Diabetic Foot
-
Upload
rashed-shatnawi -
Category
Documents
-
view
8 -
download
1
description
Transcript of Diabetic Foot

Diabetic Foot
Done by
Saed Jarrar
Supervised by
Doctor Hussein al Heis

Introduction
Diabetes is a chronic condition that can cause a number of serious complications. Problems with the feet are one of the most common.
Diabetic foot if the foot of a diabetic patient that has the potential risk of a pathologic consequences including infection, ulceration, and/or destruction of deep tissues associated with neurologic abnormalities, various degrees of peripheral vascular disease and/or metabolic complications of diabetes in the lower limbs.
Lifetime risk of diabetic patient developing foot ulcer is 25%.

Diabetic foot ulceration is the commonest major complication of DM.
Foot ulcerations is most common cause of hospital admissions for diabetics.
The incidence of major amputation is between 0.5 and 5.0 per 1000 people with Diabetes.
Diabetes is the leading cause of non-traumatic amputations.
3

4 Risk Factors
Previous foot ulcers
Prior lower extremity amputation
History of stroke
History of peripheral vascular disease (claudication)
Old age- above 60
Male
Obesity
Low socioeconomic class
Long duration of diabetes (more than 10 years)
Uncontrolled blood glucose
Other complication (nephropathy, retinopathy, neuropathy)

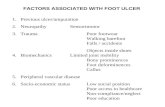
Diabetic foot problems are caused by a number of factors that comprise the pathogenesis of the disease: Neuropathy Peripheral vascular disease Trauma( sensory and motor) Infection(autonomic) Poor glycemic control Improper footwear Others: old age, smoking,
low socioeconomic status, psychological factors
5

1)Diabetic Neuropathy >50% of patients aged 60 years and above
Increases the risk of foot ulceration by 7-fold
Can affect the sensory, motor and autonomic functions
Its importance lie in the fact that it goes unnoticed by the patient, thus emphasizing the importance of regular assessment of the feet of the diabetic patient.
6

Four causes thought to be involved in neuropathy:
Microvascular disease: The first pathological change in the microvasculature is vasoconstriction, the capillary basement membrane thickening and endothelial hyperplasia, which contribute to diminished oxygen tension and hypoxia .
Advanced glycation end products (AGE): The nonenzymatic reaction of excess glucose with proteins, nucleotides, and lipids results in advance glycation end products that may have a role in disrupting neuronal integrity and repair mechanisms through interference with nerve cell metabolism and axonal transport.
Polyol pathway: Hyperglycemia causes increased levels of intracellular glucose in nerves, leading to saturation of the normal glycolytic pathway. Extra glucose is shunted into the polyol pathway and converted to sorbitol and fructose lead to abnormal action potential propagation.
Protein kinase C: PKC is implicated in the pathology of diabetic neuropathy. Increased levels of glucose cause an increase in intracellular diacylglycerol , which activates PKC.
7

8
Types of neuropathy
Motor: muscle atrophy, foot
deformity, altered foot biomechanics,
redistribution of foot pressure, which
causes the ulcers
Sensory: deaf and blind to stimuli No pain no discomfort
noticed
Autonomic: - loss of sweating dry skin cracks
and fissures- Altered regulation of cutaneous blood
flow

Sensory neuropathy
Loss of protective sensation.
Starts distally and migrates proximally causing an increase in the distribution of numbness, sensory loss, and night time pain, Pain is burning/tingling in nature ‘’earliest’’.
Pins and needles sensation is common.
Loss of proprioception is affected early.
Neuropathic ulcers starts from the combination of both sensory neuropathy and trauma. Trauma could be defined as ill-fitting footwear, walking barefoot, scalding from hot water, or hitting a foreign object, but the daily levels of physical activity does not by itself predispose to causing a foot ulcer. Remember that it goes unnoticed. Motor neuropathy with redistribution of foot pressure areas also plays a role.
9

10

Motor neuropathy
Affect intrinsic muscles of the foot intrinsic muscle wasting and altered foot biomechanics with the redistribution of foot pressure areas ( the normal being the heel, the base of 1st and 5th metatarsals and the toe)
All of that causes foot deformities. Foot deformities: hammer toes, claw toes, prominent
metatarsal heads, and hallux valgus
11

Hammer toes are generally caused by a tendon imbalance in the toes and tight muscles in the feet.12

Autonomic Neuropathy Regulates sweating and perfusion to the limb.
Loss of autonomic control inhibits thermoregulatory function and sweating.
Result is dry, scaly and stiff skin that is prone to cracking and allows a portal of entry for bacteria>> infection
13

Charcot's joint (neuroarthropathy)
Neuropathic arthropathy (or neuropathic osteoarthropathy), also known as Charcot joint (often "Charcot foot"), refers to progressive degeneration of a weight bearing joint, a process marked by bony destruction, bone resorption, and eventual deformity.
If this pathological process continues unchecked, it can result in joint deformity, ulceration and/or superinfection, loss of function, and in the worst-case scenario, amputation or death.
Its pathogenesis is simply Any condition resulting in decreased peripheral sensation, proprioception, and fine motor control and in our case the cause is diabetic neuropathy.
14

15 Charcot's joint (neuroarthropathy)
Two primary theories have been advanced:
Neurotrauma: Loss of peripheral sensation and proprioception leads to repetitive microtrauma to the joint in question; this damage goes unnoticed by the neuropathic patient, and the resultant inflammatory resorption of traumatized bone renders that region weak and susceptible to further trauma. In addition, poor fine motor control generates unnatural pressure on certain joints, leading to additional microtrauma.
Neurovascular: Neuropathic patients have dysregulated autonomic nervous system reflexes, and de-sensitized joints receive significantly greater blood flow. The resulting hyperemia leads to increased osteoclastic resorption of bone, and this, in concert with mechanical stress, leads to bony destruction.

16 Charcot's joint (neuroarthropathy)
The clinical presentation depending on the severity of the disease is mild to severe swelling associated with a deformity. On examination you will find edema, erythema and increased temperature(infrared thermometer) of the affected joint +/- Pain and ulcer. Notice that in the presentation of acute charcot’s joint the skin is intact and the loss of the protective sensation is pathognomonic.
X-ray findings include osteolysis of the Distal metatarsals, fractures and joint dislocation.
Always have a high index of suspicion because it could be misdiagnosed as osteomyelitis, Cellulitis and DVT.

17

18
Osteolysis of the distal metatarsals and phalanges With licked candy stick appearance.

2)Peripheral vascular disease
It is due to:
Microvascular disease: the small blood vessels are usually the first to be affected by diabetes and the result of progressive thickening in the BM, endothelial hyperplasia ( retinopathy, nephropathy or neuropathy) , this usually ends with nerve hypoxia and low perfusion to the skin.
Macro vascular disease (atherosclerosis): in the calf (tibial & peroneal arteries) with relative sparing of proximal vessels and those in the foot .They may develop intermittent claudication, but often this seems to be absent and the patient presents with ischemic foot ulceration.
19

Typical vascular ulcer is:
Painful.
not surrounded by callus.
associated with absent or poor foot pulses.
associated with a foot that is cold to touch.
at the edge of the foot or toes.
20
Typical neuropathic ulcer is:
• Painless• Surrounded by callus• Associated with good
foot pulses (because the circulation is normal) .
• At the pressure area .

A vascular ulcer should not be confused with a venous ulcer which is due to varicose veins.
Venous ulcers are:
situated on the leg (rather than in the foot)
associated with varicose veins and often accompanied by swelling and a brownish discoloration of the leg
21

The result is:
Gangrene: necrosis of tissue associated with ischemia (dry gangrene) or infection (wet gangrene).
Dead tissue( brown/ dark blue/ black)
Not painful.
22

Infections Infections in diabetic patients are not only more
common but more severe than those non diabetic pateints .
Polymicrobial in nature (staph, strep, proteus, pseudomonas, anaerobes, such as bacteriod.)
The main predisposing factors leading to diabetic foot infection are:-
1) neuropathy- ‘’autonomic, dry feet’’
2) impaired immunological response (macrophages)
3) peripheral vascular disease
23

Type of infections :-
1. Superficial infections
2. Deep infections
24Infection causes increased metabolic and oxygen demands of tissues and inability to meet with this demand will increase tissue damage and necrosis.

25

26


28
Approach to Diabetic foot History:
The patient should be questioned about leg discomfort. If present, further questions should be asked that allow a quantitative assessment of symptoms:
What is the sensation felt? – Burning, numbness, or tingling (2 points); fatigue, cramping, or aching (1 point). Maximum is 2 points.
What is the location of symptoms? – Feet (2 points); calves (1 point); elsewhere (no points). Maximum is 2 points.
Have the symptoms ever awoken you at night? – Yes (1 point).
What is the timing of symptoms? – Worse at night (2 points); present day and night (1 point); present only during the day (no points). Maximum is 2 points.
How are symptoms relieved? – Walking around (2 points); standing (1 point); sitting or lying or no relief (no points). Maximum is 2 points.
The total symptom score can then be determined:

29 Approach to Diabetic foot
History: The total symptom score can then be
determined:0 to 2 – Normal
3 to 4 – Mild
5 to 6 – Moderate
7 to 9 – Severe
DON’T FORGET TO ASK ABOUT RIFK FACTORS

30 Approach to Diabetic foot
Assessment of the diabetic foot:
1) Neuropathic assessment.
2) vascular assessment.
3) Ulcer assessment.

31 1) Neuropathic assessment
Motor: Look for any foot deformity present, claw or hammer toes, Charcot's-edema , flat foot. Also muscle wasting, loss of hair. Look for ulcers and don’t forget between the toes ( tight wearing).
Autonomic: look for dry skin, cracked skin, check the temperature ‘’ Increases due to A-V shunting of the blood and decreased tissue perfusion’’ and subsequent distended veins.
Sensory, you must check vibration sensation, pressure sensation, superficial pain ’’pin-prick’’ and temperature sensation.
Assess the skin colour association, red means inflammation, black means gangrene.

32 2) Vascular assessment
The feet should be examined for signs of peripheral artery disease such as diminished foot pulses, decrease in skin temperature, thin skin, lack of skin hair, and bluish skin color.
More useful quantitative clinical tests include measurement of venous filling time, Doppler examination of lower limb pulses, and leg blood pressure measurements (eg, ankle brachial index [ABI], Transcutaneous oxygen tension and angiography.

1-Ankle brachial index:
» When below 0.9 this is indicative of ischemia.
» Maybe falsely elevated due to medial calcification of vessel walls, a phenomenon seen in diabetic neuropathy, may also cause absent pulses in palpation.
Vascular assessment:

34
1- Capillary refill and Pulses:
Femoral Artery : Mid-Inguinal point
Dorsalis Pedis Artery : Felt lateral to the tendon of extensor hallucis longus and against the navicular bone.
Post. Tibial Artery : lies one-third of the way along a line between the tip of the medial malleolus and the point of the heel.
Popliteal Artery : the most convenient Technique is to extend the patients knee, put both hands around the top of the calf with the thumbs on the tibial tuberosity with the tips of the hand behind the knee over the lower part of the popliteal fossa, push against the tibial condyle to trap the artery.

35
2- Buerger’s angle : elevate both legs to an angle of 45 degrees and hold for one to two minutes. Observe the color of the feet. Pallor indicates ischaemia. It occurs when the peripheral arterial pressure is inadequate to overcome the effects of gravity. The poorer the arterial supply, the less the angle to which the legs have to be raised for them to become pale.
normal still pink even in 90 degree
<20 degree indicates severe ischemia

3-Doppler waveform:
» Loss of the normal triphasic waveform indicates vascular disease.
4-Transcutaneous oxygen tension:
» Measured by an electrode placed on the foot.
» Accurately reflects skin oxygenation.
» Can be used to determined the severity of ischemia, the likelihood that an ulcer will heal, and an appropriate level for amputation.

5- angiography: The gold standard for both
diagnosis and planning of treatment.
37

38 3) Ulcer assessment
Site, size and shape of ulcer.
Base and floor of the ulcer: Look for granulation tissue, any bones of tendons showing, nature of the floor if its solid brown/grey dead tissue or other.
Edge of the ulcer, sloping healing ulcer or punched out, rolled, everted, undermined
Depth of the ulcer and the structures it penetrated.
Discharge, any pus or foul odor or friable tissue noticed.
Relation to adjacent structures.
State of local tissue’s blood supply and innervation.

Skin color:
-red color (inflammation).
- Blue color (ischemia). - Black color (gangrene).
Muscle wasting. dryness of the skin . Hair (Hair loss over the foot due to ischemia ). Look for nail thickening. between the toes. See if there is any deformity.
1-hammer toes.2-hallux valgus.3-charcot‘s joints.
Edema . any amputation .
Examination of the Lower Limb
Inspection:

Buerger’s angle : elevate both legs to an angle of 45 degrees and hold for one to two minutes. Observe the color of the feet. Pallor indicates ischaemia. It occurs when the peripheral arterial pressure is inadequate to overcome the effects of gravity. The poorer the arterial supply, the less the angle to which the legs have to be raised for them to become pale.
-normal still pink even in 90 degree
-<20 degree indicates severe ischemia
** If there is an ulcer describe its : Site. Size. Shape. Surface. Discharge. Skin over it (color and texture). Inspect the floor. Describe the edges: sloped , punched , rolled…etc

tenderness. temperature. Capillary refill.. Edema. pulses.(femoral/dorsalis pedis/ posterior tibial/ popliteal) Palpate the base of the ulcer. Do local neurological examination for:
-light touch.
-superficial and deep pain.
-vibration sensation.
-position sense .
palpation:

General:
-CBC
-KFT -urine analysis - lipid profile
-fasting blood glucose + HbA1c -ECG -ESR
infection: -culture and sensitivity.
-x-ray of limb (gas gangrene - deformity –foreign body). - technetium bone scan. (osteomylitis)
-MRI.
Neurological: -nerve conduction test .
Investigations:

Cumulative Risk Category This enables the physician to
1. design a treatment plan
2. determine whether the patient is at risk for ulceration or amputation


Management of Diabetic Foot

Effective management of diabetic foot disorders requires knowledge of the potential pathologies, the associated classification systems, and the principle tenets of intervention.
Ulceration, infection, and Charcot arthropathy are the most significant of these pathologies and classification systems have been developed for each entity.

Classification of diabetic foot based o the natural history of the disease. It is tailored towards the management of specific problems that might occur along the course of the disease.
It classifies the DF into categories (0, 1, 2, 3, 4, 5 ,6)
Category 0 (no pathology) :
Patient is diagnosed with DM.
Protective sensation is intact
ABI > 0.8 and toe systolic BP > 45 mmHg.
No Hx of ulceration.
Treatment :
Patient Education (patient’s foot care)
2-3 visits per year to asses the neurovascular status, Dermal Thermometry & foci of Stress ( heads of 1st and 5th metatarsal bones , heel, lateral aspect of the foot) & shoe accomodation

Category 1 (Neuropathy without deformity, Insensate Foot):
Protective sensation is absent (especially light touch)
ABI > 0.8 and toe systolic BP > 45 mmHg.
No ulceration.
No deformity.
Treatment :
same as category 0, therapeutic footwear & evaluation every 3 months

Category 2(Neuropathy with deformity):
Protective sensation is absent.
ABI > 0.8 and toe systolic BP > 45 mmHg (still intact).
No ulceration.
Foot deformity is present. (focus of stress – head of 1st metatarsal is the most common)
Treatment :
same as category 1 plus :
*Pedorthic consultation
*prophylactic surgery to alleviate the foci of stress.

Category 3 : History of pathology Protective sensation is absent.
ABI > 0.8 and toe systolic BP > 45 mmHg (still intact).
History of Neuropathic ulceration.
History of Charcot’s joint .
Foot deformity is present.
Treatment :
same as category 2 plus:
pedorthic / Ortho consultation for possible custom molded shoes accommodation
Possible prophylactic surgery to alleviate foot deformity.
more frequent visits for monitoring.

Category 4A : Neuropathic Ulceration Protective sensation is absent.
ABI > 0.80 & toe systolic >45 mmHg
Non-Infected Neuropathic Ulceration
No Acute Charcot’s joint present.
Treatment :
Pressure reduction program
Wound care program instituted

Category 4B: Acute Charcot’s Joint
Protective sensation not present.
ABI > 0.8 and toe systolic BP > 45 mmHg .
Non-infected Neuropathic ulceration may be present
Acute Charcot’s Joint
Treatment :
Same as Category 4A if ulcer is present
Pressure Reduction program instituted
Thermometric and radiographic monitoring.

Category 5: Infected Diabetic Foot
Protective sensation may be absent
Infected wound present
Charcot’s may be present
Treatment:
Same as category 4
Debride Infected necrotic tissue
Possible Hospitalization
Antibiotic Therapy (IV Antibiotics)
Contact Casting generally contraindicated until diabetic foot category drops to 4.
53

Category 6: Dysvascular Foot
ABI < 0.8 and toe systolic BP < 45 mmHg, or Pedal transcutaneous O2 tension of < 40 mmHg
Ulceration may be present
Protective Sensation may not be present
Treatment:
Vascular Consult, Possible Revascularization
If infection present, treat as category 5
Contact Casting generally Contraindicated
54

Diabetic Foot Ulcers
1Ihab Abu Al-Hamam


Wagner ulcer classification system.. depends on:
the depth of the wound extent of tissue necrosis

Wagner classification

Examples of different grades





Management of Diabetic Foot Ulcers
1. Management of comorbidities
2. Evaluation of vascular status
3. Assessment of lifestyle
4. Ulcer assessment
5. Ulcer treatment
6. Mechanical off-loading

Evaluation of vascular status

Ulcer assessment
History (Duration – first symptom – other symptoms
– progression – persistence – multiplicity)
Examination (Site – size – shape – base – edge –
depth – discharge – relations – local tissue)


Ulcer treatment
A. Debridement
B. Infection control
C. Local wound care

A. Debridement
Debridement of necrotic tissue is important for ulcer healing
Removal of areas of extensive tissue necrosis
Methods:
(sharp, enzymatic, autolytic, mechanical, and biological)

B. Infection control
The diagnosis of infection is clinical
Cultures of the ulcer base are taken after debridement and prior
to initiation of empiric antibiotic therapy

c. Local wound care
After debridement, ulcers should be kept clean and moist but free of excess fluids
Therapeutic growth factors
Gene therapy
Tissue-engineered constructs
Stem cell therapy
Advanced Wound Care Modalities

Mechanical off-loading
Reduces or eliminates pressure in the region of the ulcer, which is important for healing
1- Total contact cast
2- Cast walkers
3- Therapeutic shoes
4- Knee walkers

Diabetic Foot Infections
2

Diabetic foot infections are associated with
substantial morbidity and mortality
Risk factors: neuropathy, peripheral vascular disease, & poor
glycemic control.
non-limb-threatening VS. limb-threatening
infections

Microbiology
Most diabetic foot infections are polymicrobial, with up to five to seven different specific organisms often involved:
● Superficial diabetic foot infections (including cellulitis and infected ulcers) are likely due to aerobic gram-positive cocci (including S. aureus, S. agalactiae, S. pyogenes, and coagulase-negative staphylococci).
● Ulcers that are deep, chronically infected, and/or previously treated with antibiotics are more likely to be polymicrobial. Such wounds may involve the above organisms in addition to enterococci, Enterobacteriaceae, P.aeruginosa, and anaerobes.
● Wounds with extensive local inflammation, necrosis, malodorous drainage, or gangrene with signs of systemic toxicity should be presumed to have anaerobic organisms in addition to the above pathogens. Potential pathogens include anaerobic streptococci, Bacteroides species, and Clostridium species

Suspect osteomyelitis
In ulcers over bony prominences that do not heal after several weeks of wound care and off-loading.
● Grossly visible bone or ability to probe to bone
● Ulcer size larger than 2 cm2
● Ulcer duration longer than one to two weeks
● Erythrocyte sedimentation rate (ESR) >70 mm/h


Non-limb-threatening infections

Limb-threatening infection

Management
wound management antimicrobial therapy glycemic control fluid and electrolyte balance Surgery



Charcot Arthropathy
3

Modified Eichenholtz System
Stage 0: Early or inflammatory – There is localized swelling, erythema, and warmth with little or no radiological abnormalities.
Stage 1: Development – Swelling, redness, and warmth persist, and bony changes such as fracture, subluxation dislocation, and bony debris start to appear radiologically.
Stage 2: Coalescence – The clinical inflammatory signs decrease, and radiological signs of fracture healing, bony debris resorption, and new bone formation occur.
Stage 3: Remodelling – The redness, warmth, and swelling has settled, and bony deformity which may be stable or unstable is present. Radiographic appearances may show mature fracture callus and decreased sclerosis.

General rules in Management
Acute therapy: avoidance of weight bearing on the affected joint should be recommended until resolution of the edema and erythema occurs
In patients who present later in disease, joint disorganization is often severe and irreversible. Disease of the hindfoot and ankle appears to have a worse prognosis than disease of the midfoot
Goal of treatment in these patients is to maintain a stable plantigrade foot that is free of ulceration and infection
Surgical correction is best avoided in most patients. However, in carefully selected cases, surgery can give acceptable alignment.
Common deformities seen are the “rocker bottom foot” caused by collapse of the medial arch.

Surgical Treatment of Diabetic Foot
Class I: Elective foot surgery (performed to treat a painful deformity in a patient without loss of protective sensation)
Class II: Prophylactic foot surgery (performed to reduce risk of ulceration or re-ulceration in patients with loss of protective sensation but without open wound)
Class III: Curative foot surgery (performed to assist in healing an open wound)
Class IV: Emergent foot surgery (performed to arrest or limit progression of acute infection)
For any of these classes, the presence of critical ischemia should prompt a vascular surgical evaluation to consider the urgency of the procedure and possible revascularization prior to or subsequent to the procedure.

Amputation

Indications for Amputation
Chronic neuropathic ulcer (the most common)
Severe infections with extensive soft tissue or bony destruction, or
osteomyelitis
Removal of portions of the foot that frequently ulcerate
Creation of a functional unit that can accommodate either
normal or modified shoe gear (failed management of Charcot’s
arthropathy)
An unsalvageable extremity due to critical limb ischemia in
patients with vascular disease.

Level of Amputation
The level of the amputation is dictated by the extent of the disease, healing potential of the stump, and rehabilitation potential of the patient.
Although preservation of limb length is desirable, removal of all nonviable and infected tissue is a higher priority.



Goals of Selection of Amputation Level
Creation of a distal stump that can be easily accommodated by a
prosthesis
Creation of a distal stump that is durable and unlikely to break
down from exogenous pressure
Creation of a distal stump that will not cause muscle or other
dynamic imbalances
Healing with primary intention

Types of Amputation
Minor amputation: one or more digits Major amputation: forefoot, level of
ankle, below the knee amputation and above the knee amputation

Early complications
1. Hemorrhage
2. Hematoma
3. Abscess formation
4. Gas gangrene
5. Wound dehiscence & Flap Gangrene
6. DVT & PE

Late complications
1. Pain (Sinus formation, osteitis)
2. Bone spur (bony projections that form
along joint margins)
3. Amputation neuroma
4. Phantom Limb

Prevention