Carilion Clinic Heart Matters - HeartNet 2014
-
Upload
carilion-clinic -
Category
Documents
-
view
219 -
download
4
description
Transcript of Carilion Clinic Heart Matters - HeartNet 2014

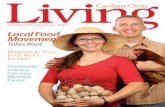
heart mattersCarilion Clinic
HEARTNET 2014
THE BOY WHO LIVEDThe teenager inexplicably defied death several times—on and off the operating table
WITHOUT MISSING A BEATNeither hurricanes nor floods nor even vice presidential candidates can deter the mission of HeartNet of the Virginias
Pace Setters Clinical care advances are helping
to ensure there’s more that can be done to mend
a broken heart

COVER PHOTOGRAPH: PETER MCARTHUR
4THE BOY WHO LIVED After his car was hit head-on not once, but twice, Connor McCauley had to undergo lifesaving open-heart surgery.
8PACE SETTERS How can you mend a broken heart? The Carilion Clinic cardiac team continues to enlarge its toolbox to be able to offer hope to a broader range of patients.
14WITHOUT MISSING A BEAT Neither hurricanes nor floods nor even vice presidential candidates can deter the mission of HeartNet of the Virginias.
18MATTERS OF THE HEART The Virginia Tech Carilion Research Institute helps set a new pace for cardiovascular research and collaboration.
Features

HEARTNET 2014 | cPHOTOGRAPHS: DARRYLE ARNOLD; ILLUSTRATION: BRIAN STAUFFER
CARILION CLINIC HEART MATTERS HEARTNET 2014
2 WELCOME
3 IN BRIEF Interventional and structural cardiology
fellowships • Chest Pain Center reaccredi-tation • Carilion Clinic’s rise in rankings
24 BACKSTORY: OPEN UP YOUR HEART
Bringing patients back from the brink of death makes it all worthwhile. by Jason Foerst, M.D.
Departments
contents
8Left: :Dr. Baker and his team operating on a wtktktk in the lab and tktktk more and more and more tktktktk and more
24
22STITCHED TOGETHER Each quilt square tells the story of a heart surgery; together, the squares reveal the power and com-passion of cardiac care.
Left: Joseph Baker, M.D., chief of cardiothoracic surgery, repairs a patient’s heart at Carilion Roanoke Memorial Hospital.

2 | CARILION CLINIC HEART MATTERS CREDIT TKTKT
welcome
IN 1899, THE YEAR CARILION ROANOKE MEMORIAL HOSPITAL WAS FOUNDED,
William McKinley was in the White House, the Alaska Gold Rush was on, and
the word “automobile” saw print for the first time.
Back then, cardiology was rudimentary at best. Although the invention
of the first electrocardiogram was only four years away, many key cardiac
treatments—from blood thinners to stents to angioplasty—were decades into
the future.
By the time HeartNet of the Virginias was formed 90 years later, the fields
of cardiology and cardiac surgery had made dramatic advances. Even so, it’s
easy to marvel at the technical limitations cardiologists faced even a quarter
century ago, at the founding of HeartNet.
But with the ever-accelerating pace of discovery, the timeline of our
astonishment is shortening. Can you believe, two years ago, that we weren’t
doing transcatheter aortic valve replacements? Or that this past winter we
didn’t have defibrillators that never touched the heart? Or just a few months
ago we had never developed a custom tricuspid valve?
Why is Carilion Clinic so focused on constantly improving the technologies
and treatments we embrace? In everything we do, our mission is excellence in
caring for the patient.
This special publication celebrates the 25th anniversary of an important aid
in ensuring that excellence of care: HeartNet. In these pages, we’re also tracing
our progression through the past and detailing our acceleration into the future
of cardiac treatment.
With heart disease the leading killer in the United States, Carilion remains
committed not only to providing the newest, most innovative, and most
effective treatments for cardiovascular disease, but also to preventing that
disease in the first place.
President and Chief Executive Officer
Nancy Howell Agee
CARILION CLINIC
1906 Belleview Avenue
P.O. Box 13367
Roanoke, VA 24033
540-981-7000
Vice President, Strategic Development
Shirley Holland
Senior Director, Marketing Mike Dame
Brand Manager Linda Staley
Editor Paula Byron
Designer Laura McFadden
Printing Chocklett Press
Special thanks to Soufian AlMahameed, M.D.; W. Scott
Arnold, M.D.; Joseph Baker, M.D.; Jason Foerst, M.D.;
Paul Frantz, M.D.; Gordon Garrett; Cathy Jennings,
D.N.P., R.N.; Melanie Johnson, R.N.; Laura Markowski;
Andrew, Connor, Drew, and Lisa McCauley; Page
Pace; Maureen Robb; Joseph Rowe, III, M.D.; David
Sane, M.D.; and Philip Shiner, M.D.
CARILIONCLINIC.ORG | 800-422-8482
Carilion Clinic is a not-for-profit health care organization based
in Roanoke, Virginia. Through our comprehensive network of
hospitals, primary and specialty physician practices, and other
complementary services, we work together to provide quality
care close to home for nearly one million Virginians. With an
enduring commitment to the health of our region, we also seek to
advance care through medical education and research to help our
community stay healthy and inspire our region to grow stronger.
© Copyright 2014 by Carilion Clinic. No part of this publication
may be reproduced or transmitted in any form or by any means
without written permission from Carilion Clinic. Articles in this
publication are written by journalists or authors who strive
to present reliable, up-to-date health information. However,
personal decisions regarding health, finance, exercise, and other
matters should be made only after consultation with the reader’s
physician or professional advisor. All editorial rights reserved.
Opinions expressed herein may or may not reflect the views of
Carilion Clinic.

HEARTNET 2014 | 3PHOTOGRAPHS: DARRYLE ARNOLD (THIS SPREAD)
in briefOn the pulse of the Carilion Clinic community
TO SERVE AND PROTECTCarilion Clinic recently expanded its car-diology fellowship offerings to include programs in interventional and structural cardiology. This spring, the Interventional Cardiology Fellowship—a one-year, ac-credited program with two positions a year—graduated its first fellows.
One of those fellows, Darron Lewis, M.D., has since become the charter member of the Adult Structural Heart and Valve Dis-eases Fellowship. The newer program, which accepts only one fellow a year, reflects Carilion’s growing emphasis on interven-tions for the treatment of structural and valvular heart disease, such as transcathe-ter aortic valve replacement.
Dr. Lewis, who grew up in South Phil-adelphia, was inspired to become a physi-cian while participating in a food drive for the elderly as an elementary school stu-dent. His interest in helping people hasn’t diminished. In fact, it has only deepened.
“I love being able to help acutely sick peo-ple become instantly better,” Dr. Lewis says. “That’s part of the joy of cardiology. Our im-pact can be immediate and dramatic.”
BEST IN CHESTThe Chest Pain Center at Carilion Roanoke Memorial Hospital was recently reaccredit-ed by the Society of Cardiovascular Patient Care. The hospital had become the first in Virginia to become accredited as a Chest Pain Center in 2005. The program, which seeks to enable patients and physicians to respond to cardiac health issues quickly and efficiently, has since helped more than 10,000 patients.
“This accreditation is more than an im-portant designation,” said David Sane, M.D., chief of cardiology. “It also reflects an inten-sive process of continuous refinement. As a result, we’re nimbler and more effective, with better outcomes for our patients.”
An Honor and a PrivilegeIn its recent 2014–15 Best Hospital list, U.S. News & World Report ranked Carilion Roanoke Memorial Hospital fourth in Virginia. Carilion’s flagship hospital earned high-performing status in 10 adult specialties, including Cardiology and Heart Surgery, Diabetes and Endocrinology, Gastroenterology and GI Surgery, Gynecology, Nephrology, Neurology and Neurosurgery, Orthopaedics, Pulmonology, and Urology.
“Our region is fortunate to have exceptional healthcare,” said Nancy Howell Agee, president and chief executive officer of Carilion Clinic. “Our caring, compassionate physicians, nurses, health professionals, and dedicated staff are passionate indeed about improving the health of the communities we serve.”
“ I love being able to help acutely sick people become instantly better. That’s part of the joy of cardiology. Our impact can be immediate and dramatic.”
—Darron Lewis, M.D.

The BoyWho Lived4 | CARILION CLINIC HEART MATTERS
AFTER HIS CAR WAS HIT HEAD-ON NOT ONCE, BUT TWICE, CONNOR MCCAULEY HAD TO UNDERGO LIFESAVING OPEN-HEART SURGERY.
PHOTOGRAPH: DAVID HUNGATE

HEARTNET 2014 | 5CREDIT TKTKT
ROAD WARRIOR: Connor McCauley and his sister were traveling down the interstate when a driver with a blood alcohol level twice the legal limit slammed into their car. And that was only the first hit.

6 | CARILION CLINIC HEART MATTERS
For nearly two miles, the Ford Explorer had been traveling south in the northbound lane of Interstate 81 near Salem, Virginia. It had already sideswiped two cars and narrowly missed nine others.
But Connor and Drew weren’t as lucky. They were cresting a hill and couldn’t see the trail of havoc that lay ahead. A single glance was all Connor had to register the 70-mile-an-hour mis-sile flying toward them. He swerved in time to save his sister from the full impact—but not himself.
Their car spun, only to be hit head-on again, this time by the sport utility vehicle following them. With the airbags already deflated, the steering wheel was now pinning Connor’s chest.
Connor had only a split second to prepare for the moment of impact, but, fortunately for him, Carilion Clinic had been preparing for that moment for decades.
AT THE READYDazed and battered, but with no serious injuries, 15-year-old Drew was able to call 911. Connor remained conscious as the rescue squad used hydraulic tools to pry him from the car. Carilion’s Life-Guard team then airlifted him to Carilion Roanoke Memorial Hospital.
There, the emergency team was ready for him. Connor was treated for a broken femur and clavicle, and his vitals were stable. But a CT scan revealed blood pooling around his heart.
An emergency department resident called the cardiothoracic surgeon on call, W. Scott Arnold, M.D., and said, “We have a kid here with a torn aorta.”
“A torn aorta? I thought, no way; he wouldn’t be alive,” Dr. Arnold later said. “But it was true. It was the kind of CT scan that would make any surgeon swallow hard. The sudden deceleration and the impact of both the airbag and the second head-on collision had led to a tricky tear in Connor’s aortic arch. I knew this one would be tough.”
Dr. Arnold drew a quick schematic of the tear for Connor’s parents, Andrew and Lisa. The surgery itself was not completely without risk, he told them. But without it, the risk to their son’s life would continue to rise with each passing hour.
As he was brought into the operating room, Connor remained calm and even stoic. When the anesthesiologist asked whether he had any questions, the teenager said he didn’t, adding, “I just want to thank you all for taking care of me.”
“Several members of the team got misty-eyed at that,” says Dr. Arnold. “I’ve been thanked after surgeries, but never before.”
Connor underwent open-heart surgery to repair the aorta, which had nearly been completely transected. The nine-hour operation,
One Saturday afternoon this past spring, 17-year-old Connor McCauley was
driving home from swim practice with his younger sister, Drew, when a Ford Explorer, hurtling
down the highway in the wrong direction, slammed into their sedan, ramped up their hood,
and crumpled their roof as it catapulted overhead.
which required induced hypothermia and the implantation of a four-branch vascular graft, was a resounding success.
THE ORDER OF THE PHOENIX“In the days following the surgery, Connor’s doctors kept stopping by to check on him,” says Lisa McCauley. “I made a comment to one of the nurses about their level of enthusiasm, and she said they were just so impressed with the boy who had survived an aortic tear.”
After Connor was safely home in Salem, his mother photographed a collage of items that had survived the crash unscathed: her children’s St. Christopher medals, their cell phones, and Connor’s glasses.
It’s tempting to think of another bespectacled teenager, Harry Potter, who was called “the boy who lived” after he too
DREAM TEAM: Connor and Drew McCauley’s swim team provided support to the entire family through local fundraisers and prayer networks that expanded even internationally.

HEARTNET 2014 | 7PHOTOGRAPHS: COURTESY OF THE MCCAULEY FAMILY
survived—with the help of some wizardry—a near-fatal encounter that left him with a jagged scar.
When asked whether he minded being likened to the famous wizard, Connor laughed. Years ago, on a family vacation to China, he said, he was asked many times whether he was Harry Potter.
THE NEXT LAPJust months after the accident, Connor, the long-distance competitor on his swim team, is back in the pool.
“I’m used to swimming at least 5,000 meters a day,” he says. “It’s not as easy as it was before, but I’m getting stronger.”
For Connor, a son of engineers, the experience has only deepened his interest in becoming a biomedical engineer.
The surgical repairs to his heart and left leg weren’t as bothersome, he says, as the fasciotomy he had to endure on his right leg when his crush injury led to compartment syndrome. It will take Connor nearly a year to recover from the nerve damage to that leg.
“As a biomedical engineer,” he says, “I might be able to invent a method for accelerating nerve regeneration.”
For his part, Dr. Arnold says he’ll always remember Connor’s grace and spirit.
“This is what we train for,” he says. “This is why we work so hard.” CC
Connor had only a split second to prepare for
the moment of impact, but, fortunately for
him, Carilion Clinic had been preparing for that
moment for decades.

8 | CARILION CLINIC HEART MATTERS
HOW CAN YOU MEND A BROKEN HEART? THE CARILION CLINIC CARDIAC TEAM CONTINUES TO ENLARGE ITS TOOLBOX TO BE ABLE
TO OFFER HOPE TO A BROADER RANGE OF HEART PATIENTS.

HEARTNET 2014 | 9PHOTOGRAPH: DARRYLE ARNOLD
S ETTERSPACEEARLY TO RISE: “At Carilion, we want to stay at the forefront of newer technologies,” says Joseph Baker, M.D., chief of cardiothoracic surgery. “We tend to be early adopters of more minimally invasive techniques.”

10 | CARILION CLINIC HEART MATTERS‘
AN ORDINARY DAY IN JANUARY 2012, first-grade teacher Vickie Hoffler felt an odd pressure in the center of her chest. So what did she do? She did what many would have done in her place: she made dinner, washed up, and went to bed.
Hoffler hadn’t been asleep long when she awoke to ribbons of pain running up her neck.
“They were really bad pains, and I thought, this is it,” Hoffler said. As her panicked husband hopped around the bedroom looking for a missing shoe, she called 911.
By the time Hoffler reached the hos-pital, she had lost consciousness and her heart attack had already done severe dam-age to her cardiac tissue.
When Hoffler awoke from a coma at Car-ilion Roanoke Memorial Hospital 10 days later, she found herself hooked up to a tem-porary pump that was keeping her alive. “It was the size of a 18-wheeler tire,” she says.
The 62-year-old from Vinton, Virginia, also found her surgeon awaiting her with a unique proposal. W. Scott Arnold, M.D., explained that some patients with advanced heart failure can benefit from an innovation known as a left-ventricular assist device, or LVAD, a mechanical circulatory device that helps pump blood throughout the body when a patient’s heart is too weak to do so.
Without a mechanical pump, Hoffler’s severely damaged heart could not func-tion properly. There was one catch: it was a surgery the hospital had never per-formed before. Would she be willing to be the first patient?
“We’re always trying to stay on the front edge of evolving science for advanced treatment of heart failure,” says Dr. Ar-nold. “I knew this miniaturized, implant-able device was one of those treatments.”
Hoffler agreed without hesitation. Days later, the team implanted the de-vice. The pump allowed her to leave the hospital wearing a harness and, around her waist, a fanny-pack-sized device; the battery-operated computer inside the pack controlled her heartbeat.
The LVAD gave Hoffler time to recover from her heart attack and resume most of her activities. For some patients, the device is a permanent solution; for others, it pro-
vides a bridge for a heart transplant. Hoffler eventually underwent a successful trans-plant at the University of Virginia.
“I am so thankful this implant was available and I was able to get it,” Hoffler says. “At that time, it was my only option.”
“We’re proud to offer innovative treat-ments like LVAD to our patients with advanced heart failure,” says Dr. Arnold. “Such treatments provide hope for people whose cardiac conditions can no longer be treated with medication.”
AT YOUR SERVICELVAD is just one of many recent additions to Carilion Clinic’s expanding array of car-diac services.
Although Carilion cardiologists had been treating heart patients for decades, it wasn’t until 1981, when Paul Frantz, M.D., became the hospital’s first cardio-thoracic surgeon, that those services began to extend to the operating room. Within a year, the cardiac surgery team had undertaken its first operation: replacement of a patient’s leaking heart valve. It was the first of thousands of lifesaving procedures.
At first, Carilion’s judicious early adop-tion of cardiac advances tended to make news on a regional level. Roanoke Memo-rial became the first hospital in the area, for example, to offer temporary mechan-ical support of a failing heart with the intra-aortic balloon pump, a device con-nected to the patient by a catheter insert-ed through an artery in the leg.
In 2000, the program took a technological leap forward with the purchase of a da Vinci Surgical System. This system allowed surgeons working at a computer to direct robotic arms to undertake minimally invasive surgery through small incisions.
“We were the second hospital in the state of Virginia to purchase and use the da Vinci system,” Dr. Frantz says.
Carilion Clinic has since become the only healthcare system in western Virginia with a hybrid operating room, I am so thankful this implant
was available and I was able to get it.”
ON
—Vickie Hoffler, recipient of a miniaturized, implantable heart pump

HEARTNET 2014 | 11PHOTOGRAPH: DARRYLE ARNOLD (THIS SPREAD)
a state-of-the-art, specially designed operating room that is also equipped with a catheterization laboratory and advanced imaging technology. This facility allows a range of specialists—including cardiac surgeons, interventional cardiologists, vascular surgeons, and interventional radiologists—to work together to perform minimally invasive procedures.
“Patients who might have otherwise required open-heart surgery can now be effectively treated with far less invasive procedures,” says Dr. Frantz. “The less in-vasive the procedure, the lower the risk of complications, the greater likelihood of a fast recovery, and the quicker a return to normal life for our patients.”
FOR THE FAINT OF HEARTOne advancement that the hybrid oper-ating room allows is transcatheter aortic valve replacement, or TAVR, a relatively new procedure that is available in only a few hundred medical centers nationally.
Interventional cardiologist Jason Foerst, M.D., brought the groundbreaking procedure to Carilion after training for nearly a year in Germany.
During this minimally invasive proce-dure, the Carilion team uses a catheter to implant an artificial heart valve by passing it through an artery in the patient’s leg. Special imaging equipment helps guide the valve into place.
The procedure is used for high-risk pa-tients and those who are not candidates for traditional open-heart surgery. It is used for patients with severe aortic ste-nosis, or narrowing of the heart’s aortic valve, which obstructs blood flow.
The Carilion team performed its first TAVR in 2012. Since then, a multispecial-ty team of cardiologists, cardiac surgeons, vascular surgeons, anesthesiologists, and cardiac catheterization and operating room staff collaborate to perform at least one procedure a week.
“TAVR is an excellent alternative for patients who may be too frail for conventional techniques,” Dr. Foerst says. “We’re able to offer TAVR—and therefore new hope—to our patients who are in their 80s and even 90s. This minimally invasive procedure offers major improvements in their quality of life.”
Earlier this year, soon after the U.S. Food and Drug Administration approved the Medtronic CoreValve, a self-expanding TAVR system, Carilion Roanoke Memorial Hospital became one of the first sites in Virginia to implant the new valve. For patients with aortic stenosis who are ineligible for surgery, the CoreValve can be inserted into an artery, usually in the leg, and positioned in the heart. There it automatically expands and replaces the damaged valve.
“The greatest advantage of this minimally invasive device is that it can be delivered through a much smaller tube,” says Dr. Foerst. “With most of our patients, we can deliver it through a tiny incision in the leg. Recovery times tend to be dramatically shorter, and our patients feel better almost immediately.”
LESS IS MOREIn the spring of 2014, the Carilion cardiology team began performing two other promising new procedures, this time in response to ab-errations in the heart’s electrical system.
Advances in technology are making implantable defibrillators safer and avail-able to more patients, says electrophysi-ologist Soufian AlMahameed, M.D. These small devices monitor the heart and, if it
beats out of rhythm, can deliver an elec-trical pulse to restore normal rhythm.
In May, in a first for Carilion, Dr. AlMahameed implanted a new, complete-ly subcutaneous cardiac defibrillator sys-tem. Older technologies use wires that run through a vein and are attached di-rectly to the heart. But the SQ-ICD device, manufactured by Boston Scientific, is the world’s first defibrillator that never touch-es the heart. Placed just beneath the skin, the SQ-ICD monitors and sends pulses to the heart remotely. With the cardiac team never having to touch the patient’s heart or blood vessels, the procedure is less in-vasive and often has fewer complications.
“As this defibrillator is completely subcutaneous, recipients don’t have any hardware inside their heart or inside their circulatory system,” Dr. AlMahameed says. “We’re excited about this new device, particularly for young and physically active patients who need implantable defibrillators to prevent sudden cardiac death.”
Another recent technological advance-ment will principally benefit patients who need both a defibrillator to restore normal rhythm and a pacemaker to help the heart maintain a healthy rhythm.
Dr. AlMahameed points out that old-er technology requires two wires—or leads—attached to different parts of the
WHO’S ON FIRST: This spring Soufian AlMahameed, M.D., and his fellow Carilion electrophysiologists became the first in the region to offer two promising new procedures.

12 | CARILION CLINIC HEART MATTERS PHOTOGRAPH: DARRYLE ARNOLD
heart. The new BiotroniK Single-Lead ICD can accomplish the same thing with a single wire. This means shorter surgeries and fewer potential complications.
“The BiotroniK ICD device has a newer technology that offers the ability to detect electrical signals from two cardiac chambers with a single lead,” Dr. AlMahameed says. “This device will enhance detection of silent atrial fibrillation and, we hope, reduce any short- and long-term complications.”
MAP OF THE HUMAN HEARTDr. AlMahameed doesn’t merely adopt new advances; he also invents them.
For the past five years, he has been refining a three-dimensional mapping system for the heart that allows a low-fluoroscopy approach to treating arrhythmias.
“With standard techniques, each com-plex procedure usually takes 60 to 100 min-
utes, which means the patient, the physician, and the staff are all exposed to more than an hour of radiation,” Dr. AlMahameed says. “But with our GPS-for-the-heart approach, we’re able to isolate arrhythmia-generating spots from the rest of the tissue in just two and a half minutes.”
Other procedures, Dr. AlMahameed adds, require no fluoroscopy at all.
“We were one of the first—and we’re still one of the few—centers in the world to do complex heart ablations without using fluoroscopy,” he says.
For the past two years, Dr. AlMaha-meed has implemented the technique in a protocolized fashion on every single case.
“When I was in training less than sev-en years ago, I couldn’t have imagined that a day would soon be coming when I’d be doing ablations for complex rhythm problems without using radiation or flu-oroscopy,” he says. “I feel like, instead of practicing contemporary electrophysiolo-
gy, we’re doing the future of electrophysi-ology now. That’s the most thrilling part.”
TAILOR MADECardiac arrhthymias haven’t been the only arena for recent innovation. This past spring, Bobby Broughman, a 75-year-old from Covington, Virginia, arrived at Carilion Roanoke Memorial Hospital with shortness of breath and congestive heart failure.
Broughman’s mitral valve was failing. It had degenerated, and one of its leaflets had developed a sudden tear. The artificial valve had been implanted 15 years earlier during open-heart surgery. But a repeat of that operation was not considered wise for Broughman, whose history of cardiac procedures was complex.
“We felt that a conventional approach with open-heart surgery was prohibitive in Mr. Broughman’s case,” says Joseph Rowe III, M.D., the cardiothoracic surgeon treating him. “We felt that to go back and do an open mitral valve operation would be a very treacherous procedure.”
Dr. Rowe had to figure out another way to treat his patient. So, after some research, he and the team decided to take a nontradi-tional approach to mitral valve replacement. Dr. Rowe fashioned a custom tricuspid valve for Broughman. He began by adapting the TAVR procedure.
“We took a valve on a catheter that was designed for the aortic position and turned it upside down so the flow would be in the correct direction,” Dr. Rowe says. “We then implanted that valve inside Mr. Broughman’s degenerated mitral valve.We were able to put together some things that were familiar with some things that were unfamiliar, yet well described in the medical literature, to come up with what we thought was a very novel solution to an otherwise unfixable problem.”
“Everything was so great,” Broughman says. “I was able to do much better even than they expected. I was up walking and
So many of the procedures we do represent a failure on the front end of medical practice—primary prevention.” —David Sane, M.D., Carilion Clinic’s Chief of Cardiology
BUILT TO ORDER: Bobby Broughman’s mitral valve was failing, and open-heart surgery was too risky. So his surgeons fashioned for him a custom tricuspid valve, to enable a minimally invasive approach to treating his congestive heart failure.
‘

HEARTNET 2014 | 13PHOTOGRAPH: COURTESY OF NATIONAL LIBRARY OF MEDICINE
It was while accompanying his father, a family
practitioner, on house calls in a horse and
buggy that Paul Dudley White, M.D., decided to
become a doctor.
Dr. White, often called the father of American
cardiology, later joined the medical staff of
Massachusetts General Hospital, where, in 1944,
he pioneered the concept of cardiovascular
disease prevention. Dr. White is most often
remembered as the doctor who cared for
Dwight Eisenhower when he went into cardiac
arrest while U.S. president.
In presenting an award to Dr. White just
months before he died in 1973, Theodore
Cooper, M.D., then director of what is now the
National Heart, Lung, and Blood Institute, said,
that Dr. White, though a visionary, could never be considered a patriarch, for he was
one of those rare people who would forever be young.
“He, himself, has young scientific ideas,” Dr. Cooper said. “He writes to me regularly
with imaginative, unexplored, daring ideas. But more than that, Dr. White will always be
young because he is forever a part of all those whom he has taught.”
Influential throughout the country, Dr. White also left a special legacy at Carilion
Clinic. For years, Dr. White mentored R. Earle Glendy, M.D., a noted heart specialist. The
two even published scientific papers together.
Dr. Glendy, who became Roanoke’s first cardiologist, practiced at Carilion Roanoke
Memorial Hospital for 31 years. Before retiring in 1977, he was director of cardiology at
the hospital, where he had also served as chief of staff and chief of medicine.
Dr. Glendy died in 1983, but not before influencing others. Philip Shiner, M.D., for
example, displays in his office two gifts from his mentor: an antique stethoscope and
a set of calipers inscribed with Dr. White’s name.
“Dr. Glendy shared an office with Dr. White before World War II and was the only
physician ever to do so,” says Dr. Shiner. “So I knew Dr. Glendy was a special person
and doctor and one with whom I wanted to work.”
Dr. Shiner in turn joined with Hayden Hollingsworth, M.D., in recruiting Paul Frantz, M.D.,
Carilion’s first cardiac surgeon and now its medical director for cardiac services. Dr. Frantz
founded the cardiac surgery program at Carilion and—with Dr. Hollingsworth and others—
HeartNet of the Virginias, a network of hospitals and physicians devoted to improving
cardiology services in western Virginia and eastern West Virginia.
“I’ve always felt Roanoke has had a direct connection to the beginning of cardiology
through Dr. White and Dr. Glendy,” says Dr. Shiner.
David Sane, M.D., Carilion’s chief of cardiology, agrees. “Dr. White’s legacy endures
within the Carilion family,” he says. “Every day we embrace his principles of cardiovascular
disease prevention and honor his influence in our daily care of patients.”
O FHEARTSTHE K INGcould do everything they required of me. And I wasn’t in any pain.”
ALL HANDS TO THE PUMPEven with all these technological advances, says David Sane, M.D., Carilion’s chief of cardiology, the most valuable tool remains teamwork.
“Historically, cardiovascular treatment has developed along two lines: the cardiolo-gist’s approach and the surgeon’s approach,” Dr. Sane says. “But in recent years the two disciplines have been merging. Just as we can do more, bigger, and better things as a team than we can do individually, there are certain things only a team of experts from different disciplines can achieve.”
All this hard work is reflected in statis-tics. Carilion Roanoke Memorial Hospital is western Virginia’s leading provider in all aspects of heart and vascular care, and it now ranks among the top three hospi-tals in Virginia for the number of heart disease patients treated.
And Carilion’s investment in new equipment and careful early adoption of advances has been paying off. In more than five years, for example, the Carilion cardiac team has not had to turn away a single patient with atrial fibrillation because there was nothing that could be done.
“Making new technologies available is part of our commitment to our patients,” Dr. Sane says. “There’s always more we can try.”
In the long run, though, Dr. Sane adds, prevention is the key.
“So many of the procedures we do rep-resent a failure on the front end of med-ical practice—primary prevention,” he says. “Statins, for example, are remark-able drugs. But even with all these med-ications and all these technological ad-vances, cardiac wards are still full. Many problems are social and economic and re-late to the health of the country and the region as much as to individual health.”
Dr. Sane says that’s why primary preven-tion is a critical part of Carilion’s misson.
“We’re committed not only to provid-ing the best, most advanced, and most effective treatments for patients with cardiac issues,” Dr. Sane says, “but also to helping our patients avoid developing cardiovascular disease.” CC

14 | CARILION CLINIC HEART MATTERS
NEITHER HURRICANES NOR FLOODS NOR EVEN VICE
PRESIDENTIAL CANDIDATES CAN DETER THE MISSION OF
HEARTNET OF THE VIRGINIAS.
BEAT

PHOTOGRAPHS: DARRYLE ARNOLD (RIGHT); ALISA MOODY (ABOVE)
TO THE RESCUE: Carilion Clinic’s Life-Guard, Virginia’s first air ambulatory service, provides 24-hour transport for the entire state of Virginia, as well as parts of West Virginia, North Carolina, and Tennessee. Below: Paul Frantz, M.D., a cofounder of HeartNet of the Virginias.
The Blue Ridge Mountains, named for their distinctive indigo-hued silhouettes, provide western Virginia and eastern West Virginia with breathtaking vistas. Yet all those rolling landscapes and bucolic backroads can be calamitous when it comes to cardiac emergencies.
In the early 1980s, Carilion established the Life-Guard air ambulance program to provide rapid transport of patients to what is now Carilion Roanoke Memorial Hospital from outlying facilities. But the hospital was already operating at capacity, and transferring everyone with a cardiac emergen-cy to Roanoke for care was not always feasible.
So, in 1989, in an effort to enhance the referral, treatment, and follow-up care of cardiac patients across the region, a group of hospitals and physicians decided to form a cardiac emergency network. Spearheaded by
HEARTNET 2014 | 15

16 | CARILION CLINIC HEART MATTERS
AND THE BEAT GOES ON A conference series has proved the lifeblood of HeartNet’s educational mission—and a much-anticipated annual pilgrimage.
PHOTOGRAPHS: EDWARD HAMILTON (TOP); COURTESY OF THE HOMESTEAD; COURTESY OF HOTEL ROANOKE; ISTOCK; ©2009 INTUITIVE SURGICAL, INC.
1989HeartNet of the Virginias is announced in May; just three months later, the first annual HeartNet conference is held at The Homestead, a historic resort in Hot Springs, Virginia. This initial planning meeting, for physicians only, focused on the concepts and direction of HeartNet.
1993
The early conferences continue to be held at sites throughout the region before moving to the Roanoke Valley in 1993. Eventually the usual site becomes Hotel Roanoke, whose maximum capacity—400 participants—is soon reached each year. A range of health care professionals are now invited.
2001The conference is held as scheduled just three days after the devastating attacks of September 11. A new sense of poignancy imbues participants’ discussions about saving lives during emergencies.
2002
A satellite feed from Carilion Roanoke Memorial Hospital allows a live-broadcast presentation of cardiac surgery during the conference. The presentation showcases the hospital’s da Vinci Surgical System, which enables surgeons to undertake minimally invasive surgery using robotics.
topography,” says Dr. Frantz. “Every day seemed like a pickup game of getting patients moved.”
Healthcare providers across the region—including HeartNet staff, regional hospital physicians and staff, air and ground transport teams, and Carilion Roanoke Memorial Hospital’s
several cardiologists and cardiothoracic surgeons—including Paul Frantz, M.D.; Hayden Hollingsworth, M.D.; and Robert Rude, M.D.—the network became known as HeartNet of the Virginias.
“We formed HeartNet in part because of the difficulties involved in transporting patients across such a challenging
SUPPORT NETWORK: For a quarter of a century, HeartNet of the Virginias has sought to promote excellence in cardiac care in western Virginia and eastern West Virginia. The network seeks to ensure advanced cardiac care to patients across the region and to provide followup care at their local hospitals.

HEARTNET 2014 | 17ISTOCK; ROANOKE STAR SENTINEL; DARRYLE ARNOLD
A conference series has proved the lifeblood of HeartNet’s educational mission—and a much-anticipated annual pilgrimage.
2003The patient whose surgery had been broadcast live to the conference the previous year is introduced on stage.
2006
Amid tornado warnings, the conference continues a years-long tradition of being plagued by natural disasters, with the travel of speakers and participants impeded at various times by flash flooding, hurricanes, and twisters.
2012Secret Service agents are stationed throughout Hotel Roanoke, as the Republican vice presidential hopeful, Paul Ryan, will be speaking at a $10,000-a-plate fundraiser that evening. A metal detector is installed, and as HeartNet organizers are packing up at the end of the conference, bomb-sniffing dogs inspect the ballroom.
2014
The HeartNet conference commemorates its 25th anniversary. A recent transcatheter aortic valve replacement performed in Carilion Roanoke Memorial Hospital’ s hybrid operating room is shown as part of the celebration.
“ WE FORMED HEARTNET IN PART BECAUSE OF THE DIFFICULTIES INVOLVED IN TRANSPORTING PATIENTS ACROSS SUCH A CHALLENGING TOPOGRAPHY.”
—Paul Frantz, M.D., Medical Director for Cardiac Services, Carilion Roanoke Memorial Hospital
Transfer Center and cardiac care teams—worked together to develop effective protocols. But streamlining patient transport was only part of the plan.
“Instead of developing a model that required local hospitals to transfer heart attack victims to the tertiary center,” says Dr. Frantz, “we also wanted to teach those hospitals to provide better cardiac care in their own facilities. So we developed training programs and helped them expand their cardiac services.”
Now celebrating its 25th anniversary, HeartNet has become a robust network of hospitals and physicians united in their mission to improve cardiac care in western Virginia and eastern West Virginia.
“We focus on being able to provide as rapid a response as possible to as many patients in cardiac distress as possible,” says Melanie Johnson, R.N., HeartNet’s clinical coordinator since 1996. “Daily instances of sudden cardiac cases might include anyone from a long-distance truck driver on the interstate, to a vacationer hiking local trails, to a farmer working a remote field. I’m just so proud of what our extended network does every day.”
During the network’s first year, 461 cardiac patients were transferred to Carilion Roanoke Memorial Hospital; transfers have since continued to climb, with several dozen regional hospitals having referred more than 30,000 patients to the hospital for advanced cardiac care.
The success of the network is measured in part, Dr. Frantz says, in the continued excellence of care in home communities and the number of people who engage in community education programs aimed at preventing cardiovascular disease. But the most important measurement, he says, is the number of lives saved.
“Over the past 25 years, HeartNet’s coordination efforts have saved countless lives by providing a high level of care not only during emergencies but during followup care as well,” Dr. Frantz says.
An annual conference held each fall is part of the strategy for ensuring that quality of care.
“Our annual conference provides important educational op-portunities,” Dr. Frantz says. “And we’re in constant communica-tion with all the hospitals. Our network is like family to us.” CC

ILLUSTRATION: BRAD YEO/THE ISPOT18 | CARILION CLINIC HEART MAT TERS
MATTERS OF THE HEART W H A T M A K E S T H E O L D T I C K E R T I C K ? S C I E N T I S T S A T T H E Virginia Tech Carilion Research Institute are hoping to find out. Well-known for its innovative, world-class brain research, the institute recently launched a major initiative in cardiovascular research, with four teams spearheading individual, yet linked, scientific programs.
“Heart disease is the nation’s number one killer,” said Michael Friedlander, Ph.D., the institute’s executive director, in announcing the expansion of the institute’s Center for Heart and Regenerative Medicine Research. “Now, with

CREDIT TKTKT CARILION CLINIC MEDICINE | 19

20 | CARILION CLINIC HEART MATTERS
Robert Gourdie, Ph.D., leads research into the repair and regeneration of diseased and injured tissues, including the heart. In addition, he has helped launch a company that is developing innovative new treatments in patients for tissue injury and repair.
Dr. Gourdie joined Virginia Tech from the Medical University of South Carolina in 2012. Prior to that, he earned his doctorate at Canterbury Uni-versity, in his home country of New Zealand, followed by postdoctoral training at University College London. A recipient of the Commonwealth Eminent Scholar Award in Heart and Regenerative Medicine, Dr. Gourdie is also a professor in the Virginia Tech–Wake Forest University School of Biomedical Engineering and Sciences.
Steven Poelzing, Ph.D., investigates the mechanisms of arrhythmias—abnormal patterns of electrical activity in the heart—that can cause loss of coordinated blood-pumping capability and even lead to sudden cardiac death. In particular, he seeks to determine how pathological insults such as cardiac inflammation and edema modulate the risk of sudden death in the young and how age changes this relationship.
Dr. Poelzing joined Virginia Tech in 2012 after serving as a research associate professor in bioengineering at the Heart Research Institute at the University of Utah School of Medicine. He received his doctorate from Case Western Reserve University, followed by postdoctoral training at MetroHealth in Cleveland. In addition to his role at the institute, Dr. Poelzing is an associate professor at the Virginia Tech–Wake Forest University School of Biomedical Engineering and Sciences.
Robert Gourdie, Ph.D.Professor and Director Center for Heart and Regenerative Medicine Research
Steven Poelzing, Ph.D.Associate ProfessorCenter for Heart and Regenerative Medicine Research
DISCOVERY CHANNEL: Steven Poelzing, Ph.D., a cardiovascular research team leader at the Virginia Tech Carilion Research Institute, is collaborating with Soufian AlMahameed, M.D., a Carilion Clinic electrophysiologist, to determine the mechanisms of atrial fibrillation.

HEARTNET 2014 | 21PHOTOGRAPHS: JIM STROUP (THIS SPREAD)
“The institute’s research teams are using some of the most advanced approaches to understanding heart development, function, damage, and repair,” Dr. Friedlander says. “They’re also embedded in a rich, interactive culture of technical innovation and intellectual creativity. The result will be an accelerated pace of discovery for better heart health.”
The individual research teams study the repair and regeneration of diseased and injured cardiac tissue, electrical currents in the heart, and the growth of new blood vessels. They are also seeking to use what they learn to help create interventions to treat these problems.
“The heart can become damaged suddenly or over time,” says Robert
Gourdie, Ph.D., director of the newly expanded center. “Why does electrical conductivity in the heart stop abrupt-ly? How do arteries become blocked? Our cardiovascular research teams are already collaborating with Carilion Clin-ic physicians to seek answers to these questions. We plan to expand these ef-forts to improve our understanding of exactly how the heart functions, why it sometimes fails to work properly, and how to prevent and repair any damage.”
Dr. Friedlander points out that many recent discoveries in cardiology were built on decades of research, often by basic bio-medical scientists and engineers.
“It’s usually collaboration across disci-plines,” Dr. Friedlander says, “that leads to the most innovative advances.” CC
four leading cardiovascular research teams working on some of the most pressing issues in cardiac health, disease, and repair, we’re poised to add to the institute’s successes in brain research with new advances in heart health.”
Together, the teams have already re-ceived more than $1.25 million a year in research funding and have another $1.8 million a year in pending grants, primarily from the National Institutes of Health. This funding, Dr. Friedland-er says, is in addition to the more than $5 million the institute has provided to launch the research programs and equip the laboratories with state-of-the-art high-resolution optical imaging, molec-ular biology, cell purification, and cardi-ac electrical monitoring technologies.
he institute’s research teams are using some of the most advanced approaches to understanding heart development, function, damage, and repair.” —Michael Friedlander, Ph.D., Executive Director,
Trained as a biomedical engineer, John Chappell, Ph.D., studies angiogenesis—the growth and regrowth of new blood vessels—in the injured heart, restoring circulation after blockage, and damage to the heart muscle.
Dr. Chappell joined Virginia Tech in 2014 from the University of North Carolina at Chapel Hill, where he undertook his postdoctoral training. He completed his doctorate at the University of Virginia. Dr. Chappell serves as an assistant professor at both the research institute and in the Virginia Tech–Wake Forest University School of Biomedical Engineering and Sciences.
James Smyth, Ph.D., leads his laboratory’s research program on heart failure and the development of effective anti-arrhythmic treatments.
Most recently, Dr. Smyth was conducting research at the Cedars-Sinai Heart Institute
in Los Angeles. Prior to that, he received his doctorate from University College Dublin in his home country of Ireland, followed by postdoctoral training at the University of California, San Francisco. Dr. Smyth is also an assistant professor of biology in Virginia Tech’s College of Science.
John Chappell, Ph.D.Assistant Professor Center for Heart and Regenerative Medicine Research
James Smyth, Ph.D.Assistant Professor Center for Heart and Regenerative Medicine Research
TVirginia Tech Carilion Research Institute

PHOTOGRAPHS: DARRYLE ARNOLD22 | CARILION CLINIC HEART MAT TERS
STITCHED TOGETHER“THANKS BE TO GOD AND DR. PAUL T. FRANTZ.” That valentine to a beloved surgeon—captured on a small cambric square—also marked the day a heart was mended.
Since 1992, quilt squares created by cardiac surgery patients and their families have adorned the walls of Carilion Roanoke Memorial Hospital. The tradition began as a way to commemorate the tenth anniversary of the cardiac surgery department.
“What began as an idea to recognize an anniversary has thrived, just as so many of our patients have,” says Cathy Jen-nings, D.N.P., R.N., a cardiac surgery clin-ical nurse specialist who founded and now oversees the quilt collection. “We now have 76 quilts lining four floors of the hospital. Most of the squares contain a patient’s name and date of surgery. But they’re so much more meaningful than those simple facts.”
Representing 30 years of lifesaving surgi-cal procedures, the quilts continue to provide a source of comfort to staff and patients alike.
“These simple squares represent lives for-ever transformed,” Jennings says. “In most cases, surgeries have allowed families to stay together. Other quilt squares remember the lives of loved ones. In all cases, the gratitude of our patients humbles us and encourages us to provide the most innovative and com-passionate care we can.” CC
EACH QUILT SQUARE TELLS THE STORY OF A HEART SURGERY; TOGETHER, THE SQUARES REVEAL THE POWER AND COMPASSION OF CARDIAC CARE.

HEARTNET 2014 | 23
“ What began as an idea to recognize an anniversary has thrived, just as so many of our
patients have.” —Cathy Jennings, D.N.P., R.N., Cardiac Surgery Clinical Nurse Specialist, Carilion Clinic

24 | CARILION CLINIC HEART MATTERS ILLUSTRATION: BRIAN STAUFFER
backstory
OPEN UP YOUR HEART Bringing patients back from the brink of death makes it all worthwhile. B Y J A S O N F OE R S T, M . D.
THE 83-YEAR-OLD WOMAN ARRIVED AT OUR clinic in florid heart failure, with a critical narrowing of her aortic valve.
She had been seeing her primary care provider in rural southern Virginia when one of our critical care nurses, rotating
in the clinic as part of nurse practitioner training, recognized the severity of the woman’s condition. The patient was referred to our valve clinic.
Remarkably, what allowed us to save the patient that day began with an innovation that happened around the time she was born. The dawn of interventional cardiology came when a German physician, Werner Forssmann, first threaded a catheter through a vein in his arm to the right atrium of his heart.
My subspecialty is in the emerging field of structural heart and percutaneous valvular inter-ventions. I completed my train-ing with a group of seasoned veterans who transitioned from a time when coronary artery by-pass grafting was the only option for revascular-ization. They experienced the challenges of early angioplasty followed by bare metal stents.
Today, modern drug-eluting stents are the pri-mary means of coronary revascularization. Since the first transcatheter valve procedure was performed a dozen years ago, we have seen a similar evolution in the treatment of valvular heart disease in patients at high risk for conventional surgical valve replacement.
The Europeans have been on the forefront of this wave, with official approval in 2007 of trans- catheter valves that we would not see commercially in this country for nearly five more years. So at the end of my training I spent nearly a year in Germa-ny—Forssmann’s home country—learning about
this frontier. There I was amazed that we could safely perform valvular interventions on octoge-narians with only conscious sedation.
Following this training I returned to the United States to help start Carilion Clinic’s program in transcatheter aortic valve replacement, or TAVR. A camaraderie among the cardiologists, heart surgeons, nurses, anesthesiologists, and radiologists quickly developed. Our multidisciplinary approach has been key to our success.
That approach certainly helped my 83-year-old patient. Within a week of her hospitalization, we had optimized her heart failure and completed her TAVR proce-dure. She was discharged several days later and now, more than six months out, she is thriving.
The opportunity to bring patients back from the brink of death—including those who would have just been treated palliatively only a short time ago—is why we are all so vested in this program.
I find it astounding that now we can not only treat coronary artery disease percutaneously, but also implant new aortic valves and send elderly patients safely home within two days.
Over the next year we will be routinely implanting a device into the pulmonary artery to remotely monitor our heart-failure patients’ volume status, repair regurgitant mitral valves through a single access in the femoral vein, and percutaneously exclude the left atrial appendage to reduce the risk of stroke in patients with atrial fibrillation.
I remain humbled by my predecessors and eager to see what the future holds. CC
Jason Foerst, M.D., is an interventional and structural cardiologist at Carilion Clinic.

HEARTNET 2014 | 25
Generations ago in western Virginia, neighbors came together to build a hospital. They figured everybody deserved to be well and stay that way. This is where Carilion Clinic began. And today, as a recognized leader providing a comprehensive system of clinical care, research, and education, it’s why we’re here. To keep everyone in our community, big and small, healthy and strong. From moment one.
CarilionClinic.org
HERE FOR EVERYONE,

Bath Community Hospital – Hot Springs, Va.
Bedford Memorial Hospital – Bedford, Va.
Bluefield Regional Medical Center – Bluefield, W.Va.
Carilion Franklin Memorial Hospital – Rocky Mount, Va.
Carilion Giles Community Hospital – Pearisburg, Va.
Greenbrier Valley Medical Center – Greenbrier, W.Va.
Carilion New River Valley Medical Center – Christiansburg, Va.
Carilion Roanoke Memorial Hospital – Roanoke, Va.
Pocahontas Memorial Hospital – Buckeye, W.Va.
Princeton Community Hospital – Princeton, W.Va.
Carilion Stonewall Jackson Hospital – Lexington, Va.
Carilion Tazewell Community Hospital – Tazewell, Va.
Wythe County Community Hospital – Wytheville, Va.
Celebrating 25 years of collaborative heart care
1989-2014
HEARTNET OF THE VIRGINIAS
ANNIVERSARY