Cardio Function 2015
-
Upload
nhelia-santos-perez -
Category
Health & Medicine
-
view
564 -
download
0
Transcript of Cardio Function 2015

ASSESSMENT OF CARDIOVASCULAR FUNCTION
Nelia B Perez RN, MSPCU - MJCN
nhelzki-2014ncm-103

LECTURE OBJECTIVES
1. Review anatomy & physiology of the cardiovascular system.
2. Discuss relevant aspects of the patient history.
3. Describe physical assessment of cardiovascular status.
4. Review diagnostic procedures, tests and medications relative to the cardiovascular system.
nhelzki-2014 ncm-103



Anatomy & Physiology
Functions of the heart & CV system
• Pumps blood to tissues to supply O2 & nutrients
• Remove CO2 & metabolic wastes
(What makes it “tick”!)
nhelzki-2014 ncm-103

CARDIAC CELLS HAVE UNIQUE PROPERTIES
• AUTOMATICITY CELLS CONTRACT INDEPENDENTLY (THEY INITIATE THEIR OWN IMPULSE)
• EXCITABILITY ION SHIFT• CONDUCTIVITY TRANSMIT
IMPULSE TO ANOTHER CARDIAC CELL
• CONTRACTILITY HOW WELL THE CELL CONTRACTS
Anatomy & Physiology
nhelzki-2014 ncm-103

PERICARDIUM / PERICARDIAL SAC
• Protects heart from trauma• Serous fluid lubricates and prevents friction• Prevents heart from over filling
Anatomy & Physiology
nhelzki-2014 ncm-103

CORONARY ARTERIES
Right & Left arteries encircle the heart and supply blood to the myocardium
during ventricular relaxation( diastole)LEFT MAIN CORONARY ARTERY
L ANTERIOR DESCENDING (LAD)
L CIRCUMFLEX (LCX)RIGHT CORONARY ARTERY
POSTERIORMARGINAL
nhelzki-2014 ncm-103

CORONARY ARTERIES
(R) ARTERY
(L) ARTERY
LAD
CIRCUMFLEX
nhelzki-2014 ncm-103

CONTRACTION OF CARDIAC MUSCLE
The heart can’t pump unless an electrical stimulus occurs
Action Potential (AP) – electrical change
(depolarization = contraction)
Brought about by release of calcium
(+ charge) into cells- mechanical change
Intrinsic Pacemakers – depolarize and generate the AP
nhelzki-2014 ncm-103

CONTRACTION OF CARDIAC MUSCLE
The pacemaker with the fastest rate of depolarization stimulates the AP
• SA node (60-100 bpm)- Upper R atrium- capable of initiating electrical impulse
• AV node (40-60 bpm)- Lower R atrium• Other pacemakers ( 40 bpm)
-what can affect SA/AV node function ?
nhelzki-2014 ncm-103

1. Cardiac Innervation: ■ Sympathetic NS excitability.
■ Parasympathetic NS (vagus) excitability.
2. Effect of ions concentration in ECF: ■ Ca2+ excitability.
■ K+ excitability.
3. Physical factors:
■ temperature excitability.
■ temperature excitability.
Factors affecting myocardial excitability

4. Blood flow:
■ Insufficient bl flow to cardiac ms excitability &
myocardial metabolism for 3 reasons: (1) lack of O2,
(2) excess accumulation of CO2, &
(3) lack of sufficient food nutrients. 5. Chemical factors (drugs):
■ Digitalis excitability.
Factors affecting myocardial excitability (continued)

1. Cardiac innervation.
2. Effect of ions concentration in ECF.
3. Physical factors.
4. Blood flow.
5. Chemical factors (drugs).
Factors affecting myocardial conductivity:

1. Cardiac Innervation: ■ Sympathetic NS conductivity.
■ Parasympathetic NS (vagus) conductivity.
2. Effect of ions concentration in ECF: ■ Ca2+ conductivity.
■ K+ conductivity.
3. Physical factors:
■ temperature conductivity.
■ temperature conductivity.
Factors affecting myocardial conductivity (continued)

4. Blood flow:
■ Insufficient bl flow to cardiac ms conductivity &
myocardial metabolism for 3 reasons: (1) lack of O2,
(2) excess accumulation of CO2, &
(3) lack of sufficient food nutrients.
5. Chemical factors (drugs): ■ Digitalis conductivity.
Factors affecting myocardial conductivity (continued)

1. Cardiac innervation.
2. Oxygen supply.
3. Calcium & potassium ions concentration in ECF.
4. Physical factors.
5. Hormonal & chemical factors (drugs).
6. Mechanical factors.
Factors affecting myocardial contractility: (Inotropic effectors)

1. Cardiac Innervation: ■ Sympathetic NS force of contraction.
■ Parasympathetic NS (vagus) atrial force of contraction w no significant effect on ventricular ms.
Factors affecting myocardial contractility (continued)

2. Oxygen supply: ■ Hypoxia contractility.
3. Calcium & potassium ions concentration in ECF:
■ Ca2+ contractility. ■ K+ contractility.
4. Physical factors: ■ Warming contractility. ■ Cooling contractility.
Factors affecting myocardial contractility (continued)

5. Hormonal & chemical factors (drugs):
■ +ve inotropics: (Adrenaline, noradrenaline,
alkalosis, digitalis, Ca2+, caffeine,…)
■ -ve inotropics: (Acetylcholine, acidosis, ether,
chloroform, some bacterial toxins (e.g. diphtheria toxins), K+, …)
Factors affecting myocardial contractility (continued)

6. Mechanical factors:
a. Cardiac ms. obeys ‘all or none law’:
i.e. minimal or threshold stimuli lead to maximal cardiac contraction, because cardiac ms. behaves as a syncytium.
Factors affecting myocardial contractility (continued)

b. Cardiac ms. can’t be stimulated while it is contracted, because its excitability during contraction is zero due to long ARP, so it can’t be tetanized.
c. Cardiac ms. can perform both isometric & isotonic types of contractions.
Factors affecting myocardial contractility (continued)

d. Starling’s law of the heart:
■ “Length-tension relationship” ‘Within limits, the greater the initial length of the
fiber, the stronger will be the force of its contraction; However, overstretching the fiber as in heart
failure its power of contractility decreases’ i.e. within limits, the power of contraction is directly proportional to the initial length of the ms.
■ Cardiac ms accommodates itself (up to certain limit) to the changes in venous return.
Factors affecting myocardial contractility (continued)

e. Cardiac ms shows staircase phenomenon (gradation), if providing all other conditions kept constant.
i.e. if an isolated heart is stimulated by successive equal & effective stimuli, the 1st few contractions show a gradual in the magnitude of contraction.
Factors affecting myocardial contractility (continued)

1. Cardiac innervation.
2. Effect of ions concentration in ECF.
3. Physical factors.
4. Chemical factors (drugs).
Factors affecting myocardial rhythmicity
(chronotropic effectors):

a. Sympathetic stimuli:
Tachycardia, by spontaneous depolarization of SA- node.
How? ■ SA- node membrane permeability to K+ less K+
efflux. ■ membrane permeability to Ca2+ more Ca2+ influx.
■ As a result, the slope of depolarization , causing rate of SA- node firing & HR.
Factors affecting myocardial rhythmicity:
1. Cardiac Innervation:

b. Parasympathetic stimuli (vagus):
Bradycardia, by spontaneous depolarization of SA- node.
How? ■ SA- node membrane permeability to K+ more K+
efflux. ■ membrane permeability to Ca2+ less Ca2+ influx.
■ As a result, the prepotential slope , causing rate of SA- node firing & HR.
Factors affecting myocardial rhythmicity:1. Cardiac Innervation (continued)


a. Warming: rhythmicity.
b. Cooling: rhythmicity.
c. Exercise: HR as a result of sympathetic n. stimulation & vagal inhibition to SA- node.
d. Endurance-trained athletes: Resting bradycardia due to high vagal activity.
Factors affecting myocardial rhythmicity:
3. Physical factors:

a. Thyroid hormones & catecholamines:
rhythmicity.
b. Ach:
rhythmicity.
c. Hypoxia:
rhythmicity.
Factors affecting myocardial rhythmicity:
4. Chemical factors (drugs):

DISRUPTION IN SERUM ELECTROLYES CAN RESULT IN ALTERATION IN CARDIAC CYCLE
• Potassium
• Calcium
• Sodium
• Magnesiumnhelzki-2014 ncm-103

MONITORING MOVEMENT OF THE CARDIAC ACTION POTENTIAL (AP)
• EKG – monitors the movement of the AP, in other words, the electrical changes.
• How are the mechanical changes ( cardiac output ) monitored ?
nhelzki-2014 ncm-103

CARDIAC CYCLE CARDIAC CYCLE – all the
activities occurring in the heart during one contraction, and subsequent period of relaxation. Graphically represented on an EKG (ECG).
nhelzki-2014 ncm-103

CARDIAC CYCLE
EKG – A 12 lead EKG is a graphic record of the electrical forces produced by the heart
nhelzki-2014 ncm-103

CARDIAC CYCLEPolarized (resting) cell – represented on
EKG as baseline or isoelectric line
Depolarization – impulse over specialized cardiac cells (not neuromuscular impulse)
Repolarized cell – returns to normal. Na moves out of cell, K moves in – requires ATP
How will ischemic tissue change the cardiac cycle ?
nhelzki-2014 ncm-103

ELECTRODE POSITIONS
“LEADS”
• Leads measure electrical activity between 2 points
• Movement toward electrode causes positive deflection
• Movement away from electrode causes negative deflection
nhelzki-2014 ncm-103

ELECTRODE POSITIONS
A 12 Lead EKG shows electrical activity from 12 different positions in the heart, concentrating on (L) ventricle
A 14 Lead EKG includes (R) ventricle activity
nhelzki-2014 ncm-103

Cardiac output
• SV-• CO-• Preload-• Afterload-• Ejection fraction • GOAL is to maintain adequate MAP so
perfusion of oxygenated blood to vital organs occurs
nhelzki-2014 ncm-103

Regulation of cardiac function & BP
• Autonomic nervous system• Sympathetic norepinephrine• Parasympathetic – acetylcholine• Stimulation of adrenals by SNS –
norepinephrine• Peripheral baro receptors• Stretch receptors• chemorecptors• hormones
nhelzki-2014 ncm-103

STROKE VOLUME (SV) & CARDIAC OUTPUT (CO)
• SV – amount of blood ejected by 1 ventricle in 1 beat
• CO – volume ejected in 1 min
Control of SV and HR = SV&HR are continually adjusted by the body, and are affected by the return of blood from the tissues (think of exercise)
CO = SVxHR
nhelzki-2014 ncm-103

STROKE VOLUME (SV) & CARDIAC OUTPUT (CO)
Extrinsic control of HR is a more powerful way of controlling CO than changing SV
11 CVP causes stretching of (R) atrial muscle which stimulates SNS & HR (to help pump all the blood returned to it)
Remember “Starling’s Law”
nhelzki-2014 ncm-103


STROKE VOLUME (SV) & CARDIAC OUTPUT (CO)
2. Stretch baroreceptors (aorta & carotid) detect in pressure which stimulates SNS & HR (to ensure adequate blood supply to heart/ brain)
3. If pressure detected, then PSNS is stimulated & HR is slowed (vagus nerve) (prevents excess arterial pressure which can damage organs)
nhelzki-2014 ncm-103

CARDIAC LOAD
Preload = degree of myocardial fiber stretch at the end of diastole and just before contraction
Afterload = pressure against which ventricles must eject blood. This pressure is affected by systemic vascular resistance (SVR)
nhelzki-2014 ncm-103

nhelzki-2014 ncm-103

Blood Pressure
• Reflects the driving pressures produced by the ventricles
• Because arterial pressure is pulsatile, a single value is used to represent the overall driving pressure. This is called the mean arterial pressure.
MAP = diastolic P + 1/3(systolic P-diastolic P)
Why does diastolic pressure account for a greater proportion of the overall value?
SVR = systemic vascular resistance
CO = cardiac output
SV = stroke volume
MAP = Q x Rarterioles
Explain how these two equations are equivalent


What factors influence blood pressure?
•Blood volume
•Vascular resistance
•Autoregulation
•Autonomic influences




Regulation of Blood Pressure
• Main coordinating center is in the medulla oblongata of the brain; medullary cardiovascular control center
• Reflex control of blood pressure
•Baroreceptor reflex



Age related changes
• Decreased myocardial contractility• Thickening of endocardium & valves• Coronary arteries rigid & thickened• Decreased elasticity of vessel walls• Decreased internal diameter of vessels
nhelzki-2014 ncm-103

CARDIAC ASSESSMENT
Cardiac status of all patients should be routinely assessed. Everyone has a
1. Objective2. Subjective CP Dyspnea FatigueWhat else ?
nhelzki-2014 ncm-103

IMMEDIATE NURSING INTERVENTIONS FOR ACUTE CARDIAC EVENT MOVIE Acronym
M- Monitor for painO- O2 and pulse oxV- Vital signs I- Intravenous fluidsE- EKG monitoring
Anything else??
nhelzki-2014 ncm-103

Pain Assessment
SLIDA or
Precipitating/alleviating factors
Quality
Radiation
Severity
Timing
nhelzki-2014 ncm-103

OTHER ELEMENTS OF CARDIAC ASSESSMENT
• Previous cardiac hx• Other medical conditions that may
affect heart function• Chest injury• Previous heart surgery• Past medical hx• Medications: prescribed, OTC, herbals• Activity tolerance• Health habits• Family hx
nhelzki-2014 ncm-103

EXAMINATION
• Inspection• Palpation• Percussion-?
• Auscultation = S1, S2 at PMI
Aortic
Pulmonic
Tricuspid
Mitral
nhelzki-2014 ncm-103


Heart RhythmRegular, Irregular, Regular Irregular
Abnormal Sounds: Gallops
Murmurs
Bruits
S3 ventricular gallop – heard in early diastole
S4 atrial gallop – generally abnormal
nhelzki-2014 ncm-103

Assessment of MurmursTurbulent blood flow in valvular disorders
and septal defects
Timing of murmurs is a must!
Systolic murmurs occur between S1 & S2
Diastolic murmurs occur between
S2 & S1
Grade 1 – 6 identifies intensity of murmur
nhelzki-2014 ncm-103


nhelzki-2014 ncm-103

Other assessments• Jugular vein pressure – assess JVD
which reflects increased filling volume and pressure on (R) side of heart
JVD associated with (R) HF, SVC obstruction (Normal is 3-10cm H20)
• Pulse deficit – the difference between apical HR and peripheral pulse-associated with Afib, and heart blocks
• Pulse pressure – the difference between systolic & diastolic pressure
nhelzki-2014 ncm-103

Other assessments
• Respiratory: Lung sounds = rate, rhythm, quality, sputum
• GI-Abdomen• Peripheral Vascular:Lower extremities
nhelzki-2014 ncm-103

Diagnostic Procedures
1. EKG 12 Lead
continuous cardiac monitoring
holter monitor
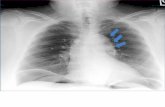
2. Chest x-ray – detects enlargement of heart & pulmonary congestion
nhelzki-2014 ncm-103

Diagnostic procedures
3. Echocardiography – ultrasound that reveals size, shape and motion of cardiac structuresEvaluates heart wall thickness, valve structure, differentiates murmurs
4. TEE – transesophageal echocardiography provides a clearer image because less tissue for sound waves to pass through
nhelzki-2014 ncm-103

Diagnostic procedures
5. Angiography / cardiac catherization
determines coronary lesion size, location, evaluate (L) ventricular function, measures heart pressures
6. Exercise tolerance test
7. Radionuclide Imaging
nhelzki-2014 ncm-103

1. Cardiac enzymes = enzymes are released when cells are damaged (MI). Enzymes are found in many tissues/muscles, and some are specific to cardiac tissue.
Serial measurement can aid in dx, and monitor course of MI
Cardiac enzymes = CPK – MB (CK-MB),myoglobin, Troponin
In general, the greater the rise in the serum level of an enzyme, the greater the degree or extent of damage to the muscle.
LDH
Lab Studies
nhelzki-2014 ncm-103

LAB studies CONT
2. Electrolytes
3. Lipid panel
4. CBC
5. C – Reactive Protein
6. BNP- Human B-Natriuretic Peptide
7. Blood coags-PT/PTT/INRnhelzki-2014 ncm-103

REVALIDATION TIME
Mary is attending a sophomore level nursing class on anatomy and physiology. Which statement, if made by Mary, demonstrates a good understanding of the anatomy and physiology of the heart?
A."The heart is encapsulated by a protective coating called the endocardium.“
B."The SA node is considered the main regulator of heart rate.“
C."The left atrium receives deoxygenated venous blood from all peripheral tissues.“
D."Stroke volume is the amount of blood ejected by the right ventricle during each diastole
nhelzki-2014 ncm-103

Kirsten is completing her graduate clinical rotation in a large urban teaching hospital in a medical coronary care unit (CCU). Which observation demonstrates a good understanding of completing a thorough cardiac examination?
• A. In an obese client, an adult cuff size of 12 to 14 cm is preferable.
• B.The carotid artery on the neck is auscultated to assess for the presence of a bruit.
• C.The apical impulse is auscultated over the fifth intercostal space in the midclavicular line.
• D.Palpation is used to determine cardiac size.
nhelzki-2014 ncm-103

Edward is a 40-year-old white male. He is an accountant who works on average 11 hours per day. He reports feeling stressed each day, even with mundane things such as a traffic jam. His father had a massive myocardial infarction at the age of 48. His mother has a history of congestive heart failure. He seldom has time to exercise, but does eat balanced meals when possible, although he does not get to eat three meals a day. Select all factors that place Edward at risk for heart disease.
• A.Family history• B.Age• C.Coping-stress tolerance• D.Race• E.Occupation
nhelzki-2014 ncm-103

Ready for more?