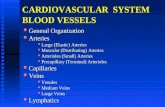
Cardiovascular System: Blood
description
Transcript of Cardiovascular System: Blood

Cardiovascular System: Blood
Clinical Anatomy
Tony Serino, Ph.D.
Biology Department
Misericordia Univ.

Blood
• Liquid connective tissue
• Arises from hemopoietic tissue: 1. myeloid tissues (Red bone marrow) 2.lymphoid tissues (thymus, spleen, lymph nodes, tonsils, etc.
• In fetus, liver and yolk sac are hemopoietic

Properties of the Blood
• Volume 4-6L (5-6L men, 4-5L women)based on body size (8% of total body weight)
• pH 7.4 + 0.1
• 5X the viscosity of water
• Hematocrit = 45

Blood Composition

Plasma Composition
• 90% water
• 10% suspended or dissolved constituents
• Plasma Constituents (10%)– 0.9% NaCl + other electrolytes– Nutrients– Plasma proteins: albumin, globulins, fibrinogen
– Dissolved gases: O2, CO2, N2

Functions of the Blood
• Transportation media
• Osmoregulation
• Acid-Base balance
• Protection

Hemopoiesis (RBC development)
• Rate controlled by erythropoietin secretion• Availability of Fe++, folic acid, vitamin B12 and
amino acid precursors for hemoglobin production

RBC Production Control

Formed Elements

RBC (erythrocyte) • Lives 120 days• Non-nucleated
biconcave disc• 4.5-5.5 million/mm3
• 1/3 of cytoplasm is hemoglobin

Rouleau

Hemoglobin

Hemoglobin Metabolism

Point Mutation in Sickle Cell

Sickle Cell Anemia

Blood Types

Blood Typing
Anti-D

ABO Blood Group Summary

WBC Development

WBC Development

Distribution of WBC

NeutrophilMost abundant circulating WBC (55-65% of WBCs), highly phagocytic, 1st to arrive at site of infection

Eosinophil2-4% of WBC, combat irritants that trigger inflammation, phagocytic for Ag-Ab complexes, destroy worm infections, limit inflammation

BasophilLeast abundant WBC (0.5% of WBC), trigger inflammation, contain vesicles with vasoactive compounds

Monocyte
3-8% of WBC, highly phagocytic and chemotaxic, arrive second to neutrophils at site of infection but in more massive numbers, can undergo diapedesis; some take up permanent residence in some tissues (often has a C-shaped nucleus)

LymphocyteSecond most abundant WBC (20-30% of WBC), function in specific immunity, two types: T and B cells

Platelet Development

Platelets
• 150-400 thousand/mm3
• 2-4 mcm in diameter• Function in clotting
and vessel repair

Hemostasis (stoppage of bleeding)
• Extravascular Mechanisms– Tightening of skin and muscles around injury– Behavior response (elevate, applied pressure)
• Vascular Mechanisms– Vasoconstriction (vascular spasms)
• Intravascular Mechanisms– Platelets –plug formation and factor secretion (PF3)
– Clotting factors (extrinsic and intrinsic system)

Platelet Plug and Clotting
The common clotting pathway
Platelet aggregation is increased by the stuck platelets releasing Thromboxane which stimulates vasoconstriction and attracts more platelets to area. Prostacyclin inhibits this and is released by non-damaged endothelial cells

Plateletstimulated
(PF3)
(TF)
(PF3) or (TF)
(Stabilizing Factor)

Coagulation Summary1. Coagulation may be triggered by intrinsic or extrinsic
pathway, but in the body the extrinsic path is the one most commonly used.
2. Activated Factors X, V, Ca2+, and PF3 or TF combine to change Xa into prothrombin activator which catalyzes prothrombin to thrombin
3. Thrombin then catalyzes Fibrinogen to Fibrin turning the blood into a gel-like state
4. Activate Factor XIII stabilizes and strengthens the fibrin.
5. Finally the platelets in the clot contract, squeezing the plasma from the clot. (Clot retraction)
6. After 2 days, enzymes in clot activate plasminogen into plasmin with begins dissolving clot

Fibrin Clot

Bleeding Disorders• Thrombocytopenia
– –decrease number of platelets
• Impaired Liver Function – responsible for many of the clotting factors in the blood
– Vit. K used as co-factor in many clotting factor syntheses; liver bile salts help in absorbing this vitamin
• Hemophilia –hereditary bleeding disorders– Class A (classical) –deficiency of factor VIII; most common
hemophilia (83%)
– Class B deficiency of factor IX• A & B is sex (X) linked trait; mainly seen in males
– Class C deficiency of factor XI –less severe; seen in both sexes