Approach to a patient with ascites
-
Upload
farwa-shabbir -
Category
Health & Medicine
-
view
80 -
download
3
Transcript of Approach to a patient with ascites
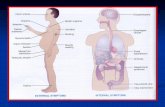
WHAT IS ASCITES?
Greek origin (askos)
and means bag or sac
It is the collection of
fluid in the peritoneal
cavity
EPIDEMIOLOGY
Mortality/Morbidity
Ambulatory patients with an episode of cirrhotic
ascites have a 3-year mortality rate of 50%. The
development of refractory ascites carries a poor
prognosis, with a 1-year survival rate of less than
50%.
Sex
Healthy men have little or no intraperitoneal fluid,
but women may normally have as much as 20
mL, depending on the phase of their menstrual
cycle.
CLASSIFICATION
Ascites exists in four grades:
Grade 1: mild, only visible on ultrasound and
CT
Grade 2: is easily detectable but of relatively
small volume.
Grade 3: detectable with flank bulging and
shifting dullness
Grade 4: directly visible, confirmed with
the fluid wave/thrill test.
ETIOLOGY
• Serum Albumin -Ascites Albumin >1.1 gm/dl
TRANSUDATIVE
• Serum Albumin -Ascites Albumin <1.1 gm/dl
EXUDATIVE
WORK UPHISTORY
AGE
child :Tuberculous ascites and nephrosis
Middle age :cirrhosis of liver
Old age : malignance
SEX
Female : meigs synd., pelvic tumours and infection and ovarian tumours
Male: alcholoism, drug abuse
ORDER OF DEVELPOMENT
cardiac causes : Leg oedema precedes ascites
Kidney causes : Puffiness of face precedes ascites
Cirrhosis of liver : Ascites is the first feature
LABORATORY ANALYSIS
DIAGNOSTIC PERITONEAL TAP
Inspection:
Most ascitic fluid is transparent and tinged yellow.
more than 20,000 red blood cells/µL will produce
distinctly blood-tinged fluid. This may result from
either a traumatic tap or malignancy
Cloudy ascitic fluid with a purulent consistency
indicates infection.
Cell count:
Normal ascitic fluid contains fewer than 500
leukocytes/µL and fewer than 250
polymorphonuclear leukocytes (PMNs)/µl
A PMN count of greater than 250 cells/µL is highly
suggestive of bacterial peritonitis
In tuberculous peritonitis and peritoneal
carcinomatosis, lymphocytes usually
predominate.
SAAG:
SAAG is the best single test for classifying
ascites into portal hypertensive (SAAG >1.1 g/dL)
and non–portal hypertensive (SAAG < 1.1 g/dL)
Culture/Gram stain:
Culture has a 92% sensitivity for the detection of
bacteria in ascitic fluid
In contrast, Gram stain is only 10% sensitive for
visualizing bacteria in early-detected
spontaneous bacterial peritonitis
Cytology:
Cytology smears are reported to be 58-75%
sensitive for detection of malignant ascites.
IMAGING STUDIES
Ultrasonography:
Volumes as small as 5-
10 mL can routinely be
visualized.
With massive ascites,
the small bowel loops
have a characteristic
polycyclic, "lollipop,"
appearance
The smallest amounts
of fluid tend to collect in
the Morison pouch and
around the liver as a
sonolucent band
Certain ultrasonographic findings suggest that the
ascites may be infected, inflammatory, or
malignant. These findings include coarse internal
echoes (blood), fine internal echoes (chyle),
multiple septa (tuberculous peritonitis,
pseudomyxoma peritonei)
In malignant ascites, the bowel loops do not float
freely but may be tethered along the posterior
abdominal wall, plastered to the liver or other
organs, or surrounded by loculated fluid
collections.
The thickening of the gallbladder is primarily a
reflection of cirrhosis and portal hypertension.
CT Scan:
Ascites is
demonstrated well on
CT scan.
A number of CT scan
features suggest
neoplasia. Hepatic,
adrenal, splenic, or
lymph node lesions
associated with
masses arising from
the gut, ovary, or
pancreas are
suggestive of
malignant ascites.
Salt restriction
Diuretics1. Spironolactone
(Aldactone)
2. Furosemide
(Lasix)
3. Amiloride
(Midamor)
4. Mannitol
(Osmitrol)
transjugular
intrahepatic
portosystemic
shunt (TIPS)