Clinical Journal of Hypertension · 2020-02-01 · EDITOR-IN-CHIEF Dr. Siddharth N. Shah RNI No....
Transcript of Clinical Journal of Hypertension · 2020-02-01 · EDITOR-IN-CHIEF Dr. Siddharth N. Shah RNI No....

EDITOR-IN-CHIEF
Dr. Siddharth N. Shah
RNI No. MAHENG 14164
www.hsindia.org
OFFICIAL PUBLICATION OF
ClinicalJournal of Hypertension
APRIL-SEPTEMBER 2019 VOL. NO. 3 ISSUE NO. 2 & 3Mumbai Published on 16th of September, 2019
Price : Rs. 20
INDIAN GUIDELINES ON HYPERTENSION-IV
ESTD : 8192

2 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Editorial Board
Editor-in-Chief
Siddharth N. Shah
Associate Editors
Falguni Parikh § Shashank R. Joshi § N.R. Rau § G.S. Wander
Assistant Editors
Nihar P. Mehta § Dilip Kirpalani
Editorial Board
M.M. Bahadur § Amal K. Banerjee § R.K. Bansal § A.M. Bhagwati § Aspi R. Billimoria Shekhar Chakraborty § R. Chandnui § R.R. Chaudhary § M. Chenniappan Pritam Gupta § R.K. Jha § Ashok Kirpalani § Girish Mathur § Y.P. Munjal
A. Muruganathan § K.K. Pareek § Jyotirmoy Paul § P.K. Sashidharan N.P. Singh § R.K. Singhal § B.B. Thakur § Mangesh Tiwaskar § Trupti Trivedi § Agam Vora
Ex-Officio
Hon. Secretary General
B.R. Bansode
Printed, Published and Edited by Dr. Siddharth N. Shah on behalf of Hypertension Society India, Printed at Shree Abhyudaya Printers, Unit No. 210, 2nd Floor, Shah & Nahar Indl. Estate, Sitaram Jadhav Marg, Sun Mill Compound, Lower Parel, Mumbai 400 013 and Published from Hypertension Society India. Plot No. 534-A, Bombay Mutual Terrace, Sandhurst Bridge, 3rd Floor, Flat No.12, S.V.P. Road, Grant Road, Mumbai 400 007.
Editor : Dr. Siddharth N. Shah

3 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
LIST OF MEMBERS I.G.H. - IV (2019) .............................................................. 5 I.G.M.H. - I (2001) ............................................................ 8 I.H.G. - II (2007) ............................................................... 8
PREAMBLE ........................................................................ 9
WHAT IS NEW IN INDIAN GUIDELINES ON HYPERTENSION - IV ...................................................10
DEFINITION AND CLASSIFICATION Definition .........................................................................11 Classification ...................................................................11
EPIDEMIOLOGY OF HYPERTENSION Global ...............................................................................12 National ............................................................................12
MEASUREMENT OF BLOOD PRESSURE Clinic Measurement (Office Blood Pressure
Measurement) .................................................................16 Precautions ......................................................................16 Home Blood Pressure Measurement ........................16 Ambulatory Blood Pressure Measurement ..............17 Pulse Pressure .................................................................17
EVALUATION Medical History ..............................................................18 Physical Examination......................................................18 Laboratory Investigations .............................................18 Factors Influencing Risk ................................................19
MANAGEMENT OF HYPERTENSION Goals of Therapy ............................................................20 Management Strategy ....................................................20 Non-pharmacologic Therapy .......................................20 Pharmacologic Therapy .................................................22
Contents: Indian Guidelines on Hypertension-IV (2019)
Antihypertensive Drug Combinations ......................25 Drug Interactions ...........................................................26 Maintenance and Follow-up of Therapy ....................27
Associated Therapies .....................................................27
Newer Modalities ...........................................................27
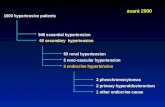
SECONDARY HYPERTENSION ................................28
COMPLICATIONS ........................................................31
HYPERTENSION IN SPECIAL SITUATIONS
Hypertension with Diabetes Mellitus ........................33
Hypertension with Cerebrovascular Disease ..........33
Hypertension in Women ..............................................34
Hypertension in Pregnancy ..........................................34
Hypertension in the Elderly .........................................35
Isolated Systolic Hypertension ...................................35
Orthostatic Hypotension .............................................36
Hypertension with Congestive Cardiac Failure ......36
Hypertension with Atrial Fibrillation .........................36
Hypertension with Chronic Obstructive Pulmonary Disease ........................................................37
Hypertension with Coronary Artery Disease .........37
Hypertension with Dyslipidaemia ..............................37
Hypertension with Obesity and Metabolic Syndrome .........................................................................37
Hypertension with Obstructive Sleep Apnea (OSA) ................................................................................38
Resistant Hypertension ................................................38
ABBREVIATIONS ..........................................................39
REFERENCES ..................................................................41
Vol. 3 • Issue No. 2 & 3 • April-September 2019
Official Publication of Hypertension Society IndiaEditor-in-Chief: Siddharth N. Shah
clinical
Journal of Hypertension

4 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Governing Body
Hon. PatronsAspi R. Billimoria (Mumbai) • N.R. Rau (Udupi)
President Executive Chairman Ashok Kirpalani (Mumbai) Siddharth N. Shah (Mumbai)
President - Elect Past President R. Chandni (Calicut) P.K. Sasidharan (Calicut)
Vice PresidentsR.R. Chaudhary (Patna) • R.K. Jha (Indore)
Secretary General Jt. Secretaries B.R. Bansode (Mumbai) Santosh B. Salagre (Mumbai) • Anita Jaiswal – Ektate (Mumbai)
TreasurerAshit M. Bhagwati (Mumbai)
Chairman: Research CommitteeGurpreet S. Wander (Ludhiana)
Editor : Clinical Journal of HypertensionSiddharth N. Shah (Mumbai)
Chairman: Epidemiology CommitteeA. Muruganathan (Tirupur)
MembersK.G. Sajeeth Kumar (Kozhikode) • P.K. Sinha (Gaya) • Shibendu Ghosh (Kolkata)
Dilip Kirpalani (Mumbai) • Nihar P. Mehta (Mumbai) • Amit Saraf (Mumbai)
MembersM. K. Parashar (Jabalpur) • Ashok Taneja (Gurgaon)

5 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
List of Members – Indian Guidelines on Hypertension-IV (2019)Core Committee
ConvenorDr. Siddharth N Shah, Mumbai
Members
Dr. Prabha Adhikari, Mangalore Dr. AK Agarwal, New DelhiDr. Navneet Agarwal, Gwalior Dr. SK Agarwal, Noida Dr. Sanjay Kumar AgarwalDr. Sharad Agarwal, Bilaspur Dr. Ishtiaq Ahmed, Bengaluru Dr. V Amuthan, MaduraiDr. Jayant Antani, Gulbarga Dr. YJ Anupama, Shimoga Dr. Parneesh Arora, Noida Dr. S Arulrhaj, Tuticorin Dr. PK Asokan, CalicutDr. P Ramesh Babu, Vijayawada
Dr. M Badgandi, Bengaluru Dr. Ananda Bagchi, Kolkata Dr. Smrati Bajpai, MumbaiDr. Samar Kumar Banerjee, Kolkata Dr. Manish Bansal, GurgaonDr. NK Bansal, JabalpurDr. Rajinder K Bansal, LudhianaDr. SB BansalDr. BR Bansode, Mumbai Dr. Ashok K Barat, Jabalpur Dr. MP Baruah, Guwahati Dr. M Basavaraj, Gulbarga Dr. A Battacharya, Bengaluru Dr. Jai Bhagwan, Gurgaon
Dr. Aspi R Billimoria, MumbaiDr. Sandhya A Kamath, MumbaiDr. M Maiya, Bangalore
Dr. Sukumar Mukherjee, KolkataDr. YP Munjal, New DelhiDr. GS Wander, Ludhiana
Dr. Ashit M Bhagwati, Mumbai Dr. Suman Bhandari, New Delhi Dr. Anil Bhansali, Chandigarh Dr. VK Bharadwaj, Jabalpur Dr. Atul Bhasin, New DelhiDr. PC Bhattacharjee, Guwahati Dr. Neil Bordoloi, Guwahati Dr. Eric D Borges, Mumbai Dr. Sandeep Budhiraja, New DelhiDr. RM Chhabra, New DelhiDr. DS Chafekar, Nasik Dr. Sekhar Chakraborty, SiliguriDr. AB Chandorkar, Pune Dr. Naval Chandra, Hyderabad
Reviewers
Dr. VK Joglekar, MumbaiDr. VR Joshi, MumbaiDr. Shashank R Joshi, MumbaiDr. Anup Khetan, BangaloreDr. Ashok Kirpalani, MumbaiDr. Vrinda Kulkarni, MumbaiDr. Saumitra Kumar, KolkataDr. Manoj Lodha, KolkataDr. Vikram Londhey, MumbaiDr. NP Misra, BhopalDr. V Mohan, ChennaiDr. PP Mohanan, ThrissurDr. Isaac C Moses, CoimbatoreDr. Milind Y Nadkar, MumbaiDr. G Narsimulu, HyderabadDr. Kashninath Padhiary, CuttackDr. Manotosh Panja, KolkataDr. KK Pareek, Kota Dr. Falguni Parikh, Mumbai
Dr. A Muruganathan, TirupurDr. M Agrawal, MumbaiDr. Amal Kumar Banerjee, Howrah Dr. Sunip Banerjee, KolkataDr. Anil Bhoraskar, MumbaiDr. K Sarat Chandra, HyderabadDr. AK Chauhan, BareillyDr. AR Chogle, MumbaiDr. Mrinal Kanti Das, Kolkata Dr. LA Gauri, BikanerDr. Aspi F Golwalla, MumbaiDr. KC Goswami, New DelhiDr. RK Goyal, AjmerDr. SK Goyal, KotaDr. RB Gulati, PuneDr. KL Gupta, Chandigarh Dr. Rohini Handa, New DelhiDr. S Jalal, SrinagarDr. Vivekanand Jha, Hyderabad
Dr. MM RajapurkarDr. YSN Raju, HyderabadDr. Devanu Ghosh Roy, KolkataDr. Banshi Saboo, Ahmedabad Dr. BK Sahay, HyderabadDr. GS Sainani, MumbaiDr. Ashok Sheth, New DelhiDr. Pankaj Singh, BangaloreDr. Rajeev Soman, PuneDr. MP Srivastava, New DelhiDr. Shyam Sunder, VaranasiDr. Mangesh Tiwaskar, Mumbai Dr. Trupti Trivedi, MumbaiDr. Rajesh Upadhyay, DelhiDr. AR Vijaya Kumar, CoimbatoreDr. Agam Vora, MumbaiDr. ME Yeolekar, Mumbai
List of Contributors
Dr. Nihar Mehta, Mumbai

6 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Dr. Sharad Chandra, LucknowDr. S Chandrasekharan, Chennai Dr. Sujit Chandratre, Nashik Dr. Shashi Shekhar Chatterjee, PatnaDr. Anil Chaturvedi, Delhi Dr. Maj. Gen. VP Chaturvedi, VSM New DelhiDr. Rajib R Choudhary, Patna Dr. MPS Chawla, New DelhiDr. HK Chopra, New DelhiDr. SN Chugh, Haryana Dr. Surrender Chugh, New Delhi Dr. Jamshed Dalal, Mumbai Dr. Ashok Kumar Das, Pondicherry Dr. DR Das, Cuttack Dr. Sambit Das, Bhubaneshwar Dr. Sidhartha Das, Cuttack Dr. Arup Dasbiswas, Kolkata Dr. Tarunkumar H Dave, Ahmedabad Dr. PK Deb, Kolkata Dr. Narayan Deogaonkar, NasikDr. Nagaraj Desai, Bengaluru Dr. Sharad N Deshmukh, Nagpur Dr. Niteen V Deshpande, NagpurDr. Air Mar S K Dham, Gurgaon Dr. Sima Duttaroy, Kolkata Dr. Sanjeev Pathak, Ahmedabad Dr. NY Fulara, Mumbai Dr. Ganapthy, Bengaluru Dr. Dhiman Ganguly, Kolkata Dr. SB Ganguly, KolkataDr. Sandeep Garg, DelhiDr. Nilesh Gautam, Mumbai Dr. Shibendu Ghosh, HooghliDr. Soumitra Ghosh, Kolkata Dr. Udas Ghosh, KolkataDr. Anupam Goel, New DelhiDr. G Goel, Faridabad Dr. A Gogia, Delhi Dr. Gokulnath, Bengaluru Dr. Anant G Gore, Mumbai Dr. Biju Govind, Vijayawada Dr. Anil Grover, Bathinda Dr. Santanu Guha, Kolkata Dr. PD Gulati, New Delhi Dr. Amit GuptaDr. Bhupendra Gupta, Delhi Dr. NK Gupta, Kota Dr. Pritam Gupta, Delhi
Dr. Rajeev Gupta, Jaipur Dr. Rakesh Gupta, DelhiDr. SB Gupta, Mumbai Dr. Vitull K Gupta, BathindaDr. KC GurudevDr. BM Hegde, Mangalore Dr. JS Hiremath, Pune Maj. Gen. (Dr.) AK Hooda, New DelhiDr. Bomi Icchaporia, Mumbai Dr. Sanjiv Indurkar, Aurangabad Dr. Shobha M Itolikar, MumbaiDr. Chakko JacobDr. Piyush Jain, New DelhiDr. Praveen Jain, Jhansi Dr. K Jaiswani, Akola Dr. Tarun Jaloka, Chinchwad Dr. Charu K Jani, MumbaiDr. Jayadeb, Vijayawada Dr. PB Jayagopal, Palakkad Dr. B Jayanti, Hyderabad Dr. NN Jha, Delhi Dr. DK Jhamb, New DelhiDr. Ajit Joshi, Kolhapur Dr. Akhil Joshi, Kota Dr. Arun Joshi, Nainital Dr. MA Kabeer, Chennai Dr. P Kamath, Mangalore Dr. S Sreenivasa Kamath, KochiDr. PS Karmakar, KolkataDr. Niteen Karnik, MumbaiDr. Rajiv Karnik, Mumbai Dr. VK Katyal, Rohtak Dr. Upendra Kaul, New Delhi Dr. Satish Kumar Kaushik, Udaipur Dr. Prafulla G Kerkar, Mumbai Dr. Vinod Khaindait, Nagpur Dr. Abdul Wahid KhanDr. Amal Kumar Khan, KolkataDr. Asit Khanna, Ghaziabad Dr. Narendra Nath Khanna, New DelhiDr. AK Khera, New DelhiDr. SB Khurana, Ludhiana Dr. HS KohliDr. Kunal Kothari, Jaipur Dr. Dilip Kirpalani, MumbaiDr. NC Krishnamani, New DelhiDr. Shriram V Kulkarni, KhopoliDr. Om Kumar
Dr. Dayanand K Kumbla, Thane Dr. Vivek KuteDr. Udai Lal, HyderabadDr. Shailesh Lodha, Jaipur Dr. RK Madhok, Jaipur Dr. Mahesh, Bengaluru Dr. PK Maheshwari, AgraDr. Sanjiv Maheshwari, Ajmer Dr. VD Maheshwari, Jaipur Dr. Biswakes Majumdar, Kolkata Dr. (Col ) SK Malani, Kolkata Dr. CN Manjunath, Bengaluru Dr. PC Manoria, Bhopal Dr. Harshwardhan Mohan Mardikar, Nagpur Dr. Umesh Masand, Indore Dr. Samuel K Mathew, Chennai Dr. Girish Mathur, Kota Dr. Anirban Mazumdar, Kolkata Dr. Chandra Bhan Meena, JaipurDr. Anand Meenawat, Jodhpur Dr. MM Mehndiratta, New DelhiDr. Sudhir Mehta, JaipurDr. SK Mishra, Brahampur Dr. Shishu Shankar Mishra, CuttackDr. Sundeep Mishra, New Delhi Dr. Trinath Kumar Mishra, BerhampurDr. Aditya Prakash Misra, New DelhiDr. JK Mitra, RanchiDr. MK Mitra, LucknowDr. A Mittal, Delhi Dr. SR Mittal, Ajmer Dr. Soura Mookerjee, KolkataDr. K Mugundhan, ChennaiDr. AK Mukherjee, KolkataDr. Supriyo Mukherjee, Samastipur Dr. J Mukhopadhyay, KolkataDr. Pramod Mundada, Nagpur Dr. Susil C Munsi, Mumbai Dr. BG Muralidhara, Bengaluru Dr. Nitish Naik, New DelhiDr. S Narendra, Hubli Dr. CL Nawal, JaipurDr. NS Neki, Amritsar Dr. Shoaib F Padaria, Mumbai Dr. Prem Pais, Bengaluru Dr. Jyotirmoy Pal, Talbukur Dr. V Palaniappen, Guzliamparai, Dindigul, TNDr. AK Pancholia, Indore

7 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Dr. D Pande, DelhiDr. Prabhat Pandey, DurgDr. Ghan Shyam Pangtey, New DelhiDr. V Parameshvara, Bengaluru Dr. (Col ) SK Parashar, Noida Dr. Shivraj Pataria, Mumbai Dr. Vijay Pathak, Jaipur Dr. CB Patil, Bengaluru Dr. NL Patney, Agra Dr. Milind Patwardhan, Sangli Dr. Basant Pawar, Ludhiana Dr. Amar Pazare, MumbaiDr. Munish Prabhakar, GurgaonDr. Anupam Prakash, New DelhiDr. VS Prakash, Bengaluru Dr. MR Prasad, Belgaum Dr. Narayan PrasadDr. Col H S Pruthi, Panchkula Dr. Abhay Narain Rai, Gaya Dr. Alok Rai, Raipur Dr. Madhukar Rai, Varanasi Dr. Rajesh Rajput, New Delhi Dr. M Rajsree, Karamnagar Dr. T Ravi RajuDr. Y Sathyanarayana Raju, Hyderabad Dr. Devi Ram, PurniaDr. GD Ramchandani, KotaDr. A Ramachandran, Chennai Dr. S Ramakrishnan, New DelhiDr. PG Raman, Indore Dr. J Ramdash, Hyderabad Dr. B Ramesh, Bengaluru Dr. Gadepalli Ramesh, SecunderabadDr. SS Ramesh, Bengaluru Dr. Anish Chanda Rana, Ahmedabad Dr. AS Chandrasekhar Rao, BengaluruDr. BP Guru Raja Rao, Bengaluru Dr. B Rao, Vizag Dr. J Shivkumar Rao, SecunderabadDr. PK Rao, Karamnagar Dr. RV Prasad Rao, Vijayawada Dr. Manish RathiDr. AG Ravikishore, Bengaluru Dr. Saumitra Ray, Kolkata Dr. KS Reddy, Guntur
Dr. BB Rewari, New DelhiDr. SM Roplekar, AurangabadDr. Satyanarayan Routray, Cuttack Dr. DK Roy, Durgapur Dr. Debabrata Roy, KolkataDr. Mrinal K Roy, Kolkata Dr. SM Raut Roy, Cuttack Dr. Sanjeeb Roy, Jaipur Dr. Deepak Saboo, Bhavnagar Dr. Lt. Gen. YP Sachdev, New DelhiDr. Arabinda Saha, Siliguri Dr. KV Saharsranam, Calicut Dr. Rakesh Sahay, Hyderabad Dr. M Saikia, Guwahati Dr. Santosh B Salagre, Mumbai Dr. UC Samal, Patna Dr. ST Sanghavi, Mumbai Dr. HV Sardesai, Pune Dr. RN Sarkar, KolkataDr. Sankha Sen, Siliguri Dr. V Seshiah, Chennai Dr. Kamal Kumar Sethi, New Delhi Dr. Rishi Sethi, LucknowDr. Ajit Shah, Pune Dr. Bharat Shah, Mumbai Dr. Hardik Shah, MumbaiDr. Shrenik Shah, Ahmedabad Dr. Pravin Shankar, Ranchi Dr. S Shanmugasundaram, ChennaiDr. V Shantaram, Hyderabad Dr. Hem Shankar Sharma, BhagalpurDr. Mridul Sharma, Rajkot Dr. Mrs. Shimpa Sharma, Navi MumbaiDr. OP Sharma, New DelhiDr. SK Sharma, New DelhiDr. SK Sharma, Jaipur Dr. Sanjeev Sharma, New DelhiDr. Sunil Sharma, Sambalpur Dr. Vinod Sharma, New DelhiDr. Sharmasvali, Hyderabad Dr. Javed Sheik, Mehsana Dr. MP Shrivastava, New DelhiDr. Mrs Gursaran Sidhu, Ludhiana Dr. RK Singal, New DelhiDr. BP Singh, Patna
Dr. DP Singh, BhagalpurDr. Kulwant Singh, Ludhiana Dr. NP Singh, New DelhiDr. Pankaj Singh, Kolkata Dr. SJ Singh, Varanasi Dr. SK Singh, Dhanbad Dr. D Singhania, Delhi Dr. Ajay Kumar Sinha, Patna Dr. GK Sinha, VisakhapatnamDr. Nakul Sinha, Lucknow Dr. Pravir Sinha, Laheriyasarai Dr. SP Sodhi, MeerutDr. Navin Kumar Soni, Ghaziabad Dr. Srikanta, Bengaluru Dr. BC Srinivas, Bengaluru Dr. M Srinivasan, Cumbum Dr. BN Srivastava, Jabalpur Dr. BJ Subhedar, Nagpur Dr. R Subramanian, Chennai Dr. NI Subramanya, Bengaluru Dr. Ajay J Swamy, PuneDr. PG Talwalkar, Mumbai Dr. RN Tandon, KanpurDr. Ashok K. Taneja, GurgaonDr. Ahmer Tarique, Gurgaon Dr. Hemant Thakker, Mumbai Dr. BB Thakur, Muzaffarpur Dr. PL Tiwari, Mumbai Dr. Kamlesh Tewary, Muzaffarpur Dr. Satyasham Toshniwal, Solapur Dr. AK Tripathi, Lucknow Dr. MP Tripathi, Bhubaneshwar Dr. Nishant Tripathi, Patna Dr. Kaushik Trivedi, Vadodra Dr. Shailendra Trivedi, Indore Dr. Kaustubh Vaidya, Mumbai Dr. PP VarmaDr. Santosh VarugheseDr. Apporva Vasawda, Surat Dr. I Vincent, Bengaluru Dr. Vijay Viswanathan, Chennai Dr. HS Wasir, Gurgaon Dr. Milind Waykole, Jalgaon Dr. A Yadav, DelhiDr. Rakesh Yadav, New Delhi

8 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
List of Members
Core CommitteeConvenor
Dr. Siddharth N Shah, MumbaiMembers
Dr. M Paul Anand, MumbaiDr. Sandhya A Kamath, MumbaiDr. M Maiya, BangaloreDr. Sukumar Mukherjee, KolkataDr. YP Munjal, New DelhiDr. GS Wander, Ludhiana
ReviewersDr. AC AnandDr. AK PandeyDr. A KirpalaniDr. Arundhati SomanDr. Balram BhargavaDr. Chetan DesaiDr. D Rama RaoDr. FD DasturDr. KS NayakDr. KV Krishna DasDr. MA AleemDr. MK ManiDr. Mrs. NA KshirsagarDr. PS BanerjeeDr. S BhandariDr. S KrishnaswamyDr. S Ramanathan IyerDr. S ShanmurgamDr. SV KhadilkarDr. Sanjay AgarwalDr. Sahidul IslamDr. Shashank JoshiDr. Siddharth Kumar DasDr. Sushum SharmaDr. V MohanDr. Viraj SuvarnaDr. Yash Lokhandwala
Core CommitteeConvenor Dr. Siddharth N ShahMembers Dr. M Paul Anand Dr. YP Munjal Dr. BM Hegde Dr. Sukumar Mukherjee
Dr. GS WanderWorking Group
I.G.M.H. – I (2001) I.H.G. – II (2007)
Dr. Prabha Adhikari Dr. Jayant Antani Dr. Aspi R Billimoria Dr. TK Biswas Dr. Jamshed J Dalal Dr. Siddhartha Das Dr. DS Gambhir Dr. Rajeev Gupta Dr. A Hakim Dr. S Joglekar Dr. Sandhya Kamath Dr. U Kaul Dr. UA Kaul Dr. PC Manoria
Dr. SR Mittal Dr. V Mohan Dr. Shoiab F Padaria Dr. Manotosh Panja Dr. B Pardiwalla Dr. A Ramachandran Dr. D Rama Rao Dr. KS Reddy Dr. KK Sethi Dr. BK Sharma Dr. RK Singal Dr. AK Talwar Dr. Urmila Thatte
Contributors
Dr. RK AgarawalDr. AK AgarwalDr. Navneet AgarwalDr. Mohammad AhmadDr. Anil BhansaliDr. Eric BorgesDr. SK DhamDr. KL DharDr. SK GoyalDr. Arun JoshiDr. MA KabeerDr. Girish J KaziDr. SZ KhanDr. SB KhuranaDr. KC KohliDr. Dayanand K KumblaDr. M MaiyaDr. Kashinath PadhiaryDr. Prem Pais
Dr. MN PasseyDr. AS Chandrasekhara RaoDr. BP Gururaja RaoDr. Murali Babu RaoLt. Gen. (Dr.) YR SachdevDr. KV SahasranamDr. BK SahayDr. JPS SawhneyDr. V ShantaramDr. (Mrs.) Shimpa SharmaDr. Pradeep K ShettyDr. Kulwant SinghDr. Rajeev N SomanDr. NK SoniDr. R SudhaDr. SH TalibDr. RN TandonDr. Vinod M VijanDr. ME Yeolekar

9 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Preamble
Hypertension is a major contributor to cardiovascular morbidity and
mortality worldwide and in India. In view of our special geographical a n d c l i m a t i c c o n d i t i o n s , e t h n i c background, dietary habits, literacy levels and socio- economic variables, there are some areas of significant differences in disease manifestation and management which need to be addressed by us. With this in mind, the Association of Physicians of India (API), Cardiological Society of India (CSI), the Indian College of Physicians (ICP), and the Hypertension Society of India (HSI) developed the “FIRST INDIAN GUIDELINES FOR THE MANAGEMENT OF HYPERTENSION - 2001.”1
The second Indian guidelines were published in 2007.2 The third Indian Guidelines on Hypertension (IGH-III) were published in 2013.3 The fourth edi t ion of the Indian Guidel ines on Hypertension (IGH-IV) is being published now in 2019. There has been significant change in the management of hypertension in the last 6 years since the last edition. Notable ones are: change in definition of hypertension by the ACC/AHA which we are not adopting and are persisting with the earlier definition, changes in target BP to be achieved after the SHIFT trial4, greater use of home blood pressure monitoring (HBPM) and ambulatory
blood pressure monitoring (ABPM), reduced interest in renal angioplasty and renal denervation therapy due t o r e c e n t d a t a a n d a n i n c r e a s e d use of spironolactone for resistant hypertension. In addition we have new epidemiological data on hypertension and hypertension mediated organ damage (HMOD), which has a lso been included. Significant changes have appeared in other guidelines released in 2017 and 2018 and we needed to look at the literature which an Indian perspective and thus provide guidelines for Indian physicians for management of hypertension. These guidelines have been prepared as a reference for treating physicians. The current level of practice patterns based on evidence-based medicine have been presented. The intention is not to cover the topic of hypertension in totality but to give useful information based on literature after Medline and Embase search and evaluation of some of the latest guidelines from other national bodies like the Australian guidelines (2016), ACC/AHA guidelines (2017), Canadian hypertension guidelines (2017) and the European ESC/ESH guidelines (2018).5-8 The primary aim of these guidelines is to offer balanced information to guide clinicians, rather than rigid rules that would constrain their judgment about the management of individual adult patients, who will differ in their personal, medical, social, economic,
ethnic and clinical characteristics. These guidelines do not include hypertension in children and adolescents.
Methodology
In consonance with the first, second and third guidelines, a revised format was evolved by the Core committee which was then reviewed by 15 eminent referees. Their comments were included and following that these were sent to 150 physicians and specialists from across the country whose inputs have been incorporated. Like the previous guidelines, this document has also been studied, reviewed, and endorsed by the Cardiological Society of India (CSI), Hypertension Society of India (HSI), Indian College of Physicians (ICP), Indian Society of Nephrology (ISN), Research Society for Study of Diabetes in India (RSSDI) and Indian Academy of Diabetes (IAD).
We hope these guidel ines wi l l help the pract ic ing physic ians to address to this very important public health problem. Treatment of essential hypertension is a life-long commitment and should not be stopped even when the blood pressure (BP) is stabilized without consulting the physician.
The core committee recognizes that the responsible physician’s judgment and decision remains paramount for individual adult patients.

10 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
What is New in Indian Guidelines on Hypertension – IV• The title of “Indian Guidelines
on Hypertension (IGH - IV)” will be used for the 2019 guidelines henceforth.
• The health related toxic effects of mercury are recognized world over and mercury sphygmomanometers are being replaced by aneroid a n d d i g i t a l o s c i l l o m e t r i c sphygmomanometers.
• The change is inevi table and Indian physicians should also move towards using these devices and wean off the use of mercury sphygmomanometers.
• HBPM should be encouraged for better patient involvement and compliance. Reliable oscillometric devices should be used.
• HBPM corre la tes be t ter wi th HMOD than the office recordings.
• Masked hypertension also needs to be diagnosed and recognized like the white coat hypertension we have been more familiar with.
• The diagnosis of hypertension will be blood pressure of ≥140/90 for office BP.
• HBPM and ABPM readings are lower than office readings. The diagnosis by HBPM and by mean daytime ABPM will be pressure of >135/85 and a 24 hour mean ABPM of >130/80.
• The latest data in India shows that presently the prevalence in urban areas is 33.8% and in rural areas, it is 27.6% with an overall prevalence of 29.8%.
• Prevalence of hypertension is increasing in India as against some
other nations since our longevity is increasing.
• The levels of control of blood pressure are very low at 20% in urban and 11% in rural population. Large public health measures need to be undertaken to improve this.
• Special features of hypertension in India have been included and discussed for the first time (Table 5).
• ACEIs and ARBs are the preferred agents in young (<60) and CCBs and diuretics are the preferred agents in those >60 years.
• Combination therapy in single pi l l i s encouraged for be t ter compliance. >70% patients need combination of drugs for control of blood pressure.
• We should start with a two drug combination, preferably in a single pill for stage 2 hypertension.
• The value of beta-blockers as first line agents in hypertension has receded and these are now recommended as agents for use in specific indications.
• For routine patients these are no longer recommended as first line agents.
• Some combinations are preferred. ACEIs/ARBs in combination with CCB’s is considered a first line combination.
• Diuretics may be used as third agent in combination.
• Treatment of hypertension even in octogenarians (more than 80 years) has been showed to be beneficial (newer data) and is recommended.
• After the recent SPRINT study and the HOPE III study the threshold for starting antihypertensive therapy and the target blood pressure has been lowered as compared to the IGH III guidelines.9-10
• T h e t h r e s h o l d f o r s t a r t i n g antihypertensive drugs should be 140/90 in most patients.
• In patients of Coronary Artery Disease (CAD) and Heart Failure (HF), antihypertensive therapy may be started beyond 130/80. Target blood pressure of <130/80 should be achieved specially in those less than 60 years.
• In elderly, the target can be between 130-140 / 80-90 and it needs to be individualized.
• Chronic kidney disease (CKD) is a common comorbidity and has been explained.
• Awareness and diagnosis of this entity will help recognize the high risk hypertensive individuals.
• Obstructive sleep apnea (OSA) and its clinical implications have also been included.
• Pa t i e n t s w i t h H F n E F d e r i ve s igni f icant benef i t with good blood pressure control and target of <130/80 should be achieved just as in HFrEF.
• S t a t i n s a r e b e n e f i c i a l i n hypertensive individuals with dyslipidemia and should be used based on the findings of the HOPE III study.
• Aspirin has no role as a prophylactic agent in hypertension.

11 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Definition and Classification
Definition
There is a continuous relationship between the level of blood pressure
and the risk of complications. Starting at 115/75 mmHg, CVD risk doubles with each increment of 20/10 mm Hg throughout the blood pressure range. Risk of CV death increases two fold if BP rises to 135/85, fourfold if BP rises to 155/95 and eightfold at 175/105.11,12
All definitions of hypertension issued by various international bodies are arbitrary. There is some evidence that the risk of cardiovascular events in Asian Indians is higher at relatively lower levels of BP. Recently, the ACC/AHA guidelines have changed the definition of hypertension to 130/80.7 However, the European guidelines and many others maintain the earlier def in i t ion of 140/90 . 8 The Indian guidelines IV will continue with the previous definition of 140/90 and also the staging that we followed in the IGH III guidelines.
So, hypertension in adults age 18 years and older is defined as systolic blood pressure (SBP) of 140 mm Hg or greater and/or diastolic blood pressure (DBP) of 90 mm Hg or greater or any level of blood pressure in patients taking antihypertensive medication.11,12
Classification
Although the c lass i f i ca t ion o f adult blood pressure is somewhat arbitrary, it is useful for clinicians who make treatment decisions based on a constellation of factors along with the actual level of blood pressure. Table 1 provides a classification of blood pressure for adults (age 18 and older).1,13
This classification is for individuals who are not taking antihypertensive medication and who have no acute illness and is based on the average of two or more blood pressure readings taken at least on two occasions, one to three weeks apart, after the initial screening. In addition to classifying stages of hypertension on the basis of average blood pressure levels , clinicians should specify presence or absence of target organ disease and additional risk factors.
The positive linear relationship between SBP and DBP and cardiovascular risk has long been recognized. This relationship is strong, continuous, graded, cons is tent , independent , predictive and etiologically significant for those with and without coronary heart disease.14,15 For persons over age 50, SBP is more important than DBP as a CVD risk factor.16 SBP is more difficult to control than DBP.17,18 SBP needs to be as aggressively controlled as DBP. When SBP and DBP fall into different categories, the higher category should be selected to classify the individual’s blood pressure.
The definition and classification of hypertension is based on office readings by the physicians. The HBPM may be taken in account for staging and therapy of the patient. More recently, the SPRINT study used automatic office blood pressure (AOBP) recording which is not always feasible and so not recommended routinely by us.9
AOBP readings are 10-15 / 5-7 mm Hg lower than the office BP readings that we routinely use for definition of hypertension.19 The classification of hypertension will still largely be based
on office recordings by the physician and will be as in Table 1.
We now feel that HBPM should also be used for definition and follow up of patients. White coat hypertension is diagnosed when office blood pressure (OBP) readings are high and home BP is normal. Masked hypertension indicates normal office BP and high home BP readings. Incidence of white coat hypertension is 10-15% and that of masked hypertension is 5-10%. Recording of OBP and HBP both are important for recognizing these entities. A recent study (2018) comparing ABPM with Clinic BP which included 63,000 subjects over 10 years has shown ABP measurements are a stronger predictor of all cause and CV mortality than clinic BP. White coat hypertension which was present in 25% is not benign. Masked hypertension (seen in around 8%) was associated with a greater risk of death than sustained hypertension (Table 2 and Figure 1).20
The cut of f levels for def ining hypertension for the OBP, HBPM and ABPM are given in Table 3.
Table 2 : Patterns of Blood Pressure
Ambulatory / Home BPNormal High
Office BP Normal True normotension
Masked
High White coat Sustained hypertension
Table 1 : Classification of blood pressure for adults age 18 and older 1,13
Category Systolic (mm Hg) Diastolic (mm Hg)Optimal** <120 and <80Normal <130 and <85High-normal 130-139 or 85-89Hypertension***
Stage 1 140-159 or 90-99Stage 2 160-179 or 100-109Stage 3 ≥180 or >110Isolated systolic hypertensionGrade 1 140-159 and <90Grade 2 >160 and <90*Not taking antihypertensive drugs and not acutely ill; **Optimal blood pressure with respect to cardiovascular risk is below 120/80 mm Hg. However, unusually low readings should be evaluated for clinical significance; ***Based on the average of two or more blood pressure readings taken at least on two visits after an initial screening.
Table 3 : Diagnosis of Hypertension
SBP (mm Hg)
DBP (mm Hg)
Office BP ≥140 ≥90Self/Home BP (mean) ≥135 ≥85Ambulatory BP
Day (mean) ≥135 ≥85Night (mean) ≥120 ≥7024 hr (mean) ≥130 ≥80
Fig. 1: Patterns of blood pressure

12 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Epidemiology of Hypertension
Global
Cardiovascular disorders (CVD) are the leading cause of morbidity and
mortality worldwide.21 They account for an estimated 17.5 million deaths annually, more than 75% of which occur in lower middle-income countries (LMIC).22 While the deaths rates due to CVD have declined in several high-income countries (HIC), the trend has not been the same in LMIC.23,24 South Asia (India, Pakistan, Bangladesh, Nepal, Sri Lanka), that represents one of the most densely populated regions in the world, experienced an increase of 73% in healthy life-years lost due to ischemic heart disease between 1990 and 2010, compared to a global increase of 30%. 25 Moreover, South Asians have been shown to experience their first myocardial infarction (MI) almost 10 years earlier compared to people from other countries.26,27 This increase is largely due to increasing prevalence of risk factors like hypertension, diabetes and dyslipidemia.
As per the World Health Statistics 2018, of the estimated 57 million global deaths in 2016, 41 million (71%) were due to non-communicable diseases (NCDs). The largest proportion of NCD deaths is caused by cardiovascular
diseases (44%). In terms of attributable deaths , ra i sed b lood pressure i s one of the leading behavioral and physiological risk factor to which 12.8% (7.5 million deaths per year) of global deaths are attributed.28 Hypertension is reported to be the fourth contributor to premature death in developed countries and the seventh in developing countries.
Globally, over 1 billion adults have hypertension and will escalate to 1.5 billion in the decade ahead.29 Earlier reports also suggest that the prevalence of hypertension is rapidly increasing in developing countries and is one of the leading causes of death and disability. While mean blood pressure has decreased in nearly all HICs, it has been stable or increasing in most African and LMICs. The prevalence of raised blood pressure in 2008 was highest in the WHO African region at 36.8% (34.0–39.7).
The Global Burden of Diseases (GBD); Chronic Disease Risk Factors Collaborating Group had reported 25-year (1980-2005) trends in mean levels of body mass index (BMI) , systolic BP and cholesterol in 199 high-income, middle-income and low-income countries. Mean SBP declined in high and middle-income countries
Fig. 2 : Increasing trend in hypertension prevalence in India in urban (top panel) and rural (bottom panel) populations according to cross sectional regional studies from 1990’s to date. The increase is greater in urban (R2 = 0.101) compared to rural (R2 = 0.046) studies. Size of bubbles corresponds to number of participants in each study.32
12
National13-25 The prevalence of hypertension in the late nineties and early twentieth century varied among different studies in India, ranging from 2-15% in Urban India and 2-8% in Rural India. The prevalence increased over six decades to 25% in urban and 15% in rural India. There have been many small single centre studies on prevalence of hypertension from 1963 -2010 from rural and urban India. These studies in 70’s and 80’s had threshold of 160/90 for diagnosis of hypertension. Subsequent studies have had 140/90 as the cut off. These studies show increasing prevalence of hypertension over these six decades in our country. The increase was greater in urban than in rural areas in the earlier studies.(Figure 1)
.
Figure 1: Increasing trend in hypertension prevalence in India in urban (top panel) and rural (bottom panel) populations according to cross sectional regional studies from 1990’s to date. The increase is greater in urban (R2 = 0.101) compared to rural (R2 = 0.046) studies. Size of bubbles corresponds to number of participants in each study.
Formatted: Font: 14 pt, Font color:Text 1
but increased in low-income countries and is now more than in high-income countries. The India specific data was similar to the overall trends in low-income countries.
National
The prevalence of hypertension in the late nineties and early twentieth century varied among different studies in India and ranged from 2-15% in Urban India and 2-8% in Rural India. The prevalence increased over six decades to 25% in urban and 15% in rural India.30,31 There have been many small, single centre studies on prevalence of hypertension from 1963 -2010 from rural and urban India. These studies in 70’s and 80’s had a threshold of 160/90 for diagnosis of hypertension. Subsequent studies have had 140/90 as the cut off. These studies show increasing prevalence of hypertension over these six decades in our country. The increase was greater in urban than in rural areas in the earlier studies (Figure 2).
The latest data shows that presently the prevalence in urban areas is 33.8% and in rural areas, it is 27.6% with an overall prevalence of 29.8%. Thus, there has been a signif icant rural urban convergence as seen with other risk factors in the last two decades due to the changing lifestyle of the ruralites.33 Various factors of economic progress might have contributed to this rising trend, such as increased life expectancy, urbanization and its related lifestyle changes including increasing salt intake. Another factor that may contribute is the increased awareness and detection.
India with a population of 1.32 billion is experiencing an increase i n C V d i s e a s e s m a i n l y d u e t o uncontrolled hypertension.34 In a meta-analysis of multiple cardiovascular epidemiological studies, it was reported that prevalence rates of CAD and stroke have more than trebled in the Indian population. In the INTERHEART and INTERSTROKE study, hypertension accounted for 17.9% and 34.6% of population attributable risk for CAD and stroke respectively.

13 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Fig. 3: Leading causes of DALY in 1990 and 2016 show an epidemiological shift from communicable to non communicable diseases36 (Modified from Global Burden of Diseases (GBD) Study)
Table 5 : Increasing trends in deaths and disability adjusted life years (DALYs) due to high systolic blood pressure in India (Global Burden of Diseases Study 2016)
1990 1995 2000 2005 2010 2016DeathsAbsolute numbers (thousands) 784.7 885.3 1005.0 1153.6 1385.6 1634.7Death Rate / 100,000 90.8 92.7 95.9 101.3 113.1 124.2% of total deaths 8.9 9.9 10.8 12.2 14.4 16.7DALY’sAbsolute numbers (millions) 20.9 23.4 26.2 29.3 34.4 39.4DALY Rate / 100,000 2415 2451 2497 2576 2807 3000% of total DALYs 3.9 4.4 5.0 5.7 7.0 8.5
As per the Registrar General of India and Million Death Study investigators (2001-2003), CVD was the largest cause of deaths in males (20.3%) as well as females (16.9%) and led to about 2 million deaths annually. The Global Status on Non-Communicable Diseases Report (2011) has reported that there were more than 2.5 million deaths from CVD in India in 2008, two-thirds due to coronary artery disease and one-third to stroke. These estimates are significantly greater than those reported by the Registrar General of India and shows that CVD mortality is increasing rapidly in the country. CVD is the largest cause of mortality in all regions of the country. According to WHO absolute number of CVD related deaths in India have been increasing and were 1.93 million in year 2000, 1.96 million in 2005, 2.25 million in 2010 and 2.48 million in 2015. Deaths from IHD were 0.91 million in 2000, 1.06 in 2005, 1.28 in 2010 and 1.45 million in 2015, respectively.35
Hypertension in India has some special features such as; onset occurs relatively early in life, a rural-urban divide in prevalence, clustering of multiple cardiovascular risk factors and a significant seasonal variation of BP (Table 5). Also, the average BP in general population has been rising in the last two decades as against a decrease seen in some western countries. The awareness of hypertension is 42% in urban and 25% in rural individuals. The treatment is taken by 38% urbans and 25% rurals. Only 20% of urbans and 11% of rurals have control of BP. This is much less than the figures in other nations like in the US where awareness, treatment and control are 81, 74 and 53%, respectively.33
There are large regional differences in cardiovascular mortality in India among both men and women. The mortality is highest in south Indian states, eastern and north eastern states
and Punjab while it is the lowest in central Indian states of Rajasthan, Uttar Pradesh and Bihar.
The increasing prevalence of high normal blood pressure has been seen in many recent studies. It was found to be around 32% in a recent urban study from Central India. In some studies from South India (Chennai) and from Delhi prevalence of high normal blood pressure has been even higher upto 36% and 44% respectively in these regions. The prevalence of hypertension increases with age in all populations. In a recent urban study it increased from 13.7% in the 3rd decade to 64% in the 6th decade.
The Global Burden of Disease Study looked at variations in epidemiological transition across the states of India from 1990-2016. They divided states of India
Table 4 : Hypertension in India - Special features
1. Onset early in life2. Rural urban divide in prevalence3. Clustering of multiple CV risk factors4. Significant seasonal variation of BP5. Rising average BP of general population6. Low awareness, treatment and control rates7. Early HMOD – possibly due to poor control.
into four epidemiological transition level (ETL) groups on the basis of ratio of DALYs from communicable, maternal, neonatal and nutritional diseases (CMNNDs) and those from NCDs and injuries combined. The states with ratios of 0·56–0·75 in 2016 were considered to have low ETLs (Bihar, Jharkhand, Uttar Pradesh, Rajasthan, Meghalaya, Assam, Chhatt isgarh, Madhya Pradesh, and Odisha; total population 626 million in 2016), those with ratios of 0·41–0·55 had lower middle ETLs (Arunachal Pradesh, Mizoram, Nagaland, Uttarakhand, Gujarat, Tripura, Sikkim, and Manipur; total population 92 million), those with ratios of 0·31–0·40 had higher-middle ETLs (Haryana, Delhi , Telangana, Andhra Pradesh, Jammu and Kashmir, Karnataka, West Bengal, Maharashtra, and union territories other than Delhi;
Leading causes in 1990 Leading causes in 2016
1. Diarrhoeal diseases
2. Lower respiratory infections
3. Neonatal Preterm Birth
4. Tuberculosis
5. Measles
6. Ischaemic Heart Disease
7. Other Neonatal
8. COPD
9. Neonatal Encephalopathy
10. Iron-deficiency Anaemia
11. Congenital Defects
12. Cerebrovascular Disease
1. Ischaemic Heart Disease
2. COPD
3. Diarrhoeal diseases
4. Lower respiratory infections
5. Cerebrovascular Disease
6. Iron-deficiency Anaemia
7. Neonatal Preterm Birth
8. Tuberculosis
9. Sense Organ Diseases
10. Road Injuries
11. Self Harm
12. Low Back and Neck Pain

14 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Table 6: Correlation of parameters of HDI, UI and ETI by GBD Study with the prevalence of hypertension by the NFHS-4 and the DLHS-4 surveys
Human Development Index (HDI)
UrbanizationIndex (Ul)
Epidemiological transition index
(ETI)
Hypertension PrevalenceMen / Women (Average) %
Data sources Government of India
Census of India GBD Study NFHS-4 DLHS-4
Andaman and Nicobar
- 35.67 - 27.9/9.0 (18.5) 37.2/26.3 (32.1)
Andhra Pradesh 0.309 33.49 0.37 16.2/10.0 (13.1) 28.3/20.7 (24.5)Arunachal Pradesh
0.124 22.67 0.55 21.6/15.0 (18.3) 27.7/21.4 (24.7)
Assam 0.138 14.08 0.62 19.6/16.0 (17.8) 21.3/16.8 (19.1)Bihar 0.158 11.30 - 9.4/5.9 (7.7) 20.2/20.8 (20.5)Chandigarh - 97.25 - 13.5/9.3 (11.4) 41.8/31.3 (37.0)Chhattisgarh 0.180 23.24 0.6 12.7/8.8 (10.8) 17.1/13.5 (15.3)Delhi - 97.50 0.38 4.2/7.6 (5.9) 27.9/22.4 (25.4)Goa 0.803 62.17 0.21 13.2/8.5 (10.9) 32.9/26.4 (29.7)Gujarat 0.477 42.58 0.46 13.0/9.7 (11.4) –
Haryana 0.493 34.79 0.4 16.8/9.2 (13.0) 28.1/20.3 (24.5)Himachal Pradesh
0.647 10.04 0.3 21.9/12.1 (17.5) 38.5/30.8 (34.7)
Jammu and Kashmir
0.479 27.21 0.34 13.7/11.6 (12.7) –
Jharkhand 0.222 24.05 0.69 12.2/7.8 (10.0) 24.7/18.8 (21.8)Karnataka 0.42 38.57 0.34 15.4/9.7 (12.6) 25.5/21.0 (23.3)Kerala 0.911 47.72 0.16 9.5/6.8 (8.2) 41.4/33.0 (37.0)Madhya Pradesh 0.186 27.63 0.6 10.9/7.9 (9.4) 19.9/16.7 (18.3)Maharashtra 0.629 45.23 0.33 15.9/9.1 (12.5) 28.2/21.8 (25.1)Manipur 0.199 30.21 0.42 20.4/11.4 (15.9) 25.7/17.6 (21.7)Meghalaya 0.246 20.08 0.64 10.4/9.9 (10.2) 22.9/18.3 (20.6)Mizoram 0.408 51.51 0.53 17.9/9.8 (13.9) 24.5/14.8 (19.7)Nagaland 0.257 28.97 0.47 23.1/16.0 (19.6) 39.6/31.8 (35.8)Odisha 0.261 16.68 0.58 12.5/9.0 (10.8) 17.2/15.6 (16.4)Puducherry - 37.49 - 15.1/9.1 (12.1) 27.3/17.6 (22.4)Punjab 0.538 68.31 0.29 21.8/13.2 (17.5) 41.4/29.4 (35.7)Rajasthan 0.324 24.89 0.66 12.4/6.9 (9.7) 23.7/16.5 (20.2)Sikkim 0.324 24.97 0.45 27.3/16.5 (21.9) 36.2/30.4 (33.5)Tamilnadu 0.633 48.45 0.26 15.5/8.3 (11.9) 27.7/18.8 (23.3)Telangana - 48.45 0.38 18.2/10.1 (14.2) 26.5/19.6 (23.1)Tripura 0.354 26.18 0.45 13.6/12.6 (13.1) 22.4/18.8 (20.6)Uttarakhand 0.426 22.28 0.46 17.2/9.6 (13.4) 32.2/22.3 (27.4)Uttar Pradesh 0.122 30.55 0.68 10.1/7.6 (8.9) 20.5/18.2 (19.4)West Bengal 0.483 31.87 0.33 12.4/10.3(11.4) 22.6/21.0 (21.8)Human Development Index (HDI) is a statistic composite index of life expectancy, education, and per capita income indicators, which are used to rank countries into four tiers of human development. Urbanization Index (UI) measures of the degree of urbanization of a population. Epidemiological transition index (ETI), District Level Household Survey 4 (DLHS-4), National Family Health Survey 4 (NFHS-4), Global Burden of Diseases (GBD) Study.
total population 446 million), and those with ratios less than 0·31 had high ETLs (Himachal Pradesh, Punjab, Tamil Nadu, Goa, and Kerala; total population 152 million). Kerala had the lowest ratio of 0·16.The major risk factors for NCDs including high SBP, high blood glucose, total cholesterol and BMI increased from 1990-2016, more so in higher ETL states. The five leading risk factors of DALYs in 2016 were child and maternal malnutrition, air pollution, dietary risks, high SBP and high fasting blood glucose. Dietary risks, high SBP, high fasting glucose, total cholesterol and
high BMI together contributed 25% of DALY in India in 2016 which is more than twice their contribution in 1990 (Figure 3). Thus showing an increasing prevalence and significance of these non-communicable diseases across different regions of the country.36 There is an increasing trend in deaths and disability adjusted life years (DALYs) due to high blood pressure in India over the last 26 years as shown by data from the GBD study in Table 4.36
According to 2016 data, IHD is responsible for largest number of deaths
in India followed by COPD, diarrheal diseases and cerebrovascular disease (CVA) in that order. Hypertension is a major risk factor for IHD and CVA.36
The prevalence of hypertension varies in di f ferent regions of the country . This var iat ion is due to social, economic, dietary differences in different parts of the country. The socio economic factors are depicted by the human development index and the urbanization index. Also, the epidemiological transition has been variable in different parts of our country. Table 6 shows state wise distribution of parameters of human development index from Government of India, Epidemiological Transition Index from the GBD study (2016), prevalence of hypertension from the national family health survey 4 (NFHS-4) and the District Level Household Survey 4 (2012-2014) (DLHS-4). The GBD study was done over 1990-2016 and it reflects the epidemiological transition index over this period in various states. The socio economic and cultural factors which are different in various states effect the prevalence of hypertension and partly explain the variation in the prevalence across our vast country.
The national family health survey 4 (2015-16) (NFHS-4) looked at 6,01,509 households which included 6,99,686 women and 1,03,525 men from 28,583 primary sampling units in 640 districts of the country. The NFHS-4 data shows significant difference in hypertension prevalence across states.37 A major shortcoming of this study is exclusion of older age adults (>50 years) who have a higher prevalence of hypertension. In the DLHS-4 study the Government of India with registrar general of India has estimated CV risk factors in all states of the country.38 In this, data on BP measurement and hypertension prevalence are available since 2012 and so reflects the latest trends in prevalence across India. The DLHS-4 survey was undertaken in 2012-2014 and are thus provides the state wise recent data. There is a significant association of state level hypertension prevalence among NFHS-4 and DLHS-4 studies in both men and women suggesting that the high prevalence of hypertension in younger population of NFHS-4 survey has tracked into the older age population of DHLS-4 survey.

15 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
The treatment of hypertension is usually l ifelong although down regulation of therapy can be done in some. 70% patients in our country are out of pocket paid and have no insurance cover. Even the new Ayushman Bharat Yojana is for the hospital admissions and OPD treatment will continue to be self-paid. Cost of medicines should be an important issue for improving drug compliance in our country as against most western countries where 80-100 % of the population is covered by insurance. The wellness clinic which will be set up under the National
Health Policy 2017 will take care of timely prevention of non communicable diseases on an OPD basis. India spends only 3.9% of its GDP on health and per capita health expenditure is 63 USD only which is much less than other nations.39
Cost of therapy thus assumes great relevance for this disease requiring lifelong therapy. The prevalence of hypertension is increasing in India. According to WHO atlas, the average SBP in urban men age 40-49 years was 120.4 in 1942, 125.2 in 1963 and 130 in 1997.29 An ICMR study estimates that hypertension is responsible for 16% of
IHD, 21% of PAD, 24% of AMI’s and 29% of strokes.40 In another analysis hypertension has been found to be directly responsible for 57% of all stoke deaths and 24% of all CHD deaths in India.41
Preventive measures are required so as to reduce obesity by increasing physical activity, decreasing the salt intake of the population and a concerted effort to promote awareness about hypertension and related risk factors.

16 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Measurement of Blood Pressure
Clinic Measurement (Office Blood Pressure Measurement)
• Blood pressure is characterized by large spontaneous variations, t h e r e f o r e t h e d i a g n o s i s o f hypertension should be based on multiple BP measurements taken on several separate occasions.
• W i t h i n c r e a s i n g a w a r e n e s s about the hazardous effects of mercury on health, the mercury sphygmomanometer should not be used now. We recognize that mercury is a potent toxin, a global priority pollutant and a persistent b io-accumulat ive . A mercury sphygmomanometer contains 70 to 90 grams of mercury.42 Health Care Without Harm (HCWH) a n d t h e W H O a r e t o g e t h e r leading a global partnership to achieve virtual el imination of mercury-based thermometers and sphygmomanometers.
• H u m a n s a r e e x p o s e d t o methylmercury almost entirely by ea t ing contaminated f i sh , seafood and wildl i fe that are at the top of the aquatic food chain. It is recommended that physicians should phase out the mercury sphygmomanometers and replace these with aneroid and digital oscillometric devices. Some mercury sphygmomanometers can be kept only for the purpose of calibration.
• The aneroid large dial apparatus is the best for use in the office. It needs calibration every six months since the spring can loosen. Proper maintenance and calibration of the sphygmomanometer should be ensured. The automated office blood pressure (AOBP) equipment has been used recently in the SPRINT trial. These are not cost effective and may not be feasible as the devices of choice. The aneroid and the d ig i ta l osc i l lometr i c sphygmomanometers should be used.
• Use a standard cuff with a bladder that is 12 cm X 35 cm. Use a large bladder for fat arms and a small bladder for children. The bladder should encircle and cover 80%
of the length of the upper arm. For measurement , inf la te the bladder quickly to a pressure 20 mm Hg higher than the point of disappearance of the radial pulse. Deflate the bladder slowly by 2 mm Hg every second. The first appearance of the sound (Phase I Korotkoff) is the systolic BP. The disappearance of the sound (Phase V Korotkoff ) is the diastolic BP. For children and in those with high output states, muffling of the sound (Phase IV Korotkoff) is taken as diastolic pressure.
Precautions
The fo l lowing precaut ions are required for correct measurement of blood pressure:• At the initial visit, an average of
three readings, taken at intervals of 2-3 minutes should be recorded.
• For confirmation of diagnosis of hypertension, record at least 3 sets of readings on different occasions, except in Stage III hypertension.
• Patients should be asked to refrain from smoking or drinking tea/coffee, exercise for at least 30 minutes before measuring the BP.
• Allow the patient to sit for at least five minutes in a quiet room before beginning BP measurement.
• Measurement should be done preferably in a sitting or supine position. Patient’s arm should be fully bared and supported at the level of the heart.
• Measure the blood pressure in both arms at the first visit and use higher of the two readings.
• In older persons aged 60 years and above, in diabetic subjects and patients on antihypertensive t h e r a p y , t h e B P s h o u l d b e measured in both, supine/sitting and in standing positions to detect postural hypotension.
• If atrial fibrillation is present, a d d i t i o n a l r e a d i n g s m a y b e required to estimate the average SBP and DBP.
• Occasionally, thigh BP (popliteal) h a s t o b e m e a s u r e d w i t h appropriately large cuff, in prone
position especially in younger p e r s o n s w i t h h y p e r t e n s i o n . Normally thigh SBP is higher and DBP a little lower than the arm BP because of the reflected pulse wave. This is important for suspected coarctat ion and nonspecific aortoarteritis, where BP is lower in the lower limb as compared to the upper limb.
Home Blood Pressure Measurement
Measurement of blood pressure outside the clinic may provide valuable information for the initial evaluation of patients with hypertension and f o r m o n i t o r i n g t h e r e s p o n s e t o treatment. Home measurement has the advantage that it distinguishes sustained hypertension from “white- coat hypertension”, a condition noted in patients whose blood pressure is elevated in the physician’s clinic but normal at other times.
Validated automated (oscillometric) machines that use the brachial artery (arm) for measurement are reliable where as finger and wrist monitors are inaccurate and are not recommended. Home Blood pressure should be used complimentary to the clinic readings for diagnosis and follow up. Validated and calibrated electronic devices that are reliable should be used. Patients are to be encouraged to make morning and evening recordings for 3-5 days. A mean of these multiple readings reflects the true home blood pressure. Besides providing real l ife blood pressure readings it also encourages patient compliance and participation in the management. The oscillometric devices may not work well in patients who have atrial fibrillation or other arrhythmias. Technique
• Caffeine, smoking, alcohol, bathing and exercise should be avoided for at least 30 minutes before the reading is taken.
• The patient should sit calmly with back support, feet flat on floor for 5 minutes before taking a reading. Upper arm should be bare. When taking a reading the arm with cuff should be supported on a firm surface (table or arm-rest) at heart level. The Cuff should fit snugly

17 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
on the arm, about ½ -1 inch above the elbow crease.
• Readings should be taken in the morning before medication and at night. Each time, two readings should be taken, separated by one to two minutes be tween readings. Take readings twice a day for 7 consecutive days. Discard the readings of the first day. The average of the remaining 12 readings is the Home blood pressure measurement.
For home blood pressure, readings of more than 135/85 mm Hg should be considered elevated.
Home BP Monitoring (HBPM) is easy to use, reproducible and had a higher prediction of target organ damage then Clinic blood pressure. It can be used to distinguish white coat hypertension from sustained hypertension. The home monitoring improves compliance and ensures better blood pressure control. We recommend use of this modality after proper patient education. The patient should be educated not to change medication without consulting their physician.
Ambulatory Blood Pressure Measurement
It has been found that at least 20-25% of patients diagnosed with s tage I-II hypertension (DB P 90-104 mm Hg) are normotensive outside the physician’s clinic.
A m b u l a t o r y b l o o d p r e s s u r e monitoring (ABPM) has been found to be clinically useful in the following
s e t t i n g s : t o i d e n t i f y w h i t e - c o a t hypertension, masked hypertension, nocturnal hypertension (non-dippers), r e s i s t a n t h y p e r t e n s i o n , e p i s o d i c hypertension, evaluate the ef fect of ant ihypertensive drugs and in individuals with hypotensive episodes while on antihypertensive medication.
For measuring ambulatory blood pressure, a portable monitor is worn on a belt connected to a standard cuff on the upper arm. BP measurements are taken over a 24-48 hour period every 15-20 minutes during the daytime (8 am to 10 pm) and every 60 minutes during nighttime.43
BP has a reproducible circadian prof i le wi th h igher va lues whi le awake and mentally and physically active, whereas, much lower values during rest and sleep . Different values have been suggested for definition of hypertension with ABPM for day time average BP (≥135/85 mm Hg) and the night-time average (≥120/70 mm Hg) (Table 7).
Early morning surge in BP for 3 or more hours during transition from sleep to wakefulness, can be an independent risk factor and needs to be managed effectively44 by addition of a second dose in the evening or a dose of a second class of antihypertensive agent in the evening or a drug with a long half-life.
The data recorded from ABPM also
identifies patterns of blood pressure variation such as dipping, non-dipping, extreme dipping and reverse dipping (Table 8). While dipping is a normal phenomenon, non-dipping and extreme dipping are associated with increase cardiovascular and cerebrovascular event rates. In the case of reverse dipping, a diagnosis of obstructive sleep apnea should be considered. Classification of BP based on ABPM
ABMP is a bet ter predic tor o f cardiovascular events and all cause mortality than clinic blood pressure. However, this procedure should not be used indiscriminately in the routine work-up of a hypertensive patient because of its high cost.
Pulse Pressure45
The Pulse Pressure (SBP-DBP) depends upon factors like arterial stiffness (the cushioning capacity of arteries) and wave reflections - speed of the forward wave (pulse wave velocity or PWV).
MBP is the pressure for the steady flow of blood to peripheral tissues. PP is the consequence of intermittent ventricular ejection from the heart and is influenced by left ventricular ejection fraction and large conduit arteries, mainly the aorta. Factors like arterial stiffness (the cushioning capacity of arteries) and wave reflections – speed of the forward wave (pulse wave velocity or PWV) are also major determinants of PP. In subjects >50 years of age the arterial stiffness and wave reflections become the main determinants of increased SBP and PP.
Novel methods of monitoring central aortic pressure are being developed. The therapeutic approaches available to reduce PP and arterial stiffness with age are ACEIs or ARBs in association with CCBs and/or diuretics.
Table 7: Ambulatory blood pressure measurement
Category Normal (mm Hg)
Hypertension (mm Hg)
24 Hours average < 130 / 80 ≥130/80Day time / awake < 135 / 85 ≥135/85Asleep / night time < 120 / 70 ≥120/70
Table 8: Patterns of blood pressure variation on ABPM
Pattern DescriptionDipping Nocturnal BP fall of about
15% of daytime values in normotensive and hypertensive patiens
Non-dipping Absence of nocturnal fall in BP by at least 10%
Extreme dipping A marked fall in BP during the night by >20%
Reverse dipping or rising
Increase in BP levels during sleep to levels higher than in daytime

18 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Evaluation
Ev a l u a t i o n o f p a t i e n t s w i t h documented hypertension has
three objectives:• To identify known causes of high
blood pressure• To assess the presence or absence
of HMOD. • To identify other cardiovascular
r i s k f a c t o r s o r c o n c o m i t a n t d i s o r d e r s t h a t m a y d e f i n e prognosis and guide treatment
Data for evaluation is acquired through medical history, physical examination, laboratory tests, and other special diagnostic procedures
Medical History
• Duration and level of elevated blood pressure, if known
• Symptoms of coronary artery disease (CAD) , hear t fa i lure , cerebrovascular disease, peripheral vascular disease and CKD
• Diabetes mellitus, dyslipidaemia, obesity, gout, sexual dysfunction and other co-morbid conditions
• Family his tory of h igh blood pressure, obesity, premature CAD
and stroke, dyslipidaemia and diabetes
• Symptoms suggesting secondary causes of hypertension
• History of smoking or tobacco use, physical activity, dietary assessment including intake of sodium, alcohol, saturated fat and caffeine
• Socioeconomic status, professional and educational levels
• History of use / intake of a l l prescribed and over-the-counter medications, herbal remedies, l i q u o r i c e ( Y a s h t i m a d h u /J e s t a m a d h a ) , i l l i c i t d r u g s , corticosteroids, NSAIDs, nasal drops. These may raise blood pressure or interfere with the effectiveness of antihypertensive drugs
• History of oral contracept ive use and hypertens ion during pregnancy
• H i s t o r y o f p r e v i o u s a n t i h y p e r t e n s i v e t h e r a p y , i n c l u d i n g a d v e r s e e f f e c t s experienced, if any
Table 9 : Factors influencing risk of cardiovascular disease46,47,48
Risk factors for coronary artery disease (RF)
Hypertension mediated organ damage (HMOD)
Associated clinical conditions (ACC)
• Age > 55 years* • Male sex• Post-menopausal women• Smoking and tobacco use• Diabetes mellitus• Family history of premature
coronary artery disease (Males < 55 years, Female < 65 years)
• Increased Waist:hip ratio• Obesity and Obstructive
Sleep Apnoea (OSA)• High LDL or Total
cholesterol • Low HDL cholesterol and
High triglycerides• High sensitivity C-reactive
protein (hs-CRP) • Estimated GFR
• Left ventricular hypertrophy detected by ECG and/or echocardiogram
• Microalbuminuria/ proteinuria and/or elevation of serum creatinine (1.2-2.0 mg/ dl)**
• Urinary ACR (albumin creatinine ratio)***
• Ultrasound or radiological evidence of atherosclerotic plaques in the carotids
• Hypertensive retinopathy• Ankle Brachial Index (<0.9)
• Cerebrovascular disease - Transient ischemic attack - Ischemic stroke - Cerebral haemorrhage• Heart disease - Myocardial infarction - Angina - Coronary
revascularization - Congestive heart failure• Renal disease - Diabetic nephropathy - Renal failure (serum
creatinine > 2.0 mg/dl)• Vascular disease - Peripheral arterial
disease including non-specific aortoarteritis
- Aortic dissection• Advanced hypertensive
retinopathy - Haemorrhages or
exudates - Papilledema
*Coronary artery disease is known to occur 10 years earlier in South Asians than in other ethnic groups.; **Microalbuminuria 30-300 mg/24hours; ***Albumin-Creatinine Ratio (ACR) ≥22 (M) or ≥31 (F) mg/g creatinine
• Psychosocial and environmental factors
Physical Examination
• Record three b lood pressure readings separated by 2 minutes, with the patient either supine or sitting position and after standing for at least 2 minutes.
• Record height, weight and waist circumference, BMI.
• E x a m i n e t h e p u l s e a n d t h e extremities for delayed or absent femoral and peripheral arterial pu lsa t ions , b ru i t s and peda l oedema.
• Look for arcus senilis, acanthosis n i g r i c a n s , x a n t h e l a s m a a n d xanthomas.
• Examine the neck for carot id bruits, raised JVP or an enlarged thyroid gland.
• Examine the heart for abnormalities in rate and rhythm, location of apex beat, fourth heart sound and murmurs.
• Examine the lungs for crepitations and rhonchi.
• Examine the abdomen for bruits, enlarged kidneys, masses and abnormal aortic pulsation.
• Examine the optic fundus and do a neurological assessment.
Laboratory Investigations
• Routine - Urine examination for protein
and glucose and microscopic examination for RBCs and other sediments.
- Haemoglobin, fasting blood glucose, serum creatinine, potassium and total cholesterol
- 12-lead electrocardiogram• Additional investigations in special
circumstances can include - Fasting lipid profile and uric
acid - Urine Albumin Creatinine
Ratio - Echocardiogram - Ultrasound of Abdomen• Other specific tests to rule out
secondary causes of hypertension

19 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Table 10: Risk stratification of patients with hypertension46,47,48
Blood pressure (mm Hg)Stage Other risk factors and
disease historyStage 1 Stage 2 Stage 3
(severe hypertension)SBP 140-159 or DBP 90-99
SBP 160-179 or DBP 100-109
SBP>180 or DBP>110
I No other risk factors Low risk Medium risk High riskII 1-2 risk factorsa Medium risk Medium risk Very high riskIII 3 or more risk factors or
TODb or diabetesHigh risk High risk Very high risk
IV ACCc Very high risk Very high risk Very high riskRisk strata (typical 10 year risk of stroke or myocardial infarction): Low risk = Less than 15% Medium risk = about 15-20% High risk = about 20-30% Very high risk = 30% or more a See Table 10; bHMOD: Hypertension Mediated Organ Damage see Table 10; cACC: Associated clinical conditions, including clinical cardiovascular disease or renal disease see Table 10
where there is a high index of suspicion are described under “secondary hypertension”.
• hs-CRP and microalbuminuria can be used in special circumstances for risk stratification.
• The cos t o f inves t igat ions in the context of the needs of an individual patient and resources a v a i l a b l e i s a n i m p o r t a n t consideration. In patients with essent ia l hypertension where there is a resource crunch, one m a y b e r e q u i r e d t o i n i t i a t e therapy without carrying out any
laboratory investigations.
Factors Influencing Risk
The overal l CV risk predict ion has been suggested in some latest guidelines for initiation of therapy at lower blood pressure levels. The Amer ican guide l ines use pooled cohort equations for calculation of 10 year ASCVD risk.46 The European guidelines use the Systemic Coronary Risk Evaluation System (SCORE) for the same. We do not have our own risk scoring system for Indians at present. European guidelines suggest a multiple
of 1.4 increased risk for south Asians. Even otherwise it has been observed that CV risk is underestimated in Indian patients with the established CVD risk calculator scoring systems.47,48,49 Primarily, age, sex, lipids, smoking habit and presence of diabetes are the five major factors in all these risk score calculation systems. We should recognize the presence of these factors along with the fact that we Indians are genetically at a higher risk for ASCVD with any given level of these risk factors.
Besides calculation of the overall risk by these factors or scoring systems the other two factors affecting the overall risk of the individual are the presence of HMOD and other associated clinical conditions (ACC). The presence of one of these three would decrease the threshold for initiation of drug therapy even at lower levels of BP, in that order. The prognosis of the patients and the choice and need for urgency of therapy, will be dependent on the overall risk stratification as shown in Table 10, depending on the ASCVD risk, HMOD and ACC respectively.

20 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Management of Hypertension
Goals of Therapy
The primary goal of therapy of hypertension should be effective
control of BP in order to prevent, reverse or delay the complications and thus reduce the overall risk of an individual without adversely affecting the quality of life. Patients should be explained that the lifestyle modifications and drug treatment is generally lifelong and regular drug compliance is important.Initiation of therapy
Having assessed the patient and determined the overall risk profile, management of hypertension should proceed as follows:• I n p a t i e n t s w i t h s t a g e I
hypertension repeat readings should be taken within 2-3 weeks along with lifestyle modification. Pharmacotherapy needs to be initiated after 1 month.
• BP needs to be recorded in both arms and in lying and standing before initiation of pharmacotherapy.
• In patients with stage II or III hypertension, shorter wait ing period (in stage III repeat readings af ter few hours only) wil l be desirable.
• T h o s e p a t i e n t s w h o h a v e evidence of ASCVD and HMOD, p h a r m a c o t h e r a p y s h o u l d b e started early.
Targets of therapy
The target blood pressure should be 130/80 amongst those <60 years and 130-140/80-90 in those >60 years. The physiological age should be looked at rather than the chronological age in elderly. In active elderly the targets should be achieved more aggressively.
In frail elderly individuals who are not very active and especially those with postural hypotension higher target BP should be accepted. Patient should not be made to feel worse and the risk of falls be kept in mind.
The BP control should not be <120/70 since at pressures lower than this the risk is increased. Recognizing the wide variation of BP readings in any given individual one should aim at having most readings in this range, fully recognizing that some would be beyond it in both directions. These guidelines need to be individualized according to age, activity level, other concomitant diseases and therapies.
Management Strategy
• Recent evidence suggests that the level of SBP control correlates better with reduction of mortality than the level of DBP control.50-57
• I m p r e s s i v e e v i d e n c e h a s accumulated to warrant greater attention to SBP as a major risk fac tor for CVDs . The r i se in SBP continues throughout life. In contrast the DBP, rises until approximately 50 years of age. It tends to level off over the next decade , and may remain the same or fall later in life. Diastolic h y p e r t e n s i o n p r e d o m i n a t e s before 50 years of age, e i ther alone or in combination with SBP elevation. DBP is a more potent cardiovascular risk factor than SBP until age 50; thereafter, SBP is more important.12
• Trials describe population averages for the purpose of developing guidelines, whereas physicians
must focus on the individual patient’s clinical responses.58
• We s h o u l d b e m o v i n g t o a n individual ized care in which the patient profi le (race, age, risk factors, associated diseases, HMOD) and the BP value will both have an equal effect on choice and need for antihypertensive medications and the targets to be achieved.
Non-pharmacologic Therapy
Life s tyle measures should be instituted in all patients including those who require immediate drug treatment. These include:• Patient education: Patients need
to be educated about the various aspects of the disease, adherence to l i fe s tyle changes on long term basis and need for regular monitoring and therapy.
• Weight reduction: Weight reduction of even as little as 4.5 kg has been found to reduce blood pressure in a large proportion of overweight persons with hypertension.59
• Physical activity: Regular aerobic physical act ivity can promote weight loss, increase functional s t a t u s a n d d e c r e a s e t h e r i s k of cardiovascular disease and all-cause mortality. A program of 30-45 minutes of brisk walking or swimming at least 3-4 times a week could lower SBP by 7-8 mm Hg. Isometric exercises such as weight lifting should be avoided as they lead to pressor effects.
• Alcohol intake: Excess alcohol intake causes a r i se in b lood pressure, induces resistance to antihypertensive therapy and also increases the risk of stroke. 60,61
Alcohol consumption should be limited to no more than 2 drinks per day (24oz beer, 10oz wine, 3oz 80-proof whiskey) for most men and no more than 1 drink per day for women and lighter weight people.12
• S a l t i n t a k e : E p i d e m i o l o g i c a l evidence suggests an association between dietary salt intake and elevated BP. The total daily intake of salt should be restricted to 6
Table 11 : Blood Pressure Levels: Threshold for treatment and Target BP to be achieved
Subjects Threshold to start treatment (≥) Target BP rangeAge <65 years
High ASCVD risk 140/90 120-130/ 70-80Low ASCVD risk 140/90 130-140/ 70-80
Age 65-80 years 140/90 130-140/70-80Age >80 years 140-150/90 130-140/70-80With other risk factors
Diabetes 140/90 130-140/70-80History of Stroke, TIA 140/90 130-140/70-80Chronic Kidney Disease 140/90 130-140/70-80Coronary Artery Disease 130 /80 120-130/70-80Heart Failure 130/80 120-130/70-80

21 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
The fall in SBP after yoga therapy has been between 2-6 mm Hg. A recent study from Puducherry shows mean SBP reduction by 4 and 6 mm Hg with l i festyle modif icat ion (LSM) and LSM + yoga respectively. Yoga also resulted in reduction of heart rate, waist circumference and l ipid levels, all of which reduce CVD prevalence and mortality.67-71
• Diet: - Vegetarians have a lower BP
compared to meat eaters.72 This is due to higher intake of fruit , vegetables, f ibers coupled with a low intake of saturated fats and not due to an absence of intake of meat protein.73
- Intake of saturated fats is to be reduced since concomitant h y p e r l i p i d a e m i a i s o f t e n present in hypertensives.
- Regular f ish consumption m a y e n h a n c e b l o o d pressure reduction in obese hypertensives.74
- Adequate potassium intake f r o m f r e s h f r u i t s a n d ve g e t a b l e s m a y i m p r o ve blood pressure control in hypertensives. Food items with high potassium content that can be benef ic ial are shown in Table 14.75
- Caffeine intake increases BP acutely but there is rapid development of tolerance to its pressor effect. Epidemiological studies have not demonstrated a direct link between caffeine intake and high BP.76
- Recent data from the PURE s t u d y s h o w s t h a t h i g h carbohydrate intake (> 60% of energy) was associated with adverse impact on total m o r t a l i t y . I n f a c t h i g h e r fa t intake was assoc ia ted w i t h l o we r r i s k o f t o t a l mortality and stroke. Indians c o n s u m e h i g h e r l e ve l o f carbohydrates than others. Use of carbohydrates should be reduced in diet.77
- T h e d i e t s h o u l d b e r i c h i n w h o l e g r a i n s , f r u i t s , vegetables and low-fat dairy products and avoid saturated
Table 12 : Lifestyle interventions for BP reduction
Intervention Recommendation Expected systolic blood pressure reduction (range)
Weight reduction Maintain ideal BMI (20-25 Kg/m2) 5-20 mm Hg per 10 kg weight lossDASH* eating plan Eat diet rich in fruit, vegetables, low-fat
dairy products. Eat less saturated and total fat
8-14 mm Hg
Dietary sodium Restriction Reduce dietary sodium intake to <100 mmol/day <2.4 g sodium or <6 g salt (sodium chloride)
2-8 mm Hg
Physical activity Regular aerobic physical activity, e.g. brisk walking for at least 30 min most days
4-9 mm Hg
Alcohol moderation Total abstinence preferred and recommended if must then Men ≤ 21 units per weekWomen ≤ 14 units per week
2-4 mm Hg
Tobacco Total abstinence*DASH= Dietary Approaches to Stop Hypertension
Table 13 : Sodium content of foods per 100 gms – Common Indian diets
<25 mg Low
25-50 mg Moderate
50-100 mg Moderately High
>100 mg High
Amla Bitter gourd (Karela)
Bottle gourd (Laukee)
Brinjal (Baingan) Cabbage
Lady finger (Bhindi)Colocasia (Arbi)
Cucumber French beans
Peas Onion Potato
Tomato ripe Yam (Jimikand)
Cow pea (Lobiya)Ragi
Vermicelli (Saviyan)Semolina (Sooji)
Wheat Maida Milk
Grapes Sweetlime
Papaya Orange
Sapota (Chikoo)
Raisins Carrots
Reddish white Black gram (Urad)
dal Green gram (Moth)
dal Red gram (Arhar/
Toor) dal Lentil (Masoor)
whole Bengal (Chana)
gram whole Banana Pineapple
Apple Mutton
Cauliflower Fenugreek (Methi)
Lettuce (Salad Patta)Field beans Beetroot Water melon Bengal gram dal Red gram
tender Liver Prawns
Beef Chicken
Amaranth (Rajgira)Bacon Egg
Lobster
gms (amounting to 3-4 gms of sodium), however, in hot summer this may be re laxed. Pat ients should be advised to avoid added salt, processed foods, and salt-containing foods such as pickles, papads , ch ips , chutneys and preparations containing baking powder. Most breads, cereals, packaged namkeen, readymade soups, canned food, pizzas and Chinese takeaway are also high in salt content. The salt content of some commonly used food items are given in Table 13 for reference.
• I n t h e I n d i a n c o n t e x t , s a l t restriction is more important as Indian cooking involves a high usage of salt. Salt intake amongst Indian patients has been found to be high. An ICMR task force study conducted in 13 states documented daily salt intake of 13.8 g per day per person.62 The SCRIPT study conducted across 4 regions of India showed that a region wise mean
daily salt intake in north, east, west and south was 14.1, 9.8, 10.1 and 9.4 g per day respectively. These are much higher than the WHO recommendation of <5 g per day which is also our IGH guideline recommendation.63
• Smoking: Smoking or consumption of tobacco in any form is the single most powerful modifiable l i festyle factor for prevention o f m a j o r c a r d i o va s c u l a r a n d non-cardiovascular disease in hypertensives.64-66 Cardiovascular benefits of cessation of smoking can be seen within one year in all age groups.59 E cigarettes are now available in our country and are being used. These are also harmful and their use needs to be strongly discouraged.
• Yo g a a n d M e d i t a t i o n : Yo g a , meditation and biofeedback have been shown to reduce b lood pressure in randomized controlled studies from India and the west.

22 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Table 14: Foods with high potassium75
Fruits VegetablesAmlaSapota (Chikoo)PeachesOrangePapayaBanana
PlumsLemonsSweetlimePineappleAppleWatermelon
CabbageBitter gourdLadies fingerCauliflowerSpinachPotatoDrumstick
Raddish whiteBrinjal (Baingan)PumpkinFrench beansColocasia (Arbi)Tapioca (Sabudana)
fat and cholesterol. Such a diet can lower the BP by up to 11 mm Hg i f you have high blood pressure. This eating plan is known as the Dietary Approaches to Stop Hypertension (DASH) diet.
Lose extra pounds and watch your waistline
§ you may reduce your blood pressure by about 1 millimeter of mercury ( m m H g ) w i t h e a c h k i l o g r a m ( a b o u t 2 . 2 pounds) of weight you lose.
§ BMI - Carrying too much weight around your waist can put you at greater risk of high blood pressure.
§ 1 tsp of salt (flattened) = 5 g of salt. A hypertensive patient should eat not more that 5 g of salt in a day.
§ adults who consumed more protein, whether from dairy, eggs, meat, or p lant sources , had lower b lood pressure levels after four years o f f o l l o w - u p . Pe o p l e with the highest protein intake—on average 102 grams a day—saw the
biggest benefit, with a 40 percent lower risk of developing high blood pressure.
Avoid 1. Bakery Products (Bread,
Biscuits, cakes) – They contain baking powder (Soda bicarb). Instead of bread sandwiches made with thick crisp chapati or bhakri are also tasty. A thick cr isp crust of bhakri also makes a good a l ternate p izza crust . Instead of cheese, low salt paneer is tasty.
D i e t Pl a n f o r t h e D a y - Total 2300-2500 calories are recommended per day
Early Morning – 2 tbsp of flax seeds / 6-7 badaams (almonds) and 2 pieces (1piece = ½ a walnut) + 1 cup of tea (Non-diabetics may take about ½ to ¾ spoonful of sugar)
Breakfast – with one cup of tea / coffee.
Upma (Rawa or Daliya – Daliya is recommended because it has more fibre) with mixed vegetables ( carrots, peas, capsicum, any other) OR
Egg Omlette with spinach OR 1 stuffed Paratha (Paratha can be made of whole wheat, jowar, ragi, multigrain) with curds OR
Oats in the form of porridge, upma, idli, dosa (should add vegetables in the idli-dosa)
3 home-made idlis or 1 dosa. Instead of rice we can make multigrain idlis, ragi idlis, etc)
Mid-morning 1 fruit – banana, orange, apple,
pear, etc 1 cup of Green tea Lunch 2 medium sized chapatis + 1
soup bowl of vegetable + 1 small bowl of dal + salad + 1 small bowl of rice or pulav (rice can be substituted by one additional chapati for those who have a preference for chapatis) + 1 bowl of chicken or fish (Avoid shell fish).
1 glass of buttermilk or a small bowl of curds to be had one hour after the meal
Snacks with 1 cup of evening tea
1 b o w l o f P u f f e d r i c e , makhanas, unsalted channa-peanuts. Upma or pohe i f no t a l ready consumed a t breakfast. Dhokla (5-6 pieces), khakra
Dinner – can be the same as lunch. Avoid foodstuffs with spices at night.
- Thus, the diet in hypertensives should be low calorie, low fat, and low sodium, with normal protein intake. The food items to be avoided in hypertensives are shown in Table 15.78,79
Pharmacologic Therapy
Principles of drug treatment
• Over the past decade, the goals o f t r e a t m e n t h a ve g r a d u a l l y shifted from optimal lowering of blood pressure, which is taken for granted, to patient’s overall well-being, control of associated risk factors and protection from future HMOD.80
• Achieve gradual reduct ion of blood pressure. Use low doses of antihypertensive drugs to initiate therapy.
• F ive c lasses o f drugs can be recommended as first line treatment for stage 1-2 hypertension. These include : 1) ACE inhibitors, 2) Angiotensin receptor blockers, 3) Calcium channel blockers, 4) Diuretics and 5) Newer β-blockers.
• The Blood Pressure Lowering Treatment Trialists’ Collaboration concluded that treatment with any commonly used reg imen reduces the risk of total major cardiovascular events and larger reduct ions in b lood pressure produce larger reductions in risk.81
• Choice of an antihypertensive agent is influenced by age, concomitant risk factors, presence of HMOD, o t h e r c o - e x i s t i n g d i s e a s e s , socioeconomic considerations, availability of the drug and past experience of the physician.
• Combining low doses of two or more drugs having synergistic
Table 15: Food items to be avoided in hypertensives78,79
A BTable saltMono sodium glutamate (Ajinomoto)Baking powderFried foodsAlcoholBakery products : Biscuits, cakes, breads and pastries
Salt preserved foodsPickles Canned foodsKetchup and saucesPrepared mixesReady to eat foodsHighly salted foodsPotato chips, cheese, peanut butter, salted butter, papads

23 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
and diltiazem). Amlodipine is the most commonly used agent in this group. Besides blood pressure lowering effect, they also have antianginal effects and are devoid of metabolic side effects. CCBs are particularly recommended for elderly patients with isolated systolic hypertension. Verapamil and diltiazem reduce heart rate and have negative inotropic effects. In the Nordic trial,90 diltiazem was shown to be as effective as t rea tment based on d iure t i cs , β-blockers or both, in preventing the combined primary endpoints of stroke, MI and CV deaths. The findings of the ASCOT-BPLA (Blood Pressure Lowering Arm) study show that an antihypertensive drug regimen starting with amlodipine (adding perindopril as required) is better than one starting with atenolol (adding thiazide as required) in terms of reducing the incidence of all types of cardiovascular events and all-cause mortality, and risk of subsequent new-onset diabetes.53
Short ac t ing dihydropyr idines ( n i f e d i p i n e ) s h o u l d b e a v o i d e d . Amlodipine has no effect on heart rate and cardiac contractility, and has been shown to be safe even in the presence of congestive heart failure.91
Diuretics
Diuretics are widely used as first line agents. They are effective and inexpensive . Al though high dose diuretic therapy was associated with side effects, currently recommended low dose diuretic therapy is generally well tolerated. Low dose diuretics have lesser metabolic side effects like worsening of glycemic control, hyperuricemia and dyslipidemia. Diuretics should be used in doses equivalent to 12.5 mg daily of chlorthalidone or hydrochlorothiazide t o a v o i d a d v e r s e m e t a b o l i c c o n s e q u e n c e s . C h l o r t h a l i d o n e i s preferred over hydrochlorothiazide as an antihypertensive.92 Indapamide use has been shown to be associated with minimal metabolic side effects and is a useful agent. Combinations of thiazides and potassium-sparing diuretics (amiloride and triamterene) are available and are effective options. The PATHWAY 3 trial (2016) a double blind randomized trial showed that a combinat ion of ami lor ide wi th hydrochlorothiazide prevents glucose intolerance and improves control of BP compared with hydrochlorothiazide alone. Thus, when hydrochlorothiazide is used as a first line agent it should be
effect is likely to produce lesser side effects. In 70 % of patients, g o a l b l o o d p r e s s u r e w i l l b e achieved with two or more agents only.
• Use fixed dose formulations to improve compliance.
• Drugs with synergistic effects should be combined pertinently to enhance BP lowering effect so as to achieve target BP.
• Use of long acting drugs that provide 24-hour eff icacy with once daily administration ensures smooth and sustained control of blood pressure; which in turn is expected to provide greater protection against the risk of major cardiovascular events and HMOD. Once daily administration also improves patient compliance.
• Although antihypertensive therapy is generally lifelong, an effort to decrease the dosage and number of antihypertensive drugs should be considered after effective control of hypertension (step-down therapy).
• Due to a greater seasonal variation of temperatures in India, marginal alterations in dosages of drugs may be needed from time to time.82,83
• T h e c o m m o n l y u s e d antihypertensive class of agents are discussed further.
Antihypertensive drugsAngiotensin Converting Enzyme inhibitors (ACE inhibitors)
ACE inhibitors are effect ive in lowering blood pressure and are well tolerated. These are first line agents in patients with diabetes, individuals with other metabolic r isk factors, post-MI and patients with heart failure. In diabetes mellitus, they retard the onset and progression of renal disease (patients with microalbuminuria and early CKD). The HOPE trial (a primary prevention trial) showed that in high and average risk individuals, use of ramipril reduced overall mortality and cardiovascular endpoints, even with small reductions in blood pressure.84 As a class, they are metabolically beneficial to other risk factors like dyslipidemia and diabetes. The most common side effect is dry cough. ACE inhibitors are contraindicated in pregnancy. Serum creatinine and potassium should be monitored in patients receiving ACE inhibitors. Ramipril and Perindopril
have greater tissue ACE inhibition effect than other agents. Perindopril in combination with Indapamide has been particularly shown to reduce mortality in patients who have survived stroke (PROGRESS trial).85
Angiotensin Receptor Blockers (ARBs)
Angiotensin receptor blockers block the angiotensin II AT-1 receptors, and thus prevent the action of angiotensin II. In the LIFE trial, losartan was better than atenolol in reducing the frequency of the primary composite endpoint of stroke, myocardial infarction and cardiovascular death.86 In the Valsartan Ant ihyper tens ive Long- term Use Evaluation (VALUE) trial, both valsartan and amlodipine reduced blood pressure in hypertensive patients at high CV risk, but the effects of the amlodipine-based regimen were more pronounced, especially in the early period.87 These drugs have many features in common wi th ACE inhib i tors , but do not cause an accumulation of bradykinin. Consequently, cough and angioedema are much less likely to occur than with ACE inhibitors.13 Initially, some fears were raised regarding increase of coronary events with use of these agents, however, these have been disproved ever since. Also, one retrospective meta-analysis suggested increase in neoplasm with ARBs, however no prospective study has suggested this and is generally believed not to be a significant issue at present. In fact, the ONTARGET trial shows telmisartan (80 mg OD) is as effective as ramipril (10 mg OD) in reducing CV events in high-risk individuals in patients with vascular disease or high-risk diabetes.88 A combination of ACEIs and ARBs should not be used due to increased risk of hypotension and hyperkalemia. In the recent randomized double blind ROADMAP 89 tr ial involving 4,447 diabetic patients with olmesartan (40 mg OD), the onset of microalbuminuria has been shown to be delayed in patients with type 2 diabetes. A caution of monitoring eGFR change and serum potassium should be added. This monitoring should be after 1 week of initiating this therapy and after each dose increase.Calcium Channel Blockers (CCBs)
The two subgroups of CCBs are d i h y d r o p y r i d i n e s ( a m l o d i p i n e , felodipine, nifedipine, cilnidipine) and non- dihydropyridines (verapamil

24 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
used in combination with amiloride.93
A l d o s t e r o n e a n t a g o n i s t s (Spironolactone , Eplerenone) are t h e p r e f e r r e d a g e n t s a s a d d - o n agents to reduce BP in patients with resistant hypertension even without documenting hyperaldosteronemia. The PATHWAY-2 study (2015) was a randomized double blind cross over trial which showed that spironolactone was superior to doxazosin and bisoprolol
as an add on agent amongst patients with resistant hypertension who were already on three drugs (ACEI/ARB + CCB + thiazide diuretic).94 In cases of heart failure and/or renal failure, loop diuretics like Furosemide (40-80 mg), Torsemide (10-40 mg) can be used. Metolazone (2.5-5 mg), is the only thiazide like diuretic which is effective in presence of renal failure.
Manrique C, Giles TD, Ferdinand KC,
et al. Realities of newer beta-blockers for the management of hypertension. J Clin Hypertens (Greenwich). 2009 Jul;11(7):369-75. doi: 10.1111/j.1751-7176.2009.00140.
Mann SJ. Redefining beta-blocker use in hypertension: selecting the r ight be ta -b locker and the r ight patient. Journal of American Society Of Hypertension, 2017, Jan; 11 (1): 54-65Newer β -blockers
Emerging evidence suggests that β-blockers are losing their pre-eminent place as first-line antihypertensive agents. This is based on the head to head trials where it was found that β-blockers are less effective than ACEIs or CCBs at reducing the risk of diabetes and stroke. This was particularly true in pat ients taking β-blockers and diuretics. In most of the studies, the β-blocker used was atenolol and in the absence of substantial data on other agents it would not be appropriate to apply this conclusion to all β-blockers. β - blockers reduce central aort ic pressure to a lesser extent than other classes and this is additional reason for lack of mortality reduction with their use. They also have limitations in patients with dyslipidemia and impaired glucose tolerance. However, they are used in young hypertensives, those with stable and unstable angina and post-MI patients with hypertension. Agents with intrinsic sympathomimetic activity and highly selective β-blockers such as b isoprolol and nebivolol have lesser metabolic adverse effects. Labetalol is an α and β blocker and is the drug of choice for hypertension in pregnancy.Other drugs
α-blockers: Prazosin, terazosin and doxazosin - effectively reduce blood pressure both as monotherapy and in combination. They have a special place in the management of elderly hypertensives with benign prostatic hyperplasia (BPH) and CKD. 12,95,96 Since postural hypotension can occur, the dose of α-blockers should be carefully up-titrated. Data from the Antihypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT) shows that patients in the doxazosin - based arm had 25% increase in the cardiovascular events and twice the risk of congestive heart failure.97
These agents are not to be used as first, second or third line agents. They are
Table 16: Guidelines for selecting the most appropriate first- line antihypertensive drugs
Class of drugs Definite Indication/s
Possible indication/s
Definite contraindication/s
Relative contraindication/s
Diuretics Heart failureElderly patientsSystolic hypertension
Diabetes Gout Dyslipidaemia
CCBs Metabolic syndromeAnginaElderlySystolic hypertensionDiabetes
Peripheral vascular diseaseCVA
Heart blocka Congestive heart failurea
ACEIs Metabolic syndromeHeart failureLeft ventricular dysfunctionPost-myocardial InfarctionSignificant proteinuriaDiabetes
CVA Pregnancy and lactationBilateral renal artery stenosisHyperkalemia
Moderate renal failure (Creatinine levels >3 mg/dl)
ARBs Metabolic syndromeDiabetes mellitusProteinuriaLV dysfunctionACE inhibitor induced cough
Heart failureCVA
Pregnancy and lactationBilateral renal artery stenosisHyperkalemia
Moderate renal failure (Creatinine levels >3 mg/dl)
aVerapamil or diltiazem
Table 17: Guidelines for other drugs
Class of drugs Definite Indication/s
Possible indication/s
Definite contraindication/s
Relative contraindication/s
β –blockers AnginaPost-myocardial infarctionTachyarrhythmiaHeart failure
PregnancyDiabetes
Heart block DyslipidaemiaPhysically activePeripheral vascular diseaseElderly persons > 50 yearsAsthma and chronic pulmonary disease (COPD)
α blockers (Doxazosin, Prazosin)
Prostatic hypertrophyChronic Kidney Disease
Glucose IntoleranceDyslipidemia
Orthostatic hypotensionCongestive Heart Failure
Centrally acting agentsα methyldopa Hypertension in
PregnancyResistant Hypertension
Acute or Chronic Liver Disease
Clonidine Resistant Hypertension
CKD Pregnancy, Lactation
Vasodilators (Hydralazine)
Resistant Hypertension Hypertension in Pregnancy
Coronary Artery Disease

25 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
generally used as an add-on therapy in resistant hypertension.
C e n t r a l l y a c t i n g d r u g s : α - m e t h y l d o p a , c l o n i d i n e a n d
moxonidine have been in use for severa l years . Met hyldopa i s an important agent for the treatment of hypertension in pregnancy. Clonidine,
though a potent antihypertensive agent, is infrequently used these days due to side effects such as postural hypotension, anticholinergic effects and problem of withdrawal-related rebound hypertension. These agents are used in patients of Chronic Renal Failure (CRF) with resistant hypertension.
Direct vasodilators: Hydralazine and minoxidil - are effect ive, but some of their side effects (such as tachycardia, headache, and retention of sodium and water ) may make it difficult to use them in modern day treatment of hypertension.
Racemic forms: of calcium channel blockers and β-blockers are presently available. However, long-term studies regarding their efficacy and safety are not available.
For a g iven pat ient the choice of agent amongst the f ive c lasses depends on age, risk factor profile and associated diseases of the patient. Table 16 presents guidelines for selecting the most appropriate antihypertensive drugs. Table 17 shows the commonly used dosages and the various agents in each class. Table 18 delineates the special circumstances in which other agents are used as add on therapy after the first line drugs have been used in combinations. The Table 19 lists some common side effects of these drugs which should always be kept in mind.
Antihypertensive Drug Combinations
Combination therapy is the method for effective control of hypertension since a majority of patients will require two or more drugs for sustained and effective control of blood pressure.12,13
O n e o f t e n n e e d s t o c o m b i n e different classes of drugs with different mechanisms of ac t ion to achieve effective control of blood pressure with minimal side effects. Combinations with addit ive hypotensive effects will produce greater blood pressure reductions than those obtained with monotherapy. When a subject is in stage 2 or above, therapy can be initiated either with two drugs or as a fixed dose combination. The ACCOMPLISH trial has shown that combination of ACEIs with CCBs is better than a combination of ACEI with diuretic and should be the preferred combination.98
Younger individuals have high renin
Table 18: Anti-hypertensive drugs and their usual dosage
Class Drug Dosage (mg/day) Dosing frequency/DayDiuretics Hydrochlorothiazide 6.25-12.5 1–2
Chlorthalidone 6.25-12.5 1 Indapamide 1.5-2.5 1Amiloride 5-10 1–2Triamterene 50-100 1–2Spironolactone 25-50 1–2
β -blockers Metoprolol 25-100 1–2Bisoprolol 2.5-10 1Nebivolol 2.5 - 5 1
α + β Blocker CarvedilolLabetalol
3.125 – 5050 -200
22
CCBs Amlodipine Cilnidipine Diltiazem Nifedipine (Long-acting) VerapamilBenidipineEfonidipine
2.5-20 5 – 1090-360 10 – 4080-240
4-820-40
1 11 1
1-2 11
Racemic isomers S-amlodipine 2.5 - 10 1ACE inhibitors Enalapril 2.5-20 1-2
Lisinopril 2.5-20 1Ramipril 1.25-10 1-2Perindopril 2-8 1-2
ARBs Losartan 50-100 1-2Candesartan 8-32 1-2Valsartan 40-160 1Irbesartan 150-300 1TelmisartanOlmesartanAzilsartanFimasartan
40-16020 - 4040 - 8060 - 120
1111
α -blockers Prazosin 2.5-10 2-3Doxazosin 1-4 1
Centrally acting drugs Clonidine 0.1-0.3 2MethyldopaMoxonidine
500-15000.2-0.4
21-2
Vasodilators HydralazineMinoxidil
25-100mg2.5-5mg
21-2
Table 19: Adverse drug reactions of anti-hypertensive drugs
Common side effects ACE inhibitor ARB Calcium channel blocker Diuretic B-blockerHeadache - - + - -Flushing - - + - -Lethargy - - - - +Impotence - - - + +Dry cough + +/- - - -Gout - - - + -Oedema - - + - -Postural hypotension + + - + -Cold hands and feet - - - - +Hyperkalemia + + - - -Hyperglycemia + +Dyslipidemia + +Angioedema + +

26 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
hypertension, hence ACEIs/ARBs or newer β-blockers are preferred; while older individuals have low renin hypertension and hence diuretics or CCBs are preferred as first line agents.
In combination, one out of the two groups A [ACE inhibitor/ ARB] or B [β-
blocker] is combined with C [calcium channel blocker] or D [thiazide diuretic] (step 2). In refractory patients, when 3 agents are to be used, A+C+D is a good choice (step 3). 13 The stepped care approach for physicians suggested by the present IGH IV guidelines for
combination therapy in hypertension is shown in Figure 4.
Certain drug combinations have synergistic effect and increase the e f fec t iveness o f the o ther agent . However, some combinations are not effective and are thus undesirable and not suggested to be used. These are shown in Table 20.
Drug Interactions
Since mult iple drugs are used in hypertensive patients and often these patients have other co-existing condit ions , certain common drug interactions should be kept in mind, as shown in Table 21.99
The sequence of drug therapy after choosing an initial agent depends on the response to the first. In case target BP is not achieved, combination should be used in a manner shown in Figure 5.
Younger Older
Step 1
Step 2
Step 3
Step 4 Resistant Hypertension:Add MRA-spironolactone, if side effects then use eplerenone
Step 5 Add Alpha blocker or beta blocker. In special situationscentrally acting drugs or direct vasodilators
A : ACE Inhibitor or angiotensin receptor blocker B : β-blockerC : Calcium Channel Blocker D : Diuretic (thiazide)
A
A
A
C or D
C or D
C D
+
+ +
*Combination therapy involving B and D may induce more new onset diabetes compared with other combination therapies. Use β blockers only in special situations. B = Newer β blockers. Younger age: 55 years. MRA=Mineralocorticoid receptor antagonist
Fig. 4: Algorithm for recommended drug combination
Table 20: Undesirable combinations
• Β-blocker and ACE inhibitor• Β-blocker and centrally acting drugs• Β-blocker and verapamil/diltiazem• ACE inhibitors and ARBs• Two drugs from the same class
Table 21: Drug interactions99
ACE inhibitors and diureticsNSAIDs including COX-2 inhibitors decrease efficacy of diuretics and ACE inhibitors Calcium channel blockers Verapamil increases the blood levels of several statins, such as atorvastatin, simvastatin and lovastatin Cyclosporin levels are increased with diltiazem and verapamil DiureticsSteroids can worsen diuretic-induced hypokalemia and reduce their effectiveness.Antiarrythmics of Class 1A (quinidine or procainamide) or Class III (sotalol, amiodarone) can prolong QT interval and may precipitate torsade de pointes in presence of diuretic-induced hypokalemia Combined use of ACE inhibitors or ARBs and potassium sparing diuretics may result in hyperkalemia β blockers Metoprolol and carvedilol metabolism is inhibited by paroxetine (Selective serotonin receptor blocker – antidepressant) and propoxyphene (opoid analgesic) resulting in increased antihypertensive effect β blockers and Concomitant use of non-dihydropyridine CCBs can result in Heart Blocks α methyldopa Concomitant use of tricyclic antidepressants with methyldopa is to be avoided
Fig. 5: Algorithm for treatment
After initial antihypertensive drug treatment
Goal blood pressure achievedGoal blood pressure
not achieved after 1 months Significant side effects
• See every 3 months (high & very high risk) and every 6 months (medium & low risk)
• Monitor BP & risk factors reinforce lifestyle measures
• Encourage HBPM to improve compliance and patient participation
• Substitute a drug or low dose combination from other classes
or
• Reduce dose and add a drug from another class
Hypertension difficult to manage
Refer to specialist physician or clinic
• If partial response, add a drug from another class and increase the dose of the first agent. Do not hesitate to use three agents in case target BP not achieved . Single pill combination of 3 agents also are available in our country
• Intensify lifestyle measures

27 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Maintenance and Follow-up of Therapy
O n c e t h e r a p y w i t h p a r t i c u l a r antihypertensive drugs is instituted, patients need to be seen at frequent i n t e r v a l s d u r i n g t h e p e r i o d o f s tabi l izat ion in order to monitor changes in blood pressure and see whether non-drug measures are being strictly followed. At least once in a fortnight, blood pressure should be measured at the clinic or at home. Other CHD risk factors as well as co-existing diseases/conditions should be monitored. The overall risk category of a patient and the level of blood pressure decide the frequency of follow up visits to a large extent. The frequency can be reduced once BP is stabilized and other risk factors are controlled. Tobacco avoidance and alcohol moderations must be promoted vigorously.
Associated Therapies
In order to reduce the overal l risk, patients with hypertension need therapies for control of other risk factors for secondary prevention and now with
recent available data even for primary prevention. Low dose aspirin should be prescribed to all hypertensives wi th card iovascular d i sease and stroke (secondary prevention). All hypertensive patients with coronary, p e r i p h e r a l , o r c e r e b r o v a s c u l a r disease with LDL levels >100 mg/dL should receive statins as secondary prevention strategies. Hypertensive pat ients without CV diseases but those in high-risk group should also receive statins for primary prevention as shown in the recently published HOPE III trial. Rosuvastatin 10 mg/day resulted in greater benefit than even antihypertensive drugs in a high risk hypertensive population.10,100,101
Aspirin has no role as a concomitant therapy in patients of hypertension without evidence of ASCVD. Recently, three primary prevention trials the ASCEND, ARRIVE and the ASPREE tr ial looked at role of aspirin for primary prevention in elderly (ARRIVE and ASPREE) and diabetic (ASCEND) individuals . Al l three tr ia ls were negative for any benefit. Thus, aspirin does not have any role as a primary
preventive agent.102-104
Newer Modalities
A n o ve l b a r o r e f l e x a c t i va t i o n therapy has been evaluated recently. It stimulates baroreceptors through an implanted device and has been shown to reduce significant change in BP in patients with resistant hypertension. This therapy is still experimental and has no clinical application as yet.
Renal sympathetic denervation therapy has been evaluated. In this radiofrequency ablation of sympathetic p l e x u s a r o u n d r e n a l a r t e r i e s i s p e r f o r m e d . I n t h e S Y M P L I C I T Y hypertension -2 trial,105 it was shown to reduce BP significantly over and above the pharmacological therapy. However, the more recent and meticulously conducted SIMPLICITY III trial has not shown any effect on BP reduction with renal denervation compared to sham controlled placebo therapy. Thus, renal denervation therapy is presently still under evaluation and is not advocated for routine clinical use.

28 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Th e p r e v a l e n c e o f s e c o n d a r y hypertension is around 5-6% of
al l hypertensives. Because of low prevalence, rout ine screening for s e c o n d a r y h y p e r t e n s i o n i s n o t essential and cost effective. Renal disease constitutes the major group of secondary hypertension.When to suspect secondary hypertension clinically?
• Absence of fami ly h is tory of hypertension
• Severe hypertension > 180/110 mm Hg with onset at age < 20 years or > 50 years
• Di f f i cul t - to - t reat or res is tant hypertension with s ignif icant end-organ damage features
• Combination of pain (headache), palpitation, pallor and perspiration – 4 P’s of phaeochromocytoma
• Polyuria, low eGFR, nocturia, p r o t e i n u r i a o r h e m a t u r i a – indicative of renal diseases
• Absence of peripheral pulses, b r a c h i o f e m o r a l d e l a y a n d abdominal or peripheral vessel bruits
• His tory o f polycys t i c k idney disease or pa lpable enlarged kidneys
• Cushingoid features, multiple neurofibromatosis
• Significant elevation of plasma c r e a t i n i n e w i t h u s e o f A C E inhibitors
• Hypertension in children• H i s t o r y o f s n o r i n g , d a y t i m e
somnolence, obesity, short and thick neck – Obstructive Sleep Apnoea
A. Hypertension in Chronic Kidney Diseases
Hyper tens ion , a f t e r d iabe tes mellitus, is the second leading cause of end stage renal disease (ESRD) and together these entities account for over 60% of ESRD patients107 E s s e n t i a l h y p e r t e n s i o n i s a n important cause of chronic kidney disease and renal parenchymal d i sease i s a wel l -es tab l i shed cause of secondary hypertension. In India diabetic nephropathy contributes to 30% of cases of CKD while hypertensive nephropathy and chronic pyelonephritis each
contribute to 10% cases of chronic renal failure.108
There are two forms of kidney diseases causing hypertension namely renal parenchymal and renovascular.
• Causes: Renal parenchymal diseases –
(Non-diabetic)107,108,109
- Chronic glomerulonephritis
- C h r o n i c i n t e r s t i t i a l nephritis
- Analgesic nephropathy - Polycystic kidney disease - Gout with renal failure - Obstructive nephropathy • Stages of Chronic Kidney
Diseases and Action Plan The funct ional s tages are
based on estimated GFR in CKD with the relevant action plan as below.111
Treatment Therapy with antihypertensives in
CKD has been found to not only control BP but also slow down the progression. The Ramipril Efficacy in Nephropathy (REIN), ACEI and progressive Renal Insufficiency ( A I P R I ) a n d m o d i f i c a t i o n o f Dietary Protein in Renal Disease (MDRD) trials established the ability of antihypertensives to slow down the progression of non-diabetic chronic kidney disease.112-
115
Threshold for initiation of Anti-Hypertensive Treatment
a. BP 140/90 Hg for pat ient without proteinuria
b. BP 130 /80 for those wi th proteinuria Target to achieve: BP < 130/80mmHg
In post renal transplant patients, hypertension is an important issue s ince certain drugs l ike cyclosporine and erythropoietin u s e d i n t h e s e p a t i e n t s c a n aggravate hypertension. At times, combination of multiple drugs including ACEI, ARB, CCB and diuretics may be required for effective BP control.110 In patients
Secondary Hypertension
Table 22: The percentage prevalence of various causes of Hypertension106,107
A. Primary or Essential 94-95%B. Secondary Renal Renal parenchymal 2-3% Renovascular 1-2% Endocrinal 0.3-1% Primary aldosteronism Phaeochromocytoma Cushing’s Syndrome Acromegaly Vascular – Coarctation of aorta Nonspecific
aortoarteritis Drugs – Oral Contraceptives,
NSAIDs Steroids, Cyclosporine
0.50%
Miscellaneous Obstructive Sleep apnoea
0.50%
Table 23: Staging system and action plan for chronic kidney disease
Stage Description GFR# (mL/min
per 1.73 m2)
Action*
– At increased risk for CKD
> 90 with risk factorsΨ
Screening CKD risk reduction
1 Kidney damage¥ with normal or increased GFR
> 90 Diagnosis and treatment.Retard progression of CKD.Treat comorbidities.Cardiovascular disease risk reduction.
2 Mild decrease in GFR
60-89 Estimate progression
3 Moderate decrease in GFR
30-59 Evaluate and treat complications
4 Severe decrease in GFR
15-29 Prepare for renal replacement therapy
5 Kidney failure
< 15 or dialysis
Renal Replacement Therapy if uremic
#Estimated GFR (eGFR) using Modification of Diet in Renal Disease (MDRD) formula: GFR (mL/min/1.73 m 2) = 186 x (Pcr) -1.154 x (age) -0.203 x (0.742 if female) x (1.210 if African American); *Includes actions from preceding stages; ΨRisk factors : hypertension, dyslipidemia, diabetes mellitus, anemia, systemic lupus erythematous, chronic analgesic ingestion; ¥Kidney damage as manifested by abnormalities noted on renal pathology, blood, urine or imaging tests.

29 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
where BP is still not controlled, clonidine, α methyl dopa or α blockers may be added.
Renovascular • The most common cause of
renovascular hypertension in India is Takayasu’s syndrome (progressive aortoarteritis),116
t h o u g h a t h e r o s c l e r o t i c renovascular disease is also being recognised more often now in early patients.
• T h e m o s t c o m m o n c a u s e of renovascular disease in We s t e r n p o p u l a t i o n a r e atherosclerotic disease in 60% of elderly population and fibromuscular dysplasia in 35% of young. Atherosclerotic renal artery stenosis patients o f t e n h a v e a s s o c i a t e d cardiovascular disease.
• Rare causes include embolic and tumor, thrombus and extrinsic reasons.
• Takayasu’s disease is a non-specific panarteritis affecting young women. Hypertension i s m a i n l y d u e t o r e n a l artery stenosis which can be unilateral or bilateral.116
• R e n o va s c u l a r d i s e a s e i s much more common than renovascular hypertension (RVH).
• Atherosclerotic disease usually involves the proximal segment while fibromuscular dysplasia involves the distal part of renal artery.
Investigations : • A paraumbilical bruit is heard
in 50-60% of patients with renovascular hypertension and 10% cases of essential hypertension. A diastolic renal bruit is more specific than systolic bruit.
• In patients with moderate d e g r e e o f s u s p i c i o n o f renovascular hypertension, n o n - i n v a s i v e t e s t s a r e recommended initially.
• Wherever there i s a h igh degree of suspicion, direct selective renal arteriography is recommended.
• Colour Doppler Ultrasound (CDUS) , CT angiography
and MRI angiography are other good and non-invasive modalities. MRI angiography has higher sensitivity (90%) and specificity (92%).
• 9 9 Tc – D T PA a n d 1 2 3 I – Hippuran scan are useful non-invasive investigations. These tests give functional status of CKD.
• Conventional angiography, though invasive, is the gold s t a n d a r d . I n t r a - a r t e r i a l i n j e c t i o n w i t h d i g i t a l s u b t r a c t i o n a n g i o g r a p h y (DSA) may be used. Once the diagnosis is confirmed, renal angioplasty with stent ing s h o w s s i m i l a r r e s u l t s a s medical therapy.
Treatment of renal artery stenosis G o a l s a r e c o n t r o l o f B P a n d
preservation of renal function. In general there are three options. :
Medical Percutaneous transluminal
renal angioplasty Surgery Pa t i e n t s w i t h f i b r o m u s c u l a r
dysplasia benefit from angioplasty or surgical revascular isat ion. Pa t ients wi th a therosc lero t i c r e n o va s c u l a r d i s e a s e d o n o t demonstrate any significant benefit from renal artery intervention but medical therapy is equally effective in these patients.116 as shown in the ASTRAL study published in 2009 and the more recent CORAL study in 2014.117-118 Renal artery s tent ing does not confer any benefit to prevent clinical events when added to medical therapy in patients of renal artery stenosis with hypertension or CKD.
B. Endocrine causes Pheochromocytoma • These chromaffin cell tumors
are mostly adrenal. • These may be extra-adrenal in
15% of the cases and bilateral adrenal in 10% of the cases. 10% of all cases are familial and 10% are malignant.
• E p i s o d i c h y p e r t e n s i o n , postural fall, pallor, throbbing headache, palpitations and perspiration are suggestive clinical features.118
• Invest igat ions : Screening tes ts inc lude p lasma and urinary biochemical assay f o r f r e e c a t e c h o l a m i n e s , metanephrines and vanillyl-mandelic acid (VMA). These tests have high specificity ( 9 9 % ) a n d s e n s i t i v i t y (85-90%). Following drugs should be withdrawn for 48 hours before doing these tests: α methyldopa, β blockers, c l o n i d i n e , p e n i c i l l i n a n d certain vegetables. Patients can be continued on CCBs and ACE inhibitors during evaluation.
• Tumor localisation: Computed Tomography scan and MRI of the abdomen have greatly simplified tumor localisation; MIBG labelled with I is the most specific way of diagnosing adrenal and extra adrenal p h e o c h r o m o c y t o m a s . 1 1 9 Other modalities include PET scan using18 F-fluorodeoxy glucose.
• Once localised, surgery should be offered to all the patients. Mortal i ty from surgery is now less than 5%. For pre-operative preparation, control of blood pressure is important and can be achieved with oral phenoxybenzamine 10 mg once daily, to be increased slowly. Oral prazosin and terazosin preferentially block post-synaptic α1-receptors on vessel wall and leave pre-synaptic α 2- receptors. As a result, tachycardia is less of a problem. Β-blockers may be given to these patients to control tachycardia and a r r h y t h m i a s , o n l y a f t e r α-blockers have been started. Two third of pat ients can be operated by minimally invasive surgery. One third require open surgery. Post-operative hypotension and hypoglycemia can be managed by continuous monitoring.120,121
Primary Aldosteronism • It is due to excess aldosterone
s e c r e t i o n b y t h e a d r e n a l cortex secreted generally by adenomas and occasionally

30 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
due to bilateral adrenocortical hyperplasia.
• This is suspected in a case of hyper tens ion showing p e r s i s t e n t h y o k a l a e m i c metabolic alkalosis in the absence of diuretic therapy.
• Plasma Aldosterone to Plasma Renin Activity (PRA) ratio more than 20 to 25 (normal < 10) is 95% sensitive and 75% spec i f i c for Pr imary Hyper Aldosteronism. It is usually diagnosed by imaging techniques.
Cushing’s Syndrome • Hypertension is present in
approximately 80% of patients with Cushing’s syndrome.
• Other clinical features include central obesity, hirsutism, polycythemia and pink striae on the abdomen.
• T h i s c a n b e s c r e e n e d b y performing early morning s e r u m c o r t i s o l l e v e l s . Hypertension remits in most p a t i e n t s a f t e r s u c c e s s f u l treatment.
Miscellaneous • Other important secondary
causes include: • Oral contraceptives • T h y r o i d d i s o r d e r s , b o t h
h y p o t h y r o i d i s m a n d hyperthyroidism
Other causes
• C o a r c t a t i o n o f a o r t a , a c o n g e n i t a l d i s e a s e n e e d s surgical correction
• S leep apnea syndrome i s one of the common causes of reversible hypertension. P o l y s o m n o g r a p h y i s diagnostic. No specific drugs
h a ve p r o ve n s u p e r i o r i n sleep apnea but use of C-PAP improves the hypertension
• Acute stressful situations cause intense sympathetic discharge and may temporarily induce h y p e r t e n s i o n . Β b l o c k e r s a r e p r e f e r r e d . C o m m o n c o n d i t i o n s i n c l u d e a c u t e mental stress, hypoglycaemia, acute intermittent porphyria, e x p o s u r e t o c o l d , b u r n s , perioperative period and post head injury
• Drugs: Non-steroidal anti-i n f l a m m a t o r y d r u g s , sympathomimetic amines, ephedrine, glucocorticoids, cocaine and amphetamines c a n a l l c a u s e s i g n i f i c a n t hypertension.

31 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
The complications of hypertension c a n b e c o n s i d e r e d e i t h e r
h y p e r t e n s i ve o r a t h e r o s c l e r o t i c . Although the extent of damage often correlates with the level of blood pressure, it is not always the case. Blood pressure and organ impairment should be evaluated separately. The various complications are as follows:1. Hypertensive Heart Disease • H y p e r t e n s i o n h a s t h e
following effects on the heart: left ventricular hypertrophy, increased risk of coronary artery disease, arrhythmias, congest ive cardiac fai lure ( H F n E F a n d H F r E F ) a n d sudden death.122
• M o s t e p i s o d e s o f l e f t v e n t r i c u l a r f a i l u r e i n hypertensive pat ients are associated with diastolic heart dysfunction.
• Treatment of hypertension c a n r e v e r s e v e n t r i c u l a r hypertrophy.123,124 However, the impact of reduction of LVH on reduction of morbidity and mortality is still debated.
2. Cerebrovascular Disease • Hypertension is the most
i m p o r t a n t m o d i f i a b l e risk factor for all types of atherothrombotic stroke125 and intracerebral haemorrhage due to rupture of Charcot-Bouchard aneurysms.
• The re la t ion between the incidence of stroke and blood pressure is continuous.126,127 A 5-6 mm Hg reduction in d i a s t o l i c b l o o d p r e s s u r e reduces the risk of stroke by 40%.128
• T h e S H E P ( S y s t o l i c H y p e r t e n s i o n E l d e r l y P r o g r a m ) s t u d y s h o w e d substantial benefit following con t r o l o f sy s t o l i c b lood pressure in the elderly.56
3. Kidney • About 20-25% of renal failure
is attributed to uncontrolled hypertension.129
• D e v e l o p m e n t o f r e n a l d a m a g e i s p r e c e d e d b y
microa lbuminur ia , which progresses to overt proteinuria and may further progress to end-stage renal disease.130
• Reduction of proteinuria can be achieved by effective blood pressure control specially with use of ACEIs and ARBs.131-32
4. Retina • Hypertensive retinopathy is
a condition characterized by a spectrum of retinal vascular signs in people with elevated blood pressure.
• The classification of Keith, Wa g e n e r a n d B a r k e r h a s been widely used. Grade I retinopathy is characterized by copper wire appearance; Grade II by arteriovenous nipping; Grade I I I by the presence of haemorrhages and exudates; and Grade IV by papilloedema.
• Grade III and IV retinopathy i s s e e n i n l o n g s t a n d i n g uncontrolled hypertension. These changes may regress with effective control of blood pressure.
• S e v e r a l r e v i e w s o f hyper tens ive re t inopathy since 1996 have questioned the usefulness of the classification system by Keith, et al and its relevance to current clinical p r a c t i c e . R e c e n t s t u d i e s show that some of the retinal s igns (e .g . , hemorrhages , microaneurysms and cotton-wool spots) predict stroke a n d d e a t h f r o m s t r o k e independently of elevated blood pressure and other risk factors.133
5. Large Vessel Disease • Hypertension is a risk factor for
development of intermittent claudication. It also increases the risk of abdominal aortic a n e u r y s m s a n d a o r t i c dissection. Eighty percent of patients with aortic dissection have hypertension.134
6. Hypertensive crises Hypertensive crises are classified
as hypertensive emergencies or urgencies.
Hypertensive emergencies: H y p e r t e n s i v e e m e r g e n c i e s
( M a l i g n a n t H y p e r t e n s i o n ) a r e c h a r a c t e r i z e d b y s e ve r e elevations in BP (>180/120 mm Hg) complicated by evidence o f impending or progress ive target organ dysfunction. They require immediate BP reduction (not necessarily to normal) often with parenteral agents over a period of 6-8 hours with constant monitoring, to prevent or limit H M O D . E x a m p l e s i n c l u d e hypertensive encephalopathy, intracerebral hemorrhage, acute myocardial infarction, acute left ventricular failure with pulmonary edema, unstable angina pectoris, aortic dissection, or eclampsia.2 IV nitroglycerine is generally used although it is not very effective, but specially useful in patients with ischaemic heart disease and lef t ventr icular fa i lure . 135 The recommended dose is initially 5mcg/min, then titrate by 5 mcg/min at 3 to 5 minute intervals, upto 10 mcg/min. Intravenous enalaprilat is useful in hypertensive emergencies, specially in presence of heart failure. It is used in dosages of 0.625 – 1.25 mg bolus every 6 hours. IV Labetalol is also being used in hypertensive emergencies in a bolus dosage of 2-10 mg and infusion of 2.5-30 mcg/kg/min. IV esmolol has been shown to be specially useful for peri-operative accelerated hypertension. Usual bo lus dose i s 80 -500 mcg/kg over 1 minute followed by an infusion of 50-300 mcg/kg/min. IV nitroprusside is required rarely, in situations like dissection of aorta and subarachnoid haemorrhage with very high blood pressure. It requires intensive care setting and very close monitoring. The dose is 0.3 mcg/kg/min to a maximum of 4 mcg/kg/min. Sublingual captopril can also be used when less rapid reduction is required.
Hypertensive urgencies H y p e r t e n s i v e u r g e n c i e s
( A c c e l e r a t e d H y p e r t e n s i o n )
Complications

32 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
are situations associated with severe elevations in BP without p r o g r e s s i v e t a r g e t o r g a n dysfunction. Examples include upper levels of stage II hypertension associated with severe headache, shortness of breath, epistaxis, or severe anxiety. The majority o f t h e s e p a t i e n t s p r e s e n t a s noncompliant or inadequately
treated hypertensives, often with little or no evidence of HMOD.
The aim should be safe, prompt and gradual lowering of blood pressure with oral medication over a period of 1-3 days.136 In most urgencies, blood pressure can be controlled with rapidly acting oral medications like calcium channel
blockers and ACEI/ARB. Sublingual nifedipine should not
be used in hypertensive crises as it can cause precipitous fall in blood pressure, reflex tachycardia and may precipitate renal, cerebral or coronary ischaemia.137

33 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Hypertension with Diabetes Mellitus
• 30% to 35% of hypertensive patients are detected to have co-existing diabetes mellitus. Similarly, the prevalence of hypertension is 1.5 to 2 times greater in patients with diabetes mellitus as compared t o n o n - d i a b e t i c s s u b j e c t s . 1 3 8 Co-exis tence of d iabetes and hypertension leads to increased cardiovascular morbidity and mortality. The progress of type 2 diabetes in India is increasing at a very fast pace and this is likely to also contribute to a significant burden of hypertension.139
• B l o o d p r e s s u r e s h o u l d b e measured on each visit of the diabetic patient and the procedure for measurement is the same as in ordinary hypertensive patients. In diabetic population it is imperative to measure the blood pressure in supine, sitting and standing positions to exclude the possibility of autonomic neuropathy.
• Some of the earl ier tr ials l ike UKPDS 140 and HOT 141 showed evidence in favour of treating h i g h n o r m a l b l o o d p r e s s u r e aggressively but subsequently, in the ESH/ESC Guidelines 2007, no definitive data was available to substantiate this. Therefore, it is recommended that in high normal blood pressure, more aggressive l i f es tyle measures should be followed while a blood pressure of more than 140/90 mmHg should be treated with pharmacotherapy to achieve cardiovascular and m i c r o va s c u l a r p r o t e c t i o n . I n pat ients with diabetes , b lood pressure targets should be less than 140/80 mmHg.142
• In the management of diabetic h y p e r t e n s i v e s , l i f e s t y l e modifications have to be more aggressive.
• Lifestyle measures include weight loss in case of obese , dietary changes like low salt and low fat. Regular exercises form the basis and are applicable at all stages of hypertension
• It has been proven that it is useful
and effective to treat hypertension in people above the age of 65 years.143
• I t h a s b e e n o b s e r v e d t h a t to effectively lower the blood pressure a combination of two or more drugs are required for controlling the blood pressure to target levels. ACEIs in the HOPE triall83 and ARBs in the ONTARGET t r i a l l 8 6 h a ve e m p h a s i s e d t h e importance of RAAS blockade to reduce the risk of complications of diabetes, specially microvascular complications and macrovascular complications. Therefore, ACEIs in type 1 diabetes are recommended as the first line drug therapy while ARBs may be used in patients who have type 2 diabetes or who are intolerant to ACE inhibitors.
• CCBs have been shown to be useful as monotherapy and in combination with ACEI in the ASCOT trial.57 The combination of amlodipine and perindopril was associated with significantly less incidence of new onset diabetes as compared to the combination of β-blocker and diuretic.
• β - b l o c k e r s p o t e n t i a l l y m a s k h y p o g l y c e m i c s y m p t o m s . β-blockers are falling into disrepute i n a n o r d i n a r y h y p e r t e n s i ve patient but in diabetic population with evidence of coronary artery d isease and congest ive hear t failure they may be quite useful. It is recommended that we may use cardioselective β-blockers like nebivolol and carvedilol. α blockers can also be used as a useful adjunct in the treatment of the above clinical scenario.
• The ACCORD trial (2010) has shown benefits of effective BP control in diabetic patients. It shows targeting a SBP of <120 as compared to <140 did not reduce composite outcome in diabetic population.144 A subgroup analysis of a high risk population l ike the one in SHIFT trial showed benefit of more tight control in the diabetic population also.140 Another analysis shows intensive BP treatment benefit was observed amongst pat ients undergoing
standard glycemic controls even amongst those without additional risk factors.145
• T h e A D VA N C E t r i a l 1 4 6 a n d INVEST trial147 show definitive improvement in the microvascular complications specially on kidneys but their effect on eye and neural complications is questionable. T h e r e w a s a s h i f t t o w a r d s improvement in macrovascular complications but it did not reach statistical significance.
• The therapy and the targets need to be individualized for each patient depending on age , comorbid conditions, cost factor and socio-psycological factors.
• The drugs which are useful in diabetic pregnant patients who are hypertensive include methyldopa, calcium channel blockers and l a b e t o l o l . T h e u s e o f A C E inhibitors/ARBs is contraindicated. Use of diuretics during pregnancy can lead to reduction of plasma volume which can result in low perfusion resulting in decreased fetal growth / fetal damage.
• SGLT2 inhibitors (Empagliflozin, Canagliflozin and Dapagliflozin) have been evaluated recent ly amongst diabetic patients in three large trials (EMPA-REG, CANVAS Program and DECLARE-TIMI 58). These agents have significant CV benefits and reduce blood p r e s s u r e . T h e y r e d u c e B P significantly in patients of diabetes or hypertension irrespective of the level of BP. This is a class effect seen with all these three agents. In the EMPA-REG trial there was a 38% relat ive r isk reduct ion in death from CV causes, 35% risk reduction in hospitalization for heart failure. There is also a significantly reduced progression of kidney disease and renal events with these agents.148-150
Hypertension with Cerebrovascular Disease
• Excessive and sudden elevation o f b l o o d p r e s s u r e i s m o r e often associated with cerebral haemorrhage than infarct ion. Moderate reduct ion in b lood
Hypertension in Special Situations

34 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
pressure is prognostically more rewarding in haemorrhagic stroke than in ischemic stroke.12
• Hypertensive encephalopathy is an emergency that needs to be identified and aggressively managed.
• In acute cerebrovascular disease, the goal is to gradually reduce the blood pressure and carefully monitor it for the first 24 hours in view of the possibility of transient hypertension.
• Treatment of acute BP elevation in cerebral haemorrhage has been addressed in two recent trials – the INTERACT 2 (2013) and the ATACH II trial (2016) have looked at benefits of intensive BP lowering in patients with acute cerebral haemorrhage. Both these trials show that early intensive lowering to less than 140 as against target of <180 has no mortality benefit although there was some improved functional outcome.151,152 We r e c o m m e n d i n i t i a t i o n o f ant ihypertensive therapy and continuous monitoring only when BP is more than 220 systolic and it should be maintained below 180/105 mm Hg.1
• Immediately after the occurrence of an ischemic cerebral infarction, it is appropriate to withhold treatment in pat ients who present with high blood pressure, unless blood pressure is very high (>220/120 mm Hg). In such patients a cautious reduction in B.P. by 10 to 15% only is suggested.12
• BP should not be aggressively reduced in ischemic stroke patients who are otherwise not candidates for thrombolysis. In patients for thrombolytic therapy, SBP of > 185 and DBP of > 110 mm Hg should be actively treated and maintained below 185/105 mm Hg.153
• In post stroke patients for long term the evidence for reduction in incidence of stroke with control of blood pressure has been consistent. In clinical trials, antihypertensive therapy has been associated with reductions in stroke incidence averaging 35% to 40%.12 In stroke survivors wi th hypertens ion, blood pressure lowering therapy has been shown to result in 43% reduction in stroke recurrence.
• In the PROGRESS TRIAL, the c o m b i n a t i o n o f p e r i n d o p r i l and indapamide reduced the r i sk of s t roke by 43% among patients who were hypertensive or normotensive. Perindopril alone was not found to have a similar reduction in the risk of stroke. Hence, a combination of a ACEI and a diuretic is preferable.85
Hypertension in Women
• S o m e o f t h e s i d e e f f e c t s o f c o m m o n l y u s e d d r u g s l i k e ACE inhibitor-induced cough, CCB-induced pedal edema, and diuretic-induced hyponatremia and hypokalemia are seen more often in women than in males.12,154
• E s t r o g e n - p r o g e s t e r o n e o r a l contraceptives cause a distinct increase in sys to l i c and to a lesser extent diastolic pressure in virtually all women. Five percent women who use the pil l for 5 years develop hypertension. Age, positive family history, history of PIH and obesity are known predisposing factors for pi l l -induced hypertension.12,155 In more than one half , blood pressure returns to normal when the pill is withdrawn.
• Hormone replacement therapy ( low dose es t rogen) in pos t -menopausal women is no longer indicated.
Hypertension in Pregnancy
Hypertension can affect 5-10 % of pregnancies and remains a major cause of maternal and fetal morbidity and mortality. Maternal risks include placental abruption, stroke, multiorgan failure and disseminated intravascular coagulation. The fetal risks include in t rauter ine growth re tardat ion , prematurity and intrauterine death.
Hyper tens ion in pregnancy i s defined as office BP measurements of SBP ≥ 140 mmHG and/or DBP measurements of ≥ 90 mmHg. It is classified as Mild hypertension if BP is 140-159/90-109 mmHg and Severe hypertension if BP is ≥160/110 mmHg.
Hypertension in pregnancy includes four entities• Pre-existing hypertension/Chronic
hypertension: precedes pregnancy or develops before 20 weeks of
gestation, and usually persists for more than 6 weeks post-partum
• Gestational hypertension: develops after 20 weeks of gestation, without significant proteinuria and usually resolves within 6 weeks post-partum.
• Pre-eclampsia: gestational hypertension with significant p r o t e i n u r i a ( > 0 . 3 g / 2 4 h or ≥30 mg/mmol ACR). I t is usually accompanied by headache, visual disturbances, abdominal pain, or abnormal laboratory tests, specifically low platelets and/or abnormal liver function. Eclampsia is the occurrence of seizures that cannot be attributed to other causes in a patient with pre- eclampsia.
• Preeclampsia superimposed on Pre-existing hypertension
Hypertension in pregnancy is diagnosed by recording phase IV or V of Korotkoff sounds with the patient lying in a lateral position. The manual auscultation is the method of choice since automated BP machines are unreliable in pregnancy and eclampsia. Ambulatory BP Monitoring is the preferred over Home BP monitoring or office BP measurements.
Investigations during pregnancy include urine analysis, blood count, haematocrit , l iver enzymes, serum creatinine and serum uric acid. A urine protein dipstick test showing >1+ warrants eva lua t ion o f ACR with values of ≥30mg/mmol being abnormal. Additional tests include ultrasonography of the kidneys and adrenals and doppler ultrasound of the uterine arteries.
In a 2014 Meta-analysis - evaluated maternal and fetal outcomes in 49 randomized trials of treatment versus no treatment of women with mild hypertension (140-159/90-109 mmHg) during pregnancy, Treatment Did Not Result In Either Fetal Benefit Or Harm. However, antihypertensive therapy Significantly Decreased the inc idence of severe hypertension by 40 to 60 %. In a 2015 the CHIPS tr ia l (Control of Hypertension in P r e g n a n c y ) - r a n d o m l y a s s i g n e d pregnant women with gestat ional or chronic hypertension to Diastolic Blood Pressure Treatment targets of 85 mmHg (tight control) or 100 mmHg

35 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
(less tight control), and demonstrated no differences in maternal, fetal, or neonatal outcomes for the two blood pressure targets. Fewer women in the t ight group developed severe hypertension. However, there was no overall effect on perinatal morbidity or mortality. Management of hypertension in pregnancy
Amongst lifestyle changes, exercise is recommended with caution. A salt restricted diet is not recommended.
Women with a moderate to high risk of preeclampsia (previous eclampsia, CKD, diabetes mellitus, chronic hypertension, autoimmune diseases, multiple pregnancy, maternal age >40 years) should start on aspirin 100-150 mg from the 12th to 36th week of pregnancy.
In Mild hypertension in pregnancy, iniation of antihypertensive medications is considered if the BP is ≥ 140/90 mmHg along with gestational hypertension or subclinical HMOD or in any patient with BP ≥ 150/95 mmHg. A BP target of < 140/90 mmHg has been suggested. • The antihypertensive agent used
should be efficacious and safe to the mother and the foetus. Methyldopa has been evaluated most extensively and is therefore recommended for women whose hypertension is first diagnosed during pregnancy. Calcium channel blockers (nifedipine), labetalol can be used.125,126
• ACE inhibitors, ARBs, and sodium nitroprusside are contraindicated in pregnancy. Use of low dose diuretics is discouraged, since pre-eclampsia is a volume-depleted state.127
In severe hypertension in pregnancy, BP ≥170/110 mmHg is considered a medical emergency and requires immediate hospitalization. • Therapy can be initiated with
Intravenous labetolol, CCB or oral methyldopa. Intravenous hydralazine can be used but is not currently available in India. IV sodium nitroprusside is contraindicated due to the risk of fetal cyanide toxicity. IV nitroglycerine is the drug of choice in severe hypertension with pulmonary edema.
• Intravenous magnesium sulphate is the drug of choice both for prevention and treatment of seizures (eclampsia).128,129
• In some cases o f ec lamps ia ,
antihypertensive treatment fails to control hypertension and the only means of controlling hypertension would be to induce delivery.
Hypertension in the Elderly
• The prevalence of hypertension increases with age. The population of India aged 65 years and above is projected to increase from 51 million in 2005 to 65 million in 2015 and 76 million in 2020.169 A community based s tudy in Mumbai170 in 1980 showed increase in BP with age, with prevalence in 15% of total population surveyed, 34.5% in those over 55 years, 38.5% in those over 65 years and 44.4% in those over 70 years.
• In elderly population, systolic hypertension is the commonest form of hypertension. It is a better p r e d i c t o r o f c a r d i o va s c u l a r /cerebrovascular events, end-stage r e n a l d i s e a s e a n d a l l - c a u s e mortality, as compared to diastolic blood pressure.171
• Precautionsinmeasurement:Blood pressure should be measured with care in elderly subjects as some older patients may have falsely high readings due to excessive vascular stiffness. Also, as older patients are more likely to have or thos ta t i c hypotens ion , one should measure BP in supine, sitting and standing positions.
• M a n a g e m e n t : L i f e s t y l e modi f i ca t ion i s impor tant in management of hypertension in elderly and should be started in all of these patients. Losing weight and cutting down on salt can lessen and even eliminate t h e n e e d f o r b l o o d p r e s s u r e lowering medications in elderly (Trial of Non-pharmacological Interventions in the Elderly - TONE).59,172
• Treatment of hypertension in elderly nowadays is accepted as a h ighly ef fect ive medical intervention. An overview of five randomised trials have shown 34% reduction in stroke, 19% in CHD and 23% in vascular deaths, with a reduction of 12-14 mm Hg SBP and 5-6 mm Hg DBP over a five year period.173
• Drug treatment: The blood pressure should be lowered gradually in
elderly hypertensives with no more than an initial 25% decrease, even in situations requiring rapid reduction in blood pressure with medications.
• Targets for BP control are <140/80 mmHg for those aged 55-79 years. However, for those aged >80 years, a systolic BP of 140-145 mmHg is acceptable.174
• Long-ac t ing d ihydropyr id ine CCBs, specially amlodipine, are considered to be the drug of choice in these patients. The CCBs are recommended because they have been shown to be effect ive in reducing mortality and morbidity. Unless there i s a compel l ing indication to use another class of drugs.
• Low dose hydrochlorothiazide, chlorthalidone (6.25 to 12.5 mg per day) or indapamide (1.25-2.5 mg per day) can also be used. Where indicated, these could be combined with ACEIs or ARBs.162,175
• B i l a t e r a l a t h e r o s c l e r o t i c renovascular disease in the elderly m u s t b e k e p t i n m i n d w h i l e treatment with ACEIs or ARBs.
• The HYVET tr ia l and HYVET Extension both add evidence of the benefit of BP lowering in the very elderly (octogenarians) patients a n d t h e i m p o r t a n c e o f e a r l y and sustained antihypertensive treatment even in very elderly people.171,174
Isolated Systolic Hypertension
• Isolated systolic HT is more often seen in the elderly than in the young. The goal of blood pressure control in older patients should be the same as in younger patients (i.e. 140/90 mm Hg).1 However, an interim value of a systol ic blood pressure below 160 mm Hg may be necessary in elderly patients with marked systol ic hypertension, especially if they develop symptoms of giddiness and light headedness when their blood pressure is reduced to 140/90 mm Hg.
• Management of isolated systolic hypertension in the elderly is the same as mentioned in the management of hypertension in the elderly.

36 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
• Isolated systolic hypertension in the young patients, although uncommon, is often successfully treated with life style modification and long-acting β-blockers.
Orthostatic Hypotension
• This is defined as a fall in the BP of more than 20 mm Hg systolic and/or more than 10 mmHg diastolic in response to moving from supine to standing posit ion within 3 minutes.
• I t s p r e v a l e n c e i s h i g h e r i n diabetics, elderly, Parkinson’s disease. It results in symptoms of l ightheadedness, giddiness, blurring of vision or syncope. I t m a y b e a s s o c i a t e d w i t h supine hypertension or a lack o f compensatory tachycardia s u g g e s t i v e o f a u t o n o m i c insufficiency.
• All antihypertensive drugs may produce OH as a s ide e f fec t , h o w e v e r t h i s o c c u r s m o r e c o m m o n l y w i t h d i u r e t i c s , α blockers, vasodilators and ACEI. OH will influence the selection and continuation of antihypertensive drugs.
• Low BP per se is of no significance, however it should be evaluated in the clinical context.
Hypertension with Congestive Cardiac Failure
• Congestive cardiac failure is a common sequel of long standing hypertension and adequate control of BP improves mortality in these patients.
• Heart failure with normal ejection fraction (HFnEF) is an entity which is being increasingly recognized now in e lderly hypertensives who present with dyspnea. The prevalence of HFnEF is equivalent to systolic HF. The prognosis is marginally better than systolic HF. Effective and good control of BP is the mainstay of therapy. Diuretics help in symptomatic improvement in these patients. Other agents like β-blockers and positive inotropes are not useful in these patients.176-178
• Several large trials of ACEIs in pat ients with lef t ventr icular dysfunction due to hypertension h a v e p r o v i d e d e v i d e n c e o f
significant reduction of morbidity, secondary to heart failure.179
• Low dose diuretics are also used in hypertension with heart failure, particularly when associated with fluid retention.
• In patients with congestive heart f a i l u r e s t a b i l i z e d w i t h A C E inhibitors and diuretics, selective β-blockers such as metoprolol, b i s o p r o l o l a n d α - β b l o c k e r carvedilol may be used wherever indicated. Use of these β-blockers has been shown to reduce mortality. These agents should be started in low doses and then gradually increased.180-87
• Amlodipine has been found to be safe in treating hypertensive pat ients with angina and lef t ventricular failure, when added to ACEIs, low dose diuretics and digoxin.78 Other calcium channel blockers are not recommended in these patients.1
• In patients with severe hypertension and acute left ventricular failure, b l o o d p r e s s u r e n e e d s t o b e brought down rapidly to normal or slightly above normal range. This can be done by administration o f i n t r a v e n o u s d r u g s s u c h as furosemide, nitroglycerine, enalaprilat or sodium nitroprusside.
• INTER CHF Heart failure registry shows that 62% of patients with HF have HTN and it is the leading risk factor responsible for it. Other risk factors like dyslipidemia 35%, tobacco use (35%), diabetes (30%), alcohol (14%), CKD (9%), history of MI (21%) are much less common.188
• The ASIAN –HF registry of more than 5000 patients from across Asia with major participation from India shows ACEIs/ ARBs were prescribed to 77%, Bb to 79% and MRA’s to 58% patients. However, guideline recommended dose was achieved in only 13-29% of patients for the three agents. We need to use maximally tolerated guideline directed doses of these agents to improve survival as was shown in this study.189
• Recent data from the PARADIGM- HF study shows that angiotensin receptor (Valsartan)–neprilysin inhibitor (Sacubitril) - ARNI was superior to Enalapril in reducing the risks of death and of hospitalization
for heart failure. This agent should be used amongst those who do not respond optimally to ACEI/ ARB.190
Hypertension with Atrial Fibrillation
• Hypertension is an important risk factor for atrial fibrillation. Atrial fibrillation increases the risk of cardiovascular morbidity and mortality by approximately 2 to 5 fold with a marked increase in the r isk of embolic stroke. Increased left ventricular mass and enlargement of the left atrium have been identified as independent determinants of new onset atrial fibrillation. Blood pressure control appears to be strictly required when anticoagulant treatment is given because stroke and bleeding episodes are more frequent when systolic blood pressure is >140 mmHg.
• A recent metaanalys is shows that there is reduced incidence of new atrial fibrillation in patients receiving an angiotensin receptor antagonist or ACE inhibitor.
• In another recent metaanalysis191 including almost 12000 patients with systolic heart failure, and therefore at high risk of atrial f i b r i l l a t i o n , β - b l o c k e r s we r e found to significantly reduce (by about 27%) the incidence of atrial fibrillation. A history of atrial fibrillation and systolic heart failure is therefore a specific indication for using β-blockers. In patients with atrial fibrillation CHA2DS2-VASc score with points as follows (C-CHF 1, H-hypertension 1, A2-age >75 years 2, D-diabetes 1, S2prior stroke 2, V-Vascular disease 1, A-age 65-74 years 1, Sc-female sex 1) should be calculated. A score of 1 is “low-moderate” risk and we can consider antiplatelet or anticoagulation depending on patient preference. However, a score of ≥ 2 is “moderate-high” risk and these patients should be put on anticoagulation for a lifelong period. Vitamin k antagonists - Warfarin or dicoumarol is used in dosages so as to keep the INR between 2-3.192 More recently newer oral anticoagulants (NOACs), d a b i g a t r a n , r i va r o x a b a n a n d apixaban are available in India

37 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
and can be used. These have the advantage of fewer side effects, very few diet and drug interactions and no need to monitor INR on regular basis. However, these are more expensive than the vitamin k antagonists.
Hypertension with Chronic Obstructive Pulmonary Disease
• Hypertension in patients with COPD and bronchial asthma is seen. It is often precipitated by the use of systemic steroids, β-agonists or nasal decongestants. Stress also plays a significant role in the development of hypertension in these patients. It is therefore recommended that the above precipitating factors should be looked for and modified.
• Long ac t ing ca lc ium channel blockers such as amlodipine have been found to be relatively safe drugs in this group of patients.1
• ACEIs have not been found to increase bronchial reactivity in these patients. It is recommended that if cough develops, angiotensin II receptor blockers should be tried as alternative to ACE inhibitors.
• β -blockers and α-β blockers are not routinely recommended as they are known to exacerbate asthma. However, α-blockers can be used as add-on therapy in patients with COPD.193
• I n h a l e d c o r t i c o s t e r o i d s a n d ipratropium bromide can be used safely in these patients.
Hypertension with Coronary Artery Disease
A m o n g a l l t h e r i s k f a c t o r s documented for pathogenesis of CAD, hypertension is reported to be the major risk factor.133 Blood pressure levels
have been shown to be positively and continuously related to the risk of major CAD events.115
• Too rapid lower ing o f b lood pressure, which can cause reflex tachycardia and sympathet i c activation, should be avoided in patients with CAD.
• One may have to set the target of BP control even below 130/80 mm Hg but not lower than 120/70. The CLARIFY registry (2016) shows levels below 120 systolic and 70 diastolic were associated with adverse CV outcomes including mortality supporting the existence of a J curve phenomenon.194,195 All other risk factors should be treated appropriately.
• HT in patients with acute coronary s y n d r o m e s h o u l d b e t r e a t e d aggressively.
• β-blockers and CCBs are the drugs of first choice in the management o f a n g i n a i n p a t i e n t s w i t h hypertension associated with CAD.
• β-blockers have been shown to reduce the risks of re-infarction and cardiovascular death by 25% in patients with MI.196
• Amlodipine has been shown to produce subjective and objective improvement in patients with angina.197
• T r e a t m e n t w i t h a m l o d i p i n e i s a s s o c i a t e d w i t h f e w e r hospi ta l i sa t ions for uns tab le angina and revascularisations in patients with angiographically documented CAD.198
• V e r a p a m i l a n d d i l t i a z e m reduce r isk of developing MI following non-Q-wave myocardial infarction.199
• After MI, therapy with ACEIs prevents subsequent heart failure a n d r e d u c e s m o r b i d i t y a n d mortality200 ACEIs in combination with digoxin or low dose diuretics, are effective in reducing morbidity and mortality in patients in heart failure.201
• S t a t i n s a n d a s p i r i n a r e recommended in patients with hypertension associated with CAD.
Hypertension with Dyslipidaemia
Dyslipidaemia often co-exists with
hypertension.202
• Lifestyle modif icat ions are of particular importance in such patients as they can lower blood pressure and improve lipid levels.
• The choice of antihypertensive a g e n t s h o u l d b e m a d e a f t e r considering the effects on the lipid profile that some of these drugs have.
• A C E I s a n d c a l c i u m c h a n n e l blockers are lipid neutral drugs a n d t h e p r e f e r r e d a g e n t s i n patients with hypertension in dyslipidemias.
• In high doses diuretics can induce a short-term increase in cholesterol, triglycerides and LDL cholesterol levels. Low dose thiazides do not produce this effect.
• β - b l o c k e r s w i t h o u t i n t r i n s i c sympathomimetic activity (ISA) may increase levels of plasma triglycerides and reduce levels of HDL-cholesterol. Despite this, these have been shown to reduce rate of sudden death, overal l mortality and recurrent MI in patients with previous MI.
• Patients with HT and dyslipidaemia warrant lipid lowering therapy (statins) just as for patients with CV disease and diabetes.203
Hypertension with Obesity and Metabolic Syndrome
• P r e v a l e n c e o f o b e s i t y a n d h y p e r t e n s i o n i s i n c r e a s i n g . O b e s i t y i s a l m o s t a l w a y s accompanied by insulin resistance, h y p e r i n s u l i n e m i a , i m p a i r e d glucose tolerance and dyslipidemia. Truncal obesity is more common in Indian population. Also, abdominal obesity is associated with sodium retention, endothelial dysfunction, m i c r o a l b u m i n u r i a , LV H a n d elevated markers of inflammation.
• T h e d i a g n o s i s o f m e t a b o l i c syndrome is made when 3 or more of the risk determinants are present (Table 24).
• Compared with Whites, Indian men and women have a higher prevalence of central obesity.205 Anthropometric parameters of Asians are different than those for white Caucasians and blacks. For example, Asian Indians have smaller body size, excess body
Table 24: Diagnostic criteria for metabolic syndrome in Indians204
Risk factor Defining levelAbdominal obesity (Waist Circumference)
Men >90 cmWomen >80 cm
Triglycerides >150 mg/dlHDL-Cholesterol
Men <40 mg/dLWomen <50 mg/dL
Blood pressure >130/>85 mm HgFasting glucose >110 mg/dL

38 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
fat, and truncal and abdominal adiposity than white Caucasians.206 In Asians, the BMI cut-offs for overweight (>23.0 kg/m2) and obesity (>25.0 kg/m2) are lower than WHO criteria. These provisional recommendations will need to be revised in the light of further validation of studies and clinical experience.154,207
• Epidemiological s tudies have c o n s i s t e n t l y s h o w n a t i g h t correlation between body weight and blood pressure, with 70% of hypertension in men and 60% in women being directly attributable to excess adiposity.208 Essential hypertension is very frequently associated with a decrease in insulin sensitivity. This insulin resistance is very often associated wi th dys l ip idaemia , obes i ty , hypertension and impaired glucose tolerance, a cluster termed the “metabolic syndrome or the insulin resistance syndrome.209
• L i f e s t yl e m o d i f i c a t i o n ( d i e t , exercise) is the cornerstone in management of hypertension in obese individuals.
• Dyslipidemia in these patients is characterised by high TG levels and low HDL levels. Such patients require f ibrates for control of dyslipidemia.
• On the basis of their favourable m e t a b o l i c p r o f i l e s , i t w o u l d appear that ACEIs, ARBs, CCBs and α-blockers can decrease blood pressure without worsening the metabol i c abnormal i t i es tha t accompany hypertension in obese patients. ACE inhibitors, low-dose diuretics and non-dihydropyridine CCBs are probably the drugs of first choice in this setting. α -blockers have particular advantages in individuals with dyslipidaemia or glucose intolerance and may be considered as add-on agents. Given that control of hypertension in the majority of hypertensive patients is unlikely to be achieved with any single drug alone, the discussion on choice of drug class may be moot.199,211
Hypertension with Obstructive Sleep Apnea (OSA)
• OSA is now considered a cause of secondary hypertension and is closely associated with obesity.
• The treatment with of OSA with c o n t i n u o u s p o s i t i v e a i r wa y pressure (CPAP) has been shown to decrease daytime and nocturnal blood pressures.210
Resistant Hypertension
• Resistant hypertension is defined as the failure to reach goal BP in patients who are adhering to full doses of an appropriate 3-drug regimen of different classes that includes a diuretic. The causes of resistant hypertension are shown in Table 25.
Clinical Approach to Resistant Hypertension
A b o u t 1 2 . 2 % o f h y p e r t e n s i ve patients have Resistant Hypertension. Ambulatory blood pressure monitoring should be done in these patients in order to classify them as follows:1. True res i s tan t hyper tens ives
(62.5%),2. Pseudo or white-coat resistant
hypertension (37.5%)True resistant hypertensive patients
are more commonly men, of younger age, with a longer duration of hypertension, smokers, diabetics, HMOD (including left ventricular hypertrophy, impaired renal function, and microalbuminuria) and overall a worse cardiovascular risk profile.
Therefore, it necessary to assess ambulatory blood pressure monitoring for a correct diagnosis and management of true resistant hypertension.210
Table 25 gives causes of resistant HT2. These causes can be readily identified and treated.Management of resistant hypertension
M o s t p a t i e n t s w i t h r e s i s t a n t hypertension need to be referred to specialized hypertension clinics after evaluation of level of compliance. More aggressive salt restriction and elimination of drugs interfering with action of anti-hypertensive agents should be looked at. Subsequently, one should look for secondary hypertension and in case no secondary cause is found these patients need multiple drugs in high dosages. After starting adequate doses of ACEI/ARB + CCB + Thiazide diuretic and making sure of compliance, in case BP is not controlled add MRA (Spironolactone). Table 25 in case BP is still not controlled, an agent out of the choices given in step 5 can be added. Besides combination pharmacotherapy intervention-based treatment modalities such as Renal Sympathetic Denervation Therapy and Carotid Baroreceptor Stimulation therapy were evaluated. However, these have not been found to be of any clinical utility till now.
Renal denervat ion therapy for resistant hypertension was shown to be of great potential in initial unblended studies. Catheter based renal artery denervation was shown to reduce BP significantly (SIMPLICITY I and I I ) . 213,105 However , a met iculously conducted prospective randomized sham controlled trial in 535 patients showed that there is no significant reduction of SBP in patients with resistant hypertension after renal artery denervation as compared to sham control (SIMPLICITY III). Following this study interest in renal denervation therapy has waned off although a recent study published in circulation showed some benefit with this therapy.214,215
Table 25: Causes of resistant hypertension
• Volume overload - Excess sodium intake - Volume retention from kidney disease• Drug - Inadequate doses - Inappropriate combinations - Nonsteroidal anti-inflammatory drugs and
cyclooxygenase 2 inhibitors - Cocaine, amphetamines, other illicit drugs - Cyclosporine and tacrolimus - Tobacco - Selected over-the-counter dietary
supplements and medicines (e.g. liquorice and cough syrups)
• Associated conditions - Obesity - Excess alcohol intake• Secondary causes of hypertension - Chronic kidney disease - Coarctation of the aorta - Non-specific aortoarteritis - Cushing syndrome and other glucocorticoid
excess states including chronic steroid therapy
- Obstructive uropathy - Pheochromocytoma - Primary aldosteronism and other
mineralocorticoid excess states - Renovascular hypertension - Obstructive sleep apnea syndrome - Thyroid or parathyroid disease

39 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
ABPM – Ambulatory Blood Pressure Monitoring
A C C – A s s o c i a t e d C l i n i c a l Conditions
ACC/AHA – American Col lege o f Card io logy / Amer ican Hear t Association
A C C O M P L I S H – A v o i d i n g Cardiovascular Events in Combination Therapy in Patients Living with Systolic Hypertension
A C C O R D – A c t i o n t o C o n t r o l Cardiovascular Risk in Diabetes
ACEI – Angiotensin Converting Enzyme Inhibitors
ACR – Albumin Creatinine RatioADVANCE – Action in Diabetes
and Vascular Disease Perterax and Diamicron MR Controlled Evaluation
AHT – AntihypertensivesAIPRI - ACEI and progressive Renal
InsufficiencyALLHAT – Antihypertensive and
Lipid Lowering Treatment to Prevent Heart Attack Trial
API - Association of Physicians of India
ARB – Angiotensin II Receptor Blockers
ARRIVE - A Randomized Trial o f I n d u c t i o n Ve r s u s E x p e c t a n t Management
ASCEND - A Study of Cardiovascular Events iN Diabetes
ASPREE - Aspir in in Reducing Events in the Elderly
ASCOT – Anglo – Scandinavian Cardiac Outcomes Trial
A S C O T - B P L A – A n g l o – Scandinavian Cardiac Outcomes Trial – Blood Pressure Lowering Arm
ASIAN -HF - Asian Sudden Cardiac Death in Heart Failure
ATA C H I I - A n t i h y p e r t e n s i ve T r e a t m e n t o f A c u t e C e r e b r a l Hemorrhage-II
BHS – British Hypertension SocietyBMI – Body Mass IndexBP – Blood PressureBPH – Benign Prostatic HypertrophyCAD – Coronary artery diseaseCCB – Calcium Channel Blockers
CDUS – Colour Doppler UltrasoundCKD – Chronic Kidney DiseaseC O P D – C h r o n i c O b s t r u c t i ve
Pulmonary DiseaseCOX-2 – Cyclo-oxygenase – 2C L A R I F Y - P r o s p e C t i v e
observational LongitudinAl RegIstry oF patients with stable coronary arterY disease CMNNDs - Communicable, Maternal, Neonatal and Nutritional Diseases
CPAP – Continuous Positive Airway Pressure
CSI - Cardiological Society of IndiaCV – Cardio-vascularCVA – Cerebro-vascular AccidentCVD – Cardio-vascular DiseaseDASH – Dietary Approaches to Stop
HypertensionDALYs - Disability Adjusted Life
Years DBP – Diastolic Blood PressureDLHS - District Level Household
Survey DM – Diabetes MellitusD S A – D i g i t a l S u b t r a c t i o n
AngiographyDTPA – Di-ethylene-triamine-penta-
acetateECG – Electro-cardiogramE S C – E u r o p e a n S o c i e t y o f
CardiologyE S H – E u r o p e a n S o c i e t y o f
HypertensionESRD – End Stage Renal DiseaseETL- Epidemiological Transition
Level GBD- Global Burden of Diseases GFR – Glomerular Filtration RateHBPM – Home Blood Pressure
MonitoringHCWH – Health Care Without HarmHDI -Human Development Index HDL – High Density LipoproteinHF – Heart FailureHFnEF – Heart Failure with normal
Ejection FractionHIC - High-Income CountriesHOPE – Heart Outcomes Prevention
Evaluation
H O T – H y p e r t e n s i o n O p t i m a l Treatment Study
HSI- Hypertension Society of IndiaHMOD - Hypertension Mediated
Organ Damage hs CRP – Highly sensitive C Reactive
ProteinHT – HypertensionHYVET – Hypertension in Very
Elderly TrialIAD - Indian Academy of DiabetesICP - Indian College of PhysiciansI G H – I n d i a n G u i d e l i n e s o n
HypertensionINR - International Normalised
Ratio INTERACT 2 - The Second Intensive
Blood Pressure Reduction in Acute Cerebral Haemorrhage Trial
INVEST – International Verapamil SR/ Trandolapril Study
ISH – Isolated Systolic HypertensionJNC – Joint National Committee on
prevention, detection, evaluation and treatment of high blood pressure
JVP - Jugular venous pressureKDIGO – Kidney Disease: Improving
Global OutcomesLDL – Low Density LipoproteinLIFE – Losartan Intervention for
Endpoint Reduction in HypertensionL M I C - L o we r M i d d l e I n c o m e
Countries LSM - lifestyle modification LV – Left VentricleLVH – Left Ventricular HypertrophyMBP – Mean Blood PressureMDRD – Modification of Dietary
Protein in Renal DiseaseMI – Myocardial InfarctionMIBG – Meta-iodo-benzyl-guanidineMRI – Magnetic Resonance ImagingNCD – Non communicable diseasesNFHS - National Family Health
Survey NICE – National Institute for Health
and Clinical ExcellenceNSAIDS – Non S tero ida l Ant i
Inflammatory DrugsOBP - Office Blood Pressure OH – Orthostatic Hypotension
Abbreviations

40 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
ONTARGET – Ongoing Telmisartan A l o n e a n d i n C o m b i n a t i o n w i t h Ramipril Global Endpoint Trial
OSA – Obstructive Sleep ApneaPAT H WAY - P r e v e n t i o n a n d
Treatment of Resistant Hypertension With Algorithm Guided Therapy
PET – Positron Emission TomographyP I H – P r e g n a n c y I n d u c e d
HypertensionPP – Pulse PressurePRA – Plasma Renin ActivityPROGRESS – Perindopril Protection
against Recurrent Stroke StudyPURE Study – Prospective Urban
Rural Epidemiology StudyPWV – Pulse Wave Velocity
R A A S – R e n i n A n g i o t e n s i n Aldosterone System
R E I N - R a m i p r i l E f f i c a c y i n Nephropathy
RBCs – Red Blood CellsRF – Risk FactorsRH – Resistant HypertensionRSSDI - Research Society for Study
of Diabetes in IndiaRVH – Renovascular HypertensionSBP – Systolic Blood PressureSCORE - Systemic COronary Risk
Evaluation System SPRINT - Systolic Blood Pressure
Intervention Trial SHEP – Systolic Hypertension in
Elderly Program
SHIFT - Systo l ic Heart fa i lure t r e a t m e n t w i t h t h e I f i n h i b i t o r ivabradine Trial
TG – TriglyceridesTIA – Transient Ischemic Attack
TOD Target Organ DamageTONE – Trial of Non-Pharmacological
intervensions in the ElderlyUI- Urbanization Index U K P D S – U n i t e d K i n g d o m
Prospective Diabetes StudyVALUE – Valsartan Antihypertensive
Long-term Use EvaluationVMA - Vanillyl-Mandelic Acid

41 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
1. Indian Guidelines Management of Hypertension 2001. Hypertension India 2001; 15:1-34.
2. http://www.apiindia.org/hsi_guideline_ii.html.
3. Association of Physicians of India. Indian guidelines on hypertension (I.G.H.) – III 2013. J Assoc Physicians India 2013; 61:6-36.
4. Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, Lerebours G, Tavazzi L, SHIFT investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. The Lancet 2010; 376:875-85.
5. Genevieve M Gabb, Arduino A Mangoni, Craig S Anderson, Diane Cowley, John S Dowden, Jonathan Golledge, Graeme J Hankey, Faline S Howes, Les Leckie, Vlado Perkovic, Markus Schlaich, Nicholas A Zwar, Tanya L Medley and Leonard Arnolda. Guideline for the diagnosis and management of hypertension in adults — 2016. Med J Aust 2016; 205:85-89.
6. Hypertension Canada’s 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults. Can J Cardiol 2017; 33:557-576. doi: 10.1016/j.cjca.2017.03.005.
7. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABS/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation and management of high blood pressure in adults: executive summary. J Am CollCardiol 2018; 71:2199-269.
8. Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–104.
9. SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103-16.
10. Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, Pais P, López-Jaramillo P, Leiter LA, Dans A, Avezum A. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. New England Journal of Medicine 2016; 374:2021-31.
11. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Prospective Studies Collaboration. Lancet 2002; 360:1903-1913.
12. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension 2003; 42:1206-52.
13. Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, et. al Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hyperten 2004; 18:139-185.
14. Su M, Haldane V, Upshur R,et al. The Impact of Treatment Adherence for Patients With Diabetes and Hypertension on Cardiovascular Disease Risk: Protocol for a Retrospective Cohort Study, 2008-2018. JMIR Res Protoc. 2019 May 31;8(5):e13571. doi: 10.2196/13571.
15. Brown RD Jr, Whitsnant JP, Sicks JD, O’Fallon WM, Wiebers D. Stroke incidence, prevalence and survival: Secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373-380.
16. Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation 2001; 103:1245-1249.
17. Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, et al. Success and predictors of blood pressure control in diverse North American settings: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich) 2002; 4:393-404.
18. Black HR, Elliott WJ, Neaton JD, Grandits G, Grambsch P, Grimm R, et al. Baseline characteristics and early blood pressure control in the CONVINCE trial. Hypertension 2001; 37:12-18.
19. Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Kaczorowski J. Measurement of blood pressure in the office: recognizing the problem and proposing the solution. Hypertension 2010; 55:195-200.
20. Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M, de la Cruz JJ, Ruiz-Hurtado G, Segura J, Rodríguez-Artalejo F, Williams B. Relationship between clinic and ambulatory blood-pressure measurements and mortality. New England Journal of Medicine 2018; 378:1509-20.
21. Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013 Circulation, 17 (2015), pp. 667-678, 10.1161/CIRCULATIONAHA.114.008720
22. World Health Organization. Global status report on noncommunicable diseases 2014. World Health Organization; 2014.
23. Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, Naghavi M, Mensah GA, Murray CJ. Demographic and epidemiologic drivers of global cardiovascular mortality. New England Journal of Medicine 2015; 372:1333-41.
24. O’Flaherty M, Buchan I, Capewell S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s?. Heart 2013; 99:159-62.
25. Institute for Health Metrics and Evaluation.. The Global Burden of Disease: Generating Evidence, Guiding Policy—South Asia Regional Edition.
26. Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, Pandey MR, Haque S, Mendis S, Rangarajan S, Yusuf S. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007; 297:286-94.
27. Rehman H, Samad Z, Mishra SR, Merchant AT, Narula JP, Mishra S, Virani SS. Epidemiologic studies targeting primary cardiovascular disease prevention in South Asia. Indian Heart Journal 2018; 70:721-30.
28. World Health Statistics 2018: Monitoring health for the SDGs. https://www.who.int/gho/publications/world_health_statistics/2018/en/.
29. https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence/en/.
30. Anand SS, Yusuf S. Stemming the global tsunami of cardiovascular disease. Lancet 2011; 377:529-532.
31. Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens 2004; 18:73-78.
32. Gupta R, Gaur K, Ram CV. Emerging trends in hypertension epidemiology in India. Journal of Human Hypertension 2018:1.
33. Wander GS, Ram CV. Blood pressure-Methods to record & numbers that are significant: Lets make a tailored suit to suit us. The Indian Journal of Medical Research 2018; 147:435.
34. Wander GS, Ram CV. Global impact of 2017 American Heart Association/American College of Cardiology hypertension guidelines: a perspective from India. Circulation 2018; 137:549-50.
35. Gupta R, Xavier D. Hypertension: The most important non communicable disease risk factor in India. Indian Heart Journal 2018; 70:565-72.
36. Dandona L, Dandona R, Kumar GA, Shukla DK, Paul VK, Balakrishnan K, Prabhakaran D, Tandon N, Salvi S, Dash AP, Nandakumar A. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. The Lancet 2017; 390:2437-60.
37. National Family Health Survey. http://rchiips.org/nfhs/abt.html. Accessed April 2, 2018.
38. District Level Household and Facility Survey. https://data.gov.in/resources/hypertension-age-18-years-and-above-dlhs-iv. Accessed 7 May 2018.
39. Wander GS, Ram CV. Optimal Blood Pressure Goals Recommended by the Latest Hypertension Guidelines: India may benefit the most. European Heart Journal Volume 2018; 39:3012–3016.
40. https://www.icmr.nic.in/sites/default/files/press_realease_files/Hypertension.pdf.
41. Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens 2004; 18:73–78.
42. http://www.epa.gov/region9/waste/p2/projects/hospital/mercury.pdf Last accessed on 10.09.2012.
43. Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. New NICE guidelines for hypertension. BMJ 2011; 343.
44. Gupta R, Guptha S, Gupta VP, Agrawal A, Gaur K, Deedwania PC. Twenty-year trends in cardiovascular risk factors in India and infuence of educational status. Eur J Cardiovasc Prev Rehabil 2011 Sep 26; Epub ahead of print.
45. Safar ME, Levy BI, Struijker-Boudier H. Current Perspectives on Arterial Stiffness and Pulse Pressure in Hypertension and Cardiovascular Diseases. Circulation 2003; 107:2864-2869.
46. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 129(Suppl.2):S49–S73.
47. McClelland RL, Jorgensen NW, Budoff M, Blaha MJ, Post WS, Kronmal RA, et al. 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in the HNR (Heinz Nixdorf Recall) study and the DHS (Dallas Heart Study). Journal of the American College of Cardiology 2015; 66:1643-53.
48. Studziński K, Tomasik T, Krzysztoń J, Jóźwiak J, Windak A. Effect of using cardiovascular risk scoring in routine risk assessment in primary prevention of cardiovascular disease: protocol for an overview of systematic reviews. BMJ Open 2017; 7:e014206.
49. DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, Blumenthal RS, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Annals of Internal Medicine 2015; 162:266-75.
50. Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension 2000; 35:1021-1024.
51. The Heart outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin converting enzyme inhibitor, ramipril on cardiovasucler events in high risk patients. N Engl J Med 2000; 342:145-53.
52. The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288:2981-2997.
53. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group Diuretic Versus -Blocker as First-Step Antihypertensive Therapy Final Results From the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension 2003; 42:239-46.
54. Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhager WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet 1997; 350:757-764.
55. Wang J, Staessen JA, Gong L, Liu L for the Systolic Hypertension in China (Syst- China) Collaborative Group. Chinese Trial on Isolated Systolic Hypertension in the Elderly. Arch Intern Med 2000; 160:211-220.
56. SHEP Cooperative Research Group. Prevention of Stroke by antinypertensive drug treatment in older persons with isolated Systolic hypertension. Final results of the Systolic hypertension in the Elderly Program (SHEP). JAMA 1991; 265:3255- 64.
57. Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al for the ASCOT investigators. Prevention
References

42 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005; 366:895-906.
58. Frohlich ED. Treating Hypertension - What Are We to Believe? N Engl J Med 2003; 348:639-641.
59. Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger Jr WH, Kostis JB, et al. For the TONE collaborative research group. Sodium reduction and weight reduction in treatment of hypertension in older patients. A randomised controlled Trial Of Non-pharmacological interventions in the Elderly (TONE). JAMA 1998; 279:839-846.
60. Stamier I, Cagguila AW, Grandito GA. Relation of body mass and alcohol, nutrient, fibre and caffeine intake to blood pressure in the special intervention and usual care groups in the Multiple Risk Factor Intervention Trial. Am J Clin Nutr 1997; 65(suppl l):338S-365S.
61. Puddey IB, Parker M, Beiten LJ, Vandongen R, Maseree JRL. Effects of alcohol and calorie restriction on blood pressure and serum lipids in overweight men. Hypertension 1992; 20:533-541.
62. Mittal RDJ, Mukherjee A, Saxena BN. Salt Consumption Pattern in India: an ICMR Task Force Study. New Delhi: Indian Council of Medical Research; 1996.
63. Kumbla D, Dharmalingam M, Dalvi K, Ray S, Shah MK, Gupta S, Sadhanandham S, Ajmani AK, Nag S, Murthy S, Murugan MA. A Study of salt and fat Consumption pattern in Regional Indian diet among hypertensive and dyslipidemic Patients-SCRIPT study. J Assoc Physicians India 2016; 64:47-54.
64. Greenberg G. Thompson SG, Brennan PJ. The relationship between smoking and the response to antihypertensive treatment in mild hypertensives in the Medical Research Council’s trial of treatment. Int J Epidemiol 1987; 16:225-230 F.
65. Gupta R, Gurm H, Bartholomew JR. Smokeless Tobacco and Cardiovascular Risk. Arch Intern Med 2004; 164:1845-1849.
66. US Department of Health and Human Services. The Health Benefits of Smoking Cessation A Report of the Surgeon General Rockville. MD: Centers for Disease Control. Center for Chronic Disease Prevention and Health Promotion. Office on Smoking and Health; DHHS publication no. (CDC) 90:8416: 1990 Pr.
67. Patel C. 12-month follow-up of yoga and bio-feedback in the management of hypertension. Lancet 1975; 1:62-64.
68. Sunder S, Agrawal SK, Singh VP, Bhattacharya SK, Udupa KN, Vaish SK. Role of yoga in management of essential hypertension. Acta Cardiol 1984; 39:203-208.
69. Datey KK. Role of biofeedback training in hypertension and stress. J Postgrad Med 1980; 26:68-73.
70. Damodaran A, Malathi A, Patil N ,Shah N, Suryavanshi, Marathe S. Therapeutic potential of yoga practices in modifying cardiovascular risk profile in middle aged men and women. J Assoc Physicians India 2002; 50:633-40.
71. Thiyagarajan R, Pal P, Pal GK, Subramanian SK, Trakroo M, Bobby Z, Das AK. Additional benefit of yoga to standard lifestyle modification on blood pressure in prehypertensive subjects: a randomized controlled study. Hypertension Research 2015; 38:48.
72. Rouse IL, Armstrong BD, Beilin LJ. The relationship of blood pressure to diet and lifestyle in two religious populations. J Hypertens 1983; 1:65-71.
73. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM. et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997; 336:1117-1124.
74. Bao DG, Mori TA, Burke V, Puddey IB, Beilin LJ. Effects of dietary fish and weight reduction on ambulatory blood pressure in overweight hypertensives. Hypertension 1998; 32:710-717.
75. Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, et al. Effects of oral potassium on blood pressure: Meta analysis of randomized controlled trials. JAMA 1999; 277:1624-1632.
76. Stamier I, Cagguila AW, Grandito GA. Relation of body mass and alcohol, nutrient, fibre and caffeine intake to blood
pressure in the special intervention and usual care groups in the Multiple Risk Factor Intervention Trial. Am J Clin Nutr 1997; 65(suppl l):338S-365S.
77. Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, Amma LI. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. The Lancet 2017; 390(10107):2050-62.
78. Srilakshmi B. Diet in diseases of cardiovascular system. In: Srilakshmi B editor. Dietetics. Revised. 5th ed. New Delhi: New Age International (P)Ltd 2005;189-213.
79. Srilakshmi B. Diet in diseases of Kidney. In: Srilakshmi B editor. Dietetics. Revised. 5th ed. New Delhi: New Age International (P)Ltd; 2005;267-291.
80. Gavras H, Gavras I. On the JNC V report. A different point of view. Am J Hypertens 1994; 7:288-293.
81. Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively designed overviews of randomised trials. Lancet 2003; 362:1527-1535.
82. Goyal A, Aslam N, Kaur S, Soni RK, Midha V, Chaudhary A, Dhaliwal LK, Singh B, Chhabra ST, Mohan B, Anand IS. Factors affecting seasonal changes in blood pressure in North India: A population based four-seasons study. Indian Heart Journal 2018; 70:360-7.
83. Goyal A, Narang K, Ahluwalia G, Sohal PM, Singh B, Chhabra ST, Aslam N, Mohan B, Wander GS. Seasonal variation in 24 h blood pressure profile in healthy adults-A prospective observational study. Journal of Human Hypertension 2019:1.
84. The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high risk patients. N Engl Med 2000; 342:145-153.
85. PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet 2001; 358:1033-41.
86. Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359:995-1003.
87. Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al, for the VALUE trial group. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004; 363:2022-2031.
88. The ONTARGET investigators. Telmisartan, Ramipril or Both in patients at High Risk for Vascular events. NEJM 2008; 358:1547-1559.
89. Haller H, et al. Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N Engl J Med 2011; 364:907-17.
90. Hansson L, Hedneer T, Lund-Johansen P, Kjeldsen SE, Lindholm LH, Syvertsen JO, et al. Randomised trial of effect of’ calcium antagonists compared with diuretics and B-blockers on cardiovascular morbidity and mortality in hypertension: the Nordic Diltiazem (NORDIL) study. Lancet 2000; 356:359-365.
91. Packer M, O’Connor CM, Ghali JK, Pressler ML, Carson PE, Belkin RN, et al. Effect of amlodipine on morbidity and mortality in severe chronic heart failure. N Engl Med 1996; 335:1107-1114.
92. Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension 2012; 59:1110-7.
93. Brown MJ, Williams B, Morant SV, Webb DJ, Caulfield MJ, Cruickshank JK, Ford I, McInnes G, Sever P, Salsbury J, Mackenzie IS. Effect of amiloride, or amiloride plus hydrochlorothiazide, versus hydrochlorothiazide on glucose tolerance and blood pressure (PATHWAY-3): a parallel-group, double-blind randomised phase 4 trial. The Lancet Diabetes & Endocrinology 2016; 4:136-47.
94. Williams B, MacDonald TM, Morant S, Webb DJ, Sever P, McInnes G, Ford I, Cruickshank JK, Caulfield MJ, Salsbury
J, Mackenzie I. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. The Lancet 2015; 386:2059-68.
95. 2003 Europeon Society of Hypertension- Europeon Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21:1011-1053.
96. Hypertension Management in Adults With Diabetes. Position Statement-American Diabetes Association. Diabetes Care 2004; 27:S65-67.
97. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288:2981-97.
98. Jamerson K, Weber MA et al for the ACCOMPLISH Trial Investigators. Benazepril plus Amlodipine or Hydrochlorothiazide for Hypertension in High-Risk Patients. N Engl J Med 2008; 359:2417-2428.
99. Opie LH. Drug interactions of antihypertensive agents. S Afr Fam Pract 2012; 54(Suppl 1):S23-S25.
100. The Heart Outcomes Prevention Evaluation Study Investigators. Vitamin E supplementation and cardiovascular events in high-risk patients. N Engl J Med 2000; 342:154-60.
101. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo controlled trial. Lancet 2002; 360:7-22.
102. ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. New England Journal of Medicine 2018; 379:1529-39.
103. McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, Kirpach B, Shah RC, Ives DG, Storey E, Ryan J. Effect of aspirin on all-cause mortality in the healthy elderly. New England Journal of Medicine 2018; 379:1519-28.
104. Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB, Howard G, Pearson TA, Rothwell PM, Ruilope LM, Tendera M. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. The Lancet 2018; 392:1036-46.
105. Symplicity HTN-2 Investigators. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. The Lancet 2010; 376:1903-1909.
106. Berglund G, Andersson O, Wilhelmsen L. Prevalence of primary and secondary hypertension : Studies in a random population sample. BMJ 1976; 2:554-556.
107. Danielson M, Dammstorm BG. The prevalence of secondary and curable hypertension. Acta Med Scand 1981; 209:451-455.
108. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Inter Suppl 2012; 2:337-414.
109. Abraham G, Arun K, Gopalakrishnan N, Renuka S, Pahari DK, Deshpande P, Isaacs R, Chafekar DS, Kher V, Almeida10 AF, Sakhuja11 V. Management of Hypertension in Chronic Kidney Disease: Consensus Statement by an Expert Panel of Indian Nephrologists. J Assoc Physicians India 2017; 65:6-22.
110. Laskow DA, Curtiss JJ. Post transplant hypertension. Am J Hypertns 1990; 3:721-725.
111. National Kidney Foundation (NKF) Kidney Disease Outcome Quality Initiative (K/DOQI) Advisory Board, K/DOQI clinical practice guidelines for chronic kidney disease : evaluation, classification and stratification. Kidney Disease Outcome Quality Initiative. Am K Kidney Dis 2002; 39(2 Suppl 2):S65.
112. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345:861-869.
113. Curb JD, Pressel SL, Cutler JA, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension.

43 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA 1996; 276:1886-1892.
114. Knauf H, Mutschler E. Diuretic effectiveness of hydrochlorothiazide and furosemide alone and in combination in chronic renal failure. J Cardiovasc Pharmacol 1995; 26:394-400.
115. Bakris GL, Simons M, Richardson D, et al. Comparative effects of an ACE inhibitor and an angiotensin receptor blocker on potassium homeostasis in patients with renal insufficiency. Kidney Int. In Press.
116. Chugh KS, Jain S, Sakhuja V, Malik N, Gupta A, Sehgal S, et al. Renovascular hypertension due to Takayasu’s Arteritis among Indian patients. QJ Med 1992; 85:833-843.
117. The ASTRAL Investigators. Revascularization versus Medical Therapy for Renal-Artery Stenosis. N Engl J Med 2009; 361:1953-1962.
118. Cooper CJ, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, Cohen DJ, Matsumoto AH, Steffes M, Jaff MR, Prince MR. Stenting and medical therapy for atherosclerotic renal-artery stenosis. New England Journal of Medicine 2014; 370:13-22.
119. Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT. Occurrence of pheochromocytoma in Rochester, Minnesota 1950 through 1979. Mayo Clin Proc 1983; 58:802-804.
120. Brano EL, Gittord RW Je. Pheochromocytoma: Diagnosis, localisation and management. N Engl J Med 1984; 311:1298-1303.
121. Rao N, Ramachandran R, Tandon N, Singh P, Kumar R. Surgical and hemodynamic outcomes in pheochromocytoma surgery: a prospective cohort study. Urology 2016; 98:103-6.
122. Frohlich ED. Classic papers symposium, History of medicine series: Surrogate indexes of target organ involvement in hypertension. Am J Med Sci 1996; 312:225-228.
123. Zanchetti A, Sleight P, Birkenhaker WH. Evaluation of organ damage in hypertension. J Hypertens 1993; 11:875-882.
124. Kannel WB. Left ventricular hypertrophy as a risk factor: The Framingham experience. J Hypertens 1991; 9(Supl 2):53-59.
125. Reddy KS. Cardiovascular diseases in India. World Health Statistics Quarterly 1993; 46:101-107.
126. Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Blood pressure, cholesterol and stroke in Eastern Asia. Lancet 1998; 352:1801-1807.
127. MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990; 35:765-774.
128. Prospective Studies Collaboration. Cholesterol, diastolic blood pressure and stroke: 13,000 strokes in 45,000 people in 45 prospective cohorts. Lancet 1995; 346:1647-1653.
129. Rosansky SJ, Hoover DR, King L, Gibson J. The association of blood pressure levels and change in renal functions in hypertension and nonhypertensive subjects. Arch Int Med 1990; 150:2073-2074.
130. Kannel WB, Stampfer MJ, Castelli WP, Verter J. The Prognostic significance of proteinuria: the Framingham Study. Am Heart J 1984; 108:1347-1352.
131. Ruilope LM. Proteinuria and renal function. Blood Pressure 1993; 2(Suppl.1):55-58.
132. Lewis EJ, Hunsicker LG, Rodby RA, Collabarative Study Group. A Clinical trial 2 diabetic nephropathy. Am J Kidney Dis 2001; 38(4 Suppl.1):S191-194.
133. Wong TY, Mitchell P. Hypertensive Retinopathy. N Engl J Med 2004; 351:2310-17.
134. Oakley CM. Aortic dissection. QJ Med 1991; 79:357-380.
135. Lauin P. Management of hypertension in patients with acute stroke. Arch Intern Med 1986; 146:66-68.
136. Herl ing IM. Intravenous nitroglycerine: Cl inical Pharmacology and Therapeutic Consideration. Am Heart J 1980; 108:141-149.
137. O’ Mailia J, Sander G, Giles T. Nifedipine associated myocardial ischemic or infarction in the treatment of hypertensive emergencies. Ann Int Med 1987; 107:185-186.
138. Simpson DC. Etiology and prevalence of hypertension in diabetic patients. Diabetes Care 1988; 11;821-827.
139. Joshi S, Shah SN. Rising Global burden of Diabetes. The Asian J Diab 1999; III:13-15.
140. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998; 317:703-713.
141. Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Menard J, et. al for HOT Study group. Effects of intensive blood pressure lowering and low-dose aspirin in patients with hypertension: Principle results of the Hypertension Optimal Treatment (HOT) randomized trial. Lancet 1998; 351:1755-1762.
142. Hypertension / blood pressure control, Goals, Executive Summary : Standards of Medical Care in Diabetes-2013. Diabetes Care 2013; 36:Suppl.1,S6-S7.
143. The HYVET Study Group. Treatment of Hypertension in Patients 80 Years of Age or Older. N Engl J Med 2008; 358:1887-1898.
144. The ACCORD study group. The effect of intensive blood pressure control in type 2 diabetes mellitus. NEJM 2010; 362:1575-1585
145. Tsujimoto T, Kajio H. Benefits of intensive blood pressure treatment in patients with type 2 diabetes mellitus receiving standard but not intensive glycemic control. Hypertension 2018.
146. The ADVANCE Collaborative Group.Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med 2008; 358:2560-2572.
147. Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010; 304;61-68.
148. Aug;72(2):323-30. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. New England Journal of Medicine 2015; 373:2117-28.
149. Neal B, Perkovic V, Mahaffey KW, De Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. New England Journal of Medicine 2017; 377:644-57.
150. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. New England Journal of Medicine 2019; 380:347-57.
151. Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, Lindley R, Robinson T, Lavados P, Neal B, Hata J. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. New England Journal of Medicine 2013; 368:2355-65.
152. Qureshi AI, Palesch YY, Barsan WG, Hanley DF, Hsu CY, Martin RL, Moy CS, Silbergleit R, Steiner T, Suarez JI, Toyoda K. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. New England Journal of Medicine 2016; 375:1033-43.
153. Spengos K, Tsivgoulis G, Zakopoulos N. Blood pressure management in acute stroke: a long standing debate. European Neurology 2006; 55:123-135.
154. Lewis CE, Grandits A, Flack J, McDonald R, Elmer PJ. Efficacy and tolerance of antihypertensive treatment in men and women with stage 1 diastolic hypertension: results of the Treatment of Mild Hypertension Study. Arch Intern Med 1996; 156:377-385.
155. Lim KG, Isles GG, Hodsman GP, Lever AF, Robertson JWK. Malignant hypertension in women of childbearing age and its relation to contraceptive pill. BMJ 1987; 294:1057-1059.
156. Saftlas AF, Olson DR, Franks AL, Atrash AK, Pokras R. Epidemiology of preeclampsia and eclampsia in the United States, 1979–1986. Am J Obstet Gynecol 1990; 163:460-5.
157. Dudley L. Maternal mortality associated with hypertensive disorders of pregnancy in Africa, Asia, Latin America and the Caribbean. Br J Obstet Gynaecol 1992; 99:547-553.
158. Lenox JW, Urugu V, Cibils LA. Effects of hypertension on pregnancy monitoring and results. Am J Obstet Gynaecol 1990; 163:1173-1179.
159. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, Hall DR, Warren CE, Adoyi G, Ishaku S.
Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 2018; 72:24-43.
160. Brown MA. Is there a role for ambulatory blood pressure monitoring in pregnancy?. Clinical and Experimental Pharmacology and Physiology 2014; 41:16-21.
161. Magee LA, von Dadelszen P, Rey E, Ross S, Asztalos E, Murphy KE, Menzies J, Sanchez J, Singer J, Gafni A, Gruslin A. Less-tight versus tight control of hypertension in pregnancy. New England Journal of Medicine 2015; 372:407-17.
162. Maryland B. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000; 183:S1-S22.
163. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 743. Low-dose aspirin use during pregnancy. Obstet Gynecol 2018; 132:e44-52.
164. Sibal BM. Treatment of hypertension in pregnant women. N Engl J Med 1996; 335:257-265.
165. Lubbe WF, Hodge JV, Kellaway GSM. Antihypertensive treatment and fetal welfare in essential hypertension in pregnancy: a retrospective survey of experience with various regimens at National women’s hospital Aukland 1970-80. 1982; 95:1-5.
166. Collins R, Yusuf S, Peto R. Overview of randomized trials of low dose diuretics in pregnancy. Br Med J (Clin Res Ed) 1985; 290:17-23.
167. Roberts JM. Magnesium for pre-eclampsia and eclampsia. N Engl J Med 1995; 333:250-251.
168. The Eclampsia Trial Collaborative Group: Which anti-convulsants for women with preeclampsia Evidence from collaboration Eclampsia Trial. Lancet 1995; 345:1455-1466.
169. Statistical outline of India 2004-2005. Tata services Limited. Department of economics and statistics.
170. Dalal PM. Hypertension: A report on community survey on casual hypertension in old Bombay, Sir. HN Hospital Research Society 1980.
171. Beckett N, Peters R, Tuomilehto O et al. Immediate and late benefits of treating very elderly people with hypertension: results from active treatment extension to Hypertension in the Very Elderly randomised controlled trial. BMJ 2011; 344.
172. National High Blood Pressure Education Program Working Group. National High Blood Pressure Education Program working group report on Hypertension in the elderly. Hypertension 1994; 23:275-85.
173. MacMahon S, Rodgers A. The effects of blood pressure reduction in older patients: an overview of five randomized controlled trials in elderly hypertensives. Clin Exp Hypertens 1993; 15:967-978.
174. Espeland MA, Whalton PK, Kostis JB, Bahnson JL, Ettinger WH, Cutler JA. Predictors and mediators of successful long.-term withdrawal from antihypertensive medications. Arch Fam Med 1999; 8:228 236.
175. Aronow WS, Fleg JL, Pepine CJ et al. ACCF/AHA 2011 Expert Consensus Document on Hypertension in the Elderly. JACC 2011; 57:2037-114.
176. Hansson L, Lindholm LH, Ekbom T, Dahlöf B, Lanke J, Scherstén B, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the swedish trial in old patients with hypertension. Lancet 1999; 354:1751-1756.
177. Klapholz M, Mitchell J, Meisner JS, et al. Clinical characteristics and co-morbid conditions of patients hospitalized for heart failure with normal systolic function: results of the New York heart failure consortium registry on diastolic dysfunction. Circulation 2001; 104(suppl II):II-689.
178. Burkhoff D, Maurer MS, Packer M. Heart Failure With a Normal Ejection Fraction. Is It Really a Disorder of Diastolic Function? Circulation 2003; 107:656-658.
179. Garg R, Yusuf S. for the collaborative Group on ACE Inhibitor Trials. Overview of Randomized trials of angiotensin converting enzyme inhibitors on mortality and morbidity in patients with heart failure. JAMA 1995; 273:1450-1456.
180. MERIT-HF Study Group: Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999; 353:2001-2007.

44 Clinical Journal of Hypertension | April-September 2019 | Vol. No. 3 | Issue No. 2 & 3
181. CIBIS-II Investigators and Committees: The Cardiac Insufficiency Biosoprolol Study II (CIBIS-II): a randomized trial. Lancet 1999; 353:9-13.
182. Krum H, Roecker EB, Mohacsi P, Rouleau JL, Tendera M, Coats AJS, et al. Effects of initiating carvedilol in patients with severe chronic heart failure. Results from the COPERNICUS study. JAMA 2003; 289:712-718.
183. Packer M, Coats AJS, Fowler MB, Hugo A. Katus HA, Krum H, Mohacsi P, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001; 344:1651-1658.
184. Australia / New Zealand Heart Failure Research Collaborative Group. Randomized, Placebo control trial of carvedilol in patients with congestive heart failure due to ischaemic heart disease. Lancet 1997; 349:375-380.
185. Parker M. European Society of Cardiology, 22nd Annual Congress, March 2000-Carvedilol Prospective randomised cumulative survival.
186. Ake Hjalmarson. Metoprolol CR/XL Randomized Interventions Trial in Heart Failure (MERIT-HF). Proceedings of the 48th Annual Conference. American College of Cardiology 7th-9th March, 1999.
187. CIBIS II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II. (CIBIS II): a randomized trial. Lancet 1999; 353:9-13.
188. Dokainish H, Teo K, Zhu J, Roy A, AlHabib KF, ElSayed A, Palileo-Villaneuva L, Lopez-Jaramillo P, Karaye K, Yusoff K, Orlandini A. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. The Lancet Global Health 2017; 5:e665-72.
189. Teng TH, Tromp J, Tay WT, Anand I, Ouwerkerk W, Chopra V, Wander GS, Yap JJ, MacDonald MR, Xu CF, Chia YM. Prescribing patterns of evidence-based heart failure pharmacotherapy and outcomes in the ASIAN-HF registry: a cohort study. The Lancet Global Health 2018; 6:e1008-18.
190. McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR. Angiotensin–neprilysin inhibition versus enalapril in heart failure. New England Journal of Medicine 2014; 371:993-1004.
191. Nasr IA, Bouzamondo A, Hulot JS, Dubourg O, Le Heuzey JY, Lechat P. Prevention of atrial fibrillation onset by β-blocker treatment in heart failure: a meta-analysis. Eur Heart J 2007; 28:457–462.
192. National Clinical Guideline Centre (June 2014). “Atrial Fibrillation: The Management of Atrial Fibrillation”. London: National Institute for Health and Care Excellence. PMID 25340239.
193. Bamidele EO. Curr Ther Res 1986; 39:554-557.
194. Vidal-Petiot E, Ford I, Greenlaw N, Ferrari R, Fox KM, Tardif JC, Tendera M, Tavazzi L, Bhatt DL, Steg PG, CLARIFY investigators. Cardiovascular event rates and mortality according to achieved systolic and diastolic blood pressure in patients with stable coronary artery disease: an international cohort study. The Lancet 2016; 388:2142-52.
195. Sorbets E, Greenlaw N, Ferrari R, Ford I, Fox KM, Tardif JC, Tendera M, Steg PG; CLARIFY Investigators. Rationale, design, and baseline characteristics of the CLARIFY registry of outpatients with stable coronary artery disease. Clin Cardiol 2017; 40:797–806.
196. Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Β blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985; 27:335-371.
197. Deanfield JE, Detry J-MRG, Lichtlen PR, Magnani B, Sellier P, Thaulow E, for the CAPE Study Group. Amlodipine reduces transient myocardial ischemia in patients with coronary artery disease: double-blind Circadian Anti-ischemia Program in Europe (CAPE Trial). J Am Coll Cardiol 1994; 24:1460-1467.
198. Pitt B, Byington RP, Furberg CD, Hunninghake DB, John Mancini GB, Miller ME, et al. Effect of amlodipine on the progression of atherosclerosis and the occurrence of clinical events. Circulation 2000; 102:1503-1510.
199. Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction; a report of the American College of Cardiology/American Heart association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1996; 28:1328-1428.
200. Pfeffer MA, Braunwald E, Moye LA, Basta L, Brown EJ, Cuddy TE, et al. for the SAVE Investigators. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction; results of the Survival and Ventricular Enlargement Trials. N Engl J Med 1992; 327:669-677.
201. Lonn EM, Yusuf S, Jha P, Montague TJ, Teo KK, Benedict CR, et. al Emerging role of angiotensin-converting enzyme inhibitors in cardiac and vascular protection. Circulation 1994; 90:2056-2069.
202. Joglekar SJ, Nanivadekar AS. Dyslipidemia- A prevalence of lipid and glycemic abnormalities in hypertensive patients: A retrospective study. Indian Heart J 1996; 371-374.
203. Sever PS, Dahlof B, Poulter NR, Wedet H, Beevers G, Caulfield M et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-then-average cholesterol concentrations, in the Anglo Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial.
Lancet 2003; 361:1149-1158.
204. Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi SR. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India 2009; 57:163-70.
205. Enas EA, Senthilkumar A, Juturu V, Gupta R. Coronary Artery Disease in Women. Indian Heart J 2001; 53:282-292.
206. Misra A, Wasir JS, Pandey RM. An Evaluation of Candidate Definitions of the Metabolic. Syndrome in Adult Asian Indians. Diabetes Care 2005; 28:398-403.
207. World Health Organization (WHO) 2000 Steering Committee of the Western Pacific Region of the WHO, the International Association for the Study of Obesity Task Force. The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Geneva: WHO, 2000.
208. Sharma AM, Pischon T, Engeli S, Scholze J. Choice of drug treatment for obesity-related hypertension: where is the evidence? J Hypertension 2001; 19:667-674.
209. Keulen L, Henricksen EJ, Jacob S, Lang R. Antihypertensive Treatment and Cardiovascular Risk Management in Patients with the Metabolic Syndrome - Focus on SNS and Insulin Resistance. J Clin Basic Cardiol 2001; 4:193-195.
210. Wofford MR, Hall JE. Pathophysiology and Treatment of Obesity Hypertension. Current Pharmaceutical Design 2004; 10:3621-3637.
211. Douketis JD, Sharma AM. The Management of Hypertension in the Overweight and Obese Patient. Is Weight Reduction Sufficient? Drugs 2004; 64:795-803.
212. De la Sierra A, Segura J, Banegas JR, Gorostidi M, De la Cruz JJ, Armario P, Oliveras A, Ruilope LM. Hypertension Classified on the Basis of Ambulatory Blood Pressure Monitoring. Hypertension 2011; 57:898-902.
213. Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 2011; 57:911-7.
214. Bhatt DL, Kandzari DE, O’neill WW, D’agostino R, Flack JM, Katzen BT, Leon MB, Liu M, Mauri L, Negoita M, Cohen SA. A controlled trial of renal denervation for resistant hypertension. New England Journal of Medicine 2014; 370:1393-401.
215. Ram CV. Status of Renal Denervation Therapy for Hypertension: Still in Search of the Magic Bullet. Circulation 2019; 139:601–603.