Arrhythmias, sudden cardiac death · 2020. 9. 25. · macroreentry-AVNRT, WPW sy microreentry-AS at...
Transcript of Arrhythmias, sudden cardiac death · 2020. 9. 25. · macroreentry-AVNRT, WPW sy microreentry-AS at...
-
Arrhythmias,
sudden cardiac death
Prof. Beata Mladosievicova, MD, PhD.
-
Arrhythmiasresult from abnormalities of
impulse formation
and/or
impulse propagation
-
Types of arrhythmias
Irregular - sinus arrhythmia- atrial fibrillation
Premature systoles -extrasystoles
atrialjunctionalventricular
Escape systoles - atrialjunctionalventricular
Rapid rhythmstachycardia
-atrial-AV junctional-ventricular
flutter-atrial-ventricular
fibrillation -atrial- ventricular
Blocks SA blockAV block 1.- 3. degreebundle branch block
-
Symptoms of arrhythmias
tachyarrhythmias - palpitations, chest pain, dyspnoe, syncope
bradyarrhythmias – fatigue, presyncope, syncope
-
conduction system
Arrhythmias
myocardium
-
distinguish - reversible causes of arrhythmiasin absence of heart disease
(drugs, alcohol, coffein, ANS dysbalance, electrolytes, acidosis, alcalosis,hormones)
- organic causes of arrhythmias in presence of heart diseaseaffecting CCS and/ or myocardium
-
CAD
CMP Heart failure Hypertrophy Dilation Inflammatory process Atrophy Fibrosis Edema Hemorrhage Congenital Surgery Radiotherapy Cytostatics
CCS and myocardium may be involved by:
-
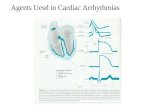
arrhythmogenic mechanism
vulnerable parameter (duration AP, conduction, excitability)
therapy (modification of ion current, receptor, CCS, myocardium)
-
abnormal automaticity (atrial tachycardia)
reentry mechanism(VT, VFi, AVNTR, AVRT, fascicular VT, AFi, AFL)
triggered activity depends on previous impulse
- during repolarisation (EAD)
- after repolarisation (DAD)
Arrhythmogenic mechanisms of tachyarrhythmias
-
Reentry
depends on refractory period and speed of conduction
concept of dual pathways
one pathway is characterised by faster conduction and longer refractory period than another
unidirectional block in one pathway
-
Dysrhythmias- supraventricular
extrasystole, tachycardia,
fibrillation and flutter.
39.
-
SVT
-
Sinus tachycardia
– Anemia
– Anxiety
– Drug intoxication/coffeine
– Hyperthyroidism
– Hypovolemia
– Infection
– Pain
– Hypoxia
– Myocardial infraction
– Heart failure
– Pulmonary embolus...
-
AV nodal reentry tachycardia
elektrophysiological dissociation – two pathways:
α pathway – slow, short RP
β pathway - fast, long RP
Atrial premature complex is conducted through αand it is blocked in β
reentry – if conduction through α is slowenough to allow to β recover excitability -
tachycardia results
Retrograde P in II,III, aVF or burried P
-
Decreased speed of conduction
inhibition of Na channels
closure of connexins in gap junctions
during ischaemia and hypoxia/anoxiaat the microscopic level
-
anatomical - fixed pathway functional - dispersion of excitability
and/or refractory period
macroreentry - AVNRT, WPW symicroreentry - AS at border zone of
scar after IM
Types of reentry
-
Accessory pathways – bypass tracts
-
Wolf-Parkinson-White sy
antegrade conductionwide QRStachycardia
-
WPW syndrome
• resulting from the presence of an
abnormal (accessory) pathway that
bypasses the AV node (Kent bundles)
between the atria and ventricles
• Wolff–Parkinson–White (WPW) pattern
on the ECG is defined by a short PR
interval and a Δ-wave reflecting early
conduction (pre-excitation):
-
ECG manifestation of accessorypathways
AP in 0.3%, AP small bounds of tissue
antegrade – with preexcitation
retrograde - without preexcitation
sometimes simultaneuosly
initiated by APC or VPC
Kent, Mahaim bypass tract
-
WPW syndrome
-
RISK of ventricular fibrillation
AFi – risk of fast conduction through bypass tract
antegrade AP - ERP less than 250 ms
higher risk !!!
-
Atrial fibrillation
Increased incidence with age
(above 75r. app. 15%)
In pts with AFi 6-fold increased risk of stroke
Every 5. pt will develop stroke
Reentry circuits esp.in dilated atria
Initiation - extrasystole
Perpetuation - longer duration, more complicatedrecovery of sinus rhythm
-
Atrial fibrillation
-
Model pathogenesis of AFi
Decreased conductionElectrolyte abnormalities
Fibrosis
Inflammation
Decreased refractery periodIncreased tonus of symp.
Thyreotoxicosis
Other factorsAlcohol
HTN
Coronary artery disease
Cardiomyopathies
Heart failure
Valvular defects (mitral stenosis)
Drugs
Pulmonary embolus
-
Classification AFiParoxyzmal
less than 48 hours
Persistentneeds intervention,longer than 48 hoursmaximally 7 days
Permanentintervention without effect
-
Clinical findings in pts with AFi
Asymptomatic
Embolic complications (brain, heart,mesenterial)
Cardiac decompensation
SymptomsStenocardial painPalpitations
Dyspnoe
Fatigue
Syncope
-
Dysrhythmias- ventricular
extrasystole, tachycardia,
fibrillation and flutter.
39.
-
Ventricular tachycardias
bellow His bundle
sustained VT (more than 30 s)
nonsustained VT (less than 30 s)
several wide ventricular complexes
100-250 beats per min
mono/polymorphic
paroxysmal/persistent
QRS duration more than 120 ms
-
Ventricular tachycardia
– Dilated cardiomyopathy
– Cardiac ischemia
– Hypoxia
– Drug toxicity
– Long QT syndrome (antipsychotics,
ATB)
– Electrolyte abnormalities
-
Extrasystole
A substrate Modifying factors
VT in context of chronic cardiac damage
-
Ventricular fibrillation -
etiology
– Acute MI (most common)
– Chronic ischemic heart disease
– Hypoxia
– Acidosis
– Anaphylaxis
– Hypokalemia
– Massive hemorrhage
-
Ventricular fibrillation
VT- VFi – SCD!!!
-
Consequences of tachyarrhythmias
LV dysfunction
reduction of blood flow in coronary aa.
embolic complications
damage of CNS
sudden cardiac death
-
Sudden cardiac death (definition, etiology, pathogenesis, arhythmogenicand non-arhythmogenic SCD).
-
SCD – natural (not by accidents, murder,suicide)
unexpected death that occurs within 1 hour aftersymptoms begin
Many sudden deaths – oftentimes within seconds and
minutes !!!
SCD – frequently in people with known or suspected
heart disease
- rare in people with no known cardiac
abnormalities
-
Sudden cardiac death is caused by decrease
in blood flow to the brain
Almost always – SCD is caused by a cardiac
arrhythmia
(ventricular tachycardia, v. fibrillation, extreme
bradycardia and heart block)
which rapidly impair the heart´s ability to pump
blood.
Vast majority will result in SCD unless CPR is
provided !!!
CHF is a more gradual process
-
Who is at risk of SCD ???
those who have survived a previous cardiac
arrest (25% risk of death per a year)
post – MI pts ( with arrhythmias or with advancedcongestive heart failure)
those with hypertrophic heart disease (high BP, genetic factors)
those with valvular heart disease (aortic stenosis)
inborn genetic disorders
medications (antihistamine allergy m., antipsychotic, ATB –Ery, antidepressants, antiarrhythmics)
-
ETIOLOGY
• Asystole (confirm in two leads)
• Ventricular fibrillation (VF)
• Pulseless ventricular tachycardia (VT)
• Consider possible reversible causes (6 Hs
and 4 Ts):
– Hypoxia, hypovolemia, hyper- and hypokalemia,
(H+), hypothermia, hypoglycemia
– Cardiac tamponade, thrombosis (pulmonary
embolism, myocardial infarction), toxins
(medications and overdoses – anabolic steroids,
cocain), trauma
-
OTHER CAUSES OF SUDDEN
DEATH
• Aortic rupture
• Abnormal coronary arteries
-
Circumstances of SCD
• death during or after exertion
• during sedentary activity
-
Conduction System
-
Life-vest wearable defibrillator