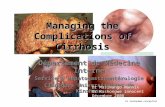
Cirrhosis and complications
description
Transcript of Cirrhosis and complications

Cirrhosis and complications
Cengiz Pata
Gastroenterology Department Yeditepe University

Overview
1) Criteria for Referral for Transplantation
2) Varices3) Ascites/TIPS4) S.B.P.5) Encephalopathy6) Hepatorenal Syndrome7) Hepatocellular Carcinoma

Etiology
• Enfections (HBV, HCV, HDV, HGV)• Hereditary disease (Wilson, Hemokromatozis, Alfa-1
antitripsin,tyrosinemia)• Toksic (alchol,drugs(Mtx)• İmmünologic (OİH)• Vasculer (corpulmonare, Budd Chiarry, Portal ven
trombosis)• Bilier Disease (PBS, Cystic
Fibrosis,Sarcoidosis,PSK,PFIK,SBS)• Malnutrision , Bypass surgery• İndian Child Age Disease• NAFLD

Reasons for Liver Transplantation: U.S.
Etiology % Disease from Hepatitis C 40 IDU 65%, BT 5%, others Alcohol 30 alcoholism PBC/PSC 10 congenital Hemochr <5 genetic HBV 5 vertical/horizontal
Biliary atresia 30 congenital Metabolic d/o 20 congenital

Fibrosis Progression: Hepatitis C
Slide courtesy of Bennett, MD.
CirrhosisSevere Fibrosis
Normal Liver Mild fibrosis

CIRRHOTIC LIVERCIRRHOTIC LIVER

CIRRHOTIC LIVERCIRRHOTIC LIVER

How do we know if a patient has cirrhosis/ portal
hypertension ?• Liver biopsy: Stage IV scarring• CT scan: hypertrophied L lobe, nodular
contour, enlarged portal vein, splenomegaly, varices, ascites
• Labs: low platelet count, elevated bilirubin, prolonged INR
• Physical exam: spider angiomata, jaundice, splenomegaly, ascites, leg edema

Timing of referral for consideration of liver
transplant ? 1 point 2 points 3 points
Albumin (g/l) >3.5 2.8-3.5 <2.8
Ascites None Slight Moderate
Bilirubin (mg/dl) <2 2-3 >3
Encephalopathy None Mild-Mod Severe
Prothrombin/INR 1-4 s/1.7
4-6 s/1.7-2.2
>6 s/>2.2
A: 5-6, B: 7-9, C: 10 or more
Modification for Bilirubin in PBC/PSC: 1-4, 4-10, >10

Timing of referral for consideration of liver transplant ?
• Since February 2002, listing for transplantation is on the basis of a MELD score and a CPT score
• MELD (Model for End-Stage Liver Disease): developed at Mayo Clinic as a separate “liver disease severity index”
• MELD: 0.38xloge(bilirubin, mg/dl) + 1.12xloge(INR) + 0.96 xloge(creatinine, mg/dl) + 0.64x etiology
Website: www.unos.org

Implication for Transplant
• Many of complications of cirrhosis were formerly considered reasons to “increase a patient’s status,” specifically:
1) Refractory variceal bleeding 2) Refractory hepatorenal syndrome 3) Refractory hepatic
encephalopathy- were accepted as reasons to make
patients on the list for transplant “2A,” and give them higher priority

Variceal Bleed
Monitor Liver FunctionPT, Alb, Bili q 3-6 months
Hepatoma SurveillanceU/S, AFP q 6 months
Varices Surveillance
Compensated Decompensated
Encephalopathy
Treatment Recommendations- Cirrhosis
Figure 1. Treatment Flow Sheet for Patients with Cirrhosis
SBP Ascites Hepatorenal Synd.
(Garcia-Tsao G, 2003)
Vaccination- in HCV,against HAV, HBV

Variability in Natural History of Cirrhosis
• Natural history is clearly variable based on:
- ongoing alcohol consumption, leading to acute exacerbations in portal pressures, particularly increasing risk for variceal hemorrhage
- relation between cirrhosis etiology and HCC (HBV>HCV>?NASH)

Morbidity and Mortality in Compensated Cirrhosis Type C: A Retrospective Follow-up Study of
384 Patients
0
5
10
15
20
25
30
35
HCC Varix Bl >1 compl
Complication
Fattovich G et al, Gastroenterology 1997;112:463
Ascites Enc/J
Mean follow-up:5 years

Morbidity and Mortality in Compensated Cirrhosis Type C: A Retrospective Follow-
up Study of 384 Patients
• 26% of patients decompensated during follow-up (8% HCC, 18% other)
• Odds of decompensation: 12% at 3 years, 18% at 5 years, 29% at 10 years
• Probability of survival after decompensation: 50% at 5 years
• Death: 51 (13%): roughly 1/3 HCC, 1/3 liver failure, 1/3 unrelated to cirrhosis
Fattovich G et al, Gastroenterology 1997;112:463

Effect of Hepatitis B and C Virus Infections on the Natural History of Compensated
Cirrhosis: A Cohort Study of 297 Patients
0
5
10
15
20
25
HCC Ascites Varix Bl Enceph/J >1 Compl
HCV+:136HBV+:161
Fattovich G et al, Am J Gastro 2002;97:2886
Median f/u:6.5 years

Effect of Hepatitis B and C Virus Infections on the Natural History of Compensated
Cirrhosis: A Cohort Study of 297 Patients
• HCV: 53% decompensated (17% HCC, 36% other) HBV: 34% decompensated (14% HCC, 20% other)• Probability of 5-year survival after decompensation:
HBV 28%, HCV 47%• Death or liver transplant: 70 (22% of HBV, 26% of
HCV)
Fattovich G et al, Am J Gastro 2002;97:2886

Gines, Hepatology 1987.
PROBABILITY OF DEVELOPING DECOMPENSATED CIRRHOSIS
257 patients with compensated cirrhosis
time in months
number being followed

Cirrhosis Natural History Studies Summary
• No decompensation: 80% 10-year survival• Decompensation is variable, imperfectly
predicted. Portal HTN vs. synthetic dysfunction
• HCC, ascites: the 2 principal forms of decompensation
• Risk of decompensation: roughly 4-5% per year in a patient with Child’s A cirrhosis
• After decompensation, probability of 5-yr survival without transplant: 35-50%

Time to disease progressionDB treatment and off-treatment
follow-upPercentage with
disease progression
Time to disease progression (months)
Placebo (n=215) ITT populationLamivudine (n=436) p=0.001
Lamivudine
Placebo
P=0.001
21%
9%

Risks of Complications of Cirrhosis
Cirrhosis
VaricealBleeding
HCC
Ascites
Encephalopathy
adapted from Bennett WG et al, Ann Intern Med 1997;127:855
0.4%
1.5%
2.5%
1.1%
percent per year
Death
Liver Transplant
11%
?20+%
?30+%

Median Survival Times in Cirrhosis
• Compensated Cirrhosis 9 yrs• Decompensated Cirrhosis 1.6 yrs
– Jaundice– Encephalopathy– Ascites– Variceal hemorrhage
• SBP 9 mos• HRS type II 6 mos• HRS type I 2 wks

Bleeding VaricesBleeding Varices

Varices-Background
• Management of acute or acutely-bleeding varices is accepted: a) IV octreotide
b) band ligation > sclerotherapy for esophageal varices, TIPS placement (or attempts at glue injection at some sites) for acutely-bleeding gastric varices. 7 days of antibiotics recommended
• Controversies: 1) Primary prophylaxis 2) Secondary prophylaxis

Primary Prophylaxis- Varices
• 15-25% of unselected cirrhotics screened endoscopically will have large or high-risk varices
• Mortality of first variceal hemorrhage remains high, 20-35%
D’Amico G et al, Hepatology 1995;22:332-54
• Fewer studies on prevalence of gastric varices in unselected cirrhotics; 4% ?
Sarin S et al, Hepatology 1992;16:1343-49

Prevention of FIRST Variceal HemorrhageMeta-Analysis (11 trials)
Control Beta-blocker
Absolute Rate
DifferenceBleeding
Rate 25% 15% -10%
(- 16 to –5)Death Rate
27% 23% -4%(- 9 to 0)
Large Varices
30%(n=411
)
14%(n=400)
-16%(- 24 to –8)
SmallVarices
7%(n=100
)
2%(n=91)
-5%(-11 to 2)
D’Amico et al. Sem Liv Dis 1999

Prediction of Large Varices
• Platelet count, Child-Pugh class independent risk factors for the presence of any varices (plts <90K) and large varices (plts <80K) in 300 cirrhotics without prior bleeding being evaluated for OLT
Zaman A et al, Arch Int Med 2001;161:2564-70

Zaman et al, Arch Int Med 2001
Clinical Feature No varices (n=97)
Small varices (n=109)
Large varices (n=94)
Encephalopathy
34%
47% 54%
Platelets (mean)
129,000 107,000 76,000
Splenomegaly (u/s)
62% 61% 73%
Ascites 44% 53% 63%
Platelet count OR 2.3, p=.001Child-Pugh class OR 2.75, p=.007
Multivariate Predictorsof Large Varices:

Primary Prophylaxis
• Beta-blockers reduce the incidence of first variceal hemorrhage compared to placebo
Poynard T et al., NEJM 1991;324:1532-1538
• Band ligation may be more effective than Propranolol in high risk patients
Sarin S et al, NEJM 1999;340:988-93

Primary Prophylaxis of Varices: An algorithm
• It is reasonable to perform endoscopic screening in all cirrhotics (stable, willing to be tx’d); it should likely be performed in all Child’s C cirrhotics
Beta blockade (Propranolol, Nadolol, goal HR 55-60) is the preferred approach; band ligation is an alternative for high risk varices or in patients who can’t tolerate Propranolol
- not as many data in gastric varices nor portal gastropathy, but prophylaxis may be similar

Secondary Prophylaxis of Varices
• Variceal hemorrhage has a 2-year recurrence rate of 80%
• Once acute bleeding has resolved, two large trials have found that beta-blockade and band ligation have similar efficacy in controlling rebleeding
Minyana J et al, Hepatology 1999;30:215A Patch D et al, J Hepatology 2000;32:34

Secondary Prophylaxis of Varices
• Banding sessions are typically repeated at 7-14-day intervals until obliteration, typically 2-4 sessions
• TIPS vs endoscopic tx: rebleeding less with TIPS, but worse encephalopathy, no change in mortality
Papatheodoridis GV, Hepatology 1999;30:612-22
Beta-blockers or banding are first-line


Hepatic encephalopathy
• GIS bleeding• Enfection• higher protein • diuresis• constipation• Elektrolit inbalance• Dehidratation• Sedative• Hepatik injury• Portasistemic shunt


Hepatic encephalopathy
• Liver failure, failure of CNS
• 1 year survive %40
• NH3, Glutamine,katekolamine, serotonine,GABA

Stages of Hepatic encephalopathy
0-1 : psychometric tests slow1 : abnormal sleep, dyscordination2 : lethargy, ataxia, disarthria,behavirol
dysinhibition, asterix, poor tests3 :confusion, delirium, semi stupor, incontinence,
disorientation, amnesia, rigidity, paranoia, abnormal reflex, nistagmus, babinski
4 : coma, no cognition, no behavior, decortica or decerebrate, dilated pupils

Hepatic encephalopathy
Treatment• General support
• Treatment of etiologic factor
• Medical : Lactulose, antibiotic (neomycin,metronidazole)
Flumazenil
• Transplantation

HRS
• impaired renal function• İmpaired arteriel circulation• Renal vazoconstruction• GFR↓• No pathologic lesion• 1 mounths survival %95• %7-15• Type 1:weeks, agrrevation important ( diuretic,
parasenthesis, SBP..)• Type 2 : mounths, better prognose

Hepatorenal Syndrome
• 2 types: Type I: rapid development of renal dysfunction (Cr rising to >2.5mg/dl in 2 weeks): median survival 2 weeks
Type II: slower rise, Cr >1.5mg/dl Management: 1) Ensure Diagnosis 2) Liver Transplantation

HRS• Major CriteriaGFR low (cre1.5mg/dl↑ or Cre clirence 40↓)No shock, nefrotocsic drug, enfection or loss of fluidGood function after stoping diuretic and 1,5 lt saline No paranchymal disease or nefrolithiasis on US500mg/d↓/day proteinuri
• Minor CriteriaUrine volume 500↓Urine Na 10 mEg/L↓Higher urine osmolarite than plasmaSerum Na 130 mEg/L↓50 red cell↓ urine

HRS
• Dopamine
• Mizoprostole
• Vazopressine (Orlipressin,terlipressin)
• TIPS
• MARS
• Transplantation

Uriz J Hepatol 2000;33:43-18
TERLIPRESSIN+ ALBUMIN IN HRS

U Heemann et al. Hepatology 2002; 36: 949-958
EXTRACORPOREAL ALBUMIN DIALYSIS MARS

Natural History of Cirrhosis in 2005: Altered by What
We Do• More aggressive screening, for
varices, HCC will mean problems are identified earlier
• Ablative therapies for HCC• Obliteration of varices/ beta-
blockade• TIPS• Liver Transplantation