Arterioscler Thromb Vasc Biol-2000-Vehkavaara-545-50
description
Transcript of Arterioscler Thromb Vasc Biol-2000-Vehkavaara-545-50

Hannele Yki-JärvinenSatu Vehkavaara, Sari Mäkimattila, Anna Schlenzka, Juha Vakkilainen, Jukka Westerbacka and
Insulin Therapy Improves Endothelial Function in Type 2 Diabetes
Print ISSN: 1079-5642. Online ISSN: 1524-4636 Copyright © 2000 American Heart Association, Inc. All rights reserved.
Greenville Avenue, Dallas, TX 75231is published by the American Heart Association, 7272Arteriosclerosis, Thrombosis, and Vascular Biology
doi: 10.1161/01.ATV.20.2.5452000;20:545-550Arterioscler Thromb Vasc Biol.
http://atvb.ahajournals.org/content/20/2/545World Wide Web at:
The online version of this article, along with updated information and services, is located on the
http://atvb.ahajournals.org//subscriptions/
at: is onlineArteriosclerosis, Thrombosis, and Vascular Biology Information about subscribing to Subscriptions:
http://www.lww.com/reprints
Information about reprints can be found online at: Reprints:
document. Question and AnswerPermissions and Rightspage under Services. Further information about this process is available in the
which permission is being requested is located, click Request Permissions in the middle column of the WebCopyright Clearance Center, not the Editorial Office. Once the online version of the published article for
can be obtained via RightsLink, a service of theArteriosclerosis, Thrombosis, and Vascular Biologyin Requests for permissions to reproduce figures, tables, or portions of articles originally publishedPermissions:
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

Insulin Therapy Improves Endothelial Function inType 2 Diabetes
Satu Vehkavaara, Sari Makimattila, Anna Schlenzka, Juha Vakkilainen,Jukka Westerbacka, Hannele Yki-Jarvinen
Abstract—A total of 75 in vivo endothelial function tests (intrabrachial artery infusions of endothelium-dependent[acetylcholine] and -independent [sodium nitroprusside] vasoactive agents) were performed in 18 type 2 diabeticpatients (aged 5862 years, body mass index 28.560.6 kg/m2, and fasting plasma glucose 229611 mg/dL) and 27matched normal subjects. These tests were performed before and 6 months after combination therapy with insulin andmetformin and before and 6 months after metformin therapy only. Before insulin therapy, blood flow responses toacetylcholine (15mg/min) were significantly blunted in type 2 diabetic patients (7.560.7 mL z dL21 z min21) comparedwith normal subjects (11.660.9 mL z dL21 z min21, P,0.01). During insulin therapy, the acetylcholine responseincreased by 44% to 10.861.6 mL z dL21 z min21 (P,0.05). Insulin therapy also significantly increased the blood flowresponses to both low and high doses of sodium nitroprusside. We conclude that insulin therapy improvesendothelium-dependent and -independent vasodilatation. These data support the idea that insulin therapy has beneficialrather than harmful effects on vascular function.(Arterioscler Thromb Vasc Biol. 2000;20:545-550.)
Key Words: endotheliumn atherosclerosisn vasodilatationn insulin therapyn type 2 diabetes
The UK Prospective Diabetes Study (UKPDS) showedthat intensive blood glucose control with insulin or
sulfonylureas, both of which significantly increase circulatingfree insulin concentrations, retards the development of mi-crovascular complications.1 The incidence of myocardialinfarction decreased by 16%, which was almost statisticallysignificant (P50.052). Neither insulin nor sulfonylureas hadadverse effects on cardiovascular outcome.1 In contrast tothese drugs, a substudy of the UKPDS suggested metforminto be cardioprotective in overweight patients.2 The patientstreated with metformin were not better controlled but gainedless weight and had lower serum free insulin concentrationsthan did those treated with other regimens.2
Endothelium-dependent vasodilatation is diminished inatherosclerotic coronary arteries3,4 and characterizes patientsat risk of developing atherosclerosis, such as those withhypercholesterolemia, type 2 diabetes, and hypertension.5–7
In patients with type 2 diabetes, the impaired vasodilatorresponse to endothelium-dependent vasodilators, such asacetylcholine (ACh), has been a rather consistent finding.8–12
In addition, responses to endothelium-independent vasodila-tor agents, such as sodium nitroprusside (SNP), have beenfound to be impaired in many8,11 although not all9,13 studies.These data suggest that the function of endothelial or vascularsmooth muscle cells or both may be abnormal in type 2diabetic patients. It is also possible that inactivation ofexogenous and endogenous nitric oxide is increased.14 It iscurrently unknown, however, whether these defects are in-
herent features of type 2 diabetes or secondary to metabolicalterations such as chronic hyperglycemia,15,16 increases infree fatty acid (FFA) concentrations,17–21 or other lipidabnormalities.18,22,23 Regarding insulin, acute studies haveshown that although physiological changes in circulatinginsulin concentrations do not alter blood flow, they potentiateACh-induced vasodilatation.24 The only treatment study hith-erto performed in type 2 diabetes examined effects ofantioxidants on endothelial function.10
The present study was undertaken to determine whetherinsulin therapy changes in vivo endothelial function inpatients with type 2 diabetes. Because metformin diminishesweight gain during insulin therapy and may improve cardio-vascular outcome,25 we chose to study the effects of 6 monthsof combination therapy with insulin and metformin on endo-thelial function. These data were compared with a group ofnormal subjects and with a group of type 2 diabetic patientschronically treated with metformin.
MethodsStudy DesignIn vivo endothelial function was measured in 18 type 2 diabeticpatients previously treated with metformin (1000 mg BID, n514;500 mg BID, n54) before and 6 months after combination therapywith bedtime human isophane insulin and metformin (effect ofinsulin therapy). A control group of 27 normal subjects was studiedto determine whether endothelial function was abnormal in the type2 diabetic patients.
Received August 5, 1999; revision accepted August 5, 1999.From the Department of Medicine, Division of Endocrinology and Diabetology, Helsinki, Finland.Correspondence to Hannele Yki-Jarvinen, MD, University of Helsinki, Department of Medicine, PO Box 340, 00029 HUCH, Helsinki, Finland. E-mail
[email protected]© 2000 American Heart Association, Inc.
Arterioscler Thromb Vasc Biol.is available at http://www.atvbaha.org
545 by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

Inclusion and Exclusion CriteriaThe type 2 diabetic patients were recruited from diabetes outpatientclinics in the Helsinki area on the basis of the following criteria: (1)aged 40 through 70 years, (2) treatment with metformin alone, (3)glycosylated hemoglobin (HbA1C) .8.5% (reference range 4.0% to6.0%), (4) current body mass index,35 kg/m2, (5) duration ofdiabetes.3 years, and (6) no history of ketoacidosis. Exclusioncriteria included the following: (1) clinically significant cardiovas-cular, hepatic, neurological, endocrinologic, or other major systemicdisease, (2) retinopathy requiring laser treatment, (3) an elevatedserum creatinine concentration, (4) history of drug or alcohol abuse,and (5) mental illness rendering the subjects unable to understand thenature, scope, and possible consequences of the study. Informedwritten consent was obtained after the purpose, nature, and potentialrisks were explained to the subjects. The experimental protocol wasdesigned and performed according to the principles of HelsinkiDeclaration and was approved by the Ethical Committee of theHelsinki University Central Hospital.
Insulin TherapyPatients considered eligible to participate in the study met with thedoctor and the diabetes nurse 4 weeks before the start of insulintreatment. At this visit, the patients underwent a complete history andphysical examination. The patients were instructed to measure theirfasting blood glucose concentrations and to record any episode ofsymptomatic hypoglycemia daily. The patients then visited thelaboratory for measurement of fasting blood glucose, HbA1c, serumconcentrations of creatinine, liver enzymes, and the urinary albuminexcretion rate. An ECG was also recorded. The results of thelaboratory tests were checked, and if acceptable, an endothelialfunction test was performed before the start of insulin treatment withbedtime human isophane. Treatment with metformin was continuedwithout changing the metformin dose. The patients were taughtself-adjustment of the insulin dose on the basis of fasting plasmaglucose measurements. The patients were asked to increase the doseby 2 and 4 IU/d if the fasting plasma glucose exceeded 144 and 180mg/dL on 3 consecutive measurements. The goal was to lowerfasting plasma glucose to#108 mg/dL and HbA1c to ,7.5%.25 Thepatients visited the hospital outpatient clinic monthly for 3 monthsafter start of insulin therapy and then at 3-month intervals. Thesecond endothelial function test was performed after the outpatientvisit at 6 months.
To determine the degree of variation in endothelial functionattributable to the method and continued treatment of type 2 diabeticpatients with metformin, 6 type 2 diabetic patients who had beentreated with metformin for 1.260.4 years (6 men, aged 5362 years,body mass index 2861 kg/m2, duration of diabetes 561 years, andHbA1c 9.160.4%) were studied twice with a 6-month interval.
Measurements
In Vivo Endothelial Function TestIn vivo endothelial function was determined by measuring forearmblood flow responses to intra-arterial infusions of endothelium-dependent (ACh) and -independent (SNP) vasodilators. The studywas begun after a 10- to 12-hour fast at 7:30AM. Venous bloodsamples were withdrawn for measurement of plasma glucose andserum free insulin, HbA1C, FFA, triglyceride, HDL, and totalcholesterol concentrations. A 27-gauge unmounted steel cannula(Coopers Needle Works) connected to an epidural catheter (Portex)was inserted into the left brachial artery. Drugs were infused at aconstant rate of 1 mL/min with infusion pumps (Braun AG). Subjectsrested in a supine position in a quiet environment for 30 minutes afterneedle placement before blood flow measurements. Normal salinewas first infused for 18 minutes. Drugs were then infused in thefollowing sequence: 3 (low dose) and 10 (high dose)mg/min SNP(Roche) and 7.5 (low dose) and 15 (high dose)mg/min ACh (IolabCorp). Each dose was infused for 6 minutes, and the infusion of eachdrug was separated by infusion of normal saline for 18 minutes,during which blood flow returned to basal values. Forearm bloodflow was recorded for 10 seconds at 15-second intervals during thelast 3 minutes of each drug and saline infusion period withmercury-in-rubber strain-gauge venous occlusion plethysmography
(EC 4 Strain Gauge Plethysmograph, Hokanson), which was con-nected to a rapid cuff inflator (E 20, Hokanson), an analog-to-digitalconverter (McLab/4e, AD Instruments Pty Ltd), and a personalcomputer, as previously described.26 Blood flow measurements wereperformed simultaneously in the infused (experimental) and controlarm. Means of the final 5 measurements of each recording periodwere used for analysis. Metformin was discontinued for 2 daysbefore the endothelial function studies to avoid any acute effects onvascular function.
Other MeasurementsPlasma glucose concentrations were measured in duplicate by theglucose oxidase method27 with the use of a Beckman GlucoseAnalyzer II (Beckman Instruments). HbA1c was measured by high-performance liquid chromatography with the use of a fully auto-mated Glycosylated Hemoglobin Analyzer System (Bio-Rad). Se-rum free insulin concentrations were determined by double-antibodyradioimmunoassay (Pharmacia Insulin RIA kit) after precipitationwith polyethylene glycol.28 Urine albumin was measured by animmunoturbidimetric (Hitachi Ltd) method with the use of anantiserum against human albumin (Orion Diagnostica). Microalbu-minuria was defined as an albumin excretion rate of 20 to 200mg/min. FFA, serum total cholesterol, and triglycerides29 along withHDL cholesterol30 were measured as previously described. Whole-body fat and fat-free mass were measured by a single frequencybioelectric impedance device (model BIA-101A, Bio-Electrical Im-pedance Analyzer System, RJL Systems).31
Statistical AnalysisData between the type 2 diabetic patients and control subjects werecompared by the Student unpairedt test. Changes induced by insulintherapy in endothelial function were calculated by ANOVA forrepeated measures because treatment groups were composed of thesame subjects, as described by Ludbrook.32 Horizontal contrastswere thereafter calculated by the pairedt test with the Bonferronicorrection. Correlation analyses were performed by the Spearmannonparametric correlation coefficient. All calculations were madewith the use of the Systat statistical package. All probability valuesare 2-tailed. A value ofP,0.05 was considered statistically signif-icant. Data are expressed as mean6SEM.
ResultsGlycemic Control, Body Composition, BloodPressure, and LipidsDuring 6 months of insulin therapy, HbA1c decreased from9.060.3% to 7.660.1% (P,0.001). The bedtime insulin doseaveraged 3264 IU (range 12 to 60 IU). Fasting serum freeinsulin concentrations increased from 1161 to 1461 mU/L(P,0.05). Body weight remained unchanged during insulintherapy (mean change 1.060.6 kg,P5NS). The percentageof body fat decreased from 29.561.6% to 28.461.7%(P,0.05), and fat-free mass increased from 58.062.0% to59.662.4% (P,0.05). Serum FFAs decreased significantlyduring 6 months of insulin therapy from 746646 to574630 mmol/L (P,0.001), and serum triglycerides de-creased by 24% (P,0.01). Other lipid concentrations andblood pressure remained unchanged (Table 1).
Basal blood flow in the experimental arm was comparablebefore (2.260.2 mLz dL21 z min21) and after (2.160.2 mLzdL21 z min21) insulin therapy and was not different from thatin the normal subjects (2.260.2 mLz dL21 z min21). Bloodflows in the control arm were similar to those in theexperimental arm basally in patients with type 2 diabetes(2.160.2 and 2.060.1 mLz dL21 z min21) and normal subjects(2.060.2 mLz dL21 z min21, P5NS) throughout the study.
546 Arterioscler Thromb Vasc Biol. February 2000
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

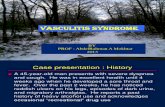
Endothelial FunctionBefore insulin therapy, blood flow during infusion of the low(6.760.6 versus 9.360.8 mLz dL21 z min21, P,0.05) andhigh (7.560.7 versus 11.660.9 mLz dL21 z min21, P,0.01)doses of ACh was significantly blunted in the type 2 diabeticpatients compared with the normal subjects. During insulintherapy, the blood flow response to the low dose of ACh didnot increase significantly, whereas that to the high dose ofACh increased by 44% (7.560.7 versus 10.861.6 mLz dL21 zmin21, before versus after;P,0.05). The responses to AChwere not different from those of the normal subjects (Figure).Forearm blood flow responses to both the low (7.860.4versus 9.160.4 mLz dL21 z min21, P,0.05) and high
(11.060.8 versus 13.060.7 mLz dL21 z min21, P,0.05) dosesof SNP also increased significantly during insulin therapy.Blood flows during SNP infusion were not significantlydifferent from those in normal subjects (Figure).
To determine the possible causes of enhanced endothelialfunctions during insulin therapy, simple correlation coeffi-cients (Spearman) were calculated between changes in met-abolic parameters and those of endothelium-dependent and-independent vasodilatation. No significant correlations wereobserved between metabolic parameters, which changed sig-nificantly during insulin therapy (HbA1C, fasting plasmaglucose, serum FFAs, serum triglycerides, and serum freeinsulin concentrations), and the absolute or relative change inblood flow during SNP and ACh infusions (Table 2).
In the type 2 diabetic patients, who were studied twice duringmetformin therapy, basal flows were comparable (2.260.2 and2.560.3 mLz dL21 z min21, P5NS). Blood flow responses to thelow (8.461.2 and 7.760.3 mL z dL21 z min21, P5NS) and high(10.862.0 and 10.562.7 mL z dL21 z min21, P5NS) doses ofSNP also remained unchanged, as did the responses to the low(7.261.0 and 7.361.1 mL z dL21 z min21, P5NS) and high(8.961.4 and 9.161.0 mL z dL21 z min21, P5NS) doses of ACh.The coefficients of variation for the 2 repeated measurements inthese patients were 1061%, 1463%, 1364%, 1062%, and1564% for infusion of saline, low-dose SNP, high-dose SNP,low-dose ACh, and high-dose ACh.
DiscussionThe present study is, to our knowledge, the first to examinethe effect of insulin therapy on endothelial function in anytype of diabetes. Before insulin therapy, endothelial functionwas impaired.8–11 Combination therapy with bedtime insulinand metformin resulted in correction of several metabolicabnormalities, including decreases in glucose, triglyceride,
Forearm blood flow responses to intra-arterial SNP and AChinfusions in type 2 diabetic patients before (F) and after (Œ)insulin therapy and in normal subjects (E). *P,0.05 for type 2diabetic patients before vs after insulin therapy. 1P,0.05 and11P,0.01 for type 2 diabetic patients vs normal subjects.
TABLE 1. Physical and Biochemical Characteristics Before and After 6 Months of InsulinTherapy in Patients With Type 2 Diabetes and in Normal Subjects
Diabetic Patients
Normal Subjects(n527)
Before Treatment(n518)
After Treatment(n518)
Sex, female/male 4/14 4/14 7/20
Age, y 5862 5962 5661
Body weight, kg 82.462.5 83.462.8 85.262.1
Body mass index, kg/m2 28.560.6 28.960.7 27.660.4
Systolic blood pressure, mm Hg 14466 14466 13166
Diastolic blood pressure, mm Hg 7962 7962 7963
Fasting plasma glucose, mg/dL 229611* 13265§ 10362
Glycosylated hemoglobin, % 9.060.3* 7.660.1§ 5.760.1
Insulin, mU/L 1161* 1461\ 661
Insulin dose, IU/kg z z z 0.3760.04 z z z
Total cholesterol, mmol/L 5.6960.27 5.4560.26 5.7360.19
LDL cholesterol, mmol/L 3.6360.18 3.6460.22 3.7560.15
HDL cholesterol, mmol/L 1.0860.04† 1.1460.03 1.3860.06
Total triglycerides, mmol/L 2.0860.25‡ 1.6060.17\ 1.3860.15
UAER, mg/min (range) 31620 (0–377) z z z 661 (0–11)
Data are mean6SEM. UAER indicates urinary albumin excretion rate.*P,0.01, †P,0.01, and ‡P,0.05 for type 2 diabetic patients before insulin therapy vs normal subjects; §P,0.01
and \P,0.05 for type 2 diabetic patients before vs after insulin therapy.
Vehkavaara et al Insulin Therapy and Endothelial Function 547
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

and FFA concentrations, and in significant improvement ofboth endothelium-dependent and -independent blood flows inforearm resistance vessels. These changes were due to acuteor chronic effects of insulin therapy rather than to metformin,in view of the fact that endothelial function remained un-changed in a control group studied twice during metformintherapy.
We chose to use combination therapy, with bedtime humanisophane and metformin as the insulin treatment regimen.This regimen improves glycemic control without inducingweight gain.25 Lack of weight gain may be beneficial duringinsulin therapy, because weight gain is associated withincreases in blood pressure and LDL cholesterol.29 In theUKPDS, patients treated with metformin gained less weightthan did those treated with other agents,2 and the UKPDS alsosuggested that metformin might be cardioprotective in over-weight patients. So far, however, it is unknown whether thedecrease in cardiovascular events in the metformin-treatedpatients was due to differences in weight gain between thevarious treatment regimens. In the present study, endothelialfunction remained unchanged when measured twice in pa-tients on chronic metformin therapy. Because the patients hadalready been treated for over a year with metformin before thefirst endothelial function test, these data do not excludepotential beneficial effects of metformin on endothelialfunction.
In all previous studies, except that of Avogaro et al,13
addressing endothelial function in type 2 diabetic patients byusing either the invasive technique used in the presentstudy8,10–12or noninvasive measurement of the brachial arterydiameter,9 endothelium-dependent vasodilatation has beenimpaired. This defect was also identified in the present study.The reason for normal endothelial function in the study ofAvogaro et al is unclear but could be due to the small numberof subjects studied (6 normal subjects and 10 patients withtype 2 diabetes). Regarding endothelium-independent butguanylate cyclase–dependent vasodilatation, endothelialfunction has been found to be either impaired8,11,12 ornormal.9,13
Multiple causes could contribute to endothelial dysfunctionin patients with type 2 diabetes compared with nondiabeticsubjects matched for age, body weight, LDL cholesterollevels, and blood pressure, as in the present study (Table 1).Such factors could include those known to be associated withincreased cardiovascular risk, such as chronic hyperglyce-mia,23 hyperinsulinemia independent of insulin resistance,33
insulin resistance, and its consequences (hypertriglyceride-mia, increased concentrations of small dense LDL particles,
low HDL cholesterol, and increases in FFA concentrations).Data on possible causes of endothelial dysfunction are sparsein previous cross-sectional studies addressing endothelialfunction in type 2 diabetic patients. We recently performed acomprehensive search for such factors and found LDL size tobe weakly correlated with endothelium-dependent vasodila-tation.34 A similar relation was also described by Watts et al11
within a group of type 2 diabetic patients. In other stud-ies,8,12,13 no significant correlations between cardiovascularrisk factors and endothelium-dependent vasodilatation havebeen identified.
Insulin therapy induces several changes that potentiallycould enhance endothelial function. Such changes includedecreases in serum triglyceride,18,35,36 FFA,17,18,21 and glu-cose37 concentrations, and all these parameters have beenassociated with endothelial function.21,35 Acute increases ininsulin concentrations also enhance ACh-induced vasodilata-tion.24 In the present study, changes in none of these param-eters during insulin therapy were significantly associated withenhanced endothelial function. Whether this reflects lack of adominant effect of a single metabolic parameter or an effectof some factor not quantified in the present study, such asgrowth and hemostatic factors and LDL size, remainsunclear.
Endothelium-independent vasodilatation, ie, vascularsmooth muscle cell–dependent vasodilatation, also increasedsignificantly during insulin therapy. Multiple factors, whichcould be either direct or indirect consequences of insulintherapy, could underlie the enhanced vascular smooth mus-cle–dependent vasodilatation. Regarding direct effects ofinsulin, insulin attenuates vascular contraction by inhibitingvoltage-dependent calcium channels38 via a mechanism thatappears coupled to the ability of insulin to increase glucosetransport in vascular smooth muscle cells.39 The ability ofinsulin to attenuate angiotensin II–mediated calcium tran-sients is blunted in cultured unpassaged vascular smoothmuscle cells in insulin-resistant spontaneously hypertensiverats.40 Insulin therapy increases in vivo insulin sensitivity ofglucose uptake in type 2 diabetic patients.17,41–43If this wouldalso happen in vascular smooth muscle, it might provide onemechanism to explain enhanced vascular smooth musclecell–dependent vasodilatation after insulin therapy. Otherpossible mechanisms include increased bioavailability ofexogenous (and endogenous) nitrates due to decreases inoxidative stress,44,45 advanced glycosylation end products,46
small dense LDL particles,22,36 and the susceptibility ofcirculating LDL to oxidation.47 Serum FFAs have also beensuggested to enhance endothelium-dependent,21 and possibly
TABLE 2. Interrelations Between Absolute and Relative Changes in Forearm Blood FlowsDuring Intrabrachial Infusions of Endothelium-Dependent (ACh) and Endothelium-Independent(SNP) Vasodilators With Changes in Metabolic Parameters
DSNP (10 mg/min) %DSNP (10 mg/min) DACh (15 mg/min) %DACh (15 mg/min)
DSerum triglycerides 20.07 20.07 20.01 0.08
DSerum FFAs 20.28 20.22 0.17 0.25
DfP glucose 20.10 20.11 20.25 20.14
DHbA1C 0.03 0.05 0.16 0.18
DfP free insulin 20.09 20.08 0.13 0.08
f P indicates fasting plasma levels.
548 Arterioscler Thromb Vasc Biol. February 2000
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

endothelium-independent,35 vasodilatation. FFAs are of inter-est because of the exquisite sensitivity of lipolysis toinsulin.17,48
To conclude, endothelium-dependent and -independentvasodilatation improves during insulin therapy. Both im-provements can be considered potentially antiatherogenic andsupport the view that insulin therapy, either via direct orindirect mechanisms, has beneficial rather than harmfuleffects on vascular function.
AcknowledgmentsThis study was supported by grants from the Academy of Finland(Drs Yki-Jarvinen and Vehkavaara), Novo-Nordisk (Dr Yki-Jarvinen), and Sigfrid Juselius (Dr Yki-Jarvinen) Foundations. Wethank Kati Tuomola and Sari Haapanen for excellent technicalassistance and the volunteers for their help.
References1. UK Prospective Diabetes Study Group. Intensive blood-glucose control
with sulphonylureas or insulin compared with conventional treatment andrisk of complications in patients with type 2 diabetes (UKPDS 33).Lancet. 1998;352:837–853.
2. Turner RC, Holman RR, Stratton IM, Cull CA, Matthews DR, ManleySE, Frighi V, Wright D, Neil A, Kohner E, Mcelroy H, Fox C, HaddenD. Effect of intensive blood-glucose control with metformin on compli-cations in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–865.
3. McLenachan JM, Williams JK, Fish RD, Ganz P, Selwyn AP. Loss offlow-mediated endothelium-dependent dilatation occurs early in thedevelopment of atherosclerosis.Circulation. 1991;84:1273–1278.
4. Siegel G, Ruckborn K, Schnalke F, Muller J. Endothelial dysfunction inhuman atherosclerotic coronary arteries.Eur Heart J. 1993;14:99–103.
5. Chowienczyk PJ, Watts GF, Cockcroft JR, Ritter JM. Impaired endothe-lium-dependent vasodilatation of forearm resistance vessels in hypercho-lesterolemia.Lancet. 1992;340:1430–1432.
6. Panza JA, Quyyumi AA, Brush JE, Epstein SE. Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension.N Engl J Med. 1990;323:22–27.
7. Cockcroft JR, Chowienczyk PJ, Benjamin N, Ritter JM. Preserved endo-thelium-dependent vasodilatation in patients with essential hypertension.N Engl J Med. 1994;330:1036–1040.
8. McVeigh GE, Brennan GM, Johnston GD, McDermott BJ, McGrath LT,Henry WR, Andrews JW, Hayes JR. Impaired endothelium-dependentand independent vasodilatation in patients with type 2 (non-insulin-dependent) diabetes mellitus.Diabetologia. 1992;35:771–776.
9. Goodfellow J, Ramsey MW, Luddington LA, Jones CJH, Coates PA,Dunstan F, Lewis MJ, Owens DR, Henderson AH. Endothelium andinelastic arteries: an early marker of vascular dysfunction in non-insulindependent diabetes.BMJ. 1996;312:744–745.
10. Ting HH, Timimi K, Boles K, Creager SJ, Ganz P, Creager MA. VitaminC improves endothelium-dependent vasodilatation in patients with non-insulin-dependent diabetes mellitus.J Clin Invest. 1996;97:22–28.
11. Watts GF, O’Brien SF, Silvester W, Millar JA. Impaired endothelium-dependent and independent dilatation of forearm resistance arteries inmen with diet-treated non-insulin-dependent diabetes: role of dyslipi-daemia.Clin Sci. 1996;91:567–573.
12. Williams SB, Cusco JA, Roddy M-A, Johnstone MT, Creager MA.Impaired nitric oxide-mediated vasodilatation in patients with non-insulin-dependent diabetes mellitus.J Am Coll Cardiol. 1996;27:567–574.
13. Avogaro A, Piarulli F, Valerio A, Miola M, Calveri M, Pavan P, ViciniP, Cobelli C, Tiengo A, Calo L, Del Prato S. Forearm nitric oxidebalance, vascular relaxation, and glucose metabolism in NIDDM patients.Diabetes. 1997;46:1040–1046.
14. Anderson TJ, Meredith IT, Ganz P, Selwyn AP, Yeung AC. Nitric oxideand nitrovasodilators: similarities, differences and potential interactions.J Am Coll Cardiol. 1994;24:555–566.
15. Tesfamariam B, Brown ML, Deykin D, Cohen RA. Elevated glucosepromotes generation of endothelium-derived vasoconstrictor prostanoidsin rabbit aorta.J Clin Invest. 1990;85:929–932.
16. Tesfamariam B, Brown ML, Cohen RA. Elevated glucose impairs endo-thelium-dependent relaxation by activating protein kinase C.J ClinInvest. 1991;87:1643–1648.
17. Taskinen M-R, Sane T, Helve E, Karonen S-L, Nikkila EA, Yki-JarvinenH. Bedtime insulin for suppression of overnight fatty-free acid, bloodglucose, and glucose production in NIDDM.Diabetes. 1989;38:580–588.
18. Taskinen M-R, Kuusi T, Helve E, Nikkila E, Yki-Jarvinen H. Insulintherapy induces antiatherogenic changes of serum lipoproteins innoninsulin-dependent diabetes.Arteriosclerosis. 1988;8:168–177.
19. Chen Y-D, Golay A, Swislocki ALM, Reaven GM. Resistance to insulinsuppression of plasma free fatty acid concentrations and insulin stimu-lation of glucose uptake in noninsulin-dependent diabetes mellitus.J ClinEndocrinol Metab. 1987;64:17–21.
20. Groop L, Bonadonna R, Ratheiser K, Zych K. Suppression of FFAturnover (TR) and FFA oxidation (OX) by insulin (I) is impaired inNIDDM. Diabetes. 1986;35:89A. Abstract.
21. Steinberg HO, Tarshoby M, Monestel R, Hook G, Cronin J, Johnson A,Bayazeed B, Baron AD. Elevated circulating free fatty acid levels impairendothelium-dependent vasodilatation.J Clin Invest. 1997;100:1230–1239.
22. Feingold KR, Grunfeld C, Pang M, Doerrler W, Krauss RM. LDLsubclass phenotypes and triglyceride metabolism in non-insulin-dependent diabetes.Arterioscler Thromb. 1992;12:1496–1502.
23. Laakso M, Lehto S, Penttila I, Pyo¨rala K. Lipids and lipoproteins pre-dicting coronary heart disease mortality and morbidity in patients withnon-insulin-dependent diabetes.Circulation. 1993;88:1421–1430.
24. Taddei S, Virdis A, Mattei P, Natali A, Ferrannini E, Salvetti A. Effect ofinsulin on acetylcholine-induced vasodilatation in normotensive subjectsand patients with essential hypertension.Circulation. 1995;92:2911–2918.
25. Yki-Jarvinen H, Ryysy L, Nikkila K, Tulokas T, Vanamo R, Heikkila¨ M.Comparison of bedtime insulin regimens in patients with type 2 diabetesmellitus.Ann Intern Med. 1999;130:389–441.
26. Makimattila S, Virkamaki A, Groop P-H, Cockcroft J, Utriainen T,Fagerudd J, Yki-Jarvinen H. Chronic hyperglycemia impairs endothelialfunction and insulin sensitivity via different mechanisms in insulin-dependent diabetes mellitus.Circulation. 1996;94:1276–1282.
27. Kadish AH, Little RL, Sternberg JC. A new and rapid method for thedetermination of glucose by measurement of rate of oxygen consumption.Clin Chem. 1968;14:116–131.
28. Desbuquois B, Aurbach GD. Use of polyethylene glycol to separate freeand antibody-bound peptide hormones in radioimmunoassay.J ClinEndocrinol Metab. 1971;33:732–738.
29. Yki-Jarvinen H, Ryysy L, Kauppila M, Kujansuu E, Lahti J, Marjanen T,Niskanen L, Rajala S, Salo S, Seppa¨la P, Tulokas T, Viikari J, TaskinenM-R. Effect of obesity on the response to insulin therapy in noninsulin-dependent diabetes mellitus.J Clin Endocrinol Metab. 1997;82:4037–4043.
30. Gidez LJ, Miller GJ, Burstein M, Eder HA. Analysis of plasma highdensity lipoprotein subclasses by a precipitation procedure: correlationwith preparative and analytical ultracentrifugation. In Lippel K, ed.Report of the High Density Lipoprotein Methodology Workshop.Bethesda, Md: US Department of Health, Education, and Welfare, PublicHealth Service, National Institutes of Health; 1998:328–340. NIH pub-lication No. 79–661.
31. Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI. Assessment offat-free mass using bioelectrical impedance measurements of the humanbody.Am J Clin Nutr. 1985;41:810–817.
32. Ludbrook J. Repeated measurements and multiple comparisons in car-diovascular research.Cardiovasc Res. 1994;28:303–311.
33. Ruige JB, Assendelft WJ, Dekker JM, Kostense PJ, Heine RJ, BouterLM. Insulin and risk of cardiovascular disease: a meta-analysis.Circu-lation. 1998;97:996–1001.
34. Makimattila S, Ming-lin L, Vakkilainen J, Schlenzka A, Lahdenpera¨ S,Syvanne M, Mantysaari M, Summanen P, Bergholm R, Taskinen M-R,Yki-Jarvinen H. Impaired endothelium-dependent vasodilatation inNIDDM: relation to LDL size, oxidized LDL and antioxidants.DiabetesCare. 1999;22:973–981.
35. Lundman P, Eriksson M, Schenck-Gustafsson K, Karpe F, Tornvall P.Transient triglyceridemia decreases vascular reactivity in young, healthymen without risk factors for coronary heart disease.Circulation. 1997;96:3266–3268.
36. Caixas A, Ordonez-Llanos J, de Leiva A, Payes A, Homs R, Perez A.Optimization of glycemic control by insulin therapy decreases the pro-portion of small dense LDL particles in diabetic patients.Diabetes.1997;46:1207–1213.
37. Williams SB, Goldfine AB, Timimi FK, Ting HK, Roddy M-A,Simonson DC, Creager MA. Acute hyperglycemia attenuates endotheli-um-dependent vasodilatation in humans in vivo.Circulation. 1998;97:1695–1701.
Vehkavaara et al Insulin Therapy and Endothelial Function 549
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from

38. Kahn AM, Seidel CL, Allen JC, O’Neil RG, Shelat H, Song T. Insulinreduces contraction and intracellular calcium concentration in vascularsmooth muscle.Hypertension. 1993;22:735–742.
39. Kahn AM, Lichtenberg RA, Allen JC, Seidel CL, Song T. Insulin-stimulated glucose transport inhibits Ca21 influx and contraction invascular smooth muscle.Circulation. 1995;92:1597–1603.
40. Touyz RM, Tolloczko B, Schiffrin EL. Insulin attenuates agonist-evokedcalcium transients in vascular smooth muscle cells.Hypertension. 1994;23:I-25–I-28.
41. Scarlett JA, Gray RS, Griffin J, Olefsky JM, Kolterman OG. Insulintreatment reverses the insulin resistance of type II diabetes mellitus.Diabetes Care. 1982;5:353–363.
42. Foley JE, Kashiwagi A, Verso MA, Reaven GM, Andrews JW.Improvement in in vitro insulin action after one month of insulin therapyin obese non-insulin-dependent diabetics.J Clin Invest. 1983;72:1901–1909.
43. Andrews WJ, Vasquez B, Nagulesparan M, Klimes I, Foley JE, Unger R,Reaven GM. Insulin therapy in obese, non-insulin-dependent diabetes
induces improvements in insulin action and secretion that are maintainedfor two weeks after insulin withdrawal.Diabetes. 1984;33:634–642.
44. Tesfamariam B, Cohen RA. Free radicals mediate endothelial cell dys-function caused by elevated glucose.Am J Physiol. 1992;263:H321–H326.
45. Hattori Y, Kawasaki H, Abe K, Kanno M. Superoxide dismutase recoversaltered endothelium-dependent relaxation in diabetic rat aorta.Am JPhysiol. 1991;261:H1086–H1094.
46. Bucala R, Tracey KJ, Cerami A. Advanced glycosylation productsquench nitric oxide and mediate defective endothelium-dependent vaso-dilatation in experimental diabetes.J Clin Invest. 1991;87:432–438.
47. Rabini RA, Fumelli P, Galassi R, Dousset N, Taus M, Ferretti G,Mazzanti L, Curatola G, Solera ML, Valdiguie P. Increased susceptibilityto lipid oxidation of low-density lipoproteins and erythrocyte membranesfrom diabetic patients.Metabolism. 1994;43:1470–1474.
48. Nurjhan N, Campbell PJ, Kennedy FP, Miles JM, Gerich JE. Insulindose-response characteristics for suppression of glycerol release andconversion to glucose in humans.Diabetes. 1986;35:1326–1331.
550 Arterioscler Thromb Vasc Biol. February 2000
by guest on September 29, 2014http://atvb.ahajournals.org/Downloaded from








![vasc dentopar[1]](https://static.fdocuments.in/doc/165x107/577c7ab51a28abe05495f271/vasc-dentopar1.jpg)