Community Urology Plenary Education Meeting December 2011 Christof Kastner Consultant Urologist...
-
Upload
brooke-christopherson -
Category
Documents
-
view
214 -
download
0
Transcript of Community Urology Plenary Education Meeting December 2011 Christof Kastner Consultant Urologist...

Community UrologyPlenary Education Meeting
December 2011
Christof Kastner Consultant Urologist Addenbrooke’s Hospital
Mark Brookes GP Nuffield Road Surgery, Cambridge
Co-chairsUrology Community Partnership, Cambs
Aaron Horner Coordinator

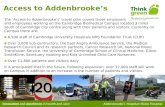
Urology 2010: Designed around the Patient
Outpatient Innovation
Community Urology
One-StopSpecialist
Clinics Follow-up Clinics
PSAFollow-up
Continence
Male LUTS

ProtecT (UK)
Results expected 2018
ERSPC (Europe)
screening reduces CaP death by 20%
BUT: screen 1400 + treat 48 to prevent 1 death
PLCO (US)
no difference in death rate
Screening forProstate Cancer

Assessment(prioritise the order according to presentation)
EXCLUDE INIDCATORS FOR CANCER:ABNORMAL PSA OR RECTAL EXAMINATION
HAEMATURIA
History of presentation including IPSS / QoL Voiding diary
Medical history identify other medical conditions which can cause symptomsMedication including herbal and over-the-counter medicines Physical examination in specific abdomen, external genitalia and digital rectal examination
Blood Creatinine (definitely if there is clinical indication of obstructive renal failure)
PSA - Give information, advice and time before offering - Consider age / life expectancy / UTI - PSA patient information leaflet Urine Dipstick +/- MSU
Christof Kastner - Consultant Urologist -
Screening forProstate Cancer
Male patients presenting with
Haematuria, LUTS and UTIs

PSA FU
Follow-up groups
•Secondary Care
•Primary Care under LES
•Normal biopsy BUT risk above normal population
•Low risk Dx, controlled 3 years after radical treatment
(up to seven years usually)
•Low to intermediate risk Dx, controlled palliative treatment
•Primary Care for Screening and Re-assurance
•Normal biopsy BUT risk as normal population

Discharge to Primary Care PSA Follow-up
Dear Dr xxxx
We recently reviewed your patient in clinic and agreed for future PSA follow up to take place in primary care, as described in the LES agreement. Details are as follows:
Yours sincerely
Mr x xxxx (Consultant)
Encl.: PSA Follow up information for GPs (GP copy only)Also available on: camurology.org.uk/general_practitioners/info_sheets_gp.php
Copy: (patient name & address)
Please acknowledge receipt of this letter, confirming the continuation of care at your practice to: [email protected] For advice on patients on the 'LES PSA FU’ scheme please email: [email protected]
Discharge letter
Diagnosis Grade Stage PSA / presentation
CA prostate Gleason 3+4 T2a 9.3
Treatment / Biopsy Year Benign Biopsy / PSA nadir
RALP 2007 0.01
Issues PSA / discharge
ED 0.01
Recommendation
FU interval Re-referral criteria
6-monthly (super-sens. PSA)PSA >0.02 or if symptomatic


Patient identified by consultant as appropriate for PSA follow-up in community (see criteria)
Community follow-up offered
Follow up stays in secondary careStructured discharge letter to GPGP and Patient information sheet
Patient held record
Patient entered onto RegisterRecall set up
PSALUTS (IPSS)
Weight (looking for loss)Bone pain
Confirmation to secure email
3/12 return to Urology department
Patient entered onto database
Results entered on databaseAudit
6/12
No concerns – recall
Abnormal
Meets criteria set out in structured discharge letter
New referral to discharging specialitymarked PSA f/u, seen as urgent
Advice via secure email address

– Primary Care PSA FU• Stable prostate cancer after treatment (~3y)• Selected PSA monitoring after normal diagnostics
– Detailed information about diagnosis, treatment and follow-up advice given on discharge
– Consider effects of finasteride and dutasteride and UTIs
– PSA FU advice via email • [email protected] – Addenbrookes patients
– Practices to confirm receipt of referralto collect and return data on visits (next quarters data due by 15th Jan 12)
– Audit shows dangerous lack of control / insight• Specialist assurance impossible• Consideration of halting and modification of community follow-up
Key MessagesPSA Follow-Up

Continence

Causes include - UTI, weak pelvic floor muscles, prolapse, atrophy, detrusor muscle dysfunction, obstruction, incompetent sphincter, urethral diverticulum, fistula, congenital lesion, cognitive impairment
Causes include - UTI, weak pelvic floor muscles, prolapse, atrophy, detrusor muscle dysfunction, obstruction, incompetent sphincter, urethral diverticulum, fistula, congenital lesion, cognitive impairment
Fast track 2 week referral to
appropriate specialty
Fast track 2 week referral to
appropriate specialty
Suspected CAHaematuriaPalpable mass
Red flags Refer direct to secondary care
Red flags Refer direct to secondary care
Specialist Continence ServiceSpecialist Continence Service
DischargeDischarge
GP/PN/midwife notes FEMALE URINARY INCONTINENCE
NO
NO
YES
Information sources
Review Symptoms improved?
Review Symptoms improved?
1st line 2 months oxybutinin (immediate release) but be aware of risk of side effects in >65s 2nd line M/R or T/D oxybutininIf no success then try alternatives
Consider vaginal oestrogen if atrophy and OAB Cambridgeshire formulary NICE
1st line 2 months oxybutinin (immediate release) but be aware of risk of side effects in >65s 2nd line M/R or T/D oxybutininIf no success then try alternatives
Consider vaginal oestrogen if atrophy and OAB Cambridgeshire formulary NICE
Ongoing symptoms
Consider using concurrent medication on advice of community continence service
Blue: GP
Green: Community Continence Service
Orange: Secondary Care
COMMUNITY CONTINENCE SERVICE (OR ACCREDITED ALTERNATIVE PROVIDER)
refer using proforma:Word, EMIS PCS, SystmOne, Vision
Assessment, advice, supervised pelvic floor exercises 3/12 and/or 6/52 bladder training
COMMUNITY CONTINENCE SERVICE (OR ACCREDITED ALTERNATIVE PROVIDER)
refer using proforma:Word, EMIS PCS, SystmOne, Vision
Assessment, advice, supervised pelvic floor exercises 3/12 and/or 6/52 bladder training
Establish predominant symptom (stress, urge or mixed)History and exam (abdo, neurol, pelvic) including dipstix urine.
Bladder diary for 3 days.
Establish predominant symptom (stress, urge or mixed)History and exam (abdo, neurol, pelvic) including dipstix urine.
Bladder diary for 3 days.
YES
Advice for all patients: Lifestyle advice, bladder diary assessment, pelvic floor exercises &
bladder training. Patient Info: Female Bladder Health
Advice for all patients: Lifestyle advice, bladder diary assessment, pelvic floor exercises &
bladder training. Patient Info: Female Bladder Health
Review 6 weeksReview 6 weeksPersistence
Choice of provider on proformaDischargeDischargeSymptoms Improved
StressStress MixedMixed UrgeUrge
Treat predominant
symptom
Treat predominant
symptom
Review 4-8 weeksSymptoms improved?
Review 4-8 weeksSymptoms improved?
Consider stopping drugs after 3-6 months
Consider stopping drugs after 3-6 months
Please forward any feedback on this pathway to [email protected]

• Key Messages
– Treatment flowchart available on various websites (GPConnect, CamUrology, CATCH)
– [All referrals initially to Community Continence]
– Use ‘Life style’, ‘bladder training’ and ‘PFE’ before drugs
– Collaboration between GP, Cont service and Spec– Secondary Care referral only after failed community
treatment
Continence

Underlying cause treated(constipation/UTI)
Review medication
Yes NoPASS FAIL
Offer ISC as alternative to catheter
PASS
without previous symptoms
Treatment naive
GP review LUTS assessment
All FAIL (unless Elderly / frail etc, GP to weigh up)PASS (unless see left)
TWOC
postGA retention(other secondary care)
TWOC request from secondary
care Urology
Urology Outpatients
(Refer using LUTS proforma)
Bladder scanBladder scan
Comfortable voiding?Post void residual <300ml?
Catheter removed by D/N or GPVoiding volumes x3
Catheter removed by D/N or GPVoiding volumes x3
Confirm date & time for bladder scan with CCS
Same day
Orange = UrologyBlue = GPGreen = Continence service
Pathway 2+TWOC
Pathway 2PAINFUL RETENTION
Prescribe α-blockerfor at least 2 days prior to TWOC
Follow plan given in discharge/clinic
letter
Back to initial page
Trials without catheter

• Key Messages
– All Male TWOCs require a PVR scan• Detection of otherwise unknown chronic retention• Reduction of emergency admissions for UTI and renal failure
– Book via District nurse– District nurse to liaise with Continence service– Availability within a week– PVR to be done within 24h
Trials without catheter

Lower Urinary Tract Symptoms (LUTS)

Normal
Anatomy of BPHBPH
Hypertrophied detrusor muscle
Obstructed urinary flow
Prostate
Bladder
Urethra
Adapted from Kirby RS et al. Benign Prostatic Hyperplasia.Health Press 1999

LUTSSymptom type Symptom
Voiding Weak urinary stream
Prolonged voiding
Abdominal straining
Hesitancy
Intermittency
Incomplete bladder emptying
Storage Frequency
Nocturia
Urgency / Urge incontinence
Associated symptoms
Dysuria
Haematuria
HaematospermiaLepor H (ed). Prostatic Diseases WB Saunders 2000: 127–142
Abrams P. BMJ 1994; 308: 929-930

International Prostate Symptom Score (IPSS)*
Not at allLess than one time in five
Less than half the time
About half the time
More than half the time
Almost always
Your Score
Incomplete emptyingIn the past month, how often have you had a sensation of not emptying your bladder completely after you finish urinating?
0 1 2 3 4 5
Frequency 0 1 2 3 4 5
Intermittency 0 1 2 3 4 5
Urgency 0 1 2 3 4 5
Weak Stream 0 1 2 3 4 5
Straining 0 1 2 3 4 5
Nocturia 0 1 2 3 4 5
TOTAL SCORE (MAX 35)
* The IPSS also includes a ‘question 8’ which asks about the patients overall quality of life

Current treatments
Behavioural / Lifestyle
Pelvic Floor Exercises / Bladder training
Alpha-blockers
5-alpha-reductase inhibitors (5ARIs)
Anticholinergics [not covered in this presentation]
Combination therapy
Surgery HoLEP / TURP[not covered in this presentation]
Recommended?
European Association of Urologists BPH Guideline. 2004
√
√
√
√
√
√
√

Lifestyle and Exercises
• Drinking– Avoid all caffeinated drinks– Avoid other drinks (fizzy, blackcurrant, alcohol)– Focus drinking to little impact times of the day
• Pelvic Floor Exercises
• Bladder Training(NICE: ‘both supervised’)

Alpha blockers
Alpha blockers
Act by relaxing smooth muscle within the prostate and the bladder neck

Alpha-blockers
European Association of Urologists BPH Guideline. 2004
• Rapid symptom relief
• Generally well tolerated (side effects including dizziness, erectile dysfunction, aesthenia and postural hypotension)
• No effect on prostate volume
• Do not reduce the overall long-term risk of AUR or surgery

5α-Reductase Inhibitors (5ARIs)
5ARIs
Act by ‘shrinking’ the prostate by means of androgen deprivation

5ARIs
McConnell JD et al. NEJM 1998; 338: 557–563Roehrborn CG et al. Urology 2002; 60: 434–441
• Improvement in BPH symptoms• Reduction in prostate volume• Reduction in risk of AUR and
surgery• Generally well tolerated
(side effects including impotence, ejaculation disorders, gynaecomastia )
• Maximal symptom improvement may take a few months to achieve

Men presenting to GPswith
LUTS (+/- pelvic pain) Painful retentionPalpable bladder Nocturnal enuresis / Nocturnal incontinence UTI
Assessment
EXCLUDE INDICATORS FOR CANCER:ABNORMAL PSA OR RECTAL EXAMINATION
HAEMATURIA
Elevated age-related PSA
Abnormal DRE
Haematuria
Previous de-obstructing surgery
>1 UTI (MSU proven)
Indicators for chronic retention: -Renal impairment suspected due to lower urinary tract dysfunction -Palpable bladder -Nocturnal enuresis -Nocturnal incontinence
Urology OutpatientsPlease ensure all info provided
Painful retention
Pathway 2Painful retention
Bothersome LUTS
Treat predominant symptom
Pathway 3ABothersome LUTS
Predominantly Voiding
2-week-ruleGuidelines
Routine / Urgent
Pathway 1Chronic retention
Pathway 2+TWOC
Pathway 3BBothersome LUTS
Predominantly Storage &
nocturnal polyuria
Please forward any feedback on this pathway to [email protected]
Orange = UrologyBlue = GPGreen = Continence service
HIGH RISK LOW RISKSuitable for GP management
on an individual basis

Assessment(prioritise the order according to presentation)
EXCLUDE INIDCATORS FOR CANCER:ABNORMAL PSA OR RECTAL EXAMINATION
HAEMATURIA
History of presentation including IPSS / QoL Voiding diary
Medical history identify other medical conditions which can cause symptomsMedication including herbal and over-the-counter medicines Physical examination in specific abdomen, external genitalia and digital rectal examination
Blood Creatinine (definitely if there is clinical indication of obstructive renal failure) PSA - Give information, advice and time before offering - Consider age / life expectancy / UTI - PSA patient information leaflet Urine Dipstick +/- MSU
Please forward any feedback on this pathway to [email protected]

PSA < 1.4 and prostate < golf ball
PSA >1.4 or prostate > golf ball
Persistence
6/12
α-blocker α-blockers & 5-ARI
Improvement
Re-assess at 6/52
Pathway 3ABOTHERSOME LUTS
Predominantly VOIDING( also known as obstructive symptoms )
Lifestyle advicePatient Info: Male LUTS
DischargeImprovement
Persistence
Re-assessat 8/52
with IPSS
Consider discharge
Bothersome= patient feels impact of symptoms justifies the side-effects of treatment
Improvement = improved IPSS/QoL + patient happy
Part-response, residual Storage symptoms
keep on α-bl / 5ARIPathway 3B
STORAGE LUTSFREQUENCY -
URGENCY - NOCTURIA
Urology Outpatients
Ensure all info provided(Refer using LUTS
proforma)
Back to initial pagePlease forward any feedback on this pathway to [email protected]
Orange = UrologyBlue = GPGreen = Continence service
Please use the PCT formulary to choose an appropriate α-blocker, 5-ARI or combinations. Consider 5ARI take effect only after ~3-4 months and that PSA measurements after 6 months of 5-ARI will be 50% less than the initial value. (available 5ARI: finasteride, dutasteride, also available as fixed dose combination with tamsulosin [Combodart] ).

• Key Messages
– NICE supports medical treatment in the community with less need of diagnostic tests
– Treatment flowchart available on various websites (GPConnect, CamUrology, CATCH)
– Use proforma to optimise the handover of gathered clinical information
– Drop in referral numbers by 25%– Better content of referral letters / use of proforma– Use of pathway in peer review of referrals– Few rejections required
Lower Urinary Tract Symptoms (LUTS)

• Key Messages
– Collaboration results inmeasurable benefits to patients, GPs, Urology departments, commissioners and the health economy as a whole
– Some organisations lack/lacked commitment, integrity and reliability– Individuals involved made it work
– Continued education and collaboration of clinicians crucial and making it worthwhile
– Promissing signs that PCT / CCS will make definite commitment– West Essex (Uttlesford) may join in some form– Other C&B providers consider joining (Cambridge Urology Partnership @
Nuffield)
– Other potential projects:• Haematuria assessment in the community• ED
Community Urology Partnership

Your comments, please