How doctors can help patients participate in their care
description
Transcript of How doctors can help patients participate in their care

How doctors can help patients participate in their care
The Good Hospital Practice Training series 2009
The Medical City

Outline of presentation
• Why is patient participation important?– What we know from research– What we know from experience
• Communicating well with patients• Communication barriers to informed consent• Good patient communication produces better health outcomes• The role of the Attending Physician• General guidelines in securing informed consent
– Consent is a continuing process– Patients can refuse treatment anytime– Information must be provided and suited to patient’s readiness– Emergency patients must consent to treatment
• Quiz

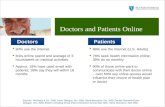
What we know from research• Many more patients want more information and
responsibility.• The average consultation time does not permit all the
information transfer that is desired.• Patients have different preferred consulting styles;
clinicians are not good at identifying the preferred consulting style.
• Patients find it easier to communicate with computers than with some clinicians they meet.
• Educational levels are less important than was thought.• Value must be addressed in preference decisions.

What we know from experience
• The patient is the only person present throughout their care.
• The education of patients is easier than the reeducation of clinicians.
• Many patients are more intelligent than clinicians.• Clinicians are always behind the Zeitgeist.• An understanding of biochemistry is not
necessary for making crunch decisions• Writing clearly for patients helps clinicians
understand.

Good patient communication produces better health outcomes
• Good patient communication enables patients to better participate in their care, thus producing better health outcomes, including – recovery of psychological and functional status– symptom recovery– recovery from emotional problems– improved blood pressure– Improved blood sugar control– Improved headache control and – better functioning after treatment. (based on 1994
review of 21 studies (11 of which are RCTs)

Key elements of effective patient communication
• MD asks many questions• MD shows support and empathy• Patients express themselves fully• Patients feel that the problem has been fully
discussed

Anatomy of a patient’s decision
Patient Googles disease.
Patient reads newspaper.
Patient watches Grey’s Anatomy.
Patient talks to neighbor.
Patient shops for MDs.
You talk to patient.

What’s wrong with how we communicate with patients?
• 45% of patients’ concerns are not elicited by MDs• 50% of psychosocial and psychiatric problems are
missed by MDs• In 50% of visits the patient and MD do not agree on the
nature of the main presenting problem• MDs interrupt patients, on average, 18 seconds into the
patient’s description of the presenting problem.• The majority of malpractice suits arise from
communication errors not competency. The patients’ most common complaint is the lack of information provided by MDs.

What we need to tell patients before beginning treatment
• “We think your diagnosis is …. It may be due to …. If untreated, you will experience….”
• The goal of treatment is…. What are your goals?”• “If treated with this option, you will experience the following
benefits:… The risks are … and they may occur in …% of patients. The side effects are … and they may occur in …% of patients. Other treatment options have the following benefits, risks and side effects:…, …, ….
• “The estimated cost of treatment is ….”• “If at anytime you feel you don’t want to go through
treatment, just let me know and I will stop.”• “Should anything unexpected happen to you, I will make
sure you know.”

Obtaining an informed consent is key to good patient communication
BEFORE obtaining an informed consent,
1. Assess readiness of patient and relatives– to receive and understand medical information– to make rational decisions – to express what they truly want
2. Address barriers to readiness– Establish rapport and show empathy– Provide visual and other communication aids– Manage medical conditions that impair ability to
receive and express communication messages

Obtaining an informed consent is key to good patient communication
3. Provide adequate information to support rational decision making to patients and relatives – Nature of illness or condition– Patient-centered goals of treatment (ask the patient
what his / her goals are) – Patient-centered description of the proposed
treatment/s (describe what will the patient experience)– Benefits, risks, side effects and estimated costs of
proposed treatment/s, other treatment options, including no treatment (and its consequences)
– Names of all participating physicians

Obtaining an informed consent is key to good patient communication
4. Assess understanding of the conveyed information– Ask questions to patient and relatives to assess that
they have understood and can retain the information long enough to use it and weigh it in the balance to arrive at a decision
– Explore impact of conveyed information on existing beliefs and attitudes of patients and relatives
– Clarify, illustrate, paraphrase unclear messages

Obtaining an informed consent is key to good patient communication
AFTER obtaining an informed consent,
5. Document the informed consent – Ensure that the consent is freely given– Ensure that the informed consent form is completely
filled up prior to initiation of treatment. Remember that the consent form is evidence of the process, not the process itself.
6. REPEAT the process whenever needed– When new treatments are proposed– When patient’s clinical course significantly changes

Consent is a continuing processFor how long is consent valid?Consent should be perceived as a continuing process rather
than a one-off decision. The AP must reaffirm consent if it appears that the patient may have changed his or her mind or there may have been clinical developments. The AP must give the patient continuing opportunities to ask further questions and to review the decision.
Do certain examinations / tests require written consent?Generally a written consent is not legally required but may be
advisable in some cases. The consent form simply documents that some discussion about the procedure or investigation has taken place.

Information must be provided and suited to patient’s readiness
What should be done when a patient asks the AP to make the decision on his or her behalf?
The AP should explain to patients the importance of knowing the treatment options open to them. If patients still insist they do not want to know in detail about their condition and its treatment, the AP must still provide basic information about the treatment before proceeding.

Information must be provided and suited to patient’s readiness
What should be done where a patient’s relative asks the AP to withhold information from the patient?
Where the patient is competent, the AP should assess his/her readiness to consent. APs should not withhold relevant information unless its disclosure would cause the patient serious harm. Although distress could constitute “harm” in some circumstances, this is not always accepted as sufficient reason to withhold relevant information.

Emergency patients must consent to treatment
Does consent need to be obtained for emergency treatment?
Yes, if the ER physician determines that the patient is competent.
Can treatment be provided in an emergency situation where the patient is unable to give consent?
Yes, provided that the medical treatment is in the patient’s best interests and is immediately necessary to save life or avoid significant deterioration in the patient’s health.

Pediatric patients must assent to treatment
Are children below 18 yrs presumed to be competent to give consent?
No, but assent must be sought from those who have sufficient understanding of the nature and possible consequences of the procedure or treatment.

These patients must consent to treatment!
1. A patient who is suffering from a mental disorder is not necessarily incompetent to consent to treatment.
2. Patients who may be temporarily incapable of giving valid consent due to fatigue, drunkenness, shock, fear, severe pain or sedation are not necessarily incompetent.
The fact that an individual has made a decision that appears to be irrational or unjustified should not be taken as evidence that the individual is incompetent. If, however, the decision is clearly contrary to previously expressed wishes, or is based on a misperception of reality, further investigation by the ER physician or AP is required.

Patients can refuse treatment anytime
Can patients withdraw consent during a procedure?
Yes. Patients can change their minds about a decision at any time, as long as they have the capacity to do so.
Can a competent patient refuse treatment?Yes. Competent adult patients are entitled to
refuse consent to treatment even when doing so may result in permanent physical injury or death, if they are properly informed and are not being coerced.

How can patients refuse treatment?
When patients decide to forego treatment, their Attending Physicians ensure that they are fully informed of the consequences of their decision.
Patients can then sign the hospital waiver form.Patients can also create advance directives to
specify what end-of-life treatments they want and do not want to receive.
Advance directives (ADs) are legal documents which allow people to convey their decisions about end-of-life care ahead of time.

How do we inform patients of advance directives?
In TMC, all patients for admission are routinely informed by admitting staff of the AD policy.
For patients and families who are likely to face end-of-life decisions, the Attending Physician initiates discussions regarding AD, either on his own or upon request of patients / families.
The patient, family and the Attending Physician are all involved in discussing and writing ADs.
Often, having an AD helps families make difficult decisions about the medical care of their loved ones when the latter are unable to decide for themselves.

What are examples of advance directives?
• Living will – instructions documenting a person's wishes about medical care intended to sustain life.
• Durable power of attorney - legal document that names a patient's health care proxy*. Once written, it should be signed, dated, witnessed, notarized, copied, distributed, and incorporated into the patient's chart. * Health care proxy - an agent (a person) appointed
to make a patient's medical decisions if the patient is unable to do so.

What types of life-sustaining care can be considered in advance?
• the use of life-sustaining equipment (dialysis machines, ventilators, and respirators);
• "do not resuscitate" orders; that is, instructions not to use CPR if breathing or heartbeat stops;
• artificial hydration and nutrition (tube feeding);• withholding of food and fluids;• palliative/comfort care; and• organ and tissue donation.

How do we manage patients who refuse treatment?
• Same as any other patient! Their refusal does not mean they expect or need less general care from us. They are entitled to
A. Continuing information and communicationB. Continuing assessment of their needs, especially relief from
pain and suffering, privacy, etc.C. Specific interventions to enhance quality of life, emotional and
physical well being, including possible referral to TMC Palliative Care program
D. Continuing participation in decision making – Do not resuscitate decisions automatically expire and must be renewed after 3 days. They can be rescinded any time.
E. Continuity of care at home, including possible enrollment in TMC Home Care program.

Summary of presentation
• Patients know more than we think. We ought to spend time communicating the right information to them.
• Good patient communication is essential to helping patients participate in their care.
• Good patient communication produces better health outcomes• In obtaining an informed consent, Attending Physicians (APs) must
take time to assess patient’s readiness and understanding. • Consent is a continuing process. APs must provide updated
information to ensure continuing consent.• Emergency patients must consent to treatment.• Patients can refuse treatment anytime. Attending Physicians must
discuss advance directives to patients and families facing end of life issues.

What have we learned?(choose as many answers as deemed applicable)
1. Good patient-physician communication leads to A. recovery from emotional problemsB. improved blood pressureC. Improved blood sugar controlD. Improved headache control Answer: ? Answer/s?
2. Research has shown that MDs interrupt patients, on average, ____ seconds into the patient’s description of the presenting problem.
a. 18b. 25c. 32d. 41Answer/s?

What have we learned?(choose as many answers as deemed applicable)
3. Good patient-physician communication is characterized by
A. MDs asking many questions
B. MDs providing complete information
C. Patients expressing themselves fully
D. Patients freely voicing out all their complaints.
Answer/s?
4. Good patient-physician communication is important because
A. Medication errors are avoided.
B. Malpractice litigations are avoided.
C. Patients adhere to their treatments better.
D. Physicians are more satisfied with their own roles.
Answer/s

What have we learned? (choose as many answers as deemed applicable)
5. The following is/are element/s of informed consent:a. Patients must be competent in making decisions. b. The physician must provide information on all possible treatment risks and side effects.c. The patient must be given ample time to think before consenting to the proposed treatment.d. The physician must assess if patient is emotionally prepared to receive the information.
Answer/s?6. An informed consent must be obtained
a. Before emergency treatment is doneb. During confinement, when substantial changes in management are neededc. Whenever patient may have changed his/her mindd. Before every course of chemotherapy
Answer/s?

What have we learned? (choose as many answers as deemed applicable)
7. An assessment of patients’ understanding includes evaluating if they a. understand what the medical treatment is, its purpose and nature and why it is being proposedb. understand its principal benefits, risks and alternativesc. can retain the information for long enough to use it and weigh it in the balance in order to arrive at a decisiond. can make logical decisions based on the given informationAnswer/s?
8. The following is/are true about advance directivesA. Only patients who are at the brink of death should make advanced
directivesB. TMC staff should not routinely inform patients of the advance directives
policy.C. Families can override the patient’s advance directives.D. None of the above
Answer/s?

What have we learned? (choose as many answers as deemed applicable)
9. Which of the following is/are NOT competent to give an informed consent?a. A patient who is suffering from a mental disorderb. A patient suffering from alcoholic intoxicationc. A patient suffering from shock and severe paind. None of the aboveAnswer/s?
10. If a patient’s relative requests the AP not to reveal the illness to the patient for fear of causing severe depression, the AP musta. Refrain from revealing the illness to the patient b. Evaluate how much information the patient already knows and how much he needs to decide on the proposed treatmentc. Reveal the illness to the patient at all costs because the patient can give informed consent only if all the facts are presentedd. Re-assess at every visit the patient’s readiness to receive informationAnswer/s?

Are you an effective patient communicator?
10 out of 10 – patient-centered champion!
8 or 9 out of 10 – budding role model
7 or 8 out of 10 – getting there
5 or 6 out of 10 – just about barely passed
3 or 4 out of 10 – you can clinch it next time!*
0, 1 or 2 out of 10 – let us try again*
* Please go over the slides again.
Answers:
1. A,B,C,D
2. A
3. A,B,C,D
4. A,B,C,D
5. A,C,D
6. A,B,C,D
7. A,B,C,D
8. D
9. D
10. B,D

Thank you!
• Practice makes perfect!
• Practice effective communication skills with your ambulatory patients.
• Practice obtaining informed consent again among your “long playing” patients.

This SIM Card certifies that
______(please overwrite with your name, thank you)__, MD
has successfully completed the
Self Instructional Module on Sedation and
Restraints.
(Sgd) Dr Alfredo Bengzon (Sgd) Dr Jose AcuinPresident and CEO Director, Medical Quality Improvement