Sternoclavicular joint arthropathy mimicking radiculopathy ...
Crystal Induced Arthropathy
description
Transcript of Crystal Induced Arthropathy

Crystal induced Arthropathy
Dr Doha Rasheedy Ali
Lecturer of Geriatrics and Gerontology
Ain Shams University

• The crystal arthropathies include gout, calcium pyrophosphate deposition disease (CPPD) or pseudogout, basic calcium phosphate (BCP) associated syndromes, and calcium oxalate arthritis.

GOUT

• Gout is a relatively common condition, and is the most common form of inflammatory arthritis.
• 90% of cases with gout occur in men between 30-50 years.
• It is rare in premenopausal females. The uric acid in postmenopausal women reaches the same levels as men due to loss of uricosuric effect of estrogen.
• Uric acid level above 6.8 mg/dL are supersaturated in bodily fluids.
• It is the monosodium urate crystal deposition disease.
• Gout is often accompanied by serious comorbid disorders (hypertension, cardiovascular disease, chronic kidney disease, and all of the component features of the metabolic syndrome)

Causes of hyperuricemia
Urate over production
Primary (idiopathic, HGPRT deficiency
Secondry :psoariasis, multiple myeloma, lymphoma, leukemia, hemolytic anemia, excess purine intake
Urate underexcetion
Primary (idiopathic)
Secondary (renal insufficiency, acidosis, dehydration, drugs, diuretics, hyperparathyroidism,
lead nephropathy
Urate over production and underexcetion
alchol
Glucose 6 phosphatase deficiency
Fructose 1 phosphatase aldolase deficiency

Purine Content of Foods and Beverages
• High: Avoid: Liver, kidney, anchovies, sardines, herring, mussels, bacon, codfish, scallops, trout, haddock, veal, venison, turkey, alcoholic beverages
• Moderate: May eat occasionally: Asparagus, beef, bouillon, chicken, crab, duck, ham, kidney beans, lentils, lima beans, mushrooms, lobster, oysters, pork, shrimp, spinach

Drugs leading to under excretion of uric acid
• Diuretics mainly thiazide
• Ethambutol
• Pyrazinamide
• Salicylate (aspirin)
• Cyclosporin
• Tacrolimus
• L dopa

Pathophysiology • Urate precipitates as needle-shaped monosodium urate (MSU) crystals, which are
deposited extracellularly in avascular tissues (eg, cartilage) or in relatively avascular tissues (eg, tendons, tendon sheaths, ligaments, walls of bursae) and skin around cooler distal joints and tissues (eg, ears).
• In severe, longstanding hyperuricemia, MSU crystals may be deposited in larger central joints and in the parenchyma of organs such as the kidney.
• At the acid pH of urine, urate precipitates readily as small plate like or irregular crystals that may aggregate to form gravel or stones, which may cause obstruction.
• Tophi are large MSU crystal aggregates that most often develop in joint and cutaneous tissue.
• An attack of acute gout follows the ingestion of urate crystals by monocytes and synoviocytes. Uncoated urate crystals are endocytosed by and activate monocytes. Inside the cells, they are processed through Toll-like receptors with result of pre-IL-1 production. The NALP-3 inflammasomes are also activated resulting in caspace-1 formation and the conversion of pre-IL-1 to IL-1 and the generation of a variety of other cytokines, adhesion molecules and chemotactic agents. The result is a very acutely inflamed joint.
• The acute inflammatory response resolves spontaneously over 10–14 days. As the monocytes mature into macrophages, they switch from producing pro-inflammatory cytokines to anti-inflammatory cytokines like transforming growth factor (TGF)-β.
• In between attacks, the tophi continue to enlarge. They are surrounded by a mantle of macrophages that are releasing cytokines and enzymes. This chronic inflammatory response is responsible for eroding bone and cartilage and causes a secondary degenerative joint disease. With enough cartilage degeneration, chronic arthritis that is symptomatically identical to primary osteoarthritis develops.


What are the four stages of gout?
• Stage 1: asymptomatic hyperuricemia.
• Stage 2: the first attack of acute articular disease.
• Stage 3: the period between attacks, described as intercritical gout.
• Stage 4: chronic tophaceous gout.

The natural history of gout progresses through four stages.
• The initial episode of acute gouty arthritis usually follows 10–30 years of asymptomatic hyperuricemia, and there is no evidence that damage occurs to any organ system during that time.
• Although most untreated cases of gout progress to chronic tophaceous gout, the course varies considerably from one patient to another. Whereas some patients experience only one or two attacks of acute gouty arthritis during their lifetime, over 80% have a second flare within 2 years of the first.
• It is quite unusual for tophi to develop in a patient with no history of acute gouty arthritis.


Acute Gouty attack Precipitating factors:
1. Surgery
2. Dehydration
3. fasting
4. heavy ingestion of alcohol.
5. Diet rich in purine.
6. a sudden increase or a sudden decrease in serum urate levels.(It is believed that these fluctuations in urate levels destabilize tophi in the gouty synovium).
Clinical picture: 1. First attack Acute monoarthritis (first meta tarsophalangeal (podagra) ,
ankle, knee, wrist) it rarely affects hip or shoulders. (sudden onset redness, hotness, swelling and pain ) (peak in 12 hours) (if left untreated spontaneous resolution in 5– 14 days).
2. Fever may also be present, Cutaneous erythema associated with the attack may extend beyond the involved jointresemble cellulitis. Desquamation of the skin may occur as the attack resolves.
3. First attack can by polyarticular in tumor lysis syndrome.





Intercritical Gout • Early in the course of the disease it is
asymptomatic period that may last for 2 years after first attack.
• Early in the intermittent stage, episodes of arthritis are infrequent and the intervals between the attacks vary from months to years. Over time, the attacks become more frequent, less acute in onset, longer in duration, and tend to involve more joints (polyarticular).

Chronic Tophaceous Gout • In the later stages of untreated disease, acute attacks are more often
polyarticular (with shorter periods of remission), and are associated with joint damage and deformity; these later stages are associated with loss of mobility, chronic pain, and formation of tophi.
• usually develops after 10 or more years of acute intermittent gout.
• The transition to chronic gout is complete when the intercritical periods are no longer pain-free.
• The involved joints are now persistently uncomfortable and may be swollen. Patients report stiffness or gelling sensations as well. Visible or palpable tophi may be detected on physical examination during this stage of gout, even though they may have been seen on radiographs prior to entry into this stage.
• Occasionally, chronic gouty arthritis and tophi are misdiagnosed as rheumatoid arthritis. The chronic symptoms are polyarticular and symmetric, and the tophaceous deposits mimic rheumatoid nodules


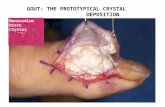
Tophi
• Site: 1. Base of big toe
2. Fingers
3. Wrists
4. Hands
5. Olecranon bursae
6. Achillis tendon
• Complications: 1. Pain
2. Deformity
3. Nerve compression
4. Joint destruction


Uric acid nephrolithiasis
• occurs most commonly, but not exclusively, in individuals with gout.
• In gout, the prevalence of nephrolithiasis correlates with the serum and urinary uric acid levels, reaching ~50% with serum urate levels of 13 mg/dL or urinary uric acid excretion >1100 mg/d.
• Uric acid stones can develop in individuals with no evidence of arthritis, only 20% of whom are hyperuricemic.
• Uric acid can also play a role in other types of kidney stones. Some nongouty individuals with calcium oxalate or calcium phosphate stones have hyperuricemia or hyperuricaciduria. Uric acid may act as a nidus on which calcium oxalate can precipitate or lower the formation product for calcium oxalate crystallization.

Urate Nephropathy • is a late manifestation of severe gout and is characterized
histologically by deposits of monosodium urate crystals surrounded by a giant cell inflammatory reaction in the medullary interstitium and pyramids.
• The disorder is now rare and cannot be diagnosed in the absence of gouty arthritis. The lesions may be clinically silent or cause
proteinuria, hypertension, and renal insufficiency.

Uric Acid Nephropathy • This reversible cause of acute renal failure is due to precipitation of uric
acid in renal tubules and collecting ducts that causes obstruction to urine flow.
• Uric acid nephropathy develops following sudden urate overproduction and marked hyperuricaciduria. Factors that favor uric acid crystal formation include dehydration and acidosis. This form of acute renal failure occurs most often during an aggressive "blastic" phase of leukemia or lymphoma prior to or coincident with cytolytic therapy but has also been observed in individuals with other neoplasms, following epileptic seizures, and after vigorous exercise with heat stress.
• The initial pathogenic events are believed to include obstruction of collecting ducts with uric acid and obstruction of distal renal vasculature.
• Appropriate therapy has reduced the mortality from about 50% to practically nil. Serum levels cannot be relied on for diagnosis because this condition has developed in the presence of urate concentrations varying from 12 to 80 mg/dL. The distinctive feature is the urinary uric acid concentration.
• In acute uric acid nephropathy the ratio of uric acid to creatinine in a random urine sample or 24-h specimen is >1, and a value that high is essentially diagnostic. because In most forms of acute renal failure with decreased urine output, urinary uric acid content is either normal or reduced, and the ratio of uric acid to creatinine is <1.

Investigations 1. Synovial fluid analysis: • The gold standard for diagnosis of gout is the demonstration of by
polarized light microscopy, either in joint fluid aspirated during an acute attack or between attacks, or from material aspirated from suspected tophi. The diagnosis is made by the presence of typical, negatively birefringent, needle-shaped monosodium urate crystals crystals seen with a polarized light microscope. The crystals may be extra- or intracellular.
• During an acute attack, the synovial fluid findings are consistent with moderate to severe inflammation. The leukocyte count usually ranges between 15,000 and 20,000 cells/mcL. The cells are predominantly polymorphonuclear leukocytes.



2. Serum uric acid levels: • may be normal during an acute attack and may not reflect pre-
attack levels. They cannot be used to exclude the diagnosis during an acute attack.
• Uric acid levels are of value in assessing the patient once the acute attack has subsided, either to establish the presence of hyperuricemia or to monitor the effectiveness of therapies that lower serum urate.
3. Markers of inflammation: • during the acute attack, the complete blood cell count may
show a leukocytosis with increase polymorphonuclear leukocytes on the differential and elevations of the erythrocyte sedimentation rate and C-reactive protein.
4. The 24-hour urine uric acid measurement: • is not required in all patients with gout but is useful for
determining potential causes of hyperuricemia, as well as determining whether uricosuric therapy can be effective, since this form of therapy is effective only in underexcreters.

5. Imaging Studies:
• In acute gouty arthritis, the only finding may be soft tissue swelling in the involved joint.
• microtophi develop only after years of disease. These abnormalities are most frequently asymmetric and confined to previously symptomatic joints.
• The advanced bony erosions of advanced gout:
• they are slightly removed from the joint space, have a rounded or oval shape, and are characterized by a hypertrophic calcified “overhanging edge.” The joint space may be preserved or show osteoarthritic type narrowing. Punched out erosion.




• As the erosion develops, the edges of the cortex can be remodelled in an outward fashion, creating an overhanging edge. The following radiograph vividly demonstrates this at the IP joint of the thumb.
• Additionally, because of the chronicity of the process, bone production leads to sclerotic borders, overhanging edges, bony enlargement, and irregular spicules at the sites of tendon and ligamentous attachments.

• joint spaces are preserved until late. Even if the joint is partially destroyed (usually on the dorsal aspect), preservation of another area of the joint (usually flexor aspect) creates the radiographic impression that the joint space is preserved. This is demonstrated at the PIP joint in the following radiograph.

• NO PERI-ARTICULAR OSTEOPENIAIn contrast to rheumatoid arthritis, mineralization is maintained and there is no predominant peri-articular osteopenia. Despite multiple erosions at the PIP joint in the following radiograph, there is no osteopenia.

6. MRI and CT scans are also sensitive methods of detecting tophi and erosions.
7. Ultrasonography can also be used to make the diagnosis. The characteristic finding is a “double contour sign,” a superficial, hyperechoic band on the surface of the articular cartilage.
8. Special Tests Patients with gout often suffer from hyperlipidemia,
glucose intolerance, hypertension, coronary artery disease, and obesity. Accordingly, it is appropriate to measure serum lipids and fasting blood sugars in patients with gout. Because renal dysfunction develops in many patients with hypertension and gout, it is appropriate to monitor serum creatinine levels as well.

• Ultrasound double contour sign. Transverse ultrasound image of the suprapatellar knee joint demonstrates two parallel hyperechoic contours on either side of the hypoechoic hyaline cartilage (HC). The deep echogenic contour (long arrows) represents the femoral cortex, while the superficial echogenic contour (arrowheads) represents uric acid crystals accumulating on the surface of the hypoechoic hyaline cartilage (HC).

DD of Gout
• Acute:
1. Septic arthritis
2. Trauma
3. Psuedo gout
4. cellulitis
• Chronic:
1. Rheumatoid arthritis
2. Osteoarthritis

Treatment
• The management of gout includes the following:
1. Providing rapid and safe pain relief.
2. Preventing further attacks.
3. Preventing formation of tophi and destructive arthritis.
4. Addressing associated medical conditions.

Treatment
Acute attack
NSAIDs
Corticosteroids
ACTH
Colchicine
Anakinra
Intercritical stage
Prohylactic colchicine or indomethacin
Treating hyperuricemia as
later

TREATING ACUTE ATTACK

Acute attack • The goal of treating the acute gout attack is to eliminate the pain
and other symptoms caused by the intense inflammation as rapidly as possible.
• The choices in this situation include nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, glucocorticoids, ACTH , and recombinant IL 1 recetors antagonist.
• Effective management of the acute attack is not so much determined by which agent is used, but rather by how quickly that agent is initiated after the onset of the attack. If a single dose is given in the first minutes of an attack, it may eradicate the symptoms and terminate the attack. If, however, medication is not taken during the first 48 hours of symptoms, it will probably take at least 2 days before control is gained.
• Once symptoms have resolved, the particular agent used should be continued at a reduced dose for another 48–72 hours

NSAIDs • NSAIDs have become the most frequently used
agents to treat gout because they are so well tolerated.
• Contraindications: GIT bleeding, drug allergy, chronic renal insufficiency.
• Aspirin is avoided because it prevent uric acid excretion.
• Choices are: Indomethacin (indocid) (50 mg 1x 4), ibuprofen (Brufen) (800 mg 1x 4), naproxen (500 mg 1x 2).
• Selective COX2 inhibitors can also be used

Colchicine • Colchicine is taken 1.2 mg orally and then 0.6 mg 1 hour later. This can be
repeated every 24 hours as needed. Gastrointestinal side effects include gas, nausea, vomiting, diarrhea, and severe cramping abdominal pain.
• Maximum dose in dialysis patients is 0.6 mg/ attack.
• Once a patient has had an acute gouty attack, the likelihood of further attacks can be reduced by prophylactic therapy with low-dose colchicine. Prophylactic therapy, however, should not be prescribed unless a urate-lowering agent is added to the regimen.
• The prophylactic use of colchicine in doses of 0.6 mg once or twice a day.
• Long-term colchicine use can cause neuromuscular complications in patients with decreased renal function, especially older patients. It is prudent to avoid using more than 0.6 mg of colchicine daily in a patient with a serum creatinine above 1.5 mg/dL.
• This toxicity manifests with proximal muscle weakness, painful paresthesias, elevated creatine kinase levels, and abnormalities on electromyograms. This axonal neuromyopathy resolves completely over several weeks after discontinuing the colchicine.

Glucocorticoids • Glucocorticoids are usually reserved for patients in
whom colchicine or NSAIDs are contraindicated or ineffective.
• Given intraarticular or systemic:
• Doses of prednisone of 20–40 mg/d have been used. tapered over 1–2 weeks after symptoms resolve.
• Intraarticular injections with 20–80 mg of methylprednisolone acetate or 10–40 mg of triamcinolone hexacetonide can also be used Preferable route for monoarticular involvement.

ACTH
• 40 to 80 IU intramuscularly once or twice /day
• For 1 or 2 days
• Mechanism of action in gout: Activation of melanocortin receptor type 3

Recombinant IL 1 recetors antagonist
• Anakinra
• Under trial
• 100 mg daily Subcutaneous for 3 days

Analgesia
• Most often the gout attack resolves with the use of one of these agents. However, when this does not occur or in the extremely severe case of gout, these agents may be used in combination. Potent analgesics, including opioids, may also be added to the regimen.

TREATMENT OF INTERCRITICAL GOUT

Nonpharmacologic urate-lowering treatment
• begins with lifestyle changes. • Diet and weight loss must be addressed. weight loss has
been shown to decrease the risk of gout. • A purine-restricted diet has often been recommended to
patients but is often unpalatable and impractical. • Reduction in alcohol intake, namely beer and liquor, can
effectively reduce urate levels. • Similarly, reduced intake of red meat and shellfish also
lowers the risk of recurrent gouty attacks. • Studies have shown an increased frequency of attacks in
patients who consume fruit juices and soft drinks containing high-fructose corn syrup, an ingredient not found in diet drinks.

Prophylactic therapy
• Prophylactic therapy with low-dose colchicine or an NSAID on a daily basis.
• Start one week before urate lowering therapy and continue for 3- 6 months after stabilizing urate level and the patient has been free from acute gouty attacks.
• Avoid drugs causing hyperuricemia

Treating hyperuricemia
• Target Uric acid< 6 mg/dL. • the duration of treatment is indefinite and must be long-term to be
effective • Choices:
1. Xanthine oxidase inhibitors (allopurinol, febuxostat) 2. Uricosuric drugs ( probencid, sulfyperazone) 3. Uricases ( raspburicase, Pegloticase).
• Indications: 1. Chronic Gouty arthritis. 2. Tophi 3. Gouty nephropathy. 4. Recurrent kidney stones 5. Frequent and disabling gouty attacks, often defined as two or three
flares annually

Xanthine Oxidase Inhibitors • Allopurinol (Zyloric or no uric) and febuxostat
(Uloric).
• It can effectively lower serum urate levels in those patients with hyperuricemia due to underexcretion and is specifically indicated for those who overproduce urate.

Allopurinol • it is recommended that patients start with 100 mg/d for a week and
gradually increase the dose until the lowest level of medication that keeps the serum urate level in the target range is reached.(300 mg/d ).
• The maximum recommended daily dose is 800 mg. • Side effects and toxicity of allopurinol include fever, headaches,
diarrhea, dyspepsia, pleuritis, skin rashes, granulomatous hepatitis, and toxic epidermal necrolysis.
• Allopurinol hypersensitivity reactions are more common in older patients with impaired renal function taking diuretics. The development of a rash in patients taking allopurinol is an indication to stop the medicine.
• Allopurinol should be avoided with the immunosuppressives azathioprine (Imuran) and 6- mercaptopurine (Purinethol) because it can increase the risk of bone marrow toxicity, as these medications are partially metabolized by xanthine oxidase.
• Allopurinol should not be taken with ampicillin owing to increased risk of rash.

Febuxostat (Uloric) • The FDA approved non-purine xanthine oxidase
inhibitor in 2009
• Febuxostat is primarily metabolized by oxidation and glucuronidation in the liver, with little renal excretion of drug; this contrasts with the renal elimination of oxypurinol, the main allopurinol metabolite.
• Start with 40 mg/d po increased to 80 mg/ d after 2 weeks.
• it can safely be taken by patients with creatinine clearance greater than 30 mL/min.

Uricosurics • Indications:
1. good renal function (glomerular filtration rate above 60 mL/minute)
2. no history of nephrolithiasis
3. avoid all salicylate ingestions
4. under 65 years of age
• Contraindications: Creatinine > 2 mg/dL , uric acid excertion > 800 mg/ 24 hour
urine, history of nephrolithiasis.
• Cautions to prevent nephrolithiasis: 1. Maintain urine output of 2 L/day
2. Alkalization of urine using potassium citrate 10 meq tid orally keep urine PH 6-7

• Probenecid:
• is started at a dosage of 250 mg twice a day and advanced slowly up to a maximum dosage of 3 g a day or until the target urate level is reached.
• The most common side effects of this agent are rash and gastrointestinal upset.
• Sulfinpyrazone: start 50 mg twice daily then over weeks to 100 – 200 mg 3 times daily . Maximal dose 800 mg/day

Adjuvants uricosuric agents
• Other drugs found to have uricosuric effects include fenofibrate, a fibric acid derivative used to treat hyperlipidemia, and the antihypertensives losartan (Cozaar) and amlodipine (Norvasc). These agents have mild uricosuric properties and may be useful adjuncts to urate-lowering therapy.
• Skim milk ingestion has been shown to lower serum urate levels through uricosuric effects.
• Lower urate levels have also been seen in patients who consume coffee, but the mechanism of action is unknown.

Recombinant uricase • Convert purine to more soluable allantoin
• Pegloticase: – The dosage is 8 mg intravenously every 2 weeks.
– it has dramatic effects on serum urate levels.
– This agent should be reserved for those with severe gout with abundant tophaceous deposits. Its use may be limited by hypersensitivity reactions and the development of blocking antibodies. Use prohylactic therapy one week before infusion till 6 month after infusion.
– Contraindicated in G6PD deficiency.
• Rasburicase: – nonpegylated recombinant uricase
– Used for prophylaxis against acute uric acid nephropathy in tumour lysis syndrome.
– Side effects: hypersensitivity reactions.

CALCIUM PYROPHOSPHATE DEPOSITION DISEASE (CPPD)

• Deposition of calcium pyrophosphate dihydrate crystals in articular cartilage can be seen on radiographs in 4.5% of adults over the age of 40. its prevalence at the knee rising to about 20% in those over age 80.
• It is almost always of
– unknown cause (sporadic/idiopathic
– associated with osteoarthritis
– but can be associated with metabolic disease (hyperparathyroidism,haemochromatosis, hypophosphatasia,hypomagnesaemia)
– or be hereditary.
• It can affects synovium, tendon, ligaments, and articular cartilages

What conditions have been associated with CPPD disease?
• Hemochromatosis • Hyperparathyroidism • Hypophosphatasia • Hypomagnesemia • Hypothyroidism • Hemosiderosis • Gout • Neuropathic joint • Amyloidosis • Wilson disease • Trauma, including surgery
– Psuedogout was associated with bisphosphonate, intra articular hyaluronic , parathyroidectomy.

The clinical presentations of CPPD disease

Presentations
• Asymptomatic : chondrocalcinosis
• Acute: – psuedogout
• Chronic: – Psuedo osteoarthritis
– Psuedo rheumatoid arthritis
– Psuedo neuropathy
– Spinal involvement
– Extra articular involvement(eye, spleen)

• The degenerative arthropathy associated with CPPD can involve joints not usually affected by osteoarthritis (eg, glenohumeral joint, wrist, patellofemoral compartment of the knee). The “pseudorheumatoid arthritis” of CPPD affects the metacarpophalangeal joints and wrists. In both conditions, radiographs demonstrate chondrocalcinosis and degenerative changes such as asymmetric joint space narrowing and osteophyte formation.

Factors that may trigger acute
pseudogout 1. Intercurrent illness, e.g., chest infection
2. Direct trauma to the joint
3. Surgery, especially parathyroidectomy
4. Blood transfusion and parenteral fluids
5. Institution of thyroxine replacement therapy
6. Joint lavage

• Differential diagnosis:
1. Septic arthritis
2. Trauma
3. Gout
4. Apatite crystal
5. Rheumatoid arthritis
6. Osteoarthritis

Laboratory tests
1. Synovial fluid examination under polarized light microscopy:
• the presence of positively birefringent, rhomboid crystals.
• The crystals may be intra- or extracellular.
• These crystals may be difficult to visualize; therefore, the absence of CPPD crystals in synovial fluid does not necessarily rule out CPPD disease.

• Positive birefringent calcium pyrophosphate dihydrate crystals

• Calcium pyrophosphate dihydrate crystals typical of pseudogout are rhomboid and demonstrate a weakly positive birefringence under polarized light.

• This rhromboid shaped crystal of calcium pyrophosphate dihydrate (CPPD), which appears bluish-white (weak positive birefringence) by polarized light with red plate.


Where is chondrocalcinosis commonly demonstrated roentgenographically?
• Chondrocalcinosis describes the radiographic appearance of CPP crystals in the joint cartilages.
• They are generally punctate and linear densities in the articular cartilages: menisci of the knees, radiocarpal joints, annulus fibrosus of intervertebral discs, and symphysis pubis.

psuedo





Specific Tests
• newly diagnosed CPPD deposition should include tests of serum calcium, phosphorus, magnesium, alkaline phosphatase, thyroid-stimulating hormone levels, and possibly ferritin levels.
• The serum ceruloplasmin levels should also be assessed if Wilson disease is suspected. Hypophosphatasia and Wilson disease need not be considered in patients who become symptomatic after the age of 60 years.

Treatment • NSAIDs are helpful in the treatment of acute episodes. Colchicine, 0.6
mg orally once or twice daily, is more effective for prophylaxis than for acute attacks. Aspiration of the inflamed joint and intraarticular injection of triamcinolone, 10–40 mg.
• Rest, splinting, and eventual joint replacement may be helpful. • However, in patients with an associated metabolic condition, such as
hyperparathyroidism, hemochromatosis, or hypothyroidism, treatment of the underlying disease may decrease the number of attacks but does not result in resorption of crystals.
• Other therapies that have been tried include: • oral magnesium carbonate • intra-articular glycosaminoglycan polysulfate • intra-articular corticosteroids • IM gold or hydroxychloroquine for type B (“pseudorheumatoid”) disease.

BASIC CALCIUM PHOSPHATE (BCP) ASSOCIATED DISEASE

• BCP crystals predominantly composed of partly carbonate-substituted hydroxyapatite, but also include octacalcium phosphate, tricalcium phosphate and magnesium whitlockite.
• BCP crystals are associated with a number of rheumatic syndromes, including acute calcific periarthritis, soft tissue calcification, osteoarthritis and other degenerative arthropathies such as Milwaukee shoulder syndrome (MSS). They have also recently been linked to breast cancer and atherosclerosis.

The key mechanisms whereby BCP crystals may cause tissue damage are
(1) the induction of mitogenesis
(2) the upregulation of matrix metalloproteinase (MMP) production
(3) the stimulation of cyclooxygenases 1 and 2 and prostaglandin E2 production
(4) the stimulation of cytokine production, in particular IL-1β
(5) the induction of nitric oxide (NO) production


• BCP crystals can destroy joints and can cause severe intra-articular or periarticular inflammation. Milwaukee shoulder syndrome is one example, a profoundly destructive arthropathy affecting predominantly elderly women that usually develops in the shoulders and (often) knees.
• Acute podagra due to periarticular BCP deposition can mimic gout; it occurs as a discrete syndrome in young women (less often in young men) and is treated the same as acute gout.




Investigations
• Synovial fluid analysis: Calcium hydroxyapetitie crystals are not visible under plain or polarized light microscopy, but may be visualized by staining with alizarin red.
• On x-ray, BCP crystals may be visible as periarticular cloudlike opacities.

• The treatment of these conditions is as per CPPD disease with NSAIDs and colchicine principally
• Intra articular glucocorticoids
• Rest, Spliting of affected joint

CA OXALATE CRYSTAL DEPOSITION DISEASE

Ca oxalate crystal deposition disease
• Ca oxalate crystal deposition is rare. • It occurs most often in azotemic patients receiving
hemodialysis or peritoneal dialysis, particularly those treated with ascorbic acid (vitamin C), which is metabolized to oxalate.
• Crystals may deposit in blood vessel walls and skin, as well as joints.
• the clinical situations that may be associated with calcium oxalate arthritis are end stage renal disease on dialysis; short bowel syndrome; diets rich in rhubarb, spinach or ascorbic acid; thiamine or pyridoxine deficiency; primary oxalosis (a rare inborn error of metabolism)

Presentation
• The clinical picture is that of an acute mono- or oligo arthritis mainly affecting the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints of the hands.
• Bursal involvement and teno-synovitis may be associated and the arthritis may become chronic.

• The crystals appear as birefringent bipyramidal structures
• Synovial fluid may have > 2000 WBC/μL.
• On x-ray, Ca oxalate crystals are indistinguishable from BCP periarticular calcifications or Ca pyrophosphate dihydrate (CPPD) crystal deposits in cartilage.

• birefringent bipyramidal structures


• The treatment of these conditions is as per CPPD disease with NSAIDs and colchicine principally
• Intra articular glucocorticoids
• Rest, Spliting of affected joint

THANK YOU