An evaluation of five different dressing materials on split ... · four female Sprague-Dawley rats...
Transcript of An evaluation of five different dressing materials on split ... · four female Sprague-Dawley rats...
International Wound Journal ISSN 1742-4801
O R I G I N A L A R T I C L E
An evaluation of five different dressing materials onsplit-thickness skin graft donor site and full-thicknesscutaneous wounds: an experimental studyMuhammet Uraloglu1, Murat Livaoglu1, Ozgur Agdogan1, Sevdegul Mungan2, Etem Alhan3
& Naci Karacal1
1 Department of Plastic and Reconstructive Surgery, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey2 Department of Pathology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey3 Department of General Surgery, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey
Key words
Dressing; Full-thickness cutaneous wounds;Split-thickness skin graft donor site
Correspondence to
M Uraloglu, MD, Karadeniz TeknikUniversitesi Tip Fakultesi, Farabi HastanesiPlastik Cerrahi Anabilim Dali, Trabzon61080, TurkeyE-mail: [email protected]
doi: 10.1111/j.1742-481X.2012.01071.x
Uraloglu M, Livaoglu M, Agdogan O, Mungan S, Alhan E, Karacal N. An evaluationof five different dressing materials on split-thickness skin graft donor site and full-thickness cutaneous wounds: an experimental study. Int Wound J 2014; 11:85–92
Abstract
The objective of this study was to investigate the healing effect of five differentproducts on split-thickness skin graft (STSG) donor sites and full-thickness cutaneouswounds (FTCWs) using an occlusive dressing model. Six groups were included:1 control and 5 experimental groups, with a total of 24 rats, using an occlusivedressing model. STSG donor sites and FTCWs were established in two separateareas, to the right and left on the animals’ backs. Wound sites were dressedwith one of the following materials: fine mesh gauze, microporous polysaccharidehemosphere (MPH), clinoptilolite, alginate, hydrogel or biosynthetic wound dressing(Biobran®). These materials were compared in terms of healing rate, healing qualityand histopathological findings. Occlusive dressings were applied to each wound ondays 0, 3, 5, 7, 10 and 14. Area measurements were taken using images of eachdressing. The alginate and clinoptilolite groups gave the best healing rate results forboth STSG donor sites (P = 0·003) and FTCWs (P = 0·003). MPH came third ineach group. The alginate group produced better results in terms of healing qualitycriteria, followed by hydrogel, MPH, clinoptilolite and Biobran®, in that order.Statistically significant results were obtained in all groups compared to the controlgroup (P < 0·0007). Rapid and good healing quality for both the STSG donor sitesand FTCWs were obtained with alginate. Healing with clinoptilolite and MPH wasrapid, but poor quality, while slower but good healing quality was obtained withhydrogel. Slower and worse quality healing was obtained with Biobran®.
Introduction
As the donor site represents a new defect following the har-vesting of a thin skin graft, it leads to morbidity and there-fore requires good wound care (1). Dressings must protectthe wound and accelerate healing, extend changing intervals,reduce the risk of local and systemic infection and pain andalso be cost-effective and non-allergic (1–4).
Wound dressings may be non-occlusive, semi-occlusive orocclusive (3). Semi-occlusive and occlusive dressings sup-port re-epithelialisation, reduce pain and healing time andabsorb blood and tissue fluids, and prevent fluid loss and
Key Messages
• new dressing materials are developed with the reinforce-ment of advanced technology, and these products areintended to further contribute to management of cuta-neous wounds
• dressing is one of the fundamental steps in frequentlypracticed procedures in plastic surgery
mechanical trauma and exogenous contamination (4). Themain semi-occlusive and occlusive dressing materials are
© 2012 The AuthorsInternational Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd 85
An evaluation of five different dressing materials M. Uraloglu et al.
paraffin gauze, alginates and hydrocolloid, foam and hydrofi-bre dressings (4,5).
We selected products with different properties from differ-ent groups capable of use in split-thickness skin graft (STSG)donor sites and full-thickness cutaneous wounds (FTCWs).Microporous polysaccharide hemosphere (MPH), clinoptilo-lite and alginate are used as haemostatic dressing materials invascular surgery in the literature (1,6,7), but their effects onwound healing have not been comprehensively studied before.
This experimental study was designed in order to evalu-ate MPH, clinoptilolite, alginate, hydrogel and Biobrane® inSTSG donor sites and FTCWs.
Materials and methods
The study was approved by local Ethics Committee. Twenty-four female Sprague-Dawley rats weighing 250–300 g wereused. These were housed in rooms maintained at 21 ± 1◦C andin a 12:12 light : dark cycle. Animals were fasted overnightbefore the experiment, but had free access to water. Carewas provided in accordance with Ethics Committee guidance.One control group and five experimental groups were planned.Four rats with two wound sites each were examined for STSGdonor sites and FTCW groups for each product:
1. fine mesh gauze (control group);2. MPH (Traumadex®, Medafor, Inc., Minneapolis, MN);3. clinoptilolite (Froximun®, Froximun AG, Schlanst-
edt, Germany);4. alginate (Kaltostat®, ConvaTec, Princeton, NJ);5. hydrogel (Elastogel®, Southwest Technologies Inc., N.
Kansas City, Kansas);6. biosynthetic wound dressing (Biobrane®, Bertek Phar-
maceuticals Inc., Morgantown, WV).
General anaesthesia was administered with intraperitoneal50 mg/kg ketamine and 10 mg/kg xylazine. Areas of 2 cm ×6 cm in size were shaved on the right and left of the back. Thecentral, healthy area was left untouched, the two areas to theright and left being investigated. The dorsum was disinfected,and STSG sites 4 cm × 2 cm in size were obtained from thetwo sites using a hand dermatome and had the same thickness(0·2 mm) (8) (Hand Dermatome, Aesculap, Germany). Abilateral 1·0-cm2 area of skin and panniculus carnosus wasexcised in the caudal direction, creating a full-thickness dorsalexcisional wound (9) (Figure 1).
Isotonic-saline-embedded tie-over dressings were appliedto the control and experimental groups using wound-careproducts on days 0, 3, 5, 7, 10 and 14 for each group and allbilateral dorsal wound areas. New closed dressings with theappropriate group materials were applied on each specifiedday to the eight STSG donor sites and eight FTCW sites.Images of every dressing, taken from the same distances(Figures 2 and 3), were loaded onto the Image J (1.42q, WayneRasband National Institutes of Health, Bethesda, Maryland)program, and donor and FTCW sites were measured. All ratswere euthanised by cervical dislocation.
The dressing materials were compared according to thefollowing criteria:
Figure 1 Sites for dressing were established. Split-thickness skin graft(STSG) donor site and full-thickness cutaneous wound (FTCW) extendingto the cephalic area from the cranial on the right and the left.
Figure 2 Appearance on the third day after dressing.
© 2012 The Authors86 International Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd
M. Uraloglu et al. An evaluation of five different dressing materials
Figure 3 Appearance on the tenth day.
1. Healing rate: Level of sites with no epithelialisationover time.
2. Healing quality: Vascularity (10), clinical findings ofinfection, erythema, induration, purulent dischargeor unpleasant odour and fibrinous wound appear-ance (5,11).
3. Histopathological findings: Masson Trichrome andhaematoxylin-eosin stains were applied in each group.
Vascularity was evaluated using orthogonal polarisationspectral (OPS) imaging (12–14). Donor sites and FTCWswere examined on dressing day 10. The OPS video micro-scope (Cytoscan A/R, Cytometrics, Philadelphia, PA) wasattached to a moveable shaft and microcirculation wasrecorded over at least 20 seconds (Figure 4). Images werestored in AVI format on the computer (Sony VGN-FW230J/H). Video sequences were performed for each and trans-ferred from the OPS imaging device to computer software(CapiScope®; Lekam Medical Ltd., Devon, UK) for furtherevaluation. The required measurements (functional capillarydensity) were performed using this software (12). Functionalcapillary density (FCD) was defined as the length of red bloodcell-perfused capillaries (cm) per observation area (cm2). Wethus selected FCD as the parameter for measuring the micro-circulation.
Macroscopic appearance of wounds was scored by sixblinded members of the staff (four assistant professors andtwo residents) from the plastic surgery unit that participated
Figure 4 Cytoscan probe fixed by a mechanical device on the dorsalpart of the animal.
in the application of the five materials studied (from 0, aninfected, fibrinous wound, to 10, a clean wound appearance).
Statistical analysis
Group comparisons for each time point were performed usingKruskal–Wallis analysis of variance (post hoc Bonferroni cor-rected Mann–Whitney U -test).
Results
MPH, a material with a granular structure, was statisticallysignificantly better in donor site and FTCW healing rate com-pared to the control group, the best result after the alginate andclinoptilolite groups. FCD values were at the highest level inFTCW dressings and were statistically significant. Histopatho-logically, there were greater inflammation, collagen formationand fibroblast proliferation. Foreign body reaction and giantcells were also observed (Figure 5). Macroscopically, it wasone of the three groups with the highest wound appearancescores.
Clinoptilolite, with a granular structure, gave statisticallysignificant good results in donor site healing. It exhibited thebest performance in the FTCW site, and the defect dimensionwas significantly better compared to the control group onday 14. It represented the group with the best macroscopicwound appearance. Microscopically, inflammation was low
© 2012 The AuthorsInternational Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd 87
An evaluation of five different dressing materials M. Uraloglu et al.
Figure 5 Microporous polysaccharide hemosphere (MPH): Fibrosisin the papillary and deep dermis and mild chronic inflammation(Histochemistry, Trikrom ×100).
Figure 6 Clinoptilolite: Foreign body reaction in the dermis andphagocytosis of foreign body multinuclear giant cells [haematoxylin-eosin (H&E) ×40].
but collagen formation and fibroblast proliferation were high(Figure 6). Multinuclear giant cells were more pronouncedcompared to those of MPH group. It was one of the groupswith the lowest FCD values.
Microscopically, inflammation, collagen formation andfibroblast proliferation were low (Figure 7) with alginate,which represented one of the best groups, especially for re-epithelialisation. Macroscopically, it provided a clean woundappearance. FCD values were lower than those of the clinop-tilolite group, one of the best performing groups.
The result of hydrogel in donor site dressing was signifi-cant on day 10, but it did not exhibit a good performance inFTCW. No expansion in FTCW was observed on the first day.Macroscopically, the wound had a fibrous, moist appearance.Microscopically, inflammation, collagen formation and fibro-sis were lower compared to the other groups (Figure 8).
Figure 7 Alginate: Minimal increase in fibroblastic activity can be seen(Histochemistry, Trikrom ×100).
Figure 8 Hydrogel: Complete surface re-epithelialisation, fibrosis in thedermis and mild chronic inflammation [haematoxylin-eosin (H&E) ×100].
Biobrane® exhibited the worst performance in terms ofhealing rate. At donor site FCD investigation, the lowest valuewas obtained in this group and this was statistically signif-icant, despite a fibrinous wound appearance. Infection wasobserved in two sites in the Biobrane® group. Staphylococcusaureus grew in the wound cultures taken for microbiologicalexamination. Microscopically, collagen tissue and inflamma-tion were higher in this group (Figure 9).
Healing rate
At investigation of the STSG donor site, statistically sig-nificant faster healing compared to the control group wasobserved on the fifth day in the alginate and clinoptilolitegroups (P < 0·0005) and on the seventh and tenth days inthe alginate, clinoptilolite and MPH groups (P < 0·0005,P = 0·003) (Table 1, Figure 10).
© 2012 The Authors88 International Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd
M. Uraloglu et al. An evaluation of five different dressing materials
Figure 9 Biobran®: Mild hyperkeratosis in the epidermis, rete elonga-tion, increased fibrosis in the dermis and severe chronic inflammatorycell infiltration [Haematoxylin-Eosin (H&E) ×100].
In the FTCW site, statistically significantly rapid healingwas observed on the 7th day in the alginate group (P = 0·001)and on the 14th day in the alginate and clinoptilolite groups(P = 0·003) (Table 2, Figure 11). Statisticaly significant heal-ing was obtained in all groups compared to the control group(P < 0·0007).
Healing quality
FCD measurements in the donor site using OPS imag-ing were statistically significantly low in the Biobrane®
group (P = 0·011). In the FTCWs, significantly high FCD
Figure 10 Comparison of the healing rates in the split-thickness skingraft (STSG) donor areas. Traumadex® (microporous polysaccharidehemosphere, MPH); Froximun® (clinoptilolite); Kaltostat® (alginate);Elastogel® (hydrogel); Biobrane® (biosynthetic wound dressing). (*)Statistically significant results in the MPH, clinoptilolite and alginategroups on days 7 and 10.
values were determined in the MPH group (P = 0·041)(Table 3).
Macroscopically, wounds had a cleaner and better healingappearance in the alginate, clinoptilolite and MPH groupscompared to the control group. Wounds in the Biobrane®
and hydrogel groups were worse, more fibrinous and had anunclean appearance. The differences were not statistically sig-nificant (Table 3).
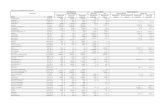
Table 1 STSG donor site area measurements (mm2): results of comparison between groups*
Day 0 Day 3 Day 5 Day 7 Day 10
Fine mesh gauze 274·7 ± 83·8 179 ± 70·5 121·5 ± 23 72·5 ± 17·5 12·2 ± 14·3MPH 316·8 ± 90·1 224·8 ± 71·5 84·5 ± 24·6 21·8 ± 25·2 0
Clinoptilolite 300·8 ± 110 173·4 ± 84·5 58·2 ± 22·4 8·6 ± 18 0
Alginate 346·9 ± 57·2 126·4 ± 26·4 9 ± 11 3·4 ± 6·1 0
Hydrogel 331·4 ± 151 282 ± 155·9 175·2 ± 55·5 89·3 ± 47·4 11·3 ± 3·2Biobrane® 289·2 ± 59·4 188·5 ± 60·5 128·5 ± 40·1 85·5 ± 61·5 53·5 ± 53
P = 0·443 P < 0·0005 P < 0·0005 P = 0·003
MPH, microporous polysaccharide hemosphere; STSG, split-thickness skin graft.∗Statistical significance was obtained for eight measures, and the values are expressed in bold.
Table 2 Full-thickness cutaneous wound (mm2) measurements by day*
Day 0 Day 3 Day 5 Day 7 Day 10 Day 14
Fine mesh gauze 97·1 ± 15·1 97 ± 23 86·1 ± 26·2 103·5 ± 18·4 73·3 ± 45·4 35·8 ± 35·3MPH 107·4 ± 19·3 95·6 ± 15·5 85·4 ± 14·3 78·5 ± 9·7 42·6 ± 12·1 18·1 ± 7·7Clinoptilolite 105·7 ± 14·9 88·7 ± 25 81·9 ± 28·6 78·6 ± 30·5 42 ± 23·1 5·6 ± 6·2Alginate 111 ± 12·5 – 82·4 ± 12·5 70 ± 10·8 33·9 ± 7.8 12·8 ± 10·6Hydrogel 106·3 ± 12 147·6 ± 45·1 140·7 ± 39·8 137 ± 25·1 84·5 ± 90 36·1 ± 54·7Biobrane® 93·5 ± 5·9 97·8 ± 30·2 76·8 ± 21·8 58·1 ± 19·7 39·1 ± 11·4 26·5 ± 12·1
P = 0·146 P = 0·088 P = 0·001 P = 0·325 P = 0·003
MPH, microporous polysaccharide hemosphere.∗Statistical significance was obtained for three measures, and the values are expressed in bold.
© 2012 The AuthorsInternational Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd 89
An evaluation of five different dressing materials M. Uraloglu et al.
Figure 11 Comparison of the healing rates in the full-thickness cuta-neous wound (FTCW) sites. Traumadex® (microporous polysaccharidehemosphere, MPH); Froximun® (clinoptilolite); Kaltostat® (alginate);Elastogel® (hydrogel); Biobrane® (biosynthetic wound dressing). (*) Sig-nificant results in the clinoptilolite and alginate groups on day 14.
Histopathological findings
Inflammation was lower in the alginate, clinoptilolite andhydrogel groups in particular and higher in the MPH andBiobran® groups.
Fibroblast proliferation, collagen formation and granulationtissue were greater in the MPH, clinoptilolite and Biobran®
groups. Foreign body reaction and multinuclear giant cellswere observed in the MPH group. More pronounced phagocy-tosis of foreign body multinuclear giant cells was observed inthe clinoptilolite group compared to the MPH group. Fibroticparameters were particularly lower in the alginate group.
Re-epithelialisation was better in the alginate, MPH andhydrogel groups. Neovascularisation was at similar levels inall groups.
Discussion
Dressing materials are mainly classified as occlusive, semi-occlusive or non-occlusive and include a broad spectrum ofchemical and physical structures (3). The first two providethe best protection against dehydration, contamination andmechanical trauma, which therefore facilitates healing. Theuse of occlusive or semi-occlusive dressings, which providea moist environment, is known to lead to earlier completionof epithelialisation (15–18). Wound healing is a complex pro-cess in which inflammation, formation of granulation tissue,production of new structures and tissue remodelling all play apart. Inadequate angiogenesis, epithelial migration and woundcontraction can all make wound healing problematic (16).
The active material in MPH is polysaccharide, which canbe absorbed in powder form. MPH is a new-generation,
absorbable, powder-like haemostatic agent. MPH is madefrom plant starch. The microspheres it contains serve asabsorbers for fluid and for small molecular components ofblood. It concentrates the larger particles within the site ofthe activity through dehydration, and subsequently acceleratesfibrin mesh formation. Research has shown that it is safe andefficacious in several tissues (19,20). However, there are nostudies evaluating MPH in dressing materials.
Clinoptilolite is manufactured using nanotechnology and ismade up of three-dimensional frames containing clinoptilo-lite silicate and aluminium tetrahedron. It contains hydratednatural micropores and 8–10-ring crystals. It is 100% non-toxic. It has positive or negative biological activity and maybe hydrated or dehydrated. Clinoptilolite serves the purposeof a cage, the molecule making it possible to capture variousions and compounds. Clinoptilolite powder exhibits antiviral,antibacterial, antifungal and absorbent properties (7,21). Zeo-lite is a naturally occurring mineral. It absorbs water fromthe wound site in an exothermic reaction that enhances theconcentration of coagulation factors and platelets and thusincreases clot formation (21). Some success in treating humanwounds has been reported from the use of these agents in thefield. According to this study, it has no negative effects onhealing.
MPH and clinoptilolite are materials with a granular struc-ture. Histopathological examination showed more multinu-clear giant cells in the clinoptilolite group in particular,because of phagocytosis by macrophages. Although MPH isabsorbable, irrigation with saline solution should be performedon every dressing when these products are used. Clinoptilolitebeing non-absorbable may be regarded as a disadvantage.
The main advantage of alginate is that it can absorbexcess fluid, but still maintain a moist wound environment.It has also been reported that it acts as a haemostatic agentfollowing release of calcium ions essential for the clot-ting cascade, and that it establishes a gel–fibre matrix thatfacilitates clotting and permits the dressing to be removedin a trauma-free manner (22). Among its advantages areease of application, maintenance of a moist wound envi-ronment, potential haemostatic properties, and excess woundfluid absorption. Alginate is not an antimicrobial dressing,although it may assist with reducing the possibility of infec-tion because it contains considerable quantities of exudateand traps micro-organisms and cell debris in the gel–fibrematrix (23,24).
Hydrogel consists of 95% water, meaning that it cannotabsorb excess water and is therefore suitable for dry woundsor those with minimal drainage. It does not adhere to thewound, and cools the skin surface to 5◦, subsequently main-taining that low temperature. These effects reduce inflamma-tory response (25). Hydrogel is suitable for first- and second-degree burns, grade 1 and 2 bed sores, superficial epithe-lium defects, skin abrasions and fine-thickness graft donorsites (1,26).
Biobrane® is a biosynthetic wound dressing that consistsof a silicone film with a nylon mesh embedded into thefilm (27). This mesh is covered by a layer of porcine collagenwhich attaches the dressing to the wound and facilitatesepithelialisation.
© 2012 The Authors90 International Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd
M. Uraloglu et al. An evaluation of five different dressing materials
Table 3 FCD values measured using OPS for skin graft donor sites and FTCW and other analyses*
FCD forFTCW
FCD for donorsite
Macroscopicappearance of
wounds
Incidenceof
infection
Microscopicinflammation
(H&E)
Microscopiccollagentissue
(Trichrome)
Fine mesh gauze 20·7 ± 6·6 29·6 ± 4 6 (1·2) 0 + + + ++MPH 28·5 ± 3·2 27 ± 3·6 8·1 (0·8) 0 ++ + + +Clinoptilolite 26·2 ± 1·8 24·9 ± 3·7 8·9 (1·8) 0 + + + +Alginate 20·8 ± 6·6 23·8 ± 8·2 8·3 (0·7) 0 + +Hydrogel 23·5 ± 5·4 30·8 ± 3·2 7·3 (1·3) 0 + ++Biobrane® 19 ± 2·9 23·1 ± 3·6 5·2 (1·4) 2/8 + + + + + +
P = 0·041 P = 0·011 P = 0·098
FCD, functional capillary density; FTCW, full-thickness cutaneous wounds; H&E, haematoxylin-eosin; MPH, microporous polysaccharide hemosphere;OPS, orthogonal polarisation spectral.∗Statistical significance was obtained for three measures, and are expressed in bold.
Studies have shown that Biobrane® is an effective andlow-trauma dressing for children with superficial partial-thickness burns, and that it does involve increased outpatientburn-care costs (28). Infection rates as high as 10·7% havebeen reported; however, levels of scarring for infected areaswere not significantly worse than the levels for non-infectedburns (29). Other studies have reported no rises in infectionin partial-thickness burns dressed with Biobrane in childrenof all ages (30). In our study, no infection was observed inany site or group, although infection was seen in two FTCWsites in the Biobrane® group.
The use of orthogonal polarisation imaging has been recom-mended for recording and quantifying changes in the micro-circulation (12). OPS (11–13) imaging has been used fornon-invasive real-time observation of functional microvascu-lar networks. Arterioles, venules and capillaries can be directlyvisualised, and the movement of individual blood cells throughthem can be observed. The technique uses optical filtration ofpolarised light that is absorbed by haemoglobin so that redblood cells appear dark. FCD, identified as the best parame-ter for the measurement of the microcirculation, was definedby Messmer (12). Elevated FCD in the early period maybe regarded as a positive characteristic in terms of healingspeed, but negative in terms of healing quality in the latestage.
We examined wound closure in rats after the application ofsix different dressing materials. Our aim was to investigate theeffect of an occlusive dressing model, frequently employed inplastic surgery departments, on STSG donor site and FTCWsite healing.
The alginate and clinoptilolite groups gave the best resultsfor both donor site and FTCW. MPH followed in third placefor both groups. There are no previous studies regardingthe effect of MPH, clinoptilolite and alginate on woundhealing. This study evaluated their effects on wound healing.Alginate provided rapid and good-quality healing. Rapidbut lower-quality healing was obtained with clinoptiloliteand MPH, while healing with hydrogel was slower, but ofbetter quality. Slower and lower-quality healing was obtainedwith Biobran®. However, healing in both wound types wasevaluated as successful in all groups compared to the controlgroup.
Acknowledgements
All the authors state that they have no financial or personalrelationship with any of the companies mentioned in the text.Authors have indicated no significant interest with commercialsupporters.
References
1. Voineskos SH, Ayeni OA, McKnight L, Thoma A. Systematicreview of skin graft donor-site dressings. Plast Reconstr Surg2009;124:298–306.
2. Birdsell DC, Hein KS, Lindsay RL. The theoretically ideal donor sitedressing. Ann Plast Surg 1979;2:535–7.
3. Kilinc H, Sensoz O, Ozdemir R, Unlu RE, Baran C. Which dress-ing for split-thickness skin graft donor sites? Ann Plast Surg2001;46:409–14.
4. Chaby G, Senet P, Vaneau M, Martel P, Guillaume JC, MeaumeS, Teot L, Debure C, Dompmartin A, Bachelet H, Carsin H, MatzV, Richard JL, Rochet JM, Sales-Aussias N, Zagnoli A, Denis C,Guillot B, Chosidow O. Dressings for acute and chronic wounds: asystematic review. Arch Dermatol 2007;143:1297–304.
5. Demirtas Y, Yagmur C, Soylemez F, Ozturk N, Demir A. Manage-ment of split-thickness skin graft donor site: a prospective clini-cal trial for comparison of five different dressing materials. Burns2010;36:999–1005.
6. Waragai T, Morgan G, Ralston T, Chaturvedi R, Lee KJ, Ben-son L. Hemostatic agent microporous polysaccharide hemospheres(MPH) does not affect healing or intact sinus mucosa. Laryngoscope2008;118:1265–9.
7. Kozen BG, Kircher SJ, Henao J, Godinez FS, Johnson AS. Analternative hemostatic dressing: comparison of CELOX, HemCon,and QuikClot. Acad Emerg Med 2008;15:74–81.
8. Gustavson EH. A simple aid to taking split-thickness skin grafts insmall experimental animals. Br J Plast Surg 1974;27:165–6.
9. Li Q, Kao H, Matros E, Peng C, Murphy GF, Guo L. Pulsedradiofrequency energy accelerates wound healing in diabetic mice.Plast Reconstr Surg 2011;127:2255–62.
10. Rennekampff HO, Rabbels J, Reinhard V, Becker ST, Schaller HE.Comparing the Vancouver Scar Scale with the cutometer in theassessment of donor site wounds treated with various dressings ina randomized trial. J Burn Care Res 2006;27:345–51.
11. Bergmann J, Hackl F, Koyama T, Aflaki P, Smith CA, RobsonMC, Eriksson E. The effect of amnion-derived cellular cytokinesolution on the epithelialization of partial-thickness donor sitewounds in normal and streptozotocin-induced diabetic swine. Eplasty2009;9:449–59.
© 2012 The AuthorsInternational Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd 91
An evaluation of five different dressing materials M. Uraloglu et al.
12. von Dobschuetz E, Biberthaler P, Mussack T, Langer S, MessmerK, Hoffmann T. Noninvasive in vivo assessment of the pancreaticmicrocirculation: orthogonal polarization spectral imaging. Pancreas2003;26:139–143.
13. Olivier WA, Hazen A, Levine JP, Soltanian H, Chung S, GurtnerGC. Reliable assessment of skin flap viability using orthogonalpolarization imaging. Plast Reconstr Surg 2003;112:547–55.
14. Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Mess-mer K, Nadeau RG. Orthogonal polarization spectral imaging: anew method for study of the microcirculation. Nat Med 1999;5:1209–12.
15. Field FK, Kerstein MD. Overview of wound healing in a moistenvironment. Am J Surg 1994;167:2S–6S.
16. Wang JF, Olson ME, Reno CR, Kulyk W, Wright JB, Hart DA.Molecular and cell biology of skin wound healing in a pig model.Connect Tissue Res 2000;41:195–211.
17. Barnea Y, Amir A, Leshem D, Zaretski A, Weiss J, Shafir R, GurE. Clinical comparative study of aquacel and paraffin gauze dressingfor split-skin donor site treatment. Ann Plast Surg 2004;53:132–6.
18. Nemeth AJ, Eaglstein WH, Taylor JR, Peerson LJ, Falanga V. Fasterhealing and less pain in skin biopsy sites treated with an occlusivedressing. Arch Dermatol 1991;127:1679–85.
19. Antisdel JL, Janney CG, Long JP, Sindwani R. Hemostatic agentmicroporous polysaccharide hemospheres (MPH) does not affecthealing or intact sinus mucosa. Laryngoscope 2008;118:1265–9.
20. Ereth M, Sibonga J, Oliver W, Nuttall G, Henderson J, DekutoskiM. Microporous polysaccharide hemospheres do not inhibit bonehealing compared to bone wax or microfibrillar collagen. Orthopedics2008;31:222.
21. Recinos G, Inaba K, Dubose J, Demetriades D, Rhee P. Local andsystemic hemostatics in trauma: a review. Ulus Travma Acil CerrahiDerg 2008;14:175–81. Review.
22. Blair SD, Jarvis P, Salmon M, McCollum C. Clinical trial of calciumalginate haemostatic swabs. Br J Surg 1990;77:568–73.
23. Disa JJ, Alizadeh K, Smith JW, Hu Q, Cordeiro PG. Evaluation ofa combined calcium sodium alginate and bio-occlusive membranedressing in the management of split-thickness skin graft donor sites.Ann Plast Surg 2001;46:405–8.
24. Porter JM. A comparative investigation of re-epithelialization of splitskin graft donor areas after application of hydrocolloid and alginatedressings. Br J Plast Surg 1991;44:333–8.
25. Ozkan A, Tosun Z, Senturk S. Greft donor alanı bakımında hidrojelkullanımı. Turk Plast Rekonstr Est Derg 2005;13:28–31 (in Tukish).
26. Singh A, Halder S, Menon GR, Chumber S, Misra MC, SharmaLK, Srivastava A. Meta-analysis of randomized controlled trials onhydrocolloid occlusive dressing versus conventional gauze dressingin the healing of chronic wounds. Asian J Surg 2004;27:326–32.
27. Demling RH. Use of Biobrane in management of scalds. J Burn CareRehabil 1995;16:329–30.
28. Lang EM, Eiberg CA, Brandis M, Stark GB. Biobrane in thetreatment of burn and scald injuries in children. Ann Plast Surg2005;55:485–9.
29. Ahmadi H, Williams G. Permanent scarring in a partial thicknessscald burn dressed with Biobrane. J Plast Reconstr Aesthet Surg2009;62:697–82.
30. Lal S, Barrow RE, Wolf SE, Chinkes DL, Hart DW, Heggers JP,Herndon DN. Biobrane improves wound healing in burned childrenwithout increased risk of infection. Conn Med 1995;59:523–9.
© 2012 The Authors92 International Wound Journal © 2012 Medicalhelplines.com Inc and John Wiley & Sons Ltd