterol, rich in fruits, vegetables, potassium, and other minerals at recommended levels
Diets were high CHO (58% of calories), high in protein, high in unsaturated fat
Researchers provided all the food for the study Each feeding period lasted 6 weeks and body weight
was kept constant.
http://www.medscape.com/viewarticle/523041

OMNI-Heart Diets
CHO Diet PRO DIET UNSAT FAT DIET
CHO % kcal 58 48 48
PRO % kcal 15 25 15
FAT % kcal 27 27 37
MFA % kcal 13 13 21
PUFA % kcal 8 8 10
SFA % kcal 6 6 6

OMNI-HEART Results
Results: All 3 diets lowered systolic blood pressure Substitution of protein or mfa for CHO lowered blood
pressure further; Compared with the carbohydrate diet, estimated 10-year coronary heart disease risk was lower and similar on the protein and unsaturated fat diets
http://www.medscape.com/viewarticle/523041

OMNI-Heart Feeding Study

U.S. Department of Health and Human
Services
National Institutes of Health
National Heart, Lung, and Blood Institute
The Seventh Report of the Joint National Committee onPrevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)Express—Succinct evidence-based recommendations. Published in JAMA May 21, 2003, and as a Government Printing Office publication.
The Seventh Report of the Joint National Committee onPrevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)Express—Succinct evidence-based recommendations. Published in JAMA May 21, 2003, and as a Government Printing Office publication.
National Heart, Lung, and Blood InstituteNational High Blood Pressure Education ProgramNational Heart, Lung, and Blood InstituteNational High Blood Pressure Education Program

For persons over age 50, SBP is a more important than DBP as CVD risk factor.
Persons who are normotensive at age 55 have a 90% lifetime risk for developing HTN.
Those with SBP 120–139 mmHg or DBP 80–89 mmHg should be considered prehypertensive who require health-promoting lifestyle modifications to prevent CVD.
New Features and Key Messages

New Features and Key Messages (Continued)
Thiazide-type diuretics should be initial drug therapy for most, either alone or combined with other drug classes.
Certain high-risk conditions are compelling indications for other drug classes.
Most patients will require two or more antihypertensive drugs to achieve goal BP.
If BP is >20/10 mmHg above goal, initiate therapy with two agents, one usually should be a thiazide-type diuretic.

Blood Pressure Classification
Normal <120 and <80
Prehypertension 120–139 or 80–89
Stage 1 Hypertension 140–159 or 90–99
Stage 2 Hypertension >160 or >100
BP Classification SBP mmHg DBP mmHg

CVD Risk
HTN prevalence ~ 50 million people in the United States.
The BP relationship to risk of CVD is continuous, consistent, and independent of other risk factors.
Each increment of 20/10 mmHg doubles the risk of CVD across the entire BP range starting from 115/75 mmHg.
Prehypertension signals the need for increased education to reduce BP in order to prevent hypertension.

Benefits of Lowering BP
Average Percent Reduction
Stroke incidence 35–40%
Myocardial infarction 20–25%
Heart failure 50%

BP Control Rates
Trends in awareness, treatment, and control of high blood pressure in adults ages 18–74
National Health and Nutrition Examination Survey, Percent
II1976–80
II(Phase 1)1988–91
II(Phase 2)1991–94 1999–2000
Awareness 51 73 68 70
Treatment 31 55 54 59
Control 10 29 27 34
Sources: Unpublished data for 1999–2000 computed by M. Wolz, National Heart, Lung, and Blood Institute; JNC 6.

BP Measurement Techniques
Method Brief Description
In-office Two readings, 5 minutes apart, sitting in chair. Confirm elevated reading in contralateral arm.
Ambulatory BP monitoring Indicated for evaluation of “white-coat” HTN. Absence of 10–20% BP decrease during sleep may indicate increased CVD risk.
Self-measurement Provides information on response to therapy. May help improve adherence to therapy and evaluate “white-coat” HTN.

CVD Risk Factors
Microalbuminuria or estimated GFR <60 ml/min
Age (older than 55 for men, 65 for women)
Family history of premature CVD (men under age 55 or women under age 65)
Hypertension*Cigarette smokingObesity* (BMI >30 kg/m2)Physical inactivityDyslipidemia*Diabetes mellitus*
*Components of the metabolic syndrome.

Target Organ Damage Heart
• Left ventricular hypertrophy• Angina or prior myocardial infarction• Prior coronary revascularization• Heart failure
Brain• Stroke or transient ischemic attack
Chronic kidney disease
Peripheral arterial disease Retinopathy

Goals of Therapy
Reduce CVD and renal morbidity and mortality.
Treat to BP <140/90 mmHg or BP <130/80 mmHg in patients with diabetes or chronic kidney disease.
Achieve SBP goal especially in persons >50 years of age.

Lifestyle Modification
Modification Approximate SBP reduction(range)
*Weight reduction 5–20 mmHg/10 kg weight loss
*Adopt DASH eating plan 8–14 mmHg
*Dietary sodium reduction 2–8 mmHg
Physical activity 4–9 mmHg
*Moderation of alcohol consumption
2–4 mmHg
*medical nutrition therapy interventions

Classification of Antihypertensive Drugs
Diuretics
—Thiazides—Loop diuretics—Potassium-sparing diuretics
Beta blockers (BB) Angiotensin II receptor blockers (ARBs) Alpha-beta blockers Alpha1 receptor blockers ACE inhibitors (angiotensin converting enzyme) Calcium antagonists Direct vasodilators

Algorithm for Treatment of Hypertension
Not at Goal Blood Pressure (<140/90 mmHg) (<130/80 mmHg for those with diabetes or chronic kidney disease)
Initial Drug Choices
Drug(s) for the compelling indications
Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB)
as needed.
With Compelling Indications
Lifestyle Modifications
Stage 2 Hypertension (SBP >160 or DBP >100 mmHg)
2-drug combination for most (usually thiazide-type diuretic and
ACEI, or ARB, or BB, or CCB)
Stage 1 Hypertension(SBP 140–159 or DBP 90–99
mmHg) Thiazide-type diuretics for most.
May consider ACEI, ARB, BB, CCB,
or combination.
Without Compelling Indications
Not at Goal Blood Pressure
Optimize dosages or add additional drugs until goal blood pressure is achieved.
Consider consultation with hypertension specialist.

Compelling Indications
These are reasons for using a particular class of medications
For example, patients with diabetes, kidney damage, and high blood pressure should begin treatment with ACE inhibitors.
Heart attack (in conjunction with hypertension) is a compelling indication for the prescription of beta-blockers and, in certain instances, ACE inhibitors
Heart failure should first be treated with ACE inhibitors and diuretics.

Classification and Management of BP for adults
BP classification
SBP* mmHg
DBP* mmHg
Lifestyle modification
Initial drug therapy
Without compelling indication
With compelling indications
Normal <120 and <80 Encourage
Prehypertension 120–139 or 80–89 Yes No antihypertensive drug indicated.
Drug(s) for compelling indications. ‡
Stage 1 Hypertension
140–159 or 90–99 Yes Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination.
Drug(s) for the compelling indications.‡
Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed.
Stage 2 Hypertension
>160 or >100 Yes Two-drug combination for most† (usually thiazide-type diuretic and ACEI or ARB or BB or CCB).
*Treatment determined by highest BP category.†Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension.‡Treat patients with chronic kidney disease or diabetes to BP goal of <130/80 mmHg.

Minority Populations
In general, treatment similar for all demographic groups.
Socioeconomic factors and lifestyle important barriers to BP control.
Prevalence, severity of HTN increased in African Americans.
African Americans demonstrate somewhat reduced BP responses to monotherapy with BBs, ACEIs, or ARBs compared to diuretics or CCBs.
These differences usually eliminated by adding adequate doses of a diuretic.

Children and Adolescents
HTN defined as BP—95th percentile or greater, adjusted for age, height, and gender.
Use lifestyle interventions first, then drug therapy for higher levels of BP or if insufficient response to lifestyle modifications.
Drug choices similar in children and adults, but effective doses are often smaller.
Uncomplicated HTN not a reason to restrict physical activity.

Web sitewww.nhlbi.nih.gov/

Your Guide to Lowering Blood Pressure

Reference Card

Lifestyle Modifications
Sodium: not more than 2.4 grams sodium/day Activity: activity like brisk walking 30 minutes/day most
days of the week Alcohol: not more than 1 drink a day for women; 2
drinks a day for men DASH diet: low in sodium, high in potassium, calcium,
cholesterol, saturated fat Weight: weight loss of as little as 10 lb can prevent or
treat high blood pressure

Weight Management
Risk of developing high blood pressure is 2-6 times higher in overweight than normal weight persons
20-30% of the hypertension in the US is attributable to excess weight
In Framingham, weight increase of 10% predicted rise in blood pressure of 7 mm/hg
Weight gain during adult life is responsible for much of the rise in blood pressure seen with aging

Weight Management
Excess body weight may increase blood pressure through increased insulin resistance and hyperinsulinemia, activation of the sympathetic nervous and renin-angiotensin systems, and changes in the kidney
Weight loss lowers vascular resistance, total blood volume, cardiac output, and sympathetic nervous system activity; improves insulin resistance
Weight loss in an overweight person is the single most effective lifestyle intervention to reduce blood pressure

Weight Management
In the Trial of Antihypertensive Intervention and Management, goal for energy intake to facilitate weight loss was 25 kcals/kg minus 500 to 1000 kcal daily to produce a .5 to 1 kg weight loss/week to achieve total weight loss of 4.5 kg.
Wylie-Rosett et al, 1993

Sodium and Hypertension
Relationship between sodium and hypertension is stronger in
Older people Those with a family history of hypertension Those with higher blood pressures at baseline 30-50% of hypertensives and 15-25% of normotensives
are salt sensitive Salt sensitivity more common in black race, obesity,
advanced age, diabetes, renal dysfunction, use of cyclosporine

Sodium and Hypertension
Addition of a sodium restriction to a DASH diet lowers SBP 3 mmHg and DBP 2 mmHg
This reduction is associated with a 17% reduction in prevalence of hypertension, 6% reduction in CHD, 15% reduction in stroke and TIA

Salt Restriction
Recommendation is for moderate salt restriction (6 grams salt, 100 mEq or 2400 mg Na daily)
Salt is the issue, because chloride ion with sodium raises blood pressure
May normalize blood pressure in Stage 1 hypertension

Levels of Na RestrictionLevels of Na Restriction
g Na mEq Na Description4 174 No added salt2-3 87-130 Mild to moderate
restriction1 43 Strict sodium restriction0.5 22 Severe sodium restriction
g Na mEq Na Description4 174 No added salt2-3 87-130 Mild to moderate
restriction1 43 Strict sodium restriction0.5 22 Severe sodium restriction

Alcohol and Hypertension
5-7% of hypertension is due to alcohol consumption
3 drinks per day is the threshold for raising blood pressure; associated with a 3 mmHg increase

Physical Activity and Hypertension
Less active persons are 30-50% more likely to develop hypertension than active persons
Medium to high levels of activity protective against stroke (Framingham)
Walking reduces blood pressure in adults by an average of 2%
In a meta-analysis of 54 randomized trials, walking reduced blood pressure an average of 4 mmHg, irrespective of weight change

Potassium
In population studies, potassium intake and blood pressure are inversely related
Sodium/potassium ratio is important Sodium/potassium ratio of 1:1 a 3.4 mmHg decrease in
systolic BP is predicted High potassium intake inversely related to stroke

Other Factors
Calcium, Magnesium, and Lipids: role still unclear DASH diet high in lowfat dairy products

Response to Dietary RxResponse to Dietary Rx
Salt sensitive respond well to sodium restriction Most respond to increased potassium in diet.
• 1.1 to 3.3 g Na is safe• 1.9 to 5.6 g K is recommended to achieve ratio Na:K of
1, which is goal If taking a potassium-wasting diuretic drug, increased
potassium in diet is essential. Most respond to increased calcium (at least the RDA)—use
the DASH diet protocol
Salt sensitive respond well to sodium restriction Most respond to increased potassium in diet.
• 1.1 to 3.3 g Na is safe• 1.9 to 5.6 g K is recommended to achieve ratio Na:K of
1, which is goal If taking a potassium-wasting diuretic drug, increased
potassium in diet is essential. Most respond to increased calcium (at least the RDA)—use
the DASH diet protocol

DASH Diet
Works within 14 days Lowers BP quite well Includes more potassium, calcium,
other nutrients

DASH Fact Sheet
www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf

DASH Diet —cont’d Pattern
—7-8 whole grains—4-5 vegetables—4-5 fruits—2-3 low-fat or fat-free dairy products—6 oz or less meat/poultry/fish—4-5 servings nuts, beans, or legumes/week—2-3 servings fat (total kcal = 27% fat)

DASH Diet Patterns for Different Calorie Levels
Kcals Grain Veg Fruit Dairy Meat/ Pro
Nuts/ Legume
Fats/ oils
1600 6 4 4 2 1 .5 1
2000 8 5 5 3 2 1 2
2600 10 5 5 3 2 1 2
3100 13 6 6 4 2 1 3

Sodium Processed and restaurant foods provide 80% of sodium
intake Read labels; sodium content of different brands varies 10% added in cooking at home and at table; 10% naturally
occurring Americans consume ~4,000 mg/day; 2005 Dietary Guidelines
for Americans recommend <2,300 mg/day; those with hypertension, African Americans and middle-aged and elderly should consume <1,500 mg/day

Food Label Terms
Sodium free, no sodium = <5 mg/serving Very low sodium = <35 mg/serving and per 100 g food Low sodium = <140 mg/serving and per 100 g food Reduced sodium = 50% less than comparison food

Salt SubstitutesSalt Substitutes
Composition: KCl, CaCl, Al-Cl KCl can provide extra potassium for those taking
diuretics KCl can be harmful if patient has renal insufficiency “Lite” salt contains sodium Some spices and herbs are low in sodium Others are high in sodium
Composition: KCl, CaCl, Al-Cl KCl can provide extra potassium for those taking
diuretics KCl can be harmful if patient has renal insufficiency “Lite” salt contains sodium Some spices and herbs are low in sodium Others are high in sodium

Classification of Antihypertensive Drugs
Diuretics
—Thiazides—Loop diuretics—Potassium-sparing diuretics
Beta blockers (BB) Angiotensin II receptor blockers (ARBs) Alpha-beta blockers Alpha1 receptor blockers ACE inhibitors (angiotensin converting enzyme) Calcium antagonists Direct vasodilators

http://www.nhlbi.nih.gov/hbp/treat/bpd_type.htm

Lifestyle Modifications for Prevention of Hypertension
Lose weight if overweight Limit alcohol Increase physical activity Decrease sodium intake Keep potassium intake at adequate levels Take in adequate amounts of calcium and magnesium Decrease intake of saturated fat and cholesterol Stop smoking

Summary
Lifestyle modifications for prevention of hypertension—quite effective!
Management of hypertension—very important to reduce risk of heart attack or stroke