Emergency Department Management of Syncope Emilia McGhee Sept 2010.
-
Upload
abraham-carson -
Category
Documents
-
view
229 -
download
0
Transcript of Emergency Department Management of Syncope Emilia McGhee Sept 2010.

Emergency Department Management of Syncope
Emilia McGheeSept 2010

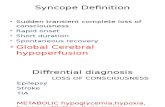
Syn.co.pe
A transient loss of consciousness and inability to maintain postural tone due to global cerebral hypoperfusion.
Characterised by a rapid onset, short duration and spontaneous complete recovery

Incidence
• 1-3 % Emergency Dept visits• 6 % of hospital admissions• USA, Japan and Europe• Occurs in up to 50% during lifetime (only 5%
after 40 yrs)• Recurs in 30%

• Due to cerebral hypoperfusion causing lack of oxygen and glucose supplly to brain
• Cerebral perfusion maintained by:– Cardiac output– Systemic vascular resistance– Mean arterial pressure– Intravascular volume– Cerebrovascular resistance with intrinsic
autoregulation– Metabolic regulation

What is not syncope
Transient LoC without global cerebral hypoperfusion
• Seizure• TIA• Metabolic disorders• Intoxication
Loss of postural tone without LoC
• Cataplexy• Drop attacks• Falls• TIA of carotid origin• Functional -
psychogenic

Syncope vs
• Triggering factor• Prodrome• Convulsion after LoC, and
<15 secs• Short duration• Quick recovery• Ongoing lethargy but no
confusion
Seizure
• Pt history• Aura• Automatisms• Convulsions at onset of LoC• Longer duration• Post-ictal phase• Tongue biting, incontinence

Classification
• Reflex – neurally mediated – 30%• Orthostatic hypotension – 10-15 %• Cardiac – electrical and mechanical – 10%

Reflex• Vasovagal
– Emotional stress– Orthostatic stress
• Situational– Coughing, micturition– GI stimulation– Post exercise, post prandial
• Carotid sinus syncope– Uncommon, caused by pressure on carotid sinus– Head turning, tight collars shaving


Orthostatic Hypotension
• Primary autonomic failure– Pure auntonomic failure, multisystem atrophy,
Parkinson’s Disease, Lewy body dementia• Secondary autonomic failure
– Diabetes, amyloidosis, uraemia, spinal cord injuries• Drug induced
– Alcohol, vasodilators, diuretics, phenothiazines, antidepressants
• Volume depletion– Vommitting, diarrhoea, dehydration, haemorrhage


“Syncope and sudden death are the same, except that in one you wake up”

Cardiac - Electrical• Ventricular arrhythmias
– VT, Torsades– Sudden onset, little prodrome– Elderly pts with known cardiac disease
• Supraventricular arrhythmias– SVT, AF with fast ventricular response– Assoc with palpitations, chest pain, dyspnoea– May occur on attempting to stand or walk– Look for evidence of WPW, Brugada, Long QT
• Bradyarrhythmias– Sick sinus, sinus brady, high grade AV block, adverse medication
reactions, pacemaker malfunction– Chest pain, dyspnoea, decreased ET, fatigue

Cardiac - Mechanical
• Low CO output states– Cardiomyopathy, CCF, valvular insufficiency
• Cardiac outflow obstruction– Sudden onset, no prodrome– Exertional in nature, murmur present– Aortic stenosis, HOCM, Mitral stenosis, pulmonary
stenosis, pulmonary embolism, Lt atrial myxoma

HOCM
• Causes of syncope:– Self terminating ventricular arrhythmias– SVT– Severe outflow tract obstruction– Bradyarrhythmia– Hypotension in response to exercise– Reflex syncope

Emergency Department Assessment
• 45% can be diagnosed on history and exam alone
• A cause will not be found for around 37%• Management is moving away from firm
diagnosis to risk stratification of patients

Aim in ED
1) Recognise life threatening conditions2) Recognise low risk conditions for discharge3) Chose appropriate FU for those who need
further diagnostic testing4) Recognise those who do not need further
investigation

History – High Yield Questions
• What were they doing - at rest (arrhythmia) - exercise / post-exercise (AS, HOCM) - laughing, micturition etc• Was there a prodrome? - vasovagal• Did they have palpitations? - an arrhythmia

• Were they SOB? - PE - tamponade• Did they have chest pain? - PE - ACS and an arrhythmia - dissection• Did they have abdominal pain? - AAA - ectopic• Did they have a headache? - SAH

• Previous arrythmias• Known CAD• Sudden or unexplained deaths in family• Known CCF• Medications - QT prolonging medications - vasodilators - anti-hypertnesives

Red Flags
• Syncope during exertion• Syncope in lying position• Absence of external factors• Family hx of SCD• Slow recovery from syncope

Examination and bedside tests
• Cardiorespiratory exam• Abdominal exam• Neurological exam• BSL• Orthostatic BP
– A drop of 20mmHg systolic, 10mmHG diastolic or increase in HR >20
– Systolic BP <90mmHg– Meaningful if they become symptomatic

Ix that are helpful• ECG
Consider on case to case basis:• FBC, EUC• Troponin, D.dimer, bHCG• UA• CXR• Echo• CSM• Tilt table• EPS• EST

Ix that are generally low yield
• CTB• MRI• Holter monitor• Carotid dopplers• EEG


Important ECG findings
• Evidence of AV conduction disorder– Prolonged PR– Mobitz 1 or 2 – CHB– RBBB or LBBB
• Evidence of underlying cardiac disease– Rt or Lt axis deviation– Significant ST or T wave changes– Rt or Lt ventricular hypertrophy

ECG findings associated with high risk of sudden cardiac death
• Hypertrophic cardiomyopathy• Long QT• Ventricular pre-excitation (WPW)• Brugada Syndrome• Short QT• Arrhythmogenic Rt ventricular dysplasia

ECG changes in HOCM
• Normal in up to 15%• Left axis deviation• LVH and strain• flipped T’s• big voltage R waves and deep, narrow Q’s in
lateral leads (I, aVL, V5 and V6) - infarct Q’s are > 1 small square where as HOCM Q’s are less than 1 small square

Risk Scores
• Risk scores should be applied once other identifiable causes have been considered
• Do not replace clinical judgment and using your brain
• Risk scores may miss rare causes with most serious outcomes

San Francisco Syncope Rule
CHESS
Congestive Cardiac FailureHaematocrit <30%ECG abnormalShortness of breathSBP <90 at triage
Any one of these factors predicts high risk and therefore pt should be admitted and investigated further

SFSR
• Endpoint was ‘serious outcome’ or any condition causing return to the hospital and admission
• Sensitivity 96% and Specificity 56% for serious outcome at 7 days
• Revalidated by external study in Canadian ED finding sensitivity 90%, Specificity 33%
• Other studies found Sensitivity 52-77%• Blanket application to all syncopes and not just
those with no diagnosis after ED evaluation

ROSE Criteria
• Predictors of serious outcome at 30 days– Raised BNP– Positive stool haemoccult– Anaemia– Hypoxia– Prescence of Q waves on ECG
Sensitivity 87%. Negative predictive value 95.5%

ACEP RecommendationsLevel A Level B Level C
Hx and exam suggesting CCF consistent with high risk
Elderly, structural heart disease and coronary artery disease high risk
Perform ECG Echo, CT and other lab tests should not be routinely performed in absence of specific findings
Admit CCF and structural heart disease. Other high risk: ECG abnormalities, haematocrit <30


What the studies agree on
• Identified risk factors:– Age >65yrs– Hx of CCF– Abnormal ECG
Normal ECG may include sinus tachy, first degree HB, non-specific ST/T wave changes.

Syncope in the Elderly
Most common causes• Orthostatic hypotension
– 25% ‘Age related’– 75% Medication related
• Reflex– CCS cause in 20%
• Cardiac arrhythmias– Advanced age, underlying cardiac disease and
comorbidities

Prolonged QT syndrome

Brugada Syndrome

WPW syndrome

HOCM

ECG changes in HOCM
• Normal in up to 15%• Left axis deviation• LVH and strain• flipped T’s• big voltage R waves and deep, narrow Q’s in
lateral leads (I, aVL, V5 and V6) - infarct Q’s are > 1 small square where as HOCM Q’s are less than 1 small square

Epsilon waves in arrhythmogenic right ventricular cardiomyopathy

Bifascicular block

Trifascicular block

ECG
CHB

ECG
Tachy-bradycardia syndrome

ECG
Torsades des pointes

Disposition of patients
• Manage indentified cause as appropriate• Admit high risk for monitoring and investigation• Consider withdrawing medication likely to be
responsible• Advise pts on how to avoid further syncope:
– VVS – avoid stimulus– OH – medication change, good hydration, standing
slowly– CSS – avoidance of tight collars, pressure on CS

Future plans for Emergency Assessment – Recommendations from Europe
• Falls and syncope service– Run by geriatrics, cardiology, neurology
• Direct access to investigation and clinic– Tilt tables, Echo
• Syncope observation unit– As part of MAU– 6 hr telemetry, hourly orthostatic BPs– Echo

Assessing fitness to drive – National Transport Commission, Australia
• Unexplained syncope: Private drivers refrain from driving for 3 months. Commercial for 6 months.
• Recurrent syncope not responsive to treatment: criteria for conditional license not met
• Cause of syncope identified and assessed as temporary – NO effect on driving status
In the first 2 instances it is the responsibility of the patient to inform the RTA

Driving fitness - Research
• ESC: Data suggests that risk of a accident in pts with syncope is not different to those without
• Prospective study of 3877 pts with syncope. Recurrence whilst driving occurred only in 10 pts. Risk of syncope related driving accidents is 0.8% per year.

Summary
• A syndrome encompassing many physiological and pathological processes
• Our role is to identify those at risk of sudden cardiac death
• Benign syncope, while having minimal mortality, has associated morbidity
• Remember – Cardiac BAD, Non-cardiac Not so bad

Thank You





![Syncope AHD[1]](https://static.fdocuments.in/doc/165x107/577d36611a28ab3a6b92ec10/syncope-ahd1.jpg)