Chronic Migraine with Medication Overuse: Clinical Pattern ... · It represents the third most...
Transcript of Chronic Migraine with Medication Overuse: Clinical Pattern ... · It represents the third most...

MEDICINE
Chronic Migraine with Medication Overuse: Clinical Patternand Evolution from a Retrospective Cohort in Seville, Spain
María del Valle López Martínez1 & Javier Pareja Román2& María Dolores Jiménez Hernández1 &
Ceferino Maestu Unturbe3& María del Carmen Ramírez-Castillejo2
Accepted: 17 July 2020# Springer Nature Switzerland AG 2020
AbstractChronic migraine (CM) with medication overuse (MO) develops in patients with a pre-existing primary headache after a regularoveruse of symptomatic medication. In these patients, headache crisis may occur together with other painful pathologies whichcan increase the frequency and intensity of the pain episodes. Such comorbidities need to be assessed as they influence the clinicalevolution of the patients. A cohort of 102 patients (89 women and 13 men) with a diagnosis of chronic migraine (CM) withmedication overuse (MO) was retrospectively analysed. Patients enrolled in the study were actively followed up 23months in theNeurology Service of the University Hospital Virgen del Rocío in Seville, Spain. We observed that most of the patients overusedmultiple symptomatic drugs (34.3%) and NSAIDs (26.5%). In this cohort, the most effective treatments were topiramate and thecombination of multiple prophylactic drugs with an effectiveness of 41.6% and 53.8%, respectively, at the end of the study. Weobserved the ratio of patients reducing their headache crisis was significantly higher among patients abandoning their medicationoveruse. Detoxification, or withdrawal of medication overuse, is linked to the reduction of the frequency and intensity of 50% ormore of the headache crisis in these patients.
Keywords Medication overuse . Detoxification . Headache comorbidities . Preventive treatment
Introduction
Chronic migraine (CM) with medication overuse (MO) is themost prevalent chronic headache disorder [1]. It is classified asa secondary headache disorder that develops in some patientswith a pre-existing primary headache as a consequence of aregular overuse of any type of analgesics or any other acute orsymptomatic headache medication. According to the
International Classification of Headache Disorders, chronicmigraine (CM) with medication overuse (MO) is defined asa headache occurring on 15 or more days/month in a patientwith a pre-existing headache disorder with a regular medica-tion overuse for more than three months that does not betteraccount for any other diagnosis [2].
It represents the third most prevalent headache conditionoverall, after migraine and tension-type headache. Chronicmigraine with medication overuse has an estimated preva-lence in Europe of 1–2%, and it rises up to 7% in some coun-tries [1, 3]. This condition is more frequent among women(2.6%) than men (0.19%) as a close relation between estro-gens and other primary headache disorders, like migraine, hasbeen already stablished [4]. CM with MO appears at olderages than primary headaches, ranging the average age of thesepatients between 40 and 45 years. These patients usuallycourse with a previous history of headache of 20 to 25 yearsof evolution, in addition to 7 to 10 years of medication abuse.
A history of primary headache is a necessary condition todevelop CM with MO as analgesics overuse alone has notbeen related to this chronic headache condition. Abuse ofanalgesics in patients with musculoskeletal pain or rheumato-logic processes does not lead to a higher prevalence of CM
This article is part of the Topical Collection onMedicine
* María del Valle López Martí[email protected]
* Javier Pareja Román
1 Neurology Service, University Hospital Virgen del Rocío,Seville, Spain
2 Health Science Technologies Research Group, Biotechnology-BVETSIAAB Department, Universidad Politécnica de Madrid,Madrid, Spain
3 Centro de Tecnología Biomédica, Universidad Politécnica deMadrid, Madrid, Spain
https://doi.org/10.1007/s42399-020-00424-8
/ Published online: 22 July 2020
SN Comprehensive Clinical Medicine (2020) 2:1514–1525

with MO [5], but these patients may develop CM with MO ifthey also have a primary headache. Thus, analgesic overusecontributes to the chronification of previous headache epi-sodes. Although medication used in the symptomatic treat-ment of headache can contribute to CM with MO develop-ment, the precise mechanism remains unclear [6]. The contin-ued use of drugs, in patients with a primary headache, leads toa phenomenon of tolerance and dependence of the drug,whereas its suppression causes a rebound headache as with-drawal syndrome. There are multiple factors that seem to playan important role in the pathophysiology of CM with MO,such as central sensitization [7], genetic predisposition [8],hypothalamic stress response [9] or behavioural and nutrition-al factors. CMwithMO can be considered a clinical conditionin the verge of drug addiction and chronic pain disorder. Thehigh uptake of analgesics increases, paradoxically, the fre-quency of pain episodes. Thus, episodic primary headacheevolves gradually towards a chronic secondary headache.
Headaches often course alongside other pain-related pa-thologies that may enhance the frequency and grade of theheadache episodes. These comorbidities are particularly im-portant in CM with MO patients as they exhibit them morefrequently [10, 11]. Such associated pathologies include psy-chiatric comorbidities, substance overuse and dependence be-haviours, sleep alterations and other painful processes. CMwith MO is strongly influenced by the presence of anxiety,depression and other neuropsychological comorbidities aswell as by a low socio-economic status and educational level[12, 13]. Therefore, most CM with MO cases need an intensepsychological evaluation. Psychiatric comorbidity is more fre-quent in patients suffering from chronic migraine (especiallythose with medication abuse) than in patients with episodicmigraine [14]. Compared to migraine, CM with MO patientshave an increased risk of suffering mood disorders, and disor-ders associated with the use of psychoactive substances. CMwith MO is a condition that worsens with symptomatic med-ication overuse, and so headaches become increasingly fre-quent [15, 16]. The presence of psychiatric alterations andthe increased risk of substance abuse disorders seem to bemore prevalent in CM with MO than in migraine patients[17]. In fact, two thirds of CMwithMOpatients are dependenton headache medication [18]. Not surprisingly, headaches areusually related to sleep alterations. The neuronal pathwayscontrolling sleep and pain are anatomically and physiological-ly cross-linked. Both neuronal systems are located in thebrainstem, hypothalamus and basal brain. Consequently, dys-functions in the neuronal networks of the brainstem (especial-ly in the serotonergic nuclei) or the hypothalamus can explainthose frequent headaches that start in the rapid eye movement(REM) phase of sleep affecting biologically predisposed peo-ple. Among the many sleep disorders described by theInternational Classification of Sleep Disorders (ICSD), insom-nia, obstructive sleep apnoea, periodic movements of the
extremities and fibrositis have been related to headaches[19]. Additionally, some painful processes, such as musculo-skeletal pain or rheumatologic disease, appear as other head-ache comorbidities at younger ages. These multiple pains leadto worse prognosis of headache [20]. The reason for thesecomorbidities is still not well understood. A unidirectionalcausality has been suggested though as well as shared endog-enous, such as genetic factors, and/or exogenous factors inboth processes. The existence of common risk factors mayfavour the appearance and development of both pathologies[21].
The most frequent drugs prescribed for headache disordersinclude non-steroidal anti-inflammatory drugs (NSAID), acombination of analgesics, triptans and opioids. These drugshave different mechanisms of action and require different dos-ages and exposure times to induce CMwithMO in susceptiblepatients. Besides, 90% of patients take more than one drug atthe same time, which can speed up the MOH development.Detoxification, which includes withdrawal of overused medi-cation, is the first treatment to be considered. Abrupt interrup-tion of drugs is recommended, especially in the case of er-gotics, triptans and non-opioid analgesic overuse.Medication suppression usually causes rebound headaches,whose intensity and duration vary upon the overused drug.In order to prevent rebound headache, the patient can start adescending NSAID treatment. Some patients may requiresymptomatic medication, such as benzodiazepines if anxietyappears. The use of amitriptyline at a dose of 10–75 mg canimprove the symptoms after withdrawal of medication [22].
In this study, we aim to provide further evidence ofoverused medication withdrawal in these patients. We alsoaim to analyse the relation between CM with MO and differ-ent comorbidities including psychiatric disorders, sleep alter-ations or other painful processes and evaluate the recommend-ed CM with MO treatments.
Materials and Methods
Study Design
This single-centre retrospective study was conducted in theNeurology Service of the University Hospital Virgen delRocío in Seville (Spain) in 2015. The medical records of pa-tients recruited between April 2010 and June 2015 wereanalysed. The data collection period was 5 years and2 months.
This hospital assists approximately 800,000 inhabitantswhich enabled us to obtain a representative sample of thepopulation in Seville.
Patients were recruited at the time of CM with MO diag-nosis and followed up to assess their evolution. The meanfollow-up period of the patients was 23 months.
1515SN Compr. Clin. Med. (2020) 2:1514–1525

Data from the patients were collected from the checkinginterviews, phone interviews and their clinical records. Everypatient included in the study had been previously informed,and the informed consents were collected.
Participants and Study Population
The participants of the study were recruited from theUniversity Hospital Virgen del Rocío of Seville.
The inclusion criteria of this study were to have been diag-nosed with CM with MO according to the beta version of thethird edition of the International Classification of HeadacheDisorders (ICHD) [23] and to have been actively followed upin the Neurology Service of the University Hospital Virgendel Rocío in Seville and seen patients with information onvariables of interest for this study.
One hundred two patients (89 women and 13 men) wererecruited for meeting the inclusion criteria.
Epidemiological and clinical data of clinical records areanalysed and collected in two checkings:
First Checking (102 Patients)
The first medical review at 4 months (mean value) of thediagnosis is checked. These data are important to know thepatient’s initial response to the therapeutic regimen. Somepatients improve and receive medical discharge, so only 87patients remain under medical follow-up.
Last Checking (87 Patients)
The last medical review at 23 months (mean value) of thediagnosis is reviewed. This is the last review of each patientin his medical history, either because he is discharged wellbecause he is still being followed up but has no further reviewsat the time of our study. It is important to know the data thatinform us of the evolution of the patient throughout his fol-low-up.
In addition, treatment and response data from the follow-upphase are collected from medical records.
Those patients lacking information on any variable of in-terest were excluded from the study. Variables of interest in-cluded those likely to influence the evolution of the disease(epidemiologic data, toxic habits, other pains and pathologies,risk factors and comorbidities, headache-related symptoms,headache-triggering factors, monthly frequency of the crisis,evolution period of the primary headache, symptomatic med-ication overuse type, overuse of benzodiazepines or caffeine,monthly frequency of drug abuse), those favouring the recov-ery of the patient (first preventive treatment prescribed and itseffectiveness, second preventive treatment prescribed and itseffectiveness, third preventive treatment prescribed and itseffectiveness, fourth preventive treatment prescribed and its
effectiveness, naproxen or prednisone descending treatment,crisis reduction of more than 50%) and those likely to worsenthe pathology (crisis and/or medication overuse relapse andmedication overuse suppression).
Statistical Analysis
In this study, we present categorical data as frequency andpercentage, while quantitative data is given as the mean valueplus its standard deviation. Fisher exact test and Pearson chi-square test were used to compare categorical data sets, where-as quantitative data were analysed with an independent-sample t test.
The association between variables was assessed with theirodds ratio or their 95% confidence intervals. Differences wereconsidered statistically significant when the p value < 0,05.The software package SPSS (version 19.0; IBM) was usedfor statistical analysis.
Results
Baseline Characteristics
Data collected from 2010 to 2015 in the University HospitalVirgen del Rocío in Seville were analysed in this retrospectivecohort. A total of 102 patients fulfilled the inclusion criteriaand enrolled as participants of this study in their first checkinginterview at the time of their CMwithMO diagnosis. The lossof follow-up at the time of the second checking interview was14.7%, meaning that 87 participants were successfully follow-ed up until the last checking interview. Of the initial 102participants, 13 (12.7%) were male and 89 (87.3%) female.The average age at the time of enrolment was 44.4 ± 14.21(mean value ± standard deviation) (Table 1).
Clinical records were analysed to look for possible comor-bidities. Thirty-nine (38.2%) patients suffered from musculo-skeletal pathologies, 17 (16.7%) had gastrointestinal patholo-gies and 20 (19.6%) had arterial hypertension. However, themost prevalent comorbidities in this study population werepsychological alterations, present in 50 (49%) patients; insom-nia, present in 43 (42.2%) patients; and other painful pathol-ogies present in 42 (41.2%) participants. Among the psycho-logical alterations, depression accounted for the highest prev-alence, followed by anxiety depressive disorder and anxiety(Table 1).
The most frequent crisis-triggering events observed werestress and menstruation in the female population. Up to 51.7%of the female population claimed that menstruation triggeredtheir crisis, and 19.6% of the total study population relatedtheir crisis to stress. The most frequent pain type during theircrisis was a pulsatile pain, followed by pulsatile and
1516 SN Compr. Clin. Med. (2020) 2:1514–1525

oppressive, and only oppressive. Other repeated symptomsincluded sickness, vomiting, photophobia and phonophobia(Table 1).
Of the patients, 90.2% were treated with a combination ofNSAIDs and triptans and 58.8% were, besides, recommendedfor a descending naproxen treatment. However, only 2.9% ofthe patients were recommended a descending prednisonetreatment. Most of the patients showed overuse of multiplesymptomatic drugs (34.3%), NSAIDs (26.5%) and a combi-nation of analgesics (13.7%). However, only 9.8% overused
caffeine-containing drugs and food. The overuse of benzodi-azepines was observed in 52% of the patients. The mean fre-quency of monthly abuse was 25.7 days (Table 2).
Treatment Effectiveness
A drug treatment is considered effective when the patient re-duces his headache crisis by 50% or more.
After CM with MO diagnosis, patients may undergo dif-ferent treatments. To date, there is no gold standard drug.
Table 1 baseline characteristics of patients
Characteristics Absolute number (%)
DemographicsGender Male 13 (12.7)
Female 89 (87.3)Age (mean ± SD) 44.4 ± 14.21Smokers No 78 (76.5)
< 10 cigarettes/day 4 (3.9)10–20 cigarettes/day 18 (17.6)> 20 cigarettes/day 24 (23.5)
ComorbiditiesMusculoskeletal pathology Yes 39 (38.2)
No 63 (61.8)Gastrointestinal pathology Yes 17 (16.7)
No 85 (83.3)Arterial hypertension Yes 20 (19.6)
No 82 (80.4)Psychological alterations No 52 (51)
Anxiety 10 (9.8)Depression 24 (23.5)Anxiety depressive disorder 13 (12.7)Others 3 (2.9)
Insomnia Yes 43 (42.2)No 59 (57.8)
Other painful pathologies Yes 42 (41.2)No 60 (58.8)
Headache-related symptomsPain type Pulsatile 48 (47.1)
Stinging 8 (7.8)Oppressive 14 (13.7)Pulsatile and oppressive 23 (22.5)Pulsatile and stinging 2 (2)Oppressive and stinging 6 (5.9)Pulsatile, oppressive and stinging 1 (1)
Sickness Yes 74 (72.5)No 28 (27.5)
Vomiting Yes 42 (41.2)No 60 (58.8)
Photophobia Yes 83 (81.4)No 19 (18.6)
Phonophobia Yes 85 (83.3)No 17 (16.7)
Crisis-triggering eventsMenstruation Yes 46 (45.1)
No 43 (42.2)N/A 13 (12.7)
Stress Yes 20 (19.6)No 82 (80.4)
Monthly crisis frequency 24.6 days/month ± 6.38Primary headache evolution 29.2 years ± 12.66
SD standard deviation, N/A non-applicable
1517SN Compr. Clin. Med. (2020) 2:1514–1525

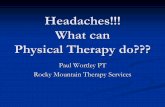
Treatments prescribed in the first and second checking inter-view did not vary much, the combination of prophylacticdrugs being the most administered ones, followed bytopiramate and amitriptyline. After the first checking, 28.4%of the patients reduced their crisis 50% or more. When treat-ment effectiveness was analysed, topiramate yielded the bestresults as 7 out the 13 patients under topiramate treatmentreduced their crisis 50% or more (53.8% effectiveness).Propranolol and the combination of prophylactic drugs hadalso good effectiveness in the first checking, as 40% and36.1% of the patients under propranolol and the combinationof prophylactic drugs respectively reduced their crisis. Theseresults were consistent in the last checking interview in whichthe effectiveness of topiramate, propranolol and the combina-tion of prophylactic drugs was 41.6%, 50% and 53.8% respec-tively (Fig. 1). Other treatments showed a greater difference intheir effectiveness in the first and last checking, because theywere prescribed to very few patients. Seven of our patientsreceive onabotulinumtoxinA (OBT-A) treatment, and we ob-served effectiveness in 80% of them.
We observed an increase in the reduction of 50% or moreof the crisis in the last checking, when 51.1% of the patientshad reduced their crisis. Remarkably, by the time of the lastchecking, 57.5% of the patients had abandoned their medica-tion abuse, while by the time of the first checking, it was only30.4% of the patients.
Suppression of Medication Overuse
Globally, a total of 61 (59.8%) patients suppressed their med-ication overuse, with 53 of them (86.9% of the patientsabandoning medication overuse) reducing 50% or more oftheir crisis (Table 3).
Crisis Reduction of 50% or More
Patients were then stratified depending on whether they re-duced 50% or more of their crisis or not. The only variableassociated with the crisis reduction is the suppression of themedication overuse (Table 4). This association resulted statis-tically significant with a p value below 0.001. There seems tobe also a tiny association between crisis reduction and patientsnot suffering from psychological alterations. Patientsexperimenting a reduction of their crisis had a significantlylower headache evolution time in the last checking with a pvalue below 0.023.We did not observe any further associationbetween the crisis reduction and other demographic or symp-tomatic variables. Globally, a total of 56 (54.9%) of the pa-tients reduced 50% or more of their crisis.
Discussion
CM with MO, as migraine and tension-type headache, has ahigher incidence in females than in males, typically in theirearly forties [24, 25]. In our study population, as much as87.3% of the patients were women and the average age was44 years. There seems to be an association between the reduc-tion of crisis in CM with MO patients and the evolution timeof their headaches.We found that patients reducing their crisis50% or more had had on average a 6-year-shorter headacheevolution time. Although in the first checking this associationwas not statistically significant, that may be because the sizeof the population reducing their crisis by the time of their firstchecking was too low.
CM with MO patients often suffer from other comorbidi-ties such as depression, anxiety, insomnia or other painfulpathologies, which hinders improvement and recovery.Among psychiatric or psychological alterations, mood disor-ders, anxiety and depression are the most common comorbid-ities [24, 26, 27] affecting 49% of the patients in our study.Such pathologies may influence the patient’s adherence to thetreatment as well as medication abuse behaviours. We ob-served, in our study, a higher percentage of patients sufferingfrom any psychological comorbidity that did not reduce theircrisis significantly. But this observation might be explained bythe lower proportion of these patients abandoning medicationoveruse. Although none of these observations resulted statis-tically significant in our study, this hypothesis is supported byother previously published data [24, 28]. Insomnia is also avery important and frequent comorbidity with a prevalencethat ranges in CM with MO patients between 30 and 70%depending on the population [27, 29]. Up to 42.2% of ourstudy population claimed to suffer from insomnia. Not onlyis insomnia an important comorbidity, but it is also a CMwithMO risk factor. CM with MO crisis occurs more frequentlyduring the night, and it is currently not known whether
Table 2 Patients overusing symptomatic drugs
Characteristics Absolut number (%)
Overused drugs Ergotics 1 (1)
Triptans 17 (16.7)
Paracetamol 5 (4.9)
NSAIDs 27 (26.5)
Opioids 3 (2.9)
Combinedanalgesics
14 (13.7)
Multiple drugs 35 (34.3)
Caffeine Yes 10 (9.8)
No 92 (90.2)
Benzodiazepines Yes 53 (52)
No 49 (48)
Monthly abusefrequency
25.7 days/month ± 6.47
1518 SN Compr. Clin. Med. (2020) 2:1514–1525

insomnia can cause or be caused by the headache crisis.However, importantly, we did not find an association betweeninsomnia and the reduction of the crisis or the withdrawal ofmedication overuse in agreement with previously publisheddata [28]. Some epidemiological studies have also identifiedcertain painful pathologies as risk factors, with arthritis andmusculoskeletal pain being the most important ones. At theHead HUNT Study in Norway, adults were asked for anyheadache and musculoskeletal symptom. They found a two-fold increase in the prevalence of musculoskeletal symptomsin the population with headache crisis [30]. In our study,41.2% of the population showed musculoskeletal symptomsas well. The most frequent pathology is low back pain follow-ed by cervical pain and polyarthrosis. However, we did notobserve any statistically significant link between these painfulpathologies and the reduction of the crisis or withdrawal ofmedication.
It is essential to know the group of drugs being overusedfor the study and characterization of CM with MO. Chronic
migraine with medication overuse was firstly described inpatients with a history of migraine and ergot overuse. It was,then, discovered that analgesics also contributed to CM withMO development. That is why, for a long time, both ergoticsand analgesic combinations were considered the drugs respon-sible for the headache crisis [23]. Triptans, which are used as atherapeutic strategy for migraines, have also being linked topre-existing headaches worsening [31]. Triptans have the ca-pacity to induce earlier CM with MO and with lower dosages[32]. In our study, we observed that the therapeutic groups ofdrugs with the greatest overuse were the combination of mul-tiple symptomatic drugs and NSAIDs. Similar patterns ofmedication abuse have been reported in other countries [33].Nevertheless, patterns differ depending on the geographicallocation [17].
Today, there is no gold standard treatment for CM withMO. Some authors suggest not to start prophylactic treatmentuntil the effect of the detoxification of the drug abuse showsup, whereas others suggest to start both strategies
Fig. 1 CM with MO election treatment and effectiveness. a Absolutenumbers of patients treated with each CM with MO treatment in thefirst (4 months) and in the last (19 months) checking interview. bEffectiveness of each CM with MO treatment both in the first interview
(4 months) and in the last one (19 months). Effectiveness has been cal-culated as the percentage of patients reducing 50% or more of their crisisin each CM with MO treatment group
1519SN Compr. Clin. Med. (2020) 2:1514–1525

simultaneously [7, 34]. In these studies, a greater reduction inthe rate of headaches was seen in patients who received pro-phylactic medication from the beginning. Most of the patientsin our study received one or several prophylactic treatmentsfrom the beginning plus symptomatic treatment to alleviatethe pain. In the first follow-up checking of our study, thecombination of prophylactic drugs yielded the highest effec-tiveness followed by topiramate and amitriptyline. These re-sults were consistent in the last follow-up checking, when thecombination of prophylactic drugs yielded again the highesteffectiveness. Other studies have also found a better effective-ness of the combination of prophylactic drugs when comparedto a simple prophylactic treatment in reducing the frequencyof crisis [35]. However, it is, as we have observed in thisstudy, the suppression of the medication abuse or detoxifica-tion that is the best approach towards reducing 50% ormore ofthe patient’s crisis as was also observed in prior publishedstudies [36]. Detoxification can, therefore, be proposed asthe main improvement condition for these patients. The resultsof this study look promising because they point to detoxifica-tion of medication overuse as the principal success strategy.However, this should be taken cautiously as clinical relevance
remains unknown. Further studies are needed to confirm ourfindings.
Many are the limitations of this study. Firstly, it is a retro-spective study that includes only part of the population livingin Seville as possible study participants, being likely biased.Secondly, it is also an observational study that lacks controlover the patient’s treatment strategy, so the results are merelydescriptive. And thirdly, as it is a hospital-based single-centrestudy, the sample size might not be large enough to provesome variable associations.
New Prophylactic Treatments: OnabotulinumtoxinA(OBT-A) and Anti-CGRP Monoclonal Antibodies
It is interesting to introduce new therapeutic alternatives forthose patients when the prophylactic treatment is not effective.In this sense, OBT-A injection is an important therapeutictool. Furthermore, phase II and III clinical trials with anti-CGRP monoclonal antibodies show positive results as pro-phylactic treatment in patients with chronic migraine. For abetter use of prophylactic therapy, it would be advisable toidentify patients with CM and offer them prophylactic
Table 3 Baseline characteristics stratified by suppression of medication abuse
Characteristics First checking (4 months) Last checking (19 months)
Medication abusesuppression
No medication abusesuppression
p value Medication abusesuppression
No medication abusesuppression
pvalue
Gender Male 3 10 0.749 6 7 0.371Female 28 61 44 30
Age (mean ± SD) 41.9 ± 15.17 45.5 ± 13.74 0.245 44.7 ± 14.45 45.9 ± 13.83 0.699
Symptomaticmedication
NSAID 9 18 0.73* 15 8 0.64*
Paracetamol 1 4 1.62* 2 2 1.37*
Triptans 7 10 0.29* 7 7 1.43*
Ergotics 0 1 1* 1 0 –*
Opioids 2 1 0.218* 0 0 –*
Combinedanalgesics
4 10 1* 9 3 0.4*
Multiple drugs 8 27 0.232* 16 17 1.8*
Monthly abuse frequency(mean ± SD)
25.2 ± 6.49 25.9 ± 6.49 0.63 25 ± 7.19 26.2 ± 5.96 0.595
Monthly crisis frequency(mean ± SD)
23.5 ± 6.53 25.1 ± 6.3 0.258 24.2 ± 6.93 25.1 ± 5.89 0.632
Headache evolution time(mean ± SD)
17.3 ± 11.88 21.5 ± 12.86 0.154 18.6 ± 12.62 22.8 ± 12.62 0.137
Psychologicalalterations
Yes 11 39 0.071 19 21 0.083No 20 32 31 16
Insomnia Yes 14 29 0.685 21 16 0.908No 17 42 29 21
Painfulpathologies
Yes 13 29 0.918 19 16 0.622No 18 42 31 21
Data is presented as absolute number of patients in each category. p value < 0.05 is considered statistically significant
SD standard deviation
*Odds ratios
1520 SN Compr. Clin. Med. (2020) 2:1514–1525

treatment as soon as possible, in order to back away from thecourse of chronicity [37].
Chronic migraine is an entity of difficult treatment. Onmany occasions, finding effective treatment is an arduoustask. When preventive treatment is ineffective, it is interestingto assess the effectiveness of treatment with OBT-A.
In our study, the first step of the therapeutic strategy isdetoxification at the same time as the preventive treatmentfor all patients. In case that preventive treatment is ineffective,the patient receives OBT-A injection.
The Phase III Research Evaluating Migraine ProphylaxisTherapy (PREEMPT) trials show the effectiveness and toler-ability of OBT-A as a preventive treatment for CM, [38], andit should be administered in at least 31 injections across 7 headand neck muscles in patients not responding to oral prophy-lactic treatment [39].
OBT-A injection at the level of the trigeminally innervatedcranio-facial-cervical region may inhibit release of CGRPfrom peripheral nociceptive neurons, and it may decrease neu-ronal hyperexcitability and, consequently, peripheral and cen-tral sensitization (pathophysiological mechanisms of CM)[40].
Tertiary headache centres in Italy conducted a surveyreporting data from their OBT-A treated patients, which de-fined the response to toxin treatment as a 30–50% reduction inheadache days. Most of the centres had been using OBT-A formore than 1 year, and the toxin was administered according tothe PREEMPT paradigm, administering toxin every 3 monthsduring the first year. For 80% of the physicians, early admin-istration of OBT-A after the onset of chronic migraine wasassociated with better outcomes [41].
The European Federation of Headache establishes guide-lines for OBT-A treatment. It is important that the patientsabandon overuse medication, and it is recommended that theyreceive 2–3 prophylactic treatments before OBT-A treatment.According to the PREEMPT protocol, the patient is injected155–195 U in 31–39 sites every 12 weeks. Treatment is con-sidered ineffective if the reduction of headache days permonth is less than 30%, and it should be discontinued if thepatient does not improve after the first 2–3 treatment cycles[42].
The REPOSE study provides us information on patientstreated with OBT-A in real life over 24 months to obtain dataabout the effectiveness, tolerability and safety of treatment.
Table 4 Baseline characteristics stratified by 50% or more reduction of crisis
Characteristics First checking (4 months) Last checking (19 months)
Crisis reduction No crisis reduction p value Crisis reduction No crisis reduction p value
Gender Male 26 63 0.753 39 35 0.344Female 3 10 5 8
Age (mean ± SD) 40.9 ± 15.22 45.7 ± 13.66 0.125 44.8 ± 14.94 45.6 ± 13.35 0.808
Descending naproxen Yes 16 44 0.637 27 28 0.717No 13 29 17 15
Monthly abuse frequency(mean ± SD)
25.3 ± 6.31 25.9 ± 6.57 0.537 25 ± 7.13 26.07 ± 6.24 0.616
Monthly crisis frequency(mean ± SD)
23.4 ± 6.61 25.1 ± 6.27 0.237 24.4 ± 6.93 24.8 ± 6.07 0.802
Headache evolution time(mean ± SD)
17.5 ± 10.75 21.3 ± 13.27 0.3 17.5 ± 12.49 23.4 ± 12.37 < 0.023
Psychological alterations Yes 12 38 0.331 16 24 0.069No
Insomnia Yes 12 31 0.92 19 18 0.901No
Painful pathologies Yes 11 31 0.675 15 20 0.238No
Smoker Yes 6 18 0.67 10 10 0.953No 23 55 34 33
Triggering event Menstruation Yes 14 32 0.793 15 21 0.064No
Stress Yes 4 16 0.351 10 8 0.635No
Medication abuse suppression Yes 27 4 < 0.001 42 8 < 0.001No 2 69 2 35
Data is presented as absolute number of patients in each category. p value < 0.05 is considered statistically significant
SD standard deviation
1521SN Compr. Clin. Med. (2020) 2:1514–1525

The patients were injected every 12 weeks, and at each visit, aseries of outcome measures and data from different question-naires were collected.
Most of the patients werewomen of amean age of 45 years.The mean injection dose was 155.1 U following SPC recom-mendations (summary of product characteristics), at 31.4(mean value) injection sites per session. The patients reducedtheir headache days from baseline mean 20.6 to 7.4 days atadministration visit 8. At each visit, the health state scoreswere improving and only 18% of patients reported adverseeffects, such as neck pain, musculoskeletal stiffness, etc. [43].
As we said previously, therapy aimed at blocking the ef-fects of calcitonin gene-related peptide (CGRP) has recentlyemerged. In this sense, the studies of anti-CGRP antibodiesare very interesting. These antibodies act by binding to theCGRP ligand or its receptor, inhibiting the neuronal hyperex-citability caused by CGPRwhen it is secreted in the trigeminalfibres during migraine attacks [37, 44]. The use of three anti-CGPR antibodies (fremanezumab, galcanezumab anderenumab) has been approved by USA and Europe.
Medication Overuse Headache (MOH) Is an Entity inPermanent Debate
Vandenbussche analyses diagnostic criteria, classification,terms of semantics, etc. for MOH [45].
In the 1930s appeared the first description of MOH.Migraine is associated with ergotamine overuse for multipleauthors [46, 47]. In 1951, Peters and Horton defined chronicheadache following overuse of ergotamine [48].
In 1982, Mathew et al. observed that overuse of analgesicinduces the transformation of episodic migraine (EM) intodaily headaches, and introduced the term “transformed orevolutive migraine” [46, 49].
The first edition of the International Classification ofHeadache Disorders (ICHD) in 1988 defined the term “drug-induced headache”, and more later, Silberstein defined “trans-formed migraine” because of the transformation of EM todaily or almost-daily headache (> 15 days/month) with med-ication overuse [46, 50].
The second edition of the ICHD in 2004 defined the termmedication overuse headache for the first time and MOH sub-types induced by simple analgesics, combination analgesics,ergots, triptans and opioids [51].
After many debates, the third edition of the InternationalClassification of Headache Disorders (ICHD-3) definedMOH as a chronic headache disorder secondary to a pre-existing headache due to overuse of drugs for the acutetreatment of headache. MOH is diagnosed if patients useheadache medication more than 10 or more than 15 daysper month, depending on the drug class, for more than3 months [23].
Despite the fact that ICHD-3 clearly establishes the basisfor the diagnosis of MOH, the scientific community continuesto debate this issue.
MOH is generally observed in patients with pre-existingheadache, so it would be appropriate to consider it as a com-plication of this condition due to the probable abuse of symp-tomatic medication, and therefore, it would be a secondaryheadache disorder.
However, some patients without medication overuse pres-ent an aggravation of their primary headache. In these cases,we can consider that medication overuse is irrelevant and thatMOH would be a primary headache that requires a treatmentwithout detoxification [52, 53].
In terms of semantics, the term “medication overuse head-ache” was questioned by Solomon et al. in 2011. The termMOH can induce stigmatization of the doctor-patient relation-ship and blame the patient for the disease. For this reason,Salomon proposed to use terms like “medication-adaptationheadache” [54].
In this regard, our study shows results that lead us to be-lieve that CM with MO is a disease that appears in patientswith a history of primary headache (migraine in this case) ofyears of evolution, and that it presents clinical features differ-ent to primary headache (it would be a “transformation” of theprimary headache). In our patients, the pain is not hemicranial,pulsatile, etc. (migraine pain), but they report a dispersedheadache. However, other clinical signs of migraine such asnausea, vomiting, photophobia, phonophobia, etc. oftenremain.
Furthermore, it is important to highlight that the vast ma-jority of patients with CM with MO have a medical history ofmedication overuse for years.
Despite this, we cannot claim that medication overuse isthe cause of CM with MO. However, in this regard, it is arelevant fact that detoxification reverses the headache (de-crease in the intensity and frequency of attacks) in the vastmajority of cases.
Some researchers such as Martelletti et al. expose thatMOH is not an independent entity, but is a sequel or com-plication of chronic migraine. Genetic factors yet to bedefined, multiple comorbidity factors and medication over-use can be considered crucial [55–57]. In this sense, theydefend the term “chronic migraine plus medicationoveruse”.
They based their idea on studies of patients with chronicmigraine treated with onabotulinumtoxinA. These patients,mostly with a co-diagnosis of MOH, reduced their medicationintake and improved their headache [56]. In our study, weconsider the term “chronic migraine with medication overuse”as the most suitable.
A theory was confirmed by the Global Burden of Diseases2016 (GBD2016), in which it also exposed the idea that MOHis a complication of chronic migraine [58].
1522 SN Compr. Clin. Med. (2020) 2:1514–1525

Martelletti considers that migraine presents a natural evo-lution towards chronicity, in which the medication overuseinduces the aggravation of the disease. In this sense, the per-ception of pain by the patient is a determining factor of dis-ability that leads to medication overuse. He proposes the de-toxification or rehabilitation of medication overuse and thereduction of factors of disability as fundamental measures[59].
Indeed, our patients often suffer disabling pain that causesimpairment, and this affects all levels of life. It is a daily oralmost daily pain that leads to medication overuse, whichoften induces the phenomenon of dependency.
It is important to analyse this problem, since psychiat-ric comorbidity (very common in CM with MO) may becaused, in part, by this situation of medication depen-dence. CM with MO is associated with significant andvaried comorbidity. We observe that patients frequentlysuffer other diseases that require medication (analgesicsor other pharmacological groups). In this sense, these pa-tients can present pharmacological interactions, which canreinforce the state of medication dependence and aggra-vate the disease.
Multidisciplinary management of chronic migrainecomplicated by medication abuse with physical, mentaland social outcomes is important [60]. In this sense, weagree with the generalized idea that CM with MO patientsshould receive a multidisciplinary treatment (pharmaco-logical, psychological support, etc.) to process the greatcomplexity of this disease.
Acknowledgements The authors would like to thank the participants ofthe study for their cooperation.
Data Availability The datasets of the current study are not available forreasons of data protection of the hospital where it has been conductedunder study.
Compliance with Ethical Standards
Ethics Approval and Consent to Participate On January 13, 2016, RoyalDecree 1090/2015 of December 4, which regulates clinical trials withdrugs, the Ethics Committees for Drug Research and the SpanishRegistry of Clinical Studies entered into force. This regulation aims toadapt to Regulation (EU) 536/2014 of the European Parliament and of theCouncil of April 16, 2014, on clinical trials of medicines for human use,which will be fully applicable in October 2018. In order to be able tocontinue carrying out the evaluative activity that it carried out up to thatmoment on clinical trials, it adhered to theMemorandum of Collaborationwith the Spanish Agency forMedicines and Health Products (AEMPS) toact as the Research Ethics Committee with medicines (CEIm).
At the beginning of the study, All participants provided written in-formed consent
Conflict of Interest The authors declare that they have no conflicts ofinterest.
Consent for Publication All authors consented.
References
1. Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, BolligerI, et al. Global, regional, and national incidence, prevalence, andyears lived with disability for 301 acute and chronic diseases andinjuries in 188 countries, 1990-2013: a systematic analysis for theGlobal Burden of Disease Study 2013. Lancet. 2015;386:743–800.https://doi.org/10.1016/S0140-6736(15)60692-4.
2. Headache Classification Committee of the International HeadacheSociety (IHS) The international classification of headache disor-ders, 3rd edition. - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/29368949. Accessed 7 Mar 2020.
3. Katsarava Z, Jensen R. Medication-overuse headache: where arewe now? Curr Opin Neurol. 2007;20:326–30. https://doi.org/10.1097/WCO.0b013e328136c21c.
4. Stewart WF, Lipton RB, Celentano DD, Reed ML. Prevalence ofmigraine headache in the United States: relation to age, income,race, and other sociodemographic factors. JAMA J Am MedAssoc. 1992;267:64–9. https://doi.org/10.1001/jama.1992.03480010072027.
5. Kocasoy Orhan E, Baykan B. Medication overuse headache: thereason of headache that common and preventable. NoropsikiyatriArs. 2013;50:47–51.
6. Abrams BM. Medication overuse headaches. Med Clin North Am.2013;97:337–52.
7. Evers S, Marziniak M. Clinical features, pathophysiology, andtreatment of medication-overuse headache. Lancet Neurol.2010;9:391–401.
8. Cevoli S, Mochi M, Scapoli C, Marzocchi N, Pierangeli G, PiniLA, et al. A genetic association study of dopamine metabolism-related genes and chronic headache with drug abuse. Eur JNeurol. 2006;13:1009–13. https://doi.org/10.1111/j.1468-1331.2006.01415.x.
9. Peres MFP, Sanchez Del Rio M, Seabra MLV, et al. Hypothalamicinvolvement in chronic migraine. J Neurol Neurosurg Psychiatry.2001;71:747–51. https://doi.org/10.1136/jnnp.71.6.747.
10. Leistad RB, Nilsen KB, Stovner LJ, Westgaard RH, RøM, Sand T.Similarities in stress physiology among patients with chronic painand headache disorders: evidence for a common pathophysiologicalmechanism? J Headache Pain. 2008;9:165–75. https://doi.org/10.1007/s10194-008-0029-7.
11. Ferrari A, Leone S, Vergoni AV, Bertolini A, Sances G, CocciaCPR, et al. Similarities and differences between chronic migraineand episodic migraine. Headache. 2007;47:65–72. https://doi.org/10.1111/j.1526-4610.2006.00629.x.
12. Radat F, Creac’h C, Guegan-Massardier E, et al. Behavioral depen-dence in patients with medication overuse headache: a cross-sectional study in consulting patients using the DSM-IV criteria.Headache. 2008;48:1026–36. https://doi.org/10.1111/j.1526-4610.2007.00999.x.
13. Baskin SM, Lipchik GL, Smitherman TA. Mood and anxiety dis-orders in chronic headache. Headache. 2006;46:S76–87.
14. Radat F, Swendsen J. Psychiatric comorbidity in migraine: a re-view. Cephalalgia. 2005;25:165–78. https://doi.org/10.1111/j.1468-2982.2004.00839.x.
15. Headache Classification Committee, Olesen J, Bousser M-G, et al.New appendix criteria open for a broader concept of chronic mi-graine. Cephalalgia. 2006;26:742–6. https://doi.org/10.1111/j.1468-2982.2006.01172.x.
16. Solomon S. New appendix criteria open for a broader concept ofchronic migraine. Cephalalgia. 2007;27:469; author reply 469-70.https://doi.org/10.1111/j.1468-2982.2007.01292_1.x.
17. Radat F, Creac’h C, Swendsen JD, et al. Psychiatric comorbidity inthe evolution from migraine to medication overuse headache.
1523SN Compr. Clin. Med. (2020) 2:1514–1525

Cephalalgia. 2005;25:519–22. https://doi.org/10.1111/j.1468-2982.2005.00910.x.
18. Radat F, Creac’h C, Guegan-Massardier E, et al. Behavioral depen-dence in patients with medication overuse headache: a cross-sectional study in consulting patients using the DSM-IV criteria.Headache. 2008;48:1026–36. https://doi.org/10.1111/j.1526-4610.2007.00999.x.
19. Thorpy MJ. Classification of sleep disorders. Neurotherapeutics.2012;9:687–701.
20. El-Metwally A, Salminen JJ, Auvinen A, et al. Prognosis of non-specific musculoskeletal pain in preadolescents: a prospective 4-year follow-up study till adolescence. Pain. 2004;110:550–9.https://doi.org/10.1016/j.pain.2004.03.021.
21. Scher AI, Stewart WF, Lipton RB. The comorbidity of headachewith other pain syndromes. Headache. 2006;46:1416–23.
22. Munksgaard SB, Madsen SK, Wienecke T. Treatment of medica-tion overuse headache-a review. Acta Neurol Scand. 2019;139:405–14. https://doi.org/10.1111/ane.13074.
23. Olesen J and HCC of the IH (IHS). Headache ClassificationCommittee of the International Headache Society (IHS) the inter-national classification of headache disorders, 3rd edition.Cephalalgia. 2018;38:5–211. https://doi .org/10.1177/0333102417738202.
24. Corbelli I, Caproni S, Eusebi P, Sarchielli P. Drug-dependencebehaviour and outcome of medication-overuse headache after treat-ment. J Headache Pain. 2012;13:653–60. https://doi.org/10.1007/s10194-012-0492-z.
25. Krymchantowski A V., Krymchantowski AGF, Jevoux C da C(2018) Medication-overuse headache. Retrospective comparisonof preventive treatments. Arq Neuropsiquiatr 76:668–673. https://doi.org/10.1590/0004-282x20180097.
26. Biagianti B, Grazzi L, Usai S, Gambini O. Dependency-like behav-iors and pain coping styles in subjects with chronic migraine andmedication overuse: results from a 1-year follow-up study. BMCNeurol. 2014;14:181. https://doi.org/10.1186/s12883-014-0181-4.
27. Caronna E, Gallardo VJ, Hernández-Beltrán N, Torres-Ferrus M,Pozo-Rosich P. OnabotulinumtoxinA: an effective tool in the ther-apeutic arsenal for chronic migraine with medication overuse. FrontNeurol. 2018;9:808. https://doi.org/10.3389/fneur.2018.00808.
28. Yan Z, Chen Y, Chen C, Li C, Diao X. Analysis of risk factors formedication-overuse headache relapse: a clinic-based study inChina. BMC Neurol. 2015;15:168. https://doi.org/10.1186/s12883-015-0422-1.
29. Sancisi E, Cevoli S, Vignatelli L, Nicodemo M, Pierangeli G,Zanigni S, et al. Increased prevalence of sleep disorders in chronicheadache: a case-control study. Headache. 2010;50:1464–72.https://doi.org/10.1111/j.1526-4610.2010.01711.x.
30. Hagen K, Einarsen C, Zwart JA, Svebak S, Bovim G. The co-occurrence of headache and musculoskeletal symptoms amongst51 050 adults in Norway. Eur J Neurol. 2002;9:527–33. https://doi.org/10.1046/j.1468-1331.2002.00451.x.
31. Catarci T, Fiacco F, Argentino C, Sette G, Cerbo R. Ergotamine-induced headache can be sustained by sumatriptan daily intake.Cephalalgia. 1994;14:374–5. https://doi.org/10.1046/j.1468-2982.1994.1405374.x.
32. De Felice M, Ossipov MH, Porreca F. Update on medication-overuse headache. Curr Pain Headache Rep. 2011;15:79–83.https://doi.org/10.1007/s11916-010-0155-1.
33. Shah AM, Bendtsen L, Zeeberg P, Jensen RH. Reduction of med-ication costs after detoxification for medication-overuse headache.Headache. 2013;53:665–72. https://doi.org/10.1111/head.12031.
34. Hagen K, Albretsen C, Vilming ST, Salvesen R, GrøningM, HeldeG, et al. Management of medication overuse headache: 1-year ran-domized multicentre open-label trial. Cephalalgia. 2009;29:221–32. https://doi.org/10.1111/j.1468-2982.2008.01711.x.
35. Altieri M, Di Giambattista R, Di Clemente L, et al. Combinedpharmacological and short-term psychodynamic psychotherapyfor probable medication overuse headache: a pilot study.Cephalalgia. 2009;29:293–9. https://doi.org/10.1111/j.1468-2982.2008.01717.x.
36. Bigal ME, Rapoport AM, Sheftell FD, Tepper SJ, Lipton RB.Transformed migraine and medication overuse in a tertiary head-ache centre - clinical characteristics and treatment outcomes.Cephalalgia. 2004;24:483–90. https://doi.org/10.1111/j.1468-2982.2004.00691.x.
37. Agostoni EC, Barbanti P, Calabresi P, et al. Current and emergingevidence-based treatment options in chronic migraine: a narrativereview. J Headache Pain. 2019;20(1):92. Published 2019 Aug 30.https://doi.org/10.1186/s10194-019-1038-4.
38. Aurora SK, Dodick DW, Turkel CC, DeGryse RE, Silberstein SD,Lipton RB, et al. OnabotulinumtoxinA for treatment of chronicmigraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 30(7):793–803.
39. Tassorelli C, Tedeschi G, Sarchielli P, Pini LA, Grazzi L, GeppettiP, et al. Optimizing the long-term management of chronic migrainewith onabotulinumtoxinA in real life. Expert Rev Neurother.2018;18(2):167–76.
40. Frampton JE, Silberstein S. OnabotulinumtoxinA: a review in theprevention of chronic migraine. Drugs. 2018;78(5):589–600.
41 . Tassore l l i C , Agugg ia M, De Tommaso M, e t a l .Onabotulinumtoxin a for the management of chronic migraine incurrent clinical practice: results of a survey of sixty-three Italianheadache centers. J Headache Pain. 2017;18(1):66. https://doi.org/10.1186/s10194-017-0773-7.
42. Bendtsen L, Sacco S, Ashina M, et al. Guideline on the use ofonabotulinumtoxinA in chronic migraine: a consensus statementfrom the European Headache Federation. J Headache Pain.2018;19(1):91. Published 2018 Sep 26. https://doi.org/10.1186/s10194-018-0921-8.
43. Ahmed F, Gaul C, García-Moncó JC, Sommer K, Martelletti P,REPOSE Principal Investigators. An open-label prospective studyof the real-life use of onabotulinumtoxinA for the treatment ofchronic migraine: the REPOSE study. J Headache Pain.2019;20(1):26. Published 2019 Mar 7. https://doi.org/10.1186/s10194-019-0976-1.
44. Goldberg SW, Silberstein SD. Targeting CGRP: a new era for mi-graine treatment. CNS Drugs. 2015;29(6):443–52.
45. Vandenbussche N, Laterza D, Lisicki M, Lloyd J, Lupi C, TischlerH, et al. Medication-overuse headache: a widely recognized entityamidst ongoing debate. J Headache Pain. 2018;19:50. https://doi.org/10.1186/s10194-018-0875-x.
46. Boes CJ, Capobianco DJ. Chronic migraine and medication-overuse headache through the ages. Cephalalgia. 2005;25:378–90. https://doi.org/10.1111/j.1468-2982.2005.00868.X.
47. Lennox W. The use of ergotamine tartrate in migraine. N Engl JMed. 1934;210:1061–5.
48. Peters GA, Horton BT. Headache: with special reference to theexcessive use of ergotamine preparations and withdrawal effects.Proc Staff Meet Mayo Clin. 1951;26:153–61.
49. Mathew NT, Stubits E, Nigam MP. Transformation of episodicmigraine into daily headache: analysis of factors. Headache JHead Face Pain. 1982;22:66–8. https://doi.org/10.1111/j.1526-4610.1982.hed2202066.x.
50. Silberstein SD, Lipton RB, Solomon S, Mathew NT. Classificationof daily and near-daily headaches: proposed revisions to the IHScriteria. Headache. 1994;34:1–7.
51. Headache Classification Subcommittee of the InternationalHeadache Society. The international classification of headache dis-orders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160.
1524 SN Compr. Clin. Med. (2020) 2:1514–1525

52. Pijpers JA, Louter MA, De Bruin ME, et al. Detoxification inmedicationoveruse headache, a retrospective controlled follow-upstudy: does care by a headache nurse lead to cure? Cephalalgia.2016;36:122–30. https://doi.org/10.1177/0333102415583146.
53. Serrano D, Lipton RB, Scher AI, Reed ML, Stewart WF, AdamsAM, et al. Fluctuations in episodic and chronic migraine status overthe course of 1 year: implications for diagnosis, treatment and clin-ical trial design. J Headache Pain. 2017;18:101. https://doi.org/10.1186/s10194-017-0787-1.
54. Solomon M, Nahas SJ, Segal JZ, Young WB. Medication adapta-tion headache. Cephalalgia. 2011;31:515–7. https://doi.org/10.1177/033310241038767.
55. Martelletti P. The journey from genetic predisposition to medica-tion overuse headache to its acquisition as sequela of chronic mi-graine. J Headache Pain. 2018;19:2. https://doi.org/10.1186/s10194-017-0830-2.
56. Negro A, Martelletti P. Chronic migraine plus medication overuseheadache: two entities or not? J Headache Pain. 2011;12:593–601.
57. Farinelli I, Dionisi I, Martelletti P. Rehabilitating chronic migrainecomplicated bymedication overuse headaches: how can we preventmigraine relapse? Intern Emerg Med. 2011;6:23–8.
58. Giamberardino MA, Martelletti P. In: Martelletti P, editor.Comorbitidies in headache disorders. Cham: SpringerInternational Publishing; 2017. p. 1–217.
59. Martelletti P. Migraine disability complicated by medication over-use. Eur J Neurol. 2018;25(10):1193–4. https://doi.org/10.1111/ene.13736.
60. Kaiser U, KopkowC, Deckert S, Neustadt K, Jacobi L, Cameron P,et al. Developing a core outcome domain set to assessing effective-ness of interdisciplinary multimodal pain therapy: the VAPAINconsensus statement on core outcome domains. Pain.2018;159(4):673–83.
Publisher’s Note Springer Nature remains neutral with regard to jurisdic-tional claims in published maps and institutional affiliations.
1525SN Compr. Clin. Med. (2020) 2:1514–1525















![Neural Plasticity in Common Forms of Chronic …...2.3. Chronic Tension-Type Headache. TTH is the most common type of headache [11]. Unlike migraine, TTH is a“featureless” headache—usually](https://static.fdocuments.in/doc/165x107/5f174ec8d2918a30ee25ae88/neural-plasticity-in-common-forms-of-chronic-23-chronic-tension-type-headache.jpg)
