Dr. Adeyemi Adekunle Assistant Grant Support Officer Dr ...pdf.usaid.gov/pdf_docs/PNABM749.pdf ·...
Transcript of Dr. Adeyemi Adekunle Assistant Grant Support Officer Dr ...pdf.usaid.gov/pdf_docs/PNABM749.pdf ·...
POST-TRAINING EVALUATION OF PHYSICIANS AND NURSES PROVIDING FAMILY PLANNING SERVICES IN GHANA
January 5 - 26, 1991
Dr. Adeyemi Adekunle Consultant Department of Obstetrics and Gynecology University College Hospital Ibadan, Nigeria
Ms. Deborah Dean Assistant Grant Support Officer JHPIEGO Corporation Baltimore, Maryland
Dr. Lynne Gaffikin Associate Director Monitoring and Evaluation Office JHPIEGO Corporation Baltimore, Maryland
EXECUTIVE SUMMARY
INTRODUCTION:
Despite the fact that Ghana has had a population policy since1969, fertility levels continue to be high as a result of social tendencies toward large families. Given current socio-economic conditions in the country, the political climate is becomingincreasingly supportive of family planning as evidenced by theinitiation of family planning programs in all regions. This hasbeen accompanied by a (donor-supported) flow of contraceptivecommodities and equipment to health facilities (coordinated by theMinistry of Health) and a substantial increase in the number ofphysicians, nurses and midwives trained in reproductive health skills. In January 1991, an evaluation of the effect of trainingin reproductive health on family planning services provided byphysicians, nurses and midwives was conducted. The findings of this evaluation form the content of this report.
OBJECTIVE:
The objective of this evaluation was to assess the effect oftraining district medical officers and nurses in reproductivehealth on the FP services that they provide.
METHODS:
The data used for the evaluation were obtained from the following sources:
o On-site inspection of facilities, equipment and supplies(in terms of the capacity of the sites to provide familyplanning services).
o On-site observation and assessment of the competencylevel of nurses and physicians who received in-service training in reproductive health.
o On-site information obtained through interviews with physicians and/or nurses/midwives regarding their knowledge of, attitude about, and practice/skills in providing and managing family planning services.
o Review of a randomly selected sample of client records and clinic log books (where available).
i
FINDINGS:
Capacity of the Sites to Provide Family Planning Services
Despite a lack of space to provide family planning services,the basic FP supplies and equipment were adequate in most centers and in good condition. Educational materials for counseling were not readily available, however, and ineffective decontamination of used instruments was observed in some centers.
Assessment of Trainees' Knowledae of and Skills in Inserting and Managing IUDs
In general, providers seemed skilled at performing physicalexaminations on potential clients in inserting IUDs. Their knowledge about managing IUD side-effects and complications was also satisfactory. Most providers, however, were not able to recognize the immediate signs associated with a perforated uterus. It was also observed that most providers were deficient in the skills needed to collect specimens, to interpret diagnostic tests and to provide follow-up treatment in cases where sexuallytransmitted diseases (STDs) were suspected. Provider-client interaction appeared to be good with adequate pre-servicecounseling and post-service instructions being offered at most centers.
Attitudes among Nurses/Midwives about Selected Reproductive Health Issues
There was general agreement among the nurses interviewed that family planning is socially and culturally acceptable in Ghana. In general they approved of pregnancy termination, especially if the pregnancy threatens a woman's life or when the fetus is deformed. Most respondents, however, did not approve of abortions for unmarried women. Overall, the group felt that the ideal family size should be between two and four children (this contrasts to the results of the 1988 Demographic Health Survey for which the averageideal family size was 7.6).
RECOMMENDATIONS:
The findings of this evaluation suggest that the training of district medical officers and nurses in reproductive health has had a positive effect on family planning programs in Ghana. The recommendations of this evaluation team are as follows:
o The coordination of the National Family Planning Program by the MOH is satisfactory and should be encouraged to
ii
continue. There is a need for more efficient coordination of the services in the private sector, however, in terms of commodity distribution and health statistics reporting. Nurses/midwives in these clinics should become more actively involved in the family planning program as a number of them have been trained in FP and,therefore, are competent to provide counseling services.
o There is a need to designate appropriate areas for familyplanning services in most of the clinics. Whenever possible, these areas should be located near well-babyclinics, as conveniently located family planningclinics/areas could potentially increase client use of these services (i.e. people could take advantage ofservices offered by two clinics with just one visit to a health care facility).
o It is important to establish storage areas for contraceptive commodities within each region to render the commodity distribution system to the clinics more effective.
o More training is needed to increase the number of service providers who are competent to perform IUD insertion and removal procedures. In addition, as new FP techniques and methods become available, it will be necessary to planand conduct update training courses for the providers.Increased training efforts should be directed at nurses/midwives aa they routinely provide the FPservices, although physicians need to be trained in management skills (e.g. planning and supervision) for the program to operate effectively.
0 Educational materials are needed for counseling to ensure that there is informed choice. The paucity of these materials in most clinics probably reflects an inadequatedistribution system. This could be improved through the use of the MOH commodities and supplies distribution network. It is also suggested that materials appropriateto the cultural setting in each region be made available.
o The management of STDs should be integrated into the family planning curriculum of all nursing/midwiferyschools. Furthermore, the family planning clinics staffed with trained service providers should be equippedwith adequate supplies to permit immediate diagnosis and appropriate management of STDs.
0 A standardized infection prevention protocol needs to be developed and integrated into the family planning service delivery system throughout Ghana.
iii
0
O There is a need to integrate Voluntary SurgicalContraception (VSC) into the national family planning program, as most providers currently consider it to be separate. It is recommended that a knowledge and attitude survey among users/potential users be conducted to provide a basis for developing strategies to promoteVSC. In addition, considerably more training should be carried out to increase the number of service providers,especially counselors, competent in VSC.
o NorplantR subdermal implants may be a good alternative to sterilization in Ghana. Thus, thought should be given to expanding NorplantR services beyond just the teachinghospitals.
There is a need to develop strategies to increase male involvement in FP programs to improve the current contraceptive prevalence rates. This will require the support of public leaders at the national, regional and district levels.
iv
INTRODUCTION:
Ghana is a country with a population of about 14.5 million people, over two thirds of whom live in the rural areas. Although a population policy has been in place since 1969, the 1988 Ghana Demographic Health Survey (GDHS) results indicate that fertilitycontinues to be high and that large families are still favored. The current average fertility rate is 5.8, although this varies considerably by place of residence and education level. For example, the total fertility rate (TFR) of urban women is 1.5 which is much lower than that of rural women. Similarly, the TFR of women with secondary or higher education is about 40% (or about two children) lower than that of all other women. Major factors contributing to the high fertility rate are early and nearlyuniversal marriage and low levels of modern contraceptive use. While 75% of married women in Ghana know of one or more methods of contraception, only 37% have ever used a method and only about 13% are currently using a method (GDHS). Over two-thirds of all married women, however, expressed a desire to limit or space their births which indicates that there is a substantial unmet need for family planning in Ghana.
The policy climate in Ghana is becoming increasinglysupportive of family planning service programs, not only as a preventive health measure but also as a socio-economic necessity.Family planning programs have been initiated in all regions, and there has been a substantial flow of commodities and equipment from donor agencies to the health facilities (coordinated by the Ministry of Health, Accra). Many problems and gaps in the FP service delivery system, however, still exist. A Birth Control Survey conducted by the Population Crisis Committee revealed that there was poor accessibility to birth control in Ghana and the doctor-to-patient ratio was high at about 1 to 15,000. More importantly, many providers were not strategically placed or supported to meet the needs of the growing family planning program.Most medical practitioners are still concentrated in the urban areas, and very few offer services in the rural areas where most Ghanaians live and work.
The number of facilities offering FP in Ghana has increased inthe past few years because of the training efforts of several USAID-sponsored programs including the Johns Hopkins Program for International Education in Reproductive Health (JHPIEGO). Since 1987, JHPIEGO has assisted in providing specialized reproductivehealth training for physicians and nurses/midwives to facilitate FP service expansion and to strengthen pre-service FP training. To date, 418 nurses and 172 physicians have received either didactic and/or clinical training in reproductive health under the auspicesof the JHPIEGO Corporation. In January 1991, JHPIEGO conducted an evaluation of the effect of training district medical officers and nurses in reproductive health on the FP services that they provide.
1
A JHPIEGO consultant and a home office staff member visited twentyeight FP facilities throughout the country to conduct on-site assessments of selected providers. This report summarizes the findings of this exercise.
OBJECTIVE:
The objective of this evaluation was to assess the effect oftraining district medical officers and nurses in reproductivehealth on FP services provided at health care facilities.
MATERIALS AND METHODS:
The team visited twenty-eight health facilities in five of the ten regions in Ghana over a period of three weeks, i.e. Greater Accra, Central, Ashanti, Northern and Eastern Regions. The health facilities visited were selected based on input from USAID, theOffice of Population and Nutrition (Dr. Blumhagen), the Ministry ofHealth, MCH/FP Division (Ms. Assan, Public Health Nursing Officer)and the senior PH nursing officer in each region. The choice ofregions and facilities to visit was restricted at the time of theevaluation due to political unrest. Initially, it was intended thatthe facilities would be selected according to the following four categories:
a) Health units staffed only by physicians who had attended an in-service reproductive health course,
b) Health units staffed only by nurses who had received inservice training,
c) Health units staffed by both categories of health providers who had received in-service training, and
d) Health units where neither the nurses nor physicians had received in-service training in reproductive health.
It was difficult, however, to find FP health facilities wherethere was no nurse or physician who had received training in reproductive health. This finding, in itself, is evidence of thepositive effect of the MOH training program. In addition, USAIDrequested that the team visit both private and public health facilities to assess differences in the two sectors. The non-random selection of sites limits the degree to which the results can begeneralized, although the data do provide some indication of the effect of the program in the regions.
2
The data used in the evaluation were obtained from the following sources:
0 On-site inspection of facilities, equipment and supplies(in terms of the capacity of the sites to provide familyplanning services).
0 On-site observation and assessment of the competencylevel of nurses and physicians who received in-service training in reproductive health.
o On-site information obtained through interviews with physicians and/or nurses/midwives regarding their knowledge of, attitude about, and practice/skills in providing and managing family planning services.
o Review of a randomly selected sample of client records and clinic log books (where available).
RESULTS AND DISCUSSION
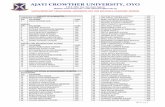
The team traveled to the health facilities over a period ofthree weeks. The distribution of sites by region and by type of facility is shown in Table 1. More health facilities were visited in the Ashanti region (28.6%) than any other region; the leastnumber were visited in the Northern Region (10.7%). Again, this reflects the feasibility of travel at the time of the evaluation and the site preferences of USAID and the MOH.
CAPACITY OF THE SITES TO PROVIDE FAMILY PLANNING SERVICES
In assessing the capacity of the sites to provide familyplanning services, it was observed that 25.0% of the sites had no areas designated specifically for family planning services,especially in the privately-owned health facilities (Table 2). Themajority of the other facilities had only one room (42.9%),although six centers (21.4%) designated more than two rooms for FP services. The use of only one room for all health services is not conducive to maintaining aseptic techniques which are needed duringthe provision of such FP methods as IUDs. Despite the lack of space, it was encouraging to note that a majority of the facilities were equipped with the basic amenities needed to provide FPservices (Table 3). This included: running water (82.1%), an examination taole (100.0%), a weighing scale (85.7%), a sphygmomanometer and stethoscope (92.9%) and toilet facilities(78.6%). As revealed by the table, many facilities were not equipped with a sterilization room/area, especially the publichealth facilities. Thermometers were not commonly available, and
3
virtually all the government-owned facilities were not equippedwith a recovery room/area. (In the private clinics, the recovery room for FP patients was the same as that used by other surgicalpatients). It is also important to note that all facilities except one (96.4%) had a clean examination room (Table 4), but only60.7% of the toilet facilities were in clean condition.
Privacy during counseling sessions was ensured in 82.1% of the facilities (Table 4), but counseling educational materials such as posters or hand-held uterine models were not generally available (Table 5). The Copper T-380A IUD was widely available for use during these sessions, and in 25.0% of the health facilities, the Lippes Loop was also available.
None of the private health facilities offering IUD insertion services had insertion or removal kits (Table 5). Instead, these providers used various instruments obtained from their general surgery set. It is important to note that two of these providers were trained during the JHPIEGO-supported private practitioners inservice training and they had not, at the time of the team's visit,received their IUD kits. Similarly, in two health facilities where nurse/midwife providers had also received in-service training, IUD insertion kits were not available. As a result, these facilities were unable to offer services to clients. About 50% of all facilities visited had two or more IUD kits available. Despite the shortage of sterile instruments, the team was informed that none of the facilities with a single IUD kit had denied clients services.
Table 6 is a breakdown of the type of clients being offered counseling services by the type of facility visited. Based on these data, it is apparent that there is a need for a stronger male initiative in family planning. Except in privately-owned health centers, there was an ample supply of modern contraceptive methods available to the facilities (Table 7). NorplantR subdermal implantservices were available in two teaching hospitals, but vasectomyservices were not available in any of the public or private health facilities.
Nurses and/or midwives were primarily responsible for providing family planning services in the health facilities visited except in privately-owned institutions where this responsibilitywas shared between the nurses and the physicians (Table 8). It was observed that the physicians in the district hospitals and polyclinics were not being used effectively in providing familyplanning services. Quite a number of them remarked that the heavyworkload in their facilities did not permit them to personallyprovide services to family planning clients. They were usuallyconsulted, however, whenever complications arose and physiciannurse interaction was observed to be very cordial in all sites. The nurses at most private health facilities were under-utilized in providing counseling services to family planning acceptors, even
4
though quite a number of them had received training in familyplanning (Table 9). The distribution of physicians observed duringthe evaluation by type of training received in IUD insertion andbilateral tubal ligation is shown in Table 10. As revealed by thedata, 86.6% of all physicians observed had received some sort ofIUD training; and almost 75% of those who had any IUD training hadreceived their training as part of an in-service training program.This suggests that the MOH MCH/FP training program has had asubstantial positive effect on the availability of IUD FP services in Ghana.
Data on the type of training received by nurses/midwives byfacility visited provided Table Allis in 11. of thenurses/midwives in the teaching hospitals had received their training as part of the in-service program. Again, this illustrates the positive effect of this program on the availabilityof FP services in the regions. Most of the nurses/midwives in the other government facilities that were visited also had received their training as part of the in-service program. A small number of the public sector nurses/midwives observed had not had any FPtraining (15.8%) which is expected given that the program has not yet reached its goal of training two providers per level B facility.
Infection prevention practices were also observed as part ofthis evaluation. In most facilities, plastic sheets were used asdrapes for the lower end of the examination table, and these wereroutinely cleaned between clients. The cloth drape underneath theplastic sheet, however, was changed only at the end of the day.The team observed that all providers washed their hands between clients.
Effective decontamination of used instruments appeared to beadequate in only six (21.4%) of the facilities visited (Table 12).In most facilities "Detol" was the disinfectant of choice but nostandardized dilution factor was used. Answers from providersregarding the dilution factor used varied from "i in 2" to "I in400"; and some providers claimed to have simply added "drops of Detol" at their discretion. In some facilities, the disinfectant was given to the providers in diluted form from hospital dispensarystaff, and, therefore, the providers did not know the solution strength.
Adequate sterilization of instruments occurred at allfacilities except two, although only a few facilities (17.9%) were equipped with autoclaves (Table 12). It appeared that most facilities, including some privately-owned clinics, are dependenton the central sterilizing department (CSD) of the teaching and central/regional hospitals, therefore,and, drums ofinstruments/gauze/gloves for autoclaving are forwarded to the CSD once or twice a week. Adequate storage of sterilized equipment,however, was available in 82.1% of the facilities visited.
5
ASSESSMENT OF TRAINEES KNOWLEDGE AND SKILLS AT INSERTION AND MANAGEMENT OF IUDs:
Despite an average of two visits per clinic, the performanceof only ten trainees could be assessed and only two removalprocedures were observed as the client-load in most facilities during the evaluation period was low. In general, the trainees' ability to perform physical examinations on potential clients wasgood (Table 13). This included general examinations (89.0%) and identification of normal and abnormal findings (100.0%). It isencouraging to note that most providers did not only perform breast examination satisfactorily but also taught the client selfexamination. Nurses at the family planning clinics that werevisited generally did not take specimens in cases when an STD was suspected, as these clients are routinely referred to the laboratory for this procedure.
The clinical skills of most providers who were observed inserting an IUD were satisfactory, especially in terms ofmaintaining aseptic techniques (80.0%), placement of the tenaculum on the cervix (80.0%), sounding the uterus (80.0%) and appropriateinsertion procedures (i.e. withdrawal technique) (90.0%) (Table14). Only 40.0% of the providers actually loaded the IUD in the package, however, as some were not trained in this procedure.
The providers' ability to manage the side-effects andcomplications of IUD use was also assessed in the areas of: breakthrough bleeding (90.0%), lost IUD string (80.0%), suspected pelvicinfection (80.0%) and pregnancy with IUD in place (90.0%) (Table15). Most providers were not knowledgeable about the immediate signs associated with perforation of the uterus during the passageof the uterine sound, as evidenced by the fact that only 40.0% provided satisfactory answers to this question during the evaluation.
The ability of the providers to manage STDs was not judged tobe satisfactory in some areas (Table 16). For example, most providers were deficient in the skills needed to collect specimens,interpret diagnostic tests and provide follow-up treatment. On theother hand, 90.0% of the providers could obtain a relevant historyon patients with suspected STDs. Similarly, all providers could perform appropriate physical examinations to screen for these diseases. In most cases, STD services were offered by the hospitallaboratory, not the FP clinics. This did not effect, however, the quality of patient care given at the clinics.
It is significant to note that all providers were able to interact effectively and efficiently with their clients. That is,all available methods of contraception and their use were clearlyexplained; clients were aided in selecting the method of their choice, and adequate instructions for follow-up care were provided
6
in all cases. Similarly, all providers were deemed able to determine the appropriateness of the IUD as the method of choice, to identify contra-indications to the method, to make referrals when appropriate, and to determine when it would be an appropriatetime to insert the device (Table 17).
SURVEY OF NURSES/MIDWIVES ON SELECTED REPRODUCTIVE HEALTH ISSUES:
A survey of attitudes among nurses and midwives towards abortion was also conducted (Table 18). Nine out of ten nurses/midwives interviewed were of the opinion that a pregnancythat threatens a woman's life should be terminated. 81.4% of the respondents also approved of pregnancy termination when it was believed that the fetus was deformed. Less than half (46.5%) of the respondents, however, approved of pregnancy termination when a woman had been raped. Seven out of ten nurses interviewed disapproved of pregnancy termination when a woman was unmarried and half of the respondents also disapproved of pregnancy termination in cases where couples could not afford to have more children. The relatively open stance towards abortion by respondents is not surprising as Ghana currently has a relatively liberal abortion law.
Nine out of ten nurses/midwives interviewed were of the opinion that the ideal family size should be between two to four children, although a majority (60.5%) felt that four children perfamily was ideal (Table 19). This is in sharp contrast to the results of the 1988 GDHS in which is was indicated that the ideal family size was 7.6. All respondents were of the opinion that family planning improves family health, and eight out of ten respondents believed that voluntary sterilization is a useful method.
Opinions among nurses/midwives regarding other selected familyplanning issues were also solicited (Table 20). About 80.0% of the respondents disagreed that family planning is foreign to Ghana's culture. While 79.1% of the respondents disagreed that familyplanning programs encourage promiscuity, about nine out of ten were of the opinion that modern contraceptive methods have too manyundesirable side effects. More than seven out of ten respondentsconsidered family planning programs rather expensive. A similar proportion of the respondents felt that Ghana should have a national population policy and that family planning should be used to control population growth in the country. All in all, the opinions expressed suggest that nurses/midwives are supportive of FP programs in Ghana.
CONCLUSIONS AND RECOMMENDATIONS:
It is apparent from the results of this evaluation that Ghana has begun to establish an effective family planning program in the regions. Clinic-based services are provided by well-trained staff
7
in both the public and private sectors. Almost all facilities visited had hormonal and barrier contraceptive methods available and wherever adequately trained personnel and equipment wereavailable, IUDs were offered. This contrasts considerably with the results of a facility survey that was conducted by the MOH in 1987 in which it was noted that fpcilities in only three of the ten regions were offering IUD sexvices. Voluntary sterilization and NorplantR subdermal implants were available only in some selected institutions, which is not surprising given that training in these two methods has been less extensive. A system exists for distributing commodities to the government clinics, and there are established procedures fcr reporting and analyzing client and commodity utilization data. The situation is different, however,in the private sector. Although the providers have been supportedthrough training and a supply of equipment, their potential for involvement has not yet been fully realized.
In general, the ability of the trainees to provide familyplanning services and to manage problems was found to be satisfactory. Those observed interacted effectively and efficiently with the clients. The findings of this evaluation suggest that the training of district health officers and nurses in reproductive health has had a positive effect on family planning programs in Ghana. The recommendations of this assessment team are:
o The coordination of the National Family Planning Programby the MOH is satisfactory and should be encouraged to continue. There is a need for more efficient coordination of the services in the private sector, however, in terms of commodity distribution and health statistics reporting. Nurses/midwives in these clinics should become more actively involved in the family planning program as a number of them have been trained in FP and,therefore, are competent to provide counseling services.
0 There is a need to designate appropriate areas for familyplanning services in most of the clinics. Whenever possible, these areas should be located near well-babyclinics, as conveniently located family planningclinics/areas could potentially increase client use of these services (i.e. people could take advantage of services offered by two clinics with just one visit to a health care facility).
0 It is important to establish storage areas for contraceptive commodities within each region to render the commodity distribution system to the clinics more effective.
o More training is needed to increase the number of service
8
providers who are competent to perform IUD insertion and removal procedures. In addition, as new FP techniques and methods become available, it will be necessary to planand conduct update training courses for the providers.Increased training efforts should be directed at nurses/midwives as they routinely provide the FP services, although physicians need to be trained in management skills (e.g. planning and supervision) for the program to operate effectively.
o Educational materials are needed for counseling to ensure that there is informed choice. The paucity of these materials in most clinics probably reflects an inadequatedistribution system. This could be improved through the use of the MOH commodities and supplies distribution network. It is also suggested that materials appropriateto the cultural setting in each region be made available.
o The management of STDs should be integrated into the family planning curriculum of all nursing/midwiferyschools. Furthermore, the family planning clinics staffed with trained service providers should be equippedwith adequate supplies to permit immediate diagnosis and appropriate management of STDs.
o A standardized infection prevention protocol needs to be developed and integrated into the family planning service delivery system throughout Ghana.
o There is a need to integrate Voluntary SurgicalContraception (VSC) into the national family planning program, as most providers currently consider it to be separate. It is recommended that a knowledge and attitude survey among users/potential users be conducted to provide a basis for developing strategies to promoteVSC. In addition, considerably more training should be carried out to increase the number of service providers,especially counselors, competent in VSC.
o NorplantR subdermal implants may be a good alternative to sterilization in Ghana. Thus, thought should be given to expanding NorplantR services beyond just the teachinghospitals.
o There is a need to develop strategies to increase male involvement in FP programs to improve the current contraceptive prevalence rates. This will require the support of public leaders at the national, regional and listrict levels.
9
Appendix I
HEALTH CARE FACILITIES VISITED BY ASSESSMENT TEAM
GREATER ACCRA
Accra
Kaneshie Polyclinic Korle-Bu Teaching Hospital Adabraka Polyclinic North Ridge Clinic Legon Hospital Planned Parenthood Association of Ghana
CENTRAL REGION
Cape Coast
University (Cape Coast) Hospital Central Hospital Adisadel Health Center London Clinic Farib Clinic Planned Parenthood Association of Ghana
ASHANTI REGION
Kumasi
Komfo-Anokye Teaching Hospital MCH/FP Center West-End Clinic Bantama Clinic Planned Parenthood Association of Ghana
Abuakwa via Kumasi
MCH/FP Health Post
Nkawie via Kumasi
MCH/FP Center
Suntreso via Kumasi
Suntreso Urban Health Center
10
NORTHERN REGION
Tamale
Tamale Regional Hospital MCH/FP Center Planned Parenthood Association of Ghana
EASTERN REGION
Koforidua
Central Hospital MCH/FP Center Planned Parenthood Association of Ghana
Nsawam
Government Hospital
Suhum
MCH/FP Center
11
TABLE 1: DISTRIBUTION OF SITES BY FACILITY TYPE AND REGION
T:ype of Facility...........
RegionDistrict
Regi.nal. Teaching Hospitals
5
Greater 1/6 (16.7) :"1:"ra ".6/28
n = 6 1/5 (20.0)
Central 1/6 (16.7) Region n = 6 1/5 (20.0)
Ashanti 1/8 (12.5) Region n = 8 1/5 (20.0)
Northern 1/3 (33.3) Region n = 3 1/5 (20.0)
Eastern 1/5 (20.0) Region n = 5 1/5 (20.0)
TOTAL N =28 5/28(17.9)
Hospitals/ Health Care
Center's
n.13
3/6 (50.0)
3/13 (23.1)
2/6 (33.3)
2/13 (15.4)
4/8 (50.0)
4/13 (30.8)
1/3 (33.3)
1/13 ( 7.7)
3/5 (60.0)
3/13 (23.1)
13/28 (46.4)
others .. Private/.
PPIAG) TOTAL
0 .28
2/6 (33.3) ( 21.4)
2/10 (20.0)
3/6 (50.0) 6/28 ( 21.4)
3/10 (30.0)
3/8 (37.5) 8/28 ( 28.6)
3/10 (30.0)
1/3 (33.3) 3/28 ( 10.7)
1/10 (10.0)
1/5 (20.0) 5/28 ( 17.9)
1/10 (10.0)
10/28 (35.7) 28/28 (100.0)
TABLE 2: DISTRIBUTION OF BITES BY FACILITY TYPE AND SPACE FOR FAMILY PLANNING SERVICES
.........................Type of FacilityNumberlof room.
designated for Family PlanningService.assrc
Regional/.Hospitals/j Teaching Health Care Hospitals Centers
Other. (Private/
PA)TOTAL
n=Sn 13 n.n10 N 28
No special room 0/7 (0.0) 1/7 (14.3) 6/7 (85.7) desi.gnated for Family 7/28 (25.0) Planning Services n=7 0/5 (0.0) 1/13 (7.7) 6/10 (60.0)
I room designated for 3/12(25.0) 9/12 (75.2) 0/12 ( 0.0) FaiyPlanning 12/28(42.9)
Services, n =12 3/5 (60.0) 9/13 (69.2) 0/10 ( 0.0)
2 rooms designated for 2/3 (66.7) 1/3 (33.3) 0/3 ( 0.0) Family Planning., 3/28 (10.7)Services =1. 2/5 (40.0) 1/13 (7.7) 0/10 ( 0.0).n
i'ii!iiii~ii !ni !sr iii i~ii!:':i Viiiilllii iiiiiiiiii!iiiiii~iiii ii'iiiil~ii!iil : ii iiiiiiiii l~iiiiiiiiii !i:il iiiii ii~ii~iiiiiiiiiiiii!i
More than 2 rooms 0/6 ( 0.0) 2/6 (33.3) 4/6 (66.7)''desi~gnated for Family 6/28 (21.4)-Planning Services n=6 0/5 ( 0.0) 2/13 (15.4) 4/10 (40.0)
TOTAL N =28 5/28( 7.9) 13/28 (46.4) 10/28 (35.7) 28 (100.0)
TABLE 3: DISTRIBUTION OF SITES BY FACILITY TYPE AND AMENITIES AVAILABLE
.Type of Facility
Amenities District
Regional/ Hospitals/ T~eaching Health Care Others... 'Hospitals Centers (PriVate/PPAG) Total
n5n 3 10 N 28
Running water 4/5 (80.0) 10/13( 76.9) 9/10 (90.0) 23/28( 82.1) n = 23____ __
Examination Table 5/5 (100.0) 13/13(100.0) 10/10 (100.0) 28/28(100.0) n =28______ __ _
Scale 4/5 (80.0) 11/13( 84.6) 9/10 (90.0) 24/28( 85.7) n =24
Sphygmomanometer/ Stethoscope 5/5 (100.0) 11/13( 84.6) 10/10 (100.0) 26/28( 92.9)
n=26____ !!i !!iil~iiiliiii~iii! i
__
i~i! : ~ t :!! !:!!::i!::ii:!:::i:i :: 2':i ~iiii~ii~ii~ii! . !: : ::S:\ Light Source 3/5 ( 60.0) 10/i3( 76.9) 8/10 ( 80.0) 21/28( 75.0) nf=21 ____
Covered Storage 5/5 (100.0) 11/13( 84.6) 8/10 ( 80.0) 24/28( 80.7) n =24 ____
sterilization 2/5 (40.0) 4/13 (30.8) 10/10 (100.0) 16/28( 57.1) Area n =16________ ___
Thermometer 2/5 (40.0) 4/13 (30.8) 6/10 ( 60.0) 12/28( 42.9)b 12
Recovery Room 0/5 (0.0) 0/13 (0.0) 5/10 ( 50.0) 5/28 ( 17.9)
Toilet Facilities 4/5 (20.0) 8/13 (61.6) 1010 (10 0.0) 22/28( 78.6) n =22
TABLE 4: DISTRIBUTION OF SITES BY FACILITY TYPE AND ADEQUACY OF SERVICE AREAS
Type of Facility]
Condition District Regional/ Hospitals/ Others Teaching ealth Care (Private/ TOTAL Hospitalsu Centers PPAG)
___ ___ __ f5 13 . 10 N 28
lean Examination Rooms n = 27 5/5 (100.0) 12/13 (92.2) 10/10 (100.0) 27/28 (96.4)
Clean counseling Areas/Rooms.n = 26 i : .. ~ 5/5 11o0.o) 11/13 (84.6) 10/10 (100.0) 26/28 (96.9)
Clean Toilet Facilities n =17 4/5 (80.0) 5/13 (38.5) 8/10 (80.0) 17/28 (60.7)
dequate Client Privacy during
:;Counseling 5/5 (100.0) 12/13 (92.3) 9/10 (90.0) 23/28 (82.1) .n,..23._____
TABLE 5: DISTRIBUTION OF SITES BY FACILITY TYPE AND AVAILABILITY OF MATERIALS/EQUIPMENT
''Materials and Equipment
________z
Adequate Educational Materials n = 7
copper T-380 Sn. 28
Lippes Loop (IUD) n= 7
Insertion/Removal Kits
None available n=5 " "_____
Kit available :n:= lO ' ••,
2 Kits available n= 4
14ore than 2 kits ,available n 10
Regional/ Teaching Hospitals
n5.13
2/5 ( 40.0)
5/5 (100.0)
1/5 (20.0)
0/5 ( 0.0)
3/5 (60.0)
0/5 ( 0.0)
2/5 (40.0)
Type of Facility
District Hospitals/ Others Health Care (Private/ TOTAL Centers PPAG)
10l N. 28
2/13 ( 15.4) 3/10 ( 30.0) 7/28 ( 25.0)
11/13( 84.6) 7/10 ( 70.0) 23/28 (82.1)
1/13 ( 7.7) 5/10 (50.0) 7/28 (25.0)
2/13 (15.4) 3/10 (30.0) 5/28 (17.9)
7/13 (30.0) 0/10 (0.0) 10/28 (35.7)
2/13 (15.4) 2/10 (20.0) 4/28 (14.3)
2/13 (15.4) 4/10 (40.0) 10/28 (35.7)
TABLE 6: DISTRIBUTION OF SITES BY FACILITY TYPE AND TYPE OF CLIENTS COUNSELED
iiiii:!~POStNal. i~Cl[itii:
Anti~!;iii!e-Naa l. C;l:in~ii;iiiii
5/5
5/5
(100.0O)
(100.0O)
13/13 (100.0O)
13/13 (100.0O)
tten...ing.
10/10
10/10
(100.0O)
(100.0O)
.let..
28/28
28/28
(100.0O)
(100.0O) ..... ..
Atte+i++++++++nng Fam:+In:++iy..+.+++ 5/5 (100.0) 13/13 (100.0) 5/10 (50.0) 23/28 ( 82.1)
S++++:++++:Planning ++.Clitn:++++ic ++++:++ 4/5 ( 80.0O) 5/13 ( 38.5) 0/10 (0.0O) 9/28 ( 32.1)
:+i+++:++i::Well.::+Baby :Clin:: ::+ii:+!+i5/5
Adolescents iii~ii~ii~!i~i! ii~~ii!!!iiiii~iii4/5
( 100.0O)
( 80.0)
9/13
13/13
( 69.2 )
(100.0)
5/10
2/10
(50.0O)
(20.0)
19/28
19/28
( 67.8)
( 67.8)
TABLE 7: DISTRIBUTION OF BITES BY FACILITY TYPE AND AVAILABILITY OF CONTRACEPTIVE METHODS
of.... .yp Kacili
Teachig......Roupt.............ca
i~~~i~[:::Iiiiiii;i~!i !~iiiii:iiiiiii!i~~ii!ii~iii!:5/5(100.0) 13/13 (100.0) 7/10 ( 70.0)
ii::i:::: : %:...........i: :i : ::i~i~i:: ::::::::::::::::.........................:i:::i::
25/28 (9.3)
.....
Tiii:i~:,ablets~ii:::::: ~i:!:: ]: !~!i]iii5 /5 (100.0o)
Injectables 5i!ii~i~iiiiiiiiiiiiiiiii/5 (100.0)
IDp 5/5 (100.0)
13/13 (100.0o)
13/13 (100.0)
13/13 (100.0)
5/10 ( 50.0o)
5/10 ( 50.0) 8/10 (.80.0)
23/28 (82.1)
23/28 (82.1)
26/28 (92.9)
Vasec tomy 0!ii!i~i~iiiiii!i~!i/5( 0.0) 0/13
klorlant b de...... ]]!ii~Im]plants :::ii!/]:!]:i~ii]i~: 2/5 ( 40.0O) 0/13
(
(
0.0)
0.0O)
0/10 (
0/10 (
0.0)
0.0O)
0/28
2/28
( 0.0)
( 7.1)
TABLE 8: DISTRIBUTION OF SITES BY FACILITY TYPE AND CATEGORY OF PERSONNEL PROVIDING FP CLINICAL SERVICES
TYPO of: FaCili .... ....
Region&I Hospitals/. Privt
Specialiste
Ouresidwive
4/5 (a80.0) 2/3.5.)n0.)
Gene.a. ..... a.
5/5 (100.0) 63/13 (138.5)
5/0
5/10 (50.0)
1128(393
..
26/28 825.1)
Others 0/5 (0.0) 2/13 (15.4) 3/10 (30.0) 5/28 (17.9)
TABLE 9: DISTRIBUTION OF SITES BY FACILITY TYPE AND PERSONNEL ASSISTING FP CLIENTS
Type of Facility ............
Pesne ~ irajDistrict: Privatei ~ .. :.:.:... .:.:~~~.*%....::. fospitals .:..........===========Teaching: :....:..+ ...... > . Mfedical'...... .. ...
Hospitals n~ra..........
iiiiiiOff:::icruRmuiutis; 5/5 (100.0O) 9/13 ( 69.2) 5/10 ( 50.0O) 19/28 ( 67.8) Otltherrsnei:.......
Spiists i !ii~i~i~ii!~i!i ii~iii~!5/5 (100.0) 2/13 ( 15.4) 8/10 ( 80.0) 15/28 ( 53.6)
Vurses! idviiliiiiii~a ii;ii~i5/5 (100.0) 13/13 (100.0) 3/10 ( 30.0) 21/28 ( 75.0)
sistants) 1/5 (20.0) 4/13:Ce(Nus(30.8) 3/10 (30.0) 8/28 (28.6)
TABLE 10: DISTRIBUTION OF PHYSICIANS BY FACILITY TYPE AND TRAINING OF PHYSICIANS
Type of Training.
Regional/ Teaching Hospitals
Type of Facility
District Hosp ita1sf Health Care. rvto/
cent.ersA TOTAL....
n9 .. n14 rn7 R3
In-4ervic. Training in:, ,IUD n =:19
Formal Trainingin IUD a 7
5/19
5/9
4/7
4/9
(26.3)
(55.5)
(57.1)
(44.4)
8/19
8/14
2/7
2/14
(42.1)
(57.1)
(28.6)
(14.3)
6/19
6/7
1/7
(31.6)
(85.7)
(14.3)
19/30
7/30
(63.3)
(23.3)
oTraining i iL n=74
TOTAL N 30 0nsrc/17
0/9
9/30 (35.3)
(0.0)
(30.0) 7/17 (1.2)
4/14 (28.6)
14/30 (46.7) 041
0/0
7/30 (23.5)
(0.0)
(23.3)
4/30 (13.3)
30/30 (100.0)
inilapromylov-raiiiiiining in:::iii: ii:i:iii aae6/17 (35.3) a 7/17 (41.2) 4/17 (23.5) 17/ 30 (56.7)
e BTLskills"reeUoteaiiyt
Formal. .. !i!i:i~i iiii:::i~ii:: 3 /7 ( 42.8 ) ::!!ii-ii:iTra in:ing in ii~iii: BTL:::::::::::i:.i:n..: i;:7:i:!iiiii:iiiiil 3 /9 (33 .3 )
!ii :ii:i:BT:Ln.:=:: 6i:::~ !:: i ::i: 0/9 (0.0)
TOTAL::::::::::::::::::N::::::=:::::::30::::: 9/30 (30.0)
efrb-aea
1 /7 ( 14.3 )
1/14 ( 7 .1 )
6/6 (100.0)
14/30 (46.7)
ua
3/'7
0/7
7/30
iain
(42.9)
(0.0)
(23.3)
sn
7/30
6/30
30/30
(23.3)
(20.0)
(100.0)
'IUD skills refer to the ability to insert and/or remove intrauterine devices.2BTL skills refer to the ability to perform bi-lateral tubal ligations using minilaparotomy/iocal anesthesia and/or laparoscopy.
TABLE 11: DISTRIBUTION OF NURSES/MIDWIVES BY FACILITY TYPE AND TYPE OF TRAINING
Typ. of In-service Formal
Type of Training::
Training No Training.TTA
,..Regional/. Teaching:
.,Hospitals
9/9
9/34
(100.0)
( 26.5)
0/19
0/4
(0.0)
( 0.0)
0/19
0/5
(0.0)
( 0.0) 9/43 (20.0)
''District Hospitals/.-Health Care Centers
15/19
15/34 _ _ _
( 78.9)
( 44.1) _ _ _ _ _ _
1/19
1/4
(
(
5.3)
25.0)
3/19
3/5 _ _ _
( 15.8)
( 60.0) _ _ _ _ _ _
19/43 ( 44.2)
_ _ _ _ _ _ _ _ _
.Private/PPAO Health :Centers
10/15 ( 66.7)
10/34 ( 29.4)
3/15
3/4
( 20.0)
( 75.0)
2/15
2/5
( 13.3)
( 40.0) 15/43 ( 34.9)
.TOTAL 34/43 (79.1) 4/43 ( 9.3) 5/43 (11.6) 43/43 (100.0)
______________ ______
TABLE 12: DISTRIBUTION OF SITES BY FACILITY TYPE AND INFECTION PREVENTION PROCEDURES
Type Of.-Facility,
Prcedures _:District
Regonal/ :,:Hspitals/ Others'...... .Teaobing. aelh (Private/.....,re ospitals, Centersa PPAG)....TTL
xxaininatiorl table cleaned, 5/5(100.0) 13/13(100.0) 10/10(100.0) 28/28(100.0) between clients..______
Providers clean hands between 5/5(100.0) 13/13(100.0) 10/10(100.0) 28/28(100.0) clients
Adequate .
decontamination of used 2/5( 40.0) 3/13 (23.1) 1/10 (10.0) 6/28 (21.4) instruments'
Adequate,sterilization
.5/5(100.0)of instruments 11/13( 84.6) 10/10(100.0) 26/28( 92.9) availableZ _ _ _ _ _ __ _ _ _ _ _ _ _ _ _ _ _
•U _ _
'Autoclave -available 1/5( 20.0) 2/13 (15.4) 2/10 ( 20.0) 5/28 (17.9) Adequate storage of sterilized. 5/5(100.0) 10/13( 76.9) 8/10 ( 80.0) 23/28( 82.1) e0quipment 3
'Adequate disinfectant solution used before washing instruments indicates treatment with bleach solution, detol or savion.
2Adequate sterilization means instruments are sterilized via steam-autoclave or dry heat in the facility or at the near by hospital.
3Adequate storage indicates stored in sterilized drums or on trolley covered with towel overnight.
TABLE 13: PERFORMANCE RATING OF PROVIDERS FOR VARIOUS PHYSICAL EXAMINATIONS
Rting
. ... 1 0..
Tyeof Exai,ait
Idnifica.ti..........minaton.o.....rmal... ......io8 ... .....aigs... 80.0) ...........bora'In!i gn, n 10e speime f STis are suspected.(100.0)....Clientsardo nt t .i
Breas Examiii+on.i~ 10+++++++i nti i++i + (100.0)i~i++ Va........a....p.....xa ina io s 80.0)% 8 ac
.... inAb o l xa...m.. i...n in . .. 9 ( 90 .0)
usu1al sen to th9abrtoyfr.hs0rceue
'In general, nurses do not take specimens if STDs are suspected. Clients are usually sent to the laboratory for this procedure.
TABLE 14: PERFORMANCE RATING OF PROVIDERS FOR VARIOUS CLINICAL SKILLS
Rating
Type of Skil
Satisfactory Unsatisfactory Performed
Use of aseptic technique 8 ( 80.0) 2 ( 20.0) 0 ( 0.0)
Placement of tenaculium on cervix 8 ( 80.0) 1 ( 10.0) 1 ( 10.0)
Sounding the uterus 8 ( 80.0) 2 ( 20.0) 0 ( 0.0)
Using appropriate insertion procedures(withdrawal technique) 9 ( 90.0) 1 ( 10.0)ii ii~i: iii i .:: i~iiii~ i~~i~ii ! !i~ i :i~ii~ii~i~~i~ !I 0 ( 0.0)
Loading ID in the *package
4 ( 40.0) _ _
1 _
( 10.0) _ _ _ _ _ _
5 _
( 50.0) _ _ _ _ _
TABLE 15: PERFORMANCE RATING OF PROVIDERS IN MANAGING THE SIDE EFFECTS AND COMPLICATIONS OF ZUD USE
Rating N 10
Type of Side Effecot_____________________
and/or complication
Satisfactory
.rakthrough Bleedin 9 (90.0)
Lost IUD string 8 (80.0)
Suspected perforation of the ..
uterus 4 ( 40.0)
Suspected pelvic infection 8 ( 80.0)
Pregnancy with IUD in place 9 ( 90.0)-
TABLE 16: PERFORMANCE RATING OF THE PROVIDERS IN MANAGING STDu
Rating
S10
Mnagement
Satisfactory Unsatisfactory Not Performed
n(%)n( n(96)
Obtain relevant history 9 (90.0) 1 ( 10.0) 0 ( 0.0)
Perform appropriate examination to screen for ,TD 10 (100.0) 0 ( 0.0) 0 ( 0.0)
Collect appropriate specimen 3 ( 30.0) 0 ( 0.0) 7 ( 70.0)
Interpret diagnostic test 4 ( 40.0) 0 ( 0.0) 6 ( 60.0)
Provide proper followup 4 ( 40.0) 0 ( 0.0) 5 ( 50.0)
TABLE 17: PERFORMANCE RATING OF THE PROVIDERS IN INTERACTING WITH CLIENTS
Rating
!ype of interaction
Satisfactory.
o (o)
.Explain*LU methods 10 (100.0)
Assist client tolohoose a, method 10 (100.0)
Explain use of the method 1.0 (100.0)
Determine the appropriateness of IUD as a method 10 (100.0)
Identify oontra-indications 10 (100.0)
Determine the appropriate time for insertion io (100.0)
Provide instruction for .follow-up 10 (100.0)
Make necessary referral io (100.0)
TABLE I6: DISTRIBUTION OF ATTITUDES AMONG NURSES/MIDWIVES TOWARDS ABORTION BY SELECTED CIRCUMSTANCES
...... ................. . ......... .................. nifet
p....a.......When ......... .....thn e... X..........life39 .0)1 (2.3.907)..(
h......n.. .h.... fetusbel..e.ed.to.b.
... 46.5)..17been raped 20 ''39.5) 6f(O14.0)
.......th X, ie ......an
...a..e.....11.).31..72.).7..16.3
.: ...................e the a. or to...h...e....... ........ 16..37.).22..51.).5..11.6
TABLE 19: DISTRIBUTION OF OPINIONS AMONG NURSES/MIDWIVES ABOUT IDEAL FAMILY SIZE
Preferred Number of, Number and :Percentage of Respon~denrts . idr.n per Family...........
1- 2.3
__ _ _ __ _ _ __ __3_ _ _ _ 14 32.*6
4 26 60.5
5 1 2.3
NO res~oflse 2.3
T:ts: 43 100.0
too:
All respondents are of the opinion that family planning would improve family health.
79.1% of respondents believe that voluntary sterilization is a useful method.
However, only 16.3% would choose vasectomy while 69.8% prefer bilateral tubal ligation. 13.9% of the respondents have no preference.
TABLE 20: DISTRIBUTION OF ATTITUDES AMONG NURSES/MIDWIVUS TOWARDS SELECTED FAMILY PLANNING ISSUES
T........i... -XN4f
ec e .ail.Pa1n . ......... ro.gly
we .......
.g .g .ne ...... e .. ..... i f r n re. D...a..e.. n (% ii%) a(~) (x
.........~~~?he~~~~ide.off..l....nin. iforeign~.t. ......ut. 3. 7.0 5 (. 16..( 23 3 35 1 56 ' r a..a... t....poxato r t .n..oshoud nxitynt cuse ( 70) ( .0) 0 ( .0) 24 55.) 1 C 0.2
lazily~~~~~~ plXigpormnorg
.etdFamily lanning 1amtooare
Ghanaavehoulda ationa population~~~~~~~ polic..31.7.) 11.2.) 1...) 0C0.)0C00
Family,: sful beset planninpoplaiocontrol- gr.hi.Ga.3. 7.) 8( 86 23 . 0...0.0