Ascites guidebased
-
Upload
rainmaker77771121 -
Category
Documents
-
view
237 -
download
0
description
Transcript of Ascites guidebased

Ascites in Cirrhosis
AASLD guidelines 2012 update


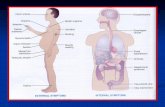
Ascites
• 80% CLD, 5% mixed, 15% other
• Important landmark - poor prognosis– 19% 1 year mortality– 44% 5 year mortality

Diagnosis
• Clinically detected when 1500cc is present
• Shifting dullness 83% sensitivity and 56%
specificity in detecting ascites.
• Confirmation – abnormal ultrasound or
paracentesis

Paracentesis
• Rapid, cost effective• Can detect and confirm infection• Complications rare – bleeding <1/1000– Higher in the setting of renal impairment
• Correction of platelets and INR – no proven benefit hemorrhagic complications despite a) no prophylactic transfusions, b) platelet counts as low as 19,000 cells/mm3 (19 106/L)(54% <50,000) and c) international normalized ratios for prothrombin time as high as 8.7 (75% >1.5 and 26.5% >2.0) 1
1Grabau, Catherine M., et al. "Performance standards for therapeutic abdominal paracentesis." Hepatology 40.2 (2004): 484-488.

Paracentesis
• Site …• 2 finger breadths (3
cm) cephalad and 2 finger breadths medial to the anterior superior iliac spine

Recommendations
1. Diagnostic abdominal paracentesis should be performed and ascitic fluid should be obtained from inpatients and outpatients with clinically apparent new-onset ascites. (Class I, Level C)
2. Since bleeding is sufficiently uncommon, the routine prophylactic use of fresh frozen plasma or platelets before paracentesis is not recommended.(Class III, Level C)

Tests to be performed
• Routine : cell count, protein, SAAG• ? Infection :– Culture, glucose, LHD, gram stain
• ? Tuberculosis• Unusual tests: pH, bilirubin,

Recommendations
3. The initial laboratory investigation of ascitic fluid should include an ascitic fluid cell count and differential, ascitic fluid total protein, and SAAG.(Class I, Level B)

Recommendations
4. If ascitic fluid infection is suspected, ascitic fluid should be cultured at the bedside in aerobic and anaerobic blood culture bottles prior to initiation of antibiotics. (Class I, Level B)5. Other studies of ascitic fluid can be ordered based on the pretest probability of disease (Class IIa, Level C)

Recommendations
6. Testing serum for CA125 is not helpful in the differential diagnosis of ascites. Its use is not recommended in patients with ascites of any type. (Class III, Level B)


Recommendation
9. First-line treatment of patients with cirrhosis and ascites consists of sodium restriction (88 mmol per day [2000 mg per day], diet education,) and diuretics (oral spironolactone with or without oral furosemide). (Class IIa, Level A)

Alcohol cessation
• Most important • Child Pugh C : 3 year survival– Abstinence 75% vs continuous users 0%
• Baclofen

Diuretics
• Spiranolactone (100mg)• Furosemide (40mg) – risks of IV treatment• Dual therapy• Amiloride (no gynecomastia) – less effective• Withheld in the setting of active gastrointestinal
bleeding, hepatic encephalopathy, Na<120 or renal dysfunction
• Weight loss - rate

Albumin
• Therapeutic: An unblinded randomized controlled trial in patients with new onset ascites demonstrates that weekly 25 g infusions of albumin for 1 year followed by infusions every 2 weeks improved survival compared to diuretics alone.
• With paracentesis: A meta-analysis of 17 trials involving 1225 patients has been published, demonstating a reduction in mortality with an odds ratio of death of 0.64 (95% CI, 0.41-0.98) in the albumin group.

Less evidence for…
• Vasopressin receptor antagonists• Bed rest• Fluid restriction in the absence of severe
hyponatraemia

What to avoid…
• Blood pressure in patients with cirrhosis and ascites is supported by elevated levels of vasoconstrictors; these vasoconstrictors are compensating for the vasodilatory effect of nitric oxide
• Arterial pressure independently predicts survival in patients with cirrhosis; those with a mean arterial pressure (MAP) >82 mmHg have a 1-year survival of 70%, compared to 40% for those ≤82 mmHg1.
1Llach J, Gines P, Arroyo V, Rimola A, Tito L, Badalamenti S, Jimenez W, et al. Prognostic value of arterial pressure, endogenous vasoactive systems, and renal function in cirrhotic patients admitted to the hospital for the treatment of ascites. Gastroetnerology 1988;94:482-487.

Avoid..
• ACEIs and ARBs should be avoided or used with caution in patients with cirrhosis and ascites.
• Propranolol – refractory ascites, RF• NSAIDs – Na retention, RF

Special situations
Tense ascites• Single large volume paracentesis– 5l without colloids– Thereafter : albumin 8g per liter of fluid removed
–Start other modalities of treatment ..

Failure of diuretic therapy
(1) Minimal response + inadequate (<78 mmol per day) urinary Na+ excretion despite diuretics or(2) development of clinically significant complications of diuretics( e.g., encephalopathy, serum creatinine greater than 2.0 mg/dL, serum sodium less than 120 mmol/L, or serum potassium greater than 6.0 mmol/L)

Refractory ascites
• Fuid overload that – (1) is unresponsive to sodium-restricted diet and high
dose diuretic treatment (400 mg per day of spironolactone and 160 mg per day furosemide), or
– (2) recurs rapidly after therapeutic paracentesis

Refractory ascites - Rx
• Stop beta blcokers• Midodrine• TIPS• Serial paracentesis• Peritoneovenous shunt

Thank you