Dofetilide for Atrial Arrhythmias in Congenital Heart Disease: A Multicenter Study
-
Upload
ronald-wells -
Category
Documents
-
view
215 -
download
1
Transcript of Dofetilide for Atrial Arrhythmias in Congenital Heart Disease: A Multicenter Study

Dofetilide for Atrial Arrhythmias in Congenital HeartDisease: A Multicenter StudyRONALD WELLS, M.D.,* PAUL KHAIRY, M.D., PH.D.,† LOUISE HARRIS, M.D.,‡C. CHRISTIAN ANDERSON, M.D.,§ and SESHADRI BALAJI, M.B.B.S., M.R.C.P. (U.K.), PH.D.*From the *Division of Pediatric Cardiology, Department of Pediatrics, Oregon Health & Science University, Portland,Oregon; †Adult Congenital Heart Center, Montreal Heart Institute, Montreal, PQ, Canada; ‡Toronto GeneralHospital, Toronto, Ontario, Canada; and §Northwest Center for Congenital Heart Disease, Spokane, Washington
Background: Very little is known about use of the class III antiarrhythmic dofetilide in patients withcongenital heart disease (CHD).
Methods: A multicenter retrospective review of experience with dofetilide in CHD patients wasundertaken.
Results: Twenty adults with CHD and refractory atrial arrhythmias were treated with dofetilide at fourinstitutions over a 7-year period. Three (15%) experienced adverse effects during in-hospital initiationof dofetilide (two with torsade de pointes, one with excessive QTc prolongation) and were not continuedon this therapy. The remaining 17 were discharged taking dofetilide, with either resolved or improvedarrhythmia. One was lost to follow-up. Five subsequently discontinued dofetilide due to waning effective-ness, manifest by recurrence of their arrhythmias. Eleven (55%) remained on dofetilide at most recentvisit, with a median follow-up of nearly 1 year. Seven of these 11, or 35% of the CHD patients originallystarted on dofetilide, experienced a complete resolution of their arrhythmia. The remaining four hadbreakthrough episodes of atrial arrhythmia, but remained on dofetilide. No patient experienced torsadede pointes after the in-hospital initiation period.
Conclusions: Used appropriately, dofetilide appears to be a viable adjunct to catheter-based ablationand alternative pharmacological approaches for the treatment of atrial arrhythmias in adult patients withcongenital heart disease. (PACE 2009; 32:1313–1318)
pediatrics, pharmacology
IntroductionAs modern medical and surgical management
of structural congenital heart disease (CHD) allowsmore patients to survive, long-term complications,including arrhythmias, become the major chal-lenge in their management.1 Atrial arrhythmiassuch as atrial fibrillation (AF), atrial flutter (AFL),and incisional atrial reentrant tachycardia (IART)are a major source of morbidity and even mortal-ity,1 particularly for patients following Fontan pal-liation.2 Current management strategies, includingcatheter-based ablation; surgical antiarrhythmiaprocedures; and medications such as flecainide,propafenone, amiodarone, and sotalol, are oftenunsatisfactory in their results. There is room foradditional therapeutic options.
The U.S. Food and Drug Administration(FDA) approved dofetilide for use in the United
Financial disclosures: None.
Address for reprints: Seshadri Balaji, M.B.B.S., M.R.C.P. (U.K.),Ph.D., 707 SW Gaines Street, CDRC-P; Portland, OR 97239. Fax:503-494-2824; e-mail: [email protected]
Received December 4, 2008; revised May 8, 2009; accepted May31, 2009.
doi: 10.1111/j.1540-8159.2009.02479.x
States on October 1, 1999, for the treatment ofpersistent atrial arrhythmia in adults3 and it isavailable in Canada through Health Canada’s spe-cial access program. The specific indications are:(1) conversion of AF/AFL to normal sinus rhythm(NSR) and (2) maintenance of NSR in patients withAF/AFL of greater than 1-week duration who havebeen converted to NSR.4 Dofetilide is a pure classIII antiarrhythmic agent, selectively blocking therapid component of the delayed rectifier current,IKr. It prolongs myocardial repolarization and theeffective refractory period.5 The QT interval is pro-longed, thus increasing risk of torsade de pointes(TdP). Information regarding dofetilide use in pa-tients with CHD is limited. Concerns about safetyand efficacy have limited its use in this popula-tion. We present the combined experience of fourcenters using dofetilide in patients with CHD.
Materials and MethodsStudy Design
This institutional review board-approvedstudy is a multicenter, retrospective study ofthe use of dofetilide to treat atrial arrhythmiasin patients with CHD from September 2000 toDecember 2007.
C©2009, The Authors. Journal compilation C©2009 Wiley Periodicals, Inc.
PACE, Vol. 32 October 2009 1313

WELLS, ET AL.
Subjects
All members of the Pediatric and CongenitalElectrophysiology Society (PACES) were con-tacted via email, and invited to submit data onpatients with CHD and atrial arrhythmia whohad been treated with dofetilide. Physicians atfour centers responded to our request and con-tributed data. One center from Europe respondedwith data on the use of intravenous dofetilidebut was rejected because this fell outside thepurview of the current study. We are unsurewhether dofetilide was used at other institutionson similar patients. Subjects at Oregon Health& Science University (OHSU) and the MontrealHeart Institute were identified by querying thepharmacy database for dofetilide dispensed, thenidentifying all instances in which the recipienthad CHD. Subjects at the other two institutionswere identified by treating physician’s personalknowledge of patients with CHD who had receiveddofetilide. Electronic and paper medical recordswere reviewed for demographic information,CHD diagnoses, prior cardiac surgeries, arrhyth-mia diagnoses, prior antiarrhythmic medication(AAM) use (including intravenous ibutilide),catheter-based ablation attempts, pacemaker use,echocardiography reports of ventricular function,and physiologic data related to initiation ofdofetilide (creatinine clearance, cardiac rhythm,QTc duration). Response to dofetilide, whetherdofetilide was continued and for how long, rea-sons for discontinuation, and adverse events weredetermined. The complete success of dofetilidetherapy was defined as conversion to or mainte-nance of NSR with minimal or no breakthrough,with no adverse effect. Partial success was definedas a reduction in the frequency and/or severityof episodes of arrhythmia, such that therapy wasdeemed worth continuing.
Analysis
Data were collected on a standardized work-sheet and tabulated. Continuous variables arepresented as mean ± standard deviation (SD)or median and range, depending on normalityof their distribution. Dichotomous variables aresummarized as frequencies and percentages. Com-parisons between baseline and peak QTc wereperformed using a nonparametric paired-signtest. A two-tailed P-value < 0.05 was consideredstatistically significant. Testing was performedwith SAS software Version 9.1 (SAS Institute,Cary, NC, USA).
ResultsTwenty patients with CHD who had received
dofetilide for atrial arrhythmia were identified and
reviewed. Table I summarizes their characteris-tics; the patients are listed in a chronological or-der by date of dofetilide initiation (earliest to mostrecent).
The median age at dofetilide initiation was30 years (range: 19–53 years). Specific CHD diag-noses are listed in Table I. All but one had under-gone prior cardiac surgery, with a mean of 2.4 ±1.2 cardiac operations per patient. Eleven of 20(55%) had completed staged palliation to Fontan.Arrhythmia diagnoses were as follows: AF (n =4), AF/IART (n = 3), and IART (n = 13). Patientshad been given an average of 3.3 ± 1.2 other AAMprior to dofetilide; see Table I for details. Three(patient numbers 3, 8, and 9) had previously re-ceived ibutilide (patient 8 did not convert to NSR;the other two did convert, but relapsed). Four-teen of 20 (70%) had undergone at least one priorcatheter-based ablation attempt (1.5 ± 0.9 per pa-tient). Ablation attempts were either unsuccess-ful, or initially successful with subsequent relapseand/or the onset of new arrhythmias. Three pa-tients had undergone prior Maze operations, allat the time of Fontan revision. Eight (40%) hadcardiac pacemakers, and three (15%) had an au-tomatic implantable cardiac defibrillator (AICD).The ventricular function of these patients as esti-mated by echocardiography was variable (Table I).Of the two patients with TdP, one had mild reduc-tion in function and the other, normal function.Neither of the two patients with severe reductionin function experienced TdP (see Table I).
The starting dose of dofetilide was at thediscretion of the treating physician. By standardcalculations, no patient had impaired creatinineclearance (average: 118 ± 29 mL/min), and no pa-tient required dosing adjustment for renal impair-ment. Ten patients were started on 500 mcg po bid,the recommended starting dose for adults withoutrenal impairment, six on 250 mcg po bid, one on125 mcg po tid, and three on 125 mcg po bid dos-ing regimens.
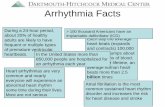
The response to dofetilide is summarized inFigure 1. Corrected QT interval (QTc) increased bya median of 7%, from 447 ms (range: 389–595 ms)at baseline to a peak of 482 ms (range: 425–600 ms),P = 0.004.
There were three (15%) immediate treatmentfailures. Two (10%) patients (#4 and #9) expe-rienced TdP. Both received a dofetilide dose of500 mcg po bid, and experienced TdP duringthe hospitalization in which dofetilide was ini-tiated. The potentially life-threatening ventriculararrhythmia was quickly recognized with success-ful resuscitation in both cases. One patient (#7)who also received 500 mcg po bid of dofetilidehad excessive QTc prolongation prompting drugdiscontinuation.
1314 October 2009 PACE, Vol. 32

DOFETILIDE IN CONGENITAL HEART DISEASE
Tab
leI.
Pat
ient
Cha
ract
eris
tics
Init
ial
Lo
ng
-P
atie
nt/
Ag
eC
HD
CH
DP
rio
rC
ath
eter
Ven
tric
ula
rD
ose
(mcg
Init
ial
Term
Use
Rea
son
Gen
der
(y)
Dia
gn
ose
sS
urg
erie
sA
rrh
yth
mia
AA
Ms
Ab
lati
on
sF
un
ctio
np
ob
id)
Eff
ect
Eff
ect
Du
rati
on
for
d/c
Effi
cacy
1/M
22D
ILV
;L-T
GA
LT-F
AF
/IAR
TS
T;P
R;
2N
500
MN
SR
WE
1.5
year
sW
EP
DG
;DI
2/M
47TO
FTO
FA
F/IA
RT
DG
;AM
2N
500
MN
SR
LTF
U?
?3/
M19
SV
AP
-FIA
RT
VR
;AM
;3
N50
0M
NS
RM
NS
R5+
year
sS
DG
;ST
4/F
35Tr
A;P
AP
VR
TrA
/PA
PV
RIA
RT
VR
;DG
;PC
0M
ild↓
500
TdP
–3
days
PrA
rF
5/F
20D
ILV
;TA
;PS
AP
-F;F
RIA
RT
AM
;DG
0N
500
MN
SR
AR
?S
AP
6/M
40D
-TG
AM
usta
rdIA
RT
VR
;DG
2M
ild↓
500
CN
SR
MN
SR
5+ye
ars
S7/
M53
TOF
TOF
;PV
RIA
RT
AT2
Sev
↓50
0M
NS
R–
1do
sein
crea
sed
FQ
Tc
8/M
34B
AV
;AS
;A
VR
;MV
IAR
TA
M;D
I;S
T2
Mod
↓50
0M
NS
RM
NS
R*
?C
ost
Pab
norm
alM
V9/
F20
DIL
VA
P-F
IAR
TP
C;S
T;
1N
500
TdP
–A
few
dose
sP
rAr
FAT
;DG
10/F
21TA
AP
-F;F
RA
F/IA
RT
FL;
AM
2N
500
MP
RD
A1+
year
P11
/M20
PA-I
VS
AP
-FIA
RT
AM
;ST
;PR
0N
125
tidM
NS
RD
A3
wee
ksS
AP
12/M
26PA
-IV
SA
P-F
;FR
AF
AM
;ST
;DI
0M
od↓
125
CN
SR
MN
SR
*9+
mon
ths
P13
/M43
D-T
GA
;PS
Mus
tard
AF
AM
;ST
;PR
;1
Mod
↓25
0M
NS
RM
NS
R6+
mon
ths
SM
P;D
G14
/F34
TAA
P-F
IAR
TA
M;S
T;
1M
od↓
250
MN
SR
MN
SR
5+m
onth
sS
BB
;VR
15/M
27D
ILV
;L-T
GA
Font
an;F
RIA
RT
DG
;AM
2S
ev↓
125
DA
DA
1+ye
arP
16/F
29TA
AP
-FIA
RT
AM
;ST
;DG
2N
250
EA
EA
11+
mon
ths
S17
/M40
DO
RV
;TG
AFo
ntan
IAR
TA
M;P
R;D
G2
N25
0M
NS
RM
NS
R*
10+
mon
ths
P18
/F49
PA;V
SD
;AP
Cno
neIA
RT
AM
;BP
0M
od↓
125
MN
SR
MN
SR
6+m
onth
sS
19/F
30D
-TG
A;V
SD
;S
enni
ngA
FA
M;S
T;D
I2
N25
0E
AE
A1+
mon
thS
sub-
PS
20/M
19A
SD
AS
DA
FP
R;S
T0
N25
0D
AA
R4
mon
ths
WE
P
AF
=at
rialfi
brill
atio
n;A
FL
=at
rialfl
utte
r;A
M=
amio
daro
ne;A
PC
=ao
rto-
pulm
onar
yco
llate
rals
;AP
-F=
atrio
-pul
mon
ary
Font
an;A
R=
arrh
ythm
iare
curr
ed;A
S=
aort
icst
enos
is;
AS
D=
atria
lsep
tald
efec
t(se
cund
um);
AT=
aten
olol
;AV
R=
aort
icva
lve
repl
acem
ent;
BA
V=
bicu
spid
aort
icva
lve;
BP
=B
isop
rolo
l;C
NS
R=
conv
erte
dto
NS
R;D
A=
decr
ease
dar
rhyt
hmia
;DG
=di
goxi
n;D
I=di
ltiaz
em;D
ILV
=do
uble
inle
tlef
tven
tric
le;D
OR
V=
doub
leou
tletr
ight
vent
ricle
;D-T
GA
=de
xtro
-tra
nspo
sed
grea
tart
erie
s;E
A=
elim
inat
edar
rhyt
hmia
;F=
failu
re;F
L=
fleca
inid
e;F
R=
Font
anre
visi
on;I
AR
T=
inci
sion
alat
rialr
eent
rant
tach
ycar
dia;
LT-F
=la
tera
ltun
nelF
onta
n;LT
FU
=lo
stto
follo
w-u
p;L-
TG
A=
levo
-tra
nspo
sed
grea
tart
erie
s;M
NS
R=
mai
ntai
ned
NS
R;M
NS
R*
=m
aint
aine
dN
SR
with
occa
sion
albr
eakt
hrou
ghar
rhyt
hmia
;Mod
=m
oder
ate;
MP
=m
etop
rolo
l;M
PR
=m
aint
aine
dpa
ced
rhyt
hm;M
V=
mitr
alva
lve;
NS
R=
norm
alsi
nus
rhyt
hm;P
=pa
rtia
l;P
rAr=
proa
rrhy
thm
ia;P
A=
pulm
onar
yat
resi
a;PA
-IV
S=
pulm
onar
yat
resi
aw
ithin
tact
vent
ricul
arse
ptum
;PA
PV
R=
part
iala
nom
alou
spu
lmon
ary
veno
usre
turn
;PC
=pr
ocai
nam
ide;
PR
=pr
opaf
enon
e;P
S=
pulm
onar
yst
enos
is;P
VR
=pu
lmon
ary
valv
ere
plac
emen
t;S
=su
cces
s;S
A=
succ
essf
ulab
latio
n;S
T=
sota
lol;
Sev
=se
vere
;SV
=si
ngle
vent
ricle
notf
urth
erde
scrib
ed;T
A=
tric
uspi
dat
resi
a;TO
F=
tetr
alog
yof
Fallo
t;Tr
A=
trun
cus
arte
riosu
s;W
E=
wan
ing
effic
acy;
VR
=ve
rapa
mil;
VS
D=
vent
ricul
arse
ptal
defe
ct;V
T=
vent
ricul
arta
chyc
ardi
a.
PACE, Vol. 32 October 2009 1315

WELLS, ET AL.
Figure 1. Response to dofetilide in CHD patients with atrial arrhythmias.
Conversion to or maintenance of NSR withno adverse effect during the 72-hour in-hospitalobservation following initiation of dofetilide wasobserved in 17 (85%) patients. These 17 were alltaking dofetilide at the time of discharge from thehospitalization during which dofetilide was ini-tiated. One of them (#2) was lost to follow-upshortly after starting dofetilide, and long-term ef-fects or adverse events could not be determined.Five of the 17 patients who left the hospital tak-ing dofetilide subsequently discontinued it as aresult of waning benefit, with recurrent arrhyth-mias. One these five discontinued the drug foreconomic reasons, despite having some reductionin the frequency of arrhythmia. Two of those whodiscontinued for waning effect went on to success-ful catheter ablation.
Eleven of 20 patients (55%) started ondofetilide in this series were still taking it at mostrecent follow-up. Duration of therapy ranged fromabout 1 month to greater than 5 years, with a me-dian follow-up approaching 1 year. Seven of the20 (35%) have had total suppression of their ar-rhythmia, and are considered complete successes.Four of the 20 (20%) continue to have occasionalbreakthrough episodes of their underlying atrialarrhythmia, but find their episodes less frequentand subjectively less severe. Despite occasionalbreakthroughs, these patients wish to continuedofetilide therapy. No patient experienced TdPsince hospital discharge.
DiscussionDofetilide successfully converted and main-
tained NSR in a significant proportion of patients
with CHD and atrial arrhythmias in this study,with small (but not negligible) incidence of seriousadverse effect.
Efficacy
The patients reported in the current studywere refractory to previously attempted therapies.They were given a variety of alternative AAMswith unsatisfactory results or intolerable side ef-fects. Fifteen of 20 (75%) had undergone at leastone prior ablation attempt.
Initial success with dofetilide was impres-sive, with 85% of patients converting to or main-taining NSR during the in-hospital observationperiod immediately following dofetilide initia-tion. Mykytsey et al. reported initial success withdofetilide in 31 of 34 patients (91%) with paroxys-mal AF and normal left ventricular (LV) function(no CHD).6 The Symptomatic Atrial FibrillationInvestigative Research on Dofetilide (SAFIRE-D)study was a double-blinded, placebo-controlled,multicenter study to determine the efficacy andsafety of dofetilide in converting to and main-taining NSR in patients with AF or AFL (noCHD).7 The investigators reported an initial phar-macologic conversion rate of 6.1%, 9.8%, and29.9% in subjects given 125, 250, and 500 mcgof dofetilide twice daily respectively, versus 1.2%in the placebo group.7 A direct comparison can-not be made between these results and those ofthe group presently reported, as some of the CHDpatients were in NSR at the time of dofetilide ini-tiation. Nonetheless, the observed initial successof dofetilide in managing atrial arrhythmias in pa-tients with CHD is encouraging.
1316 October 2009 PACE, Vol. 32

DOFETILIDE IN CONGENITAL HEART DISEASE
Perhaps more clinically meaningful is the55% long-term success rate (patients still takingthe medication with diminished or suppressedarrhythmia at a median follow-up of nearly oneyear) in patients with CHD and previously refrac-tory atrial arrhythmias. Mykytsey et al. reportedsymptomatic improvement persisted at 12 monthsin 18 of 31 (58%) in their series.6 Seven of 20 pa-tients (35%) in the presently reported series expe-rienced complete suppression of their arrhythmia.This compares favorably with the long-term suc-cess rate of dofetilide reported in patients with-out CHD. A substudy of the Danish Investiga-tions of Arrhythmia and Mortality ON Dofetilidein congestive heart failure (DIAMOND-CHF) andacute myocardial infarction (DIAMOND-MI) stud-ies specifically evaluated the efficacy of dofetilidein treating AF/AFL in patients with reduced LVfunction.8 The investigators reported that 112 of249 (45%) patients randomized to dofetilide ex-perienced and maintained spontaneous or phar-macologically induced conversion to NSR duringthe study period (minimum follow-up period of12 months), versus 35 of 257 (14%) of placebo-treated controls (P < 0.001).8 In the SAFIRE-D study, the probability of maintaining NSR at360 days following conversion by any means(pharmacologic or electric) was 40%, 37%, and58% in the 125, 250, and 500 mcg twice dailygroups, respectively, versus 25% in the placebogroup (P = 0.001 for the 500 mcg twice daily groupversus placebo).7
It is worth noting that DIAMOND-CHF,9DIAMOND-MI,10 the DIAMOND substudy ofdofetilide in patients with AF/AFL and reducedLV function,8 and SAFIRE-D7 had comparablemortality rates for patients treated with dofetilideversus placebo. Despite favorable effects on mor-bidity in many patients in the presently reportedgroup, it remains to be seen whether there is trulyany long-term mortality benefit.
Safety
Serious adverse effect, namely TdP, was ob-served in a small but significant minority of pa-tients in this series (two patients, 10% of CHDpatients given dofetilide in this series). There wasno observable correlation between occurrence ofTdP and ventricular function in these two patients.Both had been started on 500 mcg orally twicea day, which is the recommended starting dosein patients without renal impairment. In both in-stances the patient was still in the hospital, facil-itating rapid identification and resuscitation, andunderscoring the importance of adherence to cur-rent prescribing guidelines that mandate inpatientobservation with continuous monitoring for a min-imum 3 days when dofetilide is initiated. The re-
ported incidence of TdP in larger series of non-CHD patients is between 0.4% and 2.9% wheninitial dose is based on renal function as recom-mended.4 Patients with CHD may be more sus-ceptible to TdP when given dofetilide; the limitednumber of subjects in this series prevents conclu-sive evaluation of this possibility. There has beena trend to use a lower than recommended startingdose in the more recent patients reported in thisseries; the last nine patients have been initiatedon less than 500 mcg twice daily. Although thelimited sample size precludes inferential analyses,antiarrhythmic efficacy was noted at lower thanrecommended doses with no episodes of TdP de-spite ongoing therapy in all but one patient. There-fore, in patients with CHD it may be prudent toinitiate dofetilide therapy at lower than standarddoses with judicious and monitored titration asneeded.
Alternatives
The efficacy and safety of dofetilide needs tobe assessed in the context of other antiarrhyth-mic agents currently available. Alternatives in-clude class IA agents quinidine and procainamide,class IC agents flecainide11 and propafenone,12
and class III agents sotalol13 and amiodarone.14
All of these agents are associated with significantside effects, including proarrhythmia.
Limitations
Despite drawing on the experience of four in-stitutions, the present study is hampered by rel-atively limited number of subjects. It is however,to our knowledge, the only study currently avail-able evaluating the safety and efficacy of dofetilidein CHD. Inconsistency in the starting dose is oneof the inherent challenges of a retrospective eval-uation of clinical practice. Nonetheless, the po-tentially valuable observations that TdP occurredonly in two patients receiving the package-insertrecommended starting dose of 500 mcg orallytwice daily, and that as the trend in initial dosehas been toward lower doses no patient has experi-enced TdP, may be useful in clinical practice. Onemight consider a lower starting dose of dofetilidein subgroups of CHD patients even in the presenceof apparently unimpaired renal function.
ConclusionsThese findings suggest that, while dofetilide is
not the answer for every CHD patient with atrial ar-rhythmias, when used appropriately it can benefita significant proportion of these patients who areoften difficult to treat. Initial efficacy of dofetilidefor the treatment of refractory atrial arrhythmiasin CHD patients is high, with long-term efficacyhistorically comparable to patients without CHD.
PACE, Vol. 32 October 2009 1317

WELLS, ET AL.
Subtypes of patients with CHD, such as those withuniventricular physiology, may be at higher risk ofTdP when standard recommended starting dosesof dofetilide are utilized. Adherence to prescribingguidelines that mandate inpatient monitoring fora minimum 3-day observation following dofetilideinitiation is critical. Consideration should be givento using a lower than recommended starting dose,despite apparently normal renal function. In the
challenging population of CHD patients with re-fractory atrial arrhythmias, dofetilide appears tobe a viable adjunct to catheter-based ablation andalternative pharmacological approaches.
Acknowledgments: The authors wish to thank MaudeBergeron, RN (Montreal Heart Institute) for her expertassistance.
References1. Walsh EP. Arrhythmias in patients with congenital heart disease.
Card Electrophysiol Rev 2002; 6:422–430.2. Balaji S, Johnson TB, Sade RM, Case CL, Gillette PC. Management
of atrial flutter after the Fontan procedure. J Am Coll Cardiol 1994;23:1209–1215.
3. Approved Drug Products With Therapeutic Equivalence Evaluation:U.S. Government Printing Office/Washington, D.C., 2003.
4. Pfizer. Tikosyn (Dofetilide) Full Prescribing Information: 2004.5. Mounsey JP, DiMarco JP. Cardiovascular drugs: Dofetilide. Circula-
tion 2000; 102:2665–2670.6. Mykytsey A, Bauman JL, Razminia M, Zheutlin T, Wang T, Saleem
M, Leal S, et al. Observations on the safety and effectiveness ofdofetilide in patients with paroxysmal atrial fibrillation and normalleft ventricular function. J Cardiovasc Pharmacol Ther 2007; 12:36–43.
7. Singh S, Zoble RG, Yellen L, Brodsky MA, Feld GK, Berk M, BillingCB Jr. Efficacy and safety of oral dofetilide in converting to andmaintaining sinus rhythm in patients with chronic atrial fibrilla-tion or atrial flutter: The Symptomatic Atrial Fibrillation Investiga-tive REsearch on Dofetilide (SAFIRE-D) study. Circulation 2000;102:2385–2390.
8. Pedersen OD, Bagger H, Keller N, Marchant B, Kober L, Torp-Pedersen C. Efficacy of dofetilide in the treatment of atrialfibrillation-flutter in patients with reduced left ventricular func-tion: A Danish Investigations of Arrhythmia and Mortality ON
Dofetilide (DIAMOND) substudy. Circulation 2001; 104:292–296.
9. Torp-Pedersen C, Moller M, Bloch-Thomsen PE, Kober L, SandoeE, Egstrup K, Agner E, et al. Dofetilide in patients with congestiveheart failure and left ventricular dysfunction. Danish Investigationsof Arrhythmia and Mortality on Dofetilide Study Group. N Engl JMed 1999; 341:857–865.
10. Kober L, Bloch Thomsen PE, Moller M, Torp-Pedersen C, Carlsen J,Sandoe E, Egstrup K, et al. Effect of dofetilide in patients with re-cent myocardial infarction and left-ventricular dysfunction: A ran-domised trial. Lancet 2000; 356:2052–2058.
11. Fish FA, Gillette PC, Benson DW, Jr. Proarrhythmia, cardiac arrestand death in young patients receiving encainide and flecainide. ThePediatric Electrophysiology Group. J Am Coll Cardiol 1991; 18:356–365.
12. Janousek J, Paul T. Safety of oral propafenone in the treatment ofarrhythmias in infants and children (European retrospective multi-center study). Working Group on Pediatric Arrhythmias and Electro-physiology of the Association of European Pediatric Cardiologists.Am J Cardiol 1998; 81:1121–1124.
13. Beaufort-Krol GC, Bink-Boelkens MT. Sotalol for atrial tachycardiasafter surgery for congenital heart disease. Pacing Clin Electrophysiol1997; 20:2125–2129.
14. Villain E. Amiodarone as treatment for atrial tachycardias aftersurgery. Pacing Clin Electrophysiol 1997; 20:2130–2132.
1318 October 2009 PACE, Vol. 32