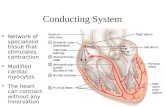
Cardiac arrhythmia. Anatomy and physiology of conduction system.
-
Upload
angel-boyle -
Category
Documents
-
view
239 -
download
3
Transcript of Cardiac arrhythmia. Anatomy and physiology of conduction system.

Cardiac arrhythmia

Anatomy and physiology of conduction system

ECG (Electrocardiogram or Electrocardiograph)

INTERPRETING THE ECG P wave: Atrial depolarization.
It is normally 2.5mm or less in height 0.11seconds or less in duration.
QRS COMPLEX: Ventricular depolarization.Less than 0.04 seconds in durationLess than 0.12 seconds in duration.
T wave : Ventricular repolarization.
U wave: Repolarization of the Purkinje fibers.

continues…..PR interval: It is measured from the beginning of
the P wave to the beginning of the QRS complex In adults, the PR interval ranges from 0.12 to 0.20
seconds. ST segment: Early ventricular repolarization,
QT interval: Total time for ventricular depolarization and repolarization. The QT interval is usually 0.32 to 0.40 seconds
TP interval: It is measured from the end of the T wave to the beginning of next P wave.

CARDIAC ARRHYTHMIA
Cardiac arrhythmia is a conduction
disorder that results in an abnormally slow or
rapid heart rate or one that dose not proceed
through the conduction system in the usual
manner.

TYPES OF ARRHYTHMIAS
1. Sinus Node Arrhythmia:a)Sinus Bradycardia: An impulse at a slower
than normal rate.Etiology:
Vagal stimulation
Drugs like calcium channel blockers, amiodaron, beta blockers.
Altered metabolic states, such as hypothyroidism.
Increased intracranial pressure (ICP).
The process of ageing,
Certain cardiac diseases, such as Myocardial Infarction.

ECG interpretation Rate: 55 Rhythm: R-R interval is
regular. P wave: present for each QRS
complex, normal configuration, and each P wave is identical.
P-R interval: falls between 0.12-0.18 seconds.
QRS complex: normal in appearance, one follows each P wave.
QRS interval: 0.04-0.08 seconds.
T wave: follows each QRS and is positively conducted.

Management:Atropine 0.5mg IV push blocks vagal stimulation to
the SA node.If the bradycardia persists, a pacemaker may be
required.

Sinus Tachycardia:Sinus tachycardia occurs when the sinus node creates an impulse at a faster than normal rate.
Etiology:Physiological and psychological stressMedications that stimulate the
sympathetic response

Continues…..
Clinical Manifestation:Tachycardia, heart rate increases,SyncopeLow blood pressureECG interpretation:Rate: 130P wave: normal configurationP-R interval: between 0.12 and
02.0 or 0.16 seconds.QRS complex: normal in
appearance, QRS interval: 0.06 seconds.T wave: is positively conducted.

Continues…. Management:
Treatment is directed towards
elimination of the cause.
Beta blockers and calcium channel
blockers, although rarely used, may be
administered to reduce the heart rate
quickly.

Atrial Arrhythmia:a) Premature Atrial Contraction: A premature
atrial complex (PAC) is a single ECG complex that occurs when an electrical impulse starts in the atrium before the next normal impulse of the sinus node.
Etiology: Stretched atrial myocardium( for example in
hypervolemia)Caffine, alcohol, nicotine, AnxietyHyperkalemia(low potassium level)Hypermetabolic states( for example with pregnancy) Atrial ischemia, injury or infarction.
Clinical Manifestation:Irregular heart rate.

Continues…
ECG interpretation:Rate & Rhythm: may be slow or fast & will be
irregular.P wave: the P wave of the premature contraction
will be distorted in shape.P-R interval: may be normal but can also be
shortened. QRS complex: with in normal limitsT wave: normally conducted.
Management:
PACs should be monitored for
increasing frequency.

Atrial FlutterIt is caused by conduction defect in the atrium & causes a rapid regular atrial rate usually between 250-400 times per minute.
Etiology:Patients with chronic obstructive pulmonary disease, valvular diseases, thyrotoxicosis, following open heart surgery & repair of congenital defects.
Clinical Manifestation:Chest painShortness of breathLow blood pressure

Continues….
ECG interpretation:Rate: 250 and 400 bpmRhythm: regular or irregularP wave:not present; instead, it is replaced by a
saw-toothed pattern . These waves are also reffered toas “F” waves.
QRS complex: normalT wave: present but may be obscured by flutter
waves.
Management:calcium channel blockerDigitalis and quinidinebeta-adrenergic blocking drugcardioversion.

Atrial fibrillationIts an uncoordinated atrial electrical activation, causes a rapid, disorganized and uncoordinated twitching of atrial musculature.
Etiology:advanced age with structural heart diseasesInflammatory or infiltrative diseases &Coronary
artery diseases.Hypertension, congenital disorder & heart failure.Diabetes, obesity, hyperthyroidism.Heavy ingestion of alcohol.Clinical Manifestation:Irregular palpitationSymptoms of heart failureHypotension, chest pain, pulmonary edema & altered
LOC

Continues….
ECG interpretation:Rate: immeasurableRhythm: irregular irregularity.P wave: replaced by fibrillatory waves, called
“little f” waves.P-R interval: not measurable.QRS complex: normalT wave: normal
Management:depends on the causes.Electrical cardioversionThe beta-adrenergic blocking drugs or calcium
ionAdenosine ( Adenocard)

Ventricular TachycardiaIt is defined as three or more premature
ventricular complexes (PVC) in a row, occurring at a rate exceeding 100 bpm.
EtiologyAcute MISyndrome of accelerated rhythm that
deteriorateMetabolic acidosisElectrolyte disturbance.Toxicity to certain drugsIntake of caffine, nicotine or alcohol.

Continues….
ECG interpretation:Rate & Rhythm : 140 and 220 bpm, regular
/irregular. P wave: not present.P-R interval: not measurable.QRS complex: broad, bizarre in configuration,
widened greater than 0.12 second.T wave: deflected opposite to the QRS complex.Management:need antiarrhythmic medications: IV procainamidelidocain used for immediate.Cardioversion

Ventricular fibrillationIts a rapid, disorganized ventricular rhythm
causes ineffective quivering of the ventricles.Etiology:
Coronary artery diseases, acute MI.
Untreated or unsuccessfully treated ventricular
tachycardia, cardiomyopathy, valvular heart diseases.
Acid-base and electrolyte abnormalities & electric
shock.
Clinical Manifestation:Absence of audible heart beat, palpable pulse,
respiration.

Continues….
ECG interpretation:
Rate: not measurable because of well-formed QRS complex.
Rhythm: Chaotic.
P wave: not present.
QRS complex: bizarre, chaotic, no definite contour.
T wave: not apparent.
Management:immediate defibrillation. If third shock is unsuccessful, begin CPR
and administer epinephrine(Adrenalin)

Ventricular Asystole:
Ventricular Asystole is commonly called flat line. Etiology: - Hypoxia - Acidosis - Severe electrolyte imbalance - Drug
overdose - Hypovolemia - Cardiac
tamponade - Coronary or pulmonary thrombosis - Trauma - Hypothermia.
Clinical Manifestation:Absence of heart beat.No palpable pulseNo respiration

Continues….
ECG interpretation:Absent QRS complexes, confirmed in two
different leads, although P wave may be apparent for a short duration.
Management:The immediate treatment is CPR.After 2 or 5 cycle CPR, a bolus of IV epinephrine
is administered and repeated at 3-5 minute intervals.
One dose of vasopressin may be administered for the first or second dose of epinephrine.A bolus of IV atropine may also be administered as soon as possible after the rhythm check.

Surgical Management:
1) CARDIAC CONDUCTION SURGERY
Indication Atrial tachycardia ventricular tachycardia
Methods Maze Procedure Catheter Ablation Therapy

Continues….
Maze Procedure: This is an open heart surgical procedure for refractory
atrial fibrillation. Small transmural incision are made through out the atria. The resulting formation of scar tissue prevents reentry conduction of the electrical impulse.
Catheter Ablation Therapy: Catheter Ablation destroy specific cells that are the
cause or central conduction route of a tachydysrrhythmia.
Ablation is by using radiofrequency, which involves placing a special catheter at or near the origin of the dysrrhythmia. High frequency, low energy sounds waves are passed through the catheter, causing thermal injury and cellular changes that result in localized destruction and scarring.

ADJUNCTIVE MODALITIES & MANAGEMENT

CARDIOVERSION & DEFIBRILLATION
Principle: an electrical current that depolarize
a critical mass of myocardial cells. When the
cell repolarize, the sinus node is usually able to
recapture its role as the heart’s pacemaker.

CARDIOVERSION
- delivery of a ‘timed’ electrical current to terminate a
tachyarrhythmia.
- the defibrillator is set to synchronize with the ECG on
cardiac monitor.
- The amount of voltage used varies from 50-360 J,
depending on the defibrillator’s technology, the type
and duration of arrhythmia.

DEFIBRILLATION
- Defibrillation is not used for patients who are
conscious or have a pulse.
- Defibrillation depolarizes a critical mass of
myocardial cells all at once; when they depolarize,
the sinus node usually recaptures its role as the
pacemaker.
- The electrical voltage required to defibrillate
the heart is usually greater than that required for
cardio version.

DIFFERENCE IN CARDIOVERSION & DEFIBRILLATION
In Cardioversion, the delivery of the
electrical current is synchronized with the
patient’s electrical events; in defibrillation, the
delivery of the current is immediate and
unsynchronized.

PACEMAKER THERAPY
A pacemaker is an electronic
device that provides electrical stimuli
to the heart muscle.
Types: Pacemakers can be permanent
or temporary.
- Temporary pacemakers are
used to support patients until they
improve or receive a permanent
pacemaker.
- Temporary pacemakers are
used only in hospital setting.

Complications of PacemakerLocal infection at the entry site
of leads for temporary pacing or
at the subcutaneous site for
permanent generator placement.
Pneumothorax.
Bleeding & hematoma
Hemothorax
pericardial effusion & rarely,
cardiac temponade.

Nursing management of patient with an implantable cardiac device:
The patient’s heart rate and rhythm are monitored by
ECG.
The incision site is observed for bleeding, hematoma
formation or infection, which may be evidenced by
swelling, unusual tenderness, drainage & increased
warmth.
A chest x-ray is usually taken after procedure.
Patient is also assessed for anxiety, depression or anger
In the perioperative & postoperative phases the nurse
carefully observes the patient & family with further
teaching as needed.

NURSES RESPONSIBILITIES: When using pads or paddles, we must observe two safety
measure.
First, good contact must be maintained between the pads
or paddles and the patient’s skin (with a conductive medium
between them) to prevent electrical current from leaking
through the air(arcing) when the defibrillator is discharged.
Second, no one is to be in contact with the patient or with
anything that is touching the patient when the defibrillator is
discharged, to minimize the chance that electrical current is
conducted to anyone other than the patient.

Other nursing care include:-
Preventing Infection:
Promoting effective coping:
Promoting home and community based care: