Clinical Features & Diagnosis of Dental Caries CHEN Zhi Wuhan University School of Stomatology.
diagnosis Occupational asthma: Clinical features, evaluation, and · 2019-09-16 · The clinical...
Transcript of diagnosis Occupational asthma: Clinical features, evaluation, and · 2019-09-16 · The clinical...

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 1/30
Official reprint from UpToDate www.uptodate.com ©2019 UpToDate, Inc. and/or its affiliates. All Rights Reserved.
Occupational asthma: Clinical features, evaluation, anddiagnosisAuthors: Catherine Lemière, MD, André Cartier, MD, Louis-Philippe Boulet, MD, David I Bernstein, MDSection Editor: Peter J Barnes, DM, DSc, FRCP, FRSDeputy Editor: Helen Hollingsworth, MD
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Aug 2019. | This topic last updated: Jul 02, 2019.
INTRODUCTION
Occupational asthma (OA) is a form of work-related asthma characterized by variable airflowobstruction, airway hyperresponsiveness, and airway inflammation attributable to exposures in theworkplace and not due to stimuli encountered outside the workplace [1]. Work-exacerbatedasthma (also known as work-aggravated asthma) is defined as preexisting or concurrent asthmathat subjectively worsens in the workplace.
The clinical features, evaluation, and diagnosis of suspected OA will be reviewed here. Thepathophysiology, epidemiology, causes, risk factors, and management of OA and reactive airwaysdysfunction syndrome are discussed separately. (See "Occupational asthma: Pathogenesis" and"Occupational asthma: Definitions, epidemiology, causes, and risk factors" and "Occupationalasthma: Management, prognosis, and prevention" and "Overview of occupational andenvironmental health" and "Reactive airways dysfunction syndrome and irritant-induced asthma".)
CLINICAL FEATURES
Lower respiratory symptoms — The typical symptoms of OA are the same as nonoccupationalasthma and include cough, sputum production, dyspnea, wheeze, and chest tightness. (See"Diagnosis of asthma in adolescents and adults", section on 'Clinical features'.)
Some patients report a pattern of increased symptoms while at work or within several hours of thecompletion of a work shift and improvement on weekends or during vacations, but this is variable.(See 'Time course' below.)
®

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 2/30
Once sensitized, workers exposed to high molecular weight (HMW) agents are more likely toreport early (eg, within an hour of workplace exposure) asthmatic reactions [2,3]. In contrast,workers exposed to low molecular weight (LMW) agents are more likely to experience lateasthmatic reactions. The delay in symptom onset with LMW agents may reflect mediation by anon-immunoglobulin E (IgE) mechanism. (See "Occupational asthma: Definitions, epidemiology,causes, and risk factors", section on 'Causative agents'.)
Extrapulmonary symptoms — Certain patterns of extrapulmonary symptoms are stronglyassociated with OA, although they are not sufficiently specific to secure a diagnosis or cause ofOA.
Rhinoconjunctivitis – Symptoms of work-related rhinoconjunctivitis (itchy eyes, tearing,sneezing, nasal congestion, rhinorrhea) often precede symptoms of OA caused by HMWproteinaceous agents [3-7], or may accompany symptoms of OA caused by other HMWagents and the LMW agents [8]. In general, workers with HMW-inducer OA are more likely toreport occupational rhinitis (OR 4.79, 95% CI 3.28-7.12) or conjunctivitis (OR 2.13, 95% CI1.52-2.98), compared with those with LMW-inducer OA, and their symptoms are often moresevere. (See "Occupational rhinitis".)
●
The report of work-related wheezing, nasal symptoms, and ocular itching substantiallyincreases the likelihood of OA, especially among workers exposed to HMW agents [8].However, these symptoms are not predictive in subjects exposed to LMW agents. (See"Occupational asthma: Definitions, epidemiology, causes, and risk factors", section on'Causative agents'.)
Allergic contact dermatitis – Several agents that cause OA (eg, diisocyanates, epoxies,latex, or cleaning agents) have been associated with allergic contact dermatitis [9-16].However, the occurrence of contact dermatitis is generally not predictive of OA [17]. (See"Common allergens in allergic contact dermatitis" and "Clinical features and diagnosis ofallergic contact dermatitis".)
●
An exception comes from a study of adolescent car painting apprentices (exposed todiisocyanates) in which occupational dermatitis was predictive of work-related asthmasymptoms [9]. Cobalt exposure has also been associated with the combination of OA andcontact dermatitis [14].
Urticaria – Work-related urticaria on exposed body parts is sometimes seen with exposure toHMW agents such as latex, mammalian proteins from furry animals, or crustaceans (eg, crab)and may suggest an IgE-mediated process, but there are no studies looking at its predictivevalue for the development of OA. (See "Chronic spontaneous urticaria: Clinicalmanifestations, diagnosis, pathogenesis, and natural history".)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 3/30
Physical examination — The physical examination in OA is generally nonspecific and may benormal during office visits away from the occupational exposure. Widespread, high-pitchedwheezes are characteristic of asthma, heard most commonly on expiration, but sometimes alsoduring inspiration. However, the presence or absence of wheezing on physical examination is apoor predictor of the presence or severity of OA. (See "Diagnosis of asthma in adolescents andadults" and "Diagnosis of asthma in adolescents and adults", section on 'Physical findings'.)
Patients with OA may also have pale, swollen nasal mucosa, suggesting concomitantoccupational rhinitis [18]. (See "Occupational rhinitis".)
Rarely, an erythematous, eczematous rash (consistent with allergic contact dermatitis) or urticarialrash may be present on skin exposed to the sensitizing agent in the workplace. (See "Clinicalfeatures and diagnosis of allergic contact dermatitis".)
EVALUATION
OA should be suspected in every adult with new onset asthma, as OA accounts for approximately10 to 15 percent of adult onset asthma with some between study variability [19,20]. For allpatients, the evaluation begins with an occupational history, focused on known or potentialsensitizing agents. Our approach to testing combines complementary tests, as individual testshave limitations when viewed in isolation. The approach differs if patients are still working andexposed to causative substances or are no longer working. (See "Occupational asthma:Definitions, epidemiology, causes, and risk factors", section on 'Epidemiology'.)
Occupational history — The onset of symptoms relative to exposure varies and a work-relatedassociation may not be spontaneously reported by the patient. Thus, the clinical history in patientswith possible OA should include detailed information about the job description and potentialexposures to causal agents, in addition to the routine evaluation of adult-onset asthma (table 1)[21]. The clinical history, while important, is not sufficient to confirm or exclude the diagnosis of OA[22-24]. (See "Diagnosis of asthma in adolescents and adults".)
Exposures — All adults with asthma should be questioned not only about their currentoccupation and exposures, but also about their previous occupations and exposures (table 2).Once the patient’s occupation is ascertained, the potential associated exposures can be evaluatedin greater detail. Asking about exposure to vapors, gas, fumes, or dust may help the patient’srecall [25].
Hoarseness – Questionnaires are poorly specific in diagnosing OA. However, amongsymptoms reported by workers referred for possible OA, wheezing, nasal, and ocular itchingat work were positively, and loss of voice negatively, associated with the presence of OA inthe case of HMW, but not LMW agents [8].
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 4/30
As examples, the job description of "engineer" or "clerk" does not yield a full account of the actualexposures in the workplace. Further questioning may reveal indirect exposure to a sensitizingagent depending upon the particular work environment (eg, auto body shop, office building, epoxypaint factory). Janitorial and healthcare work may involve use of amines or bleach in cleaning.Exposure to cigarette smoke (active or passive) can occur in many occupations and may triggersymptoms on an irritant basis.
Occupation-specific exposures – Certain industries or professions are associated withgreater contact with agents that have a high potential for provoking OA [26]. As examples,nurses may be exposed to psyllium, chlorhexidine, pharmaceutical products, enzymes,glutaraldehyde, or formaldehyde, while spray painters may be exposed to diisocyanates,acrylates, and various amines (table 2). A description of the more common causative agentsand their associated occupations is provided separately. (See "Occupational asthma:Definitions, epidemiology, causes, and risk factors", section on 'Causative agents'.)
●
Additional information on agents that cause OA is available athttps://www.csst.qc.ca/en/prevention/reptox/occupational-asthma.
Material safety data sheet (MSDS) – When OA is suspected, but the exact cause is unclear,it is important to obtain a list of all potential causative agents. If the names of the chemicals inthe workplace are not known, the worker can obtain the MSDS from the employer. In theUnited States, the Occupational Safety and Health Administration (OSHA) requires thatsuppliers include a MSDS with each shipment of an industrial material or chemical, andworkers are entitled to receive copies of these sheets.
●
Importantly, one should not depend entirely upon the information present in safety datasheets, because regulations stipulate that materials present in concentrations less than 1percent need not be reported and high molecular weight (HMW) compounds from animal andplant sources are typically omitted [27].
Nonspecific irritants – Asking about exposure to nonspecific irritants (eg, environmentaltobacco smoke, strong fumes, extremes of temperature and humidity) is important as all typesof asthma can be worsened by exposure to nonspecific irritants at work, a condition that islabeled work-exacerbated asthma [28]. This sensitivity to nonspecific irritants is particularlylikely among patients who are exposed to chemical products such as ammonia, engine-exhaust fuel, aerosols and solvents [29], have severe airway (bronchial)hyperresponsiveness, and/or are undertreated with medication. (See "Occupational asthma:Definitions, epidemiology, causes, and risk factors", section on 'Definitions'.)
●
Few studies have investigated non-allergic irritant-induced asthma in which multiple irritantexposures at low concentrations appear to induce asthma in the absence of pre-existingasthma [30]. Since there is no specific testing that can prove that asthma has been caused by

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 5/30
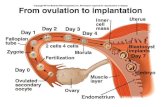
Time course — The natural history of OA is characterized by the following progression (figure1):
The latency period between the onset of exposure and the onset of symptoms is highly variable inOA, ranging from months to years. The latency period may vary according to the type of agent,being shorter with exposure to low molecular weight (LMW) agents, such as diisocyanates andplicatic acid (Western red cedar), than with HMW agents (table 2) [32].
As an example, approximately 50 percent of subjects who develop OA due to diisocyanatesexperience symptoms within the first two years after the onset of exposure, whereas the medianlatency period after exposure to HMW agents is approximately five years [32]. The latency periodalso varies between HMW agents; sensitization to laboratory animals occurs more commonly andrapidly than sensitization to flour [4].
A pattern of increased symptoms while at work or within several hours of the completion of a shift,and a definite improvement on weekends or during vacations, is common in OA, but documentingthis feature is not necessarily helpful. In a series of 162 patients referred for evaluation of possibleOA, 88 percent of patients with confirmed OA stated that their symptoms improved duringholidays, while 76 percent of patients without OA reported a similar improvement [22]. In addition,the absence of this pattern does not exclude the possibility of OA.
Workers with more advanced OA and those who are only away from work for brief intervals areless likely to report this classic pattern, possibly due to a combination of early and late phasereactions that lead to persistent symptoms. (See "Pathogenesis of asthma", section on 'Early andlate phase reactions'.)
Furthermore, workers may not be exposed to the etiologic agent every day, and intermittentexposures make it difficult to relate symptoms to work.
repetitive exposure to an irritant agent, it is often difficult to establish the diagnosis of irritant-induced asthma with certainty. However, epidemiologic studies suggest that some jobs, likecleaning and pulp mill work that are associated with exposure to high concentration ofirritants, are associated with an increasing risk for the occurrence of asthma [31]. Irritant-induced asthma is discussed separately. (See "Reactive airways dysfunction syndrome andirritant-induced asthma".)
Onset of exposure●
Sensitization●
Onset of upper and lower airway inflammation●
Clinical disease●
Cessation or persistence of exposure●
Cure, improvement, or persistence of asthma●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 6/30
Atopy — The possibility of pre-existing asthma and atopy (genetic predilection to producespecific immunoglobulin E (IgE) following exposure to allergens) should be explored in all patientswith suspected occupational asthma. Thus, we ask patients about prior symptoms suggestive ofasthma, allergic rhinitis, and atopic dermatitis. This information can help determine whether thepatient has new onset disease or a pre-existing process that has worsened. (See "The relationshipbetween IgE and allergic disease".)
However, atopy by itself has a poor positive predictive value for the presence of OA.
Skin and immunologic testing — Skin tests and immunoassays for serum specific IgE (ssIgE)have several roles in the evaluation of OA: they can identify sensitization to potential culpritallergens (when available); they can be used to identify sensitivity to common (nonoccupational)aeroallergens that can contribute to symptoms; and newer molecular methods may eventuallyimprove the ability of testing to relate specific epitope sensitivity to the likelihood of disease.
The presence of immediate skin test reactivity or ssIgE reflects specific sensitization, but apositive result can be found in some patients without symptoms of asthma or rhinoconjunctivitis.Therefore, it is important to document objective evidence of physiological changes (eg, airflowobstruction, airway hyperresponsiveness, and/or increased sputum eosinophils) related toexposure, in addition to skin test reactivity or positive testing for specific IgE.
Only approximately one-third of atopic subjects developed rhinoconjunctivitis or asthmasymptoms in the five years following onset of exposure to laboratory animals [33].
●
Atopy is weakly associated with OA due to HMW agents, but because atopy is present inalmost 50 percent of young adults, it cannot satisfactorily predict the development of OA.
●
Furthermore, pre-existing asthma is not a predisposing factor for immunologic OA.●
Skin prick test to common aeroallergens – Skin testing with a panel of commonaeroallergens is often performed to identify nonoccupational allergens (eg, pets, pollen, dustmite) that may be contributing to the patient’s asthma. (See "Overview of skin testing forallergic disease".)
●
Skin testing to potential culprit allergens – Skin test reagents for documentinghypersensitivity are only available for a few occupational agents. Extracts of HMW antigens,such as plant material (wheat), mold (Alternaria, Cladosporium), and animal proteins(laboratory animals, insects), have a sensitivity of 0.74 (95% CI 0.66-0.80) and a specificity of0.71 (95% CI 0.63-0.77), while extracts of LMW agents have a much lower sensitivity and areless commonly available [34,35].
●
Skin testing can be performed with extracts of HMW agents made in the clinic using materialprovided by the worker, but these extracts are not standardized and are not very specific orsensitive.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 7/30
Pulmonary function tests — Baseline spirometry should be obtained in virtually all patients withsuspected OA. If airflow limitation is not present, the next step is either nonspecificbronchoprovocation testing or serial peak flow or spirometry at work and at home. For patientswho are no longer working, nonspecific bronchoprovocation is used to document the presence orabsence of airway hyperresponsiveness.
Spirometry before and after bronchodilator — Baseline spirometry before and afterbronchodilator is used to determine the presence and severity of any airflow limitation [39]. Theresults of spirometry determine the most appropriate next test and are useful as a baseline forfuture assessments.
In a subject with airflow obstruction (ie, a ratio of forced expiratory volume in one second[FEV ]/forced vital capacity [FVC] below the lower limit of normal), the next step is to assessreversibility with inhaled bronchodilator. The presence of a significant increase in FEV (12 percent
Negative skin prick tests with HMW allergens (eg, relevant cereals, mites, and enzymes in abaker) virtually exclude the possibility that OA is caused by that specific antigen [19,24]. (See"Occupational asthma: Definitions, epidemiology, causes, and risk factors", section on'Combined exposures'.)
Serum specific IgE antibodies – In vitro immunoassay for IgE antibodies to occupationalsensitizers is available for a limited number of HMW agents (eg, animal danders, latex,wheat) and LMW chemical-protein conjugates (eg, diisocyanates), but these are notstandardized or not always commercially available [19]. When positive, they support but donot confirm the diagnosis of OA to that agent; furthermore, the sensitivity of this testing is low,particularly with LMW agents. (See "Overview of in vitro allergy tests", section on'Immunoassays'.)
●
Some LMW agents, such as platinum salts and trimellitic or phthalic anhydride, can bedeveloped for skin testing, but these are usually not standardized and the sensitivity of testingis low (table 2).
Recombinant allergens and component resolved diagnosis – Component resolveddiagnosis is an emerging molecular method for the diagnosis of OA and rhinitis [36-38]. Itutilizes purified recombinant allergens to identify sensitization and characterize the specificallergens involved. It appears that IgE to certain allergenic moieties is more likely to beassociated with a severe response than IgE to other moieties. As examples, gliadin-omega-5is likely to be associated with more severe wheat allergy, and specific IgE antibodies to latexHev b and Hev b 6.01 are strongly associated with positive specific inhalation challenge[36,37]. (See "Grain allergy: Clinical features, diagnosis, and management", section on 'IgEmediated presentations'.)
●
1
1

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 8/30
and >200 mL) after inhaling a bronchodilator supports the diagnosis of asthma. (See "Pulmonaryfunction testing in asthma", section on 'Bronchodilator responses'.)
Restrictive physiology in the absence of airflow limitation suggests that the patient’s symptomsmay have an alternate etiology. Further evaluation usually includes full pulmonary function testingand radiographic imaging. (See "Overview of pulmonary function testing in adults", section on'Restrictive ventilatory defect'.)
Nonspecific bronchoprovocation challenge — In the absence of airflow limitation atbaseline, the next step is to assess nonspecific bronchial (airway) responsiveness, a characteristicfeature of asthma. Typically, a pharmacologic agent, such as methacholine or histamine, is used.(See "Bronchoprovocation testing".)
If the FEV does not decrease by 20 percent with a methacholine dose of 16 mg/mL or less, thetest excludes significant bronchial hyperresponsiveness [40]. Absence of bronchialhyperresponsiveness could be due to lack of recent exposure to the sensitizing agent in a workerwho has been away from work, but virtually rules out occupational asthma in a worker who hascontinued to work and is symptomatic. For patients who have been away from the workplace andhave negative initial bronchoprovocation testing, repeat bronchoprovocation testing after anexposure to the causative agent (in the laboratory or at work) may then reveal bronchialhyperresponsiveness. (See 'Advanced testing' below.)
Serial peak expiratory flow measurement — Serial measurement of peak expiratory flow(PEF) can be useful in the investigation and assessment of OA by demonstrating work-associatedairflow limitation (eg, a decrease in peak flow by ≥20 percent at work compared with values athome) [41-43]. Serial PEF is sometimes used to confirm a diagnosis of asthma by demonstratingvariable airflow limitation, but spirometry pre and post bronchodilator is preferred. (See 'Spirometrybefore and after bronchodilator' above.)
The subject is instructed on the proper use of the peak flow meter and asked to record his or herPEF a minimum of four times per day for a period of at least two weeks at work and during asimilar period away from work [44]. The period of testing at work should be shortened if the patientdevelops pronounced airway obstruction or has severe symptoms. The normal degree of PEFvariation is <15 percent; variability ≥20 percent associated with workplace exposure supports OA[45]. (See "Peak expiratory flow monitoring in asthma".)
A number of potential problems are inherent to serial PEF monitoring, including the variablereproducibility of readings, compliance and honesty of subjects, interpretation of results, andsensitivity and specificity compared with specific inhalation challenges [20]. Newer portable peakflow meters store values electronically, enabling identification of falsified patient logs, althoughvariable patient effort remains a problem. Interpretation of graphs of serial PEF measurements can
1

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sourc… 9/30
be carried out by using a computer program called OASYS, although this is more typically used inworkplace investigations than in the care of individual patients [46,47].
Ideally, monitoring of PEF should be combined with monitoring of nonspecific bronchialresponsiveness (NSBR) at and off work (see below). When there is discrepancy between changesin PEF and NSBR, further testing such as specific inhalation challenges may be required.
Serial spirometry at work — Spirometry provides more detailed information about airflow andmore reliable results than PEF monitoring [48], but serial spirometry has limited utility in evaluatingOA. The spirometric parameter that is most reliable is the FEV ; changes in the FVC and forcedexpiratory flow at 25 to 75 percent of vital capacity are less reliable. A decrease in workplace FEV≥15 percent compared with home FEV is considered positive. (See "Office spirometry", sectionon 'Interpretation'.)
Serial spirometry can be used to identify changes in airflow limitation in and away from theworkplace, similar to the procedure for serial PEF monitoring [48]. However, unsupervised serialFEV monitoring at and off work has not proven to be as reliable as serial PEF measurement [49].Furthermore, portable spirometers are more expensive than PEF meters and the technical trainingmore complex for the worker.
Comparisons between data from exposure and nonexposure days can support (or refute) work-related exacerbations of asthma. However, a single measurement of FEV when the subject is atwork and repeating once away from work (eg, pre and post shift) does not have sufficientsensitivity nor specificity to detect a relationship between work and asthma [50-52].
Periodic spirometry measurements can be used for workplace surveillance when occupationalexposures place workers at risk for OA [39,48]. Typically, measurements are repeated at one totwo year intervals, although periodic spirometry alone is not considered a sensitive tool foridentifying new cases [53].
Advanced testing — For patients with a positive exposure history to a known inducer of OA, butnondiagnostic results from the above evaluation, additional tests (largely performed in specializedcenters) may be useful. We do sputum eosinophil counts routinely, but this test is time-consumingand requires experienced laboratory personnel.
Airway inflammation — Identifying increased airway inflammation with noninvasive tests,such as sputum eosinophil counts and fractional concentration of exhaled nitric oxide (FE ), atthe end of a period at work or following laboratory challenge can provide supportive evidence ofairway inflammation and, thus, indirect evidence of OA [54].
1
1
1
1
1
NO
Sputum cell counts – Asthmatic airway inflammation is characterized by the presence ofeosinophils in induced sputum samples; neutrophils may also be involved, especially in more
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 10/30
severe asthma. In OA, either eosinophilic or neutrophilic inflammation can be predominant,the latter being more common in OA induced by LMW agents (table 2) [55-57].
For patients who do not spontaneously raise sputum, inhalation of hypertonic saline can beused to induce sputum, ideally 7 to 24 hours after exposure [58,59]. Typically, a sample ofinduced sputum is obtained at the end of the work day, after two weeks of work, andcompared with a sample from the same time after a day at home, after two weeks off work.Inhalation of albuterol prior to sputum induction will inhibit airway obstruction induced by thehypertonic saline. We use 3 periods of 7 minutes of nebulization of increasing doses of salinesolution: 3, 4 and 5 percent. We use the Diff-Quik stain which is based upon a modification ofthe Wright Giemsa stain, although the Wright and Hansel stains are alternatives. Thenonsquamous cell differential counts are expressed as a percentage of the totalnonsquamous cell counts. This test is only available at specialized centers.
The presence of eosinophils in induced sputum (≥2 percent) suggests that either asthma oreosinophilic bronchitis is present. Eosinophilic bronchitis can be occupationally induced andcause cough and sputum production in the absence of bronchial hyperresponsiveness [60-62]. (See 'Nonspecific bronchoprovocation challenge' above and "Evaluation of subacute andchronic cough in adults", section on 'Nonasthmatic eosinophilic bronchitis'.)
The use of sputum eosinophil counts in the diagnosis of OA was compared with PEFmonitoring in a case series of 49 patients with suspected OA who were evaluated during twoweeks at work and two weeks away [54]. The combination of work-related decreases in PEFand a greater than 1 percent increase in sputum eosinophils after two weeks at workincreased both the sensitivity and specificity of OA diagnosis, compared with PEF monitoringalone. In a separate study, a 3 percent increase in sputum eosinophils following specificinhalation challenge had a positive predictive value of 75 percent for specific bronchialreactivity to occupational agents [63].
In the presence of normal airway caliber and responsiveness and no change in PEF at work,a normal induced sputum cell content in a symptomatic patient with current workplaceexposure to a known OA sensitizer excludes OA and further specific testing is not needed.
Exhaled nitric oxide – The FE generally correlates with sputum eosinophilia, but studiesexamining a role in the diagnosis of OA are conflicting [64-68]. Sputum eosinophil countsachieve a higher sensitivity and positive predictive value than FE [65], so the added valueof FE in the investigation of OA remains to be established [65]. (See "Exhaled nitric oxideanalysis and applications".)
● NO
NO
NO
The measurement of FE is appealing because it provides immediate results. However, it issensitive to confounding factors, such as smoking, atopy, and treatment with inhaledglucocorticoids. The increase in FE is not uniform among subjects who experience a
NO
NO

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 11/30
Variation in nonspecific bronchial responsiveness — Increased nonspecific bronchial(airway) responsiveness can last for years in patients with established OA; in milder OA, itresolves much more quickly, but will last for at least a day or two. Thus, nonspecific bronchialresponsiveness can be measured after two or more weeks away from work and again afterworkplace exposure to obtain more objective evidence of an occupational cause of symptoms andairflow limitation [20]. This testing is particularly helpful when the baseline spirometry and initialtesting of nonspecific bronchial responsiveness are normal.
Bronchial responsiveness is usually assessed with direct challenges using methacholine orhistamine, but indirect challenges using mannitol may also be helpful in assessing patients withoccupational asthma, especially to appreciate the severity of their disease [71]. (See"Bronchoprovocation testing", section on 'Pharmacologic challenge'.)
When assessing changes in bronchoprovocation before and after workplace or laboratoryexposure, a change of 3.2-fold (eg, 16 mg/mL to 4 mg/mL) in the concentration of methacholine orhistamine that causes a 20 percent fall in FEV is considered clinically significant [72].
When a symptomatic subject is tested within 24 hours of exposure to the suspected worksensitizer, the absence of increased bronchial responsiveness virtually excludes OA [73]. As anexception, normal responsiveness has been shown in a very few instances, generally in workerswho experience an isolated immediate reaction, without delayed bronchoconstriction severalhours later. On the other hand, absence from work for several days or longer has been associatedwith a falsely negative methacholine inhalation challenge [74,75]. If bronchoprovocation testing isnegative, but OA is still strongly suspected clinically, skin or immunoassay testing may provideevidence of sensitization. For confirmation of OA in this setting, specific inhalation challenge withthe relevant agent is needed. (See 'Specific inhalation challenge' below.)
positive asthmatic reaction during specific inhalation challenge [64,69]. Among patients with apositive specific inhalation challenge to an occupational agent, a greater increase in FE isobserved among those with sensitivity to a HMW agent than a LMW agent [70]. The use ofFE may be more useful in patients exposed to HMW agents, where an IgE-dependentreaction is involved, than in patients exposed to LMW agents [70].
NO
NO
1
Nonasthmatic eosinophilic bronchitis – When nonspecific bronchoprovocation challengetesting is negative despite ongoing exposure, induced sputum may be assessed to identifyoccupational nonasthmatic eosinophilic bronchitis as a cause of the patient’s symptoms [60].(See 'Airway inflammation' above and "Evaluation of subacute and chronic cough in adults",section on 'Nonasthmatic eosinophilic bronchitis'.)
●
Surveillance – Surveillance of asymptomatic workers is generally performed by theworkplace. Nonspecific bronchoprovocation challenge is one of the potential tools used toassess development of sensitization. In asymptomatic workers who are undergoing
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 12/30
Specific inhalation challenge — Specific inhalation challenge (SIC; also called specificbronchoprovocation challenge) with specific occupational agents is performed in specializedcenters [78]. The number of available centers is small [79,80]. Specific bronchoprovocationchallenge involves exposing subjects to occupational agents in a hospital laboratory or,occasionally, at work [81]. When these tests are carried out in a hospital laboratory, low doses ofthe occupational agent are used to avoid a nonspecific irritant effect. Dose response curves areconstructed in which the dose (concentration multiplied by duration) is progressively increasedand compared with lung function changes [82,83]. (See "Bronchoprovocation testing", section on'Antigen challenge'.)
In general, specific bronchoprovocation challenges are carried out if other tests are inconclusive,rather than being used for routine diagnosis [79,84]. For example, they can be performed inpatients with documented bronchial hyperresponsiveness when skin or immunoassay testing isnot available and results of serial peak expiratory flow or spirometry measurements are unclearabout whether asthma is occupationally induced.
In the case of high molecular weight agents, specific bronchoprovocation testing can be carriedout in a single day, because an immediate reaction that is maximal during the first hour followingexposure is expected. LMW agents often cause nonimmediate or late reactions and thereforerequire daily challenges of escalating doses of the agent on sequential days.
If airflow obstruction is not induced by inhalation of the specific agent, assessment of nonspecificbronchial responsiveness is carried out toward the end of the challenge day or at 24 hours afterinhalation. An increase in nonspecific bronchial responsiveness, sputum eosinophils, or exhalednitric oxide after specific antigen challenge supports the likelihood that the patient has OA ornonasthmatic eosinophilic bronchitis due to that agent. A negative specific bronchoprovocationchallenge in the laboratory may not exclude entirely the diagnosis of OA as the worker may havebecome “desensitized” or the wrong agent may have been used [84]. If possible, the workershould return to work and be reassessed if symptoms develop [81].
Specific inhalation challenges appear safe especially when the exposure to LMW agents is spreadover a few days with a short exposure on the first day (eg, one to four minutes), as recommended[85]. When the challenge to LMW agents was performed on a single day only, 3 percent of thepatients tested experienced a severe asthmatic reaction requiring repeated administration of ashort acting beta-2 agonist and oral or systemic glucocorticoids [86].
surveillance because of known exposure to an occupational sensitizer, an increase innonspecific bronchial responsiveness and sputum eosinophil numbers after antigen exposuremay precede the onset of asthmatic reactions and provide an early and sensitive marker of anabnormal airway response to inhalation of occupational agents [76,77]. (See 'Airwayinflammation' above.)

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 13/30
Imaging — A chest radiograph is often obtained in adults who present with new onset or work-related dyspnea to exclude causes of dyspnea and cough other than OA. The chest radiograph inOA may be normal or may show hyperinflation. High resolution computed tomography (HRCT) isusually not needed for the evaluation of a patient with suspected OA, unless an unexplainedabnormality is noted on the plain chest radiograph.
A possible exception is when a worker has known exposure to agents that cause both OA andhypersensitivity pneumonitis (eg, acid anhydrides, isocyanates). In that setting and when there issuspicion of hypersensitivity pneumonitis, an HRCT scan, combined with pulmonary functiontesting, may help in differentiating between these possibilities. (See 'Confirmation of asthma'below and "Hypersensitivity pneumonitis (extrinsic allergic alveolitis): Clinical manifestations anddiagnosis", section on 'High resolution CT scan' and "Imaging of occupational lung diseases".)
DIAGNOSIS
The diagnosis of OA is based upon a combination of exposure history (table 2), time course ofsymptom onset (eg, relative to start of a particular workplace exposure), evidence of reversibleairflow limitation, and specific testing that establishes an occupational contribution.
Confirmation of asthma — The first step in evaluating a patient with suspected OA is to confirmthat the patient indeed has asthma. The diagnosis of asthma based on history alone may not beaccurate, and therefore pulmonary function testing is warranted, starting with assessment ofspirometry pre and post bronchodilator. (See 'Pulmonary function tests' above and "Pulmonaryfunction testing in asthma" and "Diagnosis of asthma in adolescents and adults".)
Asthma is confirmed in one of the following ways:
Reversible airflow limitation demonstrated with spirometry pre and post bronchodilator. (See'Spirometry before and after bronchodilator' above.)
●
For patients with normal baseline spirometry, positive nonspecific bronchoprovocationchallenge confirms asthma. If the testing is negative in a symptomatic patient who hasongoing exposure in the workplace, OA is unlikely. However, if bronchoprovocation challengeis negative in a patient who is not working, it remains possible that nonspecific bronchialhyperresponsiveness has waned in the absence of exposure. If the patient is able to return towork, bronchoprovocation challenge should be repeated. (See 'Nonspecificbronchoprovocation challenge' above.)
●
Demonstration of variable airflow limitation by serial measurement of peak expiratory flow(PEF) or spirometry in and away from the workplace can be helpful but is less reliable for afirm diagnosis of asthma. (See 'Serial peak expiratory flow measurement' above and 'Serialspirometry at work' above.)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 14/30
Establishing occupational relationship — For those patients who have a clear diagnosis ofasthma, the next step is to establish that an occupational agent is causing the worker’s asthmaand, when possible, to identify the causative agent. Several tests are available to determinewhether a given patient's symptoms are due to OA and whether a particular occupationalexposure is the inciting agent [20]. Stepwise schemes have been proposed for the diagnosis ofOA using these various methods [87]. The exact order and combination of testing depends onwhether the patient still has workplace exposure or not and the availability of testing.
Patients who are working — For patients who continue to work or are able to return to theworkplace, serial testing of PEF during and away from workplace exposures is a standard andwidely available method for identifying OA. Skin testing and immunoassays to agents known tocause OA have limited availability, but should be performed if available. When positive in a patientwith known exposure to that agent and objective evidence of asthma, the likelihood of OA is high.However, a positive test is not diagnostic of OA, and a negative reaction does not exclude OA.Combining nonspecific bronchial responsiveness (NSBR) monitoring with serial PEF monitoring atand away from work improves the accuracy of the diagnosis.
Where available, combining monitoring of NSBR and induced sputum analysis with PEF canfurther increase the accuracy of testing. (See 'Serial peak expiratory flow measurement' aboveand 'Serial spirometry at work' above and 'Airway inflammation' above.)
Patients who are not working — A definitive diagnosis of OA can be more difficult to make inpatients who no longer have workplace exposure, because nonspecific bronchialhyperresponsiveness (NSBH) tends to wane the longer the person is away from the workplaceand serial lung function monitoring cannot be performed. The initial steps are to assess skintesting or immunoassays for potential causes of OA (where available) and confirm objectiveevidence of asthma based on spirometry pre and post bronchodilator or nonspecificbronchoprovocation challenge.
Confident diagnosis of OA – Decreases in PEF noted at work and significant reduction inNSBR away from work and an increase in eosinophils (>1 to 2 percent) at the end of the workday relative to a sample from the same time of day at home.
●
OA likely, but not definite – Work-related decreases in PEF without a work-related changein NSBR or increase in sputum eosinophils. If a definite diagnosis of OA is necessary in sucha patient, referral to a center that could perform specific inhalation challenge to the presumedculprit agent would be required. (See 'Specific inhalation challenge' above.)
●
OA unlikely – Absence of a work-related decrease in PEF, absence of NSBR changes at andoff work, and absence of an increase in sputum eosinophils. If strong clinical suspicion for OAremains, referral to a center that offers specific bronchoprovocation challenge can provide adefinitive result. (See 'Specific inhalation challenge' above.)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 15/30
DIFFERENTIAL DIAGNOSIS
A number of disease processes have symptoms that mimic OA, such as asthma due tononoccupational causes, chronic obstructive pulmonary disease (COPD), nonasthmaticeosinophilic bronchitis, work-related irritable larynx syndrome, upper respiratory tract irritation,hyperventilation syndrome, occupational rhinitis, hypersensitivity pneumonitis, and bronchiolitisobliterans. Certain distinguishing features can help to differentiate OA from the other diagnoses.The evaluation and diagnosis of asthma and occupational rhinitis are discussed separately. (See"Diagnosis of asthma in adolescents and adults" and "Occupational rhinitis" and "Diagnosis ofasthma in adolescents and adults", section on 'Differential diagnosis'.)
Likely diagnosis of OA – Positive skin test or immunoassay and objective evidence ofasthma. Resolution of asthma symptoms away from the workplace lends further support tothe diagnosis.
●
Sensitization without current evidence of OA – Positive skin test or immunoassay, butnormal spirometry and a negative bronchoprovocation challenge. As the person is no longerworking, NSBH may have resolved. If a definitive diagnosis is needed, specific inhalationchallenge, possibly followed by repeat nonspecific bronchoprovocation challenge, isindicated. (See 'Advanced testing' above.)
●
Confirmation of asthma, but diagnosis of OA unclear – Negative skin test orimmunoassay, but objective confirmation of asthma. Definitive diagnosis of OA would requirea positive specific bronchoprovocation challenge. In the absence of specific inhalationchallenge, a likely diagnosis of OA would depend on whether the history of asthma onset,exposure to a causative agent, and improvement away from the workplace strongly suggestOA. (See 'Advanced testing' above.)
●
OA unlikely – Skin test or immunoassay and nonspecific bronchoprovocation challenge arenegative. Any current symptoms would be unlikely due to OA. A small possibility remains thatthe patient’s workplace symptoms were due to OA, but the NSBH resolved after the personleft the workplace (if several weeks have elapsed). The only way to make a definitivediagnosis would be via specific bronchoprovocation challenge, possibly followed by repeatnonspecific bronchoprovocation challenge. (See 'Advanced testing' above.)
●
COPD – Workers can develop COPD due to personal or workplace exposure to tobaccosmoke or other pollutants. A careful history can elicit the intensity and duration of theseexposures. Spirometry will typically show a substantial component of irreversible airflowobstruction in patients with COPD. (See "Chronic obstructive pulmonary disease: Definition,clinical manifestations, diagnosis, and staging", section on 'Pulmonary function tests'.)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 16/30
SOCIETY GUIDELINE LINKS
Nonasthmatic eosinophilic bronchitis (NAEB) – NAEB due to occupational exposurediffers from OA by the absence of bronchial hyperresponsiveness and airflow obstruction.Sputum cell count analysis shows a significant increase in the percentage of eosinophilswhen the patient is exposed to the occupational agent to which they are sensitized, with asignificant decrease after removal from exposure. (See "Evaluation of subacute and chroniccough in adults", section on 'Nonasthmatic eosinophilic bronchitis'.)
●
Work-related irritable larynx syndrome – Work-related irritable larynx syndrome refers tohyperkinetic laryngeal symptoms triggered by sensory stimuli in the workplace, such as odorsand irritants [88]. This syndrome includes inducible laryngeal obstruction (ILO; also known asparadoxical vocal fold motion or vocal cord dysfunction), dysphonia due to laryngeal muscletension (also known as muscle tension dysphonia), globus (ie, sensation of tension in thethroat or neck), and chronic cough. In a case series, dysphonia was present in 86 percent andchronic cough in 76 percent [88]. ILO can mimic asthma and OA, and can also coexist withthese diagnoses [89]. Typically, the diagnosis of ILO is suspected when the patient hasstridorous sounds, loudest above the throat and less audible through the chest wall,dysphonia, and an abnormal inspiratory flow volume curve, and does not respond asexpected to treatment with an inhaled bronchodilator. Ascertaining the diagnosis requires thevisualization of paradoxical motion of the vocal cords during symptoms. (See "Paradoxicalvocal fold motion" and "Flow-volume loops", section on 'Variable extrathoracic obstruction'.)
●
Hyperventilation syndrome – Hyperventilation syndrome is frequently misdiagnosed asasthma [22,90]. It is characterized by a variety of somatic symptoms induced byphysiologically inappropriate hyperventilation and usually reproduced in whole or in part byvoluntary hyperventilation. (See "Hyperventilation syndrome".)
●
Hypersensitivity pneumonitis – A number of the same antigens that cause OA can alsocause hypersensitivity pneumonitis. Unlike OA, hypersensitivity pneumonitis is typicallyassociated with a restrictive ventilatory defect and interstitial opacities on radiographicimaging. (See "Hypersensitivity pneumonitis (extrinsic allergic alveolitis): Epidemiology,causes, and pathogenesis", section on 'Etiologic agents'.)
●
Bronchiolitis obliterans – Bronchiolitis obliterans presents with dyspnea and cough; airflowlimitation on spirometry, when present, is typically not reversible. Silo filler’s disease due toinhalation of high concentrations of nitrogen dioxide is a classic example of bronchiolitisobliterans. Bronchiolitis obliterans has also been reported in popcorn workers and as a raremanifestation in nylon flock workers [91,92]. (See "Bronchiolitis in adults", section on'Cessation of culprit drugs and exposures' and "Flock worker's lung".)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 17/30
Links to society and government-sponsored guidelines from selected countries and regionsaround the world are provided separately. (See "Society guideline links: Occupational asthma".)
SUMMARY AND RECOMMENDATIONS
Occupational asthma (OA) is characterized by variable airflow obstruction, airwayhyperresponsiveness, and airway inflammation attributable to a particular occupationalexposure and not due to stimuli encountered outside the workplace. (See 'Introduction'above.)
●
The typical symptoms of OA are the same as nonoccupational asthma and include cough,sputum production, dyspnea, wheeze, and chest tightness. Some patients report a pattern ofincreased symptoms while at work or within several hours of the completion of a shift andimprovement on weekends or during vacations, but this is variable. Some patients havesymptoms of work-related rhinoconjunctivitis that preceded or accompanied the onset of OA.(See 'Clinical features' above.)
●
The work history is an essential component of the evaluation of OA and should generallyinclude current and previous job titles, job descriptions, known exposures, and also anyexposures to unidentified vapors, gas, fumes, or dust (table 2 and table 1). However, the workhistory is insufficient on its own to confirm or exclude the diagnosis of OA. (See 'Occupationalhistory' above.)
●
In the case of high molecular weight agents, questions related to the presence of work-relatedwheezing and nasal symptoms are the best predictors of OA while loss of voice is a negativepredictor of OA. For low molecular weight agents, no specific question accurately predicts thepresence of OA. (See 'Occupational history' above.)
●
In general, the latency period from initiation of exposure to onset of symptoms (sensitization)is shorter with low molecular weight (LMW) agents, such as diisocyanates and plicatic acid(Western red cedar), than with high molecular weight (HMW) agents (table 2). In contrast, ona given workday, onset of symptoms occurs faster with HMW agents than LMW agents asimmediate reactions are more common with HMW agents. (See 'Occupational history' above.)
●
The evaluation of suspected OA generally requires a combination of tests to confirm asthmaand determine whether a particular occupational exposure is the inciting agent. Confirmationof asthma requires spirometry before and after bronchodilator to determine the presence,severity, and reversibility of any airflow limitation. The results of spirometry determine themost appropriate next test and are useful as a baseline for future assessments. (See'Diagnosis' above.)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 18/30
A stepwise testing approach based on whether the patient continues to work or not can beuseful to arrive at a diagnosis of OA. When available, skin test reactivity or immunoassay forspecific immunoglobulin E (IgE) can identify sensitization to known occupational sensitizers.(See 'Establishing occupational relationship' above and 'Skin and immunologic testing'above.)
●
In the absence of airflow limitation, a nonspecific bronchoprovocation challenge (eg,methacholine) is helpful to confirm or exclude current asthma. For patients who have ongoingwork exposure and are symptomatic, a negative bronchoprovocation challenge makes OAunlikely. (See 'Nonspecific bronchoprovocation challenge' above and 'Confirmation of asthma'above.)
●
For patients who meet objective criteria for asthma and continue to work, monitoring of peakexpiratory flow (PEF) and nonspecific bronchial responsiveness (if available) during and awayfrom workplace exposures is often useful to assess a workplace contribution. If this isnondiagnostic, measuring nonspecific bronchial responsiveness before and after workexposure can help identify an occupational contribution. (See 'Establishing occupationalrelationship' above and "Occupational asthma: Definitions, epidemiology, causes, and riskfactors", section on 'Low-molecular-weight'.)
●
When a patient is symptomatic during a period at work but has negative PEF monitoringdespite ongoing exposure to an agent known to cause OA (eg, Western red cedar,diisocyanates), the combined presence of normal spirometry, absence of bronchialhyperresponsiveness (ie, negative nonspecific bronchoprovocation challenge) and absence ofsignificant induced sputum eosinophilia, ideally assessed after a few days at work, virtuallyexcludes the possibility of OA. (See 'Variation in nonspecific bronchial responsiveness'above.)
●
For patients with adult-onset asthma and suspected OA, but uncertainty about theprovocative agent, specific bronchoprovocation testing may be helpful, but is only available inspecialized centers. (See 'Specific inhalation challenge' above and "Bronchoprovocationtesting", section on 'Antigen challenge'.)
●
Occupational nonasthmatic eosinophilic bronchitis is an infrequent cause of occupationalrespiratory symptoms without bronchial hyperresponsiveness and can be evaluated byassessing induced sputum for eosinophilia. (See 'Airway inflammation' above and 'Differentialdiagnosis' above.)
●
A number of disease processes can mimic OA, such as asthma due to non-occupationalcauses, chronic obstructive pulmonary disease (COPD), hyperventilation syndrome, upperrespiratory tract irritation, occupational rhinitis, hypersensitivity pneumonitis, and bronchiolitisobliterans. (See 'Differential diagnosis' above.)
●

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 19/30
ACKNOWLEDGMENT
The editorial staff at UpToDate would like to acknowledge Moira Chan-Yeung, MD and Jean-LucMalo, MD, who contributed to an earlier version of this topic review.
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Bernstein IL, Bernstein DI, Chan-Yeung M, Malo JL. Definition and classification of asthma inthe workplace. In: Asthma in the workplace, 4th, Malo JL, Chan-Yeung M, Bernstein DI (Eds), CRC Press, Boca Raton, FL 2013. p.1.
2. Quirce S, Sastre J. Occupational asthma: clinical phenotypes, biomarkers, andmanagement. Curr Opin Pulm Med 2019; 25:59.
3. Vandenplas O, Godet J, Hurdubaea L, et al. Are high- and low-molecular-weight sensitizingagents associated with different clinical phenotypes of occupational asthma? Allergy 2019;74:261.
4. Gautrin D, Ghezzo H, Infante-Rivard C, Malo JL. Natural history of sensitization, symptomsand occupational diseases in apprentices exposed to laboratory animals. Eur Respir J 2001;17:904.
5. Malo JL, Lemière C, Desjardins A, Cartier A. Prevalence and intensity of rhinoconjunctivitisin subjects with occupational asthma. Eur Respir J 1997; 10:1513.
6. Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: prevalence,aetiology and determinants. Clin Exp Allergy 2000; 30:1519.
7. Castano R, Gautrin D, Thériault G, et al. Occupational rhinitis in workers investigated foroccupational asthma. Thorax 2009; 64:50.
8. Vandenplas O, Ghezzo H, Munoz X, et al. What are the questionnaire items most useful inidentifying subjects with occupational asthma? Eur Respir J 2005; 26:1056.
9. Eifan AO, Derman O, Kanbur N, et al. Occupational asthma in apprentice adolescent carpainters. Pediatr Allergy Immunol 2005; 16:662.
10. Sastre J, Carnes J, García del Potro M, et al. Occupational asthma caused by triglycidylisocyanurate. Int Arch Occup Environ Health 2011; 84:547.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 20/30
11. Redlich CA. Skin exposure and asthma: is there a connection? Proc Am Thorac Soc 2010;7:134.
12. Bello D, Herrick CA, Smith TJ, et al. Skin exposure to isocyanates: reasons for concern.Environ Health Perspect 2007; 115:328.
13. Redlich CA, Herrick CA. Lung/skin connections in occupational lung disease. Curr OpinAllergy Clin Immunol 2008; 8:115.
14. Kusaka Y. [Asthma due to hard alloy dusts--a case of allergic bronchial asthma and contactdermatitis due to metallic cobalt]. Nihon Kyobu Shikkan Gakkai Zasshi 1983; 21:582.
15. Lynde CB, Obadia M, Liss GM, et al. Cutaneous and respiratory symptoms amongprofessional cleaners. Occup Med (Lond) 2009; 59:249.
16. Bousquet J, Flahault A, Vandenplas O, et al. Natural rubber latex allergy among health careworkers: a systematic review of the evidence. J Allergy Clin Immunol 2006; 118:447.
17. Arrandale VH, Liss GM, Tarlo SM, et al. Occupational contact allergens: are they alsoassociated with occupational asthma? Am J Ind Med 2012; 55:353.
18. Castano R, Trudeau C, Ghezzo H. Correlation between acoustic rhinometry and subjectivenasal patency during nasal challenge test in subjects with suspected occupational rhinitis; aprospective controlled study. Clin Otolaryngol 2010; 35:462.
19. Dykewicz MS. Occupational asthma: current concepts in pathogenesis, diagnosis, andmanagement. J Allergy Clin Immunol 2009; 123:519.
20. Tarlo SM, Balmes J, Balkissoon R, et al. Diagnosis and management of work-relatedasthma: American College Of Chest Physicians Consensus Statement. Chest 2008; 134:1S.
21. Le Moual N, Bakke P, Orlowski E, et al. Performance of population specific job exposurematrices (JEMs): European collaborative analyses on occupational risk factors for chronicobstructive pulmonary disease with job exposure matrices (ECOJEM). Occup Environ Med2000; 57:126.
22. Malo JL, Ghezzo H, L'Archevêque J, et al. Is the clinical history a satisfactory means ofdiagnosing occupational asthma? Am Rev Respir Dis 1991; 143:528.
23. Baur X, Huber H, Degens PO, et al. Relation between occupational asthma case history,bronchial methacholine challenge, and specific challenge test in patients with suspectedoccupational asthma. Am J Ind Med 1998; 33:114.
24. Vandenplas O, Binard-Van Cangh F, Brumagne A, et al. Occupational asthma insymptomatic workers exposed to natural rubber latex: evaluation of diagnostic procedures. J

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 21/30
Allergy Clin Immunol 2001; 107:542.
25. Quinlan PJ, Earnest G, Eisner MD, et al. Performance of self-reported occupationalexposure compared to a job-exposure matrix approach in asthma and chronic rhinitis. OccupEnviron Med 2009; 66:154.
26. Siracusa A, Folletti I, Gerth van Wijk R, et al. Occupational anaphylaxis--an EAACI taskforce consensus statement. Allergy 2015; 70:141.
27. Bernstein JA. Material safety data sheets: are they reliable in identifying human hazards? JAllergy Clin Immunol 2002; 110:35.
28. Wagner, GR, Henneberger, PK. Asthma exacerbated at work. In: Asthma in the workplace, 3rd ed, Bernstein, IL, Chan-Yeung, M, Malo, IL, Bernstein, DI (Eds), Taylor and Francis, NewYork 2006. p.631.
29. Lemière C, Boulet LP, Chaboillez S, et al. Work-exacerbated asthma and occupationalasthma: do they really differ? J Allergy Clin Immunol 2013; 131:704.
30. Malo JL. Future advances in work-related asthma and the impact on occupational health.Occup Med (Lond) 2005; 55:606.
31. Zock JP, Kogevinas M, Sunyer J, et al. Asthma characteristics in cleaning workers, workersin other risk jobs and office workers. Eur Respir J 2002; 20:679.
32. Malo JL, Ghezzo H, D'Aquino C, et al. Natural history of occupational asthma: relevance oftype of agent and other factors in the rate of development of symptoms in affected subjects.J Allergy Clin Immunol 1992; 90:937.
33. Slovak AJ, Hill RN. Does atopy have any predictive value for laboratory animal allergy? Acomparison of different concepts of atopy. Br J Ind Med 1987; 44:129.
34. van Kampen V, de Blay F, Folletti I, et al. EAACI position paper: skin prick testing in thediagnosis of occupational type I allergies. Allergy 2013; 68:580.
35. Lux H, Lenz K, Budnik LT, Baur X. Performance of specific immunoglobulin E tests fordiagnosing occupational asthma: a systematic review and meta-analysis. Occup EnvironMed 2019; 76:269.
36. Tarlo SM, Malo JL, de Blay F, et al. An Official American Thoracic Society Workshop Report:Presentations and Discussion of the Sixth Jack Pepys Workshop on Asthma in theWorkplace. Ann Am Thorac Soc 2017; 14:1361.
37. Vandenplas O, Froidure A, Meurer U, et al. The role of allergen components for thediagnosis of latex-induced occupational asthma. Allergy 2016; 71:840.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 22/30
38. Raulf M, Quirce S, Vandenplas O. Addressing Molecular Diagnosis of OccupationalAllergies. Curr Allergy Asthma Rep 2018; 18:6.
39. Redlich CA, Tarlo SM, Hankinson JL, et al. Official American Thoracic Society technicalstandards: spirometry in the occupational setting. Am J Respir Crit Care Med 2014; 189:983.
40. Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercisechallenge testing-1999. This official statement of the American Thoracic Society wasadopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 2000;161:309.
41. Burge PS, O'Brien IM, Harries MG. Peak flow rate records in the diagnosis of occupationalasthma due to isocyanates. Thorax 1979; 34:317.
42. Moscato G, Godnic-Cvar J, Maestrelli P. Statement on self-monitoring of peak expiratoryflows in the investigation of occupational asthma. Subcommittee on Occupational Allergy ofEuropean Academy of Allergy and Clinical Immunology. J Allergy Clin Immunol 1995;96:295.
43. Park D, Moore VC, Burge CB, et al. Serial PEF measurement is superior to cross-shiftchange in diagnosing occupational asthma. Eur Respir J 2009; 34:574.
44. Moore VC, Jaakkola MS, Burge CB, et al. Do long periods off work in peak expiratory flowmonitoring improve the sensitivity of occupational asthma diagnosis? Occup Environ Med2010; 67:562.
45. Reddel HK, Taylor DR, Bateman ED, et al. An official American Thoracic Society/EuropeanRespiratory Society statement: asthma control and exacerbations: standardizing endpointsfor clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180:59.
46. Gannon PF, Newton DT, Belcher J, et al. Development of OASYS-2: a system for theanalysis of serial measurement of peak expiratory flow in workers with suspectedoccupational asthma. Thorax 1996; 51:484.
47. Fishwick D, Barraclough R, Pickering T, et al. Comparison of various airflow measurementsin symptomatic textile workers. Occup Med (Lond) 2010; 60:631.
48. Townsend MC. ACOEM position statement. Spirometry in the occupational setting. AmericanCollege of Occupational and Environmental Medicine. J Occup Environ Med 2000; 42:228.
49. Leroyer C, Perfetti L, Trudeau C, et al. Comparison of serial monitoring of peak expiratoryflow and FEV1 in the diagnosis of occupational asthma. Am J Respir Crit Care Med 1998;158:827.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 23/30
50. Burge PS. Occupational asthma due to soft soldering fluxes containing colophony (rosin,pine resin). Eur J Respir Dis Suppl 1982; 123:65.
51. Bardy JD, Malo JL, Séguin P, et al. Occupational asthma and IgE sensitization in apharmaceutical company processing psyllium. Am Rev Respir Dis 1987; 135:1033.
52. Nicholson PJ, Cullinan P, Taylor AJ, et al. Evidence based guidelines for the prevention,identification, and management of occupational asthma. Occup Environ Med 2005; 62:290.
53. Malo JL. Utilization of pulmonary function measurements in the assessment of occupationalasthma. Curr Opin Allergy Clin Immunol 2002; 2:93.
54. Girard F, Chaboillez S, Cartier A, et al. An effective strategy for diagnosing occupationalasthma: use of induced sputum. Am J Respir Crit Care Med 2004; 170:845.
55. Anees W, Huggins V, Pavord ID, et al. Occupational asthma due to low molecular weightagents: eosinophilic and non-eosinophilic variants. Thorax 2002; 57:231.
56. Lemière C, Romeo P, Chaboillez S, et al. Airway inflammation and functional changes afterexposure to different concentrations of isocyanates. J Allergy Clin Immunol 2002; 110:641.
57. Racine G, Castano R, Cartier A, Lemiere C. Diagnostic Accuracy of Inflammatory Markersfor Diagnosing Occupational Asthma. J Allergy Clin Immunol Pract 2017; 5:1371.
58. Beretta C, Rifflart C, Evrard G, et al. Assessment of eosinophilic airway inflammation as acontribution to the diagnosis of occupational asthma. Allergy 2018; 73:206.
59. Lemière C. Advanced diagnostic studies: exhaled breath and sputum analyses. J OccupEnviron Med 2014; 56 Suppl 10:S45.
60. Quirce S. Eosinophilic bronchitis in the workplace. Curr Opin Allergy Clin Immunol 2004;4:87.
61. Lemière C, Efthimiadis A, Hargreave FE. Occupational eosinophilic bronchitis withoutasthma: an unknown occupational airway disease. J Allergy Clin Immunol 1997; 100:852.
62. Quirce S, Fernández-Nieto M, de Miguel J, Sastre J. Chronic cough due to latex-inducedeosinophilic bronchitis. J Allergy Clin Immunol 2001; 108:143.
63. Vandenplas O, D'Alpaos V, Heymans J, et al. Sputum eosinophilia: an early marker ofbronchial response to occupational agents. Allergy 2009; 64:754.
64. Obata H, Dittrick M, Chan H, Chan-Yeung M. Sputum eosinophils and exhaled nitric oxideduring late asthmatic reaction in patients with western red cedar asthma. Eur Respir J 1999;13:489.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 24/30
65. Lemière C, D'Alpaos V, Chaboillez S, et al. Investigation of occupational asthma: sputum cellcounts or exhaled nitric oxide? Chest 2010; 137:617.
66. Tossa P, Paris C, Zmirou-Navier D, et al. Increase in exhaled nitric oxide is associated withbronchial hyperresponsiveness among apprentices. Am J Respir Crit Care Med 2010;182:738.
67. Walters GI, Moore VC, McGrath EE, Burge S. Fractional exhaled nitric oxide in theinterpretation of specific inhalational challenge tests for occupational asthma. Lung 2014;192:119.
68. Engel J, van Kampen V, Lotz A, et al. An increase of fractional exhaled nitric oxide afterspecific inhalation challenge is highly predictive of occupational asthma. Int Arch OccupEnviron Health 2018; 91:799.
69. Piipari R, Piirilä P, Keskinen H, et al. Exhaled nitric oxide in specific challenge tests to assessoccupational asthma. Eur Respir J 2002; 20:1532.
70. Lemiere C, NGuyen S, Sava F, et al. Occupational asthma phenotypes identified byincreased fractional exhaled nitric oxide after exposure to causal agents. J Allergy ClinImmunol 2014; 134:1063.
71. Lemiere C, Miedinger D, Jacob V, et al. Comparison of methacholine and mannitol bronchialprovocation tests in workers with occupational asthma. J Allergy Clin Immunol 2012;129:555.
72. Dehaut P, Rachiele A, Martin RR, Malo JL. Histamine dose-response curves in asthma:reproducibility and sensitivity of different indices to assess response. Thorax 1983; 38:516.
73. Pralong JA, Lemière C, Rochat T, et al. Predictive value of nonspecific bronchialresponsiveness in occupational asthma. J Allergy Clin Immunol 2016; 137:412.
74. Mapp CE, Dal Vecchio L, Boschetto P, et al. Toluene diisocyanate-induced asthma withoutairway hyperresponsiveness. Eur J Respir Dis 1986; 68:89.
75. Sastre J, Fernández-Nieto M, Novalbos A, et al. Need for monitoring nonspecific bronchialhyperresponsiveness before and after isocyanate inhalation challenge. Chest 2003;123:1276.
76. Vandenplas O, Delwiche JP, Jamart J, Van de Weyer R. Increase in non-specific bronchialhyperresponsiveness as an early marker of bronchial response to occupational agentsduring specific inhalation challenges. Thorax 1996; 51:472.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 25/30
77. Lemière C, Chaboillez S, Malo JL, Cartier A. Changes in sputum cell counts after exposureto occupational agents: what do they mean? J Allergy Clin Immunol 2001; 107:1063.
78. American Thoracic Society. Selected specialized clinical tests in environmental, occupational, and population health. http://www.thoracic.org/professionals/clinical-resources/environmental-and-occupational/clinical-tests.php (Accessed on August 03, 2017).
79. Suojalehto H, Cullinan P, European Respiratory Society Task Force on Specific InhalationChallenges with Occupational Agents. Specific inhalation challenge tests for occupationalasthma in Europe: a survey. Eur Respir Rev 2014; 23:266.
80. American Thoracic Society. Selected Specialized Clinical Tests In EOH Evaluation. http://www.thoracic.org/professionals/clinical-resources/environmental-and-occupational/clinical-tests.php (Accessed on January 29, 2019).
81. Rioux JP, Malo JL, L'Archevêque J, et al. Workplace-specific challenges as a contribution tothe diagnosis of occupational asthma. Eur Respir J 2008; 32:997.
82. Vandenplas O, Malo JL. Inhalation challenges with agents causing occupational asthma. EurRespir J 1997; 10:2612.
83. Vandenplas O, Suojalehto H, Aasen TB, et al. Specific inhalation challenge in the diagnosisof occupational asthma: consensus statement. Eur Respir J 2014; 43:1573.
84. Tarlo SM. The role and interpretation of specific inhalation challenges in the diagnosis ofoccupational asthma. Can Respir J 2015; 22:322.
85. Vandenplas O, Burge PS, Moscato G, Malo JL. Functional assessment. In: Asthma in the workplace, 4th ed, Malo JL, Chan-Yeung M, Bernstein DI (Eds), CRC Press, Boca Raton, FL 2012. p.113-132.
86. Vandenplas O, D'Alpaos V, Evrard G, Jamart J. Incidence of severe asthmatic reactions afterchallenge exposure to occupational agents. Chest 2013; 143:1261.
87. Tarlo SM, Lemiere C. Occupational asthma. N Engl J Med 2014; 370:640.
88. Hoy RF, Ribeiro M, Anderson J, Tarlo SM. Work-associated irritable larynx syndrome. OccupMed (Lond) 2010; 60:546.
89. Tonini S, Dellabianca A, Costa C, et al. Irritant vocal cord dysfunction and occupationalbronchial asthma: differential diagnosis in a health care worker. Int J Occup Med EnvironHealth 2009; 22:401.
90. Thomas M, McKinley RK, Freeman E, Foy C. Prevalence of dysfunctional breathing inpatients treated for asthma in primary care: cross sectional survey. BMJ 2001; 322:1098.

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 26/30
91. van Rooy FG, Rooyackers JM, Prokop M, et al. Bronchiolitis obliterans syndrome inchemical workers producing diacetyl for food flavorings. Am J Respir Crit Care Med 2007;176:498.
92. King TE Jr. Miscellaneous causes of bronchiolitis: inhalational, infectious, drug-induced, andidiopathic. Semin Respir Crit Care Med 2003; 24:567.
Topic 550 Version 18.0

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 27/30
GRAPHICS
Helpful clues in the evaluation of occupational asthma
Does the patient have any of the following pulmonary or extrapulmonary symptoms:Dyspnea, cough, chest tightness, wheeze, sputum that began or worsened after workplace exposureRhinitis or conjunctivitis that is worse at work; may have preceded or may be contemporaneous with asthmaRash associated with work exposure
Did symptoms develop after starting new employment or with new exposure?
Is the patient exposed to vapors, gas, fumes, or dust at work?
Does the patient feel better when away from work (evenings, weekends, or vacation)?
Do other people at work have similar symptoms or have people left work because of symptoms?
Does the patient work in any of the following settings or occupations*:BakeryCleaningDental work; health careDock work; coffee, food, fish, or tobacco processing; detergent manufacturingGreenhouse work
Jewelry workHairdressingLaboratory animals; veterinary work; farmingPharmaceutical manufacturing or processingPlastics, lacquer, or epoxy manufacturing; roofing; spray paintingWelding; metal or chemical work
Wood working; carpentry
* The list of workplace exposures associated with occupational asthma is much longer; the settings listed are just asampling. Refer to UpToDate content on causes of occupational asthma.
Graphic 122138 Version 1.0

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 28/30
Major causes of occupational asthma and rhinitis
Occupation at risk
Low molecular weight chemicals
Isocyanates (eg, toluene diisocyanate, diphenylmethanediisocyanate, hexamethylene diisocyanate, naphthalenediisocyanate)
Polyurethane workers, roofers, insulators,painters
Anhydrides (eg, trimellitic anhydride, phthalic anhydride) Manufacturers of paint, plastics, epoxy resins
Metals (eg, chromic acid, potassium dichromate, nickel sulfate,vanadium, platinum salts)
Platers, welders, metal and chemical workers
Drugs (eg, beta-lactam agents, opiates, other) Pharmaceutical workers, farm workers, healthprofessionals
Wood dust (eg, Western red cedar, maple, oak, exotic woods) Carpenters, woodworkers
Dyes and bleaches (eg, anthraquinone, carmine, henna extract,persulfate, reactive dyes)
Fabric and fur dyers, hairdressers
Amines (eg, chloramine, quaternary amines) Chemists, cleaners, plastic manufacturers
Glues and resins (eg, acrylates, epoxy) Plastic manufacturers
Miscellaneous (eg, formaldehyde, glutaraldehyde, ethyleneoxide, pyrethrin, polyvinyl chloride vapor)
Laboratory workers, textile workers, paintsprayers, health professionals
High molecular weight organic materials
Animal proteins (eg, domestic and laboratory animals, fish andseafood)
Farmers, veterinarians, poultry processors,fish and seafood processors
Flours and cereals Bakers, food processors, dock workers
Enzymes (eg, pancreatic extracts, papain, trypsin, Bacillussubtilis, bromelain, pectinase, amylase, lipase)
Bakers, food processors, pharmaceuticalworkers, plastic workers, detergentmanufacturers
Plant proteins (eg, wheat, grain dust, coffee beans, tobaccodust, cotton, tea, latex, psyllium, various flours)
Bakers, farmers, food and plant processors,health professionals, textile workers
Graphic 66185 Version 6.0

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 29/30
Natural history of occupational asthma with a latency period
Graphic 80111 Version 3.0

12/09/2019 Occupational asthma: Clinical features, evaluation, and diagnosis - UpToDate
https://www.uptodate.com/contents/occupational-asthma-clinical-features-evaluation-and-diagnosis/print?search=ASMA OCUPACIONAL&sour… 30/30
Contributor Disclosures
Catherine Lemière, MD Nothing to disclose André Cartier, MD Speaker’s Bureau: Merck Frosst Canada;Boehringer-Ingelheim Canada; IC-EBM Canada [Asthma]; GSK Canada [Asthma (Mepolizumab,Fluticasone/vilanterol, Umeclidinium, Umeclidinium/vilanterol)]. Consultant/Advisory Boards: AZ Canada;Teva Canada; GSK Canada [Asthma (Mepolizumab, Fluticasone/vilanterol, Umeclidinium,Umeclidinium/vilanterol)]; Sanofi Genzyme Canada [Asthma (Benralizumab, reslizumab, mepolizumab,dupilumab)]. Louis-Philippe Boulet, MD Grant/Research/Clinical Trial Support: AstraZeneca [Asthma(Benralizumab)]; GlaxoSmithKline [Asthma (FF/UMEC/VI, GSK3772847)]; Novartis [Asthma (CSJ117)];Sanofi [Asthma (Dupilumab)]; Boston Scientific [Asthma (Bronchial Thermoplasty)]; Hoffman La Roche[Asthma]; Takeda [Asthma]; Boehringer Ingelheim [Asthma (Bi-671800 ED)]. Speaker’s Bureau: AstraZeneca[Asthma (Benralizumab)]; GlaxoSmithKline [Asthma (FF/UMEC/VI)]. Consultant/Advisory Boards:AstraZeneca [Asthma (Benralizumab)]; Novartis [Asthma (CSJ117)]. David I Bernstein,MD Grant/Research/Clinical Trial Support: Glaxo; Astra Zeneca; Pearl; Novartis; Genentech; Glenmark;Gossamer; Leo; Merck; Nerre; Aimmune [Clinical trials of asthma therapies, new COPD drugs, new forms ofimmunotherapy, biologics for treatment of asthma or hives]. Consultant/Advisory Boards: Glaxo [Anti-IL5 forasthma]; ALK America [Sublingual immunotherapy]; Gerson-Lehman; Guidepoint Global. Peter J Barnes,DM, DSc, FRCP, FRS Grant/Research/Clinical Trial Support: AstraZeneca [Asthma, COPD (Symbicort)];Novartis [COPD (Indacaterol)]; Boehringer [COPD (Tiotropium, olodaterol)]; Chiesi [Asthma, COPD (Foster)].Speaker's Bureau: AstraZeneca [Asthma (Symbicort)]; Novartis [COPD (Indacaterol, glucopyrolate, Ultibro)];Boehringer [COPD (Tiotropium, olodaterol)]; Chiesi [Asthma (Foster)]. Consultant/Advisory Board:AstraZeneca [Asthma, COPD]; Novartis [COPD]; Boehringer [COPD]; Teva [COPD]; Pieris [Asthma]. HelenHollingsworth, MD Nothing to disclose
Contributor disclosures are reviewed for conflicts of interest by the editorial group. When found, these areaddressed by vetting through a multi-level review process, and through requirements for references to beprovided to support the content. Appropriately referenced content is required of all authors and must conformto UpToDate standards of evidence.
Conflict of interest policy