Non invasive evaluation of arrhythmias
-
Upload
sunil-reddy-d -
Category
Health & Medicine
-
view
382 -
download
0
Transcript of Non invasive evaluation of arrhythmias

NON INVASIVE EVALUATION OF ARRHYTHMIAS - I
Dr D SUNIL REDDY

THE EVALUATION …
• There is a constant clinical interest for non-invasive identification of patients at risk of fatal arrhythmias.
• Variety of methods have been developed for this purpose.
• Most of these tests have a good negative predictive value with a lesser positive predictive accuracy .

METHODS
1. Electrocardiography2. Ambulatory electrocardiography ( HOLTER )3. Event recorder4. Head up tilt table test5. Exercise testing6. Signal-Averaged Electrocardiography7. Spectral analysis (TWA)8. Imaging etc

ELECTROCARDIOGRAPHY• An ECG taken during the episode of arrhythmia may be
diagnostic in itself , obviating the need for further diagnostic testing
• An ECG involves measuring electric potentials from very few points on the body surface far away from the heart.
• These measurements lack sensitivity (may fail to detect abnormal activity) and specificity (may fail to accurately classify the arrhythmia or determine its location)

SOME ECG ABNORMALITIES IN RESTING RHYTHM THAT SUGGEST ARRHYTHMIA POTENTIAL ( V1 LEAD )

HOLTER MONITORING1. Ambulatory ( Holter ) electrocardiography ( ECG ) is a
widely used noninvasive test to evaluate cardiac rhythm abnormalities
2. It has also been used for assessing pacemaker and ICD function, ischemia, and heart rate variability.
3. The clinical utility of the ambulatory ECG recording lies in its ability to continuously examine the patient's cardiac rhythm over an extended period of time during normal routine activity, including any physical and psychological changes.

• Ambulatory ECG recorders may be of two types
• The ones that use magnetic tape recording and those that use electronic storage system.The analytical system is the same in both the types.
• The conventional 3 channel Holter recorder is a small, battery operated, electromagnetic tape recorder that records 3 channels of electrocardiographic data on cassette or micro-cassette magnetic tape.
• More recent developments of digital technology have led to the ambulatory ECG disk recorder with 200MB of storage

RATIONALE OF HOLTER• The electrical genesis of cardiac arrhythmias
commonly requires three important components:1. Cardiac substrate – structural abnormality2. Electrical triggers – PVC s , NSVT , Bradycardia3. Physiologic or pathophysiologic modulating factors
which may alter the stability of the cardiac substrate or the frequency of the triggers.
• These modulating factors are usually transient and often brief, and include ischemia, electrolyte imbalance, pH changes, changes in ANS tone and drugs.


ELECTRODE PLACEMENT
E (Brown) Level of 5th intercostal space, midsternum
A (Black) Same level as E and I , LEFT MAL
S (Red) Top of sternum (manubrium)
I (White) Same level as E and A , RIGHT MAL
Ground (Green)
Center of sternum or any convenient location

HOLTER LEAD PLACEMENT

CHANNEL DESCRIPTIONChannel 1 E(+) to S(-) Similar to MC V1
Anterior view of the heart
Channel 2 A(+) to S(-) Similar to MC V6 Lateral view of the heart Useful for ST measurements
Channel 3 A (+) to I(-) Similar to inferior lead AVF Suitable for ST measurements

CLASS I INDICATION1. Patients with unexplained syncope, near-syncope, or
episodic dizziness in whom the cause is not obvious
2. Patients with unexplained recurrent palpitation
3. To assess antiarrhythmic drug response in individuals in whom baseline frequency of arrhythmia has been characterized as reproducible and of sufficient frequency to permit analysis
• To detect proarrhythmic responses to antiarrhythmic therapy in patients at high risk ( CLASS II a )

CLASS III INDICATION1. Patients in whom cause have been identified by
history, physical examination, or laboratory tests2. Pts with CVA , without other evidence of arrhythmia3. Patients who have sustained myocardial contusion4. Systemic hypertensive patients with LV hypertrophy5. Post-MI patients with normal LV function6. Preoperative evaluation of patients for noncardiac Sx7. Patients with sleep apnea or valvular heart disease8. Diabetic subjects to evaluate for diabetic neuropathy9. Patients with rhythm disturbances that preclude HRV
analysis (e.g., atrial fibrillation)

1. If arrhythmic events are sufficiently frequent then a 24 hour Holter is most useful.
2. If the events are episodic and not frequent, a Trans telephonic event recorder is better suited for recording the rhythm.
3. Some symptoms are so fleeting that they do not permit patient to apply electrodes / there is insufficient time to capture the arrhythmia. In those instances, the continuous loop trans telephonic recorder is indicated.
4. In patients whose symptoms include syncope the use of implantable loop event recorder is indicated.

IMPLANTABLE LOOP RECORDER
• The implantable loop recorder or insertable loop recorder (ILR) is a subcutaneous monitoring device for the detection of cardiac arrhythmias
• Such a device is typically implanted in the left pectoral region and stores events when the device is activated automatically according to programmed criteria or manually with magnet application

• This device can be useful in the evaluation of palpitations or syncope of undetermined etiology, particularly when symptoms are infrequent (eg, less than once per month)
• In such patients, conventional noninvasive testing
is often negative or inconclusive
• Among patients with neurocardiogenic syncope, an ILR may more accurately establish a causative relationship between bradyarrhythmias and syncope than provocative tests (eg, upright tilt table testing )

PARAMETERS ANALYSED BY HOLTERHEART RATE DATA TOTAL , MIN , AVG , MAX HR
HEART RATE VARIABILITY ASDNN , SDANN 5 ,SDNN , RMSSD
QT ANALYSIS QT AND QTC ( MIN, AVG, MAX )
ST EPISODE ANALYSIS ST LEVEL ( MIN, MAX )
PACER ANALYSIS SINUS, PACED, AP , VP
VENTRICULAR ECTOPY TOTAL , VT RUNS ,TRIPLETS , COUPLETS, BI / TRIGEMINY
SUPRAVENTRICULAR ECTOPY
TOTAL , ATRIAL RUNS , BI / TRIGEMINY, LONGEST RR
ATRIAL FIBRILLATION BEATS,DURATION AND NO. OF EVENTS

HEART RATE VARIABILTY
• The most commonly used measures of HRV are – ASDNN, the standard deviation of all normal to-
normal RR intervals – SDANN 5, the standard deviation of all five-
minute average RR intervals– pNN50, the proportion of beats varying by more
than 50 milliseconds from the preceding QRS and – rMSSD, the square root of the squares of successive
differences between the RR intervals

• During Holter monitoring 1. Sinus bradycardia with heart rates of 35 to 40 bpm
2. Sinus arrhythmia with pauses exceeding 3 seconds
3. Sinoatrial exit block
4. Type I (Wenckebach) 2o AV block (often during sleep)
5. Wandering atrial pacemaker
6. Junctional escape complexes and
7. Premature atrial complexes (PACs) and PVCs can be observed and are not necessarily abnormal

EVALUATION OF THE PATIENT WITH UNEXPLAINED SYNCOPE
• Ambulatory monitoring, in conjunction with clinical and electrocardiographic findings, can be a useful component of the evaluation of the patient with unexplained syncope.
• Ambulatory monitoring can also be used to determine which patients with unexplained syncope will benefit from electrophysiologic studies .

ELECTROCARDIOGRAPHIC MONITORING FOR SYNCOPEIndications CL LOEECG monitoring is indicated in patients who have clinical or ECG features suggesting arrhythmic syncope
I B
• Immediate in-hospital monitoring (in bed or telemetric) is indicated in high risk patients
I C
• Holter monitoring is indicated in patients who have very frequent syncope or pre-syncope (≥one per week)
I B
• ILR is indicated in:- An early phase of evaluation in patients with recurrent syncope of uncertain origin, absence of high risk criteria, and a high likelihood of recurrence within battery longevity of the device
I B
- High risk patients in whom a comprehensive evaluation did not demonstrate a cause of syncope or lead to a specific treatment
I B
• ILR should be considered to assess the contribution of bradycardia before embarking on cardiac pacing in patients with suspected or certain reflex syncope presenting with frequent or traumatic syncopal episodes
IIa B
• External loop recorders should be considered in patients who have an inter-symptom interval ≤four weeks
IIa B

1. Bachinsky et al assessed the importance of six clinical predictors in 141 patients with unexplained syncope who were referred for EPS
• The following findings were noted:– Organic heart disease and NSVT were highly sensitive
markers for the presence of serious ventricular tachyarrhythmias at EPS (sensitivity 100%).
– Sinus bradycardia, first-degree heart block, or BBB by ECG were sensitive for bradyarrhythmic outcomes (sensitivity 79 percent).
2. Pts without these clinical predictors were almost no risk for a serious ventricular arrhythmia, at only very slight risk of a bradyarrhythmia, and therefore unlikely to benefit from EPS
@ Bachinsky WB, Linzer M, Weld L, Estes NA 3rd. Usefulness of clinical characteristics in predicting the outcome of EP studies in unexplained syncope. Am J Cardiol 1992; 69:1044.

CORONARY HEART DISEASE• The Coronary Drug Project @ and a number of other
trials called attention to the prognostic value of frequent and complex ventricular arrhythmias in identifying post myocardial infarction patients at increased risk of death, including sudden death
• Men with complex ventricular arrhythmia had – a two-fold increased risk of death from all causes– a three-fold increased risk of sudden death.
@ Prognostic importance of premature beats following myocardial infarction. Experience in the coronary drug project. JAMA 1983; 223:1116

• Men with ventricular tachycardia had a mortality that was four to five times greater than men without ventricular arrhythmias
• Ventricular arrhythmias had an independent prognostic risk that was additive to the increased risk of an adverse outcome associated with decreased left ventricular function
• Ambulatory ECG studies in postmyocardial infarction patients have also shown that the absence of heart rate variability, as measured by the standard deviation of the RR intervals in sinus rhythm, was a powerful predictor of prognosis, independent of ventricular arrhythmias or left ventricular function

CARDIOMYOPATHY• Ambulatory electrocardiography in patients with
hypertrophic cardiomyopathy has found that approximately two-thirds of patients have frequent and complex ventricular arrhythmias.
• Ventricular tachycardia is present in approximately 25 percent of such patients, and predicts the subsequent occurrence of sudden death
@ Maron BJ, Savage DD, Wolfson JK, Epstein SE. Prognostic significance of 24 hour ambulatory electrocardiographic monitoring in patients with hypertrophic cardiomyopathy: a prospective study. Am J Cardiol 1981; 48:252.

• Complex and frequent ventricular arrhythmias are also detected by ambulatory ECG in 80 to 90 percent of patients with ischemic or nonischemic dilated cardiomyopathy
• The presence of repetitive ventricular arrhythmias is an independent predictor of sudden death in ischemic or nonischemic dilated cardiomyopathy independent of hemodynamic or neuroendocrine variables.
@ Holmes J, Kubo SH, Cody RJ, Kligfield P. Arrhythmias in ischemic and nonischemic dilated cardiomyopathy: prediction of mortality by ambulatory electrocardiography. Am J Cardiol 2002; 55:146

APPARENTLY HEALTHY SUBJECTS• Ventricular arrhythmias are found in 40 to 75 % of
normal persons assessed by 24 to 48 hours of continuous ambulatory electrocardiography
• Furthermore, frequent and complex forms have been found in 1 to 4 percent of the general population .
• The incidence and frequency of ventricular ectopy increase with age but these findings have no impact on long term prognosis in apparently healthy subjects.
• This favorable outlook is true even in the presence of asymptomatic coronary disease.
@ Bjerregaard P. Premature beats in healthy subjects 40-79 years of age. Eur Heart J 1999; 3:493.

ANTIARRHYTHMIC DRUG THERAPY• The variability of ventricular arrhythmia appears to be time
dependent, and more prominent in patients with low-density ventricular arrhythmias, coronary disease, or frequent runs of ventricular tachycardia
• The 24 to 48 hour ambulatory ECG examination is the
mainstay of evaluations used in studies examining suppression of asymptomatic arrhythmias.
• The criteria that demonstrate antiarrhythmic efficacy are
suppression by 70 to 90 percent of mean frequency of total ventricular ectopy, and total elimination of all repetitive forms.

• Resuscitated SCD pts have a high recurrence rate of malignant ventricular arrhythmias, and a decreased long-term survival when they are untreated or are treated empirically .
• Antiarrhythmic therapy that abolishes repetitive ventricular activity, as assessed by ambulatory ECG (in conjunction with exercise testing), predicts long-term survival in such patients
• Transtelephonic monitoring has also been used to evaluate antiarrhythmic therapy and has been extended to provide surveillance of specific high-risk subgroups

ESVEM trial ( NEJM 1993)• EP Study versus ECG Monitoring (ESVEM) Trial results
were as follows 1. Ambulatory ECG testing resulted in a greater no. of pts
for whom a drug was predicted to be effective, and it took less time and was less costly.
2. After a six year follow-up, the predictive accuracy of ambulatory ECG was equivalent to EPS; total, cardiac and sudden death mortalities were equivalent, and any form of arrhythmia recurrence was identical.
3. These results confirmed findings that noninvasive methods of ambulatory ECG and exercise testing were as effective as (and more cost-effective than) other methods for managing pts with ventricular arrhythmias.

EVALUATION OF PACEMAKERS• Ambulatory electrocardiography has proved to be valuable for
assessing pacemaker function during long-term FU .• The use of ambulatory electrocardiography has increased the
diagnosis of pacemaker malfunction by examining the patient over 24 hours or more during daily activities
• Furthermore, enhanced detection of pacemaker dysfunction by ambulatory electrocardiography in the early postimplant period has allowed therapeutic intervention prior to discharge @
• Holter technology is also an important aid in the visual interpretation of electrocardiograms from dual chamber and biventricular pacemakers.
@ Janosik DL, Redd RM, Buckingham TA, et al. Utility of ambulatory electrocardiography in detecting pacemaker dysfunction in the early postimplantation period. Am J Cardiol 2000, 60:1030.

THANK YOU





CONDUCTION DELAY CONDUCTION BLOCKNO CONDUCTION DELAY

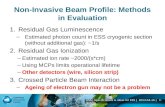
• The main approaches for non-invasive arrhythmia evaluation can be divided into three categories
1. The function of the autonomic nervous system is studied in heart rate variation analysis
2. The activation discontinuities during the ventricular depolarization – studied in late potentials and in spectral turbulence analysis
3. The heterogeneity during the repolarization of the ventricles is studied in QT dispersion analysis

• transient VT on Ambulatory ECGmonitoring is the single best
• marker of high risk for sudden deathin patients with HCM.
• 4. The use of Ambulatory ECGmonitoring to guideselection
• of antiarrhythmic drugs to preventrecurrent ventricular
• tachycardia or cardiac arrest remainscontroversial

FRAGMENTATION ANALYSIS
• The propensity for ventricular tachycardias can also be sought by detecting intra-QRS changes.
• The fragmentation of each QRS complex is characterized by the number of the extrema (M) and the product of M and the sum of scaled amplitude differences between the neighboring extrema, called fragmentation Index
• Intra QRS changes can also be analyzed by analyzing the discontinuities in frequency content of the signal which are analyzed.

REPOLARIZATION ANALYSIS
• Heterogeneity of the ventricular repolarization is also an indicator of vulnerability for malignant arrhythmias.
• The heterogeneity is studied by analyzing– the dispersion of the time from the onset of the Q
wave to the apex or the end of the T-wave (QT time) and
– the duration of the terminal part of the T-wave ( T apex – T end)

• If the patient is being evaluated for syncope or presyncope, extending the period of monitoring can increase the incidence of symptomatic events to approximately 50 percent at three days and 75 percent at 5 to 21 days (mean 9 days)