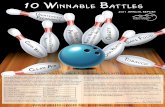
Eliminating Lymphatic Filariasis in the Americas A Winnable Battle
HIV Winnable Battle presentation
-
Upload
publichealthfoundation -
Category
Health & Medicine
-
view
635 -
download
2
description
Transcript of HIV Winnable Battle presentation

HIV Prevention
Centers for Disease Control and Prevention

Burden of HIV in the United States
1.1 million people living with HIV Net increase of 40,000 people with HIV
infections each year 56,000 new infections (2006) 16,000 deaths (2006) HIV infected people who start antiretroviral
treatment (ART) are now expected to live at least an additional 35 years
Lifetime treatment costs of ~$400,000

Number of people living with HIV continues to increase sharply
19
77
19
78
19
79
19
80
19
81
19
82
19
83
19
84
19
85
19
86
19
87
19
88
19
89
19
90
19
91
19
92
19
93
19
94
19
95
19
96
19
97
19
98
19
99
20
00
20
01
20
02
20
03
20
04
20
05
20
06
0
200,000
400,000
600,000
800,000
1,000,000
1,200,000
New HIV Infections (Incidence)People Living With HIV/AIDS (Preva-lence)
JAMA 2008;300(5):520-529.Campsmith M, et al. CROI 2009.
HIV Incidence and Prevalence, United States, 1977–2006

Stark disparities in HIV/AIDS among different groups
95% of people with AIDS are MSM, African American, Latino, or IDU
African Americans are 8 times more likely than whites to have HIV
Latinos are 3 times more likely to have HIV than whites
MSM are >40 times more likely to have HIV than other men and women
CDC, HIV Surveillance Report,2008. Published June 2010. www.cdc.gov/hiv/surveillance/resources/reportsMSM = Men having sex with menIDU = Intravenous drug users

From 2005-2008, the percentage of HIV diagnoses attributed to male-to-male sexual
contactincreased — 37 states and 5 U.S. dependent
areas
2005 2006 2007 20080
10
20
30
40
50
60
Year of diagnosis
Dia
gn
oses,
%
Male-to-male sexual contact
Heterosexual contact1
Injection drug use
Male-to-male sexual contact and injection drug use Other2
Note: Data include adults and adolescents with a diagnosis of HIV infection regardless of stage of disease at diagnosis. Data from 37 states and 5 U.S. dependent areas with confidential name-based HIV infection reporting since at least January 2005. All displayed data have been estimated. Estimated numbers resulted from statistical adjustment that accounted for reporting delays and missing risk-factor information, but not for incomplete reporting.
1Heterosexual contact with a person known to have, or to be at high risk for, HIV infection. 2 Includes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified.

In 2008, the majority of HIV diagnoses among males were attributed to male-to-male sexual contact; among females the majority were attributed to heterosexual
contact — 37 states and 5 U.S. dependent areas
72%
15%
9%
4% <1%
MalesN=31,595
84%
15%
1%
FemalesN=10,662
Heterosexual contacta
OtherbMale-to-male sexual contact Injection drug use (IDU)Male-to-male sexual contact and IDU
Note: Data include adults and adolescents with a diagnosis of HIV infection regardless of stage of disease at diagnosis. Data from 37 states and 5 U.S. dependent areas with confidential name-based HIV infection reporting since at least January 2005. All displayed data have been estimated. Estimated numbers resulted from statistical adjustment that accounted for reporting delays and missing risk-factor information, but not for incomplete reporting.
a Heterosexual contact with a person known to have, or to be at high risk for, HIV infection. b Includes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified.

From 2005-2008, the percentage of HIV diagnoses increased among Blacks/African
Americans – 37 states and 5 U.S. dependent areas
2005 2006 2007 20080
10
20
30
40
50
60
Note: Data include adults and adolescents with a diagnosis of HIV infection regardless of stage of disease at diagnosis. Data from 37 states and 5 U.S. dependent areas with confidential name-based HIV infection reporting since at least January 2005. All displayed data have been estimated. Estimated numbers resulted from statistical adjustment that accounted for reporting delays, but not for incomplete reporting.
a Hispanics/Latinos can be of any race.
Black/African American
Hispanic/Latinoa
White
American Indian/Alaska Native
Asian
Native Hawaiian/Other Pacific Islander
Multiple races
Year of diagnosis
Dia
gn
oses,
%

HIV prevention worksSaves lives and money
Our collective prevention efforts have led to a dramatic reduction in HIV infections• Estimated number of new HIV infections per year was
130,000 in 1985
• Down to an estimated 56,000 new HIV infections per year in 2006
Conservative estimates are that prevention efforts have:• Averted more than 350,000 HIV infections in the United
States
• Saved more than $125 billion in medical costsSource: Holtgrave DR. Written testimony on HIV/AIDS incidence and prevention for the US House of
Representatives Committee on Oversight and Government Reform. September 16, 2008.

Key HIV prevention strategies
Promote: Abstinence (or delaying sex) Fewer sexual partners (ideally,
monogamous relationship with an uninfected partner)
Consistent and correct use of condoms (male/female)
Not sharing syringes for injection drug use

Cost benefits of HIV prevention
Pennies
Cost of condoms
~$400,000
Lifetime cost of treating one HIV-infected person

Other HIV prevention strategies
Antiretroviral drugs (ARVs):• To prevent perinatal
transmission
• To reduce infectiousness
• To prevent new infections (as Pre-Exposure Prophylaxis [PrEP])
Male circumcision• To reduce risk of HIV
infection through penile-vaginal sex

Pre-Exposure Prophylaxis (PrEP)
Potential users: HIV-uninfected persons at high risk of becoming infected• High risk may include sexual partner who has HIV,
multiple partners, frequent STDs, or other evidence of high risk
• Recent trial demonstrates the safety and efficacy of PrEP for MSM at high risk
Cost-effectiveness depends on:• HIV incidence in target groups• Cost of medication and services• Ability to maintain or increase existing risk reduction
behavior• Adherence to medication• $34,000-$320,000 per QALY saved
Source: Paltiel et al. CID 2009:48(6):806-816 Smith, et al. MMWR 2011:60(03);65-68

PrEP with daily tenofovir/emtracitabine can reduce HIV risk in MSM
44% reduction in acquisition
Source: Grant RM et al. (2010). NEJM; published online Nov. 23, 2010.

Policy, Systems, and Environmental Change
Integrating Prevention and Healthcare
Policy development and support Guidelines and recommendations (testing,
prevention with positives, ART)
Quality measures: Development and uptake
Reimbursement coding guidance

Policy, Systems, and Environmental Change
Integrating Prevention and Healthcare
New programs and models Expanded Testing Initiative: 30 jurisdictions
covering >90% of epidemic
• Over 2.6 million HIV tests conducted; 27,000 HIV infections diagnosed
Enhanced HIV Prevention Planning: 12 urban areas covering 44% of epidemic
• Integrating HIV prevention, care, treatment services across health care system and community

Testing and diagnosis is prevention
21% (230,000) with undiagnosed HIV • Account for
approximately 50% of new HIV transmissions
79% (870,000) with diagnosed HIV• More likely than
undiagnosed to access prevention and treatment
Source: Marks G, et al (2006). AIDS 20(10): 1447-1450.

HIV testing is a prevention strategy
CDC’s 2006 HIV Testing Recommendations for Health Care Settings• Promote routine screening of patients age 13-64
Routine, opt-out screening in clinical settings costs $2,000-$6,000 per HIV
diagnosis confirmed
Source: Campsmith M et al. (2010). JAIDS 53:619--24.

Key approaches and program considerations in HIV prevention
HIV testing and linkage to care Prevention with positives Policy and structural interventions Targeted interventions Surveillance, monitoring, and evaluation Evidence-based planning Health equity Health reform Program collaboration and service
integration

Focusing resources
Burden of disease• Geographic distribution• Groups disproportionately affected by HIV (MSM, African
Americans, Latinos, injection drug users) HIV prevention services
• For people living with HIV• For people at high risk for HIV infection
Monitoring the epidemic, sharing, and using information
Discovering and operationalizing new interventions

Maximizing impact
Target programs to people and geographic areas most at risk for transmission or acquisition
Focus on interventions with evidence for large effect size
Choose feasible efforts with potential for large-scale implementation

“The United States will become a place where new HIV infections are rare and when they do occur, every person, regardless of age, gender, race/ethnicity, sexual orientation, gender identity or socio-economic circumstance, will have unfettered access to high quality, life-extending care, free from stigma and discrimination.”
—Vision of the National HIV/AIDS Strategy