CLINICAL APPLICATIONS OF BIOMATERIALS · type of electrospinning based on graphene–TiO2–ZnO...
Transcript of CLINICAL APPLICATIONS OF BIOMATERIALS · type of electrospinning based on graphene–TiO2–ZnO...

J Mater Sci: Mater Med (2017) 28:75DOI 10.1007/s10856-017-5881-z
CLINICAL APPLICATIONS OF BIOMATERIALS Original Research
Polyurethane/siloxane membranes containing graphene oxidenanoplatelets as antimicrobial wound dressings: in vitro andin vivo evaluations
Elias Shams1 ● Hamid Yeganeh2 ● Hossein Naderi-Manesh1 ● Reza Gharibi3 ●
Zuhair Mohammad Hassan4
Received: 9 November 2016 / Accepted: 8 March 2017 / Published online: 6 April 2017© Springer Science+Business Media New York 2017
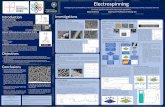
Abstract Preserving wounds from bacterial and fungalinfections and retaining optimum moist environment overdamaged tissue are major challenges in wound care man-agement. Application of wound dressings with anti-microbial activity and appropriate wound exudates handlingability is of particular significance for promoting woundhealing. To this end, preparation and evaluation of novelwound dres1sings made from polyurethane/siloxane net-work containing graphene oxide (GO) nanoplatelets aredescribed. The particular sol–gel hydrolysis/condensationprocedure applied for the preparation of dressings leads toan appropriate distribution of GO nanoplatelets in thedressing membranes. The crosslinked siloxane domains andthe presence of GO nanoplatelets within polymeric chainsoffered necessary mechanical strength for dressings.Meanwhile, a combination of hydrophilic and hydrophobicmoieties in dressing backbone enabled suitable wound
exudate management. Therefore, both of physical protectionfrom external forces and preservation of moist environmentover wound were attained by using the designed dressings.Widespread antimicrobial activity against gram-positive,gram-negative and fungal strains was recorded for thedressing with the optimum amount of GO, meanwhile, verygood cytocompatibility against fibroblast cells was noted forthese dressings. In vivo assay of the GO containing dressingon rat animal model reveals that the dressing can promotewound healing by complete re-epithelization, enhancedvascularization and collagen deposition on healed tissue.
Graphical Abstract
1 Introduction
Wound contamination happens when microscopic organ-isms enter a break in the skin [1]. The infection causes the
* Hamid [email protected]
* Hossein [email protected]
1 Department of Nanobiotechnology/Biophysics, Faculty ofBiological Sciences, Tarbiat Modares University, PO Box 14115-154, Tehran, Iran
2 Iran Polymer and petrochemical Institute, PO Box 14965/115,Tehran, Iran
3 Faculty of Chemistry, Kharazmi University, Tehran, Iran4 Department of Immunology, School of Medical Science, Tarbiat
Modares University, PO Box 14115-331, Tehran, Iran
Electronic supplementary material The online version of this article(doi:10.1007/s10856-017-5881-z) contains supplementary material,which is available to authorized users.

impediment in the healing of the wounds and may lead tolife-threatening complexities. Life-threatening wounds canpose both immediate and delayed risks of life. The former isdue to underlying organ damage or severe exsanguinations,and the latter is attributable to infection and sepsis. There-fore, wound infection is the major concern in the woundcare management. Treatment of infected injury relies onupon how serious the injury is, its area, and whether dif-ferent territories are influenced [2]. One effective methodfor treating of wound contaminations is the application of awound dressing that effectively hinders bacterial develop-ment inside and on the surface of dressing itself [3]. Byblocking development of biofilm growth on the dressing,this would hinder microscopic organisms from reseedingthe injury, which would permit the microscopic organismsto conquer the regular host protection components. Togenerate antimicrobial activity in wound dressing, theantimicrobial agents can be impregnated into the dressing[4, 5]. These active agents leach out into the wound bedgradually during their application and kill the invadedmicrobes may present in the wounded tissue [6]. Chemicalbonding of antimicrobial agent to the dressing backboneand contact killing of pathogenic microorganisms is anotherapproach for fulfilling this goal [7–10]. A combination ofthese two approaches is also possible [11, 12].
In all of the aforementioned methods, careful selection ofantimicrobial agents possesses prime importance. Nano-technology provides many potential opportunities to elim-inate the microbial pathogen [13]. Distinctive antimicrobialmetal and metal oxides nanoparticles, such as ZnO, Ag, Cu,Fe3O4, Al2O3, TiO3, and SiO3 are introduced in the scien-tific literature related to public health and some of thesematerials found their way into the commercial productsincluding wound dressing membranes. Fortunately, thesemetals and metal oxides can effectively suppress the growthof various bacteria [14–17]. However, one of the mainconcerns in using such metallic particles is their toxicity toeukaryotic cells, since they have to be released from thedressing material in order to be effective. Graphenic mate-rials (GMs) such as graphene (G), graphene oxide (GO),and reduced graphene oxide (rGO) are new nanomaterialsthat found a number of applications in the cutting-edgefields of biological and medical sciences [18–20]. Specifi-cally, generous endeavours have been committed to inves-tigating the more extensive therapeutic uses of G basedmaterials to microbial infections [21, 22]. There are reportsshowing the dependency of antimicrobial activities of gra-phenic materials to their physicochemical or structuralproperties such as lateral size, layer number, morphology,and dispersibility [23, 24]. By proper control of these fac-tors a superior inhibition ability towards bacteria growth canbe attained, therefore, promising applications for this typeof low-cost and highly effective carbon nanomaterials as the
bactericidal material is expected. Application of GMs as theantimicrobial component of wound dressings has beenconsidered very recently in few publications. In the articlereported by Deepachitra and co-workers [25], GO wasincorporated in the collagen-fibrin composite film and usedas wound dressing material. Both in vitro and in vivo stu-dies revealed faster wound healing in rats compared to thoseof collagen-fibrin and control. Khan [26] subjected GO toNIR radiation (λ= 1064 nm) to eliminate bacteria and fungiand control the wound infection. Madhavan [27] designed atype of electrospinning based on graphene–TiO2–ZnOcomposite nanofibres and claimed the potential use of thesenanofibres in an antibacterial wound dressing. The electro-spun nanofibres made from chitosan-poly (vinyl alcohol)-GO reported by Liu [28] displayed excellent antibacterialactivity against E. coli, indicated their potential for woundhealing. Chitosan-poly (vinyl alcohol) nanofibres contain-ing G were also prepared for wound healing by Lu [29].These electrospun fibres led to rapid and complete woundhealing compared to neat fibres and controls. They arguedthat the existing free electron in G could inhibit the multi-plication of prokaryotic cells without affecting the eukar-yotic cells, thus making G suitable as wound dressingcomponent. He [30] incorporated GO to sodium alginatefibres to enhance its strength. The hybrid film could swellinto hydrogel suitable for fabrication of wound dressing.Fan [31] prepared a wound dressing by cross-linking theGO–Ag composites into the polymer hydrogel, whichshowed antibacterial activity and accelerated the wound-healing. Sun [32] prepared a kind of Band-Aid with anti-bacterial property suitable for wound disinfection based onG quantum dots and a low level of H2O2.
To expand the present knowledge about utilization ofGMs for biomedical applications, a novel category ofwound dressing composed of GO incorporated poly-urethane/siloxane networks was introduced in the presentstudy. The versatile chemistry followed in this workenabled us to tune the physicomechanical and biologicalproperties of the final dressings in a way that the as-prepared membranes showed excellent wound exudatesmanagement, biocompatibility, antimicrobial activity andmechanical strength, which are necessary for proper woundcare. The performance of the prepared materials as wounddressing membranes was evaluated based on data recordedunder in vitro and in vivo conditions.
2 Materials and methods
2.1 Materials
Poly(tetramethylene ether) glycol (PTMEG, Mn 2000 gmol−1)
was supplied from Aldrich (Taufkirchen, Germany). It was
75 Page 2 of 14 J Mater Sci: Mater Med (2017) 28:75

freed from moisture by storing in a vacuum oven at 80 °Cfor 24 h. Poly(ethylene glycol) (PEG, Mn 2000 g mol−1)from Aldrich was dried through azeotropic distillation usingdry toluene as solvent. Tetraethoxysilane (TEOS) and (3-aminopropyl)triethoxysilane (APS) were obtained fromAldrich and used as received. Isophorone diisocyanate(IPDI) from Merck (Darmstadt, Germany) was vacuumdistilled. N-Methylpyrrolidone (NMP) and toluene werepurified by distillation over CaH2 and sodium, respectively.xGnP® graphene nanoplatelets, grade C-750 (average sur-face areas of 750 m2 g−1, and atomic oxygen concentrationabout 8%) from XG sciences (Lansing, MI, US) was usedwithout further treatments. Dibutyltin dilaurate (DBTDL)and tetrahydrofuran (THF) were purchased from Aldrichand used as received. Diethylene glycol from Merck wasdried via storing in a vacuum oven at 80 °C overnight. S.aureus (ATCC 6538) and E. coli (ATCC 25922) bacteriaand C. albicans (ATCC 10231) were purchased from Ira-nian Research Organization for Science and Technology(IROST, Tehran, Iran). Human skin fibroblast cells (Hu02)was purchased from Iranian Biological Resource Centre(IBRC, Tehran, Iran).
2.2 Synthesis of triethoxysilane-terminated polyurethaneprepolymer (Si-PU)
Si-PU was prepared according to the procedure reported inour previous publication [33], briefly:
A polymerization kettle was charged with PEG (21.43 g),PTMEG (50.00 g) and NMP (40 ml). Under ambient tem-perature, IPDI (15.88 g) was introduced into the reactorduring 30 min, then the temperature was increased to 85 °C.The reaction progress was monitored through measurementof free NCO content (ASTMD-2572). After completion ofthis step, a solution of diethylene glycol (1.89 g) dissolvedin NMP (25 ml) was added and the reaction was continuedat 85 °C for about 1 h. Then, the temperature was reduced toambient condition. The reactor was charged with a solutionof APS (7.90 g) dissolved in NMP (40 ml). The mixture wasstirred for 30 min, and then the temperature increased to 50°C for 3 h. The reaction product with predetermined solid
content (50 w/w%) was transferred to a glass bottle, sealedand kept in the refrigerator for subsequent use.
2.3 Preparation of GO containing polyurethane-siloxanemembranes (XSi-PU/GO)
The nanocomposite dressing membranes were preparedaccording to the formulations given in Table 1. At the first,the appropriate amount of GO powder was added to a 100ml beaker containing NMP solvent (25 ml). The mixture wasstirred at room temperature for 24 h using a magnetic stirrer.Desired amounts of Si-PU and TEOS were then added andthe resulting mixture was subjected to ultrasound irradiationusing ke 76 probe for 30 min. Finally, the catalytic amountof HCl solution (0.1M) was dropped into the beaker and theresulting mixture was stirred vigorously for 1 min. After theremoval of any trapped air by rapid evacuation, the mixturewas cast slowly into a clean Teflon mold. The mold was keptat room temperature under ambient atmospheric conditionovernight. It was then heated in an oven at 80 and 100 °C for10 and 2 h respectively. The temperature was reduced againto 80 °C and high vacuum was applied to ensure completeremoval of any residual solvent. The thickness of themembrane was adjusted by controlling the solid content ofreaction mixture.
For the preparation of a neat polyurethane/siloxanemembranes, the mixture of Si-PU, TEOS and an appropriateamount of HCl solution was dissolved in NMP (Table 1)and the rest of procedure was repeated as described above.
For purification of the prepared membrane and removalof residual raw materials and solvents, all of the sampleswere immersed into ethanol (70% w/w) for 6 h, distilledwater for another 6 h and fully dried under reducedpressure.
2.4 Characterization
2.4.1 Spectroscopic, tensile and dynamic-mechanicalanalysis
Fourier transform infrared spectra (FTIR) were recorded ona Bruker IFS 48 instrument (Bremen, Germany). All spectra
Table 1 Different formulationsof wound dressing membranes
Sample Si-PU solution (g) TEOS (g) HCl (g) GO (g) Gel content (%)a
XSi-PU 4.00 0.40 0.50 – 98.8b± 0.5
XSi PU/GO2.5% 4.00 0.40 0.50 0.06 98.7b± 0.6
XSi-PU/GO5.0% 4.00 0.40 0.50 0.12 98.5b± 0.8
XSi-PU/GO7.5% 4.00 0.40 0.50 0.18 97.6b± 1.2
According to the analysis of variances P-values of <0.05 were considered significanta The number of replicas was 3b The difference between quantities is not significant (P ≥ 0.05) for data of each column
J Mater Sci: Mater Med (2017) 28:75 Page 3 of 14 75

were obtained in the air as a function of time with 16 scansat a resolution of 4 cm−1 and a spectral range of 400–4000cm−1. The X-ray diffraction (XRD) pattern of the sampleswas recorded in a Siemens X-ray diffractometer (D5000Germany) at crystal monochromated Cu Ka radiation in theangular range 2–15 (2θ) at 35 kV operating voltage and25 mA current. Measurement of tensile strength,elongation-at-break and modulus of samples were carriedout using a tensile tester (Instron 6025, MA, US) with acrosshead speed 50 mmmin−1. Samples were cut into barsof 50 mm length and 5 mm width. The test was performed atroom temperature. For each sample, five specimens weretested. Dynamic mechanical thermal analysis (DMA) wasperformed using a Triton instrument (model Tritec 2000,England) within a temperature range of −100–200 °C, aheating rate of 3 °C/ min−1 at a frequency of 1 Hz in tensilemode. The loading amplitude was set at 20 μm. Sampledimensions were 30× 10× 1 mm3.The values of storagemodulus, loss modulus, and tan δ vs. temperature wererecorded for each sample. The maximum temperature of tanδ curves was considered as glass transition temperature.
2.4.2 Measurement of water vapor transmission rate(WVTR)
The moisture permeability of the synthesized materials wasestimated by the measurement of the water vapor trans-mission rate (WVTR) according to the procedure reportedin ASTM E96/E96M. The following equation was applied:
WVTR ¼ Wi �Wt
A� t
WVTR was expressed in g−1 m2 per day. A, Wi and Wt
designated the area of cup mouth (m2), the weight of watercontaining cup before and after placing in the oven at 37 °Cand 35% humidity and t showed the duration ofmeasurements.
2.4.3 Gel content, surface, and bulk hydrophilicity
The progress of crosslinking reaction for the preparedsamples was estimated by measuring their gel content. Forthis purpose, the membranes were dried under vacuum for24 h at room temperature and weighed. Then, the sampleswere extracted by THF in a Soxhlet extractor for 24 h. Theinsoluble part was dried at 50 °C and weighed. The gelcontent was defined as follows:
Gel content% ¼ Wd
Wi� 100;
where Wd and Wi designated the weight of dried membraneafter extraction and the initial weight of the membrane,respectively.
The static contact angle of water droplets on as-preparedfilms surface was utilized as a means for measurement ofsurface hydrophilicity. For this purpose, an optical videocontact angle system (OCA-15-plus, Dataphysics, Ger-many) was used. Bulk hydrophilicity of the samples wasalso assessed based on measurement of equilibrium waterabsorption (EWA %) in PBS buffer. Completely dried andweighed samples (20× 10 mm) were placed in the beakercontaining PBS. The swollen samples were wiped gentlywith a soft paper tissue before being weighed. EWA% wasdetermined using the following equation:
EWA% ¼ Ws �Wd
Wd;
where Wd and Ws are the weights of dry and swelled films,respectively.
2.4.4 Conductivity analysis
The electrical conductivity (S cm−1) of the samples wasmeasured at room temperature using a home-made four-point probe instrument, utilizing the following equation:
σ ¼ I Ln 2Vπdn
;
where V, I and dn represented potential in volt, current inampere and thickness of the sample in cm, respectively.
2.4.5 Cytotoxicity of dressing membranes
The freshly prepared dressing membranes were immersed inthe culture medium for 7 days at 37 °C. The possibleexistence of toxic material in this medium was examined byevaluating the metabolic activity of Hu02 fibroblast cellscultured in medium containing extracted leachates fromdifferent samples. The procedure reported in our previouswork [10] was followed for this assessment. The percentageof relative cell viability was calculated according to fol-lowing equation:
Cell viability% ¼ ODsample
ODnegative control;
where OD designates the optical density. A growth med-ium, containing cells but no extracted leachates were con-sidered as negative control. Each measurement was repeatedat least three times.
2.4.6 Cell adhesion and proliferation on dressingmembranes
Hu02 cells were cultured at 37 °C/5% CO2 in 10% bovinecalf serum, high glucose-DMEM culture medium supple-mented with 1% penicillin, streptomycin mixture. Cells at90% confluency were detached from the flask by treating
75 Page 4 of 14 J Mater Sci: Mater Med (2017) 28:75

with a trypsin-EDTA solution (0.05%). The cells werecounted using a Neobar lam. The dressing membranessoaked in PBS overnight and sterilized by UV irradiation(15 min each side). They were cut to a size fit the bottom ofeach well of a 96-well culture plate. Then, the culturemedium containing 5× 103 Hu02 fibroblast cells wereplaced on the membrane and incubated at 37 °C for 45 minto enable the cells to attach on the membrane surface. Themembrane/cell constructs were supplied with more culturemedium and the incubation period was extended to pre-determined time points (1, 3 and 5 days). At the end ofcertain time points, the seeded membranes were washedwith PBS to remove unattached cells and then the mem-branes were transferred to new culture plates. Cells wereharvested after 3 min incubation with 0.25 w% trypsin and1 mM EDTA at 37 °C, and the quantification of cells wasdone by the MTT assay using following equation:
Cell viability% ¼ ODsample � ODpositive control
ODnegative control;
A growth medium, containing cells but no membrane wasconsidered as the negative control and a medium containingmembrane but no cells were considered as positive control.Each measurement was repeated at least five times.
2.4.7 Antibacterial study
Antimicrobial activity of prepared membranes was eval-uated against S. aureus (ATCC 6538) and E. coli (ATCC25922) bacteria and C. albicans (ATCC 10231) using“colony forming count” method based on procedure repor-ted in ASTM E 2180-07. Bacteria at inoculated con-centration of 2× 108 CFU ml−1 and membranes with thedimensions of 1 cm× 1 cm were used throughout the tests.Bacterial cultures grew for 18 h at a specified temperature intryptic soy broth. 1.0 ml of inoculated agar slurry waspipetted onto the test and control samples and allowed togel. 24 h after contact; surviving microorganisms arerecovered via elution of the agar slurry inoculums from thetest substrate into neutralizing broth and extracted via vor-texing that provides complete removal of the inoculum fromthe test polymers. Serial dilutions were made and thenspread plates were made of each dilution and incubated at37 °C for 48 h. Colony numbers were counted and recordedfor each dilution plate. The geometric mean of the numberof organisms that recovered and percent reduction wasdetermined by the following equations:
Geometricmean ¼ log10X1þ log10X2þ log10X33
%Reduction ¼ a� bð Þ�100a
2.4.8 In vivo assay of dressing membranes
The wound healing characteristics of the prepared wounddressings were evaluated using a rat model. All experi-ments were performed with the approval of the AnimalUse and Care Administrative Advisory Committee ofTarbiat Moddares University. The Wistar rats with anaverage body weight of 200–250 were employed throughthese experiments. The animals were anesthetized with anintraperitoneal injection of ketamine (85 mg kg−1) andxylazin (15 mg kg−1) and then the dorsal hair of rats wasshaved and a full-thickness skin wound at about 1.5 cm2
area was prepared by excising the dorsum of the animals.Thirty-six rats were randomly divided into three groups,named as group 1, 2 and 3. The wound of group 1 rats(control group) were covered by sterilized cotton gauzewithout any other intervention. The wounds of group 2and 3 rats were covered with neat Si-PU and Si-PU/GO5.0% dressing membrane, respectively. The dressingswere fixed in the wound position by an elastic adhesivebandage.
The dissected wounds were not sterilized and the testedanimals kept in separate cages under the environmentalcondition to avoid antibacterial interference by externaldisinfectant agents. Macroscopic photographs of thewounds were taken, and the wound area was measured aftercertain postoperative time. The percentages of woundsclosure rate were calculated according to the followingformula:
Wound closure rate %ð Þ ¼ A0 � At
A0� 100;
where A0 and At were designated to initial wound area andwound area at designated time, respectively.
For the histological analysis, the dressings were removedfrom sacrificed rats and then, the healed wound skin tissueswere dissected. The cut tissue was fixed in 10% v/v buf-fered formalin, dehydrated in a graded ethanol andembedded in paraffin. Tissue sections were processed forHematoxylin & Eosin (H&E) and Malory Trichromestaining.
2.5 Statistical analysis
Statistical analyses were performed via PASW statisticsprogram package, version 18 (SPSS Inc., Chicago, IL,USA). Comparison of the obtained data for different sam-ples was performed with One-Way ANOVA using Tukeyposthoc test. The significance level was set at p ≤ 0.05.
J Mater Sci: Mater Med (2017) 28:75 Page 5 of 14 75

3 Results
3.1 Synthesis and spectroscopic characterization ofdressings
The methodology followed for the preparation of dressingmembranes was described in Supplementary Information(Schemes S1 and S2), and the formulations for these dres-sing were presented in Table 1.
FTIR spectrum of Si-PU (Supplementary InformationFig. S1a) displayed a broad band centred at 3401 cm−1
which was related to the stretching vibration of urethaneand urea N-H groups. The urethane (NH–CO–O) and urea(–NH–CO–NH–) carbonyl groups were combined anddetected as a strong broad peak centred at 1685 cm−1. Thesplitting of carbonyl peaks was not detected. Since the FTIRspectrum of Si-PU was taken as an admixture in NMPsolvent, therefore, the amide bond of the solvent was mixedwith peaks of carbonyl groups of Si-PU. The peak observedat 1543 cm−1 was related to C–N stretching, combined withN–H out-of-the-plane bending vibrations of the urethaneand urea groups. The peak appeared at about 1100 cm−1
was attributed to ether (C–O–C) bonds arising from polyolsegments. The presence of O–Si–O and urea carbonylgroups peaks at 778 and 1682 cm−1 and the absence ofNCO peak at 2230 cm−1 indicated the complete reaction ofisocyanate and NH2 groups.
The suitability of reaction condition for the sol–gelprocess was confirmed by high values for gel content of theprepared membranes measured using THF as solvent(Table 1). The chemical identity of the dressing membraneswas studied using FTIR spectroscopic method. Repre-sentative spectra of polyurethane/siloxane networks pre-pared in the presence or absence of GO (XSi-PU and XSi-PU/GO5.0%) are shown in Supplementary Information Fig.S1b, c. For both materials, the presence of the peak at about1030 cm−1, as the characteristic stretching vibration of theSi−O−Si bond and almost fading of the peak at 771 cm−1
related to stretching vibration of O−Si−O linkages con-firmed the successful formation of siloxane network throughsol–gel reaction in the presence/absence of GO additive. Inaddition, after removal of NMP solvent, the carbonyl peakof urethane groups was detected at 1717 cm−1 for dressingwithout GO. After the introduction of GO into the for-mulation of dressing, this peak was shifted to a lower fre-quency (1706 cm−1), as a result of hydrogen bonding typeinteraction of carbonyl groups with hydroxyl and carboxylicgroups present on the surface of GO.
3.2 Hydrophilicity of wound dressing membranes
EWA and WVTR were measured to find insight about theability of the designed dressing membranes for wound
exudates management (Table 2). The XSi-PU membraneshowed the EWA at around 70%. After incorporation ofGO, the EWA significantly decreased and this reductionwas the highest for that sample with a maximum amount ofGO. The WVTR data for the prepared dressing membranesand some of the commercially available dressings are alsosummarized in Table 2. The XSi-PU sample showed aWVTR at about 1950 g m−2 day. Upon introduction of GOnanoplatelets into the dressing membrane a considerablereduction in WVTR was observed.
Surface hydrophilicity of dressings is usually expressedin terms of contact angle for a water drop on the dressingsurface. The pristine membrane without GO (XSi-PU)showed the contact angle of about 65°, however, the waterdroplet contact angle was increased up to 82° for XSi-PUGO7.5% with the highest concentration of GOnanoplatelets.
3.3 Viscoelastic, tensile strength and phase structure ofdressing membranes
The viscoelastic behaviour of dressing materials with andwithout GO nanoplatelets was studied using DMA techni-que. The experiments were carried out in the tensile modeas a function of temperature from −100 to 150 °C. Typi-cally, variations in storage modulus (E′), loss modulus (E′′)and loss tangent (tan δ) as a function of temperature wererecorded and the results are displayed in SupplementaryInformation Fig. S2. The prepared membranes showed atwo-phase structure since two main transitions were detec-ted in their DMA curves. The positions of these two peakswere shifted to higher temperature upon raising of fre-quency, therefore, these peaks were attributed to the glasstransition (Tg) of different domains in the structure of theprepared samples. Upon introduction of GO nanoplateletsinto the dressing formulations, no considerable changes in
Table 2 Hydrophilicity and WVTR of the prepared wound dressingmembranes
Membranes Contact anglea WVTR (g/m2 day)b EWA (%)b
XSi-PU 65± 2c 1954± 28c 71.3± 1c
XSi-PU/GO2.5% 72± 1d 1246± 16d 53± 2d
XSi-PU/GO5.0% 73± 3d 836± 13e 43± 1e
XSi-PU/GO7.5% 82± 2e 685± 17f 35± 2f
Op Site – 792 46
Metoderm 823 –
Duoderm 886 –
According to the analysis of variances P-values of <0.05 were consideredsignificant. The difference between quantities with similar superscripts(c, d, e, or f) is not significant (P ≥ 0.05) for data of each columna The average of 9 different reading was consideredb The number of replicas was 3
75 Page 6 of 14 J Mater Sci: Mater Med (2017) 28:75

the phase structure of polymeric networks were detectedand the position of Tg peaks remained almost intact.However, an increase in the elastic modulus at rubberyplateau region was observed for these samples.
The mechanical strength of dressing membranes wasevaluated by examining their stress–strain curves (Fig. 1).Based on these curves, all of the prepared membranesshowed the general behaviour of lightly crosslinked elas-tomers as they exhibited reversible deformation, low initialmodulus, and increased modulus and tensile strength athigher deformation due to the alignment of amorphouschains in the direction of tension. The tensile strength,modulus, and elongation at break of GO containing mem-branes were significantly higher than the neat network andthese values increased with raising the GO nanoplatelets tocontent up to a maximum of 5 wt.%. The mechanicalproperty of the dressing materials was also evaluatedimmediately after removing them from PBS solution at 37 °C for 2 days. The strain-stress curves of the dressingmembranes recorded at hydrated state were also plotted inFig. 1. A reduction in the tensile strength of dressingmembranes was observed under a wet condition with thesame trend recorded for these samples under the dry state.
The prepared membranes were also subjected to XRDanalysis. The representative X-ray diffractograms for XSi-PU and XSi-PU/GO 5% dressing membranes are shown inSupplementary Information Fig. S3. The broad XRD dif-fraction peak centred at about 20° (2θ) recorded for XSi-PUsample was related to the characteristic diffraction peak ofthe amorphous polyurethane-siloxane network. With theintroduction of GO nanoplatelets into the polyurethane-siloxane network, the height of observed peak wasintensified while its broadness was decreased. The recordeddata implied the improvement in the crystallinity ofpolyurethane-siloxane network upon introduction of GO.
3.4 Cytocompatibility and antibacterial activity ofdressing membranes
To have an insight about cytocompatibility of dressings,two set of experiments were performed. Firstly, the dres-sings were put into PBS for 1 week and then the humandermal fibroblast cells were cultured in the medium con-taining leachates extracted from dressing membranes. Theviability of cells was evaluated by MTT assay and nodetectable reduction in viability of cells was recorded forthe cultivated cells. (Supplementary Information Fig. S4). Inaddition, there was no significant difference (p ≥ 0.05)between the viabilities of cells exposed to the leachates ofsamples without GO or those containing different amountsof GO nanoplatelets. Secondly, the human dermal fibroblastcells were directly seeded on the dressing membranescovered the bottom of tissue culture plate wells. The pro-liferation rate of cells grown on the surface of dressingmembranes was investigated by MTT assay at certain timeinterval. The recorded results at three certain time points(1, 2 and 3 days) are collected in Supplementary Informa-tion Fig. S5. There was no significant difference (p ≥ 0.05)between viability of cells grown on samples with variousamounts of GO. With extending the culturing time,the cells were continued their growth and proliferation forall samples.
The capability of prepared dressing for preventingwound infection was evaluated by the quantitative “colonycounting method” against E. coli and S. aureus as gram-negative and gram-positive bacteria, as well as C. albicansas a fungal strain (Fig. 2 and Table 3). Fortunately, anti-microbial activity was detected for those dressing mem-branes containing the GO nanoplatelets. Also, it was foundthat this activity was concentration dependent and increasedwith a higher concentration of GO.
3.5 In vivo wound healing study
For evaluating the wound healing process in the presence ofGO containing dressing membrane, the XSi-PU/GO5%
Fig. 1 Stress–strain curves of dressing membrane under a dry and bhydrated states
J Mater Sci: Mater Med (2017) 28:75 Page 7 of 14 75

sample was utilized for covering a full thickness woundcreated in the dorsal area of Wistar rat. XSi-PU and cottongauze were also used as control samples. The surfaces of thetreated wounds were photographed and closure rate wascalculated by measuring the area of the wounds at certaintime intervals. The images of the open excision wounds andthe percentage of wound closure at various time periodswere shown in Fig. 3a and b, respectively. Based on Fig. 3aand b findings, much better healing efficacy was noticed forthe GO containing wound dressing membrane (XSi-PU/GO5%) than the dressing without GO (XSi-PU) at the sametime intervals. On day 7, the wound covered with XSi-PU/GO5% membrane showed 55% wound closure, whereas theXSi-PU treated wounds and control groups showed woundclosures of 48 and 34%, respectively. After 14 days oftreatment, there was 89% reduction in the size of woundcovered by XSi-PU/GO5% dressing, whereas wounds sizereduction in XSi-PU treated wounds and control group were81 and 70%, respectively. On the 20th day, the woundscovered with XSi-PU/GO5% showed 98% wound closure,whereas, 91 and 81% decrease in the size of the woundwere recorded for wounds protected by XSi-PU membraneand cotton gauze, respectively.
The H&E and Malory Trichrome (MT) stained sectionsof the wounds covered with XSi-PU/GO5% and XSi-PUdressings, as well as control group covered with cottongauze on days 14 and 20 are shown in Fig. 4. Based onFig. 4 images, at day 14, the H&E stained section of thewound covered with XSi-PU/GO5% dressing showed uni-form and thick epithelium layer. Also, re-epithelization waspronounced in the wounds covered with XSi-PU sample,while in the case of the control group, epithelization wasstill in early stage. Furthermore, neovascularization atnewly formed tissue was more pronounced for the woundcovered with XSi-PU/GO5% compared to those treatedwith either XSi-PU or cotton gauze. Close inspection ofH&E stained area of the wound dressed with XSi-PU/GO5% membrane at days 20 revealed the complete re-epithelization and reconstruction of epidermis and dermis.Also, some of the secondary structures of the healed skin,like hair follicle, could be observed, which were in theirinitial stage of development.
MT staining of the wound tissue at 14th day confirmedcollagen deposition in sections of all treated woundsincluding XSi-PU/GO5%, XSi-PU, and cotton gauze. Therewas a clear difference between collagen expressions in thewounds covered with XSi-PU/GO5% and XSi-PU in com-parison to the cotton gauze groups. Although, higher col-lagen expression was observed in both groups, but thethickness of deposited collagen in the wounds covered withXSi-PU/GO5% membrane was higher than that of XSi-PUtreated the wound. On day 20, the thickness of depositedcollagen in wound treated with XSi-PU/GO5% group wasconsiderably higher than that of both XSi-PU and cottongauze treated wounds. Close inspection of MT staining
Fig. 2 Antibacterial activity ofthe prepared dressingmembranes against S. aureus,E. coli, and C.albicans
Table 3 Bacterial reduction percent of the dressing membranes
Sample E. coli S. aureus C. albicans
XSi-PU 0 0 0
XSi-PU/GO2.5% 57 58 60
XSi-PU/GO5.0% 100 100 100
XSi-PU/GO7.5% 100 100 100
75 Page 8 of 14 J Mater Sci: Mater Med (2017) 28:75

section wounds of XSi-PU/GO5% treated groups, showeddense and parallel collagen deposition with higher alignmentand maturation level in comparison to other two groups.
4 Discussion
4.1 Synthesis and characterization of wound dressingmembranes
To construct wound dressing with the ability to maintainoptimum healing milieu over a damaged area and alsoproviding the necessary protection from external mechan-ical stresses (pressure, friction, and shear) during the heal-ing process, utilization of polyurethane/siloxane basedmaterial containing GO nanoplatelets was considered in thepresent study [10, 11]. To tune the overall ability of dres-sings for managing wound exudates, a mixture of twohydrophobic (PTMEG) and hydrophilic (PEG) polyols at70/30 wt.% was introduced into the backbone of dressing
membranes. The partial chain extension of the intermediatecompound with an inferior molar concentration of diethy-lene glycol led to the formation of higher molecular weightNCO-terminated polyurethane prepolymer, which subse-quently end-functionalized with APS coupling agent. Thisstep was considered to take advantages of the inter-molecular attraction of extra urethane bonds formed duringchain extension reaction. The overall mechanical strength ofdressing membrane was improved via increasing the inor-ganic siloxane domain content by addition of TEOS to themembrane base formulations.
GO nanoplatelets were added to the base formulation atdifferent weight percent. The hydrolysis reaction of alkox-ysilane groups present in Si-PU and TEOS and co-condensation of these materials with the hydroxyl groupsalready available on the surface of GO nanoplatelets led tothe simultaneous formation of siloxane domain and inte-gration of GO into the final polyurethane/siloxane networks.High gel content of these networks and their spectroscopiccharacteristic confirmed successful incorporation
Fig. 3 Photographs (a) andclosure rate (b) of woundstreated with gauze (control),XSi-PU and XSi-PU/GO5%during the wound healingprocess for 20 days. Accordingto the analysis of variances,*P< 0.05, values aresignificantly different from thepreviously compared group
J Mater Sci: Mater Med (2017) 28:75 Page 9 of 14 75

4.2 Physical and mechanical properties of wounddressing membranes
Creation and keeping up of the optimal moist condition overinjured tissue are generally accepted as the best state forwound healing process. In fact, cells can grow, proliferateand migrate at an increased rate to optimize the formation ofnew tissue under moist environment [34]. In addition,aqueous wound medium with several nutrients and vitaminsis not only essential for cell metabolism and growth, butalso provides a transport medium for a variety of bioactive
molecules such as enzymes, growth factors, and hormones.The different cells in the wound area communicate witheach other via these mediators, making sure that the healingprocesses proceed in a coordinated manner.
Application of proper wound dressing is the main toolfor moist wound therapy. To fulfill this condition, theoptimal wound dressing should establish a balanced abilitybetween absorption of wound exudates and evaporativewater loss from the wound site. The proper ability of XSi-PU membrane for the absorption of water was devoted toembedded PEG segments with high ability for creating
Fig. 4 Representative images ofMT and H&E stainedhistological sections a day 14and b day 20 after initialwounding. Scale bars equal to200 μm. Arrows indicated theblood vessels
75 Page 10 of 14 J Mater Sci: Mater Med (2017) 28:75

hydrogen bonding type interaction with water molecules.As expected, after incorporation of GO with the hydro-phobic nature into the dressing membrane formulation, theEWA significantly decreased.
Low WVTR causes the exudate build-up below a wounddressing which is harmful to healthy skin surrounding thewounded area, meanwhile, rapid water loss across dressingmembrane due to its high WVTR can lead to surfacedehydration of wounded area and scab formation. There-fore, optimal WVTR is required to keep moist environmentover damaged tissue [35]. The presence of impermeable GOnanoplatelets with very high aspect ratio limited the watertransportation across the dressing membrane and therefore,the WVTR values decreased as a result of an increasedpenetration path of water molecules. The average measuredvalues of WVTR for the designed GO containing mem-branes, especially those containing equal or lower than 5 wt.% of GO were comparable to some related commercialproducts as depicted in Table 2. To this end, the range ofrecorded EWA and WVTR data for the prepared dressingmembranes indicated their favourable performance to keepmoist wound milieu over low to moderate exuding wounds.
Surface hydrophilicity of dressings is usually expressedin terms of contact angle for a water drop on the dressingsurface. The original dressing with no added GO showedmoderate hydrophilicity. The increased hydrophobicity ofsamples after the introduction of GO nanoplatelets wasattributed to those GO nanoplatelets that migrated to thesurface of dressings. Previous studies revealed that thesamples with water contact angles in the range of 40–80°have good affinity for supporting cell growth and adhesion[36]. Therefore, dressing membranes containing up to 5 wt.% of GO nanoplatelets (XSi-PU/GO2.5%, XSi-PU/GO 5%)with a contact angle of about 70° were favoured for sup-porting the cellular activity at the wounded tissue.
DMA study revealed a two-phase structure for the pre-pared dressing membranes. The first transition at a tem-perature range of −50 to −60 °C (derived from tan δmaxima) was attributed to Tg of soft PEG and PTMEGsegment. The second transition at the higher temperature(−15 to −20 °C) was attributed to the Tg of the hard seg-ment composed of siloxane domain and urethane/urea lin-kages. Although no considerable changes in the phasestructure of polymeric networks and the position of Tg
peaks were detected due to the added GO nanoplatelets, anincrease in the elastic modulus was observed for thesesamples. This behaviour was in accordance with previousstudies regarding incorporation of GO nanoplatelets intopolyurethane based networks [37] and it was in line with theEshelby’s and Mori-Tanaka’s theories of inclusions [38].Close inspection of DMA curves revealed a less significantincrease in the elastic modulus of the glassy region as aresult of lower filler/matrix modulus ratios in the glassy
region compared to the rubbery state. In fact, the introducedGO nanoplatelets could not reinforce the nanocomposites inglassy regions, but it significantly reinforced the poly-urethane/siloxane networks in the rubbery region. Increas-ing in rubbery plateau modulus and decreasing in dampingfactor (height of tan δ peaks) of samples containing GOnanoplatelets at high loading percentage (XSi-PU/GO5%,XSi-PU/GO 7.5%) could be attributed to participation ofGO nanoplatelets with high concentration of hydroxylgroups in the sol–gel reaction and integration with poly-urethane/siloxane network. The extension of rubbery pla-teau region up to 150 °C and consequently, preservation ofdimensional stability of GO-incorporated polyurethane/siloxane networks up to this temperature implied thatthe prepared dressings can withstand the high temperature(105 °C) needed for the autoclave sterilization procedure.
For protecting of damaged tissue from external forcesand loads applied by the patient upon movement, a wounddressing should have sufficient dimensional stability. Aswell, for proper handling and replacement of the dressing,these materials should possess appropriate tensile strength,flexibility, and elasticity [39]. To find an insight regardingthis important issue, the tensile property of dressingsmembranes was investigated (Fig. 1). Generally, the tensilestrength, modulus and elongation at break of GO containingmembranes were significantly higher than the neat networkand these values increased with raising the GO nanoplate-lets content up to a maximum of 5 wt.%. This behaviourcould be related to the presence of well dispersed GOnanoplatelets in the nanocomposites membranes. Therecorded result confirmed excellent interfacial adhesion andstrong interaction between GO nanoplatelets and poly-urethane/siloxane networks resulting from successful parti-cipation of GO in sol–gel reaction. The slight deteriorationin the tensile property of the sample with the highestloading of GO nanoplatelets (XSi-PU/GO 7.5%) can beexplained by irregular dispersion of GO and consequentformation of GO aggregates.
The applied dressing materials on the wounds site areexposed to the wound exudates. The absorbed liquid canlead to a serious drop in the overall mechanical strength ofdressing due to deterioration of intermolecular attraction ofchain segments of the polymeric network. Hence, themechanical property of the dressing materials was alsoevaluated after immersing them into PBS at 37 °C (Fig. 1).As expected, due to plasticization effect of absorbed watermolecules, the tensile strength of dressing membranes wasreduced. The trend of changing in tensile property ofsamples at hydrated state was similar to those observedunder dry condition. Both of elongation at break and tensilestrength of the dressing membranes were increased up to amaximum of 5 wt.% of added GO. A slight decrease intensile strength was detected at higher loading of GO. The
J Mater Sci: Mater Med (2017) 28:75 Page 11 of 14 75

reduction in tensile property of dressing membrane athydrated state was lower for those containing GO and thisdifference in property of the samples at dry and hydratedstates was also less important with increasing the con-centration of GO. This phenomenon was attributed to thereinforcing effect of GO nanoplatelets and also to the lowerwater absorption of the samples containing the higheramount of GO. The measured tensile strength of the pre-pared dressing membranes (2.5 to 12MPa at dry and 1 to 6MPa at hydrated state) was comparable with the tensilestrength of healthy skin (2.5–16MPa). It is worth to noticethat, the developed GO containing membranes showedsuperior tensile strength than some of the commerciallyavailable dressings like Resolut LT or Kaltostat (R), withtensile strength values of 1.7 and 0.9 MPa, respectively.
XRD analysis of the prepared dressings showedenhanced crystallinity of polyurethane-siloxane networkcontaining GO nanoplatelets. This observation was attrib-uted to the presence of exfoliated and well-dispersed GOnanoplatelets into the polyurethane-siloxane matrix. In fact,the GO sheets merged into the polyurethane-siloxane matrixduring the sol–gel reaction and acted as nucleating agent.This recorded phenomenon was in accordance with theprevious report regarding the significant increase in hardsegment crystallinity of polyurethane film upon incorpora-tion of GO [40]. The outcome of this happening was anenhancement of tensile strength for GO containing dressing.In fact, this modification increased the potential ability ofdressing for providing better protection of wounded tissueagainst external forces. Indeed this single property is notenough for proper protection of wounds. Keeping moist andhygiene environment over wounded tissue have determin-ing effects on appropriate healing of damaged skin. Theseextra properties were tuned by balancing the hydrophilicity-hydrophobicity ratio of dressing attained by chemicalmodification of dressing backbone and utilization of GO asan antimicrobial agent.
4.3 Biological properties of wound dressing membranesunder in vitro condition
Application of antibacterial agents on wound dressingmaterials may deteriorate their cytocompatibility and con-sequently have an adverse effect on growth and prolifera-tion of cells at the damaged tissue. Therefore, evaluationand controlling of this issue are crucial for the new com-pounds developed in the present study. Based on two set ofexperiments performed for evaluation of Fibroblast cellsviability in contact with either dressings or leachatesextracted from dressing, no toxicity was detected. For allsamples, the Fibroblast cells continued their growth andproliferation without any problem. The recorded resultsimplied that the based polyurethane/siloxane network
selected for the preparation of dressing membranes was nottoxic and the added GO at the studied range of concentra-tion was not influenced on excellent cytocompatibility oftheses dressing membranes.
It is well accepted that the bacterial or fungal infectionscan delay the wound healing process and even cause seriouscomplications [41]. Covering of wounds with antimicrobialdressings is an effective methodology for preventing woundinfection and subsequently accelerating the healing process[42]. Concentration-dependent antimicrobial activity wasdetected for the dressing membranes. The XSi-PU/GO2.5%sample showed moderate antibacterial activity, with effi-ciency in the range of 50–60 % against all of the studiedstrains. By increasing the GO nanoplatelets concentration,both of XSi-PU/GO5% and XSi-PU/GO7.5%samplesshowed the almost complete killing activity for the eval-uated microorganisms. The recorded results were in accor-dance with recent findings regarding antibacterial [21] andantifungal [43] activities of GMs. A three-stage mechanismwas proposed for antimicrobial action of GMs, whichincludes initial cell deposition on GMs, membrane stressbrought on by direct contact with sharp nanosheets, and theconsequent superoxide anion-independent oxidation [22]. Itis more probable that for GO containing dressings, theincorporated GO nanosheets migrated to the surface ofdressing membranes served as “cutters” to disrupt anddamage bacteria membranes. This phenomenon led to theloss of membrane integrity and releasing of intracellularcontents, and eventually microbial cells death. It seems, dueto the low electrical conductivity of the prepared GO con-taining wound dressings (2× 10−7 to 1× 10−5 S cm−1) thesecond possible mechanism for antimicrobial activity of GOcontaining membrane i.e. oxidative stress mediated by GOthrough reactive oxygen species-independent oxidativestress, was less probable in our case.
Based on data recorded by cytocompatibility and anti-microbial assays, the sample XSi-PU/GO5% with optimumphysicochemical, mechanical and biological properties wasselected for the in vivo assay.
4.4 Evaluation of wound healing under in vivo condition
In vivo evaluation of the prepared dressing was performedon Wistar rat as an animal model (Fig. 3). Acceleratedwound closure and better healing of wound dressed withXSi-PU/GO5% membrane were attributed to the favourablemoist and warm environment over the wounded tissue, aswell as maintaining a hygiene environment over woundedtissue due to the antimicrobial activity of this sample [44].
The results extracted from Fig. 4 showed promotedwound healing and higher quality of generated new skin forwound covered with GO containing wound dressing. Pre-vious studies demonstrated that the re-construction of the
75 Page 12 of 14 J Mater Sci: Mater Med (2017) 28:75

epithelium and dermis, including derma papillae and hairfollicles, are associated with the formation of blood vessels[44–46]. Therefore, enhanced epithelization of woundedtissue treated with XSi-PU/GO5% membrane can beattributed to the presence of additional blood vessels,however, secondary structures of skin like dermapapillae and hair follicles are yet to be developed at thistime period.
Higher vascularization and complete re-epithelializationof wounds covered with XSi-PU/GO5% membrane wereattributed to enhanced migration of epithelial cells resultingfrom the maintenance of the moist environment at thewounds site [47, 48]. Collagen is an integral component ofskin and plays a crucial role in the reconstruction of thedermis at the wound site and plays a pivotal role in main-taining skin structure [49–51]. Parallel alignment and highermaturation level of collagen were detected for MT stainedsection of wounds covered with XSi-PU/GO5%.
The in vivo test results revealed that the XSi-PU/GO5%dressing could encourage healing process in terms ofincreased rate of wound closure, collagen deposition, andre-epithelization. In addition to providing optimum moistenvironment over the damaged tissue, the enhanced healingefficacy of XSi-PU/GO5% dressing could be related to thepromising antimicrobial activity of this sample. This resultis in accordance with the previous report about the appli-cation of antimicrobial dressings. In fact, the reduction inthe number of pathogenic microorganisms and conse-quently, reduction of the inflammatory response at woundsite can promote the healing process.
5 Conclusion
People may die due to severe infection, improper protectionof damaged tissue from external mechanical stress and mostlikely due to dehydration of the wounded skin. GO nano-platelets as an antimicrobial and reinforcing agent wereintroduced into the backbone of novel dressing membranescomposed of a polyurethane/siloxane network. DMA andXRD data revealed the proper incorporation and distributionof GO nanoplatelets throughout the matrix. Very goodtensile strength and flexibility of the dressing after incor-poration of a proper amount of GO at both dried andhydrated states confirmed the ability of dressings to protectdamaged tissue from external forces. The balanced EWAand WVTR of dressings enabled preservation of suitablemoist environment over wounds with the low to moderateexudates formation. The GO nanoplatelets incorporateddressings could successfully kill bacterial and fungal strainswithout showing adverse effects on growth and proliferationof dermal fibroblast cells. In vivo assay on rat model con-firmed that the designed GO containing dressing could
effectively stimulate wound healing process and remodelingof newly generated skin tissue.
Conflict of interest The authors declare that they have no competinginterests.
References
1. Bowler PG, Duerden BI, Armstrong DG. Wound microbiologyand associated approaches to wound management. Clin MicrobiolRev. 2001;14:244–69.
2. Han S-K. Innovations and advances in wound healing. In: Seung-Kyu Han, editor. Infection, debridement, and biofilm. Berlin:Springer; 2016. P. 151–82.
3. Boateng J, Catanzano O. Advanced therapeutic dressings foreffective wound healing—a review. J Pharm Sci.2015;104:3653–80.
4. Abdali Z, Yeganeh H, Solouk A, Gharibi R, Sorayya M. Ther-moresponsive antimicrobial wound dressings via simultaneousthiol-ene polymerization and in situ generation of silver nano-particles. RSC Adv. 2015;5:66024–36.
5. Ignatova М, Rashkov I, Manolova N. Drug-loaded electrospunmaterials in wound-dressing applications and in local cancertreatment. Expert Opin Drug Deliv. 2013;10:469–83.
6. Tian J, Wong KKY, Ho CM, Lok CN, Yu WY, Che CM, et al.Topical delivery of silver nanoparticles promotes wound healing.ChemMedChem. 2007;2:129–36.
7. Sahraro M, Yeganeh H, Sorayya M. Guanidine hydrochlorideembedded polyurethanes as antimicrobial and absorptive wounddressing membranes with promising cytocompatibility. Mater SciEng C. 2016;59:1025–37.
8. Yari A, Yeganeh H, Bakhshi H, Gharibi R. Preparation andcharacterization of novel antibacterial castor oil-based poly-urethane membranes for wound dressing application. J BiomedMater Res Part A. 2014;102:84–96.
9. Yari A, Yeganeh H, Bakhshi H. Synthesis and evaluation of novelabsorptive and antibacterial polyurethane membranes as wounddressing. J Mater Sci Mater Med. 2012;23:2187–202.
10. Gharibi R, Yeganeh H, Rezapour-Lactoee A, Hassan ZM. Sti-mulation of wound healing by electroactive, antibacterial, andantioxidant polyurethane/siloxane dressing membranes: in vitroand in vivo evaluations. ACS Appl Mater Interfaces.2015;7:24296–311.
11. Gharibi R, Yeganeh H, Gholami H, Hassan ZM. Aniline tetramerembedded polyurethane/siloxane membranes and their corre-sponding nanosilver composites as intelligent wound dressingmaterials. RSC Adv. 2014;4:62046–60.
12. Sarhan WA, Azzazy HME, El-Sherbiny IM. Honey/chitosannanofiber wound dressing enriched with Allium sativum andCleome droserifolia : enhanced antimicrobial and wound healingactivity. ACS Appl Mater Interfaces. 2016;8:6379–90.
13. Singh AV, Aditi AS, Gade WN, Vats T, Lenardi C, Milani P, et al.Nanomaterials: new generation therapeutics in wound healing andtissue repair. Curr Nanosci. 2010;6:577–86.
14. Kumar PTS, Lakshmanan V-K, Anilkumar TV, Ramya C, ReshmiP, Unnikrishnan AG, et al. Flexible and microporous chitosanhydrogel/nano ZnO composite bandages for wound dressing:in vitro and in vivo evaluation. ACS Appl Mater Interfaces.2012;4:2618–29.
15. Cai N, Li C, Han C, Luo X, Shen L, Xue Y, et al. Tailoringmechanical and antibacterial properties of chitosan/gelatin nano-fiber membranes with Fe3O4 nanoparticles for potential wounddressing application. Appl Surf Sci. 2016;369:492–500.
J Mater Sci: Mater Med (2017) 28:75 Page 13 of 14 75

16. Lin Y-H, Hsu W-S, Chung W-Y, Ko T-H, Lin J-H. Evaluation ofvarious silver-containing dressing on infected excision woundhealing study. J Mater Sci Mater Med. 2014;25:1375–86.
17. Borkow G, Okon-Levy N, Gabbay J. Copper oxide impregnatedwound dressing: biocidal and safety studies. Wounds.2010;22:301–10.
18. Zhang B, Wang Y, Zhai G. Biomedical applications of thegraphene-based materials. Mater Sci Eng C. 2016;61:953–64.
19. Chung C, Kim Y, Shin D, Ryoo S-R, Hong BH, Min D. Bio-medical applications of graphene and graphene oxide. Acc ChemRes. 2013;46:2211–24.
20. Pinto AM, Gonçalves IC, Magalhães FD. Graphene-based mate-rials biocompatibility: a review. Colloids Surf B Biointerfaces.2013;111:188–202.
21. Ji H, Sun H, Qu X. Antibacterial applications of graphene-basednanomaterials: recent achievements and challenges. Adv DrugDeliv Rev. 2016;105B:176–89.
22. Liu S, Zeng TH, Hofmann M, Burcombe E, Wei J, Jiang R, et al.Antibacterial activity of graphite, graphite oxide, graphene oxide,and reduced graphene oxide: membrane and oxidative stress. ACSNano. 2011;5:6971–80.
23. Jastrzębska AM, Kurtycz P, Olszyna AR. Recent advances ingraphene family materials toxicity investigations. J Nanopart Res.2012;14:1320.
24. Akhavan O, Ghaderi E. Toxicity of graphene and graphene oxidenanowalls against bacteria. ACS Nano. 2010;4:5731–6.
25. Deepachitra R, Ramnath V, Sastry TP. Graphene oxide incorpo-rated collagen–fibrin biofilm as a wound dressing material. RSCAdv. 2014;4:62717–27.
26. Shahnawaz Khan M, Abdelhamid HN, Wu H-F. Near infrared(NIR) laser mediated surface activation of graphene oxide nano-flakes for efficient antibacterial, antifungal and wound healingtreatment. Colloids Surf B Biointerfaces. 2015;127:281–91.
27. Madhavan AA, Mohandas A, Licciulli A, Sanosh KP, Praveen P,Jayakumar R, et al. Electrospun continuous nanofibers based on aTiO2–ZnO–graphene composite. RSC Adv. 2013;3:25312–6.
28. Liu Y, Park M, Shin HK, Pant B, Choi J, Park YW, et al. Facilepreparation and characterization of poly(vinyl alcohol)/chitosan/graphene oxide biocomposite nanofibers. J Ind Eng Chem.2014;20:4415–20.
29. Lu B, Li T, Zhao H, Li X, Gao C, Zhang S, et al. Graphene-basedcomposite materials beneficial to wound healing. Nanoscale.2012;4:2978–82.
30. He Y, Zhang N, Gong Q, Qiu H, Wang W, Liu Y, et al. Alginate/graphene oxide fibers with enhanced mechanical strength preparedby wet spinning. Carbohydr Polym. 2012;88:1100–8.
31. Fan Z, Liu B, Wang J, Zhang S, Lin Q, Gong P, et al. A novelwound dressing based on Ag/graphene polymer hydrogel: effec-tively kill bacteria and accelerate wound healing. Adv FunctMater. 2014;24:3933–43.
32. Sun H, Gao N, Dong K, Ren J, Qu X. Graphene quantum dots-band-aids used for wound disinfection. ACS Nano.2014;8:6202–10.
33. Rezapour-Lactoee A, Yeganeh H, Ostad SN, Gharibi R, MazaheriZ, Ai J. Thermoresponsive polyurethane/siloxane membrane forwound dressing and cell sheet transplantation: in-vitro and in-vivostudies. Mater Sci Eng C. 2016;69:804–14.
34. Field CK, Kerstein MD. Overview of wound healing in a moistenvironment. Am J Surg. 1994;167:S2–6.
35. Xu R, Xia H, He W, Li Z, Zhao J, Liu B, et al. Controlled watervapor transmission rate promotes wound-healing via wound re-epithelialization and contraction enhancement. Sci Rep.2016;6:24596.
36. Tamada Y, Ikada Y. Effect of preadsorbed proteins on celladhesion to polymer surfaces. J Colloid Interface Sci.1993;155:334–9.
37. Liao K-H, Qian Y, Macosko CW. Ultralow percolation graphene/polyurethane acrylate nanocomposites. Polymer (Guildf).2012;53:3756–61.
38. Tandon GP, Weng GJ. The effect of aspect ratio of inclusions onthe elastic properties of unidirectionally aligned composites.Polym Compos. 1984;5:327–33.
39. Zaman HU, Islam JMM, Khan MA, Khan RA. Physico-mechanical properties of wound dressing material and its biome-dical application. J Mech Behav Biomed Mater. 2011;4:1369–75.
40. Pant HR, Pokharel P, Joshi MK, Adhikari S, Kim HJ, Park CH,et al. Processing and characterization of electrospun grapheneoxide/polyurethane composite nanofibers for stent coating. ChemEng J. 2015;270:336–42.
41. Ambrogi V, Donnadio A, Pietrella D, Latterini L, Proietti FA,Marmottini F, et al. Chitosan films containing mesoporous SBA-15 supported silver nanoparticles for wound dressing. J MaterChem B. 2014;2:6054.
42. Qin Y. Antimicrobial dressings for the management of woundinfection. Med Text Mater. 2016;11:145–60.
43. Sawangphruk M, Srimuk P, Chiochan P, Sangsri T, SiwayaprahmP. Synthesis and antifungal activity of reduced graphene oxidenanosheets. Carbon N Y. 2012;50:5156–61.
44. Li J, Zhai D, Lv F, Yu Q, Ma H, Yin J, et al. Preparation ofcopper-containing bioactive glass/eggshell membrane nano-composites for improving angiogenesis, antibacterial activity andwound healing. Acta Biomater. 2016;36:254–66.
45. Heller M, Frerick-Ochs EV, Bauer H-K, Schiegnitz E, Flesch D,Brieger J, et al. Tissue engineered pre-vascularized buccal mucosaequivalents utilizing a primary triculture of epithelial cells,endothelial cells and fibroblasts. Biomaterials. 2016;77:207–15.
46. Shen Y-I, Cho H, Papa AE, Burke JA, Chan XY, Duh EJ, et al.Engineered human vascularized constructs accelerate diabeticwound healing. Biomaterials. 2016;102:107–19.
47. Lin Y-J, Lee G-H, Chou C-W, Chen Y-P, Wu T-H, Lin H-R.Stimulation of wound healing by PU/hydrogel composites con-taining fibroblast growth factor-2. J Mater Chem B.2015;3:1931–41.
48. Jhong JF, Venault A, Hou CC, Chen SH, Wei TC, Zheng J, et al.Surface zwitterionization of expanded poly(tetrafluoroethylene)membranes via atmospheric plasma-induced polymerization forenhanced skin wound healing. ACS Appl Mater Interfaces.2013;5:6732–42.
49. Ruszczak Z. Effect of collagen matrices on dermal wound healing.Adv Drug Deliv Rev. 2003;55:1595–611.
50. Wang X, Wu P, Hu X, You C, Guo R, Shi H, et al. Polyurethanemembrane/knitted mesh-reinforced collagen–chitosan bilayer der-mal substitute for the repair of full-thickness skin defects via a two-step procedure. J Mech Behav Biomed Mater. 2016;56:120–33.
51. Demircan M, Cicek T, Yetis MI. Preliminary results in single-stepwound closure procedure of full-thickness facial burns in childrenby using the collagen–elastin matrix and review of pediatric facialburns. Burns. 2015;41:1268–74.
75 Page 14 of 14 J Mater Sci: Mater Med (2017) 28:75