Concussion - Connect with Kids · International Consensus Statements on Concussion Historical...
Transcript of Concussion - Connect with Kids · International Consensus Statements on Concussion Historical...

Sports-Related Concussion: Diagnosis & Management
Kenneth Barnes MD, MSc., CAQSM
Internal Medicine, Pediatrics & Sports Medicine
Kernodle Clinic Orthopaedics & Sports Medicine
Adjunct Faculty, Moses Cone Sports Medicine Fellowship
Assistant Professor, Exercise Sports Science, Elon University
Clinical Adjunct Faculty, UNC-CH School of Medicine

Disclosure
Neither I, Kenneth P. Barnes, MD, nor any
family member(s), have any relevant
financial relationships to be discussed,
directly or indirectly, referred to or illustrated
with or without recognition within the
presentation.

Concussion Videos
http://www.youtube.com/watch?NR=1&v=viIKnNvzzfM
http://www.youtube.com/watch?v=NvSNMrcKR5Q
http://www.youtube.com/watch?v=Tyv4du7BTOc
http://www.youtube.com/watch?v=1mTEzQ8vBps
http://www.youtube.com/watch?v=fcGdnvhOfNg
http://www.youtube.com/watch?v=DS1Bocgpw-
M&feature=results_video&playnext=1&list=PL410E11C33BA94
A89
http://www.youtube.com/watch?v=i3mrw2eWLOo&NR=1

Background
Sports-related concussion – huge challenge in Sports Medicine
Decisions:
– sidelines
– ice rink
– heat of the battle
Pressure:
– coaches
– parents
– the player

Overview
Concussion is more complex than previously thought
Changes in normal brain physiology
– Can persist even after
symptoms apparently clear
Potential for lasting/permanent
damage
Previous management
strategies are inadequate

Definition
Definition
– A complex pathophysiological process affecting the brain, induced by
traumatic biomechanical forces
– Characterized by a rapid onset of cognitive impairment
– Concussions are often difficult to detect since most
do not lead to a loss of consciousness
or have other immediately
recognizable symptoms
– Wide range of clinical
signs/symptoms –
highly variable presentation

Pathophysiology
Linear/rotational forces of acceleration and deceleration on or within the brain
Microscopic level:
– neuron depolarization
– ion regulation
– membrane channels
– axon integrity
– glucose metabolism
– cell membrane stability
– production of oxidative free radicals
Rare to see skull fractures, cerebral edema, intracranial bleeds, and epidural/subdural hematomas

9% of all high school sports injuries vs. 5.5% in 1997
Greater participation
Athletes bigger,
stronger, faster
Greater
awareness
Concussions on Rise

“Silent Epidemic”
– 1.6-3.8 million sports related concussions/yr
– Higher incidence or recognized more?
– Can we manage concussions better and facilitate a
better outcome for our student-athletes?
– Significant advances over the past decade –
however, still a great deal we do not understand
– High risk sports: – FB, M/W soccer, M/W basketball, softball, baseball, VB
Concussion

Female Overview
Females cognitively
impaired 1.7x more
frequently than males
Females had more
adverse effects from
concussion
50% of athletes did not
report their injury
(2005)!

Youth Coaches & Concussions
McLeod et al., 2007:
– 42% thought that LOC was
required for a concussion
– 32% did not think a Grade 1
concussion required
removal from competition
(no longer use a grading
system)
– 26% would let a
symptomatic athlete return
to play (RTP)

Classifications
Many Classifications over
the years:
– Cantu (1986)
– Colorado Medical Society
(1991)
– American Academy of
Neurology (1997)
– International Consensus
Statements (2001,2004,
2008)

Cantu Classification Guidelines, 1986
Grade 1: No loss of consciousness, Post-traumatic amnesia for fewer than 30 minutes
Grade 2: Loss of consciousness for fewer than 5 minutes OR Post-traumatic amnesia for more than 30 minutes
Grade 3: Loss of consciousness for more than 5 minutes OR Post-traumatic amnesia for more than 24 hours

Colorado Medical Society Guidelines, 1991
Grade 1: No loss of consciousness, No post-traumatic amnesia, Confusion
Grade 2: No loss of consciousness, Post-traumatic amnesia, Confusion
Grade 3: Loss of consciousness of any duration

American Academy of Neurology Guidelines, 1997
Grade 1: No loss of consciousness, Concussion
symptoms for fewer than 15 minutes
Grade 2: No loss of consciousness, Concussion
symptoms for more than 15 minutes
Grade 3: Loss of consciousness of any duration

International Consensus Statements on Concussion
Historical Overview Vienna, 2001
Broad definition, individualized approach, stepwise RTP
Prague, 2004 Stressed difference in younger patients, simple vs complex
Zurich, 2008 Abandoned simple vs complex,
No RTP same day if < 18 yo,
Stressed predisposing factors (i.e. multiple concussions)
Underscored deficits can persist long after symptoms resolve
Stressed value of neuropsychological testing (ImPact)
SCAT2, pocket SCAT2, BESS assessment

Current Standard of Classification of Concussion
According to the Zurich Conference in 2008:
– Concussion grading scales should no longer be used
– Terms “simple” and “complex” no longer used
– Concussion now considered as a single entity that can be affected by various modifying factors
BOTTOM LINE – management is more
conservative!!

Definition (Consensus Statement on Concussion in Sport: 3rd International Conference on Concussion in Sport, Zurich, November 2008)
Caused by direct blow to head, face, neck, or elsewhere on the body with an “impulsive” force to the head
Results in rapid onset of short-lived neurological impairment that resolves spontaneously
May result in neuropathological changes, but acute clinical symptoms reflect functional disturbance rather than structural injury
Results in graded set of symptoms that may or may not involve loss of consciousness. Resolution of symptoms typically follows sequential course
No abnormality is seen on standard neuroimaging

Historical Perspectives
Concussion scales:
– > 25 published by 2001;
– None based on valid scientific evidence
Canadian guidelines (2000) – four R's:
– recognition,
– response,
– rehabilitation,
– return

“perhaps the most challenging aspect of managing
sport-related concussion is recognizing the injury,
especially in athletes with no obvious signs that a
concussion has actually occurred”
Exact pathophysiological changes to the brain
following concussion are not fully understood
All concussions mandate evaluation by a medical
doctor
1. Recognition

• No longer use grading scales
• Different scales, not always congruent
• Treatment was based on “Grade”
• Severity can only be determined over time
Diagnosing Concussion

Diagnosing Concussion
History
Exam
– Sideline
– Office
Radiology

History
– Witnessed injury
– Report of injury
– LOC IS NOT
NECESSARY!
– Symptoms
Diagnosing Concussion

Concussion Assessment
Assessment of acute concussion is multifactorial
Assess signs, symptoms, behavior, and abnormal brain function
Test memory
– What team are we playing?
– Who scored last?
Test cognitive functioning
– Word recall (cat, pen)
– Digit recall (say 4-2-5 backwards)
– Months in order (recall months in backward order)
Neurological exam is paramount
– Speech, eye motion, pupils, pronator drift, balance testing
– Presence of one or more of these factors indicate high probability of concussion and should necessitate removal from field
Sport Concussion Assessment Tool (SCAT)
– Quick standardized tool for concussion assessment

Sideline evaluation
(1.) ABC’s
(2.) Exclude cervical spine injury
(3.) Evaluate concussion, use standardized tools (i.e. SCAT2) if available
(4.) Do not leave the player alone – Serial monitoring for initial few hours
following injury to observe for deterioration
(5.) Player should not be allowed to return to field on day of injury

ED/Clinic Setting
Do a complete H+P
Do a comprehensive neurological exam
Monitor for worsening signs/symptoms
Obtain additional info from other sources (parents, coaches, trainers,
etc.)
Emergent neuroimaging only if there is concern for severe brain injury
or abnormality -- Usually NOT necessary !!

Neuroimaging
CT
– Study of choice
– Greater accessibility
– Good for intracranial hemorrhage, contusion, or herniation
MRI
– More sensitive and specific than CT in identifying small cerebral contusions, edema, and small non-hemorrhagic lesions
– Prohibited by: cost, availability, claustrophobia, metal hardware in body
Other imaging studies
– Functional MRI (f MRI)
– Diffusion tensor imaging (DTI)
– Positron Emission Tomography (PET)
– Single Photon Emission Computerized Tomography (SPECT)
– Near Infrared Spectroscopy (NIRS)

Signs/Symptoms
Visual changes
Balance problems
Dizziness
Confusion
Memory loss
Irritability / changes in emotion
Difficulty concentrating
Difficulty with sleep (sleep or wake)
Headache
Light sensitivity
Diagnosing Concussion

Suspected concussion: Immediate removal
Return while symptomatic may greatly increase the
risk of more severe post-concussive symptoms and a
more prolonged post-concussive course
“Second Impact Syndrome” feared but rare
Concussion = Functional brain injury – only image if
suspect a structural injury
Neuropsych assessment: demonstrated to be an
extremely valuable tool
2. Response

Plenty of rest and fluids
– Let them sleep!
– No 2 hr rule
Avoid
– aspirin
– NSAIDs
Concussion Treatment

Concussion Management
Patience is key!
Physical AND cognitive rest until symptoms resolve.
When symptomatic, restrict/prohibit physical activity and activities involving attention and concentration.
Emphasize delay in recovery if athlete resumes these activities too soon.
Do not overlook depression, anxiety, or mood disturbances.
Recovery should be based on the individual, NOT tables or guidelines.
Several factors will modify concussion management (Table 1).

Concussion Modifiers
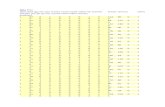
TABLE 1. Concussion Modifiers
Factors: Modifier:
Symptoms Number
Duration (>10 days)
Severity
Signs Prolonged LOC (>1 min), amnesia
Sequelae Concussive convulsions
Temporal Frequency - repeated concussions over time
Timing - injuries close together in time
‘‘Recency’’ - recent concussion or TBI
Threshold Repeated concussions occurring with
progressively less impact force or slower
recovery after each successive concussion

Concussion Modifiers (Table 1, Continued)
Factors: Modifier:
Age Child and adolescent (< 18 years old)
Co- and Pre-morbidities Migraine, depression or other mental health
disorders, attention deficit hyperactivity
disorder (ADHD), learning disabilities (LD),
sleep disorders
Medication Psychoactive drugs, anticoagulants
Behaviour Dangerous style of play
Sport High-risk activity, contact and collision sport, high sporting level

Pharmacology
Helps to manage symptoms including anxiety, depression, insomnia, and
headache
– Acute anxiety BZD’s
– Depression SSRI’s
– Insomnia BZD’s, TCA’s
– Cognitive slowing/Fatigue psychostimulants (i.e. Provigil), dopaminergic agents
(i.e. Levodopa)
– Mania/Psychosis typical/atypical antipsychotics (i.e. Risperdal)
Prior to returning to play, athlete needs to be symptom-free and off these
medications (except for antidepressants)
Initiation of these medications need close monitoring

Neuropsychological Testing
Use is heavily market driven
Provides a way to assess information relating to neurological deficits suffered post-concussion when compared to baseline neurological function
Adjunct to clinical decision making process (CAN NOT determine RTP)
No reason to test while the athlete is symptomatic
Sometimes difficult to draw accurate conclusions without a baseline test

Neuropsychological Testing
Expense ($750-$4,000) and time factor (30 min to 3 hours) limits widespread use
Recommended that trained neuropsychologists are needed to assess findings
Examples:
– Immediate Post Concussion Assessment and Cognitive Testing (ImPACT
®)
– Headminder®

General rule of thumb:
For as long as it takes for symptoms to clear, it is the same length of time before the athlete is ready to RTP
Once symptoms clear . . .
– Repeat computer test (if have baseline)
Good approach:
– Retest only asymptomatic patients
– Avoids problems with practice effects and false negatives
Neuropsychological Testing

Traditionally: Orthopedic Model
1. Phase 1: healing phase, rest, modalities
2. Phase 2: return to fxn, ROM, strength,
stability, proprioception, flexibility
3. Phase 3: return to sport, graduated increase in
sport-specific activity
3. Rehabilitation

Concussion Model
REST!!! Physical and Cognitive !!!
Symptoms aggravated by exertion (physical & cognitive)
differs from orthopedic model – absolute rest a must
fitness activity, aerobic activity, exertional ADL's
Concentration, memorization and learning can aggravate post-concussive symptoms
Rest MUST involve cognitive rest
Most difficult phase – athlete used to working through pain (needs extensive education and support)
3. Rehabilitation

Cantu Concussion Guidelines, Return to Play
Management based on first concussion:
Grade 1: Athlete may return to play if asymptomatic for one week
(if athlete is totally asymptomatic, return to play on
same day may be considered).
Grade 2: Athlete may return to play if asymptomatic for one
week.
Grade 3: Athlete may not return to play for at least one month;
athlete may then return to play if asymptomatic for one
week.

Colorado Medical Society Guidelines, Return to Play
Management based on first concussion:
Grade 1: Athlete may return to play if asymptomatic for 20 minutes.
Grade 2: Athlete may return to play if asymptomatic for one week.
Grade 3: Athlete should be transported to a hospital emergency department; athlete may return to play one month after injury if asymptomatic for two weeks.

American Academy of Neurology Guidelines, Return to Play
Management based on first concussion:
Grade 1: Athlete may return to play if asymptomatic for 15
minutes.
Grade 2: Athlete may return to play if asymptomatic for one
week.
Grade 3: Athlete should be transported to a hospital emergency
department; if athlete had brief loss of consciousness
(i.e., seconds), may return to play when asymptomatic for
one week; if athlete had prolonged loss of consciousness
(i.e., minutes), may return to play when asymptomatic for
two weeks.

International Consensus Statements on Concussion Graduated Return to Play Protocol
Step-wise process
Each step = 24 hours
Progress to next step if asymptomatic for at least 24 hours at that current level
If symptomatic, rest for 24 hours, then drop athlete down to previous asymptomatic step and try to progress again

Graduated Return to Play Protocol
TABLE 2. Graduated Return to Play Protocol
Rehabilitation Stage Functional Exercise at Each Stage of Rehabilitation Objective of Each Stage
1. No activity Complete physical and cognitive rest Recovery
2. Light aerobic exercise Walking, swimming or stationary cycling keeping Increase HR intensity, <70%
MPHR; no resistance training
3. Sport-specific exercise Skating drills in ice hockey, running drills in soccer; Add movement no head
impact activities
4. Non-contact training drills Progression to more complex training drills, eg, Exercise, coordination, and
passing drills in football and ice hockey; may start sport specific activity
progressive resistance training
5. Full contact practice Following medical clearance, participate in normal Restore confidence and
assess training activities functional skills by coaching
staff
6. Return to play Normal game play

Ongoing research…
Pediatric population
Genetic/biomarker testing
Second Impact Syndrome
Male vs. female athlete
Protective equipment (i.e.
helmets, mouthgards)

Pediatric Athlete
Not a “little” adult!
Growth and development make concussion assessment and management very difficult
Less neck and shoulder musculature less capable of transferring kinetic energy at the head throughout the body
Neurological development at risk – Ability to focus
– Sustain attention
– Memory recall
– Rapid information processing

Pediatric Athlete
No set timetable for recovery
Need to be conservative on return to play protocol
Consider extending out time of one or more steps
Emphasize cognitive rest and longer recovery period
Studies still limited in terms of the pediatric population

Genetics
Current investigations ongoing to evaluate the association of
genotypes, alleles, and genetic biomarkers to concussions
– S100B
predicts long-term disability from a head injury
– Apo E4
risk factor for Alzheimer’s
– G-219T polymorphism of ApoE promoter
increased risk for Alzheimer’s and unfavorable post-concussive
outcomes
– Tau mutation on Chromosome 17
frontotemporal dementia

Repeated Concussive Injury
http://espn.go.com/video/clip?categoryid=3060647&id=5163151
http://www.youtube.com/watch?v=f0xJT53SZqQ

Repeated Concussive Injury
Concern for Second Impact Syndrome (SIS)
– Athlete sustains head injury while still symptomatic from a previous head
injury
– Second head injury leads to metabolic disruption and loss of autoregulation
of cerebral blood supply
– Results in cerebral vascular engorgement, cerebral edema/swelling,
increased intracranial pressure, cerebral/brainstem herniation, and
ultimately, coma and death
Rare, but is of great concern in pediatric population due to immaturity
of the brain
Contact sports (i.e. football, hockey) increase risk of SIS

Repeated Concussive Injury
The Zack Lystedt Law:
– 2006 -13-year-old Zachery Lystedt, from Maple
Valley, WA, suffered a life-threatening brain injury
after he returned to play football following a hard
hit earlier in the game
– May 14 2009 - Gov. Christine Gregoire signed the
nation's toughest youth athlete return-to-play law
– Washington was the 1st State to pass concussion
legislation

The Zackary Lystedt Law
http://www.youtube.com/watch?v=llLLz6AG_-s

Gfeller-Waller Awareness Act
Matthew Gfeller died in August 2008:
– he sustained a head injury during a high school football
game in Winston-Salem
– he played for R.J. Reynolds High School
Jaquan Waller died in September 2008:
– he sustained a head injury during a high school football
game in Greenville
– He played for J.H. Rose High School
Waller suffered from Second Impact Syndrome
Gfeller died from a single concussion

Gfeller-Waller Awareness Act
NC was the 16th State to pass concussion
legislation
http://tbicenter.unc.edu/MAG_Center/gwlaw_files/gfeller_waller.pdf

Gfeller-Waller Awareness Act
Signed into law on June 16, 2011 by
Governor Purdue
Purpose: – to protect the safety of student-athletes in NC
3 major areas of focus: – education
– emergency action
– post-concussion protocol implementation, and
clearance/return to play or practice following concussion

Post-Concussion Protocol
If a student-athlete exhibits signs and symptoms consistent with
a concussion (even if not formally diagnosed), the student-
athlete is to be removed from play and is not allowed to return
to play (game, practice, or conditioning) on that day - "When in
doubt, sit them out“ !!
Student-athletes are encouraged to report their own symptoms,
or to report if peers may have concussion symptoms
Coaches, parents, volunteers, first responders, school nurse,
licensed athletic trainers (if available), are responsible for
removing a student-athlete from play if they suspect a
concussion

Post-Concussion Protocol
Following the injury, the student-athlete should be evaluated by
a qualified medical professional with training in concussion
management
It is strongly recommended that each institution seek qualified
medical professionals in the surrounding community to serve as
resources in the area of concussion management
In order for a student- athlete to return to play without
restriction, he/she must have written clearance from appropriate
medical personnel
The form that should be used for this written clearance is
posted on this website: – https://www.nchsaa.org/intranet/downloadManagerControl.php?mode=getFile&eleme
ntID=8440&type=5&atomID=11952

Take Home Points
Concussion present a complex problem
No “simple” concussions and no two concussions
are alike
Treat each athlete or patient as an individual
Education/Awareness for everyone
Baseline testing is ideal (SCAT2, SAC, BESS)
Be thorough in the initial evaluation and subsequent
follow-up

Take Home Points
Neuroimaging valid when suspicious for serious brain
injury, otherwise no imaging needed
Management is STRICT REST – physical and
cognitive
Never RTP if symptomatic
Be conservative on return to play
Be even more conservative with pediatric athletes
NO ONE returns to play same day of a suspected
concussion

“within the context of concussion, we are left
to wonder why an investment of 4 months to
rehabilitate a high ankle sprain is considered
acceptable, whereas 4 months for brain
rehabilitation is considered unacceptable”
Final Thoughts….

References
1. McCrory, P. and Meeuwisse, W. Consensus Statement on Concussion in Sport: the 3rd International Conference on
Concussion in Sport held in Zurich, November 2008. Br. J. Sports Med. 2009 (Suppl I): 43; i76-i84.
2. McCrory, P. and Johnston, K. Summary and Agreement Statement of the 2nd International Conference on Concussion in
Sport, Prague 2004. Clin. J. Sports Med: Vol 15, Number 2, March 2005, pp 48-55.
3. Aubry, M. and Cantu, R. Summary and Agreement Statement of the First International Conference in Sport, Vienna 2001.
The Physician and Sports Medicine: Vol 30, Number 3, February 2002.
4. Herring, S. and Bergfield, J. Concussion (Mild Traumatic Brain Injury) and the Team Physician: A Consensus Statement.
Official Journal of the American College of Sports Medicine, Medicine & Science in Sports & Exercise: November 2005,
pp 2012-2016.
5. Anderson, T. and Heitger, M. Concussion and Mild Head Injury. Practical Neurology 2006: Vol 6, pp 342-357.
6. Akhavan, A. and Flores, C. How should we follow athletes after a concussion?. The Journal of Family Practice: October
2005, Vol 54, Number 10.
7. Goldberg, L. and Dimeff, R. Sideline Management of Sports-related Concussions. Sports Medicine and Arthroscopy
Review: Vol 14 (4), December 2006, pp 199-205.
8. Kushner, D. Concussion in Sports: Minimizing the Risk for Complications. American Family Physician: Vol 64, Number 6,
pp 1007-1014.
9. Tator, C. Concussions are Brain Injuries and Should be Taken Seriously. Can. J. Neurol. Sci. 2009: Vol 36, pp 269-270.
10. Mayers, L. Return-to-Play Criteria After Athletic Concussion. Arch. Neurology 2008: Vol 65, Number 9, pp 1158-1161.
11. Covassin, T. and Elbin, R. Current Sport-Related Concussion Teaching and Clinical Practices of Sports Medicine
Professionals. Journal of Athletic Training: Vol 44, Number 4, August 2009, pp 400-404.
12. Davis, G.A. and Iverson, G.L. Contributions of Neuroimaging, Balance Testing, Electrophysiology, and Blood Markers to
the Assessment of Sport-related Concussion. Br. J. Sports Med 2009: Vol 43 (Suppl I), i36-i45.

References
13. Johnston, K. and Ptito, A. New Frontiers in Diagnostic Imaging in Concussive Head Injury. Clin. J. Sport Med: Vol 11, Number 3, 2001, pp 166-175.
14. Schrader, H. and Mickeviciene, D. Magnetic resonance imaging after most common form of concussion. BMC Medical Imaging 2009: Vol 9, Number 11, pp 1-6.
15. Iverson, G. Outcome from mild traumatic brain injury. Current Opinion in Psychiatry 2005: Vol 18, pp 301-317.
16. Paoli de Almeida Lima, D. and Simao Filho, C. Quality of life and neuropsychological changes in mild head trauma. Late analysis and correlation with S100B protein and cranial CT scan performed at hospital admission. Injury, Int. J. Care Injured 2008: Vol 39, pp 604-611.
17. Kristman, V. and Tator, C. Does the Apolipoprotein E4 Allele Predispose Varsity Athletes to Concussion? A Prospective Cohort Study. Clin. J. Sport Med: Vol 18, Number 4, July 2008, pp 322-328.
18. Roland Terrell, T. and Bostick, R. APOE, APOE Promoter, and Tau Genotypes and Risk for Concussion in College Athletes. Clin. J. Sport Med: Vol 18, Number 1, January 2008, pp 10-17.
19. Hutchinson, M. and Mainwaring, L. Differential Emotional Responses of Varsity Athletes to Concussion and Musculoskeletal Injuries. Clin. J. Sport Med: Vol 19, Number 1, January 2009, pp 13-19.
20. Bruce, J. and Echemendia, R. History of Multiple Self-reported Concussions is Not Associated with Reduced Cognitive Abilities. Neurosurgery: Vol 64, Number 1, January 2009, pp 100-105.
21. The ImPACT Test. Sideline ImPACT. http://www.impacttest.com/sidelineimpact.php.
22. Schatz, P. and Pardini, J. Sensitivity and specificity of the ImPACT Test Battery for concussion in athletes. Archives of Clin. Neuropsychology: Vol 21, Issue 1, January 2006, pp 91-99.
23. Cernich, A. and Reeves, D. Automated Neuropsychological Assessment Metrics Sports Medicine Battery. Archives of Clin. Neuropsychology: 22S (2007) S101-114.
24. Broglio, S and Macciochi, S. Sensitivity of the Concussion Assessment Battery. Neurosurgery: Vol 60, Number 6, June 2007, pp 1050-1058.

References
25. McCrea, M. and Barr, W. Standard regression-based methods for measuring recovery after sport-related concussion. Journal of the International Neuropsychological Society (2005): Vol 11, pp 58-69
26. Shuttleworth-Edwards, A. Central or peripheral? A positional stance in reaction to the Prague statement on the role of neuropsychological assessment in sports concussion management. Archives of Clin. Neuropsychology 2008: Vol 23, pp 479-485.
27. Guskiewicz, K. Postural Stability Assessment Following Concussion: One Piece of the Puzzle. Clin. J. Sport Med 2001: Vol 11, pp 182-189.
28. Solomon, G. and Haase, R. Biopsychosocial characterisitics and neurocognitive test performance in National Football League players: An initial assessment. Arch. of Clin. Neuropsych 2008: Vol 23, pp 563-577.
29. Boutin, D. and Lassonde, M. Neuropsychological assessment prior to and following sports-related concussion during childhood: A case study. Neurocase 2008: Vol 14, Number 3, pp 239-248.
30. Scolaro Moser, R. and Iverson, G. Neuropsychological evaluation in the diagnosis and management of sports-related concussion. Arch of Clin. Neuropsych: Vol 22, Issue 8, November 2007, pp 909-916.
31. Maroon, J. and Lovell, M. Cerebral Concussion in Athletes: Evaluation and Neuropsychological Testing. Neurosurgery: Vol 47, Number 3, September 2000, pp 659-672.
32. Grindel, S. and Lovell, M. The Assessment of Sport-Related Concussion: The Evidence Behind Neuropsychological Testing and Management. Clin. J. of Sport Med 2001: Vol 11, pp 134-143.
33. Broglio, S. and Macciochi, S. Neurocognitive Performance of Concussed Athletes When Symptoms Free. Journal of Athletic Training 2007: Vol 42, Number 4, pp 504-508.
34. Echemendia, R. and Herring, S. Who should conduct and interpret the neuropsychological assessment in sports- related concussion? Br. J. Sports Med 2009: 43 (Suppl I) pp i32-i35.
35. Putukian, M. and Aubry, M. Return to play after sports concussion in elite and non-elite athletes. Br. J. Sports Med 2009: 43 (Suppl I) pp i28-i31.
36. Cohen, J. and Giola, G. Sports-related concussion in pediatrics. Current Opinion in Pediatrics 2009: Vol 21, pp 288-293.
37. De Beaumont, L. and Theoret, H. Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain 2009: Vol 132, pp 695-708.

References
38. Covassin, T. and Swanik, C. B. Sex differences in baseline neuropsychological function and concussion symptoms of collegiate athletes. Br. J. Sports Med 2006: Vol 40, pp 923-927.
39. Covassin, T. and Schatz, P. Sex differences in neuropsychological function and post-concussion symptoms of concussed collegiate athletes. Neurosurgery 2007: Vol 61, pp 345-351.
40. Standaert, C. and Herring, S. Expert Opinion and Controversies in Sports and Musculoskeletal Medicine: Concussion in the Young Athlete. Arch Phys Med Rehabil: Vol 88, pp 1077-1079, August 2007.
41. Scolaro Moser, R. and Schatz, P. Enduring effects of concussion in youth athletes. Arch of Clin. Neuropsych 2001: Vol 17, Issue 1, January 2002, pp 91-100.
42. Field, M. and Collins, M. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. Journal of Pediatrics: Vol 42, Issue 5, May 2003.
43. Kirkwood, M. and Owen Yeates, K. Pediatric Sport-Related Concussion: A Review of the Clinical Management of an Oft-Neglected Population. Pediatrics: Vol 117, Number 4, April 2006, pp 1359-1371.
44. Ashare, A. Returning to play after concussion. Acta Paediatrica 2009: Vol 98, pp 774-776.
45. Purcell, L. What are the most appropriate return-to-play guidelines for concussed child athletes? Br. J. Sports Med 2009: Vol 43 (Suppl I) pp i51-i55.
46. Gessel, L. and Fields, S. Concussions Among United States High School and Collegiate Athletes. Journal of Athletic Training: Vol 42, Number 4, December 2007, pp 495-503.
47. Giola, G. A. and Schneider, J. C. Which symptom assessments and approaches are uniquely appropriate for paediatric concussion? Br. J. Sports Med 2009: Vol 43 (Suppl I), pp i13-i22.
48. Dick, R. W. Is there a gender difference in concussion incidence and outcomes? Br. J. Sports Med 2009: Vol 43 (Suppl I), pp i46-i50.
49. McCrory, P. Does Second Impact Syndrome Exist? Clin. J. Sport Med 2001: Vol 11, Number 3, pp 144-149.
50. Guskiewicz, K. and McCrea, M. Cumulative Effects Associated With Recurrent Concussion in Collegiate Football Players. JAMA: Vol 290, Number 19, November 19, 2003, pp 2549-2555.

References
51. McCrea, M. and Guskiewicz, K. Acute Effects and Recovery Time Following Concussion in Collegiate Football Players. JAMA: Vol 290, Number 19, November 19, 2003, pp 2556-2563.
52. Covassin, T. and Stearne, D. Concussion History and Postconcussion Neurocognitive Performance and Symptoms in Collegiate Athletes. Journal of Athletic Training 2008: Vol 43, Number 2, pp 119-124.
53. Miller, G. A Late Hit for Pro Football Players. Science: Vol 325, August 7, 2009, pp 670-672.
54. Singh, G. D. and Maher, G. Customized mandibular orthotics in the prevention of concussion/mild traumatic brain injury in football players: a preliminary study. Dental Traumatology: Vol 25, Issue 5, July 9, 2009, pp 515-521.
55. Levy, M. and Ozgur, B. Birth and Evolution of the Football Helmet. Neurosurgery: Vol 55, Number 3, September 2004, pp 656-662.
56. Levy, M. and Ozgur, B. Analysis and Evolution of Head Injury in Football. Neurosurgery: Vol 55, Number 3, September 2004, pp 649-655.
57. Benson, B. W. and Hamilton, G. M. Is protective equipment useful in preventing concussion? A systematic review of the literature. Brit. J. Sport Med 2009: Vol 43 (Suppl I), pp i56-i67.













![[MS-RTP]: Real-time Transport Protocol (RTP) …...Release: July 24, 2018 [MS-RTP]: Real-time Transport Protocol (RTP) Extensions Intellectual Property Rights Notice for Open Specifications](https://static.fdocuments.in/doc/165x107/5ecb4ebafdd0d04e1c3c1812/ms-rtp-real-time-transport-protocol-rtp-release-july-24-2018-ms-rtp.jpg)