Cardio Advances--hyperaldosteronism in Pregnancy
-
Upload
vincesumergido -
Category
Documents
-
view
214 -
download
0
Transcript of Cardio Advances--hyperaldosteronism in Pregnancy
-
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
1/11
http://tak.sagepub.com
Therapeutic Advances in Cardiovascular Disease
DOI: 10.1177/17539447081001802009; 3; 123 originally published online Jan 26, 2009;Ther Adv Cardiovasc Dis Genevive Escher
Hyperaldosteronism in pregnancy
http://tak.sagepub.com/cgi/content/abstract/3/2/123The online version of this article can be found at:
Published by:
http://www.sagepublications.com
can be found at:Therapeutic Advances in Cardiovascular DiseaseAdditional services and information for
http://tak.sagepub.com/cgi/alertsEmail Alerts:
http://tak.sagepub.com/subscriptionsSubscriptions:
http://www.sagepub.com/journalsReprints.navReprints:
http://www.sagepub.co.uk/journalsPermissions.navPermissions:
http://tak.sagepub.com/cgi/content/refs/3/2/123Citations
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/cgi/alertshttp://tak.sagepub.com/cgi/alertshttp://tak.sagepub.com/subscriptionshttp://tak.sagepub.com/subscriptionshttp://www.sagepub.com/journalsReprints.navhttp://www.sagepub.com/journalsReprints.navhttp://www.sagepub.co.uk/journalsPermissions.navhttp://www.sagepub.co.uk/journalsPermissions.navhttp://tak.sagepub.com/cgi/content/refs/3/2/123http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/cgi/content/refs/3/2/123http://www.sagepub.co.uk/journalsPermissions.navhttp://www.sagepub.com/journalsReprints.navhttp://tak.sagepub.com/subscriptionshttp://tak.sagepub.com/cgi/alerts -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
2/11
Therapeutic Advances in Cardiovascular Disease Review
Hyperaldosteronism in pregnancy
Genevieve Escher
Abstract: Aldosterone is a key regulator of electrolyte and water homeostasis and plays acentral role in blood pressure regulation. Hormonal changes during pregnancy, among themincreased progesterone and aldosterone production, lead to the required plasma volumeexpansion of the maternal body as an accommodation mechanism for fetus growth. This reviewdiscusses the regulation of aldosterone production by aldosterone synthase (CYP11B2); theimpact on aldosterone secretion due to the presence of a chimeric gene originating froma crossover between CYP11B1 and CYP11B2 in glucocorticoid remediable aldosteronism(GRA) the inherited form of hypertension; enhanced aldosterone production in aldosterone-producing adenoma (APA); and idiopathic hyperaldosteronism (IHA). Features of hyperaldos-teronism are also found in patients with apparent mineralocorticoid excess (AME), in which
glucocorticoids exacerbate activation of the mineralocorticoid receptor (MR) because ofa defect in the 11-hydroxysteroid dehydrogenase type 2 enzyme. Regulation of aldosteroneproduction and tissue-specific activation of the mineralocorticoid receptor are prerequisitesfor optimal control of body fluids and blood pressure during pregnancy and contribute largelyto the wellbeing of the mother-to-be.
Keywords: aldosterone, pregnancy, CYP11B2, GRA, mineralocorticoid receptor
IntroductionPregnancy is a physiologic process tightly
interconnecting changes in cardiovascular, endo-
crine and renal systems [Weissgerber and Wolfe,
2006]. At an early stage of pregnancy, ovarian
steroid hormones set the basic general vasodilata-
tion that, in turn, initiates a series of regulations
in which the reninangiotensinaldosterone
system (RAS) is activated and the control of anti-
diuretic hormone secretion relative to plasma
osmolality is reset. Thus, a gradual increase in
plasma volume combined with an increase in car-
diac function allows the maintenance of blood
pressure to overcome systemic vasodilatation.
A functional arteriovenous shunt forms with the
development of the utero-placental circulation.
At the end of the first trimester, a decrease in
peripheral resistance occurs in parallel to
an increase in cardiac output, and, as a conse-
quence, blood pressure decreases and
remains low until the end of the pregnancy
[Chapman et al. 1998]. The absence of these
early events could be the cause of pre-eclampsia,
the most serious hypertensive complication of
pregnancy, characterized by the triad hyper-
tension, proteinuria and edema [Roberts and
Cooper, 2001].
Aldosterone is secreted by the adrenal gland in
response to Na
deficiency or K
loading, and
accounts for Na
retention and K
excretion in
the distal tubule and the colon. Aldosterone
binds to the mineralocorticoid receptor (MR).
This receptor was first described in Na
trans-
porting tissues, and later in a range of nonepithe-
lial tissues such as cardiomyocytes and blood
vessels [Connell and Davies, 2005]. In the renal
distal tubule, aldosterone increases Na transport
by inducing the Na
/K
ATPase via SGK-1
[Lee et al. 2008]. Na
retention leads to water
retention, and inappropriately high aldosterone
concentrations therefore result in increased
blood volume and cardiac output. Together
with a reflex vasoconstriction, there is consequent
onset of hypertension. In normal pregnancy,
plasma aldosterone concentration increases in
parallel to progesterone, and these changes are
considered normal physiological requirements
for the development of the placenta [Brown
et al. 1995]. Despite this, aldosterone remains
tightly regulated, allowing the maternal body to
overcome salt restriction or loading, and its role is
central in the maintenance of volume expansion
during pregnancy. The effect of an altered regu-
lation of aldosterone production on salt and
http://tac.sagepub.com 123
Ther Adv Cardiovasc Dis
(2009) 3(2) 123132
DOI: 10.1177/1753944708100180
The Author(s), 2009.Reprints and permissions:http://www.sagepub.co.uk/
journalsPermissions.nav
Correspondence to:Genevieve Escher, PhD
University Hospital ofBerne, Division ofNephrology and
Hypertension, Berne,Switzerlandgenevieve.escher@
dkf.unibe.ch
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
3/11
water retention is enhanced when hormonal
changes such as those seen in pregnancy occur.
In 1955, Dr Jerome Conn described the classical
syndrome of primary aldosteronism characterized
by hypertension, hypokalemia due to renal potas-sium wasting, suppressed renin activity (PRA),
and increased aldosterone levels [Conn, 1955].
Since the initial description of the syndrome, var-
ious forms of primary aldosteronism have been
described [Rossi et al. 2006]. Aldosterone-produ-
cing adenoma (APA) is the most common cause
of primary aldosteronism and occurs in about
60% of cases. Idiopathic hyperaldosteronism
(IHA), which can be associated with bilateral
micronodular or macronodular adrenal hyper-
plasia, accounts for about 40% of cases.
Glucocorticoid-remediable aldosteronism (GRA)
is a very rare familial form of hyperaldosteronism[Dluhy and Lifton, 1999]. A second form of
familial aldosteronism, familial hyperaldosteron-
ism type 2 (FHII), has also been described
[Stowasser et al. 1992] and is defined by the
recurrence of aldosteronism of any form within
a kindred that is not suppressed by dexametha-
sone-like GRA. Excessive secretion of aldosterone
is associated with an increased risk of cardiovas-
cular events. The rate of stroke, myocardial infec-
tion and atrial fibrillation is increased in patients
with primary aldosteronism [Rossi et al. 2006].
Treatment consists of an adrenalectomy, if neces-
sary, or the use of the MR antagonist spironolac-tone combined with supplementation of oral
potassium. Spironolactone was developed in the
1950s and shares structural elements with proges-
terone and androgens so that it is associated with
progestogenic and antiandrogenic side effects.
It is therefore not the drug of choice during preg-
nancy [Jeunemaitre et al . 1987]. Eplerenone,
a spironolactone derivative, was designed to
enhance selective binding to the MR. Eplerenone
has only 0.1% of the binding affinity to the
androgen receptor (AR) and less than 1% to
the progesterone receptor (PR) and thus repre-
sents a good candidate to antagonize the MRduring pregnancy.
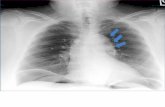
Body fluids changes and the reninangiotensinsystem in pregnancyDuring normal pregnancy, there is a marked
expansion in plasma volume starting in the first
trimester, accelerating in midgestation and
stabilizing after week 34 of gestation, as already
shown by Pirani et al . [1973] (Figure 1).
This adaptative mechanism is associated with
hemodynamic changes and correlates with
an increased concentration of circulating aldos-
terone. The composition and dynamics of body
fluids are also changed during pregnancy.
Enlargement of the fluids compartment andincrease in cardiac output occur [Longo, 1983].
Interestingly, the control mechanisms responsible
for maintaining the homeostasis accept this new
steady state in pregnancy as normal. Thus,
osmolarity thresholds for thirst sensation and
vasopressin release are reset downwards to main-
tain the effective plasma osmolarity during preg-
nancy. As a final result, there is a cumulative gain
in salt and water, enhancing placental perfusion
to protect the pregnant woman and her fetus.
Three to 5 days after administration of a low salt
diet, normal pregnant women come into balancewith significant weight loss and very little change
in plasma volume, indicating an interstitial fluid
loss. The sodium intake challenge is well toler-
ated, and little change in either weight or plasma
volume occurs. The response to an acute admin-
istration of sodium is handled appropriately and
depends on previous sodium balance. There is a
rapid sodium excretion in pregnant women
already sodium depleted, and a slower excretion
in those previously sodium depleted [Gallery and
Brown, 1987].
The appearance of an additional reninangioten-sin system (RAS) in the placenta next to the
usual one in the maternal kidney accounts for
the regulation of aldosterone production during
pregnancy. There is an early increase in circulat-
ing concentrations of renin [Pirani et al. 1973]
due to ovarian secretion and decidual
production. In the liver, an increased synthesis
of angiotensinogen is observed and attributed to
Plasmavolume(ml) 4000
3000
Weeks of pregnancy
10 20 30 40 68 weekspost-partum
Figure 1. Changes in plasma volume during gesta-tion. The dashed line represents plasma volumechanges in nonpregnant women, the black line inpregnant women.
Therapeutic Advances in Cardiovascular Disease 3 (2)
124 http://tac.sagepub.com
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
4/11
the increased circulating estrogen produced by
the growing placenta. This leads to increased
serum angiotensin II and aldosterone levels that
contribute mostly to sodium retention and the
resultant water retention required for volume
expansion in pregnancy [Gallery et al. 1979].However, the effect of angiotensin II on the
systemic vasculature; that is, an increased vaso-
motor tone, is not observed in pregnant women.
In a historic study performed by Assali and
Westersen [1961], it was shown that a two
times higher infusion rate of angiotensin II was
required to obtain the same vascular response as
in nonpregnant women. More than 10 years
later, Gant et al. [1973] showed that angiotensin
II sensitivity was downregulated during
pregnancy. These changes in angiotensin II
responsiveness in pregnancy are attributed first
to a downregulation of the AT1 receptor in thehuman placenta [Kalenga et al . 1996], and
second to progesterone that can decrease angio-
tensin II sensitivity [Gallery and Brown, 1987].
Aldosterone biosynthesisAldosterone is synthesized from cholesterol in the
adrenal zona glomerulosa by a series of reactions
(Figure 2) [Connell and Davies, 2005]. Following
translocation of cholesterol to the mitochondria
by steroidogenic acute regulatory protein
(StAR), cholesterol is converted to aldosterone
by multiple reactions catalyzed by two families
of enzymes, dehydrogenases and members of thecytochrome P450 family. The latter require adre-
nodoxin and adrenodoxin reductase for electron
transfer from the cofactor to the enzyme. First,
cholesterol is converted to pregnenolone by the
P450 side-chain cleavage enzyme (CYP11A1)
that is released to the cytosol and where it is
converted to progesterone by 3-HSD2.
Progesterone undergoes 21-hydroxylation by
CYP21A to produce 11-deoxycorticosterone
(DOC). This, in turn, is converted to aldosterone
by three successive reactions catalyzed by aldos-
terone synthase (CYP11B2) that take place
exclusively in the zona glomerulosa. First, hydro-xylation of 11-deoxycorticosterone to corticoster-
one by the 11-hydroxylase CYP11B1 takes
place; second, hydroxylation of corticosterone to
18-hydroxycorticosterone by 18-hydroxylase;
and third, methylation of 18-hydroxy-
corticosterone by 18-methyloxydase to produce
aldosterone. Since CYP11B1 also catalyses
the biosynthesis of corticosterone from DOC,
Cholesterol
Pregnenolone
Aldosterone
Corticosterone
18-OH-corticosterone
11-deoxycorticosterone
Progesterone
CYP11A1
3b-HSD2
CYP21A
CYP11B1
18-Hydroxylase
18-OxydaseAldosteronesy
nthase
(CYP11B2)
Corticosterone
CYP11B1
17-OH-pregnenolone
17-OH-progesterone
11-deoxycortisol
Cortisol
CYP17
3b-HSD2
CYP21A
Figure 2. Aldosterone biosynthesis: the CYP11B2 pathway. Zona glomerulosa is represented in orange, zonafasciculata in green.
G Escher
http://tac.sagepub.com 125
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
5/11
the late stages of cortisol and aldosterone synth-
esis are identical. CYP11B1 additionally catalyses
the formation of cortisol by hydroxylation of
11-deoxycortisol in the zona fasciculata. Thus, a
specific expression pattern of CYP11B2 and
CYP11B1 ensures the appropriate synthesis ofaldosterone and cortisol in the zona glomerulosa
and in the zona fasciculata of the adrenal gland.
The aldosterone synthase pathway can be
assessed in urine by quantifying single compo-
nents of the CYP11B2 pathway (Figure 3), and
quantification of each of these steroids as well as
detection of novel steroids are used for the clinical
diagnosis of hyperaldosteronism [Shojaati et al.
2004].
CYPB11B2 in primary hyperaldosteronismThe CYP11B2 gene, expressed in the zona glo-
merulosa of the adrenal glands, shares 90%
nucleotide sequence identity in the introns and
95% in the exons with the CYP11B1 gene
coding for the 11-hydroxylase that is essential
for cortisol synthesis. Both genes are located in
close proximity on chromosome 8q and might
have arisen from the duplication of an ancestral
gene. Despite their strong sequence homology,
they are under different regulatory mechanisms.
Whereas expression of CYP11B2 is regulated by
angiotensin II and potassium via protein kinase C
[LeHoux et al. 2000], CYP11B1 is under the
regulation of ACTH via cAMP and protein
kinase A, and this is attributed to the highly
divergent 50 upstream regions. CYP11B2
mRNA is also detected in extra-adrenal tissues
like blood vessels, heart tissue and mononuclear
leukocytes. In cardiovascular tissues, expressionofCYP11B2 is controlled by the RAS system and
potassium [Takeda et al. 1996].
The gene CYP11B2 is composed of nine exons,
and several polymorphisms have been described
in the literature so far (Figure 4). The two most
frequent polymorphisms, which are in close link-
age disequilibrium, are, first, a (344C/T) invol-
ving a C/T substitution in a putative binding site
for the steroidogenic transcription factor SF-1 in
the promoter region and, second, intron 2 con-
version, in which most of the intron of CYP11B2
is replaced by that of CYP11B1. Although the
DOC, THDOC
THB, THA
18-OH-THA
THAldo
Urinary steroid
metabolites
Hyperaldsoteronism GRA
THAldo
THAldo
THE + THF + 5a-THF18-OH-F
18-oxo-F
THAldo
Deoxycorticosterone
18-OH corticosterone
18-Oxydase
18-Hydroxylase
CYP11B2pathway
Aldosterone
Corticosterone
CYP11B1
Figure 3. CYP11B2 pathway and its corresponding urinary steroids in normal and disease state.DOC: deoxycorticosteron; THDOC: tetrahydrodeoxycorticosteron; THB: tetrahydrocorticosteron; THA:tetrahydrodehydrocorticosteron; THAldo: tetrahydroaldosteron; THE: tetrahydrocortison; THF: tetrahydro-cortisol; 18-OH-F: 18-hydroxy-cortisol; 18-oxo-F: 18-oxo-cortisol.
CYP11B2
1 2 3 4 5 6 7 8 9Promoter
3-UTR
Intron
Exon
344C/T Intron 2conversion
Figure 4. Structure of the CYP11B2 gene andlocation of the most frequent polymorphisms.
Therapeutic Advances in Cardiovascular Disease 3 (2)
126 http://tac.sagepub.com
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
6/11
(344C/T) polymorphism has been widely
studied, its clinical implications with respect to
hypertension and cardiovascular disease still
remain uncertain. Subjects with the T allele in
the SF-1 binding site have a higher urinary
aldosterone excretion rate than those lackingthis allele, raising the possibility of an increased
aldosterone synthase activity [Davies et al. 1999].
Moreover, the T allele was also reported to be
more common in hypertensive individuals in a
study performed by Brand and coworkers
[1998]. In contrast with these two studies,
Tamaki et al. [1999] reported an association
with SF-1 C allele and higher aldosterone to
renin ratios in a Japanese population. However,
SF-1 homozygote rate TT and the T allele
frequency were unusually high, suggesting
either a true genetic difference between the popu-
lations and/or sampling differences. The signifi-cance of the intron 2 conversion is unclear. It has
been suggested that intron 2 might contain reg-
ulatory elements of the CYP11B genes. The fre-
quency of the Tallele and the intron 2 conversion
allele is significantly increased in patients with
hypertension [Yu et al. 2008].
Glucocorticoid remediable aldosteronism (GRA)
is an autosomal dominant form of hypertension.
This disease is characterized by early onset of
moderate to severe hypertension with high
plasma aldosterone, suppressed plasma renin
activity and production of two rare steroids,
18-hydroxycortisol (18-OHF) and 18-oxocorti-
sol (18-oxoF) [Dluhy and Lifton, 1999]. The
incidence of premature cerebrovascular events is
high in these patients since enhanced circulating
aldosterone concentrations lead to increased left
ventricular wall thickness and reduced diastolicfunction [Stowasser et al. 2005]. In GRA, aldos-
terone secretion is mainly regulated by ACTH
rather than angiotensin II, so that administration
of ACTH exacerbates the symptoms but gluco-
corticoids normalize them. The cause of the
disease is attributed to the presence of a chimeric
gene originating from a crossover between
CYP11B1 and CYP11B2 (Figure 5). The hybrid
gene contains the promoter region of CYP11B1
at the 50 end and CYP11B2 at the 30 end, so that
this hybrid gene is ectopically expressed in the
zona fasciculata through CYP11B2 promotor,
thus exposing cortisol to aldosterone synthaseactivity. As a consequence, aldosterone,
18-hydroxy-cortisol (18-OHF), and 18-oxocorti-
sol (18-oxoF) are produced. Clinical diagnosis is
based on the detection of increased tetrahydroal-
dosterone (THAldo), 18-OHF and 18-oxoF in
urine (Figure 4). The latter two urinary steroids
are almost undetectable in urine of healthy
people. The dexamethasone suppression test is
the next step in GRA diagnosis. Since ACTH
drives abnormal steroidogenesis, 3 days of dexa-
methasone treatment switches the mechanism of
negative feedback regulation on, so that high
aldosterone levels are suppressed and 18-OHF
5 3
5 3
5 3
CYP11B1
CYP11B2
GRA
Unequal cross-over
5 3
ACTH
responsive promoter
Aldosterone production
Promotor
Australian population
Common recombination
Promotor Coding region
Coding region
Promotor Coding region
Coding region
Figure 5. Recombination of CYP11B1 and CYP11B2 in glucocorticoid remediable aldosteronism.
G Escher
http://tac.sagepub.com 127
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
7/11
and 18-oxoF concentrations in urine decrease.
However, the gold standard for GRA diagnosis
remains the detection of the chimeric gene by
long-amplification PCR [Mulatero et al. 1998].
The presence of the chimeric gene is the final
proof of GRA. In an Australian population ofGRA patients, Miyahara et al. [1992] found a
second recombination between CYP11B1 and
CYP11B2. In this case, the fusion protein is com-
posed of exons 14 of CYP11B1 with the car-
boxy-terminal part (exon 59) of CYP11B2
(Figure 5, second recombination). As recombi-
nations between CYP11B1 and CYP11B2 were
already found to occur at two different sites,
one might speculate that other recombinations
could take place and would explain the absence
of the chimeric gene when urinary steroid pattern
and dexamethasone suppression test mimic the
GRA ones.
Wyckoff et al. [2000] performed a retrospective
analysis of pregnancy outcome in 39 mothers
with GRA. Sufficient outcome information was
found for only 16. A higher risk of developing
pre-eclampsia was suspected for the following
reasons. First, since RAS is thought to play a
role in the development of pre-eclamspsia, the
dysregulation of volume homeostasis by RAS as
seen in GRA might also influence the risk of
developing pre-eclampsia. Second, the placenta
produces corticotropin-releasing hormone
[Goland et al. 1986]. As aldosterone productionis solely under the control of ACTH in GRA, one
might anticipate hyperaldosteronism exacerba-
tion during pregnancy in a GRA patient. Third,
hyperaldosteronism per se could affect the risk of
developing pre-eclampsia. Finally, GRA mothers
develop hypertension that is an additional risk for
eclampsia, regardless of the cause. Interestingly,
the conclusion of this study revealed that women
with GRA actually had no increased risk of devel-
oping pre-eclampsia. However, GRA women
with chronic hypertension were at risk of exacer-
bated hypertension during pregnancy. Blood
pressure followed the same pattern in GRA andnormal pregnant women, but the baseline was
higher in GRA. Study of pregnancy outcome of
GRA patients has provided essential information
for the clinicians caring for them.
Increased aldosterone synthase activity was mea-
sured in isolated mononuclear leukocytes (MNL)
of patients with IHA and was significantly
increased when compared with that of patients
with APA or to normal controls. This increase
correlated with increased CYP11B2 mRNA
expression in MNL [Miyamori et al . 2000].
However, no mutation was detected in the geno-
mic DNA of these patients, so that overexpres-
sion of CYP11B2 was attributed to the presence
of regulatory factors. A year later, Mulatero et al.[2001] reported that the presence of the C allele
was in excess in IHA patients when compared to
hypertensive groups with normal aldosterone
levels. In a Japanese study, however, the presence
of the T allele at (344) was considered as an
independent risk factor for hypertension
[Matsubara, 2000].
They are only few cases of IHA in pregnancy
reported in the literature. Neerhof et al. [1991]
described a severely hypertensive patient who was
treated with high doses of four antihypertensive
agents and experienced a drastic improvement inblood pressure with enalapril maleate. However,
emergency delivery at 26 weeks was performed
due to deterioration of the state of the fetus.
This example underlines the tremendous and
potentially life-threatening effect of hormonal
changes during pregnancy on blood pressure
regulation.
Oda et al. [2006] found that CYP11B2 expres-
sion was increased in RNA isolated from adrenal
tumor resection of patients with APA. If an adre-
nal tumor is diagnosed during pregnancy, surgi-
cal intervention in the second trimester has thebest outcome. Kreze et al. [1999] described the
fatal outcome of a 28-year-old woman who
refused to undergo surgery. She developed a ges-
tosis in week 27 of pregnancy and the infant died
9 days after emergency delivery. The patient later
underwent a laparoscopic adrenalectomy and
blood pressured and potassium levels normal-
ized. Solomon et al. [1996] described another
case that underwent adrenalectomy in week 15
of gestation. Following the intervention, antihy-
pertensive treatment and potassium supplemen-
tation could be withdrawn and a healthy child
was born after 36 weeks of gestation. These twoexamples emphasize the importance of fast action
upon diagnosis of APA during pregnancy.
Little is known about FHII, another familial
variety of primary aldosteronism that includes
tumors and that is not glucocorticoid-suppressi-
ble. Although the molecular basis remains
unclear, a recent linkage analysis study showed
an association with chromosomal region 7p22
[So et al. 2005].
Therapeutic Advances in Cardiovascular Disease 3 (2)
128 http://tac.sagepub.com
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
8/11
Apparent aldosterone excessUnder normal conditions, aldosterone binds with
high affinity to the mineralocorticoid receptor
(MR) to stimulate renal sodium reabsorption
and potassium excretion (Figure 6). Upon enter-
ing the cell, aldosterone binds to MR to form
the aldosteroneMR complex that moves into
the nucleus. There it binds to specific DNA-
hormone response elements sequences, thereby
altering the transcription of messenger RNA
and protein synthesis, ultimately leading to
sodium retention. In a screening of 75 hyperten-
sive patients, a mis-sense mutation resulting in
the substitution of a leucine for a serine
(S810L) in exon 6, codon 810 (MRL810) was
detected [Geller et al. 2000]. Women harboring
this mutation experienced a dramatic exacerba-
tion of hypertension during pregnancy. Later, it
was shown that MRL810 could be activated by
cortisone [Rafestin-Oblin et al. 2003] and proges-
terone, explaining why the hypertensive pheno-
type was enhanced during pregnancy.
Plasma cortisol levels are an order of magnitude
higher than those of aldosterone, and cortisol has
an equally high affinity for the MR [Funder,
2007]. Its ability to activate MR in aldosterone
target tissues is limited by 11-hydroxysteroid
dehydrogenase type 2 (11-OHSD2), the
enzyme that inactivates cortisol into cortisone
[Albiston et al. 1995]. Thus, MR is protected
from high exposure to glucocorticoids
(Figure 6). If this enzyme is blocked by carbenox-
olone or carries a loss-of-function mutation as in
the syndrome of apparent mineralocorticoid
excess, described for the first time in 1977 by
New in a three-year-old American Indian girl
[New et al. 1997], cortisol becomes an MR
agonist and mimics the effect of aldosterone.
During pregnancy, 11-OHSD2 is a major pla-
cental enzyme critically important for providing
the appropriate environment for the normal
development of the fetus. In the placenta, 11-
OHSD2 activity is upregulated during the differ-
entiation of cytotrophoblasts to syncytiotropho-
blast [Schoof et al . 2001]. Loss-of-function
mutation accounts for low birth weight, and
reduced 11-OHSD2 activity is associated with
intrauterine growth retardation [Dave-Sharma
et al. 1998]. Mutations in 11-OHSD2 could
also form part of the explanation of the high
rate of failed pregnancies found in a family with
AME [Krozowski et al. 1997].
Cardiac output
Blood pressure
MR
Progesterone
20a-OH-Progesterone
RAS
Glomerular filtration rate
Na+ retention
Plasma volume
Cortisol
Cortisone
11b-OHSD2
Aldosterone
Vasodilatation
CYP11B2
11-DOC
20a-OHSD
Figure 6. Blood pressure regulation during pregnancy. Beside aldosterone, MR occupancy is protected by11-OHSD2 and 20-OHSD enzymes to avoid excess binding and consequent sodium retention byglucocorticoids and progesterone. Progesterone also acts as an inhibitor of 11-OHSD2.
G Escher
http://tac.sagepub.com 129
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
9/11
A third steroid showing affinity for the MR exists,
namely progesterone. Despite its high affinity for
the MR in vitro, progesterone confers only a low
agonistic mineralocorticoid activity in vivo
(Figure 6) [Myles and Funder, 1996]. During
pregnancy, progesterone increases to reach a con-centration more than 100-fold higher than that of
aldosterone. The reason why aldosterone still acts
as a potent mineralocorticoid in these situations
is not fully understood. Possible explanations are,
first, a ten-fold higher plasma protein binding of
progesterone compared with aldosterone;
second, a higher stability of the aldosterone-MR
complex than the progesterone-MR complex;
and, third, local metabolism of progesterone to
20-OH-progesterone by 20-OHSD in a
mechanism similar to the protection of cortisol
by 11-OHSD2 [Quinkler et al . 2003]
(Figure 6). This protective mechanism impliesthat little MR activation should be seen in the
presence of high progesterone concentrations, in
accordance with the progressive plasma volume
expansion occurring during pregnancy. Since
20-OH-progesterone has less affinity for the
MR, one might anticipate that mutations in
20-OHSD could indirectly affect blood pressure
regulation, especially during pregnancy. The
anti-MR effect of progesterone is best illustrated
by the fact that pregnant women with Addisons
disease require increased 9-fluorocortisol sub-
stitution to maintain blood pressure and serum
potassium in normal range [Wieacker et al .
1989]. Moreover, in women with primary aldos-
teronism, serum potassium and blood pressure
often normalize during pregnancy, with recur-
rence of hypokalemia and hypertension after
delivery, when progesterone concentrations go
back to normal [Murakami et al. 2000]. The ulti-
mate proof of the in vivo anti-MR potency of
progesterone was given by Quinkler et al .
[1999]. By challenging males or postmenoposal
females with adrenal insufficiency with a contin-
uous aldosterone infusion followed by a proges-
terone infusion, he observed an increase in
urinary sodium to potassium ratio and urinary
sodium excretion during progesterone infusion,
indicating an anti-MR effect of progesterone
in vivo. This effect, however, was much weaker
than would be expected from the rise in circulat-
ing progesterone concentrations, an observation
explained, on one hand, by the enzyme-mediated
protection of the MR, and, on the other hand,
by 11-OHSD2 inhibition by progesterone
[Quinkler et al. 2003] (Figure 6).
Although MR seems to be at first nonselective,
local regulation of its occupancy by 11-OHSD2
and 20-OHSD allows its appropriate activation,
leading to adequate sodium and potassium bal-
ance within the body. Therefore, regulation of
these two enzymes plays a central role forplasma volume regulation during pregnancy,
when the maternal body is challenged with
increasing progesterone concentrations.
ConclusionThe role of aldosterone in body fluid regulation
during pregnancy and its mechanism of action via
MR are of pivotal importance for a successful
pregnancy outcome. The medical profession has
come a long way since Conn described the first
patient with primary aldosteronism. Medical
imagery and improvement of molecular biologytechniques have largely contributed to the under-
standing of the different subclasses of hyperaldos-
teronism and their underlying mechanisms. The
development of new classes of antimineralocorti-
coid agents and laparoscopic interventions
improved the wellbeing of pregnant women and
the survival rate of the fetus. Body fluids are regu-
lated during pregnancy by aldosterone as well as
by an appropriate activation state of the MR. On
a molecular level, inappropriate local activation
of the MR by glucocorticoids or progesterone
excess due to decreased 11-OHSD2 or 20-
OHSD enzyme activity, respectively, are respon-sible for sodium retention and K
excretion in
the absence of increased aldosterone plasma con-
centrations. Thus, a tiny dysregulation at the
genetic or prereceptor level leads to an alteration
of appropriate volume expansion, causing
damage on both the maternal and fetal side.
The unveiling of the underlying causes of hyper-
aldosteronism in pregnancy is a demonstration of
a successful collaborative effort of fundamental
laboratory research and clinical application.
AcknowledgmentsThis work was supported by a grant Nr 310000-
109774 from the Swiss National Science
Foundation to GE.
Conflict of interest statementNone declared.
ReferencesAlbiston, A.L., Smith, R.E., Obeyesekere, V.R. andKrozowski, Z.S. (1995) Cloning of the 11-HSD
Therapeutic Advances in Cardiovascular Disease 3 (2)
130 http://tac.sagepub.com
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
10/11
type II enzyme from human kidney, Endocr Res 21:
399409.
Assali, N.S. and Westersten, A. (1961) Regional flow-
pressure relationship in response to angiotensin in theintact dog and sheep, Circ Res 9: 189193.
Brand, E., Chatelain, N., Mulatero, P., Fery, I.,Curnow, K., Jeunemaitre, X. et al. (1998)Structural analysis and evaluation of the aldosterone
synthase gene in hypertension, Hypertension 32:
198204.
Brown, M.A., Thou, S.T. and Whitworth, J.A. (1995)
Stimulation of aldosterone by ACTH in normal andhypertensive pregnancy, Am J Hypertens 8: 260267.
Chapman, A.B., Abraham, W.T., Zamudio, S.,
Coffin, C., Merouani, A., Young, D. et al. (1998)Temporal relationships between hormonal and
hemodynamic changes in early human pregnancy,
Kidney Int 54: 20562063.
Conn, J.W. (1955) Primary aldosteronism, J Lab Clin
Med 45: 661664.
Connell, J.M. and Davies, E. (2005) The new biologyof aldosterone, J Endocrinol 186: 120.
Dave-Sharma, S., Wilson, R.C., Harbison, M.D.,
Newfield, R., Azar, M.R., Krozowski, Z.S. et al.(1998) Examination of genotype and phenotype rela-
tionships in 14 patients with apparent
mineralocorticoid excess, J Clin Endocrinol Metab 83:22442254.
Davies, E., Holloway, C.D., Ingram, M.C.,Inglis, G.C., Friel, E.C. et al. (1999) Aldosterone
excretion rate and blood pressure in essential
hypertension are related to polymorphic differences in
the aldosterone synthase gene CYP11B2, Hypertension33: 703707.
Dluhy, R.G. and Lifton, R.P. (1999) Glucocorticoid -remediable aldosteronism, J Clin Endocrinol Metab84: 43414344.
Funder, J.W. (2007) Why are mineralocorticoid
receptors so nonselective? Curr Hypertens Rep 9:
112116.
Gallery, E.D. and Brown, M.A. (1987) Control ofsodium excretion in human pregnancy, Am J KidneyDis 9: 290295.
Gallery, E.D., Hunyor, S.N. and Gyrory, A.Z. (1979)
Plasma volume contraction: a significant factor in both
pregnancy-associated hypertension (pre-eclampsia)and chronic hypertension in pregnancy, J Med 48:
593602.
Gant, N.F., Daley, G.L., Chand, S., Whalley, P.J. andMacDonald, P.C. (1973) A study of angiotensin II
pressor response throughout primigravid pregnancy,
J Clin Invest 52: 26822689.
Geller, D.S., Farhi, A., Pinkerton, N., Fradley, M.,
Moritz, M., Spitzer, A. et al. (2000) Activatingmineralocorticoid receptor mutation in hypertension
exacerbated by pregnancy, Science 289: 119123.
Goland, R.S., Wardlaw, S.L., Stark, R.I., Brown Jr,
L.S. and Frantz, A.G. (1986) High levels
of corticotropin-releasing hormone immunoactivity
in maternal and fetal plasma during pregnancy,
J Clin Endocrinol Metab 63: 11991203.
Jeunemaitre, X., Chatellier, G., Kreft-Jais, C.,
Charru, A., DeVries, C., Plouin, P.F. et al. (1987)Efficacy and tolerance of spironolactone in essential
hypertension, Am J Cardiol 60: 820825.
Kalenga, M.K., De Gasparo, M., Thomas, K. and
De Hertogh, R. (1996) Down-regulation of angioten-
sin AT1 receptor by progesterone in human placenta,
J Clin Endocrinol Metab 81: 9981002.
Kreze Jr, A., Kothaj, P., Dobakova, M. and Rohon, S.
(1999) Primary aldosteronism caused by
aldosterone-producing adenoma in pregnancy
complicated by EPH gestosis, Wien Klin Wochenschr
111: 855857.
Krozowski, Z.S., Stewart, P.M., Obeyesekere, V.R.,
Li, K. and Ferrari, P. (1997) Mutations in the11-hydroxysteroid dehydrogenase type II enzyme
associated with hypertension and possibly stillbirth,
Clin Exp Hypertens 19: 519529.
Lee, I.H., Campbell, C.R., Cook, D.I. and
Dinudom, A. (2008) Regulation of epithelial Na
channels by aldosterone: role of Sgk1, Clin Exp
Pharmacol Physiol 35: 235241.
LeHoux, J.G., Dupuis, G. and Lefebvre, A. (2000)
Regulation of CYP11B2 gene expression by protein
kinase C, Endocr Res 26: 10271031.
Longo, L.D. (1983) Maternal blood volume and
cardiac output during pregnancy: a hypothesis
of endocrinologic control, Am J Physiol 245:
R720729.
Matsubara, M. (2000) Genetic determination of
human essential hypertension, Tohoku J Exp Med
192: 1933.
Miyahara, K., Kawamoto, T., Mitsuuchi, Y., Toda, K.,
Imura, H., Gordon, R.D. et al. (1992) The chimeric
gene linked to glucocorticoid-suppressible hyperal-
dosteronism encodes a fused P-450 protein possessing
aldosterone synthase activity, Biochem Biophys ResCommun 189: 885891.
Miyamori, I., Inaba, S., Hatakeyama, H.,
Taniguchi, N. and Takeda, Y. (2000) Idiopathic
hyperaldosteronism: analysis of aldosterone synthase
gene, Biomed Pharmacother 54: 77s79s.
Mulatero, P., Schiavone, D., Fallo, F., Rabbia, F.,
Pilon, C., Chiandussi, L. et al. (2001) CYP11B2
gene polymorphisms in idiopathic hyperaldosteronism,
Hypertension 35: 694698.
Mulatero, P., Veglio, F., Pilon, C., Rabbia, F.,
Zocchi, C., Limone, P. et al. (1998) Diagnosis of
glucocorticoid-remediable aldosteronism in primary
aldosteronism: aldosterone response to dexamethasone
and long polymerase chain reaction for chimeric gene,
J Clin Endocrinol Metab 83: 25732575.
G Escher
http://tac.sagepub.com 131
by Vincent Sumergido on September 15, 2009http://tak.sagepub.comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/ -
7/29/2019 Cardio Advances--hyperaldosteronism in Pregnancy
11/11
Murakami, T., Watanabe Ogura, E., Tanaka, Y. andYamamoto, M. (2000) High blood pressure loweredby pregnancy, Lancet 356: 1980.
Myles, K. and Funder, J.W. (1996) Progesteronebinding to mineralocorticoid receptors: in vitro andin vivo studies, Am J Physiol 270: E601607.
Neerhof, M.G., Shlossman, P.A., Poll, D.S.,Ludomirsky, A. and Weiner, S. (1991) Idiopathicaldosteronism in pregnancy, Obstet Gynecol 78:489491.
New, M.I., Levine, L.S., Biglieri, E.G., Pareira, J. andUlick, S. (1977) Evidence for an unidentified steroid ina child with apparent mineralocorticoid hypertension,
J Clin Endocrinol Metab 44: 924933.
Oda, N., Takeda, Y., Zhu, A., Usukura, M.,Yoneda, T., Takata, H. et al. (2006) Pathophysiologicalroles of the adrenal renin-angiotensin system inpatients with primary aldosteronism, Hypertens Res29: 914.
Pirani, B.B., Campbell, D.M. and MacGillivray, I.(1973) Plasma volume in normal first pregnancy,
J Obstet Gynaecol Br Commonw 80: 884887.
Quinkler, M., Johanssen, S., Grossmann, C., Bahr, V.,Muller, M., Oelkers, W. et al. (1999) Progesteronemetabolism in the human kidney and inhibition of11beta-hydroxysteroid dehydrogenase type 2 byprogesterone and its metabolites, Clin Endocrinol Metab84: 41654171.
Quinkler, M., Meyer, B., Oelkers, W. andDiederich, S. (2003) Renal inactivation, mineralocor-ticoid generation, and 11beta-hydroxysteroid dehy-drogenase inhibition ameliorate theantimineralocorticoid effect of progesterone in vivo,
J Clin Endocrinol Metab 88: 37673772.
Rafestin-Oblin, M.E., Souque, A., Bocchi, B.,Pinon, G., Fagart, J. and Vandewalle, A. (2003) Thesevere form of hypertension caused by the activatingS810L mutation in the mineralocorticoid receptor iscortisone related, Endocrinology 144: 528533.
Roberts, J.M. and Cooper, D.W. (2001) Pathogenesisand genetics of pre-eclampsia, Lancet 357: 5356.
Rossi, G.P., Bernini, G., Caliumi, C., Desideri, G.,Fabris, B., Ferri, C. et al. (2006) A prospective studyof the prevalence of primary aldosteronism in1,125 hypertensive patients, J Am Coll Cardiol 48:22932300.
Schoof, E., Girstl, M., Frobenius, W.,Kirschbaum, M., Repp, R., Knerr, I. et al. (2001)Course of placental 11beta-hydroxysteroid dehydro-genase type 2 and 15-hydroxyprostaglandin
dehydrogenase mRNA expression during humangestation, Eur J Endocrinol 145: 187192.
Shojaati, K., Causevic, M., Kadereit, B., Dick, B.,Imobersteg, J., Schneider, H. et al. (2004) Evidence forcompromised aldosterone synthase enzyme activity inpreeclampsia, Kidney Int 66: 23222328.
So, A., Duffy, D.L., Gordon, R.D., Jeske, Y.W.,Lin-Su, K., New, M.I. et al. (2005) Familialhyperaldosteronism type II is linked to thechromosome 7p22 region but also shows predictedheterogeneity, Hypertens 23: 14771484.
Solomon, C.G., Thiet, M., Moore Jr, F. andSeely, E.W. (1996) Primary hyperaldosteronism inpregnancy, J Reprod Med 41: 255258.
Stowasser, M., Gordon, R.D., Tunny, T.J.,Klemm, S.A., Finn, W.L. and Krek, A.L. (1992)Familial hyperaldosteronism type II: five families witha new variety of primary aldosteronism, Clin ExpPharmacol Physiol 19: 319.
Stowasser, M., Sharman, J., Leano, R., Gordon, R.D.,Ward, G., Cowley, D. et al. (2005) Evidence forabnormal left ventricular structure and functionin normotensive individuals with familial
hyperaldosteronism type I, J Clin Endocrinol Metab90: 50705076.
Takeda, Y., Miyamori, I., Yoneda, T., Hatakeyama, H.,Inaba, S., Furukawa, K. et al. (1996) Regulation ofaldosterone synthase in human vascular endothelialcells by angiotensin II and adrenocorticotropin, J ClinEndocrinol Metab 81: 27972800.
Tamaki, S., Iwai, N., Tsujita, Y. and Kinoshita, M.(1999) Genetic polymorphism of CYP11B2gene and hypertension in Japanese, Hypertension 33:
266270.
Weissgerber, T.L. and Wolfe, L.A. (2006)Physiological adaptation in early human pregnancy:
adaptation to balance maternal-fetal demands, ApplPhysiol Nutr Metab 1: 111.
Wieacker, P., Alexopoulos, A., DeGregorio, G. andBreckwoldt, M. (1989) Pregnancy in Addisons dis-ease, Dtsch Med Wochenschr 114: 11171120.
Wyckoff, J.A., Seely, E.W., Hurwitz, S.,Anderson, B.F., Lifton, R.P. and Dluhy, R.G. (2000)Glucocorticoid-remediable aldosteronism andpregnancy, Hypertension 35: 668672.
Yu, H., Lin, S., Zhang, Y. and Liu, G. (2008) Intron-2
conversion polymorphism of the aldosteronesynthase gene and the antihypertensive response toangiotensin-converting enzyme inhibitors, J Hypertens26: 251256.
Visit SAGE journals onlinehttp://tac.sagepub.com
Therapeutic Advances in Cardiovascular Disease 3 (2)
132 http://tac.sagepub.com
by Vincent Sumergido on September 15 2009http://tak sagepub comDownloaded from
http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/http://tak.sagepub.com/















![Hyperaldosteronism new[1]](https://static.fdocuments.in/doc/165x107/556b17ddd8b42adb338b4776/hyperaldosteronism-new1.jpg)
