Cabanas & Bachman - The Impact of EMS Sepsis Care.11.16 · The Impact of EMS Sepsis Care: Data...
Transcript of Cabanas & Bachman - The Impact of EMS Sepsis Care.11.16 · The Impact of EMS Sepsis Care: Data...
The Impact of EMS Sepsis Care: Data Needs & Evaluation
Jose G. Cabanas, MD, MPH, FACEP, Medical Director Michael Bachman, EMT-P, MHS, Deputy Director of Clinical Affairs Wake County EMS
The Plan • Burden of sepsis• Changes to definitions • Review important literature• Understand data needs and challenges to evaluate impact•Wake County EMS sepsis activation process
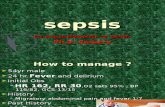
Case History• 29 y/o female S/P C-‐section, C/O -‐ fever, N/V, low back pain
EMS Findings• Temp 106.9, HR -‐ 150-‐160, Resp. Rate 30+, ETCO2 <25 (5 minutes apart)• 1200 cc fluid during transportOutcome• Septic shock from gram negative bacteremia• Dx. pyelonephritis• Did well and was D/H on hospital day 5
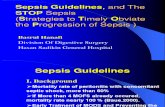
The Problem• Approx. 1M cases per/year in the US
o52% are diagnosed in the EDo35% on the hospital wardso13% in the ICU
•Mortality rate between 20-‐50%• Over $16 Billion spent every year• Clinical performance goals are not met for a high number of patients.
Angus DC. Crit Care Med. 2001;;29(7):1303-1310.
Today
>1M cases of severe sepsis/year in the US*
Future
200,000
400,000
600,000
800,000
1,000,000
1,200,000
1,400,000
1,600,000
1,800,000
2001 2025 2050
Year
100,000
200,000
300,000
400,000
500,000
600,000
Severe Sepsis Cases
US Population
Sepsis Cases
Total US Population/1,000
Incidence projected to increase by 1.5% per year
Purpose for Existence?
What is Sepsis?• Traditional definition
oLife threatening infection• 1991 & 2001 consensus conferences:
o Infection with at least 2 SIRS criteria• SIRS reflects ongoing inflammatory process
oRecent efforts to standardize definitionsoDifferentiate between sepsis from uncomplicatedinfection
Sepsis-3 Task Force• New definitions of “sepsis”
oLife-‐threatening organ dysfunction caused byan aberrant or dysregulated host response toinfection
• Recommendation to transition away from SIRS criteria in definition of sepsisoConcerns SIRS is neither sensitive nor specific
Proposal for New Definition of Septic Shock
Hypotensive (MAP < 65) after fluidsand
Vasopressors required to maintain MAPand
Lactate > 2 after adequate fluid resuscitation
Scoring Systems to predict in-hospital mortality
qSOFAAmong Patients with suspected infection• Respiratory Rate of 22 or more• GCS of 13 or less• Systolic BP of 100 mm or less2 or more of these criteria correlated
with amajor increased risk of in-‐hospital
mortality
Risk of a Bad Outcome
23% risk of a bad outcome. This is a prompt to consider that sepsis is very likely.
www.qSOFA.org
SIRS vs qSOFA
Ref -‐ http://emcrit.org/pulmcrit/problems-‐sepsis-‐3-‐definition/
SIRS and qSOFA have a similar overall test performance. qSOFA has a higher specificity than SIRS, at the cost of a lower sensitivity.
• Retrospective analysis of 2,600 patients • Mortality increased progressively with increase in the time to receipt of the first dose of antibiotic from the onset of sepsis-‐induced hypotension. • 5% to 15% decrease in survival with every hour of delay over the first 6 h.
Critical care 2006
• Community-‐based cohort of all nonarrest, nontrauma King County EMS
encounters (2000 to 2009)
• Incidence rate of severe sepsis = 3.3 per 100 EMS encounters, greater
than for AMI (2.3) or stroke (2.2) per 100 EMS encounters
• More than 40% of all severe sepsis hospitalizations arrived at the
ED after EMS transport
o 80% of cases were diagnosed on admission.
• Pre-‐hospital care intervals, on average, exceeded 45 minutes for
those hospitalized with severe sepsis.
• Prospective observational study of ED patients with severe sepsis treated with EGDT. o primary outcome was time to initiation of antibiotics
• 311 patients with 51.4% transported by EMS. o EMS patients had more organ failure (organ failure assessment score 7.0 vs. 6.1, p =0.02)
o shorter time to first antibiotics (111 vs. 146 min p=0.001)
o shorter time from triage to EGDT (119 vs. 160 min p=0.005)
• If EMS provider indicated clinical impression sepsis oshorter time to antibiotics (70 vs. 122 minutes, p=0.003) oshorter time to EGDT initiation (69 vs. 131 minutes, p=0.001)
n Feasibility of sepsis alert protocol using point-‐of-‐care lactate– EMS transported 67 severe sepsis patients
n Identified 32 of the 67 severe sepsis patients correctly (47.8%)
n Overall mortality for the sample severe sepsis patients transported by EMS was 26.7%. – Mortality for the sample of severe sepsis patients for whom the Sepsis Alert Protocol was initiated was 13.6%
Role of EMS Sepsis Care
Early recognition
Suspected infection
Sepsis AlertUtilize Screening
criteria
Fluid ResuscitationEarly Intervention
Vasopressors Refractory Hypotension
Appropriate DestinationED/ICU Care
Desired Outcome
Paramedics identify sepsis with high degree of accuracyExpedite process for sepsis patientsMeet clinical performance goalsOngoing performance Improvement
Objectives
-‐Increase Sepsis recognition-‐ Decrease morbidity/mortality -‐Immediate feedback-‐Assess overall system performance-‐Assess individual performance
Plan
-‐Use Actual cases-‐Real-‐time data exchange -‐Automated tracking-‐Educ./PI review-‐PDSA per data findings
Sepsis System of Care
EMS Systems Implementation of Sepsis Protocols• Orlando, FL• Greenville, SC• Charleston, SC• Raleigh, NC• Nashville, TN• Anchorage, AL• Columbus, OH• Broward, FL• Memphis, TN
• New York City, NY• OKC/Tulsa, OK• San Francisco, CA• Palm Beach, FL• San Diego, CA• Atlanta, GA• Albuquerque, NM• Seattle, WA• Colorado Springs, CO
Systematic Review (Limited Data)• Methodology variability across studies• The use of screening tools improves prehospital sepsis recognition • Need for validation studies to determine whether prehospital sepsis screening confer clinical benefit
Sepsis Activation Process
EMS ID of Sepsis Activation Criteria
Presence of Sepsis Activation Criteria
EHR
Need for ED Sepsis CareHospital EHR
HDE
This is a measure of EMS performance
This is a measure of criteria performance
Data Needs • Prehospital variables
oClinical assessmentoSepsis screening criteria oClinical interventions
• Receiving facilityoLinkage with prehospital recordoConfirmatory process
• Reliable feedback process for system improvement
Data Challenges• Various definitions
oCMS Sepsis MeasuresoNew Sepsis-‐3 Task Force
• No accepted US yet…• Clinical pathways across healthcare networks
oVariability across institutions •Multiple repositories of data
oPrehospitaloBillingo In-‐hospital data sources
Impact Measures• EMS System Performance
o Sensitivity, Specificity o System Process measures
• Time to recognition• Time to antibiotics • Lactate clearance
• Case feedback• Individual provider performance • Quality Reporting Measures
o CMS Sepsis Measures
EMS Sepsis AlertEMS System Activation Sepsis No Sepsis
EMS Activation True Positive (TP) False Positive (FP)
No EMS Activation False Negative (FN) True Negative (TN)
EMS Sepsis AlertEMS System Activation Sepsis No Sepsis
EMS Activation True Positive (TP) False Positive (FP)
No EMS Activation False Negative (FN) True Negative (TN)
Sensitivity Specificity
EMS Sepsis AlertEMS System Activation Sepsis No Sepsis
EMS Activation True Positive (TP) False Positive (FP)
No EMS Activation False Negative (FN) True Negative (TN)
Data integration is critical to understand system performance
CMS Sepsis Within 3 hours:• Lactate• 30mL/kg crystalloid fluids• Blood cultures • Antibiotics•Within 6 hours of presentation:• Repeat serum lactate if initial lactate is >2
• All patients with Septic Shock (as defined by CMS) require a 30 ml/kg IV bolus of crystalloid fluids• CMS allows for the prehospital fluids administered by EMS to be counted toward this total fluid requirement• There are very strict CMS documentation requirements which are currently not allowing hospitals to claim “credit” for EMS fluids
CMS Sepsis
https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier1&cid=1121785350606
CMS RequirementsFrom: Sep-‐1 Additional Notes for Abstraction, v5.0b
• Prospective cohort study among sepsis alerts activated by EMSo ≥2 SIRS criteria and ETCO2 ≤25 mmHg in patients with suspected infection
• 330 sepsis alerts, 183 met all protocol criteria. Sepsis alerts more frequently diagnosed with sepsis (78% vs 43%) severe sepsis (47% vs 7%) • Low ETCO2 levels -‐ strongest predictor and association lactate • Sepsis alerts had a sensitivity of 90% (95% CI 81-‐95%), a specificity of 58% (95% CI 52-‐65%)
Wake County EMS System Sepsis Activation Process• Early identification of patients with sepsis
o Clinical presentation + Criteria (etCO2 <26)o Declare Sepsis Alerto Fluid Resuscitation
• Receiving facilities have a clinical pathway for patients with sepsis• First aim to show feasibility of process
o Improve process and impact morbidity/mortalityo Prevent delays in recognition and treatmentoMinimize time to antibiotics
Take Away• Sepsis is a time-‐critical condition• EMS Systems have a role in recognition and early intervention• Need standardized definitions to evaluate impact• Utilize a standardized screening criteria• Build a process for system performance improvement