Facial nerve anatomy 1
-
Upload
shambhunath-mukherjee -
Category
Documents
-
view
467 -
download
4
Transcript of Facial nerve anatomy 1

Dr S N Mukherjee

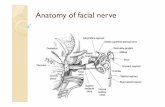
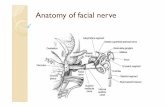
The facial nerve, or cranial nerve (CN) VII, is the nerve of facial expression. The pathways of the facial nerve are variable, and knowledge of the key intratemporaland extratemporal landmarks is essential for accurate physical diagnosis and safe and effective surgical intervention in the head and neck.

The facial nerve is composed of approximately 10,000 neurons, 7,000 of which are myelinated and innervate the nerves of facial expression. Three thousand of the nerve fibers are somatosensory and secretomotor and make up the nervus intermedius. The course of the facial nerve and its central connections can be roughly divided into the segments listed

SupranuclearCerebral cortexNA BrainstemMotor nucleus of facial nerve, superior salivatory
nucleus of tractus solitariusNA Meatal segmentBrainstem to internal auditory canal
(IAC)13-15mm Labyrinthine segmentFundus of IAC to facial hiatus3-4mm Tympanic segmentGeniculate ganglion to pyramidal
eminence8-11mm Mastoid segmentPyramidal process to stylomastoid
foramen10-14mm Extratemporal segmentStylomastoid foramen to pes
anserinus15-20mm

Embryology of facial n. By the third week of gestation, the fascioacoustic
primordium gives rise to CN VII and VIII. During the fourth week, the chorda tympani can be discerned from the main branch. The former courses ventrally into the first branchial arch and terminates near a branch of the trigeminal nerve that eventually becomes the lingual nerve. The main trunk courses into the mesenchyme, approaching the epibranchialplacode.

The geniculate ganglion, nervus intermedius, and greater superficial petrosal nerve are visible by the fifth week. The second branchial arch gives rise to the muscles of facial expression in the seventh and eighth week. To innervate these muscles, the facial nervecourses across the region that eventually becomes the middle ear. By the eleventh week, the facial nerve has arborized extensively. In the newborn, the facial nerve anatomy approximates that of an adult, except for its location in the mastoid, which is more superficial.

Central Connections
Crosby and DeJonge, along with Nelson, have provided 2 of the most complete descriptions oCortex and internal capsule
The voluntary responses of the facial muscles (eg, smiling when taking a photograph) arise from efferent discharge from the motor face area of the cerebral cortex. The motor face area is situated on the precentral and postcentral gyri. The facial motor nerves are represented on the homunculus diagram below with the forehead uppermost and the eyelids, midface, nose, and lips sequentially located more inferiorly.

Discharges from the facial motor area are carried through fascicles of the corticobulbar tract to the internal capsule, then through the upper midbrain to the lower brainstem, where they synapse in the pontine facial nerve nucleus. The pontine facial nervenucleus is divided into an upper and a lower half, bilaterally.

The corticobulbar tracts from the upper face cross and recross en route to the pons; the tracts to the lower face cross only once.
In 1987, Jenny and Saper performed an extensive study of the proximal facial nerve organizations in a primate model and found evidence that in monkeys, upper facial movement is relatively preserved in upper motor neuron injury, because these motor neurons receive relatively little direct cortical input.

In contrast, the lower facial muscles are more severely affected, because their motor neurons depend on significant cortical innervation. The authors believe these observations also explain similar findings in humans.

In their study, Jenny and Saper found that the descending corticofacial fibers in monkeys innervated the lower facial motor nuclear region bilaterally but with contralateral predominance. The upper facial motor nuclear regions received scant direct cortical innervation on either side of the brain.

The deficits observed with unilateral ablation of the corticobulbar fibers reflect the fact that upper facial motor neurons do not receive significant cortical innervations and that lower facial motor neurons contralateral to the lesion, which have functional loss, are dependent on direct contralateral cortical innervation, with the remaining ipsilateral cortical projections being insufficient to drive them.

These findings may explain why a focal lesion in the facial area on 1 side of the motor cortex in humans spares eyelid closure and forehead movement but results in paralysis of the lower face.

Posterior auricularPosterior auricularPulls ear backward
Occipitofrontalis, occipital bellyMoves scalp backward
TemporalAnterior auricularPulls ear forward
Superior auricularRaises ear
Occipitofrontalis, occipital bellyMoves scalp forward
Corrugator superciliiPulls eyebrow medially and downward
ProcerusPulls medial eyebrow downward

Temporal and zygomaticOrbicularis oculiCloses eyelids and contracts skin around eye
Zygomatic and buccalZygomaticus majorElevates corners of mouth BuccalZygomaticus minorElevates upper lip Levator labii superiorisElevates upper lip and midportion nasolabial fold Levator labii superioris alaeque nasiElevates medial nasolabial fold and nasal
ala RisoriusAids smile with lateral pull BuccinatorPulls corner of mouth backward and compresses cheek Levator anguli orisPulls angles of mouth upward and toward midline OrbicularisCloses and compresses lips Nasalis, dilator narisFlares nostrilsNasalis, compressor narisCompresses nostrils

Buccal and marginal mandibularDepressor anguliorisPulls corner of mouth downward
Depressor labii inferiorisPulls lower lip downward
Marginal mandibularMentalisPulls skin of chin upward
CervicalPlatysmaPulls down corners of mouth

Caution is advised in using preservation of forehead function to diagnose a central lesion. Patients may have sparing of forehead function with lesions in the pontine facial nerve nucleus, with selective lesions in the temporal bone, or with an injury to the nerve in its distribution in the face.

An accurate neurologic diagnosis is best made by examining deficits in conjunction with "the company they keep." A cortical lesion that produces a lower facial deficit is usually associated with a motor deficit of the tongue and weakness of the thumb, fingers, or hand on the ipsilateral side.

Nerve fibers influencing emotional facial expression are thought to arise in the thalamus and globuspallidus. Supranuclear pyramidal lesions spare movements of the face initiated as emotional responses and reflexes. With nuclear and infranuclearlesions, loss of involuntary and voluntary facial movement occurs.

The facial nerve nuclei also receive afferent input from other brainstem nuclei. Input from the trigeminal nerve and nucleus form the basis of the trigeminofacial reflexes; eg, the corneal reflex. Input from the acoustic nuclei to the facial nerve nucleus forms part of the stapedial reflex response to loud noises.

Extrapyramidal system
The extrapyramidal system consists of the basal ganglia and the descending motor projections other than the fibers of the pyramidal or corticospinal tracts. This system is associated with spontaneous, emotional, mimetic facial motions. The interplay between the pyramidal and extrapyramidal systems accounts for resting tone and stabilizes the motor responses.

The masked facies associated with Parkinsonism are known to be the result of destruction of the extrapyramidal pathways. The facial dystonia seen in Meige syndrome is thought to be due to basal ganglion disease.

Lower midbrain
A lesion in the lower midbrain above the level of the facial nucleus may cause contralateral paresis of the face and muscles of the extremities, ipsilateral abducens muscle paresis (due to effects on the abducens nerve), and ipsilateral internal strabismus. If the lesion extends far enough laterally to include the emerging facial nerve fibers, a peripheral type of ipsilateral facial paralysis may be apparent.

Pons The facial motor nucleus is located in the lower third of the
pons, beneath the fourth ventricle. The neurons leaving the nucleus pass around the abducens nucleus as they emerge from the brainstem. Involvement of the facial nerve nucleus and VI nerve nucleus are suggestive of a lesion near the fourth ventricle. A lesion near the ventricle at the level of the superior salivatory nucleus may result in a dry eye in addition to a peripheral facial paralysis and abducensparesis.

Cerebellopontine Angle and the Internal Auditory Canal The facial nerve emerges from the brainstem with the nerve of
Wrisberg, ie, the nervus intermedius (see the image below). The nervus intermedius gained its name from its position as it courses across the cerebellopontine angle (CPA) between the facial nerve and the vestibulocochlear nerves (ie, CN VII, CN VIII). The average distance between the point where the nerves exit the brainstem and the place where they enter into the internal auditory canal (IAC) is approximately 15.8 mm. The facial nerve and the nervus intermediuslie above and slightly anterior to CN VIII.

The nervus intermedius conveys (1) afferent taste fibers from the chorda tympani nerve, which come from the anterior two thirds of the tongue; (2) taste fibers from the soft palate via the palatine and greater petrosal nerves; and (3) preganglionicparasympathetic innervation to the submandibular, sublingual, and lacrimal glands.

The fibers for taste originate in the nucleus of the tractus solitarius (NTS), and the fibers to the lacrimal, nasal, palatal mucus, and submandibular glands originate in the superior salivatory nucleus. Fibers to the lacrimal gland are carried with the greater superficial petrosal nerve until it exits the skull, at which point the fibers branch off as the Vidian nerve.

Nervus intermedius and vestibulocochlear nerve
The nervus intermedius also has a small cutaneous sensory component from afferent fibers originating from the skin of the auricle and postauricular area.
The close anatomic association between the facial nerve, the nervus intermedius, and the vestibulocochlear nerve at the level of the CPA and in the IAC may result in disturbances in tearing, taste, salivary gland flow, hearing, balance, and facial function as a result of lesions at this level.

Common examples are the symptoms of tinnitus, unilateral hearing loss, and balance disturbances often associated with acoustic schwannomas. Large acoustic schwannomas may progress to involve the facial nerve and even CN V, CN IX, CN X, and CN XI.

The facial nerve and the nervus intermedius enter the IAC with the vestibulocochlear nerve. The gross and microscopic anatomic relationships among the locations of CN VII, CN VIII, and the nervusintermedius are of surgical importance. The vestibulocochlear nerve enters the IAC inferiorly (caudad).

The facial nerve runs superiorly (cephalad) along the roof of the IAC. A useful mnemonic for remembering this relationship is "Seven-up over Coke." At the fundus of the IAC, the falciform crest (crista falciformis) divides the IAC into superior and inferior compartments. The facial nerve passes along the superior part of the ledge, separated from the superior vestibular nerve by a vertical bony ridge named the Bill bar (after the esteemed Dr William House).

Intratemporal Course of the Facial Nerve The facial nerve travels through the petrous temporal
bone, as shown in the image below, in a bony canal called the fallopian canal (after Gabriel Fallopius). No other nerve in the body travels such a long distance through a bony canal. Because of this bony shell around the nerve, inflammatory processes involving the central nervous system (CNS) and the facial nerve or traumatic injuries to the temporal bone can produce unique complications.

Labyrinthine (proximal) segment
The labyrinthine segment of the facial nerve lies beneath the middle cranial fossa and is the shortest segment in the fallopian canal (approximately 3.5-4mm in length). In this segment, the nerve is directed obliquely forward, perpendicular to the axis of the temporal bone, as shown above. The facial nerve and the nervus intermedius remain distinct entities at this level.

The term labyrinthine segment is derived from the location of this segment of the nerve immediately posterior to the cochlea. The nerve is posterolateral to the ampullated ends of the horizontal and superior semicircular canals and rests on the anterior part of the vestibule in this segment.

The labyrinthine segment is the narrowest part of the facial nerve and is susceptible to compression by means of edema. This is the only segment of the facial nerve that lacks anastomosing arterial cascades, making the area vulnerable to embolic phenomena, low-flow states, and vascular compression.

After traversing the labyrinthine segment, the facial nerve changes direction to form the first genu (ie, bend or knee), marking the location of the geniculate ganglion. The geniculateganglion is formed by the juncture of the nervus intermediusand the facial nerve into a common trunk. Additional afferent fibers from the anterior two thirds of the tongue are added to the geniculate ganglion from the chorda tympani. Three nerves branch from the geniculate ganglion: the greater superficial petrosal nerve, the lesser petrosal nerve, and the external petrosal nerve.

Petrosal nerves
The greater petrosal nerve emerges from the upper portion of the ganglion and carries secretomotor fibers to the lacrimal gland. The greater petrosal nerve exits the petroustemporal bone via the greater petrosal foramen to enter the middle cranial fossa. The nerve passes deep to the Gasserian ganglion (ie, trigeminal ganglion) to the foramen lacerum, through which it travels to the pterygoid canal.

In the pterygoid canal, the greater petrosal nerve joins the deep petrosal nerve to become the nerve of the pterygoid canal. Axons from this nerve synapse in the pterygopalatine ganglion; postganglionic parasympathetic fibers, which are carried via branches of the maxillary (V2) divisions of the trigeminal nerve (CN V), innervate the lacrimal gland and mucus glands of the nasal and oral cavities.

The external petrosal nerve is an inconstant branch that carries sympathetic fibers to the middle meningeal artery; however, it is not as well known.[5]
The lesser petrosal nerve carries secretory fibers to the parotid gland. This nerve carries parasympathetic contributions from the tympanic plexus (from CN IX) and the nervus intermedius.

Tympanic (horizontal) segment
The tympanic segment extends from the geniculate ganglion to the horizontal semicircular canal and is 8-11mm in length. The nerve passes behind the cochleariform process and the tensor tympani. The cochleariform process is a useful landmark for finding the facial nerve. The nerve lies against the medial wall of the cavum tympani, above and posterior to the oval window. The wall can be very thin or dehiscent in this area, and the middle ear mucosa may lay in direct contact with the facial nerve sheath.

The fallopian canal has been reported to be dehiscent in the area of the oval window in 25-55% of postmortem specimens. Always anticipate finding a dehiscent or prolapsed facial nerve in its tympanic segment, especially in patients with congenital ear deformities.

The distal portion of the facial nerve emerges from the middle ear between the posterior wall of the external auditory canal and the horizontal semicircular canal. This is just distal to the pyramidal eminence, where the facial nerve makes a second turn (marking the second genu).

The most important landmarks for identifying the facial nerve in the mastoid are the horizontal semicircular canal, the fossa incudis, and the digastricridge. The second genu of the facial nerve runs inferolateral to the lateral semicircular canal. This is a relatively constant relationship.

In cases in which the lateral canal is difficult to identify (eg, cholesteatoma, tumor), the use of other landmarks, along with cautious exploration, is advised.
The digastric ridge points to the lateral and inferior aspect of the vertical course of the facial nerve in the temporal bone. In poorly pneumatized temporal bones, the digastric ridge may be difficult to identify.

The distal aspect of the tympanic segment can be surgically located via a facial recess approach. The chorda tympani nerve and the fossa incudis can be used to identify the nerve when performing a facial recess approach,

The long process of the incus points toward the facial recess. The chorda tympani nerve serves at the lateral margin of the triangular facial recess. The chordatympani nerve can be exposed along its length and can be followed inferiorly and medially to its takeoff from the main trunk of the facial nerve. In practice, surgeons most likely employ cues from all these landmarks in respecting the integrity of the facial nerve.

Mastoid segment The second genu marks the beginning of the mastoid
segment. The second genu is lateral and posterior to the pyramidal process. The nerve continues vertically down the anterior wall of the mastoid process to the stylomastoidforamen. The mastoid segment is the longest part of the intratemporal course of the facial nerve, approximately 10-14mm long. During middle ear surgery, the facial nerve is most commonly injured at the pyramidal turn.

The 3 branches that exit from the mastoid segment of the facial nerve are (1) the nerve to the stapedius muscle, (2) the chorda tympani nerve, and (3) the nerve from the auricular branch of the vagus. The auricular branch of the vagus nerve arises from the jugular foramen and joins the facial nerve just distal to the point at which the nerve to the stapedius muscle arises. Pain fibers to the posterior auditory canal may be carried with this nerve.

The chorda tympani is the terminal branch of the nervus intermedius. The chorda runs laterally in the middle ear, between the incus and the handle of the malleus. The nerve crosses the middle ear cavity and exits through the petrotympanic fissure (ie, canal of Huguier) to join the lingual nerve. The chordatympani nerve carries preganglionic secretomotorfibers to the submaxillary and sublingual glands.

. The chorda also carries special sensory afferent fibers (ie, taste fibers) from the anterior two thirds of the tongue and fibers from the posterior wall of the external auditory canal responsible for pain, temperature, and touch sensations.

The facial nerve exits the fallopian canal via the stylomastoid foramen. The nerve travels between the digastric and stylohyoid muscles and enters the parotid gland. A sensory branch exits the nerve just below the stylomastoid foramen and innervates the posterior wall of the external auditory canal and a portion of the tympanic membrane.

Extratemporal Facial Nerve A number of useful landmarks are used to locate the facial
nerve. Topographic landmarks, shown in the image below, can serve as guides for locating the course of the facial nerve and its branches. For example, a line drawn between the mastoid tip and the angle of the mandible can serve as a useful landmark for the superior limits of a neck dissection. Removal of parotid tissue inferior to this line can be performed relatively safely.

The topographic trajectory of the frontal and/or marginal branches should be identified during a rhytidoplasty, submandibular gland excision, and/or neck dissection. The frontal branch can be roughly located along a line extending from the attachment of the lobule (approximately 5mm below the tragus), anterior and superior to a point 1.5cm above the lateral aspect of the ipsilateral eyebrow

Surgical landmarks to the facial nerve include the tympanomastoid suture line, the tragal pointer, and the posterior belly of the digastric muscle. The tympanomastoid suture line lies between the mastoid and tympanic segments of the temporal bone and is approximately 6-8mm lateral to the stylomastoidforamen.

The main trunk of the nerve can also be found midway between (10mm posteroinferior to) the cartilaginous tragal pointer of the external auditory canal and the posterior belly of the digastric muscle. The nerve is usually located inferior and medial to the pointer.

During surgical dissection, the surgeon may encounter a branch from the occipital artery that lies lateral to the facial nerve. Brisk bleeding at this time may be a sign that the nerve is in close proximity; hemostasisshould be obtained using bipolar electrocautery, and further dissection should proceed cautiously. The styloid process is deep to the main trunk of the nerve.

In the infant and young child, these landmarks are not applicable because of differences in the rate of anatomic development of the parotid gland and mastoid. The modified Blair incision most commonly used in adults is often avoided in children because the facial nerve is located more superficially, and the risk of injury is increased with elevation of the skin flaps.

Many textbooks on pediatric otolaryngology provide detailed descriptions of the safe placement of surgical incisions for exposing the facial nerve and its branches in children.
Once it has exited the fallopian canal at the stylomastoid foramen, the facial nerve gives off several rami before it divides into its main branches.

Below the stylomastoid foramen, the posterior auricular nerve leaves the facial nerve and innervates the postauricular muscles. Two small branches innervate the stylohyoid muscle and posterior belly of the digastric muscle.
The facial nerve crosses lateral to the styloid process and penetrates the parotid gland. The nerve lies in a fibrous plane that separates the deep and superficial lobes of the parotid gland. In the parotid gland, the nerve divides at the pesanserinus into 2 major divisions; ie, the superiorly directed temporal-facial and the inferiorly directed cervicofacialbranches.

After the main point of division, 5 major branches of the facial nerve exist, as follows:
Temporal (ie, frontal)
Zygomatic
Buccal
Marginal mandibular
Cervical

The facial nerve innervates 14 of the 17 paired muscle groups of the face on their deep side. The 3 muscles innervated from other sources are the buccinator, levatoranguli oris, and mentalis muscles. Frequent connections between the buccal and zygomatic branches exist. The temporal and marginal mandibular branches are at highest risk during surgical procedures and are usually terminal connections without anastomotic connections.

Superficial musculoaponeurotic system
The superficial musculoaponeurotic system (SMAS) is a superficial fascial layer that extends throughout the cervical facial region. In the lower face, the SMAS invests the facial muscles and is continuous with the platysma muscle. Superiorly, the SMAS ends at the level of the zygoma because of attachments of the fascial layers to the zygomatic arch.

The temporoparietal fascia is not continuous with the SMAS, but they are most likely embryologic equivalents. The temporoparietal fascia extends from the zygomatic arch as an extension of the deep temporal fascia. In the temporal region, the frontal branch of the facial nerve crosses the zygomatic arch and courses within the superficial layer of the deep temporal fascia (temporoparietal fascia).

In the scalp, the equivalent of the SMAS is the galeaaponeurotica, which splits to ensheathe the frontalis, occipitalis, procerus, and some of the postauricularmuscles. In the upper face, the neurovascular structures exit their bony foramina and penetrate the SMAS to run within its superficial aspects or on its surface.

The SMAS encloses all of the facial muscles and is their only attachment to the overlying dermis, thus transmitting contractions of the facial muscles to the overlying skin. A conceptual understanding of the anatomy of the SMAS is important to the surgeon. In the lower face, the facial nerve always runs deep to the platysma and SMAS and innervates the muscles on their undersurfaces (except for the buccinator, levator anguli oris, and mentalis muscles).

The SMAS also helps the surgeon to identify the location of the facial nerve during dissection toward the midline of the face, where the nerve can be found running on top of the masseter muscle just below the SMAS.

Temporal branches The relationships of the temporal branch are complex and only
briefly described in this article. Refer to Larrabee and Makielskifor a more complete anatomic description.[7] The temporal branch of the facial nerve exits the parotid gland and runs within the SMAS over the zygomatic arch into the temple region. The frontal branch enters the undersurface of the frontalis muscle and lies superficial to the deep temporalis fascia. To avoid injury to the frontal branch during elevation of facial flaps, the surgeon should elevate either in a subcutaneous plane or deep to the SMAS.

Marginal branches The mandibular (or marginal) division lies along the body
of the mandible (80%) or within 1-2cm below (20%). This is a critical landmark in head and neck surgery. The marginal branch lies deep to the platysma throughout much of its course. It becomes more superficial approximately 2cm lateral to the corner of the mouth and ends on the undersurface of the muscles. Injury to the marginal branch results in paralysis of the muscles that depress the corner of the mouth.

Facial Nerve Paralysis
The spectrum of facial motor dysfunction is wide, and characterizing the degree of paralysis can be difficult. Several systems have been proposed, but since the mid-1980s, the House-Brackmann system has been widely used. In this scale, grade I is assigned to normal function, and grade VI represents complete paralysis. Intermediate grades vary according to function at rest and with effort.

GradeDescriptionCharacteristics
INormalNormal facial function in all areas
II Mild dysfunction - Slight weakness noticeable on close inspection; may have very slight synkinesis.
III Moderate dysfunction - Obvious, but not disfiguring, difference between 2 sides; noticeable, but not severe, synkinesis, contracture, or hemifacial spasm; complete eye closure with effort y slight synkinesis

House Brackmann grading IV-Moderately severe dysfunction -Obvious weakness
or disfiguring asymmetry; normal symmetry and tone at rest; incomplete eye closure
V -Severe dysfunction - Only barely perceptible motion; asymmetry at rest
VI -Total paralysis --No movement

Vascular Supply of the Facial Nerve
The cortical motor area of the face is supplied by the Rolandic branch of the middle cerebral artery. Within the pons, the facial nucleus receives its blood supply primarily from the anterior inferior cerebellar artery (AICA). The AICA, a branch of the basilar artery, enters the internal auditory canal (IAC) with the facial nerve. The AICA branches into the labyrinthine and cochlear arteries.

The superficial petrosal branch of the middle meningeal artery is the second of 3 sources of arterial blood supply to the extramedullary (ie, intrapetrosal) facial nerve. The posterior auricular artery supplies the facial nerve at and distal to the stylomastoid foramen. Venous drainage parallels the arterial blood supply.

THANK YOU.