Glycemic control and excess mortality in type 1 diabetes mellitis
Glycemic Management in Type 2 Diabetes
description
Transcript of Glycemic Management in Type 2 Diabetes

Glycemic Management in Type 2 Diabetes
1

AACE Comprehensive Care Plan
Disease management from a multidisciplinary team
Antihyperglycemic pharmacotherapy
Comprehensive diabetes self-education for the
patient
Therapeutic lifestyle change
Comprehensive Care Plan
2
Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.

Glycemic Management in Type 2 Diabetes
Therapeutic Lifestyle Change
3

Components of Therapeutic Lifestyle Change
• Healthful eating• Sufficient physical activity• Sufficient sleep• Avoidance of tobacco products• Limited alcohol consumption• Stress reduction
4
Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.

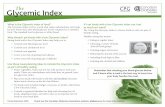
AACE Healthful Eating Recommendations
5
Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.
Topic RecommendationGeneral eating habits
Regular meals and snacks; avoid fasting to lose weight Plant-based diet (high in fiber, low calories, low glycemic index, high in phytochemicals/antioxidants) Understand Nutrition Facts Label information Incorporate beliefs and culture into discussions Informal physician-patient discussions Use mild cooking techniques instead of high-heat cooking
Carbohydrate Understand health effects of the 3 types of carbohydrates: sugars, starch, and fiber Target 7-10 servings per day of healthful carbohydrates (fresh fruits and vegetables, pulses, whole
grains) Lower-glycemic index foods may facilitate glycemic control:* multigrain bread, pumpernickel bread,
whole oats, legumes, apple, lentils, chickpeas, mango, yams, brown riceFat Eat healthful fats: low-mercury/low-contaminant-containing nuts, avocado, certain plant oils, fish
Limit saturated fats (butter, fatty red meats, tropical plant oils, fast foods) and trans fats Use no- or low-fat dairy products
Protein Consume protein from foods low in saturated fats (fish, egg whites, beans) Avoid or limit processed meats
Micronutrients Routine supplementation not necessary except for patients at risk of insufficiency or deficiency Chromium; vanadium; magnesium; vitamins A, C, and E; and CoQ10 not recommended for glycemic
control*Insufficient evidence to support a formal recommendation to educate patients that sugars have both positive and negative health effects

AACE Medical Nutritional Therapy Recommendations
• Consistency in day-to-day carbohydrate intake• Adjusting insulin doses to match carbohydrate intake
(eg, use of carbohydrate counting)• Limitation of sucrose-containing or high-glycemic index
foods• Adequate protein intake• “Heart-healthy” diets• Weight management• Exercise• Increased glucose monitoring
6
Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.

• ≥150 minutes per week of moderate-intensity exercise – Flexibility and strength
training– Aerobic exercise (eg, brisk
walking)• Start slowly and build up
gradually
• Evaluate for contraindications and/or limitations to increased physical activity before patient begins or intensifies exercise program
• Develop exercise recommendations according to individual goals and limitations
AACE Physical Activity Recommendations
7
Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.

Glycemic Management in Type 2 Diabetes
Antihyperglycemic Therapy
8

Noninsulin Agents Available for Treatment of Type 2 Diabetes
Class Primary Mechanism of Action Agent Available as-Glucosidase inhibitors
Delay carbohydrate absorption from intestine
Acarbose Precose or genericMiglitol Glyset
Amylin analogue Decrease glucagon secretion Slow gastric emptying Increase satiety
Pramlintide Symlin
Biguanide Decrease HGP Increase glucose uptake in
muscleMetformin Glucophage or generic
Bile acid sequestrant
Decrease HGP? Increase incretin levels?
Colesevelam WelChol
DPP-4 inhibitors Increase glucose-dependent
insulin secretion Decrease glucagon secretion
Alogliptin NesinaLinagliptin TradjentaSaxagliptin OnglyzaSitagliptin Januvia
Dopamine-2 agonist
Activates dopaminergic receptors
Bromocriptine Cycloset
9HGP, hepatic glucose production.
Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.

Noninsulin Agents Available for Treatment of Type 2 Diabetes
Class Primary Mechanism of Action Agent Available as
Glinides Increase insulin secretionNateglinide Starlix or genericRepaglinide Prandin
GLP-1 receptor agonists
Increase glucose-dependent insulin secretion
Decrease glucagon secretion Slow gastric emptying Increase satiety
Exenatide Byetta
Exenatide XR Bydureon
Liraglutide Victoza
SGLT2 inhibitor Increase urinary excretion of
glucoseCanagliflozin Invokana
Sulfonylureas Increase insulin secretion
Glimepiride Amaryl or genericGlipizide Glucotrol or generic
Glyburide Diaeta, Glynase, Micronase, or generic
Thiazolidinediones Increase glucose uptake in
muscle and fat Decrease HGP
Pioglitazone Actos
Rosiglitazone* Avandia
*Use restricted due to increased risk of myocardial infarction (MI)10
HGP, hepatic glucose production.Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.

Insulins Available for the Treatment of Type 2 Diabetes
Class Primary Mechanism of Action Agent Available as
Basal
Increase glucose uptake Decrease HGP
Detemir LevemirGlargine Lantus
Neutral protamine Hagedorn (NPH) Generic
Prandial
Aspart NovoLogGlulisine ApidraLispro HumalogRegular human Humulin, generic
PremixedBiphasic aspart NovoLog MixBiphasic lispro Humalog Mix
11
Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.

Pharmacokinetics of Insulin
12
Agent Onset (h) Peak (h) Duration (h) Considerations
BasalNPH 2-4 4-10 10-16 Greater risk of nocturnal
hypoglycemia compared to insulin analogues
Glargine ~1-4 No pronounced peak*
Up to 24 hours†
Less nocturnal hypoglycemia compared to NPHDetemir
PrandialRegular ~0.5-1 ~2-3 Up to 8 Must be injected 30-45 min
before a meal Injection with or after a meal
could increase risk for hypoglycemia
Aspart <0.5 ~0.5-2.5 ~3-5 Can be injected 0-15 min before a meal
Less risk of postprandial hypoglycemia compared to regular insulin
Glulisine
Lispro
* Exhibits a peak at higher dosages.† Dose-dependent.
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].

Combination Agents Available for the Treatment of Type 2 Diabetes
Class Added Agent Available as
Metformin + DPP-4 inhibitor
Alogliptin Kazano
Linagliptin Jentadueto
Sitagliptin Janumet
Metformin + glinide Repaglinide Prandimet
Metformin + sulfonylureaGlipizide Metaglip and generic
Glyburide Glucovance and generic
Metformin + thiazolidinedionePioglitazone ACTOplus Met
Rosiglitazone* Avandamet
Thiazolidinedione + DPP-4 inhibitor Pioglitazone + alogliptin Oseni
Thiazolidinedione + sulfonylureaPioglitazone Duetact
Rosiglitazone* Avandaryl
*Use restricted due to increased risk of myocardial infarction (MI)
13

Principles of the AACE/ACE T2DM Algorithm
• Ongoing lifestyle optimization essential– Requires support from full diabetes team
• Set A1C target based on individual patient characteristics and risk– ≤6.5% optimal if it can be achieved safely– Targets may change over time
• FPG and PPG regularly monitored by patient with SMBG
Garber AJ, et al. Endocr Pract. 2013;19:327-336.
Glucose Targets
14

• Choose medications based on individual patient attributes– Minimize risk of hypoglycemia– Minimize risk of weight gain– Combine agents with
complimentary mechanisms of action for optimal glycemic control
• Prioritize safety and efficacy over medication cost– Medication cost small portion of
total cost of diabetes– Risk of adverse effects
considered part of “cost” of medication
• Evaluate treatment efficacy every 3 months– A1C, FPG, and PPG data– Hypoglycemia– Other adverse events (weight
gain; fluid retention; hepatic, renal, or cardiac disease)
– Comorbidities and complications
– Concomitant drugs– Psychosocial factors affecting
patient care
Principles of the AACE/ACE T2DM Algorithm
15
Garber AJ, et al. Endocr Pract. 2013;19:327-336.
Antihyperglycemic Medications

16

17

18

19

Common Principles in AACE/ACE and ADA/EASD T2DM Treatment Algorithms
• Individualize glycemic goals based on patient characteristics• Promptly intensify antihyperglycemic therapy to maintain
blood glucose at individual targets– Combination therapy necessary for most patients– Base choice of agent(s) on individual patient medical history,
behaviors and risk factors, ethno-cultural background, and environment
• Insulin eventually necessary for many patients• SMBG vital for day-to-day management of blood sugar
– All patients using insulin– Many patients not using insulin
20Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.
Garber AJ, et al. Endocr Pract. 2013;19:327-336.

21
ADA/EASD T2DM Treatment Algorithm
Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.

ADA/EASD T2DM Treatment Algorithm: Sequential Insulin Strategies
Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379.
22

Early Insulin Use in Type 2 Diabetes
23
ORIGIN Trial Investigators. N Engl J Med. 2012;367:319-328.
Outcome Reduction With an Initial Glargine InterventionCV risk factors + prediabetes or T2DM (N=12,537)

Pipeline Classes and Agents (2013)
ClassPhase of Development Agents Description
Dual peroxisome proliferator activated receptor - (PPAR-) agonistPhase 3
AleglitazarImprove insulin sensitivity in the periphery as well as lipid profilesApproved agents may reduce both cardiovascular risks and potential for diabetes complications
Short-acting GLP-1 receptor agonist Lixisenatide Human-derived molecule with effects similar to exenatide
Long-acting GLP-1 receptor agonistsPhase 3
AlbiglutideTaspoglutide
Effects probably similar to currently available GLP-1 receptor agonistsLonger duration of action will permit longer intervals between injections
Insulin Phase 3
Degludec Ultra-long-acting basal insulin (half-life ~25 hours) with low within-subject variability and potential for reduced incidence of hypoglycemia
DegludecPlus Premixed insulin containing degludec plus aspart, providing both fasting and postprandial glucose control
SalicylatesPhase 3
Salsalate Generically available anti-inflammatory medication currently approved for treatment of arthritis; inhibits activity of NF-B, an inflammatory factor
Sodium-dependent glucose cotransporter 2 (SGLT-2) inhibitorsPhase 3
DapagliflozinEmpagliflozinTofogliflozin
Act in the kidneyReduce hyperglycemia by inhibiting glucose reabsorption into the bloodstream from the renal filtrate, increasing urinary excretion of glucose
11-Hydroxysteroid dehydrogenase type 1 (11HSD-1) inhibitorsPhase 2
INCB13739RG4929
Inhibit 11HSD-1 mediated conversion of low-activity cortisone to cortisol, which is primarily produced in the liver and adipose tissueMay lessen stress-induced obesity, improve insulin sensitivity, enhance insulin-secretory responsiveness, and improve glucose tolerance in patients with metabolic syndrome and/or type 2 diabetes
24Bakris GL, et al. Kidney Int. 2009;75:1272-1277; Calado J, et al. Kidney Int Suppl. 2011:S7-S13;
Garber AJ. Expert Opin Investig Drugs. 2012;21:45-57; Goldfine AB, et al. Ann Intern Med. 2010;152:346-357;King A. J Fam Pract. 2012;61:S28-S31; Tahrani AA, et al. Lancet. 2011;378:182-197;
Tahrani AA, et al. Lancet. 2012;379:1465-1467.

Glycemic Management in Type 2 Diabetes
Technology for Type 2 Diabetes Management
25

Noninsulin Users• Introduce at diagnosis• Personalize frequency of
testing• Use SMBG results to inform
decisions about whether to target FPG or PPG for any individual patient
Insulin Users• All patients using insulin should
test glucose– ≥2 times daily– Before any injection of insulin
• More frequent SMBG (after meals or in the middle of the night) may be required– Frequent hypoglycemia– Not at A1C target
SMBG in Type 2 Diabetes: AACE/ACE Recommendations
26
Testing positively affects glycemia in T2DM when the results are used to:• Modify behavior• Modify pharmacologic treatment
SMBG, self-monitoring of blood glucose.Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.

Active control group (n=227)Structured testing group (n=256)
7.2Baseline
7.4
7.6
7.8
8.0
8.2
8.4
8.6
8.8
9.0
M1 M3 M6 M9 M12
-0.3%(P=0.04)
Adj
uste
d M
ean
A1C
(%)
SMBG in Noninsulin Using Patients With T2DM
ACG, active cotnrol group; STG, structured testing group.Polonsky WH, et al. Diabetes Care. 2011;34:262-267.
ACG 8.9%(0.08)
8.7%(0.1)
8.2%(0.1)
7.9%(0.1)
8.0%(0.1)
8.0%(0.1)
STG 8.9%(0.07)
8.5%(0.09)
7.9%(0.09)
7.9%(0.09)
7.6%(0.09)
7.7%(0.09)
27

• Absolutely insulin-deficient• Take 4 or more insulin
injections a day• Assess blood glucose levels 4
or more times daily• Motivated to achieve tighter
glucose control
• Mastery of carbohydrate counting, insulin correction, and adjustment formulas
• Ability to troubleshoot problems related to pump operation and plasma glucose levels
• Stable life situation• Frequent contact with members
of their healthcare team, in particular their pump-supervising physician
CSII in Type 2 Diabetes: Patient Candidates
CSII, continuous subcutaneous insulin infusion.Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53.
28

Glycemic Management in Type 2 Diabetes
Surgical Intervention
29

Surgical Intervention inType 2 Diabetes
30
Schauer PR, et al. N Engl J Med. 2012;366:1567-1576.
MonthsMonths
3.5
2.5
1.5
0.50.0
1.0
2.0
3.0
Baseline 3 6 9 12
Aver
age
no. d
iabe
tes
med
icat
ions
P<0.001
P<0.001
-2
-6
-10-12
-8
-4
0
Baseline 3 6 9 12
B
MI (
kg/m
2 )P<0.001
P<0.001
20
-40
-100
-140-160
-120
-60
-20
-80
0
Baseline 3 6 9 12
F
PG (m
g/dL
)
P=0.02
P<0.001
0.0
1.0
2.0
3.03.5
2.5
1.5
0.5
Baseline 3 6 9 12
A
1C (%
)
P<0.001
P<0.001
Intensive medical therapy Sleeve gastrectomy Roux-en-Y gastric bypass

Glycemic Management in Type 2 Diabetes
Safety Concerns: Hypoglycemia
31

Type 2 Diabetes Pathophysiology: Origins of Hypoglycemia
Cryer PE. Am J Physiol. 1993; 264(2 Pt 1):E149-E155.
Defect
β-cells Increased insulin availability due to use of secretagogues or exogenous insulin
Liver Suppressed hepatic glucose production due to impaired counter-regulatory response
Skeletal muscle Increased glucose uptake due to exercise
α-cells Suppressed glucagon due to impaired counter-regulatory response
Brain Hypoglycemia unawareness
32

Hypoglycemia: Risk FactorsPatient Characteristics
• Older age• Female gender• African American ethnicity• Longer duration of
diabetes• Neuropathy• Renal impairment• Previous hypoglycemia
Behavioral and Treatment Factors• Missed meals• Elevated A1C• Insulin or sulfonylurea
therapy
Miller ME, et al. BMJ. 2010 Jan 8;340:b5444. doi: 10.1136/bmj.b5444.
33

0
1020
304050
6070
8090
100
Blood Glucose (mg/dL)
Decreased insulin secretion
Increased glucagon, epinephrine, ACTH, cortisol, and growth hormone
Palpitation, sweatingDecreased cognition, hungerAberrant behaviorSeizures, coma
Neuronal cell death
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].
Symptoms and Signs with Progressive Hypoglycemia
34

Hypoglycemia: Clinical Consequences
Acute• Symptoms (sweating,
irritability, confusion)• Accidents• Falls
Long-term• Recurrent hypoglycemia
and hypoglycemia unawareness
• Refractory diabetes• Dementia (elderly)• CV events
– Cardiac autonomic neuropathy
– Cardiac ischemia– Fatal arrhythmia– Angina
Cryer PE, et al. Diabetes Care. 2003;26:1902-1912.ADA. Diabetes Care. 2013;36(suppl 1):S11-S66.
Zammit NN, et al. Diabetes Care. 2005;28:2948-2961.
35

Treatment of Hypoglycemia: AACE/ACE Recommendations
Cryer PE, et al. Diabetes Care. 2003;26:1902-1912.
Blood Glucose Level
Classification Typical Signs and Symptoms Treatment
~50-60 Mild hypoglycemia Neurogenic: palpitations, tremor, hunger, sweating, anxiety, paresthesia
Neuroglycopenic: behavioral changes, emotional lability, difficulty thinking, confusion
Consume glucose-containing foods (fruit juice, soft drink, crackers, milk, glucose tablets); avoid foods also containing fat
Repeat glucose intake if SMBG result remains low after 15 minutes
Consume meal or snack after SMBG has returned to normal to avoid recurrence
<50 Moderate hypoglycemia
Severe hypoglycemia
Severe confusion, unconsciousness, seizure, coma, death
Requires help from another individual
Glucagon injection, delivered by family member or other close associate
Victim should be taken to hospital for evaluation and treatment after any severe episode
36

Elements of Hypoglycemia Prevention
Set appropriate glycemic targets for individual patients
More stringent goals: young, newly diagnosed, no comorbidities, no micro- or macrovascular disease, strong and effective self-care skills
Less stringent goals: older, limited life expectancy, history of hypoglycemia, longer disease duration, established comorbidities, established vascular disease, limited self-care skills
Educate patients
Signs and symptoms of hypoglycemia Dietary education for improved glycemic control and appreciation of triggers for
hypoglycemia Avoiding missed or delayed meals Appropriate self-treatment Understanding of hypoglycemia unawareness Importance of reporting hypoglycemia
Use self-monitoring of blood glucose
Patient education: technique and action Observation of patient’s procedure and reaction Patient access to providers for purposes of reporting results and for providing guidance Provider reaction to results increases effectiveness of SMBG
Hold a high index of suspicion for hypoglycemia
Understand patients may not report “typical” symptoms When hypoglycemia is suspected, adjust therapy Consider use of continuous glucose monitoring to detect unrecognized hypoglycemia
Choose appropriate therapy
Use agents with a low risk of hypoglycemia Be aware of additive effects of combination therapies on hypoglycemia risk Recognize that long-term costs of hypoglycemia may offset the cost of using older, less
physiologic medications37
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].

GLP-1 receptor agonists
DPP-4 inhibitors
TZDs
Insulin (basal, basal-plus, premixed)
Sulfonylureas
Metformin
Less Hypoglycemia
MoreHypoglycemia
Initial Treatment Additional Treatment
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].
Hypoglycemia Risk With Antihyperglycemic Agents Added
to Metformin
38

Percentage of Patients Treated in 1 Year
0
1%
2%
3%
4%
5%
6% Mixtures, Rapid-acting, Basal-bolus
Insulin
Basal
Sulfonylureas
DPP-4 inhibitors, GLP-1 receptor agonists, Metformin, TZDs
Meglinitides
Frequency of Severe Hypoglycemia With Antihyperglycemic Agents
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].
39

Increasing rates of hypoglycemia
Most frequent
Prandial and
premixed
Morefrequent Basal +
Lessfrequent
Basal only
Human insulinAnalogue insulinsPremixed (70/30, 75/25)
Basal plus 2-3 prandialBasal plus one prandial
NPHBasal analogues (glargine, detemir) Pipeline basal analogues(degludec, pegylated lispro)
Moghissi E, et al. Endocr Pract. 2013;Feb 20:1-33. [Epub ahead of print].
Relative Rates of Severe Hypoglycemia with Insulin
40

Glycemic Management in Type 2 Diabetes
Safety Concerns: Weight
41

Antidiabetic Agents and Weight
• Risk of additional weight gain must be balanced against the benefits of the agent– Sulfonylureas may negate weight loss benefits of GLP-1 receptor agonists or
metformin– Insulin should not be withheld because of the risk of weight gain
Inzucchi SE, et al. Diabetes Care. 2012;35:1364-1379. Garber AJ, et al. Endocr Pract. 2013;19:327-336.Handelsman Y, et al. Endocr Pract. 2011;17(suppl 2):1-53. Stenlof K, et al. Diabetes Obes Metab 2013;15:372-382.
42
Class Agent(s) Weight EffectAmylin analog Pramlintide ↓Biguanide Metformin ↓GLP-1 receptor agonists Exenatide, exenatide XR, liraglutide ↓SGLT-2 inhibitor Canagliflozin ↓-Glucosidase inhibitors Acarbose, miglitol ↔Bile acid sequestrant Colesevelam ↔DPP-4 inhibitors Alogliptin, linagliptin, saxagliptin, sitagliptin ↔Dopamine-2 agonist Bromocriptine ↔Glinides Nateglinide, repaglinide ↑Sulfonylureas Glimepiride, glipizide, glyburide ↑Insulin Aspart, detemir, glargine, glulisine, lispro, NPH, regular ↑↑Thiazolidinediones Pioglitazone, rosiglitazone ↑↑

Glycemic Management in Type 2 Diabetes
Safety Concerns: Cancer Risk
43

Insulin and Cancer Risk
44
Study Hazard Ratio (95% CI)
Outcome Reduction With an Initial Glargine Intervention (ORIGIN)N=12,537; prospective RCTMedian follow-up: 6.2 years
Any cancer: 1.00 (0.88-1.13); P=0.97Death from cancer: 0.94 (0.77-1.15); P=0.52
Northern European Database StudyN=447,821; observationalMean follow-up:
Glargine users: 3.1 yearsOther insulin users: 3.5 years
Breast cancer (women): 1.12 (0.99-1.27)Prostate cancer (men): 1.11 (1.00-1.24)Colorectal cancer (men and women): 0.86 (0.76-0.98)
Kaiser-Permanente CollaborationN=115,000; observationalMedian follow-up:
Glargine users: 1.2 yearsNPH users: 1.4 years
Breast cancer (women): 1.0 (0.9-1.3)Prostate cancer (men): 0.7 (0.6-0.9)Colorectal cancer (men and women): 1.00 (0.8-1.2)All cancers (men and women): 0.9 (0.9-1.0)
MedAssurant Database StudyN=52,453; observationalMean follow-up:
Glargine users: 1.2 yearsNPH users: 1.1 years
No increased risk for breast cancer
ORIGIN Trial Investigators. N Engl J Med. 2012;367:319-328. Kirkman MS, et al. Presented at the American Diabetes Association 72nd Scientific Sessions. June 11, 2012. Session CT-SY13. Philadelphia, PA.

Glycemic Management in Type 2 Diabetes
Special Populations and Situations
45

Management Considerations for Elderly Patients with
Diabetes
46Bourdel Marchasson I, et al. J Nutr Health Aging. 2009;13:685-691. Handelsman Y, et al. Endocr Pract. 2011;17(suppl
2):1-53. Schwartz AV, et al. Diabetes Care. 2008;31:391-396. Zammitt NN, Frier BM. Diabetes Care. 2005;28:2948-2961.
Increased risk of and from falling
• Impaired vision• Reduced strength and
stamina• Sensitivity to
medication side effects• Frailty• Susceptibility to
hypoglycemia
Hypoglycemia unawareness and
recurrent hypoglycemia
• Impaired counter-regulatory mechanisms
Impaired capacity, understanding, and/or motivation for proper
self-care• Cognitive decline and
dementia• Depression• Impaired vision
Other complicating factors
• Diminished kidney function
• Urinary incontinence• Status of social support
and/or caregiver• Drug-drug interactions
Consider risks before prescribing:
• Sulfonylureas and glinides (hypoglycemia risk)• Thiazolidinediones (fracture risk)• Metformin (risk of lactic acidosis with decreased kidney function)
Consider when establishing treatment goals
• Patient overall health and well-being• Self-care capacities• Social/family support

Risk Considerations for Religious/Cultural Fasting
Risk Category Features
Low
Glycemia well-controlled with antihyperglycemic agent that does not cause hypoglycemia (eg, metformin, thiazolidinedione, DPP-4 inhibitor, GLP-1 receptor agonist)
Otherwise healthyModerate Glycemia well-controlled with glinides
High
Moderate hyperglycemia (A1C 7.5-9.0%), renal insufficiency, cardiovascular complications, and/or other comorbid conditions
Living alone, especially if taking sulfonylureas, insulin, or drugs that affect mentation Elderly, especially with poor health
Very high
History of recurrent hypoglycemia, hypoglycemia unawareness, or episode of severe hypoglycemia within 3 months prior to Ramadan
Poor glycemic control Ketoacidosis or hyperosmotic hyperglycemic coma within 3 months prior to Ramadan Acute illness or chronic dialysis Intense physical labor Pregnancy47
Al-Arouj M, et al. Diabetes Care. 2005;28:2305-2311.
Main Risks of Fasting• Hypoglycemia• Hyperglycemia• Diabetic ketoacidosis• Dehydration and thrombosis

Glycemic Management During Religious/Cultural Fasting
48
Al-Arouj M, et al. Diabetes Care. 2005;28:2305-2311.
• Frequent glucose monitoring—break fast immediately if patient has: – Hypoglycemia
• SMBG <70 mg/dL while taking insulin or sulfonylureas• SMBG <60 mg/dL while on other therapies
– Hyperglycemia: >300 mg/dL• Healthful eating before and after each fasting period
– Complex carbohydrates prior to fast– Avoid ingesting high-carbohydrate, high-fat foods when breaking fast
• Avoid excessive physical activity but maintain normal exercise routines
• Avoid fasting while ill