Emery and Rimoin's Principles and Practice of Medical Genetics || Genetic Lipodystrophies
Transcript of Emery and Rimoin's Principles and Practice of Medical Genetics || Genetic Lipodystrophies

C H A P T E R
91Genetic Lipodystrophies
Abhimanyu Garg
Division of Nutrition and Metabolic Diseases, Department of Internal Medicine, Center for Human Nutrition, UT Southwestern Medical Center at Dallas,
Dallas, TX, USA
© 2013, Elsevier Ltd. A
91.1 INTRODUCTION
Lipodystrophies are disorders of adipose tissue charac-terized by selective loss of body fat and a predisposition to develop insulin resistance and its complications (1). The prevalence of metabolic and other manifestations of insulin resistance, such as impaired glucose tolerance, diabetes, hyperinsulinemia, dyslipidemia, hepatic ste-atosis, acanthosis nigricans, polycystic ovarian disease and hypertension, varies among the different subtypes of lipodystrophies and is generally determined by the extent of adipose tissue loss (1). The loss of adipose tis-sue is readily apparent in females, and thus the diagnosis of lipodystrophies is relatively easy in them but it may be missed in affected males as many normal men look muscular and have much less body fat that women. Lipodystrophies can be classified into genetic syndromes and acquired disorders due to various causes (1,2). The inherited lipodystrophy syndromes can be subclassified into autosomal-recessive or autosomal-dominant disor-ders and a classification is given in Table 91-1 (2). The precise mode of inheritance still remains to be character-ized for some disorders.
A great deal of progress has been made recently in elucidating the genetic basis of many types of inherited lipodystrophies (1,2); however, the defective genes for some disorders still remain to be discovered. The discov-eries of the molecular mechanisms underlying various types of genetic lipodystrophies has added to our under-standing of adipocyte biology and has revealed potential pathways, which may be implicated in development of insulin resistance in these disorders as well as in other common disorders of adipose tissue such as generalized and regional obesity (3).
91.2 MECHANISMS OF INSULIN RESISTANCE AND ITS COMPLICATIONS IN LIPODYSTROPHIES
The underlying mechanisms causing insulin resistance in patients with lipodystrophies may be similar to those implicated in obesity. For example, in patients with
ll rights reserved. 1
severe forms of obesity and lipodystrophies, there may be limitation in further storage of triglycerides in adipose tissue resulting in diversion of dietary and endogenously synthesized triglycerides to aberrant sites, such as the liver and skeletal muscles resulting in insulin resistance (4). The frequency of hepatic steatosis differs in patients with various lipodystrophies. For example, nearly all patients with congenital generalized lipodystrophy (CGL) have some degree of hepatic steatosis since birth whereas only a few patients with familial partial lipo-dystrophies (FPL) may develop hepatic steatosis (5,6). Accumulation of triglycerides in skeletal muscle has not been studied systematically. Slight increase in skeletal muscle triglyceride was noted even in patients with CGL (7). The ectopic triglyceride accumulation may induce hepatic and skeletal muscle insulin resistance; however, the precise molecular mechanisms by which this occurs have not been elucidated. Hypertriglyceridemia and low-ering of high-density lipoprotein (HDL) cholesterol in patients may be related to severity of hepatic steatosis. Clinically, a dramatic reduction in insulin resistance as well as hepatic steatosis is observed when patients reduce energy intake because of either exogenous leptin therapy or otherwise (8,9).
The mechanisms of diabetes mellitus seem to be similar to that noted in patients with type 2 diabetes. Marked islet amyloidosis and pancreatic β cell atrophy was observed on autopsy of two lipodystrophic patients with diabetes, one with CGL and another with Familial Partial Lipodystrophy, Dunnigan variety (FPLD) (6,10). Diabetes in patients with lipodystrophies is usually ketosis resistant and many patients require extremely high doses of insulin to achieve good glycemic control (8). Whether the resistance to ketosis is due to residual endogenous insulin secretion or due to reduced flux of free fatty acids, the substrates for production of ketones, is not clear.
Extremely high serum levels of insulin may be impli-cated in other clinical manifestations noted in patients with lipodystrophies such as acanthosis nigricans, acromegaloid features (enlargement of mandible, hands

2 CHAPTER 91 Genetic Lipodystrophies
TABLE 91-1 Classification of Genetic Lipodystrophies
A. Autosomal-Recessive Syndromes 1. Congenital generalized lipodystrophy (CGL; Berardinelli–Seip Syndrome) a. CGL Type 1: AGPAT2 (1-acylglycerol-3-phosphate O-acyltransferase 2) mutations b. CGL Type 2: BSCL2 (Berardinelli–Seip congenital lipodystrophy 2) mutations c. CGL Type 3: CAV1 (Caveolin 1) mutation d. CGL Type 4: PTRF (polymerase I and transcript release factor) mutations e. Other varieties 2. Mandibuloacral dysplasia (MAD)-associated lipodystrophy a. Partial lipodystrophy (Type A pattern): LMNA (lamin A/C) mutations b. Generalized lipodystrophy (Type B pattern) ZMPSTE24(zinc metalloproteinase) mutations c. Other varieties: Unknown 3. Autoinflammatory syndromes a. JMP syndrome: PSMB8 (proteasome subunit, beta-type, 8) mutations; b. CANDLE syndrome: PSMB8 mutations 4. Familial Partial Lipodystrophy (FPL): CIDEC (cell death-inducing DNA fragmentation factor a-like effector c) mutation 5. SHORT (Short stature, Hyperextensibility or inguinal hernia, Ocular depression, Rieger anomaly and Teething delay) syndrome: Unknown 6. Mandibular hypoplasia, Deafness, Progeroid features (MDP)-associated lipodystrophy: Unknown 7. Neonatal Progeroid (Weidemann–Rautenstrauch) Syndrome: Unknown
B. Autosomal-Dominant Syndromes 1. Familial Partial Lipodystrophy (FPL) a. FPL, type 1, Kobberling variety: Unknown b. FPL, type 2, Dunnigan variety (FPLD): LMNA (lamin A/C) mutations c. FPL type 3: PPARG (peroxisome proliferator-activated receptor-γ) mutations d. FPL type 4: AKT2 (v-AKT murine thymoma oncogene homolog 2) mutation e. FPL, type 5: PLIN1 (perilipin 1) mutations f. Other varieties: Unknown 2. Atypical progeroid syndrome: LMNA mutations 3. Hutchinson–Gilford progeria syndrome: LMNA mutations 4. SHORT syndrome: Unknown
and feet), generalized organomegaly and clitoromegaly as well as polycystic ovarian disease. These may occur because of “specificity spillover phenomenon” and actions of high levels of insulin through other receptors such as those for insulin-like growth factors, I and II. The precise molecular mechanisms involved in various clinical manifestations are expected to be revealed in the near future as we make progress in understanding bio-logical processes related to the genes implicated in caus-ing genetic lipodystrophies.
91.3 GENETIC LIPODYSTROPHIES
Most of the patients with genetic lipodystrophies reveal a classical autosomal-recessive (congenital generalized or mandibuloacral dysplasia (MAD)-associated) or autoso-mal-dominant inheritance pattern (FPL). However, for the SHORT-syndrome-associated lipodystrophy, both autosomal-recessive and autosomal-dominant inheri-tance patterns have been reported. In the following sec-tion, each type of inherited lipodystrophy is discussed.
91.3.1 Autosomal-Recessive Types
91.3.1.1 Congenital Generalized Lipodystrophy (Berardinelli–Seip Syndrome). This autosomal-recessive disorder (Online Mendelian Inheritance in Man #269700)
was reported originally by Berardinelli from Brazil approximately 57 years ago (11). Shortly thereafter, Seip from Norway provided detailed description of the phenotype (12). The diagnosis of CGL is made usually at birth or shortly thereafter. Approximately 300 cases have been reported from all over the world. It is more commonly reported from the racial and ethnic groups such as from Brazil and Lebanon, where consanguinity is common (13,14). If the reported cases represent only one-fourth of the actual cases, the estimated prevalence of this disorder is about 1 in 10 million.
91.3.1.1.1 Clinical and Biochemical Charac-teristics. The affected newborns appear “strikingly muscular” because of almost complete absence of adi-pose tissue. They grow at an accelerated rate and their bone age may be advanced. Children display markedly increased appetite. Slight enlargement of the hands, feet and mandible (“acromegaloid” features) are apparent (Figure 91-1A). Umbilical hernia or enlargement of the umbilicus is observed commonly. Acanthosis nigricans usually develops late in the childhood or adolescence and may affect extensive area of the body such as the trunk, hands, elbows, knees and ankles besides the common sites at the neck, axillae and groins.
Hepatomegaly is usually noticed during infancy and is due to hepatic steatosis. A few patients develop cirrho-sis and its complications later on in life. Many patients

develop splenomegaly. In postpubertal females, mild hir-sutism, clitoromegaly, oligoamenorrhea and polycystic ovaries are common. Most affected women are unable to get pregnant but successful pregnancy has been reported. Affected men usually have normal reproductive ability. Many patients develop focal lytic lesions in the appen-dicular bones after puberty, commonly involving the humeri, but also sometimes affecting the femur, radius, ulna, carpal, tarsal and phalangeal bones (15). These lytic lesions may be related to the lack of bone marrow fat and inability to replace hematopoietic marrow with adipose tissue during childhood and adolescence. Hyper-trophic cardiomyopathy and mild mental retardation have been reported in some patients (16–19).
Patients have marked fasting and postprandial hyper-insulinemia suggestive of severe insulin resistance. Extreme hypertriglyceridemia predisposes patients to recurrent episodes of acute pancreatitis. Levels of HDL cholesterol also tend to be low. Diabetes is usually noted during the pubertal years; however, the onset of diabetes
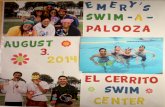
FIGURE 91-1 CGL. Panels A and B show anterior and posterior views, respectively, of a 37-year-old female of African-American origin with congenital generalized lipodystrophy type 1, showing generalized lack of fat, extreme muscularity and acromegaloid features. She developed diabetes mellitus at the age of 17 years. Acanthosis nigricans was present in the neck, axillae and groin. She had a homozygous mutation (IVS4-2A>G resulting in prematurely truncated protein Gln196fsX228) in the AGPAT2 gene.
CHAPTER 91 Genetic Lipodystrophies 3
has occurred as early as 6 weeks of life (18). In some neonates, diabetes occurs transiently during period of stress or infection only to recur later in life. Patients require high doses of insulin to control diabetes.
Consistent with the near total absence of body fat, the serum levels of adipocytokines, such as leptin and adiponectin, are low (20). It is likely that hypoleptinemia contributes to excessive appetite and metabolic compli-cations in patients with CGL.
91.3.1.1.2 Genetic Defect and Pathophysiology. Using genome-wide linkage analysis, we reported the first locus for CGL on human chromosome 9q34 (21) and described genetic heterogeneity in 17 pedigrees. Subse-quently, another locus was found on chromosome 11q13 (13). Positional cloning approach led us to identify muta-tions in the 1-acylglycerol-3-phosphate-O-acyltransferase 2 (AGPAT2) gene in affected patients from pedigrees linked to 9q34 (17). The defective gene on chromosome 11q13 was found to be a novel gene, called Berardinelli–Seip Congenital Lipodystrophy 2 (BSCL2) and the prod-uct of the gene was named Seipin, after Seip (13). Recently, candidate gene approach has led to the identification of two additional CGL loci, caveolin 1 (CAV1) (22) and polymerase I and transcript release factor (PTRF) (23).
The AGPATs belong to the acyltransferase family of enzymes and 11 isoforms, each encoded by a different gene are known currently (24–26). The AGPATs cata-lyze an important step in the biosynthesis of glycero-phospholipids and triglycerides. These enzymes acylate lysophosphatidic acid (1-acylglycerol-3-phosphate) to phosphatidic acid (1,2 diacylglycerol-3-phosphate) (24,27) (Figure 91-2). Each isoform may have substrate specificity for different fatty acids but precise nature of it remains unclear. These isoforms may also differ in subcellular localization and may play different roles in mitochondrial or microsomal synthesis of triglyceride or phospholipids. There may also be heterogeneity as far as expression of these isoforms in various tissues, particu-larly among adipose tissue depots localized at different regions of the body.
Of the two major isoforms of AGPAT, 1 and 2, we reported that AGPAT2 is highly expressed in the omen-tal adipose tissue (17), but AGPAT1 showed an equal expression in the liver and its expression was nearly twofold in the skeletal muscle. Thus, it can be hypoth-esized that mutations of AGPAT2 gene may cause lipo-dystrophy either by reducing triglyceride deposition in the adipocytes or by affecting adipocyte function result-ing from the lack of synthesis of phospholipids. AGPAT2 consists of 278 amino acids and shares two highly conserved motifs, Asn-His-x-x-x-x-Asp (amino acids 97–103, with x denoting any amino acid) and Glu-Gly-Thr-Arg (amino acids 172–175) with other acyltransfer-ases. These motifs are critical for the enzymatic activity (24,28). Besides the well-conserved motifs, we have recently reported that carboxy-terminal residues are also important determinants of the AGPAT2 enzymatic

4 CHAPTER 91 Genetic Lipodystrophies
amcaarsppu
ctivity (29). Using in vitro expression of wild-type and utant forms of AGPAT2 in Chinese Hamster Ovary
ells, we found that null mutants had markedly reduced ctivity to convert lysophosphatidic acid to phosphatidic cid and the missense mutants had mild to moderate eduction in activity (29). However, because of reduced ample size, compound heterozygous mutations in many atients, and the fact that most of the CGL patients do resent with near-total absence of body fat, we were nable to find a genotype–phenotype relationship.
The BSCL2 encodes a 398-amino-acid transmem-brane protein, seipin, which does not reveal any striking homology to any other protein. It contains a CAAX motif at the C-terminal and a glycosylation site, Asn-Val- Ser, at position 88–90. We previously reported a weak but not insignificant homology of seipin to the linker region of the protein called midasin (30). Interestingly, missense mutations in the glycosylation motif of seipin have been reported to cause distal hereditary motor neuropathy and Silver syndrome most likely by aggresome formation (31). Recent data suggest the role of seipin in lipid droplet for-mation and in adipocyte differentiation (32–34).
Caveolin 1 is expressed in caveolae, which are spe-cialized microdomains on cell membranes of adipocytes (35). It contributes to lipid droplet formation by binding
Fbthss2csEM
fatty acids and translocating those to lipid droplets. PTRF is also known as cavin, and plays a role in biogen-esis of caveolae. PTRF regulates expression of caveolins 1 and 3 (23).
91.3.1.1.3 Genotype and Phenotype Variation. There are phenotypic differences in the two most preva-lent types of CGL, called type 1 (AGPAT2 related) and type 2 (BSCL2 related) (17–19). Patients with CGL, type 2 have increased prevalence of cardiomyopathy and mild mental retardation (17–19), while focal lytic lesions in appendicular skeleton are more prevalent in CGL type 1 (36). In both the types, metabolically active adipose tissue, which is found in most subcutaneous (sc) areas, intra-abdominal and intrathoracic regions, and bone marrow, is nearly completely lost (36). The mechanical adipose tissue depots located in the palms, soles, under the scalp, retro-orbital and periarticular regions are spared in CGL, type 1 but severe loss of fat also occurs from these depots in patients with CGL, type 2 (5,36,37). Serum leptin levels also tend to be lower among those with type 2 CGL compared to those with type 1 CGL but interestingly, they have increased serum adiponectin levels (18).
CGL, type 3 has been reported in only one Brazilian girl who had a homozygous CAV1 mutation and had
IGURE 91-2 Pathways for biosynthesis of triacylglycerol: glycerol-3-phosphate (G3P) is the initial substrate for acylation at sn-1 position y the enzyme glycerol-3-phosphate acyltransferase (GPAT), to form 1-acylglycerol-3-phosphate or lysophosphatidic acid (LPA). LPA is fur-er acylated at sn-2 position by 1-acylglycerol-3-phosphate acyltransferase (AGPAT, aka LPAAT) to form phosphatidic acid (PA). In the next
tep, phosphate group is removed by phosphatidate phosphohydrolase (PAP) to produce diacylglycerol (DAG). DAG is further acylated at n-3 position by diacylglycerol acyltransferase (DGAT) to produce triacylglycerol (TG). In addition, TG can be synthesized via the acylation of -monoacylglycerol by the enzyme monoacylglycerol acyltransferase (MGAT), which is highly expressed in small intestine. DAG kinase (DGK) an phosphorylate DAG to synthesize PA. PA and DAG are also substrates for the synthesis of glycerophospholipids such as phosphatidylino-itol (PI), cardiolipin, phosphatidylcholine (PC), phosphatidylethanolamine (PE) and phosphatidylserine (PS). (Reproduced with permission from lsevier. Agarwal, A. K.; Garg, A. Congenital Generalized Lipodystrophy: Significance of Triglyceride Biosynthetic Pathways. Trends Endocrinol. etab. 2003, 14 (5), 214–221.)

CHAPTER 91 Genetic Lipodystrophies 5
short stature and presumed Vitamin D resistance (22). Type 4 CGL due to PTRF mutations has been reported in approximately 21 patients. Peculiar finding in these patients include congenital myopathy, percussion-induced myoedema, pyloric stenosis and atlantoaxial instabil-ity. Of particular concern are arrhythmias including prolonged QT interval and exercise-induced ventricular tachycardia, and sudden death (23,38,39). Patients with CAV1 and PTRF mutations have well-preserved mechan-ical and bone marrow fat (22,36,38,40). There are a few patients with CGL who do not have mutations in the four known loci and may lead us to yet more novel loci.
In our experience as well as of that of others, nearly all patients of African origin harbor the founder muta-tion (IVS4-2A>G) in AGPAT2, whereas patients of Leb-anese origin have a founder mutation (659delGTATC) in BSCL2 (18) (Figures 91-3 and 91-4). Patients of Euro-pean and Asian descent have been reported to harbor mutations in either of the two genes. CGL, type 3 has been reported from Oman in several pedigrees.
91.3.1.1.4 Molecular and Differential Diagnosis. Patients with CGL can be easily diagnosed at birth or
immediately thereafter. The two main types of CGL can be distinguished based on their clinical features. Diagno-sis at the molecular level may be needed in some but it raises economic and ethical issues. Couples with a child affected with CGL may use molecular diagnosis to know their risk of having another child with CGL. Finally, molecular diagnosis can be used for prenatal screening.
Many different syndromes can present phenotype similar to CGL such as acquired generalized lipodys-trophy with onset during early infancy, leprechaunism, atypical Werner syndrome, pubertal-onset generalized lipodystrophy due to rare LMNA mutations and neona-tal progeroid syndrome.91.3.1.2 Mandibulo-Acral Dysplasia (MAD)- Associated Lipodystrophy. MAD (OMIM #248370) is a rare autosomal-recessive disorder characterized by hypopla-sia of the mandible and clavicles, and acro-osteolysis (resorption of the terminal phalanges) (41,42). Patients also have delayed closure of cranial sutures, joint con-tractures, mottled cutaneous pigmentation and short stature. Features of accelerated aging called “progeroid features” such as bird-like facies, high-pitched voice and
5’ 1 2 3 4 5 6
+1G>A
T65XR68X
-2A>G
S100N
P128AfsX19
140delF
G136R
+1G>A -1G>C
317_588 del-2A>G +2T>G
-2A>C 916C>G
W168CfsX16E172KD180TfsX71F189XY190X
K215XK216X Q226X
L228PA238GA239V252delMRT
P112L
FIGURE 91-3 Structure of AGPAT2 gene and various mutations found in the affected individuals with CGL. Boxes represent exons and small arrows show location of primers used for exons amplifications. (Reproduced in a modified form with permission from Agarwal, A. K.; Barnes, R. I.; Garg, A. Genetic Basis of Congenital Generalized Lipodystrophy. Int. J. Obesity 2004, 28, 336–339.)
5’ 3’1 2 3 4 5 6 7 8 9 10 11
L100FfsX1
V108FfsX5
T142A
P105FfsX6
+1G>A
A212P
+5G>A -2A>G-3C>G
L227XI262HfsX11
E189X
R275X
Y187CE177XL155P
R138X
A218WfsX51
-11A>G
L48FY53SfsX40
P65RfsX28
Y106CfsX6
T109NfsX5
-2A>C
-2A>G
F65GfsX10
FIGURE 91-4 Structure of BSCL2 gene and various mutations found in the affected individuals with CGL. Boxes represent exons and small arrows show location of primers used for exons amplifications. (Reproduced in a modified form with permission from Agarwal, A. K.; Barnes, R. I.; Garg, A. Genetic Basis of Congenital Generalized Lipodystrophy. Int. J. Obesity 2004, 28, 336–339.)

6 CHAPTER 91 Genetic Lipodystrophies
ectodermal defects, such as skin atrophy, pigmentation, alopecia, and nail dysplasia are also seen in some patients. Only a few patients have had hypogonadism and senso-rineural deafness. Approximately 40 patients with MAD have been reported in the literature (Figure 91-5).
Patients with MAD display two patterns of lipodys-trophy: type A pattern with partial loss of sc fat from the extremities and type B pattern with more generalized loss of sc fat involving the face, trunk and extremities (41). Hyperinsulinemia, insulin resistance, impaired glucose tolerance, diabetes mellitus and hyperlipidemia have been reported but are usually mild to moderate in severity (41).
91.3.1.2.1 MAD-Associated Partial Lipodystrophy due to LMNA Mutations. Novelli et al. (42) reported a homozygous Arg527His mutation in LMNA gene in MAD patients with type A (partial) lipodystrophy of Italian origin. The heterozygotes had no phenotypic manifestations of MAD. LMNA encodes lamins A and C by alternative splicing in exon 10 (43). Prelamin A has a CAAX motif at its C-terminal, which undergoes posttranslational modification involving an endoprote-ase called zinc metalloproteinase (ZMPSTE24) to form
FIGURE 91-5 MAD. A. Lateral view of a 20-year-old Hispanic female with MAD due to homozygous Arg527His missense muta-tion of the LMNA gene. She had reconstructive surgery for microgna-thia. She had loss of fat from the extremities leading to a muscular appearance and prominent subcutaneous veins and had excess fat accumulation in the face and neck region. Note the mottled skin pigmentation over the trunk. B. Hands show rounding of the finger tips and clubbing appearance due to acro-osteolysis of the terminal phalanges. There is atrophy of the skin on the dorsum of hands especially over the interphalangeal joints and metacarpophalangeal joints.
mature lamin A (Figure 91-6). The lamins belong to the intermediate filament family of structural proteins. Lam-ins A and C form hetero- or homodimeric coiled-coil struc-tures and are integral components of the nuclear lamina; a polymeric structure intercalated between chromatin and the inner membrane of the nuclear envelope (44,45). The mechanisms by which this LMNA mutation causes predominantly skeletal and cutaneous dystrophy but less-severe lipodystrophy in patients with MAD, remain unclear. By now, a total of 30 patients with MAD due to various LMNA mutations have been reported (41,42,46–48). Some patients have more-severe progeroid man-ifestations, such as those seen in Hutchinson–Gilford progeria syndrome (HGPS) such as alopecia, loss of eye-brows, delayed sexual maturation and premature loss of teeth. Most of the LMNA mutations causing MAD are located in the C-terminal region affecting exons 8–10. How these specific LMNA mutations cause resorption of bones such as mandible, clavicles and terminal phalanges remains unclear.
91.3.1.2.2 MAD-Associated Generalized Lipo-dystrophy due to Zinc Metalloproteinase (ZMP-STE24) Mutations. On the basis of the critical role of ZMPSTE24 in posttranslational maturation of prelamin A to its mature form lamin A and the phenotype of lipo-dystrophy and skeletal abnormalities in ZMPSTE24-deficient mice (49,50), we sequenced ZMPSTE24 gene in MAD patients who did not have mutations in LMNA gene. We found compound heterozygous mutations in the ZMPSTE24 gene in a Belgian woman with MAD (51). She also had progeroid features and generalized lipodystrophy (51). She died prematurely at age 24 years of complications of chronic renal failure due to collapsing variety of focal segmental glomerulosclerosis (51). Given the role of ZMPSTE24 in posttranslational proteolytic processing of prelamin A, cellular accumula-tion of prelamin A and/or lack of mature lamin A may be responsible for phenotypic features (52). A recent study suggests toxic effects of prelamin A accumula-tion to be responsible for the phenotype in ZMPSTE24- deficient mice (53). In our cohort of patients with MAD, some patients do not have any variants in either LMNA or ZMPSTE24 genes, suggesting additional as yet unmapped loci (51).
91.3.1.2.3 Genotype and Phenotype Variation. About 30 patients have been reported to have MAD due to LMNA mutations, but only eight MAD patients have ZMPSTE24 mutations. Several MAD patients have been reported from Italy and all of them have a founder LMNA Arg527His mutation (42). MAD patients with LMNA or ZMPSTE24 mutations share features of man-dibular and clavicular hypoplasia and acro-osteolysis but patients with ZMPSTE24 mutations are prema-ture at birth, have early onset of skeletal defects includ-ing acro-osteolysis, have more progeroid appearance and develop sc calcified nodules on the phalanges. We have reported focal segmental glomerulosclerosis in two

CHAPTER 91 Genetic Lipodystrophies 7
Farnesyl diphosphateFarnesyl Transferase (FT)
Zinc Metalloproteinase (ZMPSTE24)
Isoprenyl Cysteine Carboxymethyl Transferase (ICMT)
ZMPSTE24 or other endoprotease
647 661Peptide Fragment 26461 Mature Lamin A
6461 661
662 6646461S-adenosyl methionine
661
6461 664
6461 664
Prelamin A
661
PeptideFragment 1
661
FIGURE 91-6 Posttranslational processing of prelamin A. Prelamin A contains 664 amino acids and a conserved CAAX motif at the carboxy terminal. The cysteine residue in the CAAX motif is first farnesylated by the farnesyl transferase (shown by filled circles) followed by first proteolytic cleavage of the three extreme C-terminal residues by zinc metalloproteinase (ZMPSTE24). Then, the farnesylated cysteine residue is methylated by isoprenylcysteine carboxyl methyl transferase (ICMT) using S-adenosyl methionine as the methyl donor (shown by unfilled triangle). Thereafter, ZMPSTE24 or other endoprotease cleave the 15 amino acids from the C-terminal forming the mature lamin A with 646 residues. (Reproduced with permission from Elsevier Inc. Garg, A.; Misra, A. Lipodystrophies: Rare Disorders Causing Metabolic Syndrome. Endocrinol. Metab. Clin. North Am. 2004, 33, 305–331.)
patients with ZMPSTE24 deficiency; kidney pathology has not been reported in those with LMNA mutations (51). Interestingly, the remaining patients, who do not harbor LMNA or ZMPSTE24 variants, do not seem to develop clavicular resorption or acro-osteolysis.
91.3.1.2.4 Molecular and Differential Diagnosis. Ascertaining molecular diagnosis may help predict pecu-liar clinical features noted in different genetic varieties of MAD. Patients with MAD have several overlapping clin-ical features with HGPS and those with atypical Werner syndrome (all due to heterozygous mutations in LMNA) and should be differentiated from such patients. Patients with several other genetic syndromes, such as, Hajdu–Cheney, congenital insensitivity to pain with anhidrosis, Haim–Munk, and Papillon–Lefevre syndromes present with acro-osteolysis as well and need to be differentiated from patients with MAD.91.3.1.3 Autoinflammatory Syndromes.
91.3.1.3.1 Joint Contractures, Muscle Atrophy, Microcytic Anemia and Panniculitis-Induced (JMP) Lipodystrophy. Recently, an autosomal-recessive, auto-inflammatory, JMP syndrome was reported by us in a patient from Portugal and two siblings from Mexico (54). These patients started developing progressive panniculitis-induced lipodystrophy during childhood. Previously, three patients with very similar features were reported from Japan (55,56). Other reported features of JMP syndrome include intermittent fever, hypergammaglobulinemia, ele-vated erythrocyte sedimentation rate, hepatosplenomeg-aly and calcification of basal ganglia (Figure 91-7).
Genome-wide linkage analysis was conducted by us in the two pedigrees with JMP syndrome and we looked for regions of extended homozygosity in the affected
patients. These studies linked JMP syndrome to chro-mosome 6. Sequencing of immune response genes in this region led us to a homozygous, missense (Thr75Met) loss of function, mutation in proteasome subunit, beta-type, 8 (PSMB8) gene in affected patients from both the pedigrees (57). PSMB8 encodes the β5i subunit of the immunopro-teasome (58). Immunoproteasomes are responsible for proteolysis of antigens presented by major histocompat-ibility complex class I molecules and result in generation of immunogenic epitopes. We believe that the mutation in PSMB8 may trigger autoinflammatory response which results in panniculitis and other autoinflammatory mani-festations. Two other groups from Japan have recently confirmed our findings and have reported another missense mutation, Gly201Val, in PSMB8 in patients with autoinflammation and lipodystrophy (59,60).
91.3.1.3.2 Chronic Atypical Neutrophilic Derma-tosis with Lipodystrophy and Elevated Temperature (CANDLE) Syndrome. This is a relatively new syn-drome reported by two groups in a total of five patients. Clinical manifestations include onset of recurrent fever and annular violaceous plaques during infancy which result in loss of sc fat from the face and upper limbs (61,62). Patients develop violaceous swelling of the eyelids, hepatosplenomegaly, arthralgias, hypochromic anemia, raised erythrocyte sedimentation rate and basal ganglia calcifications. On the basis of limited data, the mode of transmission seems to be autosomal recessive. Recently, homozygous Cys135X and Thr75Met muta-tions in PSMB8 have been reported in patients with CANDLE syndrome (63).91.3.1.4 Familial Partial Lipodystrophy (FPL) due to CIDEC Mutation. A single patient with

8 CHAPTER 91 Genetic Lipodystrophies
autosomal-recessive FPL has been reported to harbor a homozygous missense mutation in cell death-inducing DNA fragmentation factor a-like effector c (CIDEC) (64). The sc adipose tissue of the patient had multilocu-lar, small lipid droplets in adipocytes as has been seen previously in the knockout mouse model (64,65).91.3.1.5 SHORT Syndrome-Associated Lipodystro-phy. The acronym of SHORT syndrome is based on several clinical features such as short stature, hyper-extensibility of joints and/or inguinal hernia, ocular depression, Reiger anomaly and teething delay. Only about 30 patients have been reported to have SHORT
(A) (B)
(C)
(D)
FIGURE 91-7 JMP syndrome. A. 26-year-old Hispanic female with more marked loss of sc fat from the face, neck, chest and upper extremities than from the abdomen, hips and lower extremities, which were spared. The breasts were atrophic and the neck and chest showed many discrete, small, erythematous nodular skin lesions. B. View of the hand showing flexion contracture at the wrist. The metacarpophalangeal joints were hyperextended and the proximal and distal interphalangeal joints showed variable flexion contractures. C. She had mild contractures of the foot joints. D. Hematoxylin and eosin stain of the skin and subcutaneous tissue biopsy specimen showing lymphocytic infiltrate permeating deep dermal collagen and subcutaneous adipose tissue, with a perivas-cular component (lower left part of field) consistent with pannicu-litis. No vasculitis or fat necrosis is seen (200×). (Figures A and D are reproduced with permission from the Endocrine Society. Garg, A.; Hernandez, M. D.; Sousa, A. B.; Subramanyam, L.; de Villar-real, L. M.; Dos Santos, H. G.; Barboza, O. An Autosomal Reces-sive Syndrome of Joint Contractures, Muscular Atrophy, Microcytic Anemia and Panniculitis-Associated Lipodystrophy. J. Clin. Endocrinol. Metab. 2010, 95, E58–E63.)
syndrome and both autosomal-recessive (66,67) and -dominant (68–70) modes of transmission have been reported (66–68). Features of Reiger anomaly include eye abnormalities such as hypoplasia of iris stroma, prominent Schwalbe ring, iridocorneal synechiae, micro- or megalocornea and teeth anomalies such as hypodon-tia, microdontia, enamel hypoplasia and atypical teeth. Some patients also manifest intrauterine growth retar-dation with slow postnatal weight gain, delayed speech development with normal intellect, frequent childhood illnesses, small head circumference, bilateral clinodactyly and sensorineural hearing loss.
Different patterns of fat loss have been reported. In many patients, lipodystrophy affects the face, upper extremities and sometimes the trunk, with relative sparing of the lower extremities. On the other hand, a few pedi-grees with autosomal-dominant SHORT syndrome had lipodystrophy affecting only the face, gluteal region and elbows (69,70). Diabetes occurs as early as the second and third decade of life. The genetic basis remains unknown.91.3.1.6 Mandibular Hypoplasia, Deafness, and Progeroid Features—Associated Lipodystrophy (MDP Syndrome). We recently reported this new syndrome distinct from MAD as these patients did not have acro-osteolysis (71). All males with MDP syndrome had unde-scended testes and hypogonadism. One adult female showed lack of breast development. The molecular basis of this syndrome remains unknown.91.3.1.7 Neonatal Progeroid Syndrome (Wiedemann–Rautenstrauch Syndrome). This is an autosomal-recessive syndrome with a total of approximately 25 reported cases (72–74). The clinical features are evident at birth and include a triangular, old-looking face with relatively large skull (progeroid appearance), prominent veins on the scalp, sparse scalp hair, large anterior fonta-nelle and generalized lipodystrophy. Interestingly, sc fat in the sacral and gluteal areas is spared and can be promi-nent (74,75). Approximately, half of them die before the age of 6 years but patients surviving up to the age of 16 years have been reported (74–77). The genetic basis remains to be elucidated.
91.3.2 Autosomal-Dominant Types
91.3.2.1 Familial Partial Lipodystrophy (FPL). Patients with FPL have variable loss of body fat from the extremities as well as from the truncal region. They follow an autosomal-dominant inheritance pattern. Recognition of affected men is very difficult because even many normal adult men appear muscular. Consequently, nearly all the reported pedigrees have been ascertained from female probands. The diagnosis can be suspected in patients with early onset of diabetes and hypertriglyceridemia in the second or third decades who do not have generalized obesity and display marked loss of fat from the extremities, especially from the gluteal region. There are several distinct subtypes of FPL as described below.

91.3.2.1.1 Familial Partial Lipodystrophy, Dunni-gan Type due to LMNA Mutations. This lipodystrophy (OMIM #151660) was initially described by Ozer et al. (78) in a brief abstract form and later Dunnigan et al. pro-vided a detailed phenotypic description (79). Initial reports of this syndrome described only affected females but sub-sequently, approximately 300–500 men and women have been reported to have FPLD (80,81). Nearly all of them are of European origin, but Asian Indian and African–American patients have also been reported (Figure 91-8).
91.3.2.1.1.1 Clinical and Biochemical Character-istics. It is difficult to recognize affected subjects before puberty as they have normal body fat distribution. The onset of lipodystrophy occurs during childhood or at the time of puberty and sc adipose tissue from the extremi-ties and trunk is lost gradually. The loss of sc fat is more evident from the anterior truncal region than the posterior region (82). Concurrent with the onset of lipodystrophy, excess fat deposition occurs at the chin (“double chin”),
FIGURE 91-8 FPL. A 38-year-old white woman with FPL, Dunni-gan variety due to heterozygous missense mutation in the LMNA gene. She had loss of fat from the extremities and trunk beginning at puberty and had excess fat accumulation in the face and neck region. She has had surgical removal of fat from the chin, neck, axillae and mons pubis previously. She had acanthosis nigricans in the axillae and groins. (Reproduced with permission from Elsevier Inc. Garg, A.; Misra, A. Lipodystrophies: Rare Disorders Causing Metabolic Syn-drome. Endocrinol. Metab. Clin. North Am. 2004, 33, 305–331.)
CHAPTER 91 Genetic Lipodystrophies 9
supraclavicular area, and face (“Cushingoid appearance”) and sometimes over the dorsocervical region (“Buffalo hump”). Magnetic resonance imaging reveals particularly prominent intermuscular (in-between the muscular fas-ciae) fat deposition at the level of thighs and pelvis (81). In many patients, excess fat accumulates in the intra-abdom-inal and intrathoracic regions. FPLD is easier to diagnose in women but the diagnosis in affected men is challenging. Some affected men do show a muscular phenotype despite no resistance exercise training and show accumulation of fat in the face and neck. About one-fifth to one-third of the patients have acanthosis nigricans, hirsutism, men-strual abnormalities, and polycystic ovaries (82).
Women seem to be particularly severely affected by the metabolic complications of insulin resistance than men (80). The prevalence of diabetes among affected women is more than 50% in pedigrees collected by us versus only about 20% in the men. Diabetes usually develops after the second decade and multiparity and excess fat deposi-tion in the nonlipodystrophic regions, such as the chin, can be predisposing factors for diabetes (83). Affected women also have higher prevalence of hypertriglyceri-demia, low serum-HDL-cholesterol concentrations, and atherosclerotic vascular disease, including coronary heart disease (80,84). Some patients also develop cardiac con-duction system disturbances resulting in atrial fibrillation and congestive heart failure, manifestations of associated cardiomyopathy (85).
91.3.2.1.1.2 Genetic Defect and Pathophysiology. Using genome-wide linkage analysis approach in five large informative pedigrees with FPLD, we reported the FPLD locus on chromosome 1q21–22 (86). Sub-sequently, screening for candidate genes in the 5-Mb interval, Cao and Hegele (87) reported a missense mutation, Arg482Gln, in lamin A/C (LMNA) gene in a Canadian pedigree. Since then, several missense muta-tions in LMNA gene have been reported in patients with FPLD, most of them substituting C-terminal resi-dues (83,85,87–89). Interestingly, other heterozygous or homozygous mutations in LMNA have been implicated now in various other disorders such as idiopathic car-diomyopathy, limb-girdle, Emery–Dreifuss and congeni-tal muscular dystrophies, Hutchinson–Gilford progeria syndrome, Charcot–Marie tooth neuropathy, MAD and atypical Werner syndrome (42,90–95). Some patients manifest overlapping clinical features of some of these disorders, which led us to propose that LMNA muta-tions cause a multisystem dystrophy syndrome affecting adipose tissue, cardiac, skeletal muscle, nerve, cutaneous and skeletal tissue (85). However, how specific mutations in LMNA cause adipocyte loss from certain areas of the body remains unknown. It is probably those defective interactions of lamins A and C with chromatin or other nuclear lamina proteins during the cell division leading to apoptosis and premature cell death of adipocytes. The gain of fat in nonlipodystrophic regions may be merely a compensatory phenomenon.

10 CHAPTER 91 Genetic Lipodystrophies
91.3.2.1.1.3 Genotype and Phenotype Variation. Most of the missense mutations in patients with FPLD have been reported in exon 8, encoding the globular C-terminal (tail) portion of the protein (83,85,87–89,96). Arginine residue at position 482 seems to be a hot spot with approximately 75% of the patients harboring a mutation resulting in substitution of this residue to tryp-tophan, glutamine or leucine (83). We have reported an atypical, less-severe FPLD in a pedigree with Arg582His mutation in exon 11 (which can only affect lamin A and not lamin C) (97). We and others have found a strong association between FPLD and cardiomyopathy mani-festing as congestive heart failure, atrial fibrillation and other conduction system disturbances requiring pace-maker implantation in patients with exon 1 mutations (Arg28Trp, Arg60Gly, Arg62Gly and Asp192Val) (85). Some patients manifest overlapping features of mild proximal myopathy or muscular dystrophy with slightly increased serum creatine kinase levels (85,98).
91.3.2.1.1.4 Molecular and Differential Diagnosis. Since the clinical diagnosis is difficult in affected men and prepubertal boys and girls, molecular diagnosis may be helpful in them. Genotyping for mutations may be particularly important for identifying those with exon 1 LMNA mutations at high risk of cardiomyopathy and conduction system disturbances (85). Whether molecular diagnosis in children and adolescents can help in preven-tion of diabetes and other metabolic complications later in life by maintaining an active life style with intense physical activity and prevention of undue weight gain remains to be proven.
Many syndromes can present challenge in diagnosis of FPLD such as Cushing’s syndrome, truncal obesity, multiple symmetric lipomatosis due to alcohol intake, acquired generalized lipodystrophy, and lipodystrophy in HIV-infected patients. Patients with FPL due to PPARG mutation generally have milder loss of fat from the limbs compared to those with FPLD. Subcutaneous fat from the trunk is not affected in those with PPARG mutations.
91.3.2.1.2 Familial Partial Lipodystrophy due to Peroxisome Proliferator-Activated Receptor-γ (PPARG) Mutation. Candidate gene approach in many patients affected with FPL, who did not harbor a muta-tion in LMNA gene, resulted in identification of a het-erozygous missense mutation, Arg397Cys, in the PPARγ gene in a 64-year-old woman with diabetes, hypertri-glyceridemia, hypertension and hirsutism, who had lipo-dystrophy of the face and extremities (OMIM #604367) (99). Subsequently, ~30 more FPL subjects with variable presence of disorders associated with insulin resistance such as diabetes, hypertension and hypertriglyceridemia with heterozygous PPARG mutations have been reported (100–102). The age of onset of lipodystrophy appears to range from second decade to later during adulthood but the pattern of progression of fat loss remains to be defined. All affected subjects have been reported to have lost sc fat from the distal extremities; however, facial fat
has been variously reported to be reduced, normal or increased (99–101).
The PPARγ protein plays a central role in adipogen-esis. It is a ligand-inducible nuclear transcription factor, which forms a heterodimer with the retinoid X recep-tor and induces transcription of adipocyte-specific genes in response to activation by hormones or other agonists (103,104). PPARγ is highly expressed in the adipose tis-sue, further suggesting its important role in adipose tis-sue function. Thus, lipodystrophy in FPL patients with missense mutations in PPARγ may be due to reduced adipogenesis. Why only selective adipose tissue depots are affected in patients with PPARG mutations remains unclear.
91.3.2.1.3 Familial Partial Lipodystrophy due to v-AKT Murine Thymoma Oncogene Homolog 2 (AKT2) Gene Mutations. Recently, George et al. (105) reported a heterozygous missense mutation, Arg274His, in AKT2 gene in four subjects from a family who had insulin resistance and diabetes mellitus. The proband was a 35-year-old Caucasian female who developed diabetes mellitus at age 30 years, whereas her mother and grand-mother harboring the same mutation developed diabetes during late thirties and a maternal uncle, a middle-aged person, had no diabetes but had hyperinsulinemia. Three of the four affected subjects had hypertension. The pro-band also had reduced body fat and partial lipodystro-phy affecting mainly her extremities (Stephen O’Rahilly, personal communication), however, in depth character-ization of the phenotype related to body fat distribution has not been conducted.
AKT2 belongs to the family of phosphoinositide-dependent serine/threonine kinases and is also known as protein kinase B (PKB) (106). The three isoforms of AKT share more than 80% amino acid identity. AKT1 is almost ubiquitously expressed, whereas AKT2 is pre-dominantly expressed in insulin-sensitive tissues and AKT3 in the testes and brain. As compared to the over-expression of wild-type AKT2 in 3T3-L1 mouse preadi-pocytes, the mutant form, Arg274His, showed markedly reduced lipid accumulation (105). Previously, a knock-out mouse model has shown features of lipodystrophy, insulin resistance and diabetes with increasing age (107). Thus, taken together, lipodystrophy in patients with AKT2 mutations may be related to reduced adipocyte differentiation and to dysfunctional postreceptor insulin signaling.
91.3.2.1.4 Familial Partial Lipodystrophy due to Perilipin 1 (PLIN1) Gene Mutations. Gandotra et al. (108) recently reported two heterozygous frameshift mutations in PLIN1 in three families with FPL of French ancestry. A total of five patients had mutations in PLIN1; and all of them had fatty liver, hypertriglyceridemia and hyperinsulinemia. Three of them had diabetes mellitus. HDL-cholesterol levels were reduced in four of them. Lipodystrophy was most striking in the lower limbs and femorogluteal depot. Acanthosis nigricans was present in

CHAPTER 91 Genetic Lipodystrophies 11
all the probands and two of them also had a cushingoid appearance.
Histology of the sc adipose tissue from four patients revealed reduced size of adipocytes and increased mac-rophage infiltration and adipose tissue fibrosis. Retro-virally transfected preadipocytes (3T3L-1) with mutant PLIN1 showed smaller lipid droplets compared with those transfected with the wild-type PLIN1. Perilipin is the most abundant protein coating lipid droplets in adipocytes. It is essential for formation and maturation of lipid droplets, storage of triglycerides and release of free fatty acids from droplets. Recent data suggest that PLIN1 mutants fail to bind to AB-hydrolase contain-ing 5 (ABHD5), which results in constitutive coactiva-tion of adipose triglyceride lipase and increased basal lipolysis (109).
91.3.2.1.5 Other Types of Familial Partial Lipo-dystrophy. It appears that four loci for FPL, LMNA, PPARG, AKT2 and PLIN1 may not be able to explain the genetic basis of all the patients with FPL and there is likelihood of additional loci (99,100). In-depth charac-terization of the clinical phenotype related to the pattern of loss of fat in FPL patients with mutations in different genes may be helpful in identification of different pheno-types without resorting to molecular diagnosis.91.3.2.2 Atypical Progeroid Syndrome due to LMNA Mutations. Approximately 30 patients with partial or generalized lipodystrophy, insulin resistant diabetes and progeroid features have been reported to harbor mis-sense mutations in the LMNA gene (94,111,112). They also present with mottling, pigmentations and sclerosis of skin, hepatic steatosis, cardiomyopathy and valvular lesions, short stature, and deafness. Lack of breast tissue is prominent in many females while some women report premature ovarian failure.91.3.2.3 Hutchinson–Gilford Progeria Syndrome. Approximately 100 patients have been reported with HGPS so far. These patients appear normal at birth but soon thereafter develop features of early aging even as neonates (113). These features include, severe alopecia, graying of hair, micrognathia, beaked nose, shrill voice, and extensive wrinkling of the skin due to loss of under-lying adipose tissue, poor sexual development, joint con-tractures and severe atherosclerosis (113). Many of them died between the ages of 6 and 20 years. Most of the HGPS patients have synonymous heterozygous mutation Gly608Gly of the LMNA gene (93). This mutation pres-ents a cryptic splice site, which leads to a mutant form of prelamin A with 50 carboxy-terminal amino acid deleted. The mutation occurred de novo in all patients and was demonstrated to be of paternal origin in some of the patients (93). Only one patient had a missense Gly608Ser mutation (93,114,115). Although at birth, the children with HGPS look normal, progressive and generalized loss of body fat occurs later and they develop severe lipodys-trophy with increasing age. The precise pattern of body fat loss in patients with HGPS remains to be studied.
91.3.3 Other Extremely Rare Types of Genetic Lipodystrophies
An autosomal-dominant variety of generalized lipo-dystrophy with acromegaloid features and onset after 18 years of age was reported in a pedigree from Brazil (116). We have also observed lipodystrophy of the lower extremities in two siblings with unbalanced transloca-tion involving chromosome 8p and 10p.
91.4 LONG-TERM COMPLICATIONS
Patients with lipodystrophies are predisposed to long-term complications of diabetes, i.e. nephropathy, reti-nopathy and neuropathy. A few patients with CGL have developed end-stage renal disease requiring renal transplantation (117). Blindness due to retinopathy has also been seen in some. Many patients develop recurrent attacks of acute pancreatitis due to extreme hypertriglyc-eridemia. In some patients, hepatic steatosis can result in further liver dysfunction such as steatohepatitis and cirrhosis. Patients with CGL, type 4 have been reported to have died suddenly most likely due to arrhythmias (39). Some patients with MAD die during childhood of unknown reasons and while some others die during early adulthood due to complications of renal failure due to focal segmental glomerulosclerosis (118,119). Accel-erated atherosclerosis causing coronary heart disease, peripheral vascular disease and cerebrovascular acci-dents has been noted in patients with FPL, particularly among women (6,80,84,120). Other patients with HGPS are also prone to develop severe atherosclerosis.
91.5 TREATMENT OPTIONS
Management of severe insulin resistance and its compli-cations, such as severe diabetes, hypertriglyceridemia, hepatic steatosis, polycystic ovarian disease and acan-thosis nigricans, in patients with lipodystrophies is chal-lenging. Because many patients may have abnormally elevated serum alanine aminotransferase and aspartate aminotransferase levels indicating liver dysfunction, the choice of therapeutic agents may differ. Briefly, various therapeutic options available are as follows.
91.5.1 Diet and Physical Activity
Metabolic complications such as dyslipidemia, diabe-tes and hepatic steatosis can be mitigated with reduced energy intake and increased physical activity. Patients with partial lipodystrophies must avoid gain of excess fat in nonlipodystrophic regions to reduce their risk of developing metabolic complications. However, appetite is difficult to control in young patients with generalized lipodystrophies. Children also require energy for growth and development and thus diet should allow for adequate growth in young patients. For patients with extreme

12 CHAPTER 91 Genetic Lipodystrophies
hypertriglyceridemia, low-fat diet is appropriate to avoid formation of chylomicrons. Whether extremely low-fat diets will be beneficial for CGL patients remains to be investigated. To reduce risk of atherosclerosis, attempt should be made to reduce low-density-lipoprotein cho-lesterol levels (or non-HDL cholesterol levels in hyper-triglyceridemic patients) to minimum by limiting intake of saturated and trans fats as well as cholesterol (121).
91.5.2 Drug Therapy
Diabetes control can be achieved with oral hypoglyce-mic drugs or insulin. Metformin is particularly attrac-tive since it improves insulin sensitivity, reduces appetite and can induce ovulation in patients with polycystic ovarian disease. However, efficacy of metformin ther-apy has not been systematically studied in patients with lipodystrophies. On the other hand, thiazolidinediones such as rosiglitazone and pioglitazone, which are PPARγ agonists, may be particularly attractive for FPL patients with PPARG mutations; however, limited experience in two such patients resulted in equivocal results (101). In most patients with severe insulin resistance, high doses of insulin remain the mainstay of therapy. Rigorous effort to improve glycemic control is needed to manage hypertriglyceridemia.
If hypertriglyceridemia persists despite good glycemic control, fibric acid derivatives (PPARα agonists) such as gemfibrozil, fenofibrate or clofibrate are helpful in reducing serum triglycerides. For those unable to toler-ate fibrates or with liver dysfunction, ω-3 polyunsatu-rated fatty acids from fish oils should be used in high doses (5–10 g/day). In some patients, a combination of low-dose statins and fibrates can be tried for maximal reduction of non-HDL cholesterol levels. Niacin should be avoided as it can induce insulin resistance and can exacerbate hyperglycemia (122). In women, oral estro-gens should also be avoided as they can induce extreme hypertriglyceridemia and acute pancreatitis (6).
Recently, sc recombinant leptin therapy has been reported to be efficacious in improving hyperglyce-mia, dyslipidemia and hepatic steatosis in patients with severe lipodystrophies and hypoleptinemia (8,123–125). Leptin therapy reduces appetite and results in substantial weight loss, which seems to be a primary mechanism for improving metabolic complications (8). However, leptin therapy is still investigational.
REFERENCES
1. Garg, A. Acquired and Inherited Lipodystrophies. N. Engl. J. Med. 2004, 350, 1220–1234.
2. Garg, A. Lipodystrophies: Genetic and Acquired Body Fat Disorders. J. Clin. Endocrinol. Metab. 2011, 96, 3313–3325.
3. Garg, A.; Misra, A. Lipodystrophies: Rare Disorders Caus-ing Metabolic Syndrome. Endocrinol. Metab. Clin. North Am. 2004, 33, 305–331.
4. Garg, A.; Misra, A. Lipodystrophies and Diabetes. In Inter-national Textbook of Diabetes Mellitus; DeFronzo, R. A., Ferrannini, E., Zimmet, P., Eds.; Wiley: New York, 2004; pp 655–672.
5. Chandalia, M.; Garg, A.; Vuitch, F.; Nizzi, F. Postmortem Findings in Congenital Generalized Lipodystrophy. J. Clin. Endocrinol. Metab. 1995, 80, 3077–3081.
6. Haque, W. A.; Vuitch, F.; Garg, A. Post-Mortem Findings in Familial Partial Lipodystrophy, Dunnigan Variety. Diabet. Med. 2002, 19, 1022–1025.
7. Szczepaniak, L. S.; Babcock, E. E.; Schick, F., et al. Mea-surement of Intracellular Triglyceride Stores by 1H Spec-troscopy: Validation In Vivo. Am. J. Phys. 1999, 276, E977–E989.
8. Oral, E. A.; Simha, V.; Ruiz, E., et al. Leptin-Replacement Therapy for Lipodystrophy. N. Engl. J. Med. 2002, 346, 570–578.
9. Mora, P. F.; Ramirez, L. C.; Lender, D.; Raskin, P. Insu-lin Requirements in Lipodystrophic Diabetes. Diabet. Med. 1993, 10, 863–865.
10. Garg, A.; Chandalia, M.; Vuitch, F. Severe Islet Amyloido-sis in Congenital Generalized Lipodystrophy. Diabetes Care. 1996, 19, 28–31.
11. Berardinelli, W. An Undiagnosed Endocrinometabolic Syn-drome: Report of 2 Cases. J. Clin. Endocrinol. Metab. 1954, 14, 193–204.
12. Seip, M. Lipodystrophy and Gigantism with Associated Endocrine Manifestations: A New Diencephalic Syn-drome? Acta Paediatr. 1959, 48, 555–574.
13. Magre, J.; Delepine, M.; Khallouf, E., et al. Identification of the Gene Altered in Berardinelli–Seip Congenital Lipo-dystrophy on Chromosome 11q13. Nat. Genet. 2001, 28, 365–370.
14. Gomes, K. B.; Fernandes, A. P.; Ferreira, A. C., et al. Muta-tions in the Seipin and AGPAT2 Genes Clustering in Con-sanguineous Families with Berardinelli–Seip Congenital Lipodystrophy from Two Separate Geographical Regions of Brazil. J. Clin. Endocrinol. Metab. 2004, 89, 357–361.
15. Fleckenstein, J. L.; Garg, A.; Bonte, F. J.; Vuitch, M. F.; Peshock, R. M. The Skeleton in Congenital, Generalized Lipodystrophy: Evaluation Using Whole-Body Radiographic Surveys, Magnetic Resonance Imaging and Technetium-99m Bone Scintigraphy. Skeletal Radiol. 1992, 21, 381–386.
16. Seip, M.; Trygstad, O. Generalized Lipodystrophy, Congeni-tal and Acquired (Lipoatrophy). Acta Paediatr. Suppl. 1996, 413, 2–28.
17. Agarwal, A. K.; Arioglu, E.; de Almeida, S., et al. AGPAT2 Is Mutated in Congenital Generalized Lipodystrophy Linked to Chromosome 9q34. Nat. Genet. 2002, 31, 21–23.
18. Agarwal, A. K.; Simha, V.; Oral, E. A., et al. Phenotypic and Genetic Heterogeneity in Congenital Generalized Lipodys-trophy. J. Clin. Endocrinol. Metab. 2003, 88, 4840–4847.
19. Van Maldergem, L.; Magre, J.; Khallouf, T. E., et al. Genotype– Phenotype Relationships in Berardinelli–Seip Congenital Lipo-dystrophy. J. Med. Genet. 2002, 39, 722–733.
20. Haque, W. A.; Shimomura, I.; Matsuzawa, Y.; Garg, A. Serum Adiponectin and Leptin Levels in Patients with Lipodystro-phies. J. Clin. Endocrinol. Metab. 2002, 87, 2395–2398.
21. Garg, A.; Wilson, R.; Barnes, R., et al. A Gene for Congenital Generalized Lipodystrophy Maps to Human Chromosome 9q34. J. Clin. Endocrinol. Metab. 1999, 84, 3390–3394.
22. Kim, C. A.; Delepine, M.; Boutet, E., et al. Association of a Homozygous Nonsense Caveolin-1 Mutation with Berardinelli–Seip Congenital Lipodystrophy. J. Clin. Endo-crinol. Metab. 2008, 93, 1129–1134.
23. Hayashi, Y. K.; Matsuda, C.; Ogawa, M., et al. Human PTRF Mutations Cause Secondary Deficiency of Caveolins Result-

CHAPTER 91 Genetic Lipodystrophies 13
ing in Muscular Dystrophy with Generalized Lipodystrophy. J. Clin. Invest. 2009, 119, 2623–2633.
24. Leung, D. W. The Structure and Functions of Human Lyso-phosphatidic Acid Acyltransferases. Front. Biosci. 2001, 6, d944–d953.
25. Li, D.; Yu, L.; Wu, H., et al. Cloning and Identification of the Human LPAAT-Zeta Gene, a Novel Member of the Lyso-phosphatidic Acid Acyltransferase Family. J. Hum. Genet. 2003, 48, 438–442.
26. Agarwal, A. K.; Garg, A. Congenital Generalized Lipodys-trophy: Significance of Triglyceride Biosynthetic Pathways. Trends Endocrinol. Metab. 2003, 14, 214–221.
27. West, J.; Tompkins, C. K.; Balantac, N., et al. Cloning and Expression of Two Human Lysophosphatidic Acid Acyl-transferase cDNAs that Enhance Cytokine-Induced Signaling Responses in Cells. DNA Cell Biol. 1997, 16, 691–701.
28. Lewin, T. M.; Wang, P.; Coleman, R. A. Analysis of Amino Acid Motives Diagnostic for the Sn-Glycerol-3-Phosphate Acyltransferase Reaction. Biochemistry 1999, 38, 5764–5771.
29. Haque, W.; Garg, A.; Agarwal, A. K. Enzymatic Activ-ity of Naturally Occurring 1-Acylglycerol-3-Phosphate-O- Acyltransferase 2 Mutants Associated with Congenital Gen-eralized Lipodystrophy. Biochem. Biophys. Res. Commun. 2005, 327, 446–453.
30. Agarwal, A. K.; Garg, A. Seipin: A Mysterious Protein. Trends Mol. Med. 2004, 10, 440–444.
31. Windpassinger, C.; Auer-Grumbach, M.; Irobi, J., et al. Het-erozygous Missense Mutations in BSCL2 Are Associated with Distal Hereditary Motor Neuropathy and Silver Syn-drome. Nat. Genet. 2004, 36, 271–276.
32. Szymanski, K. M.; Binns, D.; Bartz, R., et al. The Lipodys-trophy Protein Seipin Is Found at Endoplasmic Reticulum Lipid Droplet Junctions and Is Important for Droplet Mor-phology. Proc. Natl. Acad. Sci. U.S.A. 2007, 104, 20890–20895.
33. Fei, W.; Shui, G.; Gaeta, B., et al. Fld1p, A Functional Homologue of Human Seipin, Regulates the Size of Lipid Droplets in Yeast. J. Cell Biol. 2008, 180, 473–482.
34. Payne, V. A.; Grimsey, N.; Tuthill, A., et al. The Human Lipodystrophy Gene BSCL2/Seipin May Be Essential for Normal Adipocyte Differentiation. Diabetes 2008, 57, 2055–2060.
35. Garg, A.; Agarwal, A. K. Caveolin-1: A New Locus for Human Lipodystrophy. J. Clin. Endocrinol. Metab. 2008, 93, 1183–1185.
36. Simha, V.; Garg, A. Phenotypic Heterogeneity in Body Fat Distribution in Patients with Congenital Generalized Lipo-dystrophy Due to Mutations in the AGPAT2 or Seipin Genes. J. Clin. Endocrinol. Metab. 2003, 88, 5433–5437.
37. Garg, A.; Fleckenstein, J. L.; Peshock, R. M.; Grundy, S. M. Peculiar Distribution of Adipose Tissue in Patients with Congenital Generalized Lipodystrophy. J. Clin. Endocrinol. Metab. 1992, 75, 358–361.
38. Shastry, S.; Delgado, M. R.; Dirik, E.; Turkmen, M.; Agar-wal, A. K.; Garg, A. Congenital Generalized Lipodystrophy, Type 4 (CGL4) Associated with Myopathy Due to Novel PTRF Mutations. Am. J. Med. Genet. A 2010, 152A, 2245–2253.
39. Rajab, A.; Straub, V.; McCann, L. J., et al. Fatal Cardiac Arrhythmia and Long-QT Syndrome in a New Form of Con-genital Generalized Lipodystrophy with Muscle Rippling (CGL4) Due to PTRF-CAVIN Mutations. PLoS. Genet. 2010, 6, e1000874.
40. Simha, V.; Agarwal, A. K.; Aronin, P. A.; Iannaccone, S. T.; Garg, A. Novel Subtype of Congenital Generalized Lipo-dystrophy Associated with Muscular Weakness and Cer-
vical Spine Instability. Am. J. Med. Genet. A 2008, 146A, 2318–2326.
41. Simha, V.; Garg, A. Body Fat Distribution and Metabolic Derangements in Patients with Familial Partial Lipodys-trophy Associated with Mandibuloacral Dysplasia. J. Clin. Endocrinol. Metab. 2002, 87, 776–785.
42. Novelli, G.; Muchir, A.; Sangiuolo, F., et al. Mandibuloac-ral Dysplasia Is Caused by a Mutation in LMNA-Encoding Lamin A/C. Am. J. Hum. Genet. 2002, 71, 426–431.
43. Lin, F.; Worman, H. J. Structural Organization of the Human Gene Encoding Nuclear Lamin A and Nuclear Lamin C. J. Biol. Chem. 1993, 268, 16321–16326.
44. Fisher, D. Z.; Chaudhary, N.; Blobel, G. cDNA Sequencing of Nuclear Lamins A and C Reveals Primary and Second-ary Structural Homology to Intermediate Filament Proteins. Proc. Natl. Acad. Sci. U.S.A. 1986, 83, 6450–6454.
45. Burke, B.; Stewart, C. L. Life at the Edge: The Nuclear Enve-lope and Human Disease. Nat. Rev. Mol. Cell Biol. 2002, 3, 575–585.
46. Shen, J. J.; Brown, C. A.; Lupski, J. R.; Potocki, L. Mandibu-loacral Dysplasia Caused by Homozygosity for the R527H Mutation in Lamin A/C. J. Med. Genet. 2003, 40, 854–857.
47. Cao, H.; Hegele, R. A. LMNA Is Mutated in Hutchinson-Gilford Progeria (MIM 176670) but not in Wiedemann–Rautenstrauch Progeroid Syndrome (MIM 264090). J. Hum. Genet. 2003, 48, 271–274.
48. Plasilova, M.; Chattopadhyay, C.; Pal, P., et al. Homozy-gous Missense Mutation in the Lamin A/C Gene Causes Autosomal Recessive Hutchinson–Gilford Progeria Syn-drome. J. Med. Genet. 2004, 41, 609–614.
49. Pendas, A. M.; Zhou, Z.; Cadinanos, J., et al. Defective Prelamin A Processing and Muscular and Adipocyte Altera-tions in Zmpste24 Metalloproteinase-Deficient Mice. Nat. Genet. 2002, 31, 94–99.
50. Bergo, M. O.; Gavino, B.; Ross, J., et al. Zmpste24 Defi-ciency in Mice Causes Spontaneous Bone Fractures, Muscle Weakness, and a Prelamin A Processing Defect. Proc. Natl. Acad. Sci. U.S.A. 2002, 99, 13049–13054.
51. Agarwal, A. K.; Fryns, J. P.; Auchus, R. J.; Garg, A. Zinc Metalloproteinase, ZMPSTE24, Is Mutated in Mandibuloa-cral Dysplasia. Hum. Mol. Genet. 2003, 12, 1995–2001.
52. Sinensky, M.; Fantle, K.; Trujillo, M.; McLain, T.; Kupfer, A.; Dalton, M. The Processing Pathway of Prelamin A. J. Cell Sci. 1994, 107 (Pt 1), 61–67.
53. Fong, L. G.; Ng, J. K.; Meta, M., et al. Heterozygosity for Lmna Deficiency Eliminates the Progeria-Like Phenotypes in Zmpste24-Deficient Mice. Proc. Natl. Acad. Sci. U.S.A. 2004, 101, 18111–18116.
54. Garg, A.; Hernandez, M. D.; Sousa, A. B., et al. An Autosomal Recessive Syndrome of Joint Contractures, Muscular Atrophy, Microcytic Anemia, and Panniculitis-Associated Lipodystro-phy. J. Clin. Endocrinol. Metab. 2010, 95, E58–E63.
55. Horikoshi, A.; Iwabuchi, S.; Iizuka, Y.; Hagiwara, T.; Amaki, I. A Case of Partial Lipodystrophy with Erythema, Dactylic Deformities, Calcification of the Basal Ganglia, Immunologi-cal Disorders and Low IQ Level (Author’s Transl). Rinsho Shinkeigaku—Clinical Neurology 1980, 20, 173–180.
56. Tanaka, M.; Miyatani, N.; Yamada, S., et al. Hereditary Lipo-Muscular Atrophy with Joint Contracture, Skin Erup-tions and Hyper-Gamma-Globulinemia: A New Syndrome. Intern. Med. 1993, 32, 42–45.
57. Agarwal, A. K.; Xing, C.; DeMartino, G. N., et al. PSMB8 Encoding the Beta5i Proteasome Subunit Is Mutated in Joint Contractures, Muscle Atrophy, Microcytic Anemia, and Panniculitis-Induced Lipodystrophy Syndrome. Am. J. Hum. Genet. 2010, 87, 866–872.
58. Rivett, A. J.; Hearn, A. R. Proteasome Function in Anti-gen Presentation: Immunoproteasome Complexes, Peptide

14 CHAPTER 91 Genetic Lipodystrophies
Production, and Interactions with Viral Proteins. Curr. Pro-tein Pept. Sci. 2004, 5, 153–161.
59. Kitamura, A.; Maekawa, Y.; Uehara, H., et al. A Mutation in the Immunoproteasome Subunit PSMB8 Causes Autoin-flammation and Lipodystrophy in Humans. J. Clin. Invest. 2011, 121, 4150–4160.
60. Arima, K.; Kinoshita, A.; Mishima, H., et al. Proteasome Assembly Defect Due to a Proteasome Subunit Beta Type 8 (PSMB8) Mutation Causes the Autoinflammatory Disorder, Nakajo–Nishimura Syndrome. Proc. Natl. Acad. Sci. U.S.A. 2011, 108, 14914–14919.
61. Torrelo, A.; Patel, S.; Colmenero, I., et al. Chronic Atypical Neutrophilic Dermatosis with Lipodystrophy and Elevated Temperature (CANDLE) Syndrome. J. Am. Acad. Dermatol. 2010, 62, 489–495.
62. Ramot, Y.; Czarnowicki, T.; Maly, A.; Navon-Elkan, P.; Zlotogorski, A. Chronic Atypical Neutrophilic Dermatosis with Lipodystrophy and Elevated Temperature Syndrome: A Case Report. Pediatr. Dermatol. 2010, epub ahead of print.
63. Liu, Y.; Ramot, Y.; Torrelo, A., et al. Mutations in PSMB8 Cause CANDLE Syndrome with Evidence of Genetic and Phenotypic Heterogeneity. Arthritis. Rheum. 2011.
64. Rubio-Cabezas, O.; Puri, V.; Murano, I., et al. Partial Lipo-dystrophy and Insulin Resistant Diabetes in a Patient with a Homozygous Nonsense Mutation in CIDEC. EMBO Mol. Med. 2009, 1, 280–287.
65. Nishino, N.; Tamori, Y.; Tateya, S., et al. FSP27 Contributes to Efficient Energy Storage in Murine White Adipocytes by Promoting the Formation of Unilocular Lipid Droplets. J. Clin. Invest. 2008, 118, 2808–2821.
66. Sensenbrenner, J. A.; Hussels, I. E.; Levin, L. S. CC—A Low Birthweight Syndrome, Rieger Syndrome. Birth Defects 1975, 11, 423–426.
67. Gorlin, R. J.; Cervenka, J.; Moller, K.; Horrobin, M.; Witkop, J. Rieger Anomaly and Growth Retardation (The S-H-O-R-T Syndrome). Birth Defects 1975, 11, 46–48.
68. Sorge, G.; Ruggieri, M.; Polizzi, A.; Scuderi, A.; Di Pietro, M. SHORT Syndrome: A New Case with Probable Auto-somal Dominant Inheritance. Am. J. Med. Genet. 1996, 61, 178–181.
69. Bankier, A.; Keith, C. G.; Temple, I. K. Absent Iris Stroma, Narrow Body Build and Small Facial Bones: A New Associa-tion or Variant of SHORT Syndrome? Clin. Dysmorphol. 1995, 4, 304–312.
70. Aarskog, D.; Ose, L.; Pande, H.; Eide, N. Autosomal Domi-nant Partial Lipodystrophy Associated with Rieger Anom-aly, Short Stature, and Insulinopenic Diabetes. Am. J. Med. Genet. 1983, 15, 29–38.
71. Shastry, S.; Simha, V.; Godbole, K., et al. A Novel Syn-drome of Mandibular Hypoplasia, Deafness, and Progeroid Features Associated with Lipodystrophy, Undescended Tes-tes, and Male Hypergonadism. J. Clin. Endocrinol. Metab. 2010, 95, E192–E197.
72. Rautenstrauch, T.; Snigula, F.; Krieg, T.; Gay, S.; Muller, P. K. Progeria: A Cell Culture Study and Clinical Report of Familial Incidence. Eur. J. Pediatr. 1971, 124, 101–111.
73. Wiedemann, H. R. An Unidentified Neonatal Progeroid Syn-drome: Follow-Up Report. Eur. J. Pediatr. 1979, 130, 65–70.
74. Pivnick, E. K.; Angle, B.; Kaufman, R. A., et al. Neonatal Progeroid (Wiedemann–Rautenstrauch) Syndrome: Report of Five New Cases and Review. Am. J. Med. Genet. 2000, 90, 131–140.
75. Korniszewski, L.; Nowak, R.; Okninska-Hoffmann, E.; Skorka, A.; Gieruszczak-Bialek, D.; Sawadro-Rochowska, M. Wiedemann–Rautenstrauch (Neonatal Progeroid) Syn-drome: New Case with Normal Telomere Length in Skin Fibroblasts. Am. J. Med. Genet. 2001, 103, 144–148.
76. Hoppen, T.; Naumann, A.; Theile, U.; Rister, M. Siblings with Neonatal Progeroid Syndrome (Wiedemann–Rautenstrauch). Klin. Padiatr. 2004, 216, 70–71.
77. Thorey, F.; Jager, M.; Seller, K.; Krauspe, R.; Wild, A. Kyphoscoliosis in Wiedemann–Rautenstrauch Syndrome (Neonatal Progeroid Syndrome). Z. Orthop. Ihre. Grenzgeb. 2003, 141, 341–344.
78. Ozer, F. L.; Lichtenstein, J. R.; Kwiterovich, P. O.; McKu-sick, V. A. A New Genetic Variety of Lipodystrophy. Clin. Res. 1973, 21, 533 (abstract).
79. Dunnigan, M. G.; Cochrane, M. A.; Kelly, A.; Scott, J. W. Familial Lipoatrophic Diabetes with Dominant Transmis-sion. A New Syndrome. Q. J. Med. 1974, 43, 33–48.
80. Garg, A. Gender Differences in the Prevalence of Metabolic Complications in Familial Partial Lipodystrophy (Dunnigan Variety). J. Clin. Endocrinol. Metab. 2000, 85, 1776–1782.
81. Garg, A. Lipodystrophies. Am. J. Med. 2000, 108, 143–152. 82. Garg, A.; Peshock, R. M.; Fleckenstein, J. L. Adipose Tissue
Distribution in Patients with Familial Partial Lipodystrophy (Dunnigan Variety). J. Clin. Endocrinol. Metab. 1999, 84, 170–174.
83. Haque, W. A.; Oral, E. A.; Dietz, K.; Bowcock, A. M.; Agarwal, A. K.; Garg, A. Risk Factors for Diabetes in Famil-ial Partial Lipodystrophy, Dunnigan Variety. Diabetes Care 2003, 26, 1350–1355.
84. Hegele, R. A. Premature Atherosclerosis Associated with Monogenic Insulin Resistance. Circulation 2001, 103, 2225–2229.
85. Garg, A.; Speckman, R. A.; Bowcock, A. M. Multisystem Dystrophy Syndrome Due to Novel Missense Mutations in the Amino-Terminal Head and Alpha-Helical Rod Domains of the Lamin A/C Gene. Am. J. Med. 2002, 112, 549–555.
86. Peters, J. M.; Barnes, R.; Bennett, L.; Gitomer, W. M.; Bowcock, A. M.; Garg, A. Localization of the Gene for Familial Partial Lipodystrophy (Dunnigan Variety) to Chromosome 1q21–22. Nat. Genet. 1998, 18, 292–295.
87. Cao, H.; Hegele, R. A. Nuclear Lamin A/C R482Q Mutation in Canadian Kindreds with Dunnigan-Type Familial Partial Lipodystrophy. Hum. Mol. Genet. 2000, 9, 109–112.
88. Speckman, R. A.; Garg, A.; Du, F., et al. Mutational and Haplotype Analyses of Families with Familial Partial Lipo-dystrophy (Dunnigan Variety) Reveal Recurrent Missense Mutations in the Globular C-Terminal Domain of Lamin A/C. Am. J. Hum. Genet. 2000, 66, 1192–1198.
89. Shackleton, S.; Lloyd, D. J.; Jackson, S. N., et al. LMNA, Encoding Lamin A/C, Is Mutated in Partial Lipodystrophy. Nat. Genet. 2000, 24, 153–156.
90. Bonne, G.; Di Barletta, M. R.; Varnous, S., et al. Mutations in the Gene Encoding Lamin A/C Cause Autosomal Domi-nant Emery–Dreifus Muscular Dystrophy. Nat. Genet. 1999, 21, 285–288.
91. di Barletta, M.; Ricci, E.; Galluzzi, G., et al. Different Muta-tions in the LMNA Gene Cause Autosomal Dominant and Autosomal Recessive Emery-Dreifuss Muscular Dystrophy. Am. J. Hum. Genet. 2000, 66, 1407–1412.
92. Muchir, A.; Bonne, G.; van der Kooi, A. J., et al. Identifi-cation of Mutations in the Gene Encoding Lamins A/C in Autosomal Dominant Limb Girdle Muscular Dystrophy with Atrioventricular Conduction Disturbances (LGMD1B). Hum. Mol. Genet. 2000, 9, 1453–1459.
93. Eriksson, M.; Brown, W. T.; Gordon, L. B., et al. Recurrent De Novo Point Mutations in Lamin A Cause Hutchinson-Gilford Progeria Syndrome. Nature 2003, 423, 293–298.
94. Chen, L.; Lee, L.; Kudlow, B. A., et al. LMNA Mutations in Atypical Werner’s Syndrome. Lancet 2003, 362, 440–445.
95. De Sandre-Giovannoli, A.; Chaouch, M.; Kozlov, S., et al. Homozygous Defects in LMNA, Encoding Lamin A/C Nuclear-Envelope Proteins, Cause Autosomal Recessive

Axonal Neuropathy in Human (Charcot–Marie–Tooth Dis-order Type 2) and Mouse. Am. J. Hum. Genet. 2002, 70, 726–736.
96. Vigouroux, C.; Bourut, C.; Guerci, B., et al. A New Mis-sense Mutation in the Calcium-Sensing Receptor in Familial Benign Hypercalcaemia Associated with Partial Lipoatrophy and Insulin Resistant Diabetes. Clin. Endocrinol. 2000, 53, 393–398.
97. Garg, A.; Vinaitheerthan, M.; Weatherall, P.; Bowcock, A. Phenotypic Heterogeneity in Patients with Familial Partial Lipodystrophy (Dunnigan Variety) Related to the Site of Mis-Sense Mutations in Lamin A/C (LMNA) Gene. J. Clin. Endocrinol Metab. 2001, 86, 59–65.
98. Vantyghem, M. C.; Pigny, P.; Maurage, C. A., et al. Patients with Familial Partial Lipodystrophy of the Dunnigan Type Due to a LMNA R482W Mutation Show Muscular and Car-diac Abnormalities. J. Clin. Endocrinol. Metab. 2004, 89, 5337–5346.
99. Agarwal, A. K.; Garg, A. A Novel Heterozygous Mutation in Peroxisome Proliferator-Activated Receptor-γ Gene in a Patient with Familial Partial Lipodystrophy. J. Clin. Endo-crinol. Metab. 2002, 87, 408–411.
100. Hegele, R. A.; Cao, H.; Frankowski, C.; Mathews, S. T.; Leff, T. PPARG F388L, A Transactivation-Deficient Mutant, in Familial Partial Lipodystrophy. Diabetes 2002, 51, 3586–3590.
101. Savage, D. B.; Tan, G. D.; Acerini, C. L., et al. Human Metabolic Syndrome Resulting From Dominant-Negative Mutations in the Nuclear Receptor Peroxisome Proliferator-Activated Receptor-Gamma. Diabetes 2003, 52, 910–917.
102. Al-Shali, K. Z.; House, A. A.; Hanley, A. J., et al. Genetic Variation in PPARG Encoding Peroxisome Proliferator- Activated Receptor Gamma Associated with Carotid Athero-sclerosis. Stroke 2004, 35, 2036–2040.
103. Rosen, E. D.; Sarraf, P.; Troy, A. E., et al. PPAR Gamma Is Required for the Differentiation of Adipose Tissue In Vivo and In Vitro. Mol. Cell 1999, 4, 611–617.
104. Knouff, C.; Auwerx, J. Peroxisome Proliferator-Activated Receptor-Gamma Calls for Activation in Moderation: Les-sons from Genetics and Pharmacology. Endocr. Rev. 2004, 25, 899–918.
105. George, S.; Rochford, J. J.; Wolfrum, C., et al. A Family with Severe Insulin Resistance and Diabetes Due to a Mutation in AKT2. Science 2004, 304, 1325–1328.
106. Vanhaesebroeck, B.; Alessi, D. R. The PI3K-PDK1 Connec-tion: More than Just a Road to PKB. Biochem. J. 2000, 346 (Pt 3), 561–576.
107. Garofalo, R. S.; Orena, S. J.; Rafidi, K., et al. Severe Dia-betes, Age-Dependent Loss of Adipose Tissue, and Mild Growth Deficiency in Mice Lacking Akt2/PKB Beta. J. Clin. Invest. 2003, 112, 197–208.
108. Gondotra, S.; Le Dour, C.; Bottomley, W., et al. Perilipin Deficiency and Autosomal Dominant Partial Lipodystrophy. N. Engl. J. Med. 2011, 364, 740–748.
109. Gondotra, S.; Lim, K.; Girousse, A., et al. Human Frame Shift Mutations Affecting the Carboxyl Terminus of Perilipin Increase Lipolysis by Failing to Sequester the Adipose Triglyc-eride Lipase (ATGL) Coactivator AB-Hydrolase-Containing 5 (ABHD5). J. Biol. Chem. 2011, 286, 34998–35006.
110. Herbst, K. L.; Tannock, L. R.; Deeb, S. S.; Purnell, J. Q.; Brunzell, J. D.; Chait, A. Kobberling Type of Familial Partial
CHAPTER 91 Genetic Lipodystrophies 15
Lipodystrophy: An Underrecognized Syndrome. Diabetes Care. 2003, 26, 1819–1824.
111. Caux, F.; Dubosclard, E.; Lascols, O., et al. A New Clinical Condition Linked to a Novel Mutation in Lamins A and C with Generalized Lipoatrophy, Insulin-Resistant Diabetes, Disseminated Leukomelanodermic Papules, Liver Steatosis, and Cardiomyopathy. J. Clin. Endocrinol. Metab. 2003, 88, 1006–1013.
112. Herbst, K. L.; Tannock, L. R.; Deeb, S. S., et al. Kobberling Type of Familial Partial Lipodystrophy: an Underrecognized Syndrome. Diabetes Care. 2003, 26, 1819–1824.
113. Pollex, R. L.; Hegele, R. A. Hutchinson–Gilford Progeria Syndrome. Clin. Genet. 2004, 66, 375–381.
114. D’Apice, M. R.; Tenconi, R.; Mammi, I.; van den Ende, J.; Novelli, G. Paternal Origin of LMNA Mutations in Hutchinson–Gilford Progeria. Clin. Genet. 2004, 65, 52–54.
115. De Sandre-Giovannoli, A.; Bernard, R.; Cau, P., et al. Lamin a Truncation in Hutchinson–Gilford Progeria. Science 2003, 300, 2055.
116. Pardini, V. C.; Victoria, I. M.; Rocha, S. M., et al. Leptin Levels, Beta-Cell Function, and Insulin Sensitivity in Fami-lies with Congenital and Acquired Generalized Lipoatrophic Diabetes. J. Clin. Endocrinol. Metab. 1998, 83, 503–508.
117. McNally, M.; Mannon, R. B.; Javor, E. D., et al. Successful Renal Transplantation in a Patient with Congenital Gener-alized Lipodystrophy: A Case Report. Am. J. Transplant. 2004, 4, 447–449.
118. Ahmad, Z.; Zackai, E.; Medne, L.; Garg, A. Early Onset Mandibuloacral Dysplasia Due to Compound Heterozy-gous Mutations in ZMPSTE24. Am. J. Med. Genet. A 2010, 152A, 2703–2710.
119. Agarwal, A. K.; Zhou, X. J.; Hall, R. K., et al. Focal Segmen-tal Glomerulosclerosis in Patients with Mandibuloacral Dys-plasia Due to Zinc Metalloproteinase Deficiency. J. Investig. Med. 2006, 54, 208–213.
120. Misra, A.; Garg, A. Clinical Features and Metabolic Derangements in Acquired Generalized Lipodystrophy: Case Reports and Review of the Literature. Medicine 2003, 82, 129–146.
121. Expert Panel on Detection E Treatment of High Blood Cho-lesterol in A. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). [see comments]; JAMA 2001, 285, 2486–2497.
122. Garg, A.; Grundy, S. M. Nicotinic Acid as Therapy for Dyslipidemia in Non-Insulin-Dependent Diabetes Mellitus. JAMA 1990, 264, 723–726.
123. Simha, V.; Szczepaniak, L. S.; Wagner, A. J.; DePaoli, A. M.; Garg, A. Effect of Leptin Replacement on Intrahepatic and Intramyocellular Lipid Content in Patients with Generalized Lipodystrophy. Diabetes Care. 2003, 26, 30–35.
124. Petersen, K. F.; Oral, E. A.; Dufour, S., et al. Leptin Reverses Insulin Resistance and Hepatic Steatosis in Patients with Severe Lipodystrophy. J. Clin. Invest. 2002, 109, 1345–1350
125. Simha, V.; Subramanyam, L.; Szczepaniak, L., et al. Compar-ison of Efficacy and Safety of Leptin Replacement Therapy in Moderately and Severely Hypoleptinemic Patients with Familial Partial Lipodystrophy of the Dunnigan Variety. J. Clin. Endocrinol. Metab. 2012, 97, 785–792.

16 CHAPTER 91 Genetic Lipodystrophies
Biography
Abhimanyu Garg, MD is a professor of Internal Medicine and is Chief, Division of Nutri-tion and Metabolic Diseases at UT Southwestern. He holds a Distinguished Chair in Human Nutrition Research. Dr Garg’s research has focused on the problems of nutrition for patients with diabetes and management of dyslipidemia in patients with type 2 diabetes. In addition, he has contributed to the understanding of the relationship of body fat distribution and insulin resistance. He has carefully characterized the phenotype of various disorders of adipose tissue, called lipodystrophies, which has led to discovery of many novel genes for these disorders. Dr Garg’s group identified deficiency of AGPAT2 enzyme, which is critical for triglyceride and phospholipid biosynthesis, as the cause of congenital generalized lipodystrophy, type 1. His group also linked peroxisome proliferator-activated receptor-γ gene, the key adipocyte differentiation transcription factor, to familial partial lipodystrophy. His team has also identi-fied the second locus for mandibuloacral dysplasia, i.e. zinc metalloproteinase (ZMPSTE24), that is responsible for posttranslational processing of prelamin A to its mature form lamin A. Recently, he discovered mutation in proteasome subunit, beta-type 8 (PSMB8) as the underly-ing basis of a novel autoinflammatory lipodystrophy syndrome. He demonstrated that patients with generalized lipodystrophy have profound leptin deficiency and proposed that leptin defi-ciency might contribute to the metabolic complications in the disorder. This led him to initiate a collaborative trial that demonstrated dramatic improvement in hyperglycemia, dyslipidemia, and fatty liver with leptin therapy.