Cardio Notes
-
Upload
ma-honeycho -
Category
Documents
-
view
229 -
download
5
description
Transcript of Cardio Notes

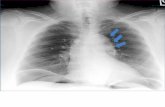
PNEUMOTHORAX – partial / or complete collapse of lungs due to entry or air in pleural space.
Types:
1. Spontaneous pneumothorax – entry of air in pleural space without obvious cause.Eg. rupture of bleb (alveoli filled sacs) in pt with inflamed lung conditions
Eg. open pneumothorax – air enters pleural space through an opening in chest wall
-Stab/ gun shot wound
2. Tension Pneumothorax – air enters plural space with @ inspiration & can’t escape leading to over distension of thoracic cavity resulting to shifting of mediastinum content to unaffected side.Eg. flail chest – “paradoxical breathing”
Predisposing factors:
1.Chest trauma
2.Inflammatory lung conditions
3.Tumor
S/Sx:
1. Sudden sharp chest pain 2. Dyspnea3. Cyanosis4. Diminished breath sound of affected lung5. Cool moist skin6. Mild restlessness/ apprehension7. Resonance to hyper resonance
Diagnosis:
1. ABG – pO2 decrease –2. CXR – confirms pneumothorax
Nursing Mgt:
1. Endotracheal intubation2. Thoracenthesis3. Meds – Morphine SO4- Anti microbial agents4. Assist in test tube thoracotomy
Nursing Mgt if pt is on CPT attached to H2O drainage
1. Maintain strict aseptic technique2. DBE3. At bedside
a.) Petroleum gauze pad if dislodged Hemostanb.) If with air leakage – clamp c.) Extra bottle
4. Meds – Morphine SO4Antimicrobial
5. Monitor & assess for oscillation fluctuations or bubblinga.) If (+) to intermittent bubbling means normal or intact
1

- H2O rises upon inspiration
- H2o goes down upon expiration
b.) If (+) to continuous, remittent bubbling
1. Check for air leakage
2. Clamp towards chest tube
3. Notify MD
c.) If (-) to bubbling
1. Check for loop, clots, and kink
2. Milk towards H2O seal
3. Indicates re-expansion of lungs
When will MD remove chest tube:
1. If (-) fluctuations2. (+) Breath sounds3. CXR – full expansion of lungs
Nursing Mgt of removal of chest tube
1. DBE2. Instruct to perform Valsalva maneuver for easy removal, to prevent entry of air in pleural space. 3. Apply vaselinated air occlusive dressing - Maintain dressing dry & intact
Flail Chest
Affected side goes down during inspiration and up during expiration
Sucking Chest Wound
(Sucking Open Pneumothorax)
Sucking sound with respiration
Pain Decreased breath
sounds Anxiety
Pneumothorax
Collapse of lung due to alteration of air in intrapleural space
Dyspnea Pleuritic pain Restricted movement
on affected side Decreased/absent
breath sounds Cough Hypotension
Implementation
Monitor for shock
Humidified oxygen
Thoracentesis (aspiration of fluid from pleural space)
Chest Tubes
Tracheostomy Tube Cuff
Purpose—prevents aspiration of fluids Inflated
o During continuous mechanical ventilationo During and after eatingo During and 1 hour after tube feedingo When patient cannot handle oral secretions
2

Oxygen Administration: assess patency of nostril, apply jelly
Face mask: 5-10 l/min (40-60%) Partial rebreather mask: 6-15 l/min (70-90%); keep reservoir bag 2/3 full during inspiration Non-rebreather mask: (60-100%); keep reservoir bag 2/3 full during inspiration Venturi mask: 4-10 l/min (20-50%); provides high humidity and fixed concentrations, keep tubing free of kinks Tracheostomy collar or T-piece: (20-100%); assess for fine mist; empty condensation from tubing’ keep water container full Croupette or oxygen tent:
o Difficulty to measure amount of oxygen deliveredo Provides cooled, humidified airo Check oxygen concentration with oxygen analyzer q4 hourso Clean humidity jar and fill with distilled water dailyo Cover patient with light blanket and cap for heado Raise side rails completelyo Change linen frequentlyo Monitor patient’s temperature
Chest Tubes Implementations
Use to utilize negative pressure in lungs
Fill water-seal chamber with sterile water to 2 cm
Fill suction control chamber with sterile water to 20 cm
Maintain system below level of insertion
Clamp only momentarily to check for air leaks
Ok to milk tubing towards drainage
Observe for fluctuation in water-seal chamber
Encourage patient to change position frequently
Chest Tube Removal:
Instruct patient to do valsalva maneuver
Clamp chest tube Remove quickly Occlusive dressing
applied
Complications of Chest Tubes:
Constant bubbling in water-seal chamber=air leak
Tube becomes dislodged from patient, apply dressing tented on one side
Tube becomes disconnected from drainage system, cut off contaminated tip, insert sterile connector and reinsert
Tube becomes disconnected from drainage system, immerse end in 2 cm of sterile water
CVP: measures blood volume and efficiency of cardiac work; tells us right side of heart able to manage fluid
“0” on mamometer at level of right atrium at midaxilliary line Measure with patient flat in bed Open stopcock and fill manometer to 18-20 cm Turn stopcock, fluid goes to patient Level of fluid fluctuates with respirations Measure at highest level of fluctuation After insertion
o Dry, sterile dressingo Change dressing, IV fluids, manometer, tubing q24 hours
3

o Instruct patient to hold breath when inserted, withdrawn, tubing changedo Check and secure all connections
Normal reading—3-11 cm water Elevated>11, indicates hypervolemia or poor cardiac contractility (slow down IV, notify physician) Lowered<3, hypovolemia Chest tray at bedside
Oxygen Toxicity
S/S - nonproductive cough, substernal pain, nasal stuffiness and hypoventilation
Treatment :
- use of CPAP, BiPAP or PEEP
- give the least amount of O2 necessary to maintain SaO2 levels
- use Venturi Mask when client needs precise amount of O2 delivered such as those with COPD
Types of Ventilator alarms ...
Volume alarm: Ventilator (L) - alarm indicate low exhaled volume d/t disconnection, cuff leak, and tube displacement
Pressure alarm: Ventilator (H) - alarm indicate excess secretions, client biting the tubing, kinks and client coughing
Apnea alarm: Ventilator indicate that the ventilator does not detect spontaneous respiration
Hemodynamic Readings ** the intravascular volume in older adult clients is often reduced; therefore, the nurse should anticipate lower hemodynamic readings, particularly if dehydration is a complication
ELEVATED results are indicative of HF and pulmonary problems
Central Venous Pressure (CVP) 1-8 mmHg
Pulmonary Artery Systolic (PAS) 15-26 mmHg
Pulmonary Artery Diastolic (PAD) 5 - 15 mmHg
Pulmonary ARtery Wedge Pressure (PAWP) 4-12 mmHg
Cardiac Output (CO) 4-6L/min
Mixed Venous Oxygen Saturation (SvO2) 60% - 80%
Arterial/Pulmonary Artery Line Insertion - Pace the client in supine or trendelenburge position
- level transducer with phlebostatic axis (4th intercostal space, mid-axillary line)
- zero system with atmospheric pressure
- hemodynamic pressure lines must be calibrated to read atmospheric pressure as zero, and the transducer should be positioned at the right atrium
** HOB when obtaining readings should be 15-30 deg
4

Angina - Warning sign of an impending acute MI
- described as: TIGHT, SQUEEZING, heavy pressure, or constricting feeling in the chest. the pain can radiate to the jaw, neck, or arm.
Types of Angina - stable angina (exertional): occurs with exercise or emotional stress and is relieved by rest or nitroglycerin (Nitrostat)
- unstable angina (preinfarction angina): occurs with exercise or emotional stress, but it increases in occurrence, severity, and duration over time
- variant angina (Prinzmetal's angina): dt a coronary artery spasm, often occurring during periods of rest.
** Pain unrelieved by rest or nitroglycerin and lasting more than 15 in differentiates an MI from angina
Angina vs MI Angina
- precipated by exertion or stress
- relieved by rest or nitroglycerin
- sx last <15 min
- not associated with nausea, epigastric distress, dyspnea, anxiety, diaphoresis
MI - con occur w/o cause, often in the morning after the rest
- relived only by opioids (MORPHINE)
- sx last > 30 min
- associated with nausea, epigastric distress, dyspnea, anxiety, diaphoresis
Lab tests - myoglobin: levels no longer evident after 24 hrs
- Creatnine kinase MB: levels n longer evident after 3 days
- Troponin I: levels NO longer evident after 7 days
- Troponin T: levels no longer evident after 14-21 days
Heart Failure/ Cardiogenic shock - injury to LEFT ventricle can lead to decreased CO and HF
- progressive HF leads to cardiogenic shock
S/S
- hypotension
- tachycardia
- altered level of consciousness
- respiratory distress (crackles/ tachypnea)
- decreased peripheral pulses
- chest pain
5

s/s: Left sided heart failure - S3 gallop
- orthopnea
- oliguria
- frothy sputum
- displaced apical pulse
s/s: right sided heart failure - jugular vein distension
- ascending dependent edema
- polyuria at rest
- abdominal distension (ascites
- weight gain
- hepatomegaly and tenderness
Lab tests: HF - Human B-type natriuretic peptides (hBNP): Elevated in HF; used to differentiate dyspnea rt HF vs respiratory problem
- <100 pg/mL = no HF
- 100 to 300 pg/mL = HF is present
- > 300 pg/mL = mild HF
- >600 pg/mL = moderate HF
- >900 pg/mL - severe HF
Diuretics - Loop: Lasix and Bumex
administer Lasix no faster than 20 mg/min Thiazide: hydrochlorothiazide Potassium sparing diuretics: spironolactone (aldactone) Afterload reducing agents - ACE inhibitors: "prils" Angiotensin receptor II blockers: losartan (Cozaar) contraindicated for clients who have renal deficiency monitor for HYPOTENSION
Client Education
notify MD if sense of taste decrease notify MD if swelling of the face or extremities occurs take BP 2 hrs after initial does to detect hypotension Inotropic agents- digoxin, duutamine, primacor Increase the contractility and thereby improve CO
Nx considerations
-digoxin: take apical pulse for 1 min; < 60/min hold the med and notify MD - monitor urine output client education - if pulse is irregular; hold meds and notify MD
6

- take digoxin dose same time each day - DO NOT take digoxin with antacids; separate by 2 hrs apart - toxicity signs: fatigue, muscle weakness, confusion, loss of appetite. Therapeutic range: digoxin 0.8 to 2 ng/mL
Toxicity:
decreased potassium level decreased apical rate < 60 blurred vision dysrhythmia leg cramps anorexia altered mental status
Vasodilators
Nitroglycerine (Nitrostat) and isosorbide mononitrate (Imdur): prevent coronary artery vasospasms and reduce preload and afterload, decreasing myocardial O2 demand.
Nx Considerations
caution with other antihypertensive medications can cause ORTHOSTATIC HYPOTENSION
Client Education
HEADACHE is common side effects Encourage the client to site and lie down slowly
hBNPs nesiritide (Natrecor): used to treat acute HF by casing natriuresis (loss of sodium and vasodilation)
Nx Considerations
can cause HYPOTENSION BNP levels will increased while on this med
Client Education
client can be asymptomatic with low BP
Pulmonary Edema
Nx Actions
restrict fluid intake administer rapid acting diuretics (lasix/bumex), vasodilators (nitroglycerin), inotropic agents (digoxin),
antihypertensive ("pril" and "olol") Client education notify md if gain of more than 2lb in a day or 5 lb in a week diet: low sodium and fluid restriction report: SOB, swelling of feet or ankles, or angina
Complications ...
7

Acute Pulmonary edema s/s
tachycardia ascending fluid level within the lungs (CRACKLES, productive cough, blood tinged sputum)
Emergency response
position in high-Fowler's Administer O2, positive airway pressure, and/or intubation and mechanical ventilation IV morphine IV Lasix ** effectiveness = diuresis, reduction in respiratory distress, improved lung sounds, and adequate O2
Cardiovascular System
8

Pericardium
Parietal layer Pericardial Visceral layer
Fluid – prevent
Friction rub
Layer
1. Epicardium – outermost2. Myocardium – inner – responsible for pumping action/ most dangerous layer - cardiogenic shock3. Endocardium – innermost layer
Chambers
1. Upper – collecting/ receiving chamber - Atria2. Lower – pumping/ contracting chamber - Ventricles
Valves
1. Atrioventricular valves - Tricuspid & mitral valve Closure of AV valves – gives rise to 1st heart sound or S1 or “lub”
2. Semi lunar valvea.) Pulmonicb.) AorticClosure of semilunar valve – gives rise to 2nd heart sound or S2 or “dub”
Extra heart Sound
S3 – ventricular Gallop – CHF
S4 – atrial gallop – MI, HPN
Heart conduction system
1. Sino atrial node (SA node) (or Keith-Flock node) Loc – junction of SVC & Rt atrium
Fx- primary pace maker of heart
-Initiates electric impulse of 60 – 100 bpm
2. Atrioventicular node (AV node or Tawara node)Loc – inter atrial septum
Delay of electric impulse to allow ventricular filling
3. Bundle of His – location interventricular septumRt main Bundle Branch
Lt main Bundle Branch
4. Purkenjie Fiber Loc- walls of ventricles-- Ventricular contractions
Complete heart block – insertion of pacemaker at Bundle Branch
Metal – Pace Maker – change q3 – 5 yo
9

Prolonged PR – atrial fib T wave inversion – MI
ST segment depression – angina widening QRS – arrhythmia
ST – elev – MI
CAD – coronary artery Disease or Ischemic Heart Disease (IHD)
Atherosclerosis – Myocardial injury
Angina Pectoris – Myocardial ischemia
MI- myocardial necrosis
ATHEROSCLEROSIS ARTEROSCLEROSIS
- Hardening or artery due to fat/ lipid deposits at tunica intima.
- Narrowing or artery due to calcium & CHON deposits at tunica media.
ATHEROSCLEROSIS
Predisposing Factor
1. Sex – male2. Black race3. Hyperlipidemia4. Smoking5. HPN6. DM7. Oral contraceptive- prolonged use8. Sedentary lifestyle9. Obesity10. Hypothyroidism
Signs & Symptoms
1. Chest pain2. Dyspnea3. Tachycardia4. Palpitations5. Diaphoresis
Treatment
P – percutaneous
T – tansluminar
C – coronary
A – angioplasty
Obj:
1. To revascularize the myocardium2. To prevent angina
10

3. Increase survival rate
PTCA – done to pt with single occluded vessel .
Multiple occluded vessels - CABG
Nsg Mgt Before CABG
1. Deep breathing cough exercises2. Use of incentive spirometer3. Leg exercises
ANGINA PECTORIS- A clinical syndrome characterized by paroxysmal chest pain usually relieved by REST or NGT nitroglycerin, resulting from temp myocardial ischemia.
Predisposing Factor:
1.sex – male2.African American3.hyperlipidemia4.smoking5.HPN6.DM7.oral contraceptive - prolonged8.sedentary lifestyle9.obesity
10.hypothyroidism
Precipitating factors
4 E’s
1. Excessive physical exertion2. Exposure to cold environment - Vasoconstriction3. Extreme emotional response
4. Excessive intake of food – saturated fats.
Signs & Symptoms
1. Initial symptoms – Levine’s sign – hand clutching of chest 2. Chest pain – sharp, stabbing excruciating pain. Location – substernal
-radiates back, shoulders, axilla, arms & jaw muscles
-relieve by rest or NGT
3. Dyspnea 4. Tachycardia5. Palpitation6. Diaphoresis
Diagnosis
1. History taking & PE
11

2. ECG – ST segment depression
3. Stress test – treadmill = abnormal ECG
4. Serum cholesterol & uric acid - increase.
Nursing Management
1.) Enforce CBR
2.) Administer meds
NTG – small doses – venodilator
Large dose – vasodilator
1st dose NTG – give 3 – 5 min
2nd dose NTG – 3 – 5 min
3rd & last dose – 3 – 5 min
Still painful after 3rd dose – notify doc. MI!
Medication:
A. NTG- Nsg Mgt:
1. Keep in a dry place. Avoid moisture & heat, may inactivate the drug.2. Monitor S/E:
o orthostatic hypotension – dec bpo transient headacheo dizziness
3. Rise slowly from sitting position4. Assist in ambulation.
5. If giving NTG via patch:
o avoid placing it near hairy areas-will dec drug absorptiono avoid rotating transdermal patches- will dec drug absorptiono avoid placing near microwave oven or during defibrillation-will burn pt due aluminum foil in
patch
B. Beta blockers – propranolol
C. ACE inhibitors – captopril
D. Ca antagonist - Nefedipine
3.) Administer O2 inhalation
4.) Semi-fowler
5.) Diet- Decrease Na and saturated fats
6.) Monitor VS, I&O, ECG
7.) HT: Discharge planning:
Avoid precipitating factors – 4 E’s Prevent complications – MI
12

Take meds before physical exertion-to achieve maximum therapeutic effect of drug Importance of follow-up care.
MI – MYOCARDIAL INFARCTION – heart attack – terminal stage of CAD
- Characterized by necrosis & scarring due to permanent mal-occlusion
Types:
1. Trasmural MI – most dangerous MI – Mal-occlusion of both R&L coronary artery2. Sub-endocardial MI – mal-occlusion of either R & L coronary artery
Most critical period upon dx of MI – 48 to 72h
- Majority of pt suffers from PVC premature ventricular contraction.
Predisposing factors Signs & symptoms Diagnostic Exam
1.sex – male2.black raise3.hyperlipidemia4.smoking5.HPN6.DM7.oral contraceptive
prolonged8.sedentary lifestyle9.obesity10. hypothyroidism
1. chest pain – excruciating, vice like, visceral pain located substernal or precodial area (rare)
- radiates back, arm, shoulders, axilla, jaw & abd muscles.
- not usually relived by rest r NTG
2. dyspnea
3. erthermia
4. initial increase in BP
5. mild restlessness & apprehensions
6. occasional findings
a.) split S1 & S2
b.) pericardial friction rub
c.) rales /crackles
d.) S4 (atrial gallop)
1. cardiac enzymes
a.) CPK – MB – Creatinine Phosphokinase
b.) LDH – lactic acid dehydrogenase
c.) SGPT – (ALT) – Serum Glutanic Pyruvate Transaminase- increased
d.) SGOT (AST) – Serum Glutamic Oxalo-acetic - increased
2. Troponin test – increase
3. ECG tracing – ST segment increase,
widening or QRS complexes – means arrhythmia in MI indicating PVC
4. serum cholesterol & uric acid - increase
5. CBC – increase WBC
Nursing Management
1. Narcotic analgesics – Morphine SO4 – to induce vasodilation & decrease levels of anxiety.
2. Administer O2 inhalation – low inflow (CHF-increase inflow)
3. Enforce CBR without BP
a.) Bedside commode
4. Avoid Valsalva maneuver
5. Semi fowler
13

6. General liquid to soft diet – decrease Na, saturated fat, caffeine
7. Monitor VS, I&O & ECG tracings
8. Take 20 – 30 ml/week – wine, brandy/whisky to induce vasodilation.
9. Assist in surgical; CABAG
10. Provide pt HT
a.) Avoid modifiable risk factors
b.) Prevent complications:
1. Arrhythmias – PVC
2. Shock – cardiogenic shock. Late signs of cardiogenic shock in MI – oliguria
3. thrombophlebitis - deep vein
4. CHF – left sided
5. Dressler’s syndrome – post MI syndrome
-Resistant to medications
-Administer 150,000 – 450,000 units of streptokinase
c.) Strict compliance to meds
- Vasodilators
1. NTG
2. Isordil
- Antiarrythmic
1. Lydocaine blocks release of norepenephrine
2. Brithylium
- Beta-blockers – “lol”
1. Propanolol (inderal)
- ACE inhibitors - pril
1. Captopril – (enalapril)
- Ca – antagonist
1. Nifedipine
- Thrombolitics or fibrinolytics– to dissolve clots/ thrombus
1. Streptokinase
2. Urokinase
14

3. Tissue plasminogen adjusting factor
Monitor for bleeding:
- Anticoagulants
1. Heparin 2. Coumadin – delayed reaction 2 – 3 days
PTT PT
If prolonged bleeding prolonged bleeding
Antidote- Protamine sulfate antidote Vitamin- K
- Anti platelet (aspirin)
d.) Resume ADL – sex/ activity – 4 to 6 weeks
Post-cardiac rehab
1.)Sex as an appetizer rather then dessert –
Before meals not after, due after meals increase metabolism – heart is pumping hard after meals.
2.) Position – non-weight bearing position.
When to resume sex/ act: When pt can already use staircase, then he can resume sex.
e.) Diet – decrease Na, Saturated fats, and caffeine
f.) Follow up care.
CHF – CONGESTIVE HEART FAILURE - Inability of heart to pump blood towards systemic circulation.
- Backflow
15

1.) Left sided heart failure:
Predisposing factors:
1.) 90% mitral valve stenosis – due RHD, aging
RHD affects mitral valve – streptococcal infection
Dx: - Aso titer – anti streptolysine O > 300 total units
- Steroids
- Penicillin
- Aspirin
Complication: RS-CHF
Aging – degeneration / calcification of mitral valve
Ischemic heart disease
HPN, MI, Aortic stenosis
S/Sx
Pulmonary congestion/ Edema
1. Dyspnea2. Orthopnea (Diff of breathing sitting pos – platypnea)3. Paroxysmal nocturnal dysnea – PNO- nalulunod4. Productive cough with blood tinged sputum5. Frothy salivation (from lungs)6. Cyanosis7. Rales/ crackles – due to fluid8. Bronchial wheezing 9. PMI – displaced lateral – due cardiomegaly10. Pulsus alternons – weak-strong pulse11. Anorexia & general body malaise12. S3 – ventricular gallop13.
Dx
1. CXR – cardiomegaly2. PAP – Pulmonary Arterial Pressure
PCWP – Pulmonary CapillaryWedge Pressure
PAP – measures pressure of R ventricle. Indicates cardiac status.
PCWP – measures end systolic/ diastolic pressure
PAP & PCWP:
Swan – ganz catheterization – cardiac catheterization is done at bedside at ICU
(Trachesostomy – bedside) - Done 5 – 20 mins – scalpel & trachesostomy set
CVP – indicates fluid or hydration status
Increase CVP – decrease flow rate of IV
16

Decrease CVP – increase flow rate of IV
3. Echocardiography – reveals enlarged heart chamber or cardiomayopathy
4. ABG – PCO2 increase, PO2 decrease = = hypoxemia = resp acidosis
2.) Right sided HF
Predisposing factor
1. 90% - tricuspid stenosis 2. COPD3. Pulmonary embolism4. Pulmonic stenosis5. Left sided heart failure
S/Sx
Venous congestion
- Neck or jugular vein distension- Pitting edema- Ascites- Wt gain- Hepatomegalo/ splenomegaly- Jaundice- Pruritus- Esophageal varies- Anorexia, gen body malaise
Diagnosis:
1. CXR – cardiomegaly2. CVP – measures the pressure at R atrium
Normal: 4 to 10 cm of water
Increase CVP > 10 – hypervolemia
Decrease CVP < 4 – hypovolemia
Flat on bed – post of pt when giving CVP
Position during CVP insertion – Trendelenburg to prevent pulmonary embolism & promote ventricular filling.
3. Echocardiography – enlarged heart chamber / cardiomyopathy
4.Liver enzyme
SGPT ( ALT)
SGOT AST
Nsg mgt: Increase force of myocardial contraction = increase CO
3 – 6L of CO
1. Administer meds:
17

Tx for LSHF: M – morphine SO4 to induce vasodilatation
A – aminophylline & decrease anxiety
D – digitalis (digoxin)
D - diuretics
O - oxygen
G - gases
a.) Cardiac glycosides (Increase myocardial = increase CO) - Digoxin / Antidote: digibind
b.) Loop diuretics: Lasix – effect with in 10-15 min. Max = 6 hrs
c.) Bronchodilators: Aminophillin (Theophyllin). Avoid giving caffeine
d.) Narcotic analgesic: Morphine SO4 - induce vasodilaton & decrease anxiety
e.) Vasodilators – NTG
f.) Anti-arrythmics – Lidocaine
2. Administer O2 inhalation – high! @ 3 -4L/min via nasal cannula
3. High fowlers
4. Restrict Na!
5. Provide meticulous skin care
6. Weigh Pt daily. Assess for pitting edema. Measure abdominal girth daily & notify MD
7. Monitor V/S, I&O, breath sounds
8. Institute bloodless phlebotomy. Rotating tourniquet or BP cuff rotated clockwise q 15 mins = to promote decrease venous return
9. Diet – decrease salt, fats & caffeine
10. HT:
a) Complications :shock
Arrhythmia
Thrombophlebitis
MI
Cor Pulmonale – RT ventricular hypertrophy
c.) Dietary modifications
Digoxin ( Lanoxin) 0.5 – 2.0 ng/mL
18

Digitalis toxicity includes.. N - nauseaA - anorexiaV - vomitingD - diarrheaA - abdominal pain
Digitalis toxicity is the result of the body accumulating more digitalis than it can tolerate at that time. Patient will complain visual change in color, and loss of appetite
The first sign of ARDS is increased respirations. Later comes dyspnea, retractions, air hunger, cyanosis.
Normal PCWP is 8-13. Readings of 18-20 are considered high.
First sign of PE (pulmonary embolism) is sudden chest pain, followed by dyspnea and tachypnea.
High potassium is expected with carbon dioxide narcosis (hydrogen floods the cell forcing potassium out). Carbon dioxide narcosis causes increased intracranial pressure.
Pulmonary sarcoidosis leads to right sided heart failure.
Serum Amylase: normal (25-151 units/dL)
Serum Ammonia: normal (35 to 65 mcg/dL)
Albumin level: normal (3.4 to 5 g/dL)
Serum Osmolality: normal (285 to 295 mOsm/kg) - high value indicates dehydration
Safe Suction Range: normal [Infant] 50-95 mm Hg
[Child] 95-115 mm Hg
[Adult]100-120 mm Hg)
Central Venous Pressure: < 3 mm Hg = inadequate fluid and >11 mm Hg = too much fluid
ELECTROLYTES
Potassium: 3.5-5.0 mEq/L
Sodium: 135-145 mEq/L
Calcium: 4.5-5.2 mEq/L or 8.6-10 mg/dL
Magnesium: 1.5-2.5 mEq/L
Chloride: 96-107 mEq/L
Phosphorus: 2.7 to 4.5 mg/dL
Cholesterol: 140 to 199 mg/dL
LDL: <130 mg/dL
HDL: 30 to 70 mg/dL
19

Triglycerides: <200 mg/dL
Serum creatinine: 0.6 to 1.3 mg/dL
BUN: 9-25 mg/dL
Normal CK is 26-174 U/L
Troponin I value: normal (<0.6 ng/mL)
Troponin T >0.1 to 0.2 ng/mL = MI
COAGULATION STUDIES
Partial Thromboplastin Time (aPTT): normal (20-36 seconds) therapeutic 1.5-2.5
Prothrombin Time: normal (Male: 9.6-11.8 seconds) (Female: 9.5-11.3 seconds)
International Normalized Ratio(INR): 2.0 - 3.0 for standard Coumadin therapy
3.0 – 4.5 for high-dose Coumadin therapy
Clotting time: 8 – 15 minutes
Platelet count: 150,000 to 400,000 cells/Ul
Bleeding time: 2.5 to 8 minutes
SERUM GASTROINTESTINAL STUDIES
Albumin: 3.4 to 5 g/dL
Cholesterol: 120 – 200mg/dL
Lipase: 31 -186 U/L
Lipids: 400 – 800 mg/dL
Triclycerides: Normal range: 10 – 190 mg/dL
Borderline high: 200 – 400 mg/dL
High: 400 – 1000mg/dL
Very high: greater than 1000mg.dL
Protien: 6.0 – 8.0 g/L
RENAL FUNCTION TEST
Creatinine: 0.6 – 1.3 mg/dL
Blood urea nitrogen (BUN): 5 – 20 mg/dL
Hypokalemia Assessments Hypokalemia Implementations
20

K+ < 3.5 mEq/L Muscle weakness Paresthesias Dysrhythmias Increased sensitivity to digitalis
Potassium Supplements Don’t give > 40 mEq/L into peripheral IV or without
cardiac monitor Increase dietary intake – oranges, apricots, beans,
potatoes, carrots, celery, raisins
Hyperkalemia Assessments
K+ >5.0 mEq/L EKG changes Paralysis Diarrhea Nausea
Hyperkalemia Implementations
Restrict oral intake Kayexalate Calcium Gluconate and Sodium Bircarbonate
IV Peritoneal or hemodialysis Diuretics
Hyponatremia Assessments
Na+ < 135 mEq/L Nausea Muscle cramps Confusion Increased ICP
Hyponatremia Implementations
I & O Daily weight Increase oral intake of sodium rich foods Water restriction IV Lactated Ringer’s or 0.9% NaCL
Hypernatremia Assessments
Na+ >145 mEq/L Disorientation, delusion, hallucinations Thirsty, dry, swollen tongue Sticky mucous membranes Hypotension Tachycardia
Hypernatremia Assessments
I & O Daily Weight Give hypotonic solutions: 0.45% NaCl or 5%
Dextrose in water IV
Hypocalcemia Assessments
Ca+ < 4.5 mEq/L Tetany Positive Trousseau’s sign Positive Chvostek’s sign Seizures Confusion Irritability, paresthesias
Hypocalcemia Implementations
Oral calcium supplements with orange (maximizes absorption)
Calcium gluconate IV Seizure precautions Meet safety needs
Hypercalcemia Assessments
Ca+> 5.2 mEq/L Sedative effects on CNS Muscle weakness, lack of coordination
Hypercalcemia Implementations
0.4% NaCl or 0.9% NaCl IV Encourage fluids (acidic drinks: cranberry juice) Diuretics
21

Constipation, abdominal pain Depressed deep tendon reflexes Dysrhythmias
Calcitonin Mobilize patient Surgery for hyperparathyroidism
Hypomagnesemia Assessments
Mg+< 1.5 mEq/L Neuromuscular irritability Tremors Seizures Tetany Confusion Dysphagia
Hypomagnesemia Implementations
Monitor cardiac rhythm and reflexes Test ability to swallow Seizure precautions Increase oral intake—green vegetables, nuts,
bananas, oranges, peanut butter, chocolate
Hypermagnesemia Assessments
Mg + > 2.5 mEq/L Hypotension Depressed cardiac impulse
transmission Absent deep tendon reflexes Shallow respirations
Hypermagnesemia Implementations
Discontinue oral and IV magnesium Monitor respirations, cardiac rhythm, reflexes IV Calcium to antagonize cardiac depressant
activity (helps to stimulate heart)
22