History of arrhythmias
-
Upload
asadsoomro1960 -
Category
Health & Medicine
-
view
105 -
download
3
Transcript of History of arrhythmias

CARDIAC CARDIAC ARRHYTHMIASARRHYTHMIAS
Diagnosis and ManagementDiagnosis and ManagementDr. Asadullah Khan Soomro
Diploma Cardiology Royal Brompton
National Heart &Lung Institute
University of London
King Fahad Hofuf Hospital
Email; [email protected]

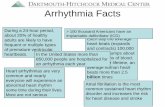
IntroductionIntroductionCCardiac arrhythmias leading to ardiac arrhythmias leading to
sudden cardiac death is estimated to sudden cardiac death is estimated to claim claim 2,50,0002,50,000 lives annually or lives annually or 2525 lives per million people per week in Unites lives per million people per week in Unites States.States.
IIn more than n more than 80%80% of cases sudden of cases sudden death is caused by abrupt onset of death is caused by abrupt onset of ventricular tachycardia and may progress ventricular tachycardia and may progress to ventricular fibrilation.to ventricular fibrilation.

• Family physicians &nurses working at primary, secondary and tertiary care hospital, are usually confronted with cardiac rhythm problems, which need to be high litened with regards to practical diagnosis and management, which is based not only on electrocardiogram but thorough history and physical examination indeed,

History of ArrhythmiasHistory of Arrhythmias• 1903 – Willem Einthoven developed
electrocardiogram.
• 1876 – Marey discover extra systoles
• 1827 – Robert Adams was first to recognize atrial fibrillation as a sign of mitral stenosis.
• 1867 – Cotton described first supraventricular tachycardia.

• 1761 – Morgagni recognized CHB as most ancient arrhythmias.
• 1862 – Panum induced ventricular tachycardia.
• 1909 – First ECG of V.T. in man was published by Thomas Lewis.
• 1842 – Ventricular fibrillation was first described by Erichsen.
• 1902 – Mackenzie described sick sinus syndrome.
• 1928 – Paul Dudley white discover WPW syndrome.

Major Arrhythmias and AV BlocksMajor Arrhythmias and AV Blocks
Arrhythmias Interpretation
Sinus P wave of normal shape in front of each QRS with regular R.R. interval
Nodal P waves may be absent or if present occur after QRS and are inverted
Atrial P waves of unusual shape, abnormal number of P waves per QRS, absent P waves
Ventricular Wide, bizarre-looking QRS

A.V. Blocks Interpretation
1st degree Prolongation of PR interval (> .20)
2nd degree
Type I (Wenckebach)
Type II
2:1, 3:1 AV block
Progressive prolong P-R interval with drop QRS
Some P waves are not conducted but conducted beats have normal constant PR interval.
Third degreeP waves and QRS complexes are entirely independent “complete AV dissociation”
Regular R-R with slow heart rate.


Causes of Cardiac Causes of Cardiac ArrhythmiasArrhythmias
Coronary artery diseaseCoronary artery diseaseRheumatic heart diseaseRheumatic heart disease
Congenital heart defectsCongenital heart defects
CardiomyopathiesCardiomyopathies
Pericardial diseasesPericardial diseases
HypertensionHypertension
MiscellaneousMiscellaneous

CardiacCardiac ArrhythmiasArrhythmiasSymptomaticSymptomatic______________________
AsymptomaticAsymptomatic
Structural heartStructural heartDiseaseDisease
__________________________
Normal heartNormal heart
Normal Normal E.F. >50%E.F. >50%
Normal heart sizeNormal heart size
________________________EnlargedEnlarged
heart sizeheart size
Cardiac originCardiac origin________________________Non-cardiacNon-cardiac
originorigin

Regular rhythm Irregular rhythmREGULAR RHYTHMREGULAR RHYTHM
a. a. Normal rateNormal rate
Sinus rhythm
Non-sinus (pacemaker)
b. Rapid rateb. Rapid rate
Sinus tachycardia
Supraventricular tachycardia
Ventricular tachycardia
c. Slow ratec. Slow rate
Sinus bradycardia
AV nodal rhythm
AV block
Analysis of ArrhythmiasAnalysis of Arrhythmias


Analysis of ArrhythmiasAnalysis of ArrhythmiasThere are different ways of approaching
arrhythmias, the choice depends upon the level of understanding of the reader.
For rhythm analysis, ask the following questions.
• Is the rhythm regular?• If so, is the rate normal, rapid, slow?
• If irregularRegularly irregular?Irregularly irregular?

Arrhythmias EvaluationArrhythmias Evaluation• Asymptomatic
•Symptomatic PalpitationDizzinessNausea/vomitingSyncopeAnginaDyspnoeaNeurological defecit

Arrhythmias EvaluationArrhythmias Evaluation
• Thorough Physical Examination Pulse (Regular, irregular)Blood pressureJVP, TemperatureCarotidsThyroid glandPre-cordial (Palpation, Auscultation)

Arrhythmias EvaluationArrhythmias Evaluation• Investigations
Routine, renal function, electrolytesThyroid function test, drug level12 lead ECG with rhythm stripX-ray chestECG at time of symptom24 hour Holter monitoringStress testEchocardiogramStress thalliumCardiac catheter, angiogramElectrophysiological studies

IRREGULAR RHYTHMIRREGULAR RHYTHM
a. Regular irregulara. Regular irregular
Sinus arrhythmias
Bigeminy, trigeminy
Wenckebach
b. Irregularly irregularb. Irregularly irregular
Atrial fibrillation
Atrial flutter with block
Ventricular fibrillation
c. Infrequent irregularlyc. Infrequent irregularly
PVC, APC
AV dissociation
2nd degree block
Analysis of ArrhythmiasAnalysis of Arrhythmias

Sinus tachycardiaSinus tachycardiaIt is usually a physiological response
but may be precipitated by sympathomimetic drugs or endocrine disturbance.
• Rate rarely exceed 200/min.• Each P wave is followed by QRS.• P wave morphology and axis are normal.• Height of P wave may increase PR shorten.• With fast tachycardia P wave merged in T
wave.

Causes of Sinus TachycardiaCauses of Sinus Tachycardia• Physiological.
– Exertion, anxiety and pain.
• Pathological. – Fever, anaemia, hypovolaemia, hypoxia.
• Endocrine.– Thyrotoxicosis, pheochromocytoma.
• Pharmacological.• Adrenaline, salbutamol, alcohol, coffeine.

Supra-ventricular Supra-ventricular tachycardiatachycardia
From the atria or SA node:• Sinus tachycardia.• Atrial fibrilation.• Atrial flutter.• Atrial tachycardia.
From the atrio-ventricular node:• Atrioventricular Re-entrant tachycardia.• Atrio-ventricular nodal Re-entrant
tachycardia.

ECG characteristic of Atrial ECG characteristic of Atrial ArrhythmiasArrhythmias
Sinus tachycardia.• P wave have normal morphology.
• Atrial rate 100-200 beats/min.
• Regular ventricular rhythm.
• Atrial tachycardia• Abnormal P wave morphology
• Atrial rate 250-350 beats/min.

Atrial FibrillationAtrial Fibrillation• P waves absent baseline f (fibrillation)
waves.• Atrial rate 350-600 beats/min.• Irregular ventricular rhythm.• Ventricular rate 100-180/min.
• Atrial flutter• Saw toothed flutter F waves• Atrial rate 250-350/min.• Regular rhythm



ECG Characteristics of ECG Characteristics of vventricular Tachycardiaentricular Tachycardia
• Rate is normally 120-300 beats/min.
• Rhythm is almost regular
• A positive QRS in AVR
• Usually right bundle morphology
• QRS is bizarre
• Broad QRS > .14 sec
• Presence of capture or infusion beats













Broad Complex TachycardiaBroad Complex TachycardiaVentricular.Regular:• Monomorphic V.T.
• Fasicular tachycardia.
• Rt. Ventricular outflow tract tachycardia.
Irregular:• Torsades de-points tachycardia
• Polymorphic V.T.

Broad Complex Broad Complex TachycardiaTachycardia
Supra-ventricular:
• Bundle branch block with aberrant conduction.
• Atrial tachycardia with pre-excitation.

ECG in WPW ECG in WPW SyndromeSyndrome
•Short PR interval
•Delta wave
•Wide initial QRS

Classification of Wolff Parkinson Classification of Wolff Parkinson “white syndrome”“white syndrome”
Type A (dominant R in V1).Maybe confused with.• Rt. Bundle branch block.• Rt. Ventricular hypertrophy.• Posterior myocardial infarction.
Type B (negative QRS in V1)Maybe confused with.• Left bundle branch block.• Anterior myocardial infarction.










CONCLUSIONCONCLUSION• Cardiac arrhythmias due to coronary artery
disease is the most frequent cause of death and disability all over the world and in the Kingdom of Saudi Arabia indeed.
• Atrial fibrillation is the most common sustained rhythm abnormality encountered at primary to tertiary care levels, is the main precipitant of heart failure syndrome. And is one of the commonest cause of thrombo-embolic Stroke.

• Prompt diagnosis is possible only if precise history is taken along with thorough physical examination and off course concrete investigations too.
• Management of arrhythmias includes various factors, however it needs to be individualized, from low cost digoxin to highly expensive automatic implantable cardio-verter and defibrillator.

GoalsGoals• Symptoms relief• Prevention of tachycardia induced
LV dysfunction• Improved exercise capacity• Improved quality of life• Reduction in embolic risk• Improved survival

Management of Cardiac Management of Cardiac ArrhythmiasArrhythmias “Options”“Options”
• Medical
• Surgical correction
• Radio frequency ablation
• Pacemaker
• Automatic implantable
Cardioverter / defibrillator

Management of Atrial ArrhythmiasManagement of Atrial Arrhythmias• Paroxysmal Atrial Atrial Fibrillation
Tachycardia “Ask” - new onset / chronic
- Re-assurance - possible cause- Carotid massage - haemodynamic
stability- Valsalva maneuver - Heart / function- Ice chewing- Monitor the rhythm Successful – OK
unsuccessfull _ Narrow QRS- I/V Verapamil 5mg.

Management of Cardiac Management of Cardiac ArrhythmiasArrhythmias
• Depend upon AgeSymptomsOrganic heart diseaseNon cardiac pathologyHaemodynamic stabilityLab resultsTechnological observation

Most common arrhythmias, prevalence
is 1%-1.5% increase with age 10% over 70 years of age.
Atrial Fibrillation
Paroxysmal Persistent Permanent

• Paroxysmal Atrial FibrillationIf the current episode has been present for less than 7 days and there is
history of 1 or more episode of self terminating.
• Recent Onset Atrial FibrillationWhen the current symptomatic episode
is the first by history and its duration is longer than 48 hours and less than 7 days.
• Chronic Atrial FibrillationIf the current episode has lasted for
seven or more days (≥7 days).

Causes of Atrial FibrillationCauses of Atrial Fibrillation• Ischaemic heart disease.• Hypertensive heart disease.• Rheumatic heart disease.• Thyrotoxicosis.• Alcohol misuse (acute or chronic).• Sick sinus syndrome.• Post cardiac surgery.• Chronic pulmonary disease.• Idiopathic (lone).

Atrial FibrillationAtrial FibrillationHemodynamically Stable/unstable
• Acute Infarction• Pulmonary edema Referral• Chronic course• Known precipitating cause• Drug non compliance• No Digoxin before – digitalize• Uncontrolled rate, add β block / Verapamil• If large heart Amiodarone• Control hypertension and diabetes

Atrial FibrillationAtrial Fibrillation• Hemodynamically Stable• Rate controlled / increased• Chronic course• Known etiology• Drug non compliance• Drug adjustment / Addition

Ventricular TachycardiaVentricular TachycardiaIt is defined as three or more ventricular
extrasystoles in succession at rate of > 120/min. It may be self terminating or “sustained” if it last longer than 30 seconds. It could be monomorphic (commonest) or polymorphic.
Monomorphic VT usually occurs after myocardial infarction and is a sign of extensive myocardial damage.

Ventricular ArrhythmiasVentricular ArrhythmiasMiddle Age / Elderly• Asymptomatic/Atypical symptoms• Positive risk factors• Positive family history of sudden death• Normal ECG• Normal echocardiogram• Stress test positive for myocardial
ischaemia and arrhythmias
• Early re-vascularization

Management of ventricular Management of ventricular ArrhythmiasArrhythmias
• Young age• Asymptomatic ectopics• No structural heart disease• No family history sudden death
Reassurance

Ventricular ArrhythmiasVentricular Arrhythmias• Symptomatic (syncope, angina, heart failure).• Sustained / unsustained VT rapid / slow• Nitrates, β blockers, K, Mg supplement,
xylocaine.• ECG + X-ray chest (PA/ lat.)• Echocardiogram• Structural heart disease (congenital,
acquired)• Depressed /preserved systolic function• Above 40 years cardiac cath & coronary
angiogram.

-Valve replacement with or without Coronary Artery by pass Surgery”
- Pacemaker implantation
- Automatic implantable cardioverter defibrilator

Cardiac Arrhythmias Cardiac Arrhythmias and Pregnancyand Pregnancy
• Paroxysmal Atrial tachycardia• Atrial fibrillation (RHD)Rapid rate
Hypotension
Heart failureCardioversion
(followed by β blockers, Verapamil

Cardiac Arrhythmias and Cardiac Arrhythmias and PregnancyPregnancy
Rapid rate
Normotension
No heart failure• Reassurance• Carotid massage• Valsalva• Β blockers/Verapamil/Digitalization• Look for etiology/precipitating factors

Causes of Re-admission in Causes of Re-admission in Patients with arrhythmiasPatients with arrhythmias
• Myocardial ischaemia
• Infections
• Poor compliance
• Inadequate drug treatment
• Iatrogenic factors
• Inadequate discharge planning
• Poor social/family support

Orally Available Anti-Arrhythmic Orally Available Anti-Arrhythmic DrugsDrugs
Class IIa: Quinidine, Procainamide, Disopyramide
Ib: Moricizine, Mexiletine
Ic: Propafenone, Flecainide, Cibenzoline
Class II: β-adrenergic receptor antagonist
Class III: Amiodarone, Sotalol, Dofetilide
Class IV: Verapamil, Diltiazem

Antiarrhythmic TherapyAntiarrhythmic TherapyAntiarrhythmic drug therapy is frequently
very frustrating for both the patient and physician. The recommended approach to therapy is to begin with relatively low dosage i.e. lowest dosage with reasonably chance of producing a favourable response and titrating the dose upward as needed. Dose titration should be guided by clinical response and drug level at appropriate time.

Selection of Initial DoseSelection of Initial Dose• The success or failure of drug depends in part
on the selection of drug, too low an initial dosage can prolong the patient’s risk of arrhythmia recurrence and increase the duration of the patient’s hospitalization and ultimate increase cost of treatment.
• Too high a dose can put the patient at risk of cardiac and noncardiac toxicity of drugs. Therefore, individualization of treatment is necessary to optimize the chances of achieving a satisfactory result in treatment.

Drugs MonitoringDrugs Monitoring
• Digoxin (K. level, renal functions, toxicity)
• B-blockers/ Ca antagonists• Amiodarone, (Thyroid, lungs,
eyes, liver)• Warfarine (PT, INR)

Electronic DevicesElectronic DevicesA. Immediate
–Cardioversion
–Defibrillation
–Temporary pacemaker
B. Long term– Permanent pacemaker
– Implantable cardioverted / defibrillator

Risk to Benefit Ratio of Risk to Benefit Ratio of DrugsDrugs
• Benefits– Symptom
reduction• Haemodynamic• Nausance
– Sudden cardiac death
RisksRisksCardiacCardiac
ProarrhythmiaProarrhythmia
Negative Negative ionotrophyionotrophy
Non-cardiacNon-cardiac
Adverse effectsAdverse effects
Organ toxicityOrgan toxicity