EPI Issue #6 Winter
-
Upload
logan-plaster -
Category
Documents
-
view
221 -
download
2
description
Transcript of EPI Issue #6 Winter

THE
ISSUEAFRICA
ethiopiaAn in-depth report from a developing health system
botswanaA Swede’s observations of an up-and-coming EM program
Issue 6 // november 2011 www.epIjournal.com
Why isn’t the UN talking about acute care?
MSF: Pediatric emergencies in Galgaduud
Bahrain: Detained docs spark global outcry
EMERGENCY PHYSICIANSINTERNATIONAL
the
issueAFRICA

2 November 2011 // Emergency Physicians International www.epijournal.com 3 2 November 2011 // Emergency Physicians International www.epijournal.com 3
EPiad_fa.fh11 10/12/11 11:18 AM Page 1
Composite

2 November 2011 // Emergency Physicians International www.epijournal.com 3 2 November 2011 // Emergency Physicians International www.epijournal.com 3
After what had seemed like years of relative neglect, emergency medicine has taken great strides forward in Africa over the past several years. If you are reading this issue of Emergency Physicians International in Cape Town, at the “Emergency Medicine in the Developing World” conference, you are probably aware of some
of these coordinated efforts to develop this pivotal medical specialty. If you’re reading EPI online, there are no shortage of ways to get involved in EM development work in Africa.
Recent African EM developments to highlight include the formation of the African Federa-tion for Emergency Medicine (AFEM) as well as the publication of the federation’s new peer-reviewed journal, the African Journal of Emergency Medicine (www.afjem.org). There are new EM residency training programs in Tunisia, Ghana, Tanzania, Madagascar, South Africa, and Kenya (among others), and there has been an increase in participation by African emergency physicians at international EM conferences. In addition, there is a growing African presence in the International Federation for Emergency Medicine (IFEM), with the Emergency Medicine Association of South Africa and the Tunisian Society for Emergency Medicine being “Full” members of IFEM, the Madagascar Association of Urgent Medicine and Reanimation Anes-thetists being an “Affiliate” member, and AFEM being an “Ex-officio” member.
As Terry Mulligan, Lee Wallis and others have pointed out in prior presentations and pub-lications, many African countries are undergoing significant demographic and epidemiologic changes which make having quality emergency care delivery systems all the more necessary. Multiple factors, including urbanization of populations, increased road traffic, aging of popu-lations, and greater occurrence of armed conflict and violence have contributed to an increased incidence of trauma and cardiopulmonary illness. Not only are these concerns well cared for by emergency care specialists, but they have been experienced around the world, making a global dialogue on EM development highly relevant and practical.
In Africa, acute care issues have actually outpaced HIV, malaria, and the other infectious diseases – which have received perhaps disproportionate attention and financing – as a public health threat. It has only been recently that the World Health Organization (WHO) has wo-ken up to the need to promote and develop better trauma care as a health system priority for developing countries. Similarly, it wasn’t until this Fall that the United Nations held a high-level meeting that brought focus and attention to the increasing problem of non-communica-ble diseases, which account for over 63% of deaths in the world today.
The world is taking note that there has been a shift in global morbidity and mortality, and emergency medicine is a key part of the answer. EM can act as a safety net for these skyrocket-ing health issues like heart disease and trauma, and it can do so efficiently and effectively.
There is huge potential for emergency medicine to improve public health throughout the African continent, and I encourage you to become involved, if you are not already. Providing training materials, participating in training development programs, hosting exchange African medical students and EM residents and physicians, are some of the ways you can contribute. Hope to meet you at this Cape Town conference!
C. James Holliman, MD, FACEP, FIFEM editorial director
Editor’s dEsk
Obstacles & Opportunity
In africa, acute care issues have actually outpaced HIv, malaria, and the other infec-tious diseases – which have received perhaps dispropor-tionate attention and financ-ing – as a public health threat. It has only been recently that the world Health organization (wHo) has woken up to the need to promote and develop better trauma care as a health system priority for developing countries.
About EPIwith a quarterly print and digi-tal distribution and an online network of more than 1,200 members, epI is the new hub connecting global emergency care, sparking dialogue and creating a space for new col-laborations. Find copies of the print magazine at interna-tional em conferences around the world, or read it online at www.epijournal.com
THE
ISSUEAFRICA
ethiopiaAn in-depth report from a troubled healthcare system
botswanaA Swede’s observations of an up-and-coming EM program
Issue 6 november 2011 www.epIjournal.com
Why isn’t the UN talking about acute care?
MSF: Emergent medical needs in Galgaduud
Bahrain: Detained docs spark global outcry
EMERGENCY PHYSICIANSINTERNATIONAL
the
issueAFRICA
conference program for “Emergency
Medicine in the Developing
World” starts on back cover cover illustration
by tracey jolliffe

4 November 2011 // Emergency Physicians International www.epijournal.com 5 4 November 2011 // Emergency Physicians International www.epijournal.com 5
publisher Logan [email protected]
editorial director C. JamEs HoLLiman, md
executive editors PEtEr CamEron, md tErry muLLigan, do, mPHLEE WaLLis, md mark PLastEr, md
associate editorLonniE stoLtZFoos
regional corespondents Conrad buCkLE, md marCio rodriguEs, mdCarLos rissa, mdkatrin Hruska, mdsubroto das, mdmoHamEd aL-asFoor, mdJiraPorn sri-on, md
editorial advisorsariF aLPEr CEvik, md katE dougLass, md HayWood HaLL, md CHak-WaH kam, md grEg Larkin, md ProF. dongPiLL LEE sam-bEom LEE, md gLadys LoPEZ, md aLbErto maCHado, mdJorgE otEro, md advertisingmiCHELLE ruCks [email protected] College AvenueAnnapolis, MD 21401
Submissions & LettersC/o Logan PLastEr Emergency Physicians International210 Columbia HeightsBrooklyn, NY [email protected]
EP International is a product of M.L. Plaster Publishing Co., LLC ©2010
Founder / CEO mark L. PLastEr, md
Executive Vice President rEbECCa r. PLastEr
This issue of EPI is dedicated to emergency medicine development on the continent of Africa. But which Africa? The second largest continent comprises 54 sovereign states and more than a billion people – among whom are spoken around two thousand languages. Think emergency medicine is complicated where you live?
Try living in Chad and writing your discharge instructions in four dialects of Kanuri. Africa’s emergency medical establishment is nearly as diverse as its geography and lin-
guistics, yet there are common themes that bind it together. Namely, Africa has become a place that inspires innovative medical collaborations rarely seen elsewhere. In 2006, Canadians, Americans and Ethiopians established a CME training seminar in Ethiopia that has since become an annual symposium (read our in-depth report on Ethiopian de-velopments on page 17). Likewise, the MUHAS residency in Tanzania is supported by a unique consortium of five institutions from Cape Town to California (read the Tanzania Source report on page 14). And nowhere is this spirit of collaboration more evident than in South Africa’s Adopt-a-Delegate program. The concept, which pairs African emergency care workers who may have difficulty attending a regional EM conference with a financial sponsor, was initiated at the second “EM in the Developing World” conference in South Africa. The first year saw 13 delegates apply and receive sponsorship; the second year saw that number more than double. Sponsored delegates receive more than financial assistance, says program founder Steven Bruijns. They are able to build and maintain a professional relationship with their sponsor long after the conference is over, giving new emergency physicians important confidence and critical contacts.
While most emergency care systems in Africa are still in their early stages of develop-ment, African emergency medicine is teaching the world a thing or two about creative, multi-national collaboration. So whether you work in New Zealand, New Guinea or New York, get involved – there has never been a better time to roll up your sleeves and take part in emergency medicine development in Africa. Not sure where to start? Just say hello. Meet colleagues from all over Africa on the EPI Network (www.epijournal.com).
Logan PlasterPublisher
ConnECt WitH intErnationaL CoLLEaguEs on EmErgEnCy
mEdiCinE’s LargEst ProFEssionaL nEtWork
Join more than 1,200 members from more than 60 countries
Create a professional profile for networking and communicating internationally
Post international events and learn about new conferences being held
Share photos, videos and educational materials with colleagues
Join a discussion in progress or start a thread of your own
on the web
LEttEr From tHE PubLisHEr
Continental Collaborators
www.epijournal.com

4 November 2011 // Emergency Physicians International www.epijournal.com 5 4 November 2011 // Emergency Physicians International www.epijournal.com 5

6 November 2011 // Emergency Physicians International www.epijournal.com 7 6 November 2011 // Emergency Physicians International www.epijournal.com 7
EVENT CALENDAR 12/11–11/12
1 2 m o n t h s o f i n t e r n a t i o n a l
e m c o n f e r e n c e s
JANUARY/20122nd International Conference on Preparedness and Responses to Emergencies and Disasters // Tel Aviv, IsraelJanuary 15 – 19, 2012 www.ipred.co.il
The 1st Global Network Conference on Emergency Medicine// Dubai, UAEEmail papers to: [email protected] January 13 – 17, 2012www.emergencymedicineme.com
MARCHThe 16th Annual Scientific Assembly of the Israeli Association of EM // Tel Aviv, IsraelEmail for abstract submission: [email protected] 13-14, 2012www.kldltd.co.il
32nd International Symposium on Intensive Care and Emergency Medicine // Brussels, BelgiumMarch 20-23, 2012www.intensive.org
MAYThe Inter-American Emergency Medicine Conference // Buenos Aires, ArgentinaThis collaboration with the American Academy of Emergency Medicine (AAEM) consists of three days of lectures as well as a range of pre-conference workshops. May 16 – 18, 2012International-em.org
JUNEFirst International Congress of Pediatric Emergency Medicine // Leon Guanajuato, MexicoThis congress will cover topics from controversies in pediatric resuscitation to pediatric airway management to the organization of emergency service. June 14 – 16, 2012www.anmuep.org.mx
The 2012 International Conference on Emergency Medicine (ICEM) // Dublin, IrelandThe theme of ICEM 2012 is ‘Bridging the Gap between Evidence and Practice’ and topics will include Disaster Medicine, Biomedical Research, Paediatric Emergency Medicine, Prehospital Care and Resuscitation among many others. June 27 – 30, 2012www.icem2012.org
OCTOBEREuSEM 2012 // Antalya, TurkeyThe 7th European Congress on Emergency Medicine October 3 – 6, 2012www.eusem.org
The American College of Emergency Physicians Scientific Assembly // Colorado, United StatesThe annual meeting of the largest emergency medicine society in the world October 8 – 1, 2012www.acep.org/sa
Pan-Pacific Emergency Medicine Congress 2012 (PEMC 2012) // Seoul, KoreaThe Korean Society of Emergency Medicine (KSEM) will host a joint meeting between the American Academy of Emergency Medicine (AAEM) and KSEM. October 23 – 26, 2012www.pemc2012.org
3rd EurAsian Congress on Emergency Medicine // Antalya, TurkeyCo-Organizers: Emergency Medicine Association of Turkey (EMAT), SUNY-DownState, Singapore Society for Emergency Medicine (SSEM) September 19 – 22, 2012
LiSt yoUr Next iNterNatioNaL eveNt For Free
oN the ePi NetWork – WWW.ePijoUrNaL.coM
In ThIs Issuewww . e p i j o u r n a l . c o m
03 | editor’s Desk
08 | relief Pediatric emergencies in somalia
09 | Policy Terry Mulligan reports from the un
Source10 | Dispatches Who is doing development work in Africa? how can you get involved?
11 | Bahrain how the recent imprisonment of Bahraini physicians points to a critical disconnect between medical workers and national medical leadership.
12 | turkey Government reform has brought positive change in the eurasian medical establishment.
13 | tanzania The east African nation’s first eD could become a center for eM education
Reports14 | african eM research sAeM’s Adam Levine reviews three practice-changing studies from across Africa
15 | a Swede in Botswana A scandinavian eP working in Botswana witnesses firsthand the rise of evidence-based emergency medicine in southern Africa.
16 | eM Development in ethiopia An in-depth dossier on eM development in one of Africa’s more troubled healthcare systems.
19 | ieM Fellowship Directory
22 | Grand rounds Peter Cameron on the problem with “efficient” emergency medicine

6 November 2011 // Emergency Physicians International www.epijournal.com 7 6 November 2011 // Emergency Physicians International www.epijournal.com 7
The 1st Global Network Conference on Emergency MedicineDubai International Convention and Exhibition Centre, Dubai, UAE
13 – 17 January 2012
www.emergencymedicineME.com
Endorsed by: Media Partners:
Chairman: Prof. Abdelouahab Bellou, President of the European Society for Emergency Medicine
Pre-Conference Workshops
Main Conference
09:00 - 18:00
Friday 13th January Pre-Conference Courses
Saturday 14th January Pre-Conference Courses
WS 1 WS 2 WS 3 WS 4 WS 1 WS 2 WS 3 WS 4 WS 5
Ultrasound Simulation Pediatric Emergency Metabolic Ultrasound Simulation Pediatric
Emergency Administration Disaster Medicine
09:00 - 12:30
13:00 - 14:00
14:00 - 18:00
Sunday 15th JanuaryConference
Monday 16th January Conference
Tuesday 17th January Conference
Track 1 Track 2 Track 3 Track 1 Track 2 Track 3 Track 1 Track 2 Track 3
Intensive Care Administration Cardiovascular Pre-Hospital Research Trauma Toxicology Sepsis Education
Lunch Break Lunch Break Lunch Break
Ultrasound Administration Disaster Medicine International Pediatric ResidentsSession
Q&ASession
To BeConfirmed Education
Organised by:
Emergency Medicine_AD_EPi Magazine.indd 1 10/16/11 12:39 PM

8 November 2011 // Emergency Physicians International www.epijournal.com 9 8 November 2011 // Emergency Physicians International www.epijournal.com 9
u malnutrition rates are very high in large parts of south and central somalia, but the ongoing conflict makes it difficult for international organizations like doctors Without borders/médecins sans Frontières (msF) to operate at full capacity. Where msF can work, our doctors face immense pres-sure due to the large num-bers of people who need emergency assistance.
dr. Faiza adan abdirah-man is the medical doctor in charge of the pediatric department at istarlin hos-pital in galgaduud, where msF has been working since January 2006. she spoke by phone on august 30:
I’m in charge of the pediatric department, where I deal with newborns and children up to the age of 14. Our main focus at the moment is the large number of malnourished children coming to us.
The children we’re treating are severely sick. [Today] it’s only 3pm and we’ve already admitted 70 children. These are children who are so ill that they can’t even take medicine on their own. In our out-patient department, we are receiving a lot of patients.
Before the droughts, less than 20 percent of our patients were malnourished, but now the number is closer to 50 percent. With malnourishment, come all manner of other diseases. Many of these children are suffering from watery diarrhea and pneumonia. We’re also seeing other problems and complications such as measles and renal and heart problems.
For children whose condition is critical and a second medical opin-ion is necessary, we use telemedicine technology to connect with a pediatric specialist based in Nairobi. We have been holding real-time medical consultations between Guri El and Nairobi since last Decem-ber. So far the results have been positive.
A lot of the children we’re treating are very young, of breastfeeding age. Breast milk contains vital antibodies that babies need to fight off infection, and without it, they’re left defenceless. But we’re in a situa-tion where mothers themselves have nothing to eat and, as a result, are not producing milk. This means children aren’t being breastfed and are left vulnerable. We’re seeing the results of this on a daily basis.
Let me tell you about one patient we’re currently treating: Seven-year-old Bishaaro was brought to us in a very bad state. She was weak and had ulcers all across her body, which were all infected. She also
had liver problems, was severely anemic and, after we ran some tests, we found she also had kala azar, which is a tropical disease transmitted by sandflies that is deadly if left untreated.
We started treating her immediately, giving her medicine and a blood transfusion. But then she started bleeding from her nose and her mouth. She lost so much blood that we had to give her a second blood transfusion. Bishaaro is getting better now and her bleeding stopped. We all have high hopes that she’ll recover fully and go home soon.
We’re facing a lot of challenges here at the moment, so many, in fact, that we’d probably be here all day if I listed them all. We have parents who are opting for traditional medicine when their children fall ill, with traditional doctors burning and cutting the children’s skin in an attempt to heal them. These wounds get infected and, as these children’s defences haven’t fully developed, they either die or come to us in terrible shape with all sorts of infections.
We have parents taking away their children before they complete their treatment, and then returning them to us when their condition has deteriorated even further.
Most of all, space is the biggest issue. We’re currently treating the largest number of patients at the hospital since I’ve been working here, and space is at a premium. We are over capacity and are constantly working out ways of keeping malnourished patients apart from those suffering from TB or measles. Putting them together is simply not an option.
Despite all these major challenges, lives are being saved and we are able to assist these children, many of whom would have died.
disastEr rELiEF
SoMaLia
Pediatric Emergencies in Galgaduud
space is the biggest issue. we are over capacity and are constantly working out ways of keep-ing malnour-ished patients apart from those suffer-ing from Tb or measles. putting them together is simply not an option.
© M
SF

8 November 2011 // Emergency Physicians International www.epijournal.com 9 8 November 2011 // Emergency Physicians International www.epijournal.com 9
U.N. Puts NCDs On the Map Positive effort by United Nations to curb non-communicable diseases falls short of setting targets and fails to address global emergency medicine development issues. by terry mulligan, md
On September 19-20, 2011, the United Nations held a global summit that took an important step towards ad-dressing non-communicable
diseases (NCDs) such as cancer, heart disease, lung disease and diabetes. The summit was devoted to curbing, preventing, recognizing and treating these often-preventable problems that cause 63% of deaths worldwide.
The two-day general assembly meeting, at-tended by more than 30 heads of state and at least 100 other senior ministers and experts, adopted a declaration calling for a multi-pronged campaign by governments, industry and civil society. The plans address the need to curb the risk factors behind four major groups of NCDs – cardiovascular diseases, cancers, chronic respiratory diseases and diabetes – by the year 2013.
Secretary-General Ban Ki-moon noted that over a quarter of all people who die from NCDs succumb in the prime of their lives, the vast majority of them in developing countries. The overall annual death toll from NCDs is estimated at 36 million worldwide.
“Cancer, diabetes, and heart diseases are no
longer the diseases of the wealthy,” said Ban Ki-moon. “Today, they hamper the people and the economies of the poorest popula-tions even more than infectious diseases. This represents a public health emergency in slow motion.
“The prognosis is grim,” he continued. “According to the World Health Organization (WHO), deaths from NCDs will increase by 17 per cent in the next decade. In Africa, that number will jump by 24 percent.”
Noting that “the rising prevalence, mor-bidity and mortality” of NCDs can be largely prevented and controlled through collective and multi-sectoral action by all member states and other relevant stakeholders, the NCD declaration highlights the need for universal national health coverage and strengthened in-ternational cooperation to provide technical assistance and capacity-building to develop-ing countries.
“This will be a massive effort, but I am convinced we can succeed,” Secretary-Gener-al Ban Ki-moon told the opening session of the landmark summit, only the second ever to deal with health (the first was HIV/AIDS in 2001).
POLICY//The prognosis is grim. ac-cording to the wHo, deaths from ncDs will increase by 17% in the next decade.”-ban ki-moon
What about emergency medicine, trauma and acute care?
This historic meeting brought together many national and interna-tional organizations. Most prominent was the NCD Alliance (ncdalli-ance.org), an organization of four international federations uniting a network of over 2000 organizations. These four organizations, namely the International Diabetes Foundation, the World Heart Federation, the Union for International Cancer Control, and the International Union Against Tuberculosis and Lung Disease, represent the four main NCDs outlined in the World Health Organization’s 2008-2013 Action Plan for NCDs – cardiovascular disease, diabetes, cancer, and chronic respiratory disease. These conditions share common risk factors (in-cluding tobacco use, physical inactivity and unhealthy diets) and also share common solutions, which provide a mutual platform for collabo-ration and joint advocacy.
Absent from the UN meeting were any major national or inter-national organizations representing trauma and injury, or emergency medicine. Largely unnoticed in Europe and North America, trauma has become a rapidly expanding epidemic in the world’s low and middle-in-come countries. Every 5 seconds someone in the world dies as a result of an injury. In fact, injuries kill about 5.8 million people each year, more than malaria, tuberculosis and HIV/AIDS combined. Tens of millions more suffer injuries that lead to hospitalization, emergency treatment or other care. Among the causes of injury are acts of violence, traffic ac-cidents, burns, drowning, falls and poisoning. Currently, trauma from road-traffic accidents alone is the 6th most common cause of death in middle-income countries, and 9th in the world. Many countries are experiencing a rapid fiscal growth and with it expansion of their infra-structures. The increase in personal wealth means, for many, a gradu-ation from foot or bicycle transport to motorcycles and automobiles. Sadly, this is also reflected in a commensurate increase in road-traffic injury rates. The WHO estimates that by 2030 trauma from traffic ac-cidents alone will be the 3rd most common cause worldwide of both mortality and disability (as measured in disability-adjusted life years, or DALYs), and the majority of these accidents will happen in lower/middle-income countries, precisely those areas with the least developed emergency care and trauma systems.
Although a declaration adopted at the UN Summit laid out the eco-nomic and social importance of eradicating chronic disease, it fell short in two ways. It failed to address trauma systems and emergency care systems, and it did not provide concrete targets. Instead, the politi-cal declaration included suggestions, such as promoting healthier di-ets, tobacco-free workplaces, access to cancer screening programs, and breast-feeding for about six months from birth.
In addition, further attention needs to be paid to trauma morbid-ity and mortality, to the establishment of trauma and emergency care systems, and to the role of emergency medicine and acute care as the safety net for acute and chronic presentations of non-communicable diseases and communicable diseases from all categories. While major benefits will result from attention to primary prevention of the verti-cally integrated five major areas of NCDs, global health policy makers need to also focus on secondary prevention of NCDs by a horizontally integrated emergency medicine and acute care systems.
© M
SF

10 November 2011 // Emergency Physicians International10 November 2011 // Emergency Physicians International
SOURCE // DISPATCHESrEadEr-submittEd uPdatEs From tHE EPi nEtWork
24-28 October, 2011
As the number of interdisciplinary emergency departments grows internationally,where can ED leaders acquire the administrative skills they need to build andsustain successful emergency departments?
The International Emergency Department Leadership Institute (IEDLI) was createdby Harvard Medical School faculty and other international experts in order toprovide ED leaders with the skills and knowledge they need to successfully operateemergency departments in any part of the world.
In this one-week course of over 35 hours of interactive lectures andworkshops, leaders will explore strategies to:
• Establish the ED’s role within the hospital• Improve efficiency and control costs• Decrease overcrowding• Develop quality improvement programs• Educate and motivate ED doctors and nurses• Develop an emergency medicine training program• Form a strong administrative structure
This program is designed for doctors, nurses and administrators.
International Emergency Department Leadership Institute
Boston, Massachusetts, USA
The International Emergency Department Leadership Institute is a collaboration between
Harvard Medical Faculty Physicians at BIDMC and Brigham and Women’s Hospital.
LOGOIEDLIInternational Emergency Department
Leadership Institute
Save the date: IEDLI 2012
October 22-26Leuven, Belgium
www.IEDLI.org
If you would be interested
in working in EM development in Africa, where would you be in-
terested in plugging in, and in what
capacity?
If you have worked in EM
development in Af-rica in the past, briefly
describe a project in which you took
part. If you are currently involved
in EM development in Africa, where are you involved? What
work are you doing?
My big interest is
flow and triage. From what I hear, poor people
still die in the waiting rooms because there often is no triage
and the stronger/richer gets ahead of the cue. Triage tools
could be translated and devel-oped to suit the environment.
Stefan BodetoftSWEDEN
Worked with
Global Emergency Care Skills, a non-profit voluntary
organisation that has run five training programmes in East Africa,
from Nairobi’s Mater Hospital to Lusaka University Teaching Hospital in Zambia
and the Queen Elizabeth University Hospital in Blantyre, Malawi. The most
recent course was held in Muhim-bili University Hospital in Dar Es
Salaam, Tanzania.Jean O’Sullivan
IRElAND
Provid-ing advisory
and consultancy services for develop-
ment and organisation of emergency care services
and education.V. Anantharaman
SINGAPORE
Teaching
in the following locations: JFK Hospital Redemption and Phebe
hospitals in Liberia; Korle-bu in Ghana; Addis Abada.
I’m the ACEP lead ambassa-dor to Ghana and Liberia.
Kathryn ChallonerUSA
Partici-pated in a faith-
based group that goes 4 times a year and runs a
clinic in Ethiopia. Clinic is set up with few EPs, ophthalmol-ogy and optometrist, dentistry
and pediatrics. Jose Muniz
PUERTO RICO
Pend-ing project
in Gabon with U.S. militaryRobert Suter
USA
Happy to go most
places in sub Saharan Africa, especially: Mada-gascar, Zambia, Zimba-
bwe, South Africa, Gabon, Rwanda, Tanzania, Malawi,
DRC, Ethiopia.Justin Venable
NEW ZEAlAND
I’ve worked in
East Africa (Rwan-da) before, know the
healthcare system, and speaks English and
French. Dan Brun Petersen
DENMARk
Mo-zambique,
Southerrn/East Africa developing
emergency services/ womans health
Uk
I am involved in EM
developement in Nige-ria. I started the first EMS in
the country and started the first CPR training for health care provid-ers in 1992. This led me to bring in AHA programs in 2003 and became the ITC coordinator. I have trained over 4000 doctors and nurses in
BLS, ACLS, and PALS.Nnamdi Nwauwa
NIGERIA
www.epijournal.com 11

10 November 2011 // Emergency Physicians International10 November 2011 // Emergency Physicians International
SoURCE
In September, twenty Bahraini doc-tors, nurses and paramedics were sentenced before a military court to up to 15 years in prison. These sentences, which were immediately
decried by the global human rights com-munity, came after six months of unlawful imprisonment and many well-documented abuses.
“It is unlike anything that I have seen in my 20 years of investigating human rights and violations of medical neutrality,” said Richard Sollom of Physicians for Human Rights (PHR) in an interview with CNN. “The type of abuses that are actually occur-ring are serial, are so horrific and so wide spread and systematic.”
Charges against the doctors included possession of unlicensed weapons, inciting the overthrow of the government, provoking sectarian hatred and forceful occupation of a public building, officials said. Prosecutors have alleged that, at the height of the pro-tests earlier this year, the accused medical personnel refused to help patients at Sal-maniya Medical Complex, the main hospital in the capital city, Manama. But the interna-tional community has seen these statements as the attempts of the Bahraini government to abuse power and circumvent the justice system.
“These are simply ludicrous charges against civilian professionals who were working to save lives amid very trying cir-cumstances,” said Philip Luther of Amnesty International
As a specialist in emergency and disaster medicine who worked at Salmaniya Medi-cal Complex (SMC) for more than 13 years, I’ve known many of those physicians, nurses and paramedics who witnessed these events first hand. I listened as one doctor described how he was abducted by armed, masked and unidentified military and police personnel
from the operating theater without any ar-rest permit. He was dragged barefoot, hand-cuffed to the back, blindfolded, in front of his colleagues and staff. The armed abduc-tors broke in to his office where they started torturing him and confiscating his computer and belongings. Then they dragged him throughout the corridors of the hospital, and to the overnight stay doctors’ hostel looking for other colleagues to be arrested.
I also heard from a medic who described how he was tortured physically and abused verbally. All were blindfolded and hand-cuffed. They were interrogated and continu-ally threatened with death and sexual assault. They were not allowed to contact their fami-lies or their lawyers nor were they offered any lawyer from the police side.
But these false imprisonments and abuses of power are only part of the story – the part that makes international headlines. They also tell of deep, systemic problems relating to emergency and disaster management in this small yet important country in the Per-sian Gulf.
Before we get to the mistakes made by the medical establishment, we have to step back to last February, to the massive series of protests that, according to CNN, may have amassed as many as 600,000 people. People came out into the streets, united at first in a desire for reforms. But when some peaceful protesters were killed, the crowds swelled and the desire changed to a complete change of power. What followed was a mas-sive crackdown on protesters by the govern-ment, resulting in more than 40 deaths and hundreds of injuries. Thousands were dis-missed from work. The professional societies were shut off, and their presidents were or still arrested and sentenced to long term of imprisonment. The Bahrain Medical Society and the Bahrain Teachers Society were first to suffer.
BAHRAiNHow the recent imprisonment of Bahraini physicians
points to a critical disconnect between medical workers and national medical leadership
by dr. mohamed al-asfoor
The medical body found itself trapped between escaping protesters from tear gas, ballets guns and live ammunitions, seeking shelters in the main hospital premises and car park area and a government wishing to end any means of protests quickly, no mat-ter how harsh it can be with complete media and news blockage.
At this point, the health ministry began making a series of mistakes that were indica-tive of a lack of disaster planning and quali-fied disaster personnel.
The first mistake was that the minister of health denied the emergent state of the situation. As he reported to the media about few casualties (around 7), the hospital was flooded with literally hundreds – as many as 700 casualties reported within a short period. Many casualties were from tear gas, ballets guns and rubber bullets as well as live ammunitions-related injuries. Also at some point ambulances were prevented from go-ing out to reach outside emergency calls. This resulted in the frustration of the medical staff and caused a worsening of the already bad situation. The medical staff felt betrayed by a minister whom they expected to pro-vide support. I was personally informed by in-hospital physicians and nurses who were desperate, overwhelmed and unable to cope with situation, even days after.
The second mistake was that the media started a campaign against doctors and other medics, characterizing them by their sects and ethnicity. This directly created fear in some patients and prevented medical staff from carrying out their duties. This move of using sectarian language to divide people only exacerbated the chaos in the country, and resulted in the birth of the strongly pro-government party.
The third major mistake was the military occupation of the only secondary and ter-tiary government hospital. This act, which was clearly filmed and reported by many news channels, brings us back to the initial story. The occupation is what led to the ar-rest and abduction of injured patients and their doctors, nurses and paramedics. There were reports of torture and the deprivation of human rights. The doctors and other staff were prevented from leaving or entering the hospital for some time, essentially held hos-tage on their wards. Checkpoints were set in each ward. I still recall my conversation
791,000Total population
LifE ExpECTANCY Men: 73
Women: 76
pROBABiLiTY Of dYiNg BEfORE
AgE 1 9 per 1,000 live births
TOTAL ExpENdiTURE
ON HEALTH pER CApiTA$1,557
(international dollars, 2009)
4.5Total expenditure
on health as percent of GDP
www.epijournal.com 11

12 November 2011 // Emergency Physicians International12 November 2011 // Emergency Physicians International
Since 2002, one of the major sub-jects of the Turkish government has been the implementation of a more individualized health care system. In surveys, the public
constantly mentions health as the govern-ment’s most important success. The new sys-tem enjoys such strong public support that it may help the leading party to garner at least 50% of the vote in Turkey’s 2011 election. There are very few countries that have done what Turkey has in terms of healthcare, and it has a direct relationship to voting.
During the past eight years, the govern-ment has essentially moved toward a person-oriented, equally-shared healthcare system. The government ended restrictions on the pharmaceutical markets, allowed the public to use their state benefits at private and universi-ty hospitals, and has provided “Green Cards” guaranteeing free treatment to more than 9 million low earners. The national network of family doctors has expanded to the point that there is now one for every 3,500 citizens. The family doctors are catching conditions like diabetes and obesity earlier, treating minor problems, and referring only more serious cases to hospitals. This helps to ensure that pa-tients are treated more cheaply than hospitals, according to a government budget watchdog’s 2009 report. In addition to streamlining gen-eral health care management, an initiative to formalize emergency department management was declared in 2009, effectively strengthen-ing the emergency medicine (EM) specialty
compared to its previous status.It is believed that a party leader was mo-
tivated to make these changes after he was transferred from hospital to hospital follow-ing a car accident in the late 1980s. The same leader is also an anti-smoking advocate, and cigarettes are banned from restaurants and bars. National highway regulations were also revised, improving highway capacity and in-frastructure in all regions with strict speed and safety enforcements. It is difficult to evalu-ate the short-term effects of cigarette regula-tions, but highway regulation has significantly decreased the number of deaths from traffic accidents. All of these strategies have had a positive cumulative effect on Turkey’s health, success that should be shared with other coun-tries. Because of its geographical location, collaborating with neighboring countries on healthcare infrastructure is an important po-tential initiative for Turkey. Although medical tourists can enjoy high quality specialty care in Turkey, sharing successful healthcare strate-gies with neighbors and old Ottoman nations will require real effort and non-governmental organization (NGO) support.
Today, there are 450 EM specialists and 700 trainees in EM residency programs in Turkey. These numbers are insufficient for staffing its EM departments (>1,200) but they symbolize a turning point for Turkish EM. Two big national specialty NGOs, EMAT and EPAT, are working to improve EM. Over the pat 16 years EMAT has been the leading organization of Turkish EM since the specialty
officially existed, especially with re-gards to forging friendships and collaborating with other interna-tional NGOs. EMAT has helped clarify the EM needs of Turkey and guided the processes involved.
There is still much room for development. EMAT recently be-came a member of the Asian Soci-ety for Emergency Medicine. Col-laborating with Asian Countries and learning from their experienc-es will surely create great benefit for Turkish EM, and will provide an opportunity for Turkey to share the success of its own health strate-gies in EM.
TURkEYRecent government interest has led to an expansion
of family practice and improved highway safety.by arif alper cevic, md
over the phone with one of the doctors who seemed terrified at the time the army entered the hospital. He was slapped and pushed and his room was searched by police dogs.
Some of the individual physicians con-cerned have detailed their testimonies on their own words in the web site www.doc-torsinchains.org. The website was originally set up by MedWorm which is a medical web-site that has decided to support a campaign for Bahrain doctors. It is now run by a group of medical professionals from across differ-ent countries outside of Bahrain, who all feel the need to speak out in solidarity against the way these doctors have been treated.
How did a series of well-intentioned protests end up with government occupied hospitals? The problems are deeply rooted in Bahrain and they are an accumulation of mistakes and corruptions, with no simple answer. The health authority and the govern-ment are the ones who should have to answer for all of this. The bottom line from a disas-ter preparedness standpoint is that if you are not prepared with a plan, a mass medical emergency can quickly go from manageable to being an unmitigated disaster.
Thanks in part to pressure from the inter-national community, there will be a retrial for the detained medics. But the process is still unclear and no one really knows exactly how or where it will take place. On October 23, before a civilian court, the public pros-ecutor asked the court to drop all confes-sions taken from the twenty medics, saying they were taken under torture. Whatever the result of this retrial, the health care situ-ation in Bahrain will remain fragile and vul-nerable. Many doctors have been dismissed from work while others left the country and applied for asylum abroad.
These days the situation is still far from quiet in Bahrain; nightly protests take place in the villages, cities and the periphery of the capital. Protesters are injured daily but remain unable to go to hospitals for fear of detention, given the militarized state of the hospitals. Instead, most are treated in home clinics.
For a positive resolution, there will need to be a clear article in the constitution re-garding the right of all patients and injured to have unrestricted access to emergency medical care and there will need to be a clear and effective disaster plan. Doctors should never be prevented from their work in treat-ing patients. This all is achievable through freedom and real democracy, and will ulti-mately benefit all people.
Traffic in Istanbul. Vast improvements in highway infrastructure have significantly decreased the number of motor vehicle accident
deaths in Turkey.l
www.epijournal.com 13

12 November 2011 // Emergency Physicians International12 November 2011 // Emergency Physicians International
The United Republic of Tanzania is an East African country with a population of 43 million people, more than 70% of whom live in rural areas. The Tanzanian
public health system is a pyramidal referral system with a broad base of dispensaries that refer up through heath centers, district and regional hospitals, and ultimately to tertiary urban-based consultant hospitals. Muhimbili National Hospital is one of four such refer-ral hospitals, and is located in Dar es Salaam, Tanzania’s largest city.
Prior to 2010, patients arriving at Muhim-bili were received in a casualty area staffed with rotating personnel with no dedicated emergency care training. Initial resuscitation and stabilization were often delayed and treat-ment was inconsistent as there were no formal protocols to direct management. Specialist medical or surgical interventions were also delayed and there was high mortality among critically ill patients.
In 2010, in a joint effort of the Tanza-nia Ministry of Health and Social Welfare, Muhimbili National Hospital, and the Ab-bott Fund-Tanzania, a dedicated full-service emergency department (ED) was opened at Muhimbili National Hospital and is the first
ED in Tanzania. Facilities include treatment and resuscitation rooms with critical care ca-pacity including cardiac monitoring and ven-tilator support.
In the first 12 months of operation the de-partment served over 35,000 patients with an average of 100 patients per day. Patients are mostly referred from other hospitals, but may also be “referred” by the police, as in the case of acute trauma. The number one patient con-dition at the ED overall is trauma, and respi-ratory illnesses are the most common medical complaint seen. The approximate admission rate is 78 percent.
The key to the department’s success so far has been the dedication to specialized training and growing the department’s own training capacity. Throughout the planning and early operations of the department, board-certified emergency physicians from abroad acted as technical advisors, providing training and advice on operations. The advisors supported the establishment of treatment protocols and a training curriculum for the department, and created a supportive teaching environment in the ED. Currently, visiting nurse mentors spe-cialized in emergency medicine, senior emer-gency residents, and emergency medicine faculty, provide clinical teaching throughout
TANzANiAThe East African nation’s first emergency department
could become a center for EM educationby renatus tarimo & teri reynolds
the year on a monthly rotating basis. Local ED personnel are now beginning to take over this training, as new generations of providers arrive.
The academic field of emergency medicine is new to Tanzania and East Africa. The ED was opened with dedicated nurse and registrar physician staffing, as there were no emergency specialists in Tanzania. Less than a year later, in order to ensure the sustainability of emer-gency medicine in Tanzania, the first emergen-cy medicine residency in Tanzania was estab-lished at the affiliated Muhimbili University of Health and Allied Sciences (MUHAS) and based in the ED. The first class of eight resi-dents began in October 2010 and is expected to complete the 3-year program in 2013. The seven residents of the class of 2014 began in October 2011.
The residency is run by MUHAS and the clinical teaching is supported by a unique academic consortium of five institutions, the University of Cape Town South Africa, the University of California San Francisco, Carolinas Medical Center, the University of Chicago and the University of Maryland. The academic consortium members collaborate to provide materials to support the MUHAS curriculum, and provide clinical faculty to support the residency program.
Crucial to the success of the project has been engagement throughout with the Tanza-nian Ministry of Health, who have embraced the ED and integrated it into larger national plans for the dissemination of emergency care. Trainees within the ED have established the Emergency Medicine Association of Tanza-nia (EMAT), a professional organization for emergency providers of all cadres. EMAT has been ratified by the Ministry of Health and this organization has allowed emergency per-sonnel to participate in activities such as na-tional and international sporting events, inter-national meetings, and public health outreach programs. EMAT’s current projects include the development of dedicated, regionally-appropriate basic and advanced emergency care training programs for a variety of clinic, hospital and pre-hospital providers.
In 2012, the ED and the residency will continue working to advocate for the develop-ment of emergency care in Tanzania, as well as to integrate with other African emergency care initiatives. Main areas of focus within the ED are standardizing care and training in the department and conducting research to estab-lish best practices.
Muhimbili registrar Magdalena Mbeyale intubates a trauma patient. Trauma is the top reason for a visit tothe Muhimbili National Hospital emergency department.
43.7 MiLLiONTotal population
70%Live in rural areas
LifE ExpECTANCY Men: 53
Women: 58
pROBABiLiTY Of dYiNg UNdER
AgE 5108 per 1,000
live births
TOTAL ExpENdiTURE
ON HEALTH pER CApiTA
$68 (international dollars, 2009)
5.1Total expenditure
on health as percent of GDP
l
www.epijournal.com 13

14 November 2011 // Emergency Physicians International www.epijournal.com 15 14 November 2011 // Emergency Physicians International www.epijournal.com 15
Abstracts from Africa by Adam C. Levine, MD, MPH
on behalf of the Global Medical Literature Review Group
South Africa_Validation of weight estimation by age and length based methods in the Western Cape, South AfricaGeduld H, Hodkinson PW, Wallis LA. Validation of weight estimation by age and length based methods in the Western Cape, South Africa population. Emerg Med J. 2010.
Many different methods of weight estimation exist for pediatric resuscitation, including the
Broselow tape, the Advanced Pediatric Life Support formula, the Best Guess, and the Luscombe and Owens formula. These formulas are frequently geographically or ethnically specific and therefore may vary in how well they predict weight depending on the region. In this study, the authors assessed which method is most accurate for their population of South African chil-dren. They prospectively enrolled patients between 1 and 10 years of age that presented to the Red Cross War Memorial Children’s Hospital in Cape Town. A Bland-Altman analysis was performed to compare the four different weight estimations. Outcome measures were fit - a predicted weight within 10% of the mea-sured weight – and mean percentage error – how much the estimate deviated from the measured weight. They enrolled 2832 patients during a nine-month period. The Broselow tape emerged as the best estimator of their population (64.2% of estimates were within 10% of the measures weight and the mean percentage error was the smallest at 0.89%).
This study answers a simple question that is a cur-rent focus of international EM research: Can we apply developed world tools to developing world populations? Geduld, et al. demonstrate that weight estimations can be applied to developing countries, but should be validated for the region. Strengths of the study include its large sample size and utilization of a generalizable measure of fit, which allows for easy comparison to age-matched controls in other stud-ies conducted in the US, India, and Hong Kong. A desirable addition would have been a graph with the breakdown of ethnicity and socioeconomic status of the study population. This would have potentially al-lowed other African nations to apply the Western Cape data to their own population rather than conducting another study. In general, this study is exemplary of
research we hope to see more of in developing coun-tries in that it is cost-effective, easily implementable, and can have widespread impact. -AL, EG
Kenya_A novel ED-based sexual assault centre in west-ern KenyaRanney M, Rennert-May E, Spitzer R, Chitai M.A., Mamlin S.E., Mabeya H. A novel ED-based sexual assault centre in western Kenya: description of pa-tients and analysis of treatment patterns. Emergency Medicine J. 2010.
In sub-Saharan Africa, sexual assault and violence remains a major health issue. In this study, an ED-
based sexual assault center was established to study the demographics of sexual assault in Western Kenya, and to assess whether newly established protocols could provide HIV prophylaxis, STI treatment and emer-gency contraception (EC) at rates similar to those in high-income countries. Thirteen months after imple-menting the new protocols, the Centre for Assault Recovery-Eldoret (CAR-E) conducted a retrospec-tive study of the demographic, assault, and treatment characteristics of the patient population served. Over 300 patients were seen at the clinic, with 94% being female. Mean age was 15.9 years, with 50% under the age of 15. Overall, 89% of patients received testing for HIV, 80% for syphilis, and 73% for pregnancy. The study also found relatively high rates of STI prophy-laxis (84%), HIV prophylaxis (63%) and EC (70%) for eligible patients treated at the center. Only 43% of the assaults were reported to the police, and only 44% of patients received counseling, which were both lower than expected.
Sexual assault is common in sub-Saharan Africa, with Kenya being one of the few countries where sex-ual violence is against the law. This study shows that a community focused, ED-based sexual assault center is not only feasible, but can provide effective diagnosis and treatment for patients in a low-income country without the addition of significant external resources. Post-sexual assault counseling is likely to be the most difficult component of the CAR-E sexual assault as-sessment and treatment protocol to implement. This was the most resource-intensive component of their
protocol and implementation was limited by lack of availability of trained counselors, especially after hours. However, despite the low level of post-assault counsel-ing or police reporting, the study highlights that with a little education and concentrated effort, effective diag-nosis and treatment for victims of sexual violence can be provided in a resource-limited setting. -AL, SK
Kenya_Mortality and health among internally displaced personsFeikin DR, Adazu K, Obor D, Ogwang S, Vulule J, Hamel MJ, Laserson K. Mortality and health among internally displaced persons. Bulletin of the World Health Organization. 2010; 88(8):601-8.
Feikin et al. conducted this cohort study among people displaced by the post-election violence in
Kenya in 2008. The authors used demographic surveil-lance survey data to classify recent arrivals to the study area as internally displaced persons (IDPs). Morbidity and mortality between the local and IDP populations were compared. The authors found that IDP children < 5 years of age were 2.95 times more likely to be hos-pitalized than local children (RR, 95% CI: 2.44-3.58), but had equivalent mortality rates. They also found that almost twice as many of the deaths due to HIV that occurred among those age 5 years or older were IDPs compared to non-IDPs (53% versus 25-29%, p<0.001).
The authors leveraged an existing demographic surveillance system to identify a population of IDPs and then compared them to the pre-existing local population. Although this method may have incor-rectly identified as IDPs some recent arrivals who were not displaced by the post-election violence, this over-estimation was likely small. The findings of this study are consistent with previous research that has shown that IDPs are often a vulnerable group – in this case evidenced by more severe presentation of childhood illness and disproportionate mortality due to HIV among individuals over age 5. Nevertheless, this study does give hope by showing that with appropriate treat-ment, excess mortality can be avoided among inter-nally displaced children less than 5 years of age.-AL, KL
Al: ADAM LEVINE, MD, MPH; Sk: SAMPSA KIURU, MD; kl: KEVIN LUNNEY, MD; EG: ELIZABETH GOLDBERG, MD
global Lit review
ReportR

14 November 2011 // Emergency Physicians International www.epijournal.com 15 14 November 2011 // Emergency Physicians International www.epijournal.com 15
Some things are the same everywhere. Airway comes first, then breathing, circulation, disability and exposure – the latter two sometimes replaced by “Don’t Ever Forget Glu-cose” and a laugh. I got to appreciate the universal nature of the EM alphabet first hand when I traveled from Swe-
den to Botswana to practice emergency medicine this year. More and more, we’re all beginning to speak the same language; and a common language sure facilitates communication.
In Sweden, where the model has been for different specialties to handle their own emergencies, it has been hard to explain how one specialty could integrate that knowledge and increase the quality of care. As a result, as an emergency physician you are constantly explain-ing and defending the specialty. For a new perspective, I wanted to travel somewhere where emergency medicine was already established. I considered several countries, but somehow, I ended up working in Bo-tswana, where the development of emergency medicine as a specialty has only just begun.
Botswana is an upper middle income country, placed in the same economic class as Romania, Turkey and Argentina by the World Bank. Eighty percent of health expenditures are provided by the government and primary care is widely available. In the past, due to its population of less than two million, Botswana has sent students abroad for medical studies. Starting three years ago, however, the medical school in Bo-tswana accepted its first students. Just like in Sweden, higher education is free. Here the students even get housing and a small allowance. One of the students I talked to was the youngest of ten siblings, and neither parent had been to university, which to me is an impressive indication that higher education is open to everyone.
In Botswana a doctor is simply a doctor, or a medical officer (MO as they are called here). After a year of internship they are expected to be able to work wherever the government assigns them. There is, of course, some element of choice, but in the end it is up to the Ministry of Health to decide. Specialists have mostly been recruited from abroad and the few Batswana specialists have all trained abroad.
That all is beginning to change. Emergency medicine is now one of six residency programs available in Botswana and three first year residents are training in the Princess Marina Hospital in Gaborone, the capital of Botswana.
In some ways the emergency medicine pathway is easier in Botswana than in Sweden. In many Swedish university hospitals you have to do rotations in different clinics, such as gynecology, ENT and pediatrics, to cover the whole emergency department. There you will be super-vised by the respective specialist, who rarely understands the scope of emergency medicine. To establish emergency medicine as a specialty
in Sweden (as well as in many European countries with similar sys-tems) it does not suffice to increase the competence of the doctors in the emergency departments. All the emergency departments have to be reorganized, which of course involves transferring resources from other departments.
That battle does not have to be fought here in Botswana where the MOs in the emergency department see the unsorted acutely ill patients of all ages. What they lack is specialists to oversee the care given to pa-tients. Currently, there are three foreign emergency medicine specialists in Bostwana to train these future specialists. The curriculum is based on the South African curriculum and very similar to ones from Eu-rope. The residents are taught evidence-based emergency medicine in the same manner as most of their colleagues around the world. Herein lies one of the great training challenges. There is precious little evidence currently available regarding common ED diagnoses in a black African population, particularly when a quarter of the adult population is HIV positive. The launch of the African Journal of Emergency Medicine this summer was a great step in creating this evidence.
Emergency medicine is about more than producing competent emergency physicians, though. It is about developing systems where an adequate amount of time and resources is spent on each individual while making sure that urgent care is not withheld from any patient within the department. Time wasted on unnecessary interventions on one patient could end up harming another patient. This requires good management on the floor and teamwork from nurses and doctors. Cre-ating that system in Botswana is not easy, partially because of cultural norms – doctors, nurses, even patients have an amazing acceptance for malfunctioning equipment and lacking supplies. The major challenge for our future colleagues here will be to establish patient processes that involve all levels of staff and ensure a systematic approach to all major patient categories.
Each day that I practice here I am reminded of – and instructed by – the distinct cultural differences between Sweden and Botswana. In Botswana it is the disease that kills the patient, not the inadequate interventions by the doctor. No one here demands you prove that a common cold is not a pulmonary embolism or five minutes of chest discomfort a threatening acute coronary syndrome. It makes me real-ize just how much of our workup in Sweden merely serves to comfort either the doctor or the patient, and how our impatience brings these investigations to the emergency departments instead of the outpatient setting of primary care. We take full responsibility for the patients medical condition, leaving very little up to the patient, except to place the blame on us if we fail.
botswana
EM Takes Its Place in Gaboronea scandinavian EP working in botswana wit-nesses firsthand the rise of evidence-based emergency medicine in southern africa.
by Katrin Hruska, MD
Report / botswanaR
Batswana emergency nurses
outside of the A&E department in Gaborone.
l
no one here demands you prove that a common cold is not a pulmonary embolism. . . It makes me realize just how much of our workup in sweden mere-ly serves to comfort either the doctor or the patient.

16 November 2011 // Emergency Physicians International www.epijournal.com 17 16 November 2011 // Emergency Physicians International www.epijournal.com 17
Challenge, Progress & PossibilitiesAn in-depth dossier on emergency medicine development in Ethiopia
by Fikre Germa, mD, FcFp; Tesfaye bayleyegn, mD; Kidist barolomios, mpH; Tsegazeab Ke-bede, mD; jim Ducharme mD cm Frcp
The health care needs of Ethiopia are im-mense and complicated. This ancient country situated in the horn of Africa is home to over 80 million people (Table 1),
most of whom are impoverished and live in rural set-tings. The population is growing rapidly and targeted to exceed 100+ million by 2020. Complicating mat-ters further is the fact that the communicable diseases most associated with poverty have been superseded by diseases of urbanization and economic development, such as cardiovascular diseases and vehicular trauma.
Ethiopia has one of the highest road traffic crashes and fatality rates in Africa. An estimated 60% of the crashes occur in Addis Ababa, the nations capital city of 3.5 million residents. There are about 8,400 road traffic crashes annually, resulting in 1,800 fatalities and $2.1 million in property loss annually. Pedestrians are the highest proportion (81.5 per cent) of people involved in traffic accidents, followed by vehicle occu-pants (15.2 per cent) and drivers (3.3 per cent). Most traffic accidents in Addis Ababa involve people from 15 to 45 years of age.
Pre-hospital and Hospital EM in Addis Ababa, Ethiopia
Addis Ababa has no organized EMS system. Criti-cally injured or ill patients arrive at poorly equipped and disorganized emergency units through the Addis Ababa Red Cross (AARC) or an informal network of private cars and taxis that transport patients to hospi-tals. Private hospital ambulances operate on a strictly fee-for-service basis. There is no air ambulance ser-vice.
In addition, there is no citywide designated emer-gency phone (i.e., a single 9-1-1 dispatch system). Each agency involved in emergency response has its own emergency number comprised of three to six dig-its. AARC has 10 ambulances and provides services via a 9-9-2 number, however, they can only run four per day due to a limited municipal budget. The AARC ambulances are equipped with a bed and basic sup-plies but do not have life support equipment and the staff have only minimal medical training. There is no standardized training or certification of emergency medical technicians (EMTs), and there is no commu-nication between ambulance staff and receiving hos-pitals. In addition, there are no national or regional
guidelines for triage, patient delivery decisions or pre-hospital treatment plans.
The Public/Private Divide
Government-run hospitals in Addis Ababa do not have designated emergency departments. Rather, there is usually a “receiving area” where both scheduled and emergency patients are seen. The lack of a designated ER makes it difficult to provide dedicated emergency care with appropriate triage protocols, rapid diagnosis and timely treatment. In most hospitals, each major department provides “receiving area” coverage for pa-tients with scheduled or emergency outpatient visits. Triage can be provided by a general practitioner and a health assistant or a nurse on duty. Triage is rarely practiced by persons with the ability to recognize the early signs of life or limb threatening illness, therefore those who could benefit most from early intervention are often forced to wait while those who do not require immediate care are seen first. Often the hospital’s labo-ratory and radiology departments are far from the ED and many do not have the capacity or personnel to provide quick turnaround of requested tests. In many hospitals, the responsibility of transporting patients to tests, providing bedside non-medical care, such as feeding and toileting patients, falls almost exclusively on the patients’ families.
In almost all of the public and private clinics and hospitals in Ethiopia, facilities and equipment for ad-ministering emergency care are inadequate. Even in hospitals that have dedicated space and staff for receiv-ing acute care patients, basic equipment and medi-cations are lacking. The receiving areas of even the best-equipped and best staffed public hospitals lack the human and material resources to care for a person in distress – often efforts to support airway function, provide sedative and pain medications, or rapidly di-agnose such patients are impeded. Most hospitals lack the ability to provide fundamental cardiac care because of the lack of basic equipment such as ECG machines, cardiac monitors or even oxygen.
There are 28 private hospitals in Addis Ababa with a total capacity of 925 beds. The city’s private hospitals offer services on a fixed fee basis. Some of these hospi-tals have ambulance services for inter-hospital transfer and can also be used to transport patients to the hospi-tal. Emergency care is often not even initiated without a down payment so investigative and therapeutic pro-cedures are often withheld until payment is received. Patients who lack sufficient funds are directed to seek care at government hospitals. Many for-profit (and
even not-for-profit private hospitals) feel they lack both the personnel and resources to provide “open door” emergency treatment.
The Need to Strengthen Ethio-pia’s EM Education
Prior to the early 90s initiative, Ethiopia had no systematic program in place to improve the knowledge and practice of health professionals working in the emergency unit. In 1993 initiatives to introduce the concept of contemporary emergency medicine were started. In 1996, the first shock/resuscitation room with two beds and basic life support equipment was established in the Black Lion Hospital (BLH) outpa-tient surgical department.
In 1998, the Addis Ababa Health Bureau (AAHB), in cooperation with interested local staff and Israel’s emergency medicine association, held the first emer-gency medicine workshop in Addis Ababa for 20 doc-tors and 10 nurses (see table 2A) selected from Addis Ababa hospital outpatient departments (including
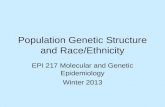
TAblE 1: SElECTED DEMOGRAPhy AND hEAlTh INDICATORS IN EThIOPIA
Population 80 million
Health service coverage 90%
Hospital beds/population 1:6,150
Infant mortality rate 67 per 1000
Child mortality rate (<5yr) 124 per 1000
Maternal death rate 7 per 1000
Life expectancy at birth 56
Source: Ethiopian Ministry of Health6
TAblE 2A: ADDIS AbAbA EMERGENCy MEDICINE TRAINING WORkShOPS, 1998-2007
year Days of Training
No. of Participants
1998 10 20
1999 5 85
2002 2 40
2003 3 40
2004 10 520
2006 7 70
2007 7 80
In-Depth / EthiopiaID

16 November 2011 // Emergency Physicians International www.epijournal.com 17 16 November 2011 // Emergency Physicians International www.epijournal.com 17
university, Army and police hospitals). Since then, there have been several workshops aimed at improving initial triage and treatment.
In Ethiopia, in some hospitals, general practitio-ners, nurses and /or residents affiliated to the univer-sity manage the emergency units. Undergraduate and postgraduate physician, nurse and other health care provider training lacks EM content. Physician train-ing related to emergency medicine focuses on making the right diagnosis — not the principles of triage and emergency management. This does not prepare Ethio-pia’s doctors for emergency department care where the most pressing requirement is sorting sick patients, and making appropriate triage and treatment decisions.
What Has Been Achieved So Far — What Challenges Lie Ahead
In 1993, work to develop an Ethiopian EM sys-tem got underway, thanks to the local emergency medicine advocacy and the international community. The advocacy group faced many challenges, from getting buy-in from health care professionals to the high turnover among EM policy makers to the lack of acute care space in hospitals. But despite the chal-lenges, great progress were made from 1993 to 2007.The country’s medical community embraced the EM concept and built on the foundation started in 1993. In 2001, AAHB, in collaboration with the World Health Organization (WHO) partnered with the peo-ple involved in the EM initiatives, instituted a trauma registry system in the emergency departments of six hospitals in Addis Ababa documenting close to 10,000 injury related emergency visits in one year. Given that injuries account for a quarter of outpatient ED visits, the pilot data collection demonstrated the feasibility of establishing such a system in hospitals. For several years, the Ethiopia North American Health Profes-sional Association (ENAHPA) has engaged in dia-logue with all stakeholders helping to develop emer-gency medicine infrastructure. In 2006, ENAHPA and the Addis Ababa Health Bureau organized and hosted an international stakeholders meeting in Addis Ababa with the goal of improving emergency medi-cine. Representatives from a cross-section of Ethiopian society, from local women’s groups to the WHO to the Clinton Foundation, attended the meeting. In addition to allowing interested parties to define their priorities and assets for developing a viable emergency medicine system in Ethiopia, it laid the basis for future collaborations.
Also in 2006, Canadian and American universities’ faculties of emergency medicine and volunteer aca-demic staff launched CME sessions in collaboration with the Ethiopian Medical Association (EMA). Since then, there have been large annual symposia, including an international EM symposium which was organized by the EMA and hosted physicians from Canada, the United States, Uganda, South Africa and Ethiopia. To date, over 600 Ethiopian physicians and nurses have attended EM symposia focused on leadership, pre-hospital care, basic and advanced life support, and the evaluation and treatment of minor and major trauma. These events also provided opportunities for attend-
ees to increase their awareness of Ethiopia’s need for emergency medicine. In addition to these national level symposia, there have been multiple CME initia-tives which have focused on the transfer of appropri-ate technologies and updates in scientific and medical advances.
These efforts provided key building blocks to estab-lish an EM infrastructure in Ethiopia, specifically:
1 Increased awareness among the Federal Ministry of Health, leaders in medical education and safety
agencies such as fire departments, the Addis Ababa Red Cross and others about the need for an Ethiopian Emergency Medicine infrastructure;
2 A team of consultants were engaged in developing the National Injury & disability plan and strategy
for the ministry of health in Ethiopia in which a work-ing document was submitted to the Federal Ministry of Health for approval.
3The completion of physical modifications at a few hospitals to accommodate room for critical ill or
injured patients in ER;
4Publication of what has been accomplished to share findings with EM professionals in other
countries;
5Initiation of CME programs in emergency medi-cine; and
6 Launching of an EM residency program in AAUMF.
Ongoing efforts include:
1High-level support from MOH: Multiple pro-grams led by Ethiopia’s Ministry of Health to de-
velop a national EM system under the auspices of a high-level task force that oversees and coordinates all of Ethiopia’s EM activities.
2Establishment of specialized training programs. Ethiopian physicians and other health care provid-
ers, physicians and hospitals from around the world (including Canada) have donated teaching materials and medical equipment. One result of these gener-ous donations has been the establishment of an ultra-sound-training program at St. Paul’s Hospital in Addis Ababa, Ethiopia. Engineers from Canada travelled to Ethiopia to install the equipment, troubleshoot and provide staff training.
3Public private partnership: The establishment of a local public-private partnership between St. Paul’s
General Specialized Hospital and Ayder Referral Hos-pital which uses international support to train nurses in triage processes and protocols. Development of a paramedic-training program is underway, focusing on specific training and protocols, equipment, supplies and first responder skills.
Discussion
Future planning is the essential first step in any emergency system development. All core stakeholders in Addis Ababa must unanimously agree on primary definitions, as well as on the ultimate desired goals to be attained. Ideally, this task group would be target-ing goals for 5 and 10 years into the future. Once the definitions and goals have been established, all other stakeholders that may potentially be impacted should be included in the next round of discussions to allow adequate time for their systems and services to adapt to the changes the emergency medicine project will impact. Ideally these types of discussions and consen-sus agreements would occur before starting the system change process.
There needs to be a general agreement about how EM will be defined and what its scope will be in Ethio-pia. The Ethiopian model, while based on the same principles of emergency medicine utilized around the world, will have to be customized to its culture, its geography and its resources. No other national model should be simply “dropped into place”. The Interna-tional Federation for Emergency Medicine (IFEM) has developed basic definitions for emergency medi-cine, emergency physician, emergency nurse, EMS, etc. Those definitions might act as a useful starting point for Ethiopia to define its own terms and scope.
It is reasonable to recognize that some initiatives must take place while this vision and future plan is be-ing developed. Also some steps already underway may require redirection or reconsideration. These include:1) Integration of pre-hospital care system. All core stakeholders in pre-hospital response, specially the Ad-dis Ababa Red Cross, fire and Emergency department, Police/traffic and hospital-based ambulance services should discuses and integrate their response efforts.
CLAriTy oF ViSioN
Ethiopia needs a clear vision, an overall strategy and an action plan for develop-ing sustainable EM. The action plan must include:
+ Disaster planning and care, and strategies for developing strong public/private partnerships to integrate biomedical engineering and research and telemedicine evaluation and quality assurance+ Developing a pre-hospital care policy+ Identifying the leading agency+ Mandating the assignment of a medical director for pre-hospital care.+ Assess and upgrade existing resources (emergency rooms, ambulances and communication system).
+ New and renovated hospital architectural designs must be accessible to EM.+ Reduce the brain drain of its physicians and other health care providers trained in Ethiopia and other African countries.+ A sustainable EM system requires broad, long-term financing, in addition to the (most welcome) special project funding.+ Ethiopia’s predominantly poor, rural population must have access to EM care.+ Developing and sustaining an effective EM system requires the participation and involvement of Ethio-pia’s communities and all of its citizens.+ Developing/delivering EM education and training requires books, teaching and training modules and materials in Amharic, Ethiopia’s national language.

18 November 2011 // Emergency Physicians International www.epijournal.com 19 18 November 2011 // Emergency Physicians International www.epijournal.com 19
YOUR PATIENTS ARE ON THE CUTTING EDGE...ARE YOU? T-RING ADVANTAGES:
IMMEDIATELY STOPS BLEEDING, PROVIDING IDEAL WOUND VISUALIZATION
ONLY METHOD THAT APPLIES A SAFE, RELIABLE PRESSURE EVERY TIME!
HIGHLY VISIBLE—IMPOSSIBLE TO ACCIDENTALLY FORGET ON THE DIGIT
MINIMIZES THE RISKS ASSOCIATED WITH OTHER DIGITAL TOURNIQUETS
FASTER, EASIER AND SAFER TO USE THAN ALL OTHER METHODS!
“ONE SIZE FITS ALL!”
“BLOODLESS EXPLORATION THROUGH CAREFUL TOURNIQUET APPLICATION IS
“CRITICAL” TO MINIMIZE RISK!” (ACEP’s Emergency and Primary Care of the hand).
"A CONSPICUOUS TOURNIQUET THAT APPLIES THE LOWEST PRESSURE NECESSARY
TO ACHIEVE HEMOSTASIS MUST BE USED!" (Lahham, WJEM Nov 2010)
“THE WORLD’S FASTEST, SAFEST AND MOST EFFECTIVE FINGER TOURNIQUET!”
CONTACT: PRECISION MEDICAL DEVICES
(302) 778-2335
FOR MORE PRODUCT INFORMATION
WWW.THETRING.COM
There are essentially no ambulances; the ambulances that are in place lack even basic equipment and trained personnel. Those who have completed training of-ten leave. A well developed EMS system with a centralized dispatch system (for each region) and a well publicized and coordinated public education campaign are required. This system should start in all major cities at the same time if pos-sible. This will require establishment of a well-structured maintenance base for the ambulances (and the equipment within), training of personnel and develop-ment of a coordinated public campaign. Oversight should be by a FMOH to ensure standardization, with municipal or regional personnel administering to their local needs.2) Building of standardized emergency departments or modification of exist-ing emergency rooms should have complied with the basic physical constructs of ED such as spacing, ergonomics, personnel and equipment proportional to anticipated needs over the following 5-10 years. No such active site yet exists in Ethiopia, which allows time for a standardized approach to be established. The current physical plant of Addis Ababa hospitals should not be considered a model to be emulated. Restructuring of hospital systems will be required as it is recognized that the large majority3) Multiple ancillary services will have to be structured and available in the ED: social work to allow patients to be discharged with home support, commu-nity nurses who could arrange home care rather than admission, physiotherapists to assess patients requiring outpatient care, etc.4) Sites to lead emergency medicine development should be identified. In the development of emergency medicine, a very distinct pattern became evident. Well-established bastions of medicine with well-deserved international reputa-tions were often the least willing to embrace emergency medicine residency pro-grams. Many felt that their current system was effective; others resisted because of specialists who refused to accept change. The primary reason however seemed to be the inertia of large medical centers to major change. Medicine is a naturally conservative domain; change only occurs with evidence that patient well being is not at risk. It has been shown that on average, implementation of new knowledge requires 10-12 years after proof of that new knowledge’s efficacy. It thus occurred that most of the new programs in emergency medicine opened in newer, more flexible universities and hospitals. It may well be easier to have the first full emer-gency medicine systems (EMS, emergency department, full hospital integration and residency program) set up in smaller, younger centres such as in Debub, Mekelle or Bahirdar Universities. In such new facilities there is more openness to change that is not inherent in longer established hospitals. Furthermore, the ex-haustive changes required will be economically less prohibitive in a smaller region than in well-established universities; unanticipated errors or consequences that occur during the process could be rectified with less cost. When bigger centers start their programs, it will be with the experience of other, smaller sites so that implementation will occur with much less risk for error and with more experience than is currently happening.
Peter W. Hodkinson has written about the urgent need to determine key strat-egies to help guide EM maturity in the developing world. These strategies must be practical, take into account existing health care systems and allow integration into these systems. There is clear evidence that well-established systems of emer-gency care can reduce morbidity and mortality from many common conditions in the developing world. To build on the progress that Ethiopia and its many partners have achieved, taking EM to the next level will take action in five criti-cal areas:
Conclusion
It is an exciting time for clinicians and other health care providers to be in-volved in fostering EM in Ethiopia through collaboration with local professionals to support CME initiatives and outcome-based research projects. Investing in medical student and resident exchanges is always enriching to everyone involved. In our highly interconnected world, everyone can benefit from transglobal con-versations and idea exchange. Ethiopia and other nations that do not have mature
In-Depth / EthiopiaID
continued on page 21

18 November 2011 // Emergency Physicians International www.epijournal.com 19 18 November 2011 // Emergency Physicians International www.epijournal.com 19
gLOBALIFEM FellowshipFocus: GlobalContact: Peter Cameron, [email protected]
AUsTRALiA/ NEw zEALANdAustralasian College of Emergency Medicine (ACEM)Focus: Global, Australia, NZ & South PacificContact: Peter Cameron, [email protected] Gerard [email protected]
CANAdAUniversity of Toronto / Canadian Association of Emergency Physicians (CAEP)Focus: Global, AfricaContact: Valerie [email protected]
MExiCOPACE Global FellowshipFocus: Latin AmericaContact: Haywood Hall, MDCinco de Mayo, # 11San Miguel de Allende,Guanajuato Mexicolength: 1-2 yearsSalary: CompetitiveShifts: FlexibleDegree: Independent MPH encouragedPositions: 4Deadline: January 15( (800) 770-68538 [email protected]: www.pacemd.org
THE NETHERLANdsThe NVShA (Dutch Society for Emergency Medicine)Contact Dr. Pieter van [email protected]: 1 to 2 yearsNumber of positions: 1 or 2Degrees: Subspecialty/Fellowship
Status in Dutch EM SystemDeadline: Rolling. Currently open only to Dutch EPs( +31 624 11 3566: nvsha.nl
sOUTH AfRiCASouth Africa: Univ. Cape Town / Stellenbosch Univ. / EM Society of South Africa (EMSSA)Focus: Africa, South AfricaContact: Lee Wallis, [email protected]
THE UNiTEd sTATEsCalifornia harbor-UClA/IMC Global health FellowshipFocus: Iraq, Haiti, otherContact: Ross I. Donaldson, MD, MPH, Harbor-UCLA Medical Center Department of EM1000 West Carson Street, Box 21Torrance, CA 90509length: 1-2 yearsSalary: Very CompetitiveShifts: 5 per monthDegree: MPH, DTMH availablePositions: 1-2Deadline: November 1( (310) 222-3500 [email protected]:www.emedharbor.edu/Global.html:internationalmedicalcorps.org keck School of Medicine at USCFocus: Chile, Ghana, Mumbai, Thai-Myanmar border, British GuyanaContact: Billy Mallon, MDDepartment of EM1200 North State StreetRoom 1011Los Angeles, CA 90033Fax: (323) 226-6454length: 1-2 yearsSalary: CompetitiveShifts per week: 2Degree: MPH, DTMHPositions: 1Deadline: December 1( (323) 226-66678 [email protected]: www.cbooth.info
loma linda UniversityFocus: Vietnam, China, and KenyaContact: Debbie Washke, MDDepartment of EM11234 Anderson St,. RM A108Loma Linda, CA 92354Fax: (909) 558-0121length: 1-2 yearsSalary: About $80,000Degree: MPH with 2-year programPositions: 1Deadline: March 1( (909) 824-43448 [email protected]
Stanford International Emergency Medicine FellowshipContact: S.V. Mahadevan and Matthew StrehlowStanford University701 Welch Rd. Bldg CPalo Alto, CA 94304Fax: 650 723-0121length: 1-2 yearsPositions: 1-2Salary: Please contacthours per week: approx. 15Degree: MPH possible for 2 yr candidateDeadline: ACEP Scientific Assembly( (650) 723-00638 [email protected]: emed.stanford.edu/fellowships/international.html
UClA-CIM International Medicine FellowshipContact: Nicole Durden, UCLA Medical Center Dept. of EM924 Westwood Blvd., Ste 300 Los Angeles, CA 90024length: 1-2 yearsSalary: CompetitiveShifts: 5 per month Degree: MPH, PhD Positions: 1Deadline: October 15( (310) [email protected]:http://cim.ucla.edu
ConneCtiCut yale University School of MedicineFocus: AfricaContact: Simon Kotlyar, MDDepartment of EM464 Congress Ave, Suite 260New Haven, CT 06519-1315Fax: 203-785-4580
length: 2 yearsPositions: 1 Salary: PGY level, MSc tuition, travel stipend, excellent benefitsShifts/hours per week: 0.5 FTEDegree: MS, London School of Hygiene and Tropical MedicineDeadline: December 1( (203) [email protected] :medicine.yale.edu/emergencymed/fellowships/global/index.aspx
Delaware Christiana Care health SystemFocus: AfricaContact: Susan E. Thompson, DOChristiana Care Health SystemsDept. of EM Administration4755 Ogletown-Stanton Road Newark, DE 19718length: 1 – 2 yearsShifts: Between two and three 8- or 9-hour shifts/weekDegree: MPH with 2-year programDeadline: November 15( (302) [email protected]
washington D.C. George Washington UniversityFocus: India, Malawi, Egypt, El Salvador, Ethiopia, Peru Contact: Kate Douglass, MD, MPH 2150 Pennsylvania Avenue, NW, 2B-417, Washington, DC 20037Fax: (202) 741-2921length: 2 years (1 year possible under special circumstances)Salary: Highly competitive, MPH tuition and generous CMEDegree: MPH Positions: 1-2Deadline: November 15((202) 741-2954 [email protected]:www.gwemediem.com
floriDa University of Florida College of Medicine - JacksonvilleContact: Elizabeth DeVos MD, MPH Department of EM 655 W 8th St Jacksonville, FL 32209
The IEM Fellowship Directory

20 November 2011 // Emergency Physicians International www.epijournal.com 21 20 November 2011 // Emergency Physicians International www.epijournal.com 21
Deadline: Check with department ((904) [email protected]
georgia Emory University Contact: Scott Sasser, MD Department of EM 531 Asbury Circle - Annex Suite N - 340 Atlanta, GA 30322 Fax: 404-778-2630 length: 2 years Positions: 1 Salary: Instructor Deadline: Check with department ((404) [email protected] Medical College of GeorgiaFocus: Peru, BangkokContact: Hartmut Gross, MD 1120 15th StreetAugusta, Georgia 30912Fax: (706) 721-7718length: 1 yearSalary: Competitive salary, benefits, CME, int’l travel fundsShifts per month: half-time EM clinical faculty positionDegree: NonePositions: 1( (706) 721-4412 [email protected]:www.mcg.edu/ems/residency/internationalMedFellow.htm
illinois Cook County hospitalContact: Jamil Bayram, MD & Robert Simon, MDCook County Hospital, Rush University Medical CenterDept. of EM1653 W. Congress Parkway, 177 MurdockChicago, IL 60612Fax: (312) 942-4021 length: 2 years (with MPH)Salary: Very competitive, benefits, tuition fees for the MPH, travel expenses and stipendsPositions: 1- 2Deadline: Open( (312) 942-49788 [email protected]
Univ. of Illinois at ChicagoContact: Janet Lin, MD, MPHDepartment of EM, College of Medicine East Suite 469A808 South Wood StreetChicago, IL 60612length: 2 yearsSalary: N/APositions: 1-2Deadline: Open((312) 413-7393 [email protected]
MarylanD Johns hopkins UniversityContact: Alexander Vu, DO, MPH International Emergency MedicineCenter for Public Health and Human Rights5801 Smith Avenue, Suite 3220Baltimore, MD 21212Fax: (410) 502-8881length: 2 yearsSalary: Competitive Positions: 1-2Degree: MPHDeadline: September 15((410) 735-6436 [email protected]
University of MarylandFocus: China, Egypt, South Africa, Botswana, The NetherlandsContact: Veronica Pei, MD, MPHUniversity of Maryland Department of Emergency Medicine110 S. Paca Street, 6th Floor, Suite 200Baltimore, MD 21201length: 2 yearsSalary: Competitive Positions: 1Degree: MPHDeadline: Open( Phone: (410)328-8025 [email protected]
MassaChusetts harvard University / beth Israel Deaconess Medical CenterContact: Philip D. Anderson, MDDepartment of EMOne Deaconess RoadW/CC -2Boston, MA 02215length: 2 yearsSalary: Competitive, benefits, CME benefits and MPH tuitionPositions: One
Degree: MPH Deadline: December 1( (617) 754-23248 [email protected] harvard University / brigham and Women’s hospitalFocus: VariousContact: Stephanie Rosborough, MD, Department of EM75 Francis StreetBoston, MA 02115length: 2 yearsPositions: OneSalary: Competitive with excellent benefitsShifts/Week: 1-2Degree: MPHDeadline: November 20( (617) 732-58138 [email protected]: www.brighamandwomens.org/dihhp/iem
Minnesota Regions hospitalContact: Matthew Morgan, MDRegions Hospital Department of EM640 Jackson St.St. Paul, MN 55104length: 2 yearsDegree: MS in development policy or certificate in tropical medicine( (651) 254-3336 [email protected]:www.regionsem.org/fellowships/international-medicine
new york bellevue hospital Center/New york University School of MedicineContact: Michael Mojica, MDEmergency Care Institute Room 345A, Bellevue Hospital Center27th Street and First AvenueNew York, NY 10016length: 1 - 2 yearsSalary: CompetitivePositions: 1( (212) 562-8147 [email protected]
kings County hospital/SUNy Downstate College of MedicineContact: Christina Bloem, MDSUNY Downstate Medical Center
Department of EM450 Clarkson AvenueBrooklyn, NY 11203( (718) 245-4790 [email protected]
New york - Presbyterian: The University hospitals of Columbia and CornellFocus: Africa (Uganda, Tanzania, Kenya, Sudan, Ghana, Malawi, Sierra Leone); India, Sri Lanka, Montenegro, Dominican Republic, Burma; WHO in GenevaContact: Rachel T. Moresky, MD, MPHColumbia University Medical Center - Center for EM622 West 168th Street PH 1-137New York, NY 10032length: 2 yearsSalary: CompetitivePositions: 2Degree: MPHDeadline: November 1( (212) 304 [email protected]: www.nypemergency.org/fellowships
North Shore - long Island Jewish health SystemContact: Sassan Naderi, MDDept. of EM270-05 76th AveNew Hyde Park, NY 11040length: 1 yearPositions: 1 - 2Salary: $90,000hours per week: 18Deadline: Rolling ( (718) 470-75018 [email protected] St. luke’s Roosevelt hospital Center - Global health FellowshipFocus: HIV/TB/Tropical Contact: John D. Cahill, MDDept. of EM1111 Amsterdam AvenueNew York, NY 10025length: 2 yearsPositions: 2Salary: $87,000hours per week: 20Degree: MPH optionalDeadline: Rolling ( (212) 523-33308applications@
The IEM Fellowship Directory

20 November 2011 // Emergency Physicians International www.epijournal.com 21 20 November 2011 // Emergency Physicians International www.epijournal.com 21
slredglobalhealth.com: www.slredglobalhealth.comUniversity of Rochester Medical CenterContact: David H. Adler, MDDept. of EM601 Elmwood Avenue, Box 655Rochester, NY 14642length: 2 yearsSalary: $80,000 - $100,000/year depending on clinical time; CME, benefits, 5k/year travelPositions: 1Degree: MPH, clinical investigation, or medical managementDeadline: April 15( (585) 463-2945 8david_adler@ :www.urmc.rochester.edu/emergency-medicine/education/international.cfm north Carolina
Duke International EM Fellowship/Global health Residency ProgramFocuses: East Africa, Casualty department epidemiology, trauma epidemiology research, validation of trauma scoring in resource limited settings Contact: Charles J. Gerardo, MDDuke University, DUMC 3096Durham, NC, 27710length: 2 yearsPositions: 1Salary: Competitive, including tuition for advanced degreeDegree: MS in Global Health (MSc-GH)Deadline: September 24( 919-681-44588 [email protected] : www.dukeglobalhealth.org:globalhealth.duke.edu
oregon
Oregon health & Science University - Global health FellowshipContact: Amy Marr, MDOHSU Dept. of EM3181 SW Sam Jackson Park Road, CDW-EMPortland, OR, 97068length: 2 yearsPositions: 1-2Salary: PGY level, CME allowance, benefitsShifts per week: 1Degree: Master’s or certificate options (tuition support provided)Deadline: Rolling( (503) 494-82208 [email protected]: www.emergencyresidency.com Pennsylvania
University of PittsburghContact: Allan B. Wolfson, MDDept. of EM230 McKee Place, Ste. 500Pittsburgh, PA 15213length: 2 yearsSalary: NegotiableShifts per week: NegotiableDegree: MPH offered from the University of Pittsburgh Graduate School of Public Health( (412) [email protected]: affiliatedresidency. health.pitt.edu
rhoDe islanD
Rhode Island hospitalFocus: Liberia, Rwanda, Uganda, Kenya, and HaitiContact: Lawrence Proano, MDUniversity EM Foundation593 Eddy Street, Providence, RI 02903
length: 2 yearsSalary: $87,500Positions: 1-2hours per Week: 16Degree: MPH from Brown University( (401) [email protected]
tennessee Vanderbilt University International EM FellowshipFocus: South AmericaContact: Seth Wright, MDVanderbilt University703 Oxford HouseNashville, TN, 37232length: 1-2 yearsPositions: 2Salary: $92,000 + excellent benefits, tuition, travel expensesHours per week: 14.75Degree: MPH, DTMHDeadline: Rolling( (615) [email protected]: emergencymedicine.mc.vanderbilt.edu
texas
baylor College of Medicine / Texas Children’s hospital Focus: VariousContact: Charles G. Macias, MD, MPH Texas Children’s Hospital 6621 Fannin, MC 1-1481 Houston, TX, 77030 length: 4 years (pediatrics trained); 3 years (EM trained) with Board eligibility in PEM at completion Salary: PGY level Positions: 1 hours per week: 32-40 Conferences/week: 4 hours, except PICU rotationDegrees: MPH, MEd, MS, MBA
Deadline: August 31 through ERAS (apply for PEM Fellowship)( (832) 824-54688pwomack@:texaschildrenshospital.org
University of Texas Southwestern (Dallas-Parkland)Focus: Mexico/Latin America. Others negotiable.Contact: Robert E. Suter, DO, MHADiv. Emergency MedicineUT Southwestern Medical Center at Dallas5323 Harry Hines Boulevard CS2.122Dallas, TX, 75390-8579length: 2 years Salary: CompetitivePositions: 4 hours: 56 clinical hours/monthDegrees: MPH Deadline: December 1( (214) [email protected]
utah
University of Utah Focus: Ghana, Thailand, India, Peru Contact: Erik Barton, MD, MS, MBAUniversity of Utah Health Care30 North 1900 East, Rm 1C26Salt Lake City, UT 84132length: 1 to 2 yearsSalary: competitivePositions: 1 or 2Shifts: 7 per month/54 hoursDegrees: MPHDeadline: Rolling( (801) [email protected]
The IEM Fellowship Directory
EM systems can be helped to develop the surveillance research infrastructure they need to deal with emerg-ing infections and strengthen global health security. In a recent article in the Canadian Family Physicians Journal, titled “Motivating Action: Why Canadian Physicians Should Participate in Research, Education
and Patient Care in Developing Countries”22, Pro-fessor Peter A. Singer describes the scientific oppor-tunities, compelling economic reasons, bio-security considerations, human capital and peace and develop-ment issues that are pragmatic, motivating factors for physician participation.
As a new specialty, international emergency medi-
cine can make inroads to build capacity in Ethiopia. There is a great opportunity to transfer knowledge, provide research capacity, help with needs assessment and develop a model of relationship between aca-demia, business and the international Ethiopian pro-fessional diaspora. Together, all can work closely and achieve mutual benefits.
In-Depth / Ethiopia
continued from page 18

22 November 2011 // Emergency Physicians International22 November 2011 // Emergency Physicians International
OSometimes it feels like we are investigating and treating patients who have
an inevitable outcome, in spite of our best endeavors. There is a conveyer belt of humanity that we “tinker” with as it passes through the emergency department. Many patients will recover, some will die, a small number re-quire immediate life-saving interventions and some require relief of pain or discomfort. Significantly, there are some patients who would benefit from avoiding the ED altogether and don’t fit neatly into our disease and symptom based protocols.
Does emergency medicine add value to the conveyer belt? Are we provid-ing a service that helps society? There is increasing demand across emergency systems internationally and little chance of this changing in the foreseeable future. Projections from some regions predict that if present demand trends continue, more than 50% of GDP could be consumed by provision of health-care by mid century. Clearly the main drivers for this inexorable demand must be identified and strategies developed to manage it.
In emergency medicine, we have been held captive by the need to deliver more “efficient care”, in order to provide high level services within present budgetary constraints. Politicians and administrators have been more com-fortable with the idea of improving “efficiency” as opposed to questioning the drivers of increased demand. There has been little dialogue with the com-munity on what it expects from money spent on health care and what is the highest priority for health care spending. The closest to a debate occurred when “Obama death panels” were demonized in the popular press in the USA (the Obama administration suggested that some patients might be better off not receiving high technology/high cost care).
As an emergency doctor I have real concerns regarding increased “effi-ciency” and the possible impairment of effective delivery of “good emergency care” in my ED. Using process mapping, lean thinking and various other or-ganizational review techniques, many EDs have “improved efficiency”. For ex-ample, early ordering of X-Rays – even from triage, direct admission to wards for “obvious admissions”, immediate pain relief for patients presenting with pain. All of these procedures may ultimately result in faster transition through the ED. However, do such initiatives ultimately result in greater efficiencies in the health system? More importantly, do they improve the experience for patients and deliver lower costs across the whole episode of care?
Elderly patients, with undifferentiated illness are particularly susceptible to disadvantage in the “efficient” emergency system model. For example, an elderly frail man inadvertently takes a double dose of sedative because his wife is out of the house, playing cards. This patient falls in his house, is heard by the neighbor, an ambulance is called and he is brought to the ED for assess-ment. It is night, the LMO is not available, the wife hasn’t yet returned from her outing, the patient is confused because of the tablets – and gets more con-
fused because he has been taken from his home. This patient can’t go home from the ED, so he is admitted quickly to the ward for his acute confusional state within a couple of hours of arrival (efficient). He has had blood tests, CT brain and X-rays (all normal). His disorientation and confusion worsens, he wanders at night, falls again and fractures his NOF and spends weeks in hospital, never truly returning to his premorbid state. The end result is nurs-ing home or death.
Variations on this story occur on a daily basis in hospitals around the globe. The measured care is extremely efficient, times are met, illnesses are treated, but the whole hospital episode is probably preventable.
A further issue is the problem of determining a good outcome. Survival is not the most important outcome for many patients. For example, those patients (or their carers), with terminal illness, advanced dementia or debili-tating illness, might regard death as preferable to being taken by ambulance to a hospital, especially when good nursing care and a comfortable environ-ment can be provided in their residential care institution – or with support from their families. If a demented elderly patient in a nursing home falls and has a head injury in my country, it is highly likely that they will be taken by ambulance to hospital, in a cervical collar and assessed in the ED. The col-lar may be left on for hours to days, as the imaging and clinical situation are difficult to assess. They will receive a CT and sometimes even get admitted to hospital. The resultant discomfort to the patient, the futility of any surgi-cal treatment, possible harm caused by immobilization and assessment and the distress of the relatives are rarely assessed in a balanced way. There seems little consensus amongst my emergency colleagues and even less amongst my inpatient colleagues about the best management plan for this situation. If the patient and family were fully informed of the advantages and disadvantages of conservative versus active management it is likely that most would chose to leave the patient in the residential care or community setting – provided there was adequate support.
From the perspective of measured efficiency, the emergency system can whisk the patient quickly to hospital, get scans and into a medical ward within hours. Alternatively, an experienced clinician could assess the situation at a nursing home, discuss with relatives and usual doctor and keep the patient in their usual surroundings. Which is better for the patient? What is best for the system?
As EPs, we have a duty to develop the emergency system to do what is right for the patient. We are in a position to inform the community and patients of relative risks and likely outcomes. Much of the “conveyer belt” of incoming patient load could be prevented by better community structures and more informed discussions with patients and relatives in the ED. Spending time developing community processes, links and educating the community is not seen as “efficient care”. Fully assessing patients and their complicated social/psychological situations in the ED may look like “wasted time” from an ED process improvement model. However from a societal perspective it is essen-tial for efficient use of the hospital system and to ensure appropriate use of scarce resources.
Dr. Cameron is the president of the International Federation for Emergency Medicine (IFEM)
The Problem with “Efficient” Medicine Doing the right thing for the patient often means slowing down care and assessing the big picture.
One day as I watched the relentless line of am-bulance trolleys coming through the front door and the slow pace of patients leaving the emer-gency department, I reflected on exactly what I was trying to achieve in my chosen profession of emergency medicine.
Grand Rounds With Peter caMeroN, MD

22 November 2011 // Emergency Physicians International22 November 2011 // Emergency Physicians International
The Global Emergency Medicine Initiative: Building a Global Emergency Medicine Network for Comprehensive Acute Care Systems Development
National and Independent Responses to Trends in EM
EM and acute care systems are growing in over 50 countries. Over the past 40 years, emergency medicine specialists, EM societies, federations and emergency health professionals have assisted in establishing:
u Training programs for EM physicians and specialists
u Schools for emergency nursing, medics and paramedics
u Professional societies for EM specialists
u Disaster medicine and disaster management programs
u Trauma systems and trauma training programs
u Ambulance and pre-hospital systems
u Injury and acute disease surveillance systems
u Global and National research programs
DEVElOPING SUCCESSFUl NATIONAl AND INDEPENDENT RESPONSES INTO A GlObAl COOPERATIVE. Emergency physicians and EM Societies who are engaged in EM development are now seeking to create larger, more comprehensive partnerships and networks in order to build more comprehensive EM and acute care systems on a national and regional scale.
The Need for Emergency Medicine and Acute Care Systems is a Global Crisis
Emergency medicine and acute care systems are in demand in every country in the world, yet most systems are vastly under-staffed, under-resourced, under-funded and under-developed.
The Global Emergency Medicine Initiative (GEMI) will address this need by creating a Global Emergency Medicine Network, which will link together and create the multilevel, multi-professional, multi-dimensional partnerships – EM societies, governments, NGOs, universities and private investors & corporations – that are necessary for comprehensive emergency medicine and acute care systems development.
Through the Global EM Network, GEMI will focus on key areas of emergency medicine and acute care systems development in order to provide expertise and development in all aspects of EM and AC systems development:
u Education
u Service
u Research
u Systems development
“Cancer, diabetes, and heart diseases are no longer the diseases of the wealthy. Today, they hamper the people and the economies of the poorest populations even more than infectious diseases. This represents a public health emergency in slow motion.”-United Nations Secretary-General ban ki-moon, addressing the UN high-level meeting on NCD’s, Sept 19-20, 2011

CANCERS
ISCHAEMIC HD
STROKE
ACUTE RESPIRATORY INFECTIONS
2005 2010 2015 2020 2025 2030
0
2
4
6
8
10
1
TUBERCULOSISMALARIA
HIV/AIDSPERINATALROAD TRAFFIC ACCIDENTS
DE
AT
HS
IN
MIL
LIO
NS
The New Global Burden of DiseaseNon-communicable diseases are a giant wave approaching in global public health. For the first time in history, non-communicable diseases (NCDs) have surpassed traditional communicable diseases as the major global causes of death and disability. And not just in more developed nations–this has happened all over the world, in nearly every country.
Why the monumental shift? The world is changing in unprecedented ways:
1The Aging of the Population: Fewer deaths from increased life expec-tancy and decreased childhood mortality now allow people to survive
to older ages, exposing them to different disease patterns. There is now also a greater percentage of people older than 60 than at any other time in history. In a few decades, the majority of older people will no longer live in the developed world, but instead will live in underdeveloped areas with less developed health care systems.
2Increased Urbanization: As of 2006, for the first time in recorded his-tory, the majority of the world’s population lives in cities. This has never
happened before. Urban life brings key changes in diet, exercise, work, life-style, and new disease patterns
3Globalization of Trade and Marketing: There has been a progressive increase in unhealthy lifestyle patterns (tobacco use, diet, physical
inactivity and the harmful use of alcohol), and new disease pat-terns with them.
Global health policy makers are starting to recognize that emergency medicine systems will be the next major health-care concentration along with primary care. The developing world is starting to recognize that treatment for noncom-municable diseases in a communicable disease setting is becoming increas-ingly expensive and inefficient.
Trauma, cardiovascular disease, cancer, diabetes and lung disease now account for 63 percent of all deaths in the world.
According to WhO studies, the forces of demo-graphic and epi-demiologic shift have elevated non-communica-ble diseases to be the single largest cause of morbid-ity and mortality worldwide, now and increasingly into the future.

CANCERS
ISCHAEMIC HD
STROKE
ACUTE RESPIRATORY INFECTIONS
2005 2010 2015 2020 2025 2030
0
2
4
6
8
10
1
TUBERCULOSISMALARIA
HIV/AIDSPERINATALROAD TRAFFIC ACCIDENTS
DE
AT
HS
IN
MIL
LIO
NS
Q: What can meet this new NCD burden? A: Emergency Medicine and Acute Care Systems Development
What makes this shift in morbidity and mortality so important?
20th Century healthcare initiatives focused on healthcare provision for communicable diseases in outpatient and inpatient settings. The greatest 21st Century healthcare burden will be healthcare provision for non-commu-nicable diseases.
The rise of NCDs have and will continue to affect all populations of all countries. NCDs are already the largest causes of death and disability in low- and middle-income coun-tries; they are increasing more rapidly than previously expected and in precisely those areas with the least developed EM and acute care systems.
“The prognosis is grim. NCDs hit the poor and vul-nerable particularly hard, and drive them deeper into poverty. According to the WHO, deaths from NCDs will increase by 17 % in the next decade. In Africa, that number will jump by 24%”-un secretary general ban ki-moon
Without global strategic emergency medicine integration with existing healthcare facilities, the costs of healthcare provision for non-communicable diseases on a communicable disease setting will grow exponentially.
Emergency medicine and acute care systems focus on bringing the right care to the right people at the right time. It combines specialized training with skills in health care triage, management and efficiency, to form a safety net of emergency medical preparedness and secondary prevention for entire popula-tions, and results in lower NCD burden, greater access, greater quality and lower costs.
What Is Emergency Medicine?
“EM is a fully-developed medical specialty that focuses on recognition, stabilization and treatment of all emergency conditions for people of all ages. Sometimes called the ‘spe-cialty of time,’ the full practice of EM involves education, training, practice, research and systems development. EM is a combination of proper medical education care and proper systems design and management, in order to deliver medical care to the people who need it most.” -terry mulligan, do, mph // emergency physician
“EM development has universal appeal across the globe because it is the key to more effi-cient and accessible care in developed countries and in LMICs it is the key to basic health-care that is a human right for every citizen.” -peter cameron, md // president of the international federation for emergency medicine
1965 1970 1975 1980 1985 1990 1995 2000 2005 2010
40
35
30
25
20
15
10
5
# o
F c
oU
Nt
rie
SThe Number of CouNTrieS
wiTh emergeNCy
mediCiNe
While EM is still one of the youngest medical
specialties in the world, it is an officially recog-nized medical specialty
in over 50 countries, with the rate of specialty rec-ognition accelerating in
recent years .

How To Build Emergency Medicine & Acute Care Systems
Emergency medicine and acute care systems devel-opment involves more than just medical training for health care professionals. It requires simultaneous and coordinated development in multiple disciplines and in multiple stages.
Over the past 20 years, many EM societies, depart-ments and training programs have responded to this need for international EM development. The result has been the creation and growth of the field of international emergency medicine (IEM), which is concerned with the development of EM and acute care systems in countries and regions where EM is lacking and is needed.
IEM can be viewed as a natural extension of the systems-based nature of EM: it allows EPs and other health professionals who are involved in emergency medical care to learn from each other, and involves the educating and training of emergency care provid-ers throughout the world in practice, education, re-search and systems development.
Interest in IEM has also led to the development of IEM fellowships, subspecialty training programs and other educational projects for EPs and allied health-care professionals. Formal and informal international / global EM fellowships and training programs now exist in at least five countries.
Further, the International Federation for Emergency Medicine (IFEM) has emerged as the peak emergency medicine organization in the world, representing over 70 EM Societies from over 50 countries.
“International EM fellowships and training programs are designed as adjuncts to EM residencies and specialty training initiatives, which promote the clinical and non-clinical expertise that is needed for EM practice, and include training on how to support the creation, develop-ment and maturation of EM/acute care systems in other countries.”t mulligan, chobgood, pcameron. emergency medicine australasia (2011) 23, 525–529
This multi-level, multi-professional, multi-disciplinary and multi-institutional approach ensures successful medical development and health system strengthening, and ensures program longevity, sustainability, resilience and self-generation.-T. Mulligan & L. Wallis
bringing together multiple partners to build emergency medicine
International emergency medicine organizations understand the complex nature of emergency medicine and acute care systems. GEMI will construct the Global EM Network, which will provide expertise and assistance with all levels of EM and AC systems development. Many parties, organizations and individuals are currently working in international EM development all around the world: EM Societies and Federations, universities, NGOs, gov-ernments, corporations and private investors. GEMI was founded by mem-bers of these organizations, and brings together the multiple disciplines necessary to build EM systems: medicine, nursing, management, econo-mists, legislators, health policy makers, public health experts, corporations and businesses and private investors.
Bringing together the world’s experts at all levels of EM and AC education, research, service and systems development, GEMI will embody one unique organization that will build comprehensive EM systems on a national or regional scale.
TERTIARY STAGES
Public Health AgendasNational Health PolicyLegislative Structure
STAGES OF EMERGENCY
MEDICINE DEVELOPMENT
PRIMARY STAGESSpecialy Systems
Academic DevelopmentEducational SystemsPatient-care Systems
SECONDARY STAGESEconomic & Finance
Administratice & Management Systems
Local Variations
Training Programs for existing physicians and specialists Midwives, nursing, advanced health care workers
Pre-hospital and First Responder Training for Medics, Fire, Police, TaxiBasic First Aid and Community Health Workers
Basic Public Health Services
Emer
genc
y C
are
Syst
em
Basi
c Acu
te C
are
Emer
genc
y M
edic
ine
TERTIARY STAGES
Public Health AgendasNational Health PolicyLegislative Structure
STAGES OF EMERGENCY
MEDICINE DEVELOPMENT
PRIMARY STAGESSpecialy Systems
Academic DevelopmentEducational SystemsPatient-care Systems
SECONDARY STAGESEconomic & Finance
Administratice & Management Systems
Local Variations
Training Programs for existing physicians and specialists Midwives, nursing, advanced health care workers
Pre-hospital and First Responder Training for Medics, Fire, Police, TaxiBasic First Aid and Community Health Workers
Basic Public Health Services
Emer
genc
y C
are
Syst
em
Basi
c Acu
te C
are
Emer
genc
y M
edic
ine

The Global Emergency Medicine Initiative Supporting emergency medicine across the globe
IFEM
Private Investors
EM Societies
Foundations
Governments
Health Ministries
Universities
First Steps:
1Establish the Global EM Network by bringing together the many partners playing a found-
ing, directing role: interested Universities, gov-ernments, NGOs, professional societies, and private businesses.
2Establish GEMI and local Global Health and EM Institutes to offer educational courses,
certificates and degrees in all aspects of EM systems development:
3Link existing Global Health and EM Institutes to establish local, national and international
networks of GH institutes, to share resources, local knowledge and to multiply regional impact
4Continue to expand to establish GEMI as the first, go-to organization for comprehensive
EM education, research, service and systems development.
How Will GEMI Build EM Systems?
GEMI realizes that all change starts with education. GEMI will focus on EM systems development through the establishment of local Glob-al Health and EM Institutes abroad, dedicated to teaching, research, service and systems development in all levels of EM development.
Focusing on the “teach-the-teacher” philosophy, these local Global Health and EM Institutes will use a combination of on-site and on-line teaching modalities, including the best on-site teaching faculty and curricula, and the best available e-learning and distance education technologies. Courses, certificates and degrees will be available in all levels of the EM Development Pyramid—clinical and academic EM, EM administration and management, EM finance and economics, EM
legislation, and EM health policy and public health. Through these linked Institutes, GEMI will provide educa-
tion, training, research and consultation in all aspects of EM and acute care systems development, including:
Training for community health workers, mid-wives, nurses, paramedics and other health professionals
Clinical and non-clinical emergency medicine training for medical students, residents/registrars, physicians and other health professionals
Health administration and management in EM
Patient Safety and quality improvement
Health economics and finance for EM and AC systems
Legislative and health law agendas for EM development
Public health and health policy programs and agendas for EM development
GEMI: U
nifying the Emergency Medicine Network
GEMI will rapidly become the leading provider of national
and international emergency medicine and acute care train-
ing, consulting and service, and will emerge as the thought
leader and the resource of first choice for anyone seeking com-
prehensive, lasting solutions for emergency medicine, acute care
and other medical system needs.

Jeffrey Arnold, MDSanta Clara Valley Hospital, USA / California Emergency Physicians
Arif Alper Cevik MDEskisehir Osmangazi University
Medical Center, Turkey / Emergency Medicine Association of Turkey
Timothy Rainer MDChinese University of Hong Kong
Gerard O’Reilly MDMonash University, Australia
Juliusz Jakubaszko MD, PhDWroclaw University / President, Polish
Society of EM
Tamara Thomas MDLoma Linda University, USA
kumar Alagappan MDNorth Shore Long Island Jewish
Hospital, USA
Sassan Naderi MDNorth Shore Long Island Jewish
Hospital, USA
Colin Graham MDChinese University of Hong Kong
Manny hernandez MD, MbACannon Design, USA
Maaret Castren MD, PhDKarolinska Institutet, Sweden
Silvio Aguilera MDBuenos Aires, Argentina
David Sheehan, JDThomas and Libowitz Law Firm, USA
David hegstadOAO Mohn and Allen CPAs, USA
Matthew GraciePNC Bank, USA
Robert AlexanderCorporate Press, USA
logan PlasterPublisher, Emergency Physicians
International, USA
GEMI, the Global EM Network and partnerships of EM Societies, EM Federations, universities, NGO’s, governments, corporations and other organizations will work to bring emergency medicine to the world on a global scale.
GEMI will enable multi-lateral cooperation and synergies that will broaden the scope of current EM clinical, educational and research efforts, and will establish EM as the active agent for solutions for non-communicable disease burden, EM and acute care systems development.
By helping to build EM and acute care systems around the world, GEMI will provide value for multiple global partners involved in health care:
uGovernments interested in global health diplomacy
uHealth care systems interested in health system strengthening
uUniversities interested in comprehensive research and international exchanges
uBusinesses looking for new markets for health care innovations, improvements and social entrepreneurship
uNGOs looking for capacity building, creating longevity and sustainability
Today, many global health policy makers are recognizing the need for EM and acute care systems. GEMI will be the first large organization that can build EM systems on national or transnational scales. By creating the Global EM Network, by building Global Health and EM Institutes, and by bringing together multiple partners from multiple disciplines, GEMI is the organization that will enable people all over the world to receive the emergency care they deserve.
To get more information or to learn how you can partner with GEMI, visit www.globalemi.org, or send an email to [email protected]
Advisors & SupportersTerry Mulligan
University of Maryland, USa / Stellenbosch University
Lee WallisUniversity of cape town / Stellenbosch University, S.africa
Bob Cordertawam hospital, Uae / University of Maryland, USa
Peter CameronMonash University, australia / President, iFeM
Jim HollimanUniformed Services University of the health Sciences / George
Washington University School of Medicine and health Sci-ences, USa
Brian BrowneUniversity of Maryland, USa / Stellenbosch University, S.africa
Abdel Bellourennes University / President, euSeM
GEMI: Global Success Requires Global Partnerships
learn how you can get involved with GEMI at www.globalemi.org, or email [email protected]