Accolades-Decision & Information Sciences Fall/Spring 2009-2010
Decision Sciences - simdos.unud.ac.id
Transcript of Decision Sciences - simdos.unud.ac.id


Decision Sciences Journal of Innovative Education “Their support is strong, continuous, enthusiastic, prompt, and supports the long-term growth of the journal and the institute.”
Chetan S. Sankar, Editor
Institute of Food Technologists “By combining excellent customer service and a strategic view of the publishing market, they have enabled our scientific society to meet our goals...”
Jerry Bowman, Vice President of Communication
Veterinary Clinical Pathology “I continue to be impressed with both the day-to-day management, including careful atten-tion to quality issues, and long-term planning. We look forward to continuing our relationship for many years…”
Karen M. Young, Editor-in-Chief
exchanges.wiley.com/societies
EDITOR-IN-CHIEF
Christoph Plass
ASSOCIATE EDITORS
Heike Allgayer
Petra Boukamp
Adelheid Cerwenka
Hinrich Gronemeyer
Norbert Fusenig
Kari Hemminki
Peter Lichter
Magnus von Knebel Doeberitz
Anthony B. Miller
Christoph Plass
Paolo Vineis
CONSULTANT FOR BIOSTATISTICS
Annette Kopp-Schneider
EDITORIAL BOARD
Helmut Bartsch (Heidelberg, Germany)Mina J. Bissell (Berkeley, USA)C. Richard Boland (Dallas, USA)Elisabeth Brambilla (Grenoble, France)Webster K. Cavenee (La Jolla, USA)Ann F. Chambers (London, Canada)Anthony T.C. Chan (Shatin, Hong Kong)Lena Claesson-Welsh (Uppsala, Sweden)Joseph Costello (San Francisco, USA)Pierre Coulie (Brussels, Belgium)Jack M. Cuzick (London, UK)Hughes de The (Paris, France)Eleftherios P. Diamandis (Toronto, Canada)Joakim Dillner (Stockholm, Sweden)Dylan Edwards (Norwich, UK)Ros A. Eeles (Sutton, UK)Manel Esteller (Madrid, Spain)Isaiah J Fidler (Houston, USA)John K. Field (Liverpool, UK)David Forman (Lyon, France)Silvia Franceschi (Lyon, France)Eduardo L. Franco (Montreal, Canada)Simone Fulda (Frankfurt, Germany)Gary E. Gallick (Houston, USA)Martin J. Glennie (Southampton, UK)Masanori Hatakeyama (Tokyo, Japan)Harald zur Hausen (Heidelberg, Germany)Carl-Henrik Heldin (Uppsala, Sweden)Meenhard Herlyn (Philadelphia, USA)Richard Houlston (Sutton, UK)Perwez S. Hussain (Bethesda, USA)Ruth F. Jarrett (Glasgow, UK)Jos Jonkers (Amsterdam, The Netherlands)Robert S. Kerbel (Toronto, Canada)Alexander Knuth (Doha, Qatar)Ralf Küppers (Essen, Germany)
Claire E. Lewis (Sheffield, UK)Dongxin Lin (Beijing, China)Douglas R. Lowy (Bethesda, USA)Maria Li Lung (Hong Kong, Hong Kong)Elisebeth Lynge (Copenhagen, Denmark)Alberto Mantovani (Milan, Italy)Suresh Mathivanan (Melbourne, Australia)Sam M. Mbulaiteye (Bethesda, USA)Chris J.L.M. Meijer (Amsterdam, The Netherlands)Hasan Mukhtar (Madison, USA)Karl M€unger (Boston, USA)Christophe Nicot (Kansas City, USA)Hiroshi Ohshima (Suruga-ku, Japan)Mehmet Ozturk (Balcova, Turkey)Athanasios G. Papavassiliou (Athens, Greece)Jae-Gahb Park (Seoul, ROK)Donald Maxwell Parkin (Oxford, UK)Manuel Perucho (Badelona, Spain)Gerd Pfeifer (Grand Rapids, USA)Paul Pharoah (Cambridge, UK)Ranju Ralhan (Toronto, Canada)Hans-Georg Rammensee (Tübingen, Germany)Guido Reifenberger (Düsseldorf, Germany)Thomas Ried (Bethesda, USA)Harvey A. Risch (New Haven, USA)Pedro Romero (Lausanne, Switzerland)Shimon Sakaguchi (Osaka, Japan)Hél ène Sancho-Garnier (Teyran, France)Guido Sauter (Hamburg, Germany)Mark Schiffman (Bethesda, USA)Lalita Shevde-Samant (Birmingham, USA)Young-Joon Surh (Seoul, ROK)Dean G. Tang (Smithville, USA)Luisa Villa (São Paulo, Brazil)Keijo Wakabayashi (Shizouka, Japan)
15 JUNE 2019 | VOLUME 144 | NUMBER 12
EDITORIAL OFFICE
Deutsches KrebsforschungszentrumIm Neuenheimer Feld 28069120 Heidelberg, GermanyTel: +49-6221-42-4800Email: [email protected]
MANAGING EDITOR
Franca BianchiniEmail: [email protected]
ISSN 0020-7136

International Journal of Cancer
IJCAims & ScopeInternational Journal of Cancer, the official journal of the Union forInternational Cancer Control (UICC), appears 24 times per year.International Journal of Cancer invites submissions under a broad scope oftopics relevant to experimental and clinical cancer research and publishesoriginal research articles, mini reviews, short reports, and letters to theeditor. The article categories within the journal are: carcinogenesis, cancercell biology, cancer genetics, infectious causes of cancer, tumor immunology,early detection and diagnosis, epidemiology, and cancer therapy.
PublisherInternational Journal of Cancer is published on behalf of the UICC byWiley Periodicals, Inc., 111 River Street, Hoboken, NJ 07030-5774, USA;http://www.wiley.com
Information for SubscribersInternational Journal of Cancer is published in 24 issues per year.Institutional subscription prices for 2019 are: Print & Online: US$6,782(US and Rest of World), €4,376 (Europe), £3,465(UK). Prices areexclusive of tax. Asia-Pacific GST, Canadian GST/HST and EuropeanVAT will be applied at the appropriate rates. For more information oncurrent tax rates, please go to https://onlinelibrary.wiley.com/library-info/products/price-lists/payment. The price includes online access to thecurrent and all online backfiles to January 1st 2015, where available. Forother pricing options, including access information and terms andconditions, please visit https://onlinelibrary.wiley.com/library-info/products/price-lists
Terms of use can be found here: https://onlinelibrary.wiley.com/terms-and-conditions
For submission instructions, subscription and all other information visit:https://onlinelibrary.wiley.com/journal/10970215
Delivery Terms and Legal TitleWhere the subscription price includes print issues and delivery is to therecipient’s address, delivery terms are Delivered at Place (DAP); the recipientis responsible for paying any import duty or taxes. Title to all issuestransfers Free of Board (FOB) our shipping point, freight prepaid. We willendeavour to fulfil claims for missing or damaged copies within six monthsof publication, within our reasonable discretion and subject to availability.
Journal Customer ServicesFor ordering information, claims and any enquiry concerning your journalsubscription please go to https://hub.wiley.com/community/support/onlinelibraryor contact your nearest office. Americas: Email:[email protected]; Tel: +1 781 388 8598 or +1 800 835 6770 (toll freein the USA & Canada). Europe, Middle East and Africa: Email:[email protected]; Tel: +44 (0) 1865 778315.
Asia Pacific: Email: [email protected]; Tel: +65 6511 8000.Japan: For Japanese speaking support, Email: [email protected] our Online Customer Help available in 7 languages at https://hub.wiley.com/community/support/onlinelibrary
INTERNATIONAL JOURNAL OF CANCER, Print ISSN: 0020-7136;Online ISSN:1097-0215, is published bimonthly. US mailing agent:Mercury Media Processing, LLC, 1850 Elizabeth Avenue, Suite #C,Rahway, NJ 07065 USA. Periodical postage paid at Rahway, NJ.Postmaster: Send all address changes to INTERNATIONAL JOURNALOF CANCER John Wiley & Sons Inc., C/O The Sheridan Press, PO Box465, Hanover, PA 17331 USA.
Back IssuesSingle issues from current and recent volumes are available at the currentsingle issue price from [email protected]. Earlier issues may beobtained from Periodicals Service Company, 351 Fairview Avenue – Ste300, Hudson, NY 12534, USA. Tel: +1 518 822-9300, Fax: +1 518 822-9305, Email: [email protected]
Research4LifeWiley is a founding member of the UN-backed HINARI, AGORA, andOARE initiatives. They are now collectively known as Research4Life, makingonline scientific content available free or at nominal cost to researchers indeveloping countries. Please visit Wiley’s Content Access – CorporateCitizenship site: http://www.wiley.com/WileyCDA/Section/id-390082.html
Copyright and CopyingCopyright © 2019 Union for International Cancer Control. All rightsreserved. No part of this publication may be reproduced, stored ortransmitted in any form or by any means without the prior permission inwriting from the copyright holder. Authorization to copy items for internaland personal use is granted by the copyright holder for libraries and otherusers registered with their local Reproduction Rights Organisation (RRO),e.g. Copyright Clearance Center (CCC), 222 Rosewood Drive, Danvers, MA01923, USA (www.copyright.com), provided the appropriate fee is paiddirectly to the RRO. This consent does not extend to other kinds ofcopying such as copying for general distribution, for advertising orpromotional purposes, for republication, for creating new collective worksor for resale. Permissions for such reuse can be obtained using theRightsLink “Request Permissions” link on Wiley Online Library. Specialrequests should be addressed to: [email protected]
DisclaimerThe Publisher, Union for International Cancer Control and Editorscannot be held responsible for errors or any consequences arising fromthe use of information contained in this journal; the views and opinionsexpressed do not necessarily reflect those of the Publisher, Union forInternational Cancer Control and Editors, neither does the publication ofadvertisements constitute any endorsement by the Publisher, Union forInternational Cancer Control and Editors of the products advertised.
Business CorrespondenceAdvertisementsAdvertising inquiries should be addressed to the Advertising Department,Wiley Periodicals Inc., 111 River Street, Hoboken, NJ 07030, USA. Email:[email protected]; Tel: +1 201 748 6921
Commercial Reprints: E-mail: [email protected];[email protected]; or [email protected] Reprints (50–500 copies): Order online: http://www.sheridanreprints.com/orderForm.html. E-mail: [email protected]
Production InformationProduction Editor: International Journal of Cancer (email:[email protected])
SuppliersTypeset by SPi Global. Printed in the UK by Hobbs the Printers Ltd.
Wiley’s Corporate Citizenship initiative seeks to address the environmental,social, economic, and ethical challenges faced in our business and which areimportant to our diverse stakeholder groups. Since launching the initiative,we have focused on sharing our content with those in need, enhancingcommunity philanthropy, reducing our carbon impact, creating globalguidelines and best practices for paper use, establishing a vendor code ofethics, and engaging our colleagues and other stakeholders in our efforts.Follow our progress at www.wiley.com/go/citizenship
Abstracting & Indexing ServicesThe Journal is indexed by Biological Abstracts (Thomson Reuters),BIOSIS Previews (Thomson Reuters), Biotechnology & BioengineeringAbstracts (ProQuest), CAB Abstracts® VR (CABI), Chemical AbstractsService/SciFinder (ACS), CSA Biological Sciences Database (ProQuest),CSA Environmental Sciences & Pollution Management Database(ProQuest), Current Awareness in Biological Sciences (Elsevier), CurrentContents: Life Sciences (Thomson Reuters), EMBASE (Elsevier), IndexMedicus/MEDLINE (NLM), Journal Citation Reports/Science Edition(Thomson Reuters), PASCAL Database (INIST/CNRS), Science CitationIndex Expanded (Thomson Reuters), Science Citation Index (ThomsonReuters), SCOPUS (Elsevier), SIIC Databases (Sociedad Iberoamericana deInformacion Cientifica), Smoking & Health Database (TIPS), VINITI(All-Russian Institute of Science & Technological Information),Web ofScience (Thomson Reuters)OnlineOpen information is mandatory for all journals offering this service.The list of journals offering Online Open can be found on the OnlineOpenPrice List: https://authorservices.wiley.com/author-resources/Journal-Authors/licensing-open-access/open-access/onlineopen.html InternationalJournal of Cancer accepts articles for Open Access publication. Please visithttps://authorservices.wiley.com/author-resources/Journal-Authors/open-access/onlineopen.html for further information about OnlineOpen.
View this journal online at wileyonlinelibrary.com/journal/IJC

Union for International Cancer ControlURL: http://www.uicc.orgE-mail: [email protected]
Board of DirectorsPROF. SANCHIA ARANDA, President(Australia)
HRH PRINCESS DINA MIRED, President-Elect(Jordan)
DR. TEZER KUTLUK,Immediate-Past-President (Turkey)
DR. BENJAMIN O. ANDERSON (USA)DR. HEATHER BRYANT (Canada)DR. MAIRA CALEFFI (Brazil)EDUARDO CAZAP (Argentina)SALLY COWAL (United States)DR. ANIL D’CRUZ (India)
DR. JEFF DUNN (Australia)NICKGRANT (United Kingdom)MHAMED HARIF (Morocco)HUSSEIN KHALED (Egypt)ANNE LEE (Hong Kong S.A.R., China)PROF. GILBERT LENOIR (France)DR. SAUNTHARI SOMASUNDARAM(Malaysia)
ANN STEYN (South Africa)
Non Voting Liaison toUICC Board Of DirectorsDR. IAN MAGRATH (INCTR)DR. ALBERTO COSTA (ESO)DR. PETER LICHTER (IJC)DR. JOE HARFORD (NCI)DR. CHRIS WILD (IARC
About UICCThe Union for International Cancer Control (UICC) is the leadinginternational non-governmental organization dedicated to global cancercontrol.
Founded in 1933, UICC unites over 300 member organizations, specializedand engaged in cancer control, in more than 100 countries across the world.
UICC’s mission is to connect, mobilize and support organizations,leading experts, key stakeholders and volunteers in a dynamic communityworking together to eliminate cancer as a life-threatening disease forfuture generations.
UICC works closely with its member organizations and partners toimplement a comprehensive strategy that includes
• promoting the World Cancer Declaration• organizing the World Cancer Congress• raising awareness through the World Cancer Campaign• coordinating World Cancer Day annually, on 4 February• reviewing and disseminating the TNM (tumour-node-metastasis)classification of malignant tumours
• developing effective cancer control programmes especially in low- andmiddle-income countries
• changing cancer-related beliefs and behaviour through information andeducation
• creating special initiatives in prevention, early detection, access totreatment and supportive care
• awarding international cancer fellowships• producing cutting-edge scientific publications, such as the InternationalJournal of Cancer
UICC is governed by its member organizations, which meet in a generalassembly, held in conjunction with the World Cancer Congress, every twoyears. Between assemblies, a board of 17 directors, elected by the generalassembly, acts as the executive body of the UICC.
UICC works closely with the World Health Organization (WHO), theInternational Agency for Research on Cancer (IARC), and theProgramme of Action for Cancer Therapy (PACT) and has consultativestatus with the UN Economic and Social Council. It offers corporatepartners a unique opportunity to demonstrate social responsibility on aglobal scale. Every two years.
UICC is non-profit, non-political and non-sectarian. Its headquarters arein Geneva, Switzerland. www.uicc.org

Table of Contents 15 June 2019 Vol. 144 No. 12 International Journal of Cancer
IJC
Mini Review 2909 A new perspective: Exploring future therapeutic strategies for cancer byunderstanding the dual role of B lymphocytes in tumor immunityMin Liu, Qian Sun, Jian Wang, Feng Wei, Lili Yang and Xiubao Ren
Cancer Epidemiology 2918 Lung cancer risk by geologic coal deposits: A case–control study of female never-smokers from Xuanwei and Fuyuan, ChinaJason Y.Y. Wong, George S. Downward, Wei Hu, Lützen Portengen, Wei Jie Seow, DebraT. Silverman, Bryan A. Bassig, Jinming Zhang, Jun Xu, Bu-Tian Ji, Jihua Li, Jun He, Kaiyun Yang,Linwei Tian, Min Shen, Yunchao Huang, Roel Vermeulen, Nathaniel Rothman, and Qing Lan
Indoor coal combustion emissions have been designated as Group 1 carcinogens. However, the influence of
emissions from coal originating from different geological deposits remains unexplored. Lung cancer rates in
the rural counties of Xuanwei and Fuyuan in China are among the highest in the world due to indoor
combustion of bituminous (“smoky”) coal. Using detailed lifecourse data on household fuel sources, the
authors conducted the first study to show that lung cancer risk varies by the geological deposit of household
coal. Notably, childhood exposure to smoky coal may have an important impact on lung cancer risk later in
life.
2928 Cancer incidence and mortality patterns in women with breast symptoms in themammography screening programme: A matched cohort analysisDeependra Singh, Nea Malila, Janne Pitkäniemi, and Ahti Anttila
While breast cancer screening based on factors such as breast density and family history can significantly
reduce breast cancer mortality, little is known about the importance of breast symptoms in screening
programs. In this analysis of mammography screening data collected from 1992-2012 in Finland, women
who reported breast symptoms at screening had significantly increased risks of breast cancer incidence and
mortality. For women who reported a lump or retraction, breast cancer incidence was increased nearly two-
fold and mortality three-fold. The findings suggest that improvements in screening and clinical services are
needed in Finland to better serve women with breast symptoms.
2936 Citrus fruit intake and gastric cancer: The stomach cancer pooling (StoP) projectconsortiumPaola Bertuccio, Gianfranco Alicandro, Matteo Rota, Claudio Pelucchi, Rossella Bonzi,Carlotta Galeone, Francesca Bravi, Kenneth C. Johnson, Jinfu Hu, Domenico Palli,Monica Ferraroni, Lizbeth López-Carrillo, Nuno Lunet, Ana Ferro, Reza Malekzadeh, David Zaridze,Dmitry Maximovitch, Jesus Vioque, Eva M. Navarrete-Munoz, Mohammadreza Pakseresht, RaúlU. Hernández-Ramírez, Malaquias López-Cervantes, Mary Ward, Farhad Pourfarzi,Shoichiro Tsugane, Akihisa Hidaka, Zuo-Feng Zhang, Robert C. Kurtz, Pagona Lagiou, Areti Lagiou,Paolo Boffetta, Stefania Boccia, Eva Negri, and Carlo La Vecchia
The association between citrus fruit intake and cardia cancer was classified as limited/suggestive, whereas
no conclusions could be drawn on non-cardia cancer. Our pooled analysis within a global consortium of
case-control studies indicates and quantifies a protective effect of citrus fruits on both cardia and non-cardia
cancers.
2945 Mediation of associations between adiposity and colorectal cancer risk byinflammatory and metabolic biomarkersJoshua Petimar, Fred K. Tabung, Linda Valeri, Bernard Rosner, Andrew T. Chan, StephanieA. Smith-Warner, and Edward L. Giovannucci
Adiposity is one of the strongest and most consistent modifiable risk factors for colorectal cancer. Adiposity
also affects insulin resistance and is associated with low-grade chronic inflammation -- both of which have
been suggested as possible mechanisms for associations between adiposity and colorectal cancer risk.
Using a novel mediation analysis method, here the authors demonstrate that metabolic and inflammatory
biomarkers may jointly mediate associations between both BMI and adult weight gain with colorectal cancer
risk in men, with stronger results for metabolic biomarkers. The findings offer mechanistic and
methodologic insights into the underlying biology of adiposity and colorectal cancer risk.

2954 The risk of cancer attributable to diagnostic medical radiation: Estimation forFrance in 2015Claire Marant-Micallef, Kevin D. Shield, Jérôme Vignat, Enora Cléro, Ausrele Kesminiene,Catherine Hill, Agnès Rogel, Blandine Vacquier, Freddie Bray, Dominique Laurier,and Isabelle Soerjomataram
Radiation exposure from medical diagnostic procedures accounted for about 0.7% of cases in 2015,
according to a French study. The chief culprit was external radiation, like X-rays or CT scans, and the biggest
increases occurred in leukemia and bladder cancer. They considered the frequency of diagnostic procedures,
combined with the Biological Effects of Ionizing Radiation VII risk model, to estimate the resulting excess
cancer risk from these procedures. While the authors acknowledge that the benefits of medical radiation
exposure outweigh the risks, they point out that careful consideration of dosages and justifications for the
procedures could prevent some cancers.
2964 Is the positive predictive value of high-grade cytology in predicting high-gradecervical disease falling due to HPV vaccination?Farhana Sultana, Karen Winch, Marion Saville, and Julia M.L. Brotherton
A decline in the positive predictive value (PPV) of cervical cytology following population-level decreases in
cervical lesion prevalence was predicted following human papillomavirus (HPV) vaccination. Using routinely
collected registry data, here the authors demonstrate a decline in the PPV of cytology in the younger cohorts
where vaccine impact has been documented in Australia since vaccination implementation. The findings
have implications for the effectiveness of continued screening using cytology in populations with high
vaccine uptake. They call for explicit reconsideration of cervical screening strategies as vaccine coverage
rises and support Australia’s decision to switch to primary HPV testing starting at age 25.
2972 Independent and joint associations of blood lipids and lipoproteins with lungcancer risk in Chinese males: A prospective cohort studyZhangyan Lyu, Ni Li, Gang Wang, Xiaoshuang Feng, Shuohua Chen, Kai Su, Fang Li, Luopei Wei,Xin Li, Shuanghua Xie, Lanwei Guo, Yuheng Chen, Fengwei Tan, Jian Yin, Hong Cui, Hongda Chen,Jiang Li, Jiansong Ren, Jufang Shi, Shouling Wu, Min Dai, and Jie He
Lung cancer arises from more than just smoking: abnormal blood lipid levels also contribute to the disease.
In this report, the authors evaluated the role of cholesterol and triglycerides in lung cancer. They collected
information on total cholesterol, triglycerides, LDL-C, HDL-C, and non-HDL-C from more than 100,000 men in
northern China, and tracked cancer incidence for 9 years. Men whose total cholesterol or triglycerides were
either low or high had increased risk of lung cancer, they found. Low LDL-C levels also associated with an
increase. Considered jointly, the number of abnormal factors was linearly associated with lung cancer risk.
2985 Cancer incidence in Northern Uganda (2013–2016)Francis Okongo, David Martin Ogwang, Biying Liu, and Donald Maxwell Parkin
Up until recently, cancer incidence estimates in Uganda have been entirely dependent on the Kampala
Cancer Registry, which represents about 8% of the national population. Here, the authors report on the first
4 years of the Gulu Cancer Registry, which covers a predominantly rural region of northern Uganda. The
figures suggest a rather different pattern from that observed in the metropolitan population of Kampala,
with high rates of cervix and liver cancer and non-Hodgkin lymphoma (especially childhood Burkitt
lymphoma). The findings help provide a more complete picture of the national cancer profile, permitting
more targeted prevention, detection, and treatment interventions.
2992 Global trends in colorectal cancer mortality: projections to the year 2035Marzieh Araghi, Isabelle Soerjomataram, Mark Jenkins, James Brierley, Eva Morris, Freddie Bray,and Melina Arnold
A new model predicts an overall rise in colorectal cancer deaths worldwide, as the global population ages,
but mortality rates vary by cancer and by country. To guide public health professionals in planning and
allocating resources, these authors calculated predictions for mortality rates through 2035 by country.
Colon cancer mortality will continue decreasing in most countries studied, excepting Latin America and the
Caribbean. Similarly, rectal cancer mortality will decline most places, but is predicted to rise substantially in
Costa Rica, Australia, the United States, Ireland, and Canada, a worrisome trend that should be further
investigated.

3001 Cancer risk among children conceived by fertility treatmentTingting Wang, Lizhang Chen, Tubao Yang, Lesan Wang, Lijuan Zhao, Senmao Zhang, Ziwei Ye,Letao Chen, Zan Zheng, and Jiabi Qin
Fertility treatments and assisted reproduction have become increasingly common since the 1970’s. Could
these treatments increase the risk of cancer among children conceived via these technologies? In this meta-
analysis, the authors found that the answer is ‘yes’: a number of positive associations were identified. They
emphasize that these results should not deter potential parents from seeking treatment for infertility.
However, parents should be aware that their children may have an increased risk of several childhood
cancers. Further research is needed to address the underlying mechanisms.
Cancer Genetics andEpigenetics
3014 RET, a targetable driver of pancreatic adenocarcinomaMoran Amit, Shorook Na’ara, Eran Fridman, Euvgeni Vladovski, Tanya Wasserman, Neta Milman,and Ziv Gil
Changes in the expression patterns of the RET proto-oncogene occur in several tumor types, but clinical
relevance remains to be clarified. This study shows that RET is overexpressed during all stages of pancreas
tumorigenesis. Using a transgenic model, the authors reveal that in the presence of p53 knockdown, RET
activation can serve as a distinct driver for tumorigenesis in the pancreas, regardless of KRAS mutation
status. RET hence emerges as an essential co-driver of pancreatic tumorigenesis and a marker of pancreatic
ductal adenocarcinoma. RET could also be an important potential target in many cancers for sensitization to
chemotherapy or radiation.
3023 Hypermutagenesis in untreated adult gliomas due to inherited mismatchmutationsJason K. Sa, Seung Won Choi, Junfei Zhao, Yeri Lee, Jing Zhang, Doo-Sik Kong, Jung Won Choi, HoJun Seol, Jung-Il Lee, Antonio Iavarone, Raul Rabadan, and Do-Hyun Nam
Hypermutation has been observed in a subset of adult glioma patients as a direct result of temozolomide
(TMZ)-induced mutagenesis, leading to therapeutic resistance. Here, the authors identified a rare subset of
pre-treatment adult glioma patients with de novo hypermutator phenotype. TMZ-naı̈ve hypermutated tumors
lacked somatic mutation of IDH1 and MGMT promoter methylation, and harbored both germline and somatic
dysregulation of mismatch repair machinery encoding genes. Patients with TMZ-naı̈ve hypermutagenesis
demonstrated high incidence of cancer-development history in their immediate family members. Both TMZ-
naı̈ve and post-TMZ treated hypermutated tumors exhibited a significant accumulatin of neoantigen loads,
pointing towards potential implementation of immunotherapy.
Infectious Causes ofCancer
3031 High risk Epstein-Barr virus variants characterized by distinct polymorphisms inthe EBER locus are strongly associated with nasopharyngeal carcinomaKwai Fung Hui, Tsz Fung Chan, Wanling Yang, Jiangshan Jane Shen, Ki Pui Lam, Hin Kwok, PakC. Sham, Sai Wah Tsao, Dora L. Kwong, Maria Li Lung, and Alan Kwok Shing Chiang
Genetic variation in Epstein-Barr virus appears to play an important role in nasopharyngeal cancer (NPC).
These authors conducted a case-control study in Hong Kong, where NPC incidence is high. They compared
EBV genomes from NPC patients with those from population carriers. Population carriers harbored five
different EBV types, they found, while only two showed up in tumor samples. A genome-wide association
study identified a four-base-deletion in the EBER locus, which occurred in 97% of NPC cases and 40% of
population carriers. More research into the geographic distribution of EBV variants could help explain why
NPC incidence varies among populations.
Molecular CancerBiology
3043 miR-4324-RACGAP1-STAT3-ESR1 feedback loop inhibits proliferation andmetastasis of bladder cancerQiangqiang Ge, Mengxin Lu, Lingao Ju, Kaiyu Qian, Gang Wang, Chin-Lee Wu, Xuefeng Liu,Yu Xiao, and Xinghuan Wang
MicroRNAs have been reported to play important roles in bladder cancer (BCa) carcinogenesis, but
mechanisms of action remain to be fully elucidated. This study reveals that miR-4324 is one of the most
significantly downregulated miRNAs in BCa tissues. miR-4324 suppresses cell proliferation and metastasis
and enhances chemotherapy sensitivity to doxorubicin by repressing RACGAP1 expression. ESR1 can
increase the expression of miR-4324 by binding to its promoter. p-STAT3 can induce the enrichment of
DNMT3B by binding to ESR1 promoter and induce methylation of ESR1 promoter. miR-4324-RACGAP1-STAT3-
ESR1 feedback loop may thus be a critical regulator of BCa progression and potential therapeutic target.

3056 Toll-like receptor 2 regulates metabolic reprogramming in gastric cancer viasuperoxide dismutase 2You Dong Liu, Liang Yu, Le Ying, Jesse Balic, Hugh Gao, Nian Tao Deng, Alison West, Feng Yan,Cheng Bo Ji, Daniel Gough, Patrick Tan, Brendan J. Jenkins, and Ji Kun Li
Many types of tumor cells have altered metabolism, which supports their rapid growth. Pattern-recognition
receptors such as Toll-like receptors (TLRs) can have a broad range of effects on inflammation-associated
cancers such as gastric cancer (GC), and can influence proliferation, apoptosis, and migration. In this study,
the authors identified a novel TLR2- SOD2 axis that promotes metabolic reprogramming of GC cells,
mediated by multiple oncogenic signaling pathways. Increased expression of these proteins in gastric
tumors may serve as a valuable biomarker for therapy and prognosis in GC.
3070 RAB27A promotes melanoma cell invasion and metastasis via regulation of pro-invasive exosomesDajiang Guo, Goldie Y.L. Lui, Siew Li Lai, James S. Wilmott, Shweta Tikoo, Louise A. Jackett,Camelia Quek, Darren L. Brown, Danae M. Sharp, Rain Y.Q. Kwan, Diego Chacon, Jason H. Wong,Dominik Beck, Michelle van Geldermalsen, Jeff Holst, John F. Thompson, Graham J. Mann, RichardA. Scolyer, Jennifer L. Stow, Wolfgang Weninger, Nikolas K. Haass, and Kimberley A. Beaumont
Although metastasis is the primary cause of death in melanoma, we still do not fully understand the
molecular mechanisms involved. In this study, the authors found that a GTPase called RAB27A is
overexpressed in a subset of melanomas, and correlates with poor survival. RAB27A appears to stimulate
melanoma cells to secrete pro-invasive exosomes, which enhance the motility, invasiveness, and metastasis
of tumor cells. These results indicate that RAB27A overexpression may provide a useful prognostic
biomarker, as well as a potential therapeutic target for inhibiting melanoma metastasis.
Tumor Immunologyand Microenvironment
3086 Colitis-induced colorectal cancer and intestinal epithelial estrogen receptor betaimpact gut microbiota diversityAhmed Ibrahim, Luisa W. Hugerth, Linnea Hases, Ashish Saxena, Maike Seifert, Quentin Thomas,Jan-Åke Gustafsson, Lars Engstrand, and Cecilia Williams
Chronic inflammation of the colon is a risk factor for colorectal cancer (CRC). Hormone-replacement therapy
reduces CRC incidence, and the estrogen receptor beta (ERβ/ESR2) has been implicated in this protection.
The microbiota of the gut is altered in both colitis and CRC, but whether intestinal ERβ affects gut microbiota
remains to be investigated. Here, the authors demonstrate, in a mouse model, that colitis-induced CRC
reduces the gut microbiota diversity and that loss of ERβ enhances this process. The findings could enable
novel therapeutic or preventive approaches toward a more favorable microbiome in inflammatory bowel
disease and/or colon cancer development.
3099 Expression of PD-L1 in tumor-associated nerves correlates with reduced CD8+
tumor-associated lymphocytes and poor prognosis in prostate cancerRu-Jun Mo, Zhao-Dong Han, Ying-Ke Liang, Jian-Heng Ye, Shu-Lin Wu, Sharron X. Lin, Yan-Qiong Zhang, Sheng-Da Song, Fu-Neng Jiang, Wei-De Zhong, and Chin-Lee Wu
Immunotherapies targeting programmed cell death protein 1 (PD-1) and its ligand PD-L1 display durable
clinical benefit across various cancer types. However, an immunosuppressive tumor microenvironment has
been suggested to underlie the resistance to anti-PD-L1/PD-1 monotherapy in prostate cancer patients. This
study investigates stromal PD-L1 and its relationship with tumor-associated lymphocytes (TALs) in prostate
cancer. The findings indicate that PD-L1 is expressed in tumor-associated nerves (TANs) and that high
density of PD-L1+ TANs correlates with reduced CD8+ TALs and predicts poor prognosis of prostate cancer.
Combinatorial treatment targeting neural PD-L1 and TALs should be warranted in anti-PD-L1/PD-1
immunotherapies for prostate cancer.

3111 Glioma exosomes mediate the expansion and function of myeloid-derivedsuppressor cells through microRNA-29a/Hbp1 and microRNA-92a/Prkar1apathwaysXiaofan Guo, Wei Qiu, Jian Wang, Qinglin Liu, Mingyu Qian, Shaobo Wang, Zongpu Zhang,Xiao Gao, Zihang Chen, Qindong Guo, Jianye Xu, Hao Xue, and Gang Li
Myeloid derived suppressor cells (MDSC) suppress the immune system, reducing the effectiveness of
immunotherapy in various cancers. These authors investigated how hypoxia promotes the
immunosuppressive activity of MDSCs. Glioma cells, they found, use exosomes to transport miRNAs to
MDSC progenitor cells, stimulating their differentiation. Hypoxia-induced exosomes exerted a more powerful
effect on MDSC proliferation than normoxia-induced exosomes. The miRNAs induced MDSCs by targeting
two genes, Hbp1 and Prkar1a. miRNA silencing of Hbp1 induced the cell cycle progression of MDSCs. This is
the first study to demonstrate a mechanism by which glioma cells stimulate MDSC expansion.
Tumor Markers andSignatures
3127 Single tube liquid biopsy for advanced non-small cell lung cancerSanne de Wit, Elisabetta Rossi, Sabrina Weber, Menno Tamminga, Mariangela Manicone, JoostF. Swennenhuis, Catharina G.M. Groothuis-Oudshoorn, Riccardo Vidotto, Antonella Facchinetti,Leonie L. Zeune, Ed Schuuring, Rita Zamarchi, T. Jeroen N. Hiltermann, Michael R. Speicher,Ellen Heitzer, Leon W.M.M. Terstappen, and Harry J.M. Groen
Liquid biopsies may provide a convenient and patient-friendly approach to inform prognosis and prediction
of the best treatment management. Here, the authors studied the relation between overall survival and the
presence of four different cancer biomarkers from a single blood draw in 97 advanced non-small cell lung
cancer (NSCLC) patients. The presence of EpCAM high-expressing circulating tumour cells and elevated
levels of tumour vesicles and tumour DNA were associated with a poor clinical outcome, but not the
presence of EpCAM low-expressing CTC. This single tube approach enables simultaneous analysis of several
biomarkers to explore their potential as a liquid biopsy.
Cancer Therapy andPrevention
3138 exSSSRs (extracellular S100 soil sensor receptors)-Fc fusion proteins work asprominent decoys to S100A8/A9-induced lung tropic cancer metastasisRie Kinoshita, Hiroki Sato, Akira Yamauchi, Yuta Takahashi, Yusuke Inoue, I. Wayan Sumardika,Youyi Chen, Nahoko Tomonobu, Kota Araki, Kazuhiko Shien, Shuta Tomida, Hidejiro Torigoe,Kei Namba, Eisuke Kurihara, Yusuke Ogoshi, Hitoshi Murata, Ken-ichi Yamamoto,Junichiro Futami, Endy Widya Putranto, I. Made Winarsa Ruma, Hiromasa Yamamoto, Junichi Soh,Toshihiko Hibino, Masahiro Nishibori, Eisaku Kondo, Shinichi Toyooka, and Masakiyo Sakaguchi
The heterodimer complex S100A8/A9 is a suspected mediator of organ tropic metastasis, whereby tumor
cells, or “seeds,” spread to preferred organ, or “soil,” sites as cancer progresses. Here, the S100 soil
sensor receptors (SSSRs) EMMPRIN, NPTNβ, MCAM, and ALCAM, which display different expression patterns
depending on cancer type, were investigated for their ability to serve as decoys to prevent S100A8/A9
binding to endogenous SSSRs. In experiments in cancer cells and in a lung metastasis model in vivo,
purified chimera decoy SSSR proteins successfully suppressed S100A8/A9-mediated metastasis. The
findings warrant further investigation of SSSR biologics for the prevention of cancer metastasis.
3146 Preclinical evaluation of the first intravenous small molecule MDM2 antagonistalone and in combination with temozolomide in neuroblastomaLindi Chen, Fabio Pastorino, Philip Berry, Jennifer Bonner, Calum Kirk, Katrina M. Wood, HuwD. Thomas, Yan Zhao, Antonio Daga, Gareth J. Veal, John Lunec, David R. Newell, Mirco Ponzoni,and Deborah A. Tweddle
Long-term survival of high-risk neuroblastoma patients currently averages than 50%. New therapies that
both improve survival and reduce treatment toxicity are urgently needed. MDM2 antagonists are a novel
class of anti-cancer agents that stabilize the p53 pathway and lead to tumour suppression. In this preclinical
study, the authors tested a prodrug of the MDM2 inhibitor idasanutlin in mice. They found that this
compound inhibited tumour growth and increased survival, especially in combination with temozolomide.
These results support the further development of idasanutlin plus temozolomide in clinical trials for
neuroblastoma.
Short Report

3160 Modeling and multiscale characterization of the quantitative imaging basedfibrosis index reveals pathophysiological, transcriptome and proteomic correlatesof lung fibrosis induced by fractionated irradiationCheng Zhou, Mahmoud R. Moustafa, Liji Cao, Mark Kriegsmann, Martin Winter,Christian Schwager, Bleddyn Jones, Shijun Wang, Tobias Bäuerle, Ping-Kun Zhou,Martina Schnölzer, Wilko Weichert, Juergen Debus, and Amir Abdollahi
The development of fibrosis scar tissue in the lungs is a dose-limiting effect of radiotherapy for thoracic
malignancies. Molecular mechanisms driving radiation-induced lung fibrosis (RILF), however, remain
unclear. In this study, a fibrosis index (FI) was devised to quantitatively detect spatial and temporal kinetics
of lung fibrosis development. Multi-scale characterization of FI uncovered mechanisms governing lung
fibrosis, including perturbation of immune balance and microvascular integrity. Radiation dose and FI were
correlated with an inflammatory switch toward a macrophage/T-helper cell type 2-like polarized phenotype.
The findings open the way for further mechanistic study and the discovery of therapeutic targets for RILF.
Erratum E9 Erratum
Cover Illustration: Validation of specific expression of PD-L1 on nerve and PD-L1+ TANs distribution in the prostate stroma. The specificity ofPD-L1 on nerve is validated by E1L3N (b) and E1J2J (c), which showed comparative staining pattern on two consecutive sections. In morphologicbenign areas, PD-L1+ axons and fine fibers were observed in tumor-associated stroma and are occasionally close to basal cells, which are indicated bytriangles and arrows, respectively (f and g). See the related article by Mo et al., pages 3099–3110.

Short Report
exSSSRs (extracellular S100 soil sensor receptors)-Fc fusionproteins work as prominent decoys to S100A8/A9-induced lungtropic cancer metastasis
Rie Kinoshita1, Hiroki Sato2, Akira Yamauchi3, Yuta Takahashi2, Yusuke Inoue4, I. Wayan Sumardika1,5, Youyi Chen1,Nahoko Tomonobu1, Kota Araki2, Kazuhiko Shien2, Shuta Tomida6, Hidejiro Torigoe 2, Kei Namba2, Eisuke Kurihara2,Yusuke Ogoshi2, Hitoshi Murata1, Ken-ichi Yamamoto1, Junichiro Futami7, Endy Widya Putranto8, I. Made Winarsa Ruma1,5,Hiromasa Yamamoto 2, Junichi Soh2, Toshihiko Hibino9,† Masahiro Nishibori10, Eisaku Kondo11, Shinichi Toyooka2 andMasakiyo Sakaguchi 1
1Departments of Cell Biology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan2Departments of General Thoracic Surgery and Breast and Endocrinological Surgery, Okayama University Graduate School of Medicine, Dentistry and
Pharmaceutical Sciences, Okayama, Japan3Department of Biochemistry, Kawasaki Medical School, Okayama, Japan4Faculty of Science and Technology, Division of Molecular Science, Gunma University, Gunma, Japan5Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia6Departments of Bioinformatics, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan7Departments of Interdisciplinary Science and Engineering in Health Systems, Okayama University, Okayama, Japan8Department of Child Health, Faculty of Medicine, Universitas Gadjah Mada, Yogyakarta, Indonesia9Department of Dermatology, Tokyo Medical University, Tokyo, Japan10Departments of Pharmacology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama, Japan11Division of Molecular and Cellular Pathology, Niigata University Graduate School of Medical and dental Sciences, Niigata, Japan
Within the “seed and soil” theory of organ tropic cancer metastasis is a growing compilation of evidence that S100A8/A9 functions
as a soil signal that attracts cancer cells to certain organs, which prove beneficial to their growth. S100A8/A9-sensing receptors
including Toll-like receptor 4 (TLR4), advanced glycation end products (RAGE), and also important receptors we recently succeeded
in identifying (EMMPRIN, NPTNβ, MCAM, and ALCAM) have the potential to become promising therapeutic targets. In our study, we
prepared extracellular regions of these novel molecules and fused them to human IgG2-Fc to extend half-life expectancy, and we
evaluated the anti-metastatic effects of the purified decoy proteins on metastatic cancer cells. The purified proteins markedly
suppressed S100A8/A9-mediated lung tropic cancer metastasis. We hence expect that our novel biologics may become a prominent
medicine to prevent cancer metastasis in clinical settings through cutting the linkage between “seed and soil”.
Key words: decoy biologics, S100A8/A9, metastasis
Abbreviations: AGEs: Advanced Glycation End products; CCR7: C-C chemokine receptor 7; CHO: Chinese hamster ovary; CHO: Chinese
hamster ovary; CXCR4: C-X-C chemokine receptor 4; HMGB1: High mobility group box 1; HUVECs: Human umbilical vein endothelial cells;
IgG: Immunoglobulin G; NHMECs: Normal human mammary epithelial cells; NMMs: Normal mouse melanocytes; Pla2g2d: Group IID
phospholipase A2; RAGE: Receptor for Advanced glycation end products; SPECT: Single photon emission computed tomography; TLR4:
Toll-like receptor 4
Additional Supporting Information may be found in the online version of this article.†Toshihiko Hibino has passed away on Jun 1 in 2016.
Conflict of interest: The authors declare that they have no conflicts of interest.
Grant sponsor: Project for Cancer Research and Therapeutic Evolution (P-CREATE) from the Japan Agency for Medical Research and
Development (AMED); Grant numbers: JP17cm0106216; Grant sponsor: Fujii Memorial Medical Science Foundation; Grant sponsor:Kobayashi Foundation for Cancer Research; Grant sponsor: Princess Takamatsu Cancer Research Fund; Grant sponsor: Takeda ScienceFoundation; Grant sponsor: JSPS KAKENHI; Grant numbers: 17H03577
DOI: 10.1002/ijc.31945History: Received 26 Apr 2018; Accepted 18 Oct 2018; Online 26 Oct 2018
Correspondence to: Masakiyo Sakaguchi, Ph.D., Department of Cell Biology, Graduate School of Medicine, Dentistry and Pharmaceutical
Sciences, Okayama University, Okayama 700-8558, Japan, E-mail: [email protected]
International Journal of Cancer
IJC
Int. J. Cancer: (2018) © 2018 UICC
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention

IntroductionDue to its life-threatening nature, the dissemination of cancercells to remote organs is a serious problem in the process ofcancer development. Therefore, the establishment of advancedtherapeutic approaches for regulating metastasis is desired.Investigation of the principles of cancer metastasis at themolecular level should lead to further advancement of thera-peutic measures. An interesting feature of cancer metastasis isthat cancer cells frequently show organ tropic metastasis, forwhich the “seed and soil” theory (cancer as the “seed” and itsfavorite distant organ as the “soil” in metastasis) has beenproposed. Although many events in line with this theory havelong been recognized, the detailed molecular mechanismshave yet to be mapped out.
Hiratsuka et al. reported a breakthrough mechanism inwhich S100A8/A9, a heterodimer complex composed ofinflammatory S100A8 and S100A9 proteins, exhibits a “soilsignal” and functions as a ligand to TLR4. The TLR is itself a“soil sensor” located in cancer cells, enabling the cells toapproach distant soil signal-emitting organs such as the lungs,a well-known location of melanoma metastasis.1 After publi-cation of the report by Hiratsuka et al., the RAGE was alsoincluded as a soil sensor for S100A8/A9.2 We then found fur-ther evidence of other important novel soil sensors forS100A8/A9: EMMPRIN,3 NPTNβ,4 MCAM and ALCAM.5,6
We named the proteins “S100 soil sensor receptors, abbrevi-ated as SSSRs.”5,6 The relationship between S100A8/A9 andthese receptors may be applicable to broad cancer speciessince S100A8/A9 is also utilized by breast cancer cells for lungtropic metastasis.7 Since these receptors seem to be differentlyexpressed depending on the cancer species and since theirexpression seems to be upregulated in response to the pro-gression of cancer malignancy (our study and our ongoingstudies), the S100A8/A9-SSSRs axis therefore may act as animportant mediator in “seed and soil” metastasis in multiplecancer species. We hence had the idea that the extracellulardomains of SSSRs (exSSSRs) function as decoys to preventbinding of S100A8/A9 to endogenous SSSRs of cancer cellswhen they fuse with the Fc region of IgG.8 To initiate a pro-ject to investigate this possibility, we first developed an origi-nal plasmid vector9 that facilitates transgene expression inCHO cells with significantly higher levels in a stable manner.By using this plasmid vector, a marked increase in the pro-duction of exNPTNβ-Fc was consistently obtained.4 The plas-mid vector, which we named pSAKA-1B, produced large
amounts of all exSSSRs-Fc chimera proteins (exRAGE-Fc,exMCAM-Fc, exALCAM-Fc, exEMMPRIN-Fc and exNPTNβ-Fc) from each established CHO-stable clone. The aim of ourstudy was to determine the suppressive effects of the purifieddecoy proteins on S100A8/A9-mediated lung tropic cancermetastasis.
Materials and MethodsCellsDetails are provided in Supporting Information.
Recombinant proteinsPreparation of S100A8/A9 and exSSSRs-Fc decoys is providedin Supporting Information.
RNA-seq-based analysisDetails are provided in Supporting Information.
Quantitative real-time PCRDetails are provided in Supporting Information. Primer pairsare listed in Supporting Information Table 1.
Migration assayDetails are provided in Supporting Information.
Mouse studyDetails are provided in Supporting Information.
Statistical analysisThe analytical method is provided in Supporting Information.
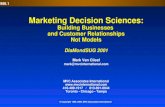
Results and DiscussionDesign and preparation of decoysThe extracellular regions of the SSSRs all consist of Ig domainslike RAGE and are able to bind with S100A8/A9. Therefore,the extracellular compositions of the receptors may be able tofunction as decoys to prevent S100A8/A9 ligand binding thatpromotes lung tropic cancer metastasis. A series of decoys(exSSSRs-Fc) were designed as a fusion form that consists ofthe extracellular portion of each SSSR and the human IgG2-Fcregion but not the commonly used Fc from human IgG1(Fig. 1a). IgG1-Fc expectedly stimulates inflammatory cells bydocking to their own cell surface Fc receptors upon S100A8/A9 binding, which may promote the soil aspect of tropic can-cer metastasis, contrary to our purpose of soil prevention.
What’s new?The heterodimer complex S100A8/A9 is a suspected mediator of organ tropic metastasis, whereby tumor cells, or “seeds,”
spread to preferred organ, or “soil,” sites as cancer progresses. Here, the S100 soil sensor receptors (SSSRs) EMMPRIN,
NPTNβ, MCAM, and ALCAM, which display different expression patterns depending on cancer type, were investigated for their
ability to serve as decoys to prevent S100A8/A9 binding to endogenous SSSRs. In experiments in cancer cells and in a lung
metastasis model in vivo, purified chimera decoy SSSR proteins successfully suppressed S100A8/A9-mediated metastasis. The
findings warrant further investigation of SSSR biologics for the prevention of cancer metastasis.
2 S100 receptor decoy prevents metastasis
Int. J. Cancer: (2018) © 2018 UICC
Can
cerTherapy
andPrevention

Therefore, we used IgG2-Fc as a prominent inflammatorycompromised Fc since human IgG2 shows significantly loweraffinity to the Fc receptor than that of IgG1. These decoys wereexpressed and efficiently secreted in CHO cell-derived stableclones of each decoy. Isolation was done by protein G affinitychromatography using the clone-cultured supernatants, result-ing in highly purified products (Fig. 1b). All of the decoysshowed similar activity in binding to S100A8/A9, but the affin-ities of the decoys were lower than that of an S100A8/A9 anti-body (Supporting Information Fig. 1).
Evaluation of the decoysAt first, we investigated the expression pattern of SSSRs inmouse melanoma B16-BL6 cells in comparison to that in nor-mal mouse melanocytes (NMMs, Supporting InformationFig. 2). Real-time PCR analysis showed higher expression of theSSSRs except for ALCAM in B16-BL6 cells than in NMMs(Fig. 1c). We found that MCAM was significantly upregulatedin B16-BL6 cells. On the other hand, the expression of S100A8/A9 was much lower in B16-BL6 cells than in NMMs. To deter-mine the activity of the decoys for preventing S100A8/A9-mediated migration, we performed a migration assayaccording to the Boyden-chamber method (Fig. 1d, top). Asshown in Figure 1d, bottom, we found that, similar to the effectof the S100A8/A9 antibody (Supporting Information Fig. 3A),all of the decoys had significantly high activity to mitigate themigration of B16-BL6 cells in response to S100A8/A9 regardlessof the marked difference in affinity to S100A8/A9 between thedecoys and the antibody. In this setting, we confirmed thatthe decoys, except for exRAGE-Fc and exNPTNβ-Fc, and theS100A8/A9 antibody had no inhibitory effect on the basalmigration of B16-BL6 cells in the absence of S100A8/A9(Supporting Information Fig. 3B). The unexpected impairmentof migration caused by the two decoys may be due to absorp-tion of other chemoattractant molecules secreted from B16-BL6cells or soluble inclusions in the 0.1% FBS set in the bottomchamber, which may selectively adapt to RAGE and NPTNβ.The decoys and the S100A8/A9 antibody did not showany appreciable disturbance in cell viability (Supporting Infor-mation Fig. 3C) and cell cycle states (Supporting InformationFig. 3D). To imitate a blood vessel, we next seeded humanumbilical vein endothelial cells (HUVECs) on the trans-wellmembrane to be confluent in the Boyden-chamber system andfound that all of the decoys functioned to greatly mitigate theS100A8/A9-mediated migration as well as invasion (SupportingInformation Fig. 4B and 4C, left). In addition, the decoys sup-pressed both the basal migration and invasion even in absenceof foreign S100A8/A9 (Supporting Information Fig. 4B and 4C,right), probably due to the similar reason as mentioned in Sup-porting Information Figure 3B. The settings include anotherfactors from HUVECs besides to B16-BL6 cells and 0.1% FBS.
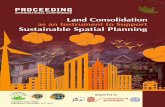
These results encouraged us to evaluate the preventiveeffects of the decoys on lung tropic metastasis in vivo.B16-BL6 cells with or without decoys were injected into the
tail veins of mice (Fig. 2a). One of the characteristics of mela-noma is the appearance of black stains, and this made it veryeasy to observe the high metastatic rate of B16-BL6 cells inthe resected lung in the absence of decoys. Among the decoys,exRAGE-Fc and exMCAM-Fc reduced lung metastasis ofB16-BL6 cells (Fig. 2b). To quantify accurately the metastaticrate, we used a CT scan to help measure the total tumor vol-ume in the whole lung and found that exMCAM-Fc showedthe highest activity for reduction of lung metastasis (Fig. 2c).exMCAM-Fc was further evaluated by an orthotopic model(Fig. 2d). The decoy also showed much higher activity in met-astatic prevention even in this model (Fig. 2e and f). We con-firmed that there was no appreciable disturbance in thehealthy states of lung tissues (Supporting Information Fig. 5)or body weights (data not shown) in the exMCAM-Fc-treatedmice compared to that in the control IgG-treated groups,which were not burdened with B16-BL6 cells. These resultssuggest that exMCAM-Fc has the highest antimetastatic activ-ity in the in vivo settings.
Timing of the administration may effect on the effectivenessof exMCAM-Fc. We found that administration 1 day beforethe injection of cancer cells was most effective for metastaticinterference among the cases of pre-, simultaneous- and post-administrations (Supporting Information Fig. 6A and 6B).However, without our expectation, prolonging of survival wasnot affected by all the timing of injections (Supporting Infor-mation Fig. 6C), probably due to the limited half-life of thedecoy in a living body. Thus, the preventive effect of the decoymay be a transient (within around 2 weeks).
To determine whether the antimetastatic effects of thedecoys are applicable in other cancers with similar lung tropicmetastasis in response to S100A8/A9, we used breast cancercells, MDA-MB-231 (human) and 4T1 (mouse). Both celllines display an S100A8/A9-mediated increase in cellularmobility (Fig. 3a and Supporting Information Fig. 7) and alsolung metastasis in a mouse model.10 At first, MDA-MB-231cells were analyzed for the expression of S100A8, S100A9 andSSSRs, and high expression levels of ALCAM, MCAM andEMMPRIN compared to those in normal human mammaryepithelial cells (NHMECs) were found in MDA-MB-231 cells(Supporting Information Fig. 8A). On the other hand,S100A8/A9 showed a significantly lower expression in MDA-MB-231 cells. The effects of the decoys on the S100A8/A9-mediated migration were evaluated as a prerequisite forin vivo assessments. We found that exMCAM-Fc andexNPTNβ-Fc functioned to prevent S100A8/A9-mediatedmigration (Supporting Information Fig. 8B). An MDA-MB-231 cell suspension together with each decoy was theninjected twice into the tail veins of mice (Fig. 3b). Significantchanges in the appearance of metastatic tumor nodules withinthe lung were detectable in the cases of controls (PBS andIgG) (Fig. 3c). Notably, somewhat different from the in vitroresults (Supporting Information Fig. 8B), all decoys showed atendency to suppress lung metastasis. Among the decoys,
Kinoshita et al. 3
Int. J. Cancer: 9999, 1–8 (2018) © 2018 UICC
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention

IgG2
-Fc
NH2
RAGE
ALCAM
MCAM
EMMPRIN
NPTNβ
V C2 C2
V C2 C2V C2
C2 V
Ig Ig Ig
(kDa)
250
150
10080
6050
(a) (b)
0 hr 12 hr
8 µm pore
medium
supplemented
with 0.1 % FBS
Lower chamber
: S100A8/A9
+ Fc fusion proteins
Upper chamber
: B16-BL6 cells: serum-free medium
(c) (d)
Tota
l Mean In
va
ded C
ells
(–) (–)
NPTN
β-F
c
EM
MPRIN
-Fc
+ S100A8/A9
****
**
**
Tota
l Mean In
va
ded C
ells
+ S100A8/A9
(–) (–)
(–) (–)
matrigel
RAG
E-F
c
ALC
AM
-Fc
MCAM
-Fc
S100A9
Rela
tive m
RN
A e
xpre
ssio
n
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6
S100A8
Re
lative
mR
NA
expre
ssio
n
**
0
0.5
1
1.5
2
NMMs B16-BL6
RAGE
MCAM
ALCAM
EMMPRIN
NPTNβ
*
0
0.5
1
1.5
2
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6
Rela
tive m
RN
A e
xpre
ssio
n
***
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n
***
0
20
40
60
80
100
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n ***
0
0.5
1
1.5
2
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n
***
RAG
E-Fc
ALCAM
-Fc
MCAM
-Fc
EMM
PRIN
-Fc
NPTN
β-FcExtracellular domains of SSSRs
0
200
400
600
800
1000
1200
Tota
l Mean In
va
ded C
ells
+ S100A8/A9
0
200
400
600
800
1000
1200
1400
1600
0
1000
2000
3000
4000
5000
6000
7000
V C2 C2V C2
40
30
IgG2
-Fc
NH2
RAGE
ALCAM
MCAM
EMMPRIN
NPTNβ
V C2 C2
V C2 C2V C2
C2 V
Ig Ig Ig
(kDa)
250
150
10080
6050
(a) (b)
0 hr 12 hr
8 µm pore
medium
supplemented
with 0.1 % FBS
Lower chamber
: S100A8/A9
+ Fc fusion proteins
mberUpper chamm
cellse: B16-BL6 cce mmediumm: serum-freee
(c) (d)
Tota
l Mean In
va
ded
Cells
(–) (–)
NPTN
β-F
c
EM
MPRIN
-Fc
+ S100A8/A9
********
****
**
Tota
l Mean In
va
ded
Cells
+ S100A8/A9
(–) (–)
(–) (–)
matrigel
RAG
E-F
c
ALC
AM
-Fc
MCAM
-Fc
S100A9
Rela
tive m
RN
A e
xpre
ssio
n
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6
S100A8
Re
lative
mR
NA
exp
ressio
n
****
0
0.5
1
1.5
2
NMMs B16-BL6
RAGE
MCAM
ALCAM
EMMPRIN
NPTNβ
*
0
0.5
1
1.5
2
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6
Rela
tive m
RN
A e
xpre
ssio
n
**************
0
0.2
0.4
0.6
0.8
1
1.2
NMMs B16-BL6Re
lative
mR
NA
exp
ressio
n
*******
0
20
40
60
80
100
NMMs B16-BL6Re
lative
mR
NA
expre
ssio
n *******
0
0.5
1
1.5
2
NMMs B16-BL6Re
lative
mR
NA
exp
ressio
n
**************
RAG
E-Fc
ALCAM
-Fc
MCAM
-Fc
EMM
PRIN
-Fc
NPTN
β-FcExtracellular domains of SSSRs
0
200
400
600
800
1000
1200
Tota
l Mean In
va
ded
Cells
+ S100A8/A9
0
200
400
600
800
1000
1200
1400
1600
0
1000
2000
3000
4000
5000
6000
7000
V C2 C2V C2
40
30
***
Figure 1. Preparation of decoys and their activity for suppression of S100A8/A9-mediated cell mobility. (a) Design of a series of S100A8/A9decoys (exSSSRs-Fc: exRAGE-Fc, exMCAM-Fc, exALCAM-Fc, exEMMPRIN-Fc and exNPTNβ-Fc). The fused Fc fragment was from human IgG2. Ig:immunoglobulin (Ig)-like domain, V: Ig-like variable (V)-type domain, C2: Ig-like constant 2 (C2)-type domain. (b) Purification of the decoyproteins. The isolated decoy proteins from conditioned media in cultures of CHO stable clones were applied to SDS-PAGE and stained withCBB. (c) Expression profiling of SSSRs in B16-BL6 cells. Quantitative real-time PCR was used to examine the expression levels of SSSRs inB16-BL6 cells compared to the levels in NMMs. Data are expressed as means � SD, *p < 0.05, **p < 0.01 and ***p < 0.001. (d) Effects ofdecoys on migration of B16-BL6 cells in response to S100A8/A9. A Boyden chamber-based in vitro migration assay was used to evaluate thesuppressive effects of decoys on S100A8/A9 function (top panel). B16-BL6 cells were placed in the top chamber and purified recombinantS100A8/A9 (100 ng/mL) was added to the bottom well in the presence or absence of the purified decoys (1,000 ng/mL). Results ofquantification of cells that migrated to the underside of the trans-well membrane are shown in the bar graph with means � SD, *p < 0.05 and**p < 0.01 (bottom panel).
4 S100 receptor decoy prevents metastasis
Int. J. Cancer: (2018) © 2018 UICC
Can
cerTherapy
andPrevention

(f)
(b)
(a)
Fc fusion proteinstreatment
2 weeks
Evaluation
B16-BL6 cell
cellinjection
Tail vein injection of cells and Fc fusion proteins
into Balb/c nu/nu
(c)
RAGE ALCAMMCAM EMMPRIN NPTNβPBS
B16-BL6
RAGE ALCAMMCAM EMMPRIN NPTNβPBS0
0.2
0.4
0.6
0.8
1
1.2
(Ratio to C
ontr
ol P
BS
)R
ela
tive a
rea
*
0
20
40
60
80
100
120
IgG MCAM
*
0
2
4
6
8
10
12
14
16
18
20
IgG MCAM
*
Th
e N
um
be
r o
f T
ota
l L
un
g F
oci
Th
e N
um
be
r o
f L
un
g F
oci
(≧
2 m
m in
dia
me
ter)
IgG
exMCAM-Fc
(d)
(e)
1 week
EvaluationB16-BL6 cell
Tail vein injection of MCAM-Fc fusion protein
into C57BL/6J when tumors reached
4-5 mm in size
MCAM-Fc fusion proteinor IgG treatment
Intradermal injection of B16-BL6 cells
into the ear
1 month
cellinjection
1
2
(f)ff
(b)
(a)
Fc fusion proteinstreatment
2 weeksB16-BL6 cell
ceinjectiocc n
cell
f cells ction ofTail vein injecteinson protand Fc fusionub/c nu/ninto Balb
(c)
RAGE ALCAMMCAM EMMPRIN NPTNβPBS
B16-BL6
RAGE ALCAMMCAM EMMPRIN NPTNβPBS0
0.2
0.4
0.6
0.8
1
1.2
(Ratio to C
ontr
ol P
BS
)R
ela
tive a
rea
**
0
20
40
60
80
100
120
IgG MCAM
**
0
2
4
6
8
10
12
14
16
18
20
IgG MCAM
**
Th
e N
um
be
r o
f T
ota
l L
ung F
oci
Th
e N
um
be
r o
f L
ung F
oci
(≧
2 m
m in
dia
me
ter)
IgG
exMCAM-Fc
(d)
(e)
1 week
EvaluationB116-BL6 cell
Tail veMCAM-Fc fusion protein
into C57BL/6Jwhen tumors reached
4-5 mm in size
MCAM-Fc fusion proteinor IgG treatment
ein injection ofFc fusion protein
al injection IntradermBL6 cellsof B16-he ear into th
1 month
cellinjection
1
2
Evaluation
Figure 2. Effect of decoys on lung metastasis of mouse melanoma. (a) Schematic representation of the protocol of lung tropic cancer metastasisin experimental forced model. Mouse malignant melanoma B16-BL6 cells (2 × 105 cells) with or without decoys (50 μg) were injectedintravenously into immunocompromised Balb/c nu/nu mice. (b and c) Evaluation of lung metastasis of B16-BL6 cells. Two weeks later, lungmetastasis was monitored by images (b, bottom side) from melanoma-based black color in the dissected mouse lung and by images (b, topside) and quantified data (C) from CT scan-based total tumor volume in the whole lung. Data are expressed as means � SD, *p < 0.05. (d)Schematic representation of the experimental protocol of lung tropic cancer metastasis in orthotopic autonomous model. Mouse malignantmelanoma B16-BL6 cells (1 × 105 cells) were intradermally injected to back side of one ear. After raising tumors with 4–5 mm diameter in sizefor 1 month, either exMCAM-Fc decoy (50 μg) or control IgG (50 μg) was injected intravenously into tail of immunocompetent C57BL/6 J mice.(e and f ) Evaluation of lung metastasis of B16-BL6 cells. One week later, lung metastasis was monitored by images (e) from melanoma-basedblack foci in the dissected mouse lung and quantified by counting on ground of clear foci (f ). The quantified data were graphed for total foci(left panel) and also for big foci reached more than 2 mm diameter in size (right panel). Data are expressed as means � SD, *p < 0.05.
Kinoshita et al. 5
Int. J. Cancer: 9999, 1–8 (2018) © 2018 UICC
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention

exRAGE-Fc and exMCAM-Fc had the most pronounced sup-pressive effects. For a more detailed examination of the condi-tions of metastatic cancer cells, lung tissue sections in thedecoy groups with either exRAGE-Fc or exMCAM-Fc wereobserved using H&E staining and compared to the PBS con-trol (Fig. 3d). The results of histological examination weresimilar to the CT scan results, i.e., many tumor-originatingfoci of various sizes (circled) were observed in the PBS andwere significantly decreased with exRAGE-Fc as well as withexMCAM-Fc. Interestingly, there were very few metastatictumor foci in the exMCAM-Fc group. exMCAM-Fc alsoshowed the greatest suppressive effect on 4T1 cell lung
metastasis (Supporting Information Fig. 9A and 9B). Throughthe in vivo experiments, we confirmed that there was noappreciable sign of liver tropic metastasis of B16-BL6 cells,MDA-MB-231 cells and 4T1 cells (data not shown). Takentogether, the results indicated that exMCAM-Fc had the mostprominent biological characteristics among the decoys we pre-pared to mitigate S100A8/A9-associated lung tropicmetastasis.
The suppressive effects of exMCAM-Fc can be explainedby the down-regulation of a series of metastatic soil-inducinggenes trigged by S100A8/A9 within the lungs. To determinewhether cancer-mediated gene alteration in the lungs is
(a) (b)
Tail vein injection of cells and Fc fusion proteins
into Balb/c nu/nu
1 month 1 monthMDA-MB-231 cell
Fc fusion proteinstreatment
cellinjection
Fc fusion proteinstreatment Evaluation
(c)
(d)
Tota
l Mean M
igra
ted C
ells
10000
8000
6000
4000
2000
0S100A8/A9(–)
**
RAGE ALCAMMCAM EMMPRIN NPTNβPBS IgG
* ****
0
0.2
0.4
0.6
0.8
1
1.2
Rela
tive a
rea
exRAGE-Fc exMCAM-FcPBS
(Ratio to C
ontr
ol P
BS
)
(a) (b)
Tail vein injection of cells and Fc fusion proteins
into Balb/c nu/nu
1 th1 month 1 th1 monthMDA-MB-231 cell
Fc fusion proteinstreatment
cellinjection
Fc fusion proteinstreatment Evaluation
(c)
(d)
Tota
l Mean M
igra
ted
Cells
10000
8000
6000
4000
2000
0S100A8/A9(–)
**
RAGE ALCAMMCAM EMMPRIN NPTNβPBS IgG
** ***********
0
0.2
0.4
0.6
0.8
1
1.2
Rela
tive a
rea
exRAGE-Fc exMCAM-FcPBS
(Ratio to C
ontr
ol P
BS
)
Figure 3. Effect of decoys on lung metastasis of human breast cancer. (a) S100A8/A9-mediated increase in migration ability of MDA-MB-231cells. MDA-MB-231 cells were confirmed to respond to S100A8/A9 in a migration assay. (b) Schematic representation of the experimentalprotocol of lung tropic cancer metastasis. Human triple negative malignant breast cancer MDA-MB-231 cells (5 × 105 cells) with or withoutdecoys (50 μg) were injected intravenously into immunocompromised Balb/c nu/nu mice. After the injection, decoys (50 μg) were injectedagain intravenously at a one-month interval. (c and d) Evaluation of lung metastasis of MDA-MB-231 cells. One month after the secondinjection of decoys, lung metastasis was monitored by CT scan-based total tumor volume in the whole lung (c) and microscopy of HE-stainedlung tissue sections (d). Data in (c) are expressed as means � SD, *p < 0.05 and **p < 0.01.
6 S100 receptor decoy prevents metastasis
Int. J. Cancer: (2018) © 2018 UICC
Can
cerTherapy
andPrevention

affected by exMCAM-Fc, we performed a RNA-seq-basedcomprehensive analysis of gene expression in mice lungs. Toavoid contamination of mouse lung RNAs with mouse can-cer RNAs, we did not use lungs resected from mice that hadbeen injected with mouse cancer cells but used lungsresected from mice injected with human MDA-MB-231 cellstreated or not treated with decoys. We found that quite alarge number of genes were differentially expressed in eachdecoy group compared to that in the PBS group. Knowingthat, we decided to focus on soluble factors, since the meta-static soil feature is critically affected by certaininflammation-related soluble factors.11 We then narroweddown genes encoding soluble factors to genes that weredominantly (p < 0.05) downregulated by exMCAM-Fc treat-ment compared to those in the PBS group (SupportingInformation Fig. 9C). Notably, the selected genes includedgenes encoding the secretory proteinases Mmp12, Mmp13and Pla2g2d, the interleukin Il33, chemokines Ccl19, Ccl1,Ccl2, Ccl5, Ccl8, Ccl12, Ccl21, Cxcl12 and Cxcl5/6, and thecomplement factor C5. The expression levels of the selectedgenes were compared in the decoy groups. Heat map imagesshowed similar patterns in the exMCAM-Fc and exRAGE-Fcgroups. Ccl19, Ccl1, Ccl2, Ccl8 and Ccl12 were genes show-ing a tendency to be downregulated by all decoy treatmentsin a consistent manner.
Mmp12 and Mmp13 contribute to cancer invasion viamatrix collapse in cancer microenvironments. Mmp13 alsocontributes to the maturation of immune-suppressing Tregcells.12 Regarding to this, Il33 involves in activation of Tregcells13 and Pla2g2d plays a critical role in immune suppres-sion.14 Hence, an immune suppressive environment triggeredby them is possibly involved in onset of metastatic soil forma-tion and after its ripeness. For the identified chemokines, wewere particularly interested in Ccl19, Ccl2, Ccl21 and Cxcl12.Receptor CCR7, which binds with both Ccl19 and Ccl21,mediates metastasis of breast cancer to lymph nodes.15 TheCxcl12 receptor CXCR4 promotes breast cancer metastasis tothe lungs.16 The CCL2 promotes lung metastasis of breastcancer cells.17 Furthermore, complement C5 functions tostrongly attract cancer cells.18
Among these chemokines, Eisenblaetter et al. recentlyreported an unusual role of Ccl2 in S100A8/A9-mediatedbreast cancer metastasis to the lung.7 They succeeded in vivoimaging of S100A8/A9 using its antibody-based SPECT andrevealed that Ccl2 mediates tumor metastatic niche formation
in the lung before cancer cells migrate to the lung. Namely,breast cancer located in the mammary fat pad stimulates Ccl2induction in the remote lung and causes an increase in theCCR2highCX3CR1low monocyte population in the same place,where Ccl2 readily binds to its receptor CCR2 in theCCR2highCX3CR1low monocytes, resulting in a large amountof S100A8/A9 secretion from the monocytes. Interestingly,this process is associated with increase in Treg cells in thelung. These results may explain the greater suppressive effectsof the decoys on lung metastasis in the case of breast cancercells since our decoys, especially exMCAM-Fc and exRAGE-Fc, markedly reduced Ccl2 expression in the breast cancer-bearing mouse lung (Supporting Information Fig. 9C).
Due to the contribution of various normal cells to the can-cer metastatic processes, there might be different patterns ofdecoy effectiveness in in vitro (Fig. 1d) and in vivo (Fig. 2b, c,3c, d and Supporting Information Fig. 8B) settings. Thus, theresults may indicate that the identified soluble factors play acritical role in metastatic soil formation in the lungs throughmodulating inflammation, immune activity and chemotacticattraction and that a series of simultaneous downregulationsof all of the identified genes may induce the greatest suppres-sive effect by exMCAM-Fc on lung tropic metastasis of MDA-MB-231 cells.
The use of decoys may not be restricted to S100A8/A9since each receptor’s extracellular region is capable of interact-ing with several ligands that are related to cancer progression.For example, RAGE interacts with AGEs,19 HMGB120 andmost S100 family proteins21; MCAM interacts with galectin-322 and Wnt5a23; and EMMPRIN interacts withcyclophilin A.24 Thus, interactions with these factors may pro-vide additional decoy-mediated suppressive effects. The differ-ences in affinity and specificity to the ligands may alsocontribute to the inconsistent results found among the differ-ent decoys. We do not consider the lower specificity to ligandsas a shortcoming. This is in fact a strong point for decoysbecause of absorption simultaneously with multiple ligands.
AcknowledgementsThis research was supported by the Project for Cancer Research and Ther-apeutic Evolution (P-CREATE) from the Japan Agency for MedicalResearch and Development (AMED, Grant Number JP17cm0106216) toM.S., JSPS KAKENHI (Grant Number 17H03577) to M.S., Takeda ScienceFoundation to M.S., Princess Takamatsu Cancer Research Fund to M.S.,Kobayashi Foundation for Cancer Research to M.S., and Fujii MemorialMedical Science Foundation to M.S.
References
1. Hiratsuka S, Watanabe A, Aburatani H,et al. Tumour-mediated upregulation of chemoat-tractants and recruitment of myeloid cells prede-termines lung metastasis. Nat Cell Biol 2006;8:1369–75.
2. Sakaguchi M, Murata H, Aoyama Y, et al. DNAX-activating protein 10 (DAP10) membrane adaptorassociates with receptor for advanced glycation
end products (RAGE) and modulates the RAGE-triggered signaling pathway in human keratino-cytes. J Biol Chem 2014;289:23389–402.
3. Hibino T, Sakaguchi M, Miyamoto S. S100A9 is anovel ligand of EMMPRIN that promotes mela-noma metastasis. Cancer Res 2013;73:172–83.
4. Sakaguchi M, Yamamoto M, Miyai M, et al. Iden-tification of an S100A8 receptor Neuroplastin-β
and its heterodimer formation with EMMPRIN.J Invest Dermatol 2016;136:2240–50.
5. Ruma IM, Putranto EW, Kondo E, et al. MCAM,as a novel receptor for S100A8/A9, mediates pro-gression of malignant melanoma through promi-nent activation of NF-κB and ROS formationupon ligand binding. Clin Exp Metastasis 2016;33:609–27.
Kinoshita et al. 7
Int. J. Cancer: 9999, 1–8 (2018) © 2018 UICC
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention
Can
cerTherapy
andPrevention

6. Sumardika IW, Youyi C, Kondo E, et al. ß-1,-3-galactosyl-O-glycosyl-glycoprotein ß-1,6-N-acetylglucosaminyltransferase 3 increases MCAMstability, which enhances S100A8/A9-mediatedcancer motility. Oncol Res 2018;26:431–44.
7. Eisenblaetter M, Flores-Borja F, Lee JJ,et al. Visualization of tumor-immune interaction -target-specific imaging of S100A8/A9 reveals pre-metastatic niche establishment. Theranostics 2017;7:2392–401.
8. Czajkowsky DM, Hu J, Shao Z, et al. Fc-fusionproteins: new developments and future perspec-tives. EMBO Mol Med 2012;4:1015–28.
9. Sakaguchi M, Watanabe M, Kinoshita R,et al. Dramatic increase in expression of a trans-gene by insertion of promoters downstream of thecargo gene. Mol Biotechnol 2014;56:621–30.
10. Bailey-Downs LC, Thorpe JE, Disch BC,et al. Development and characterization of a pre-clinical model of breast cancer lung micrometa-static to macrometastatic progression. PLoS One2014;9:e98624.
11. Martin M, Wei H, Lu T. Targeting microenviron-ment in cancer therapeutics. Oncotarget 2016;7:52575–83.
12. Lu L, Feng M, Gu J, et al. Restoration of intrahe-patic regulatory T cells through MMP-
9/13-dependent activation of TGF-β is critical forimmune homeostasis following acute liver injury.J Mol Cell Biol 2013;5:369–79.
13. Schiering C, Krausgruber T, Chomka A,et al. The alarmin IL-33 promotes regulatory T-cell function in the intestine. Nature 2014;513:564–8.
14. Miki Y, Kidoguchi Y, Sato M, et al. Dual roles ofgroup IID phospholipase A2 in inflammation andcancer. J Biol Chem 2016;291:15588–601.
15. Cunningham HD, Shannon LA, Calloway PA,et al. Expression of the C-C chemokine receptor7 mediates metastasis of breast cancer to thelymph nodes in mice. Transl Oncol 2010;3:354–61.
16. Mukherjee D, Zhao J. The role of chemokinereceptor CXCR4 in breast cancer metastasis.Am J Cancer Res 2013;3:46–57.
17. Kitamura T, Qian BZ, Soong D, et al.CCL2-induced chemokine cascade promotesbreast cancer metastasis by enhancing retention ofmetastasis-associated macrophages. J Exp Med2015;212:1043–59.
18. Darling VR, Hauke RJ, Tarantolo S,et al. Immunological effects and therapeutic roleof C5a in cancer. Expert Rev Clin Immunol 2015;11:255–63.
19. Xue J, Rai V, Singer D, et al. Advanced glycationend product recognition by the receptor for AGEs.Structure 2011;19:722–32.
20. Nguyen AH, Detty SQ, Agrawal DK. Clinicalimplications of high-mobility group Box-1(HMGB1) and the receptor for advanced glycationend-products (RAGE) in cutaneous malignancy: asystematic review. Anticancer Res 2017;37:1–7.
21. Leclerc E, Fritz G, Vetter SW, et al. Binding ofS100 proteins to RAGE: an update. Biochim Bio-phys Acta 2009;1793:993–1007.
22. Colomb F, Wang W, Simpson D,et al. Galectin-3 interacts with the cell-surfaceglycoprotein CD146 (MCAM, MUC18) andinduces secretion of metastasis-promoting cyto-kines from vascular endothelial cells. J BiolChem 2017;292:8381–9.
23. Wang W, Runkle KB, Terkowski SM,et al. Protein Depalmitoylation is induced byWnt5a and promotes polarized cell behavior.J Biol Chem 2015;290:15707–16.
24. Seizer P, Ochmann C, Schönberger T,et al. Disrupting the EMMPRIN (CD147)-cyclophilin a interaction reduces infarct size andpreserves systolic function after myocardial ische-mia and reperfusion. Arterioscler Thromb VascBiol 2011;31:1377–86.
8 S100 receptor decoy prevents metastasis
Int. J. Cancer: (2018) © 2018 UICC
Can
cerTherapy
andPrevention